Abstract
Background
Time to treatment is critical for survival from sudden cardiac arrest. Every minute delay in defibrillation results in a 7% to 10% reduction in survival. This is particularly problematic in rural and remote regions, where emergency medical service response is prolonged and automated external defibrillators (AEDs) are often not available. Our primary objective was to examine the feasibility of a novel AED drone delivery method for rural and remote sudden cardiac arrest. A secondary objective was to compare response times between AED drone delivery and ambulance to mock sudden cardiac arrest resuscitations.
Methods and Results
We conducted 6 simulations in 2 rural communities in southern Ontario, Canada. In the first 2 simulations, the drone and ambulance were dispatched from the same paramedic base. In simulations 3 and 4, the drone and ambulance were dispatched from separate paramedic bases; and in simulations 5 and 6, the drone was dispatched from an optimized location. During each simulation, a “mock” call was placed to 911 and a single AED drone and an ambulance were simultaneously dispatched to a predetermined destination. On scene, trained first responders retrieved the AED from the drone and initiated resuscitative efforts on a mannequin until paramedics arrived. No difficulties were encountered during drone activation by dispatch, ascent, landing, or bystander retrieval of the AED from the drone. During simulations 1 and 2, the distance to the scene was 6.6 km. For simulations 3 and 4, the ambulance response distance increased to 8.8 km while drone remained at 6.6 km; and in simulations 5 and 6, the ambulance response distance was 20 km compared with 9 km for the drone. During each flight, the AED drone arrived on scene before the ambulance, between 1.8 and 8.0 minutes faster.
Conclusions
This study suggests AED drone delivery is feasible, with the potential for improvements in response time during simulated sudden cardiac arrest scenarios. Further research is required to determine the appropriate system configuration for AED drone delivery in an integrated emergency medical service system as well as optimal strategies to simplify bystander application of a drone‐delivered AED.
Keywords: automated external defibrillation, cardiopulmonary resuscitation, drones, emergency medical service, out‐of‐hospital cardiac arrest
Subject Categories: Cardiopulmonary Arrest, Sudden Cardiac Death, Health Services
Nonstandard Abbreviations and Acronyms
- AED
automated external defibrillator
- BVLOS
beyond visual line of sight
- EMS
emergency medical service
- OHCA
out‐of‐hospital cardiac arrest
Clinical Perspective
What Is New?
Previous research has demonstrated the potential for automated external defibrillator (AED) delivery by drones to decrease response time in out‐of‐hospital cardiac arrest.
In this Canadian study taking place in rural communities, we were able to demonstrate that drone delivery of AED was feasible and decreased response time in a simulated 911 emergency response using trained first responders.
What Are the Clinical Implications?
Survival from out‐of‐hospital cardiac arrest in rural and remote communities around the world remains strikingly low for a simple reason: we cannot get an AED to the patient fast enough with our current emergency medical service response.
The addition of drone technology to our standard 911 response provides the potential to decrease time to first shock in these communities, improving the odds of meaningful survival.
Further research is required to determine the appropriate system configuration for AED drone delivery in an integrated emergency medical service system as well as optimal strategies to simplify bystander application of a drone‐delivered AED.
Immediate high‐quality cardiopulmonary resuscitation and rapid defibrillation are the most important interventions when a patient collapses from sudden cardiac arrest.1, 2 However, bystander use of public automated external defibrillators (AEDs) during sudden cardiac arrest3, 4 is poor, at 2% to 3%. 3 Although increasing the number of public AEDs in the community is important, it may be insufficient to significantly improve bystander use as the location of cardiac arrests is often unpredictable, and the vast majority of cases occur in private residences. 4 Ensuring an AED is available when someone experiences a cardiac arrest is challenging. These challenges are magnified in remote and rural areas, where population density is low and emergency medical service (EMS) response times are long. Survival from cardiac arrest in these locations continues to be poor. 5 , 6 , 7 , 8 New models for early defibrillation must be considered to address these challenges.
Advances in technology have changed the way we view health and healthcare delivery. One example is the use of drones, otherwise known as unmanned aerial vehicles. Drone technology has improved vastly over the past decade, making their use feasible in a variety of situations, including the delivery of merchandise, 9 legal documents, 10 and medicine. 11 Drones have further been proposed to deliver AEDs to the scene of a cardiac arrest, 12 , 13 and although some technical challenges need to be addressed, drone‐delivered AEDs are a potential transformative innovation in the provision of emergency care to patients experiencing cardiac arrest, especially in rural and remote settings.
There is an emerging body of evidence that supports the idea of timely, feasible AED drone delivery. Through use of mathematical modeling and system optimization, Boutilier et al 14 were able to demonstrate that a drone network could significantly reduce the time to AED arrival at the scene of a cardiac arrest by up to 10.6 minutes in rural regions. 14 Similarly, research performed in Salt Lake County, UT, 15 looked at the theoretical benefit of launching drones from each EMS station to both urban and rural sudden cardiac arrests. They found a theoretical increase in AED delivery to the scene within 1 minute of call to 911 from 4.3% to 80% if a drone was launched from each EMS station. Although promising, these studies involved the use of theoretical models and there is limited evidence involving actual drone flights. Claesson et al 16 found a significant reduction in response times with drone delivery of AEDs during simulated cardiac arrest to locations with physical barriers to ambulance response (eg, fjords). There are no studies that examine the use of drone delivery of AEDs in rural or remote locations.
The objective of this study was to examine the feasibility of integrating drone‐delivered AEDs into a 911 response system and determine the time to AED application during simulated cardiac arrest scenarios. Our hypothesis was that drone delivery of AEDs would be feasible and result in faster AED delivery than paramedic response.
Methods
This was a feasibility study of simulated AED drone response to sudden cardiac arrest. Our primary outcome of interest was to determine the feasibility of using AED drone delivery during simulated cardiac arrest. Our feasibility outcome included receiving appropriate regulatory approval from Transport Canada to allow for flights to take place and examining barriers to ascent, flight using “beyond visual line of sight (BVLOS)” technology, landing the drone at the scene, and bystander retrieval of the AED from the drone. We examined feasibility using 2 distinct systems. First, drones and ambulances were dispatched from paramedic bases with the use of a command team dedicated to the drone response. The second system involved the drone being dispatched from a location to optimize the drone response and was controlled by a paramedic‐led team. Our secondary outcome was to compare the response times between the drone and the ambulance.
All times were manually recorded throughout the simulations, including the time of drone and ambulance dispatch, the time of drone and ambulance arrival, time required to remove the AED from the drone, and time to application of the AED to the mock cardiac arrest victim. Distances traveled by drone and ambulance were also recorded. Data from this research will not be made available beyond what is printed in the article for future research.
Setting
We conducted the study in 2 distinct rural communities (Town of Caledon and County of Renfrew) in Ontario, Canada. The Town of Caledon has a total population of 66 502 and spans an area of 378.6 km (175.7 population per km2). Renfrew County has a total population of 88 512 and spans an area of 7419 km (11.9 population per km2). Each community is covered by a single municipally run ambulance service. In Ontario, Canada, each region is covered by a paramedic service that is run by the city or the municipal government. The distribution of ambulance bases within these settings is typical of ambulance coverage across North America, situated to optimize response times within the region.
Drone and AED Description
We used the Sparrow X1000 drone (Drone Delivery Canada, Toronto, Canada) for flights in the Town of Caledon and the InDro M210C drone (Indro Robotics, Salt Spring Island, British Columbia, Canada) for flights in the County of Renfrew (Figure 1). The Sparrow X1000 drone has a maximum speed of 80 km/h, with a flight range of 25 km. It has a maximum flight altitude of 900 m (≈3000 ft) with a maximum payload of 4.5 kg. The InDro M210C drone has a maximum speed of 55 km/h, with a flight range of 25 km. It has a maximum flight altitude of 1000 m and a maximum payload of 4.0 kg.
Figure 1. Sparrow X1000 drone (Town of Caledon) and Indro Robotics M210C drone (County of Renfrew).

A, Sparrow X1000 drone (picture courtesy of Drone Delivery Canada). B, M210 C drone. Picture courtesy of Indro Robotics.
The AED used for each flight differed on the basis of the size of each drone. The Zoll AED3 (Zoll Medical, Chelmsford, MA) was carried in the Sparrow X1000 drone. The AED has dimensions (height×width×depth) of 12.7×23.6×24.7 cm and a weight of 2.5 kg (battery included) and was carried within the payload portion of the drone. The FRED Easyport AED (Schiller AE, Baar, Switzerland) was carried in the InDro M210C drone. The AED has dimensions (height×width×depth) of 3.5×12.6×13.3 cm and a weight of 490 g and was carried via a holding mechanism external to the drone. Both AEDs are shown in Figure 2.
Figure 2. Automated external defibrillators used during feasibility flights.
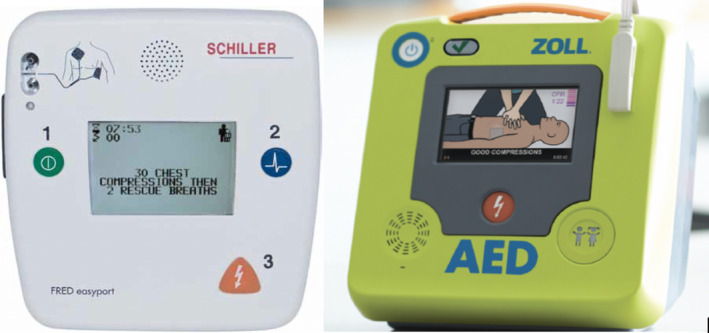
Schiller FRED Easyport defibrillator (left) and Zoll AED3 defibrillator (right). Pictures courtesy of Schiller and Zoll Medical.
BVLOS Flight and Drone Command During Testing
Drones were operated using BVLOS technology during the simulated responses. BVLOS flight of a drone is defined as “an operation in which no crew member maintains unaided visual contact with the aircraft sufficient to be able to maintain control of the aircraft and know its location.” 17 The flight of drones using BVLOS technology differs significantly from visual line of sight drones (defined as “unaided visual contact with the drone sufficient to be able to maintain operational control of the aircraft, know its location, and be able to scan the airspace in which it is operating to decisively see and avoid other air traffic or objects”) 17 often used for recreational purposes. Details of the differences between BVLOS and visual line of sight are summarized in Table 1.
Table 1.
Differences Between BVLOS and VLOS Drones
| Parameter | VLOS Drone | BVLOS Drone |
|---|---|---|
| Visualize | Must be within line of sight of user | UAV monitored remotely |
| Altitude | 15–90 m | 90–900 m |
| Weather conditions | Must be able to see unaided | Below the cloud line |
| Payload | 2.25 kg | ≥13.75 kg |
| Air speed | 50 km/h | 120 km/h |
| Range | 500 m maximum | 15–100 km |
| Useful for AED transport | No | Yes |
| Navigation | Manual/semiautomated | Fully automated |
| Advanced technologies required | None | “Sense and avoid” and “detect and avoid” |
AED indicates automated external defibrillator; BVLOS, beyond VLOS; UAV, unmanned aerial vehicle; and VLOS, visual line of sight.
Drone command during flights differed between the 2 communities. Flights taking place in the Town of Caledon were monitored remotely by Drone Delivery Canada using FLYTE technology, allowing control of the drone over a large area from a remote flight command. Flights taking place in Renfrew County were monitored by a paramedic‐led drone command system that was available in their ambulance. Both systems used global positioning system tracking as well as multiple communication techniques to ensure knowledge of the position of the drone at all times. Oversight by Transport Canada was facilitated through visual observers (Town of Caledon) or occurred through the use of a special flight operations certificate, allowing the use of drones under specific conditions (County of Renfrew).
Description of Simulated Emergency Responses
The first 4 test flights took place in the Town of Caledon. During the first 2 flights, the drone and ambulance were dispatched from the same paramedic station. During the second 2 flights, the ambulance and drone were dispatched from 2 distinct paramedic stations, which added 2.2 km to the ambulance response. During each flight, a simulated 911 call was placed to a dispatcher, who simultaneously dispatched the ambulance response vehicle and the drone. During the simulated responses, the paramedic was instructed to take the most direct route to the location of the call while obeying all traffic laws. As this was a simulated 911 call, the ambulance did not use lights and sirens during the response. The coordinates of the emergency call were provided to the drone team from the dispatcher, who then programmed the most direct route to the call. At the scene of the simulated out‐of‐hospital cardiac arrest (OHCA), there were 2 off‐duty trained 911 first responders (a firefighter and a paramedic) who performed cardiopulmonary resuscitation on a mannequin until arrival of the ambulance. When the drone landed, one of the responders removed the AED from the drone and incorporated it into the resuscitation effort. Neither responder had any previous training specific to this scenario with the drone. The drone landed in an area on the opposite side of a parking lot from where the simulated cardiac arrest occurred (≈90 ft away).
The last 2 simulated 911 responses occurred in the County of Renfrew. During these flights, the drone was simultaneously dispatched from a location that optimized the drone response to cardiac arrest within the region. This technique was used to account for the much larger size of the rural community than the first 4 test flights, and to establish a “real‐life” positioning of drone resources in a rural community used to optimize the drone response. We believed this technique would allow for maximal improvement in 911 response times with the use of an AED drone. During this phase of the project, the ambulance used lights and sirens during the simulated response.
Our primary outcome of interest was to examine any concerns with feasibility of dispatching drones during a 911 emergency response. We defined our feasibility outcomes as any barriers that we encountered that did not enable us to get the AED to the scene of the cardiac arrest. This included legislative barriers that would not allow us to fly the drones between our launch site and the scene of the call, issues that occurred during ascent, flight, or descent that prohibited the drone from landing on scene, and any barriers that did not allow the bystanders to retrieve the AED from the drone. Our secondary objective was to evaluate the difference in response times between the ambulance and the drone. Times were recorded manually throughout the simulations, including the time of ambulance and drone dispatch, the time of drone and ambulance arrival, and the time required to retrieve the AED from the drone and apply it to the mannequin. The distances traveled by the drone and ambulance were also recorded.
After reviewing the study protocol, the Research Ethics Board at the lead institution determined the study qualified for Research Ethics Board exemption on the basis of the Tri‐Council Policy Statement: Ethical Conduct for Research Involving Humans. 18
Results
We performed a total of 6 test flights during the study. The first 4 flights occurred on the same day in May 2019, whereas the last 2 flights occurred over a single day in November 2019. The weather on each of the flight days was clear, with no precipitation (snow or rain), low wind speed, and mild temperatures.
Overall, there were no feasibility concerns identified during drone takeoff, flight, or landing at the scene of the cardiac arrest. The drones were able to fly (BVLOS) and deliver the AED to the appropriate predetermined location using both methods of drone delivery. We identified that controlled decent of the drone slowed down the overall response and negated a portion of the improved response times of the drone. There were no safety concerns identified during the flights or landing of the drone and bystander retrieval of the AED. Responders were able to easily retrieve the AED from the drone and incorporate it into the simulated resuscitation.
During the first 2 flights (drone and ambulance dispatched from the same location), the distance traveled by the ambulance and the drone to the scene was 6.6 km. The response time to the scene for the drone was 5.8 minutes for both test flights. The ambulance response time was 7.6 and 7.5 minutes for flights 1 and 2, respectively.
During flights 3 and 4 (drone and ambulance dispatched from separate paramedic bases), the distance traveled by the drone remained 6.6 km; however, the distance traveled by the ambulance was 8.8 km. During the 2 simulated flights, the drone response was 6.7 and 6.3 minutes, whereas the ambulance response times were 11.1 and 8.4 minutes, respectively.
During the last 2 flights (drone dispatched from geographical location to optimize cardiac arrest response in the region), the distance traveled by ambulance to the scene was 20 km, whereas the drone response occurred from a distance of 8.8 km. During the 2 simulations, the response time for the drone was 13.0 and 11.0 minutes, whereas the response time for the ambulance was 20.0 and 19.0 minutes. In all our test flights, the drone was able to deliver the AED to the scene of the cardiac arrest before arrival of the ambulance. The AED was applied between 1.7 minutes (test flight 1) and 8.0 minutes (test flight 6) earlier when delivered via drone. The times and distances of each flight are reported in Table 2.
Table 2.
Ambulance and Drone Response Times During Each Test Flight
| Variable | Flight 1 | Flight 2 | Flight 3 | Flight 4 | Flight 5 | Flight 6 |
|---|---|---|---|---|---|---|
| EMS response time, min | 7.6 | 7.5 | 11.1 | 8.4 | 20.0 | 19.0 |
| Drone response time, min | 5.8 | 5.8 | 6.7 | 6.3 | 13.0 | 11.0 |
| EMS distance traveled, km | 6.6 | 6.6 | 8.8 | 8.8 | 20.0 | 20.0 |
| Drone distance traveled, km | 6.6 | 6.6 | 6.6 | 6.6 | 8.8 | 8.8 |
EMS indicates emergency medical service.
Discussion
Our study demonstrates that the use of drones to deliver AEDs is feasible as part of an integrated response to OHCA. We were able to perform all 6 test flights without any identified issues in terms of drone ascent, drone flight, or removal of the AED from the drone.
In all flights, the drone had a faster response time to the scene compared with the ambulance. The test results were consistent using 2 different drones carrying 2 different AEDs and 2 similar flight control systems, suggesting there may be multiple solutions available for differing rural and remote communities. Given the time‐dependent survival from time of collapse to first defibrillation, the response time savings noted in all test flights could conceivably result in shorter time to first defibrillation, which may ultimately improve survival from rural and remote OHCA. 19
To improve the time to defibrillation for cardiac arrest patients, it is important to explore novel methods of AED delivery, such as the use of drones. The versatility, speed, and ability to fly beyond line of sight make drones a promising option to improve timely access to AEDs during OHCA. Being able to fly beyond line of sight is an essential feature for the use of drones during a 911 response as this allows drones to be placed in locations that optimize the response to the scene without the requirement of having the operator close by. Although optimizing EMS response times is paramount for improving survival, 20 , 21 there is a lower limit for EMS response times in which it is not possible to improve beyond, and there are diminishing returns as response times approach this lower threshold. This issue is magnified in rural and remote regions, where it is not practical to reduce ambulance response times beyond a certain duration because of low call volumes and population density. As well, given the paucity of AEDs found in most rural communities, drone‐delivered AEDs may be the only viable method to provide early defibrillation in these communities.
There are several factors that must be considered when determining the utility of AED drone response, including the distance to the patient, traffic patterns, weather, and terrain. The location of drones in comparison to current emergency response resources is essential in determining the optimal response of drones and their use in the context of an organized 911 response. In our study, although the drone was faster than the ambulance response in all simulations, we found the largest improvements in response time when we dispatched drones from locations that optimized the drone response. This is consistent with previous research that has shown it is possible to use mathematical modeling to optimize drone response in several different settings. 14 , 22 The size of the drone used and the size of the payload carried may also impact decision making. As noted in our study, smaller drones may be appropriately used with smaller defibrillators, whereas larger AEDs may require larger drones to ensure optimum speed and travel distance. The utility of drone responses will be determined through a combination of these factors, which will ultimately impact the ability of the drone to improve response time to OHCA.
Our findings are similar to previous research examining the feasibility of AED drone delivery. A feasibility study by Claesson et al 16 compared the delivery of an AED using fully autonomous drones with EMS response times for simulated OHCA. The median (interquartile range) time from emergency call to dispatch of EMS providers was 3.0 (2.0–5.5) minutes, compared with 3 seconds from dispatch to drone launch. The median (interquartile range) time from dispatch to arrival of the drone was 5.3 (3.0–8.5) minutes versus 22.0 (17.8–29.0) minutes for EMS. The drone arrived to the scene faster than EMS providers in all 18 simulations, with a median reduction in response time of 16.7 minutes (95% CI, 13.8–20.2 minutes). No adverse events or technical issues occurred during any flights. Claesson et al 16 found a larger reduction in response times; however, the settings where the drones were deployed in their study differed significantly. In the study by Claesson et al, 16 AED drones were used in remote communities with fjords and waterways, which made ambulance access difficult. In our study, we have used AED drones in communities with low population densities but without physical barriers to ambulance access. We believe that our setting is more generalizable to most settings in North America. It is reasonable to assume in situations where there are physical barriers to ambulance access that AED drones could provide further improvements in emergency response times.
The potential of public access defibrillation programs to improve outcomes from OHCA in public locations has been demonstrated in multiple studies. 23 The harsh reality of public access defibrillation programs, however, is they are unable to deliver an AED to most cardiac arrests, which occur in private locations. Research from the Resuscitation Outcomes Consortium demonstrates an extremely low use of AEDs for OHCA in private locations, significantly diminishing the overall benefit of public access defibrillation programs. 24 Drone delivery of AEDs has the potential benefit of delivering AEDs to cardiac arrests in private and public locations, providing a solution to improving current public access defibrillation programs.
Our feasibility study has several limitations. Our study used a small number of test simulations aimed at determining feasibility of drone flights and was not developed to test specific hypotheses related to response times. Second, our test flights were done during simulations and may not replicate real‐life emergency responses in which a lay responder would be required to interact with a drone carrying an AED. Our testing assumes a smooth transition between the drone‐delivered AED and the lay bystander using the AED in an emergency situation. Further community consultation is required to ensure lay rescuers are comfortable with this concept. Third, as these were simulated encounters, the ambulance did not use lights and sirens during the first 4 simulated responses, so we are unsure if response times would be different during actual calls for OHCAs. In the last 2 simulations, however, a lights and sirens response was used and we still noted a decrease in response times with the AED drones. Furthermore, we believe that the use of lights and sirens during these responses would result in minimal time savings as the responses were in rural communities with little traffic and a maximum of 2 stoplights (situations where lights and sirens typically save time during a 911 response). Fourth, our flights occurred during optimal weather conditions (sunny with little wind) and may not be replicated in environments with high winds or colder temperatures. Previous testing has suggested that drone flight is feasible during inclement weather conditions. 25 The drones used in this study have been tested, with no adverse effects, in temperatures as low as −30°C and in wind speeds up to 20 to 30 km/h, with larger drones being able to withstand higher winds (Drone Delivery Canada, personal communication, March 13, 2020). As well, cardiac arrest is a 24/7 medical emergency and as such drone flights need to occur during both the night and the day to be effective, although most BVLOS flight systems have the capacity for night flight. Last, although drones improved response times in all our tested scenarios, the precision of the controlled drone descent blunted the time savings that occurred during the response to the scene. Optimization of drone decent at the scene needs to be further researched before use in 911 response. It is not known whether it is optimal to land the drone at the scene or to drop the AED using a tether or other method of controlled drop. Current research to optimize drone descent is underway, which may improve response times further.
Conclusions
Our study suggests AED drone delivery is feasible, with improvements in response times during simulated OHCA scenarios. AED drone delivery has the potential to decrease the time to defibrillation in rural and remote communities. Further research is required to optimize the integration of drones into the emergency response system, as well as improve strategies to simplify bystander application of a drone‐delivered AED.
Sources of Funding
The authors would like to acknowledge grant funding received from the Cardiac Arrhythmia Network of Canada and Zoll Medical Corporation for this research.
Disclosures
Dr Cheskes has received speaking honorarium for educational events on cardiopulmonary resuscitation quality from Zoll Medical and Stryker Corporation. Dr Cheskes has received grant funding from Zoll Medical for AED on the Fly, Community Responder Program for Peel Region, and Monitoring Ventilation During OHCA research studies. Dr Cheskes sits on the Advisory Board of Drone Delivery Canada. Dr Brooks has received funding from a Canadian Institutes of Health Research Operating Grant for research related to PulsePoint community responder cell phone application. The remaining authors have no disclosures to report.
Acknowledgments
We would like to thank Zoll Medical Corporation and Schiller AE for the use of the AED3 and FRED Easyport defibrillators during our research and Drone Delivery Canada and Indro Robotics for their subject matter (drone) expertise during our research. Finally, we would like to thank Peel Regional Paramedic Service and County of Renfrew Paramedic Service for their support.
(J Am Heart Assoc. 2020;9:e016687 DOI: 10.1161/JAHA.120.016687.)
For Sources of Funding and Disclosures, see page 7.
References
- 1. Larsen MP, Eisenberg MS, Cummins RO, Hallstrom AP. Predicting survival from out‐of‐hospital cardiac arrest: a graphic model. Ann Emerg Med. 1993;22:1652–1658. [DOI] [PubMed] [Google Scholar]
- 2. Valenzuela TD, Roe DJ, Cretin S, Spaite DW, Larsen MP. Estimating effectiveness of cardiac arrest interventions: a logistic regression survival model. Circulation. 1997;96:3308–3313. [DOI] [PubMed] [Google Scholar]
- 3. Buick JE, Drennan IR, Scales DC, Brooks SC, Byers A, Cheskes S, Dainty KN, Feldman M, Verbeek PR, Zhan C, et al. Improving temporal trends in survival and neurological outcomes after out‐of‐hospital cardiac arrest. Circ Cardiovasc Qual Outcomes. 2018;11:e003561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hansen SM, Hansen CM, Folke F, Rajan S, Kragholm K, Ejlskov L, Gislason G, Kober L, Gerds TA, Hjortshoj S, et al. Bystander defibrillation for out‐of‐hospital cardiac arrest in public vs residential locations. JAMA Cardiol. 2017;2:507–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Jennings PA, Cameron P, Walker T, Bernard S, Smith K. Out‐of‐hospital cardiac arrest in Victoria: rural and urban outcomes. Med J Aust. 2006;185:135–139. [DOI] [PubMed] [Google Scholar]
- 6. Mathiesen WT, Bjorshol CA, Kvaloy JT, Soreide E. Effects of modifiable prehospital factors on survival after out‐of‐hospital cardiac arrest in rural versus urban areas. Crit Care. 2018;22:99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Masterson S, Wright P, O'Donnell C, Vellinga A, Murphy AW, Hennelly D, Sinnott B, Egan J, O'Reilly M, Keaney J, et al. Urban and rural differences in out‐of‐hospital cardiac arrest in Ireland. Resuscitation. 2015;91:42–47. [DOI] [PubMed] [Google Scholar]
- 8. Stapczynski JS, Svenson JE, Stone CK. Population density, automated external defibrillator use, and survival in rural cardiac arrest. Acad Emerg Med. 1997;4:552–558. [DOI] [PubMed] [Google Scholar]
- 9. Kannan P. UAE develops delivery drones to improve government services. The National February 10, 2014. https://www.thenational.ae/uae/government/uae-develops-delivery-drones-to-improve-government-services-1.685853. Accessed November 20, 2019.
- 10. Hackman M, Nicas J. Drone delivers medicine to rural Virginia clinic. The Wall Street Journal July 17, 2015. https://www.wsj.com/articles/drone-delivers-medicine-to-rural-virginia-clinic-1437155114. Accessed November 20, 2019.
- 11. D'Onfro J. Meet the startup that's using drones to change the world. Business Insider Australia November 9, 2014. https://www.businessinsider.com.au/matternet-uav-delivery-drones-2014-11. Accessed November 20, 2019.
- 12. Delft University of Technology . TU Delft's ambulance drone drastically increases changes of survival of cardiac arrest patients. Delft University of Technology News Release. October 24, 2014. https://www.tudelft.nl/en/2014/tu-delft/tu-delfts-ambulance-drone-drastically-increases-chances-of-survival-of-cardiac-arrest-patients/. Accessed November 20, 2019.
- 13. Reece P. Drones that save lives. Salt Spring Exchange. June 26, 2014. https://saltspringexchange.com/2014/06/26/drones-that-save-lives/. Accessed November 21, 2019.
- 14. Boutilier JJ, Brooks SC, Janmohamed A, Byers A, Buick JE, Zhan C, Schoellig AP, Cheskes S, Morrison LJ, Chan TCY. Optimizing a drone network to deliver automated external defibrillators. Circulation. 2017;135:2454–2465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Pulver A, Wei R, Mann C. Locating AED enabled medical drones to enhance cardiac arrest response times. Prehosp Emerg Care. 2016;20:378–389. [DOI] [PubMed] [Google Scholar]
- 16. Claesson A, Backman A, Ringh M, Svensson L, Nordberg P, Djarv T, Hollenberg J. Time to delivery of an automated external defibrillator using a drone for simulated out‐of‐hospital cardiac arrests vs emergency medical services. JAMA. 2017;317:2332–2334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Transport Canada . Remotely piloted aircraft systems operational risk assessment. Advisory Circular. Draft. https://www.unmannedsystems.ca/wp-content/uploads/2019/07/DRAFT-AC-903-001-RPAS-Operational-Risk-Assessment.pdf. Accessed February 15, 2020.
- 18. Canadian Institutes of Health Research, Natural Sciences and Engineering Research Council of Canada, and Social Sciences and Humanities Research Council . Tri‐Council Policy Statement: Ethical Conduct for Research Involving Humans. 2018. [Google Scholar]
- 19. Drennan IR, Lin S, Thorpe KE, Morrison LJ. The effect of time to defibrillation and targeted temperature management on functional survival after out‐of‐hospital cardiac arrest. Resuscitation. 2014;85:1623–1628. [DOI] [PubMed] [Google Scholar]
- 20. Burger A, Wnent J, Bohn A, Jantzen T, Brenner S, Lefering R, Seewald S, Grasner JT, Fischer M. The effect of ambulance response time on survival following out‐of‐hospital cardiac arrest. Dtsch Arztebl Int. 2018;115:541–548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. O'Keeffe C, Nicholl J, Turner J, Goodacre S. Role of ambulance response times in the survival of patients with out‐of‐hospital cardiac arrest. Emerg Med J. 2011;28:703–706. [DOI] [PubMed] [Google Scholar]
- 22. Bogle BM, Rosamond WD, Snyder KT, Zegre‐Hemsey JK. The case for drone‐assisted emergency response to cardiac arrest: an optimized statewide deployment approach. N C Med J. 2019;80:204–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hallstrom AP, Ornato JP, Weisfeldt M, Travers A, Christenson J, McBurnie MA, Zalenski R, Becker LB, Schron EB, Proschan M; Public Access Defibrillation Trial Investigators . Public‐access defibrillation and survival after out‐of‐hospital cardiac arrest. N Engl J Med. 2004;351:637–646. [DOI] [PubMed] [Google Scholar]
- 24. Weisfeldt ML, Sitlani CM, Ornato JP, Rea T, Aufderheide TP, Davis D, Dreyer J, Hess EP, Jui J, Maloney J, et al. Survival after application of automatic external defibrillators before arrival of the Emergency Medical System: evaluation in the Resuscitation Outcomes Consortium population of 21 million. J Am Coll Cardiol. 2010;55:1713–1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Drone Delivery Canada . Drone delivery Canada BVLOS pilot program—Moosonee/Moose Factory ON. October 5, 2018. https://dronedeliverycanada.com/video-repository/. Accessed February 15, 2020.


