Abstract
Background
Heart failure (HF) imparts a significant clinical and economic burden on the health system in the United States.
Methods and Results
We used the National Inpatient Sample database between September 2002 and December 2016. We examined trends of comorbidities, inpatient mortality, and healthcare resource use in patients admitted with acute HF. Outcomes were adjusted for demographic variables, comorbidities, and inflation. A total of 11 806 679 cases of acute HF hospitalization were identified. The burden of coronary artery disease, peripheral vascular disease, valvular heart disease, diabetes mellitus, hypertension, anemia, cancer, depression, and chronic kidney disease among patients admitted with acute HF increased over time. The adjusted mortality decreased from 6.8% in 2002 to 4.9% in 2016 (P‐trend<0.001; average annual decline, 1.99%), which was consistent across age, sex, and race. The adjusted mean length of stay decreased from 8.6 to 6.5 days (P<0.001), but discharge disposition to a long‐term care facility increased from 20.8% to 25.6% (P<0.001). The inflation adjusted mean cost of stay increased from $14 301 to $17 925 (P<0.001) (average annual increase, 1.52%), which was partially explained by the higher proportion of procedures (echocardiogram, right heart catheterization, use of ventricular assist devices, coronary artery bypass grafting) and the higher incidence of HF complications (cardiogenic shock, respiratory failure, ventilator, and renal failure requiring dialysis).
Conclusions
This national data set showed that despite increasing medical complexities, there was significant reduction in inpatient mortality and length of stay. However, these measures were counterbalanced by a higher proportion of discharge disposition to long‐term care facilities and expensive cost of care.
Keywords: heart failure, mortality, resource use
Subject Categories: Heart Failure
Nonstandard Abbreviations and Acronyms
- HF
heart failure
- ICD‐9‐CM
International Classification of Diseases, Ninth Revision, Clinical Modification
- ICD‐10‐CM
International Classification of Diseases, Tenth Revision, Clinical Modification
- NIS
Nationwide Inpatient Sample
Clinical Perspective
What Is New?
Between September 2002 and December 2016, while the burden of chronic cardiovascular and noncardiovascular diseases increased in patients admitted with acute heart failure, the inpatient mortality and length of stay had decreased.
Total inpatient cost of stay had increased, which was partially explained by increase in procedure use and complications of heart failure.
A higher proportion of patients were discharged to long‐term care facilities.
What Are the Clinical Implications?
Despite increasing medical complexities, management strategies appear to improve survival and decrease length of stay in patients admitted with acute heart failure.
However, the perceived benefit of early discharge was offset by the increased cost of care and a higher number of discharges to long‐term care facilities.
Health strategies should aim to provide cost‐effective care in patients with heart failure.
Congestive heart failure (HF) is a highly prevalent condition accounting for over 6 million patients in the United States. 1 Since the incidence of HF increases with advancing age, acute HF exacerbation is among the most frequent causes of hospitalization among elder Americans. 1 To counter this epidemic, major initiatives were taken by the end of the second millennium to reduce complications and resource use. 2 , 3 More recently, the Hospital Readmissions Reduction Program was passed in 2010 to reduce the healthcare use by targeting readmission rates. 4 While the focus of such initiatives was to reduce the cost of care, concerns existed that any potential financial benefits might be compromised by increased length of stay and suboptimal quality of care. 4 In the same framework, data have signaled a rise in mortality corresponding to increasing clinical complexities. 5 In perspective, it is imperative to examine the clinical and economical patterns in patients admitted with acute HF. Herein, we studied a nation‐level database to illustrate trends in demographic and clinical profile, inpatient mortality, and resource use in patients with HF.
METHODS
Study Data
This study was exempted from institutional review board approval, given the deidentified nature of the Nationwide Inpatient Sample (NIS) database and public availability. Because of the sensitive nature of the data collected for this study, requests to access the data set from qualified researchers trained in human subject confidentiality protocols may be sent to The Healthcare Cost and Utilization Project. The NIS database is part of Healthcare Cost and Utilization Project databases and is sponsored by the Agency for Healthcare Research and Quality. The NIS is the largest publicly available all‐payer administrative claims–based database that contains information about clinical and resource use abstracted from discharges data from 47 US states encompassing >97% of the US population. The annual sample covers ≈8 million discharges, which represents 20% of US inpatient hospitalizations across different hospital types and geographic regions. National estimates of the entire US hospitalized population were calculated using the Agency for Healthcare Research and Quality sampling and weighting method. 6 Trend weights provided were used for trend analysis until 2011, and discharge weights provided were used for analysis after 2011. 7
Study Population and Design
The International Classification of Diseases, Ninth Revision, Clinical Modification (ICD‐9‐CM) codes to differentiate between acute and chronic HF were introduced in September 2002; therefore, data were analyzed from September 01, 2002, to December 31, 2016. We identified acute HF admissions in adults (≥18 years) using ICD‐9‐CM and International Classification of Diseases, Tenth Revision, Clinical Modification (ICD‐10‐CM) codes (Table S1). Discharge disposition was categorized as (1) home (including routine or home health); (2) short‐term care facility; (3) long‐term care facility (including skilled nursing and intermediate care facility); and (4) against medical advice.
Study Outcomes
The outcomes of interest were trends of (1) burden of comorbidities, (2) inpatient mortality, (3) mean length of stay and discharge disposition, and (4) mean cost of stay.
Statistical Analysis
We divided the study population into three 5‐year periods from 2002 to 2016. Categorical variables were presented as frequencies and percentages, and continuous variables were reported as means and SDs. Categorical variables were compared using a Pearson chi‐squared test and Fisher’s exact test, and continuous variables were compared using independent samples t test. For outcomes of interest, adjustment was done using univariate ANCOVA by the general linear model. Adjustments were done for variables, age, sex, race, median income, urban/rural hospital, hospital bed size, and 30 Elixhauser comorbidities (Tables S2 and S3). The Healthcare Cost and Utilization Project Cost‐to‐Charge Ratio File was used to calculate costs, by multiplying the charges by the cost‐to‐charge ratio. The mean cost of stay was adjusted for inflation with comparison to December 2016. 8 Prespecified analyses were performed for determining the components of cost of care, for example, complications and use of medical and procedural resources (Table S4). Statistical significance was set at 5%. Analyses were performed using Statistical Package for Social Science version 26 (IBM Corporation, Armonk, NY) and R Project for Statistical Computing version 3.5.
RESULTS
A total of 11 806 679 weighted acute adult cases of HF hospitalization were identified. Over the study period, the proportion of admissions to urban centers (86.4%–90.6%; P<0.001), medium‐bed‐size hospitals (27.8%–28.4%; P<0.001), and smaller‐bed‐size hospitals (9.8%–16.1%; P<0.001) were increased (Table 1). The proportion of patients with Medicare (77.4%–76.1%; P<0.001) and private insurance (12.7%–11.5%; P<0.001) were decreased, but Medicaid (5.9%–8.0%; P<0.001) was increased.
Table 1.
Demographic Characteristics and Burden of Comorbidities in Patients Hospitalized With Acute Heart Failure
| Variable, N (%) |
2002–2006 (n=297 112) |
2007–2011 (n=4 039 603) |
2012–2016 (n=7 469 964) |
P Value |
|---|---|---|---|---|
| Age, y, mean (SD) | 73.0 (13.6) | 73.6 (14.0) | 72.5 (13.8) | <0.001 |
| Female | 167 152 (56.3) | 2 084 589 (51.6) | 3 687 864 (49.4) | <0.001 |
| Race | ||||
| White | 157 595 (73.3) | 2 553 894 (72.7) | 5 101 784 (71.4) | <0.001 |
| Black | 38 362 (17.8) | 590 572 (16.8) | 1 223 065 (17.1) | |
| Hispanic | 12 337 (5.7) | 220 037 (6.3) | 483 690 (6.8) | |
| Other | 6699 (3.2) | 149 707 (4.2) | 341 180 (4.8) | |
| Comorbidities | ||||
| Acquired immune deficiency syndrome | 286 (0.1) | 6305 (0.2) | 12 090 (0.2) | <0.001 |
| Alcohol abuse | 7129 (2.4) | 107 309 (2.7) | 250 320 (3.4) | <0.001 |
| Chronic artery disease | 134 908 (44.0) | 2 166 795 (51.3) | 3 872 004 (51.8) | <0.001 |
| Anemia | 57 864 (19.9) | 1 152 422 (28.5) | 2 345 870 (31.4) | <0.001 |
| Collagen vascular disease | 6357 (2.2) | 116 487 (2.9) | 251 930 (3.4) | <0.001 |
| Chronic pulmonary disease | 105 604 (36.2) | 1 390 074 (34.4) | 2 796 605 (37.4) | <0.001 |
| Coagulopathy | 11 453 (3.9) | 248 375 (6.1) | 629 805 (8.4) | <0.001 |
| Depression | 17 453 (6.0) | 361 854 (9.0) | 815 905 (10.9) | <0.001 |
| Diabetes mellitus | 113 242 (38.9) | 1 662 937 (41.1) | 3 346 645 (44.8) | <0.001 |
| Hypertension | 154 908 (53.2) | 2 614 742 (64.7) | 5 178 669 (69.3) | <0.001 |
| Liver disease | 5142 (1.8) | 92 739 (2.3) | 262 205 (3.5) | <0.001 |
| Lymphoma | 2406 (0.8) | 40 655 (1.0) | 82 030 (1.1) | <0.001 |
| Neurological disorders | 14 519 (5.0) | 293 484 (7.3) | 615 720 (8.2) | <0.001 |
| Obesity | 26 838 (9.2) | 584 480 (14.5) | 1 619 885 (21.7) | <0.001 |
| Peripheral vascular disease | 25 999 (8.9) | 493 630 (12.2) | 1 023 120 (13.7) | <0.001 |
| Paralysis | 4236 (1.5) | 87 401 (2.2) | 190 855 (2.6) | <0.001 |
| Pulmonary circulation disorders | 5460 (1.9) | 181 991 (4.5) | 337 795 (4.5) | <0.001 |
| Solid tumors | 4884 (1.7) | 73 846 (1.8) | 147 185 (2.0) | <0.001 |
| Renal failure | 60 743 (20.8) | 1 473 343 (36.5) | 3 095 580 (41.4) | <0.001 |
| Peptic ulcer | 296 (0.1) | 1351 (0.0) | 147 185 (2.0) | <0.001 |
| Valvular disease | 14 160 (4.9) | 262 093 (6.5) | 557 755 (7.5) | <0.001 |
| Hospital location | ||||
| Rural | 40 345 (13.6) | 479 686 (11.9) | 775 310 (10.4) | <0.001 |
| Urban nonteaching | 120 745 (40.6) | 1 717 713 (42.5) | 2 362 484 (31.6) | |
| Urban teaching | 136 056 (45.8) | 1 842 335 (45.6) | 4 332 170 (58.0) | |
| Bed size of the hospital | ||||
| Small | 29 188 (9.8) | 444 429 (11.0) | 1 200 100 (16.1) | <0.001 |
| Medium | 82 582 (27.8) | 981 131 (24.3) | 2 121 964 (28.4) | |
| Large | 185 376 (62.4) | 2 614 174 (64.7) | 4 147 900 (55.5) | |
| Median household income percentile | ||||
| 0–25th | 89 755 (31.0) | 1 208 602 (30.6) | 2 338 315 (31.9) | <0.001 |
| 26th–50th | 71 958 (24.8) | 1 059 623 (26.8) | 1 937 944 (26.4) | |
| 51st–75th | 68 443 (23.6) | 936 898 (23.7) | 1 699 145 (23.2) | |
| 76th–100th | 59 554 (20.6) | 749 978 (19.0) | 1 356 950 (18.5) | |
| Primary expected payer | ||||
| Medicare | 229 646 (77.4) | 3 104 447 (77.0) | 5 677 334 (76.1) | <0.001 |
| Medicaid | 17 628 (5.9) | 263 393 (6.5) | 596 800 (8.0) | <0.001 |
| Private insurance | 37 618 (12.7) | 487 046 (12.1) | 854 250 (11.5) | <0.001 |
| Self‐pay | 7471 (2.5) | 109 160 (2.7) | 189 405 (2.5) | <0.001 |
| No charge | 617 (0.2) | 9107 (0.2) | 15 985 (0.2) | <0.001 |
Trends in Demographics and Comorbidities
There were significant temporal changes in the demographic profile and comorbidity burden in patients with HF. The mean age of the patients varied from 73.0 ± 13.6 years in 2002 to 2006 to 72.5 ± 13.8 in 2012 to 2016 (P<0.001). The proportion of females (56.3%–49.4%; P<0.001), whites (73.3%–71.4%; P<0.001) and blacks decreased (17.8%–17.1%; P<0.001); but the proportion of Hispanics increased (5.7%–6.8%; P<0.001). The prevalence of coronary artery disease, peripheral vascular disease, valvular heart disease, anemia, lymphoma, solid tumors, depression, chronic pulmonary disease, chronic renal disease, chronic liver disease, diabetes mellitus, hypertension, and obesity increased over time (P<0.001; Table 1).
Trends in Inpatient Mortality
A total of 4.9% (576 288 patients) died during hospitalization. The adjusted inpatient mortality in the total cohort decreased from 6.8% in 2002 to 4.8% in 2010 and then plateaued to 4.9% in 2016 (P‐trend<0.001; average annual decline, 1.95%; Figure 1A). The decline in adjusted inpatient mortality was consistent in patients who were <65 years (4.5%–3.5%; average annual decline, −1.55%) or ≥65 years old (7.2%–5.4%; average annual decline, 1.74%; Figure 1B); males (8.0%–5.2%; average annual decline, 2.44%) or females (5.8%–4.6%; average annual decline, 1.44%; Figure 1C); Hispanics (5.7%–4.9%; average annual decline, 0.98%), whites (7.0%–5.0%; average annual decline, 1.99%), or blacks (5.6%–4.4%; average annual decline, 1.49%; P‐trend<0.001 for all; Figure 1D).
Figure 1.
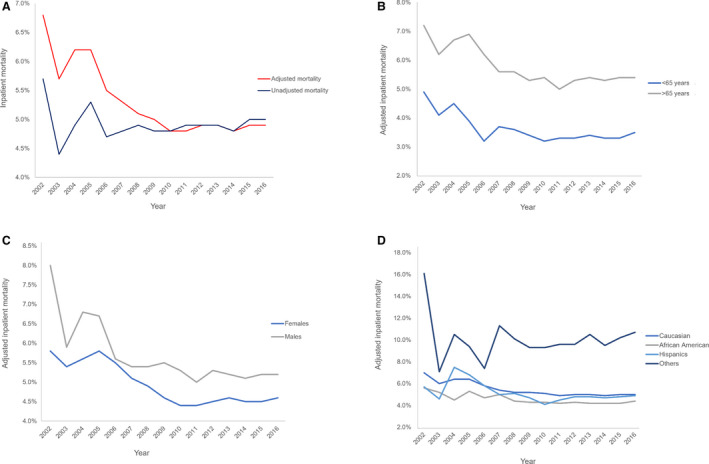
Trends in in‐hospital mortality in patients admitted with acute heart failure. A, Overall trends in in‐hospital mortality. B, Trends in in‐hospital mortality stratified by age. C, Trends in in‐hospital mortality stratified by sex. D, Trends in in‐hospital mortality stratified by race. Study duration extends from September 2002 to December 2016.
Trends in Length of Stay and Resource Use
The adjusted mean length of stay significantly decreased from 8.6 to 6.5 days (Figure 2A). Discharges to home decreased (70.4%–65.4%; P<0.001) and long‐term care facility increased (20.8%–25.6%; P<0.001; Table 2). The adjusted mean cost of stay increased from $14 301 to $17 925 (P<0.001; average annual increase, 1.52%; Figure 2B). The total adjusted cost per year is illustrated in Figure 3A. This rise in cost burden was partly explained by a rise in proportion of total procedures (19.2%–24.5%; P‐trend<0.001; average annual increase, 1.93%; Figure 3B) and HF‐related complications (Table S4). The most notable rise was noticed in the use of right heart catheterization; cardiogenic shock; use of vasopressors, hemodynamic support devices, and ventilators; and renal failure requiring dialysis.
Figure 2.
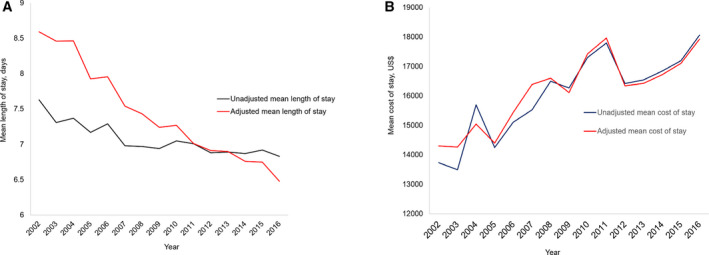
Trends in length of stay and cost of stay in patients admitted with acute heart failure. A, Overall trends in length of stay. B, Overall trends in mean cost of stay. Study duration extends from September 2002 to December 2016.
Table 2.
Hospital Encounter Outcomes and Resource Use in Patients Hospitalized With Acute Heart Failure
| Variables, N (%) |
2002–2006 (n=297 146) |
2007–2011 (n=4 039 735) |
2012–2016 (n=7 469 964) |
P Value |
|---|---|---|---|---|
| Died at discharge | 14 409 (4.9) | 190 554 (4.7) | 371 325 (5.0) | <0.001 |
| Discharge disposition of alive patients | ||||
| Home discharge | 209 010 (70.4) | 2 666 367 (66.0) | 4 883 454 (65.4) | <0.001 |
| Short‐term care facility | 10 057 (3.4) | 121 997 (3.0) | 234 280 (3.1) | |
| Long‐term care facility | 61 807 (20.8) | 1 030 413 (25.5) | 1 909 570 (25.6) | |
| Against medical advice | 1529 (0.5) | 25 304 (0.6) | 64 530 (0.9) | |
| Resource use, mean (SD) | ||||
| Length of stay, mean (SD), d (unadjusted) | 7.1 (7.9) | 6.8 (7.2) | 6.9 (7.5) | <0.001 |
| Cost of hospitalization, mean (SD), $ (unadjusted) | 14 648.3 (21 812.1) | 17 015 (25 508.7) | 17 094.7 (26 546.5) | <0.001 |
Figure 3.
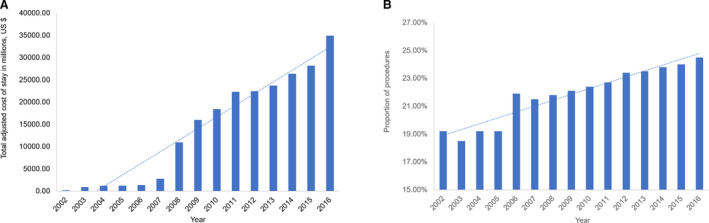
Trends in total adjusted cost of stay and proportion of procedures in patients admitted with acute heart failure. A, Trends in total cost of stay. B, Trends in proportion of procedures. Study duration extends from September 2002 to December 2016.
DISCUSSION
In this large‐scale report of over 14 years of in‐hospital trends in acute HF, we illustrate (1) an increasing burden of comorbidities among patient with HF; (2) the inpatient mortality in HF has declined considerably regardless of age, sex, and race; (3) total inpatient cost stay has increased despite shortened length of stay, which was partially explained by increase in procedure use and complications of HF; and (4) the decrease in length of stay was counterbalanced by an increase in long‐term care facility usage.
The clinical profile of patients hospitalized for HF is getting incrementally complex, predominantly attributable to the burden of noncardiovascular comorbidities. 5 Over 40% of patients with HF had more than 5 noncardiovascular comorbidities among US Medicaid beneficiaries and approximately 75% of patients with HF had at least 1 noncardiovascular comorbidity in the European Society of Cardiology HF pilot survey. 9 , 10 In the Get With the Guidelines–Heart Failure Registry, the burden of hematologic diseases, cancer, depression, chronic noncardiovascular diseases, diabetes mellitus, hypertension, and obesity increased over time. 5 Our study confirms the extension of these patterns.
The risk of hospitalization has a direct association with chronic noncardiac comorbidities, which account for almost comparable proportions in rehospitalization rates to cardiovascular diseases. 9 , 11 For instance, the proportion of patients with anemia, renal failure, and obesity increased over time in our study. Since these diseases are associated with decompensation of HF, patients with these comorbidities were more likely to be hospitalized and reflected higher trends of noncardiovascular burden over time. 5 The Acute Decompensated Heart Failure National Registry showed that on admission, >50% patients with HF had at least moderate renal insufficiency. 12 Similarly, the prevalence of anemia was estimated to be 50% to 70% in patients with HF, encompassing both ambulatory and inpatient settings. 13 While the noncardiovascular comorbidities are expected to compromise survival, as noncardiovascular mortality is unlikely to be modified by the use of HF‐targeted therapies, 5 our findings represent contrasting prognostic patterns over time. These results might be the reflection of initiatives taken by cardiovascular societies to curb the comorbidity burden in HF. 14 Moreover, the improved outpatient clinical practices targeting both cardiovascular and noncardiovascular entities might have translated into improved inpatient survival in patients with HF. 15
For years, the goals of inpatient HF management were to expedite the treatment of patients, narrow the duration of hospital stay, and discharge them swiftly to minimize the cost of care. 3 , 16 The Hospital Readmissions Reduction Program introduced the model of financial penalties for early readmissions, which proved to be a tipping point in shifting the focus from “early” to “effective” discharge. 16 However, since this risk‐standardized 30‐day readmission penalty metric relied on administrative claims, without adequately adjusting for medical complexity or illness severity, data signaled toward a higher mortality rate in patients with HF after implementation of the Hospital Readmissions Reduction Program. 4 , 17 , 18 Moreover, concerns existed that such strategies might lead to increased length of hospitalization. 4 Conversely, our report documents reduced inpatient mortality and length of stay, which were persistent after multivariate adjustments. More importantly, a uniform reduction in mortality across different demographic subgroups was a particularly encouraging finding.
Prior data trended the mortality rise with reference to implementation of Hospital Readmissions Reduction Program and accounted for 30‐day to 1‐year mortality rates in HF patients. 4 , 17 , 18 Our figures focus exclusively on the in‐hospital trends and extend the findings from a prior NIS report suggesting a continued decline in mortality up to 2016. 19 Explanations include improvement in medical and revascularization strategies encountering acute coronary syndrome, advancements of HF‐targeted therapies, and provision of adequate cardiopulmonary support to mitigate the risk of life‐threatening complications. Moreover, use of nontraditional methods, such as targeting natriuretic peptides as risk markers, might have played a role in improving outcomes in patients. 20
While the shift in administrative policies has appeared to safeguard the survival in HF cohorts, 10 , 16 the control measures employed to minimize the readmission rates have proved to be financially counterproductive. Prior national trends reported a total estimated cost of >$11 billion in 2014 for index hospitalization. 19 Our results validate this impression by reporting a 1.52% annual rise in cost burden since 2002 and a 4.3% rise since 2010. These national statistics are different from other cardiovascular disease economics. For instance, the hospital cost for acute myocardial infarction decreased from $12.4 billion in 2001 to $11.3 billion in 2011 (9% decrease). 21 The inflation‐adjusted cost of surgical or transcatheter aortic valve interventions reduced to $42 416 and $48 020 in 2016, respectively. 22 Our data suggest that a rise in proportion of procedures and complications appeared to be the culprits, keeping in mind that the cost of procedures has also increased over time. 23 Moreover, a perceived benefit of early discharge was counterbalanced by higher discharge rates to long‐term care facilities.
Prior data showed that discharging patients to long‐term care facilities was associated with higher mortality and readmission rates. In a study of 1840 long‐term care facilities encompassing 500 322 residents, patients with HF had >45% annual mortality rates than those without HF. 24 Another study of 15 459 elderly patients showed higher 30‐day and 1‐year mortality compared with those who were discharged home. 25 Similarly, HF accounted for >70% of all 30‐day readmissions from nursing facilities in 2004. These statistics suggest that patients in long‐term care facilities were less likely to receive guideline‐directed treatment, or use of therapies that influence the quality of life and prognosis, such as cardiac rehabilitation or renin‐angiotensin system inhibitors. 26 , 27
Our data are restricted to inpatient HF economic burden in the United States and do not represent outpatient cost or global financial expenditure. However, with advancing age and increasing concurrent medical complexities, rates of hospitalization are expected to increase, generating an exponential rise in cost of stay. As per the American Heart Association 21 policy statement, the total cost of care is expected to increase from $31 billion in 2012 to $70 billion in 2030. 1 Current data report alarming figures for the healthcare policy makers, stakeholders, and payers and call for more efforts to provide value‐based care.
Limitations
The NIS is an administrative database designed for billing purposes. It relies on ICD coding and hence is subject to misclassification and coding. However, Healthcare Cost and Utilization Project data are shown to be reasonably accurate for estimating diagnosis, trending procedures, and healthcare expenditure. 22 Given that the main objective for this study was to trend components of resource use, it is unlikely that results were confounded by inaccurate data. The NIS database exclusively contains discharge data and lacks information on the individuals or data related to readmissions or longitudinal outcomes. Therefore, we could not analyze recurrent hospitalizations, or assess outcomes at a particular day of the admission or at longer follow‐ups. Because of the same shortcomings, costs generated by each procedure could not be estimated. The difference in proportions of certain comorbidities or components of healthcare resource use were very close. Therefore, in such scenarios, given such a large sample size, significant findings may not actually be clinically meaningful or relevant. There was a difference in the ICD coding from 2015 to 2016, given a shift from ICD‐9 to ICD‐10 in the last quarter of 2015. Moreover, there could be a minor variation in the methodology of collecting samples after 2011; however, adjustments for that were done using weights provided by Healthcare Cost and Utilization Project. By the same account, these trends do not represent outpatient clinical and economic dynamics of patients with HF. Finally, our analysis could not incorporate pharmacotherapy, laboratory, or echocardiographic data because of the lack of information in this database. Despite these limitations, the NIS remains the most comprehensive database to examine long‐term trends of hospitalization in the United States.
Conclusions
This 15‐year contemporary analysis of HF hospitalization in the United States documents declining in‐hospital mortality and length of stay but rising costs and use of intermediate care facilities after discharge.
Sources of Funding
None.
Disclosures
None.
Supporting information
Tables S1–S4
(J Am Heart Assoc. 2020;9:e016782 DOI: 10.1161/JAHA.120.016782.)
For Sources of Funding and Disclosures, see page 6.
References
- 1. Heidenreich PA, Albert NM, Allen LA, Bluemke DA, Butler J, Fonarow GC, Ikonomidis JS, Khavjou O, Konstam MA, Maddox TM, et al. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail. 2013;6:606–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Gheorghiade M, Braunwald E. Hospitalizations for heart failure in the United States—a sign of hope. JAMA. 2011;306:1705–1706. [DOI] [PubMed] [Google Scholar]
- 3. Bueno H, Ross JS, Wang Y, Chen J, Vidan MT, Normand SL, Curtis JP, Drye EE, Lichtman JH, Keenan PS, et al. Trends in length of stay and short‐term outcomes among Medicare patients hospitalized for heart failure, 1993–2006. JAMA. 2010;303:2141–2147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gupta A, Fonarow GC. The hospital readmissions reduction program: evidence for harm. JACC Heart Fail. 2018;6:607–609. [DOI] [PubMed] [Google Scholar]
- 5. Sharma A, Zhao X, Hammill BG, Hernandez AF, Fonarow GC, Felker GM, Yancy CW, Heidenreich PA, Ezekowitz JA, DeVore AD. Trends in noncardiovascular comorbidities among patients hospitalized for heart failure: insights from the Get With the Guidelines–Heart Failure Registry. Circ Heart Fail. 2018;11:e004646. [DOI] [PubMed] [Google Scholar]
- 6. Munkhaugen J, Sverre E, Otterstad JE, Peersen K, Gjertsen E, Perk J, Gullestad L, Moum T, Dammen T, Husebye E. Medical and psychosocial factors and unfavourable low‐density lipoprotein cholesterol control in coronary patients. Eur J Prev Cardiol. 2017;24:981–989. [DOI] [PubMed] [Google Scholar]
- 7. Khan MZ, Munir MB, Khan MU, Osman M, Agrawal P, Syed M, Ghaffar YA, Alharbi A, Khan SU, Balla S. Trends, outcomes, and predictors of revascularization in cardiogenic shock. Am J Cardiol. 2020;125:328–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Harper CR, Jacobson TA. Using apolipoprotein B to manage dyslipidemic patients: time for a change? Mayo Clin Proc. 2010;85:440–445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Braunstein JB, Anderson GF, Gerstenblith G, Weller W, Niefeld M, Herbert R, Wu AW. Noncardiac comorbidity increases preventable hospitalizations and mortality among Medicare beneficiaries with chronic heart failure. J Am Coll Cardiol. 2003;42:1226–1233. [DOI] [PubMed] [Google Scholar]
- 10. van Deursen VM, Urso R, Laroche C, Damman K, Dahlstrom U, Tavazzi L, Maggioni AP, Voors AA. Co‐morbidities in patients with heart failure: an analysis of the European Heart Failure Pilot Survey. Eur J Heart Fail. 2014;16:103–111. [DOI] [PubMed] [Google Scholar]
- 11. Mentz RJ, Felker GM. Noncardiac comorbidities and acute heart failure patients. Heart Fail Clin. 2013;9:359, vii. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Heywood JT, Fonarow GC, Costanzo MR, Mathur VS, Wigneswaran JR, Wynne J. High prevalence of renal dysfunction and its impact on outcome in 118,465 patients hospitalized with acute decompensated heart failure: a report from the ADHERE database. J Card Fail. 2007;13:422–430. [DOI] [PubMed] [Google Scholar]
- 13. Anand IS. Anemia and chronic heart failure implications and treatment options. J Am Coll Cardiol. 2008;52:501–511. [DOI] [PubMed] [Google Scholar]
- 14. Bozkurt B, Aguilar D, Deswal A, Dunbar SB, Francis GS, Horwich T, Jessup M, Kosiborod M, Pritchett AM, Ramasubbu K, et al. Contributory risk and management of comorbidities of hypertension, obesity, diabetes mellitus, hyperlipidemia, and metabolic syndrome in chronic heart failure: a scientific statement from the American Heart Association. Circulation. 2016;134:e535–e578. [DOI] [PubMed] [Google Scholar]
- 15. Chen J, Normand SL, Wang Y, Krumholz HM. National and regional trends in heart failure hospitalization and mortality rates for Medicare beneficiaries, 1998–2008. JAMA. 2011;306:1669–1678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Felker GM, Whellan DJ. Inpatient management of heart failure: are we shooting at the right target? Ann Intern Med. 2017;166:223–224. [DOI] [PubMed] [Google Scholar]
- 17. Dharmarajan K, Wang Y, Lin Z, Normand ST, Ross JS, Horwitz LI, Desai NR, Suter LG, Drye EE, Bernheim SM, et al. Association of changing hospital readmission rates with mortality rates after hospital discharge. JAMA. 2017;318:270–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ibrahim AM, Dimick JB, Sinha SS, Hollingsworth JM, Nuliyalu U, Ryan AM. Association of coded severity with readmission reduction after the hospital readmissions reduction program. JAMA Intern Med. 2018;178:290–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Jackson SL, Tong X, King RJ, Loustalot F, Hong Y, Ritchey MD. National burden of heart failure events in the United States, 2006 to 2014. Circ Heart Fail. 2018;11:e004873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. McQuade CN, Mizus M, Wald JW, Goldberg L, Jessup M, Umscheid CA. Brain‐type natriuretic peptide and amino‐terminal pro‐brain‐type natriuretic peptide discharge thresholds for acute decompensated heart failure: a systematic review. Ann Intern Med. 2017;166:180–190. [DOI] [PubMed] [Google Scholar]
- 21. Sugiyama T, Hasegawa K, Kobayashi Y, Takahashi O, Fukui T, Tsugawa Y. Differential time trends of outcomes and costs of care for acute myocardial infarction hospitalizations by ST elevation and type of intervention in the United States, 2001–2011. J Am Heart Assoc. 2015;4:e001445 DOI: 10.1161/JAHA.114.001445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Alkhouli M, Alqahtani F, Ziada KM, Aljohani S, Holmes DR, Mathew V. Contemporary trends in the management of aortic stenosis in the USA. Eur Heart J. 2020;41:921–928. [DOI] [PubMed] [Google Scholar]
- 23. Alkhouli M, Alqahtani F, Aljohani S, Alvi M, Holmes DR. Burden of atrial fibrillation‐associated ischemic stroke in the United States. JACC Clin Electrophysiol. 2018;4:618–625. [DOI] [PubMed] [Google Scholar]
- 24. Hutt E, Elder SJ, Fish R, Min SJ. Regional variation in mortality and subsequent hospitalization of nursing residents with heart failure. J Am Med Dir Assoc. 2011;12:595–601. [DOI] [PubMed] [Google Scholar]
- 25. Allen LA, Hernandez AF, Peterson ED, Curtis LH, Dai D, Masoudi FA, Bhatt DL, Heidenreich PA, Fonarow GC. Discharge to a skilled nursing facility and subsequent clinical outcomes among older patients hospitalized for heart failure. Circ Heart Fail. 2011;4:293–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Aronow WS, Rich MW, Goodlin SJ, Birkner T, Zhang Y, Feller MA, Aban IB, Jones LG, Bearden DM, Allman RM, et al. In‐hospital cardiology consultation and evidence‐based care for nursing home residents with heart failure. J Am Med Dir Assoc. 2012;13:448–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Dolansky MA, Zullo MD, Hassanein S, Schaefer JT, Murray P, Boxer R. Cardiac rehabilitation in skilled nursing facilities: a missed opportunity. Heart Lung. 2012;41:115–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Tables S1–S4


