Abstract
Background
There have been few studies on the relationship between long‐term changes in sodium intake and blood pressure. A method of reducing sodium intake in a population that is known for high‐sodium intake based on homemade cooking is also needed.
Methods and Results
Our study was based on a baseline survey of 15 350 individuals aged 18 to 69 years with multistage random sampling and a 3‐year salt‐restriction campaign across Shandong Province, China. We included 339 individuals from six districts/counties in this cohort study, and the 24‐hour urinary sodium‐potassium ratio (Na+/K+) served as an indicator of sodium intake. The average change in ratio was 2.39 (95% CI, 2.17–2.61) from 6.81 (95% CI, 6.41–7.21) at baseline to 4.41 (95% CI, 4.18–4.64) during the resurvey. Following a reduction from low to high quartiles of urinary Na+/K+ ratio, the average increases were 10.9 (95% CI, 8.9–12.9), 9.2 (95% CI, 6.9–11.5), 6.3 (95% CI, 4.0–8.6), and 5.3 (95% CI, 2.9–7.7) mm Hg for systolic blood pressure (P for trend=0.019) and 3.8 (95% CI, 2.4–5.2), 2.9 (95% CI, 1.7–4.2), 1.6 (95% CI, 0.4–2.8), and −0.3 (95% CI, −1.4–0.8) mm Hg for diastolic blood pressure (P for trend=0.002), respectively. A reduction in salt intake was evident for people using a 2‐g salt‐restriction spoon for cooking (−3.49 versus −2.22; P=0.027) after adjustment of confounding factors, compared with nonusers. Similar findings were obtained for other salt‐restriction spoon–based indicators.
Conclusions
Our study indicated that using a salt‐restriction spoon for cooking was associated with reduced salt intake that led to a blunting of blood pressure deterioration. This finding further supports the salt‐restriction spoon–based strategy for people whose primary salt intake is from homemade cooking.
Keywords: blood pressure, cohort, salt‐restriction spoon, sodium intake
Subject Categories: High Blood Pressure, Risk Factors, Primary Prevention, Epidemiology
Nonstandard Abbreviations and Acronyms
- BP
blood pressure
- DBP
diastolic blood pressure
- Health ABC
Health, Aging, and Body Composition
- PURE
Prospective Urban Rural Epidemiology
- SBP
systolic blood pressure
- SMASH
Shandong Ministry of Health Action on Salt Reduction and Hypertension
Clinical Perspective
What Is New?
This study provides the first evidence indicating an association between long‐term changes in 24‐hour urinary Na+/K+ ratios and blood pressure in a real‐world population.
This study is also the first to indicate that the use of a salt‐restriction spoon may be an important strategy for population‐based salt reduction for blunting blood pressure deterioration.
What Are the Clinical Implications?
Studies with flawed methodologies have generated controversy and cast doubt on current salt‐restriction campaigns, but this study lends a support to an etiological relationship between salt intake and blood pressure in a large‐scale background population that receives policy‐based salt‐restriction interventions.
• This study suggests the use of a salt‐restriction spoon–based strategy in countries in which there is a dietary culture of high sodium intake mainly from salt added to home‐cooked foods.
A high‐sodium diet is well known as an important risk factor for hypertension, contributing to 1.65 million deaths from cardiovascular events worldwide in 2010.1 Population‐based salt restriction has been implemented in many countries such as the United Kingdom,2 United States,3 Canada,4 and China.5 However, studies with flawed methodologies such as the PURE (Prospective Urban Rural Epidemiology) study, the Health ABC (Health, Aging, and Body Composition) study, and a meta‐analysis have generated controversy and cast doubt on current salt‐restriction campaigns.6, 7, 8, 9, 10, 11
The World Health Organization recommends a 30% reduction in salt intake by 2025, with an eventual target of <5 g/d worldwide.12 However, this target remains challenging for people with traditionally high‐sodium diets. Situations in the real world are far more complicated than those in the ideal context of randomized controlled trials, which impose relatively short‐term effects of salt restriction upon hypertension.6, 13, 14 Furthermore, evidence from industrialized countries such as the United Kingdom shows that salt‐restriction strategies have mainly focused on reducing salt in packaged and processed food, which has resulted in a 15% reduction in the average salt intake of the population within 7 years.2 However, in many countries such as China, 76% of dietary sodium is derived from salt added to home‐cooked meals, which is dramatically different from Western countries such as the United Kingdom, where processed foods contribute to as much as 95% of sodium intake.15 Therefore, the salt‐restriction strategies from industrialized countries are likely not suitable for Chinese people and other populations with similar dietary cultures.
Salt‐restriction spoons have been extensively used in population‐based salt‐reduction campaigns such as the Shandong Ministry of Health Action on Salt Reduction and Hypertension (SMASH) in China. However, a randomized community intervention study failed to find an association between using a salt‐restriction spoon and reduction in 24‐hour urinary sodium levels.16 Thus, the use of salt‐restriction spoons is not listed in the Hypertension Management Section of the National Primary Public Health Services of China, which currently includes around 100 million patients with hypertension.17 A 24‐hour urinary Na+/K+ ratio, rather than the 24‐hour urinary sodium or potassium excretion rates, is most closely associated with blood pressure (BP).18 Moreover, encouraging potassium intake, such as consumption of fruits, vegetables, and potassium‐enriched salt, was here considered an important piece of health knowledge to disseminate to the public as part of the SMASH project. For this reason, isolated concentration of sodium or potassium could not actually reflect the effects of this comprehensive intervention.
Nevertheless, no investigations on the association of long‐term changes in both salt intake and BP have been performed to date, and it is also unclear whether salt‐restriction spoons for cooking may serve as a link between reduced salt intake and BP. Therefore, the purpose of the current study was to investigate the association between long‐term changes in salt intake, which was indicated by the 24‐hour urinary Na+/K+ ratio, and BP and salt‐related indicators in a population‐based cohort.
Subjects and Methods
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Study Population
This study was based on the SMASH project, which includes the entire population of Shandong Province (approximately 96 million people) in China.5 The SMASH baseline survey, which used staged‐cluster sampling, was conducted in June and July 2011. Figure 1 shows that of a total of 140 districts/counties across Shandong, 20 were randomly sampled, using proportional probability sampling, of which 48 communities and 108 villages from these 20 districts/counties were used for sampling participants at baseline conditions. According to the study guidelines, 100 individuals were randomly selected from a detailed list of names from each unit, and 15 350 individuals (18–69 years old) were finally recruited into the baseline survey. Of these individuals, 24‐hour urine samples were randomly collected from 2 184 individuals. Among 20 districts/counties, we randomly selected 2 districts and 4 counties (Figure 2) in which 661 individuals had qualified 24‐hour urine collected. In October and November 2014, we resurveyed 339 of 661 individuals and obtained their complete data including qualified 24‐hour urine. The baseline characteristics of these 339 individuals and the total population of 15 350 people are shown in Table 1. Overall, the resurveyed individuals were generally similar to the background population with regard to baseline characteristics such as sex, smoking, BP, hypertension, and body mass index (kg/m2) despite being older and having lower levels of education. None of the cohort population at baseline had taken any antihypertensive medicines within the previous 2 weeks, and in the resurvey we found that 28 individuals took this medicine within 2 weeks of follow‐up. This study received ethical approval from the Ethics Review Committee of the National Center for Chronic and Noncommunicable Disease Control and Prevention, the Chinese Center for Disease Control and Prevention. All participants received information on the study and provided written informed consent to participate.
Figure 1. Flowchart for recruitment of subjects.
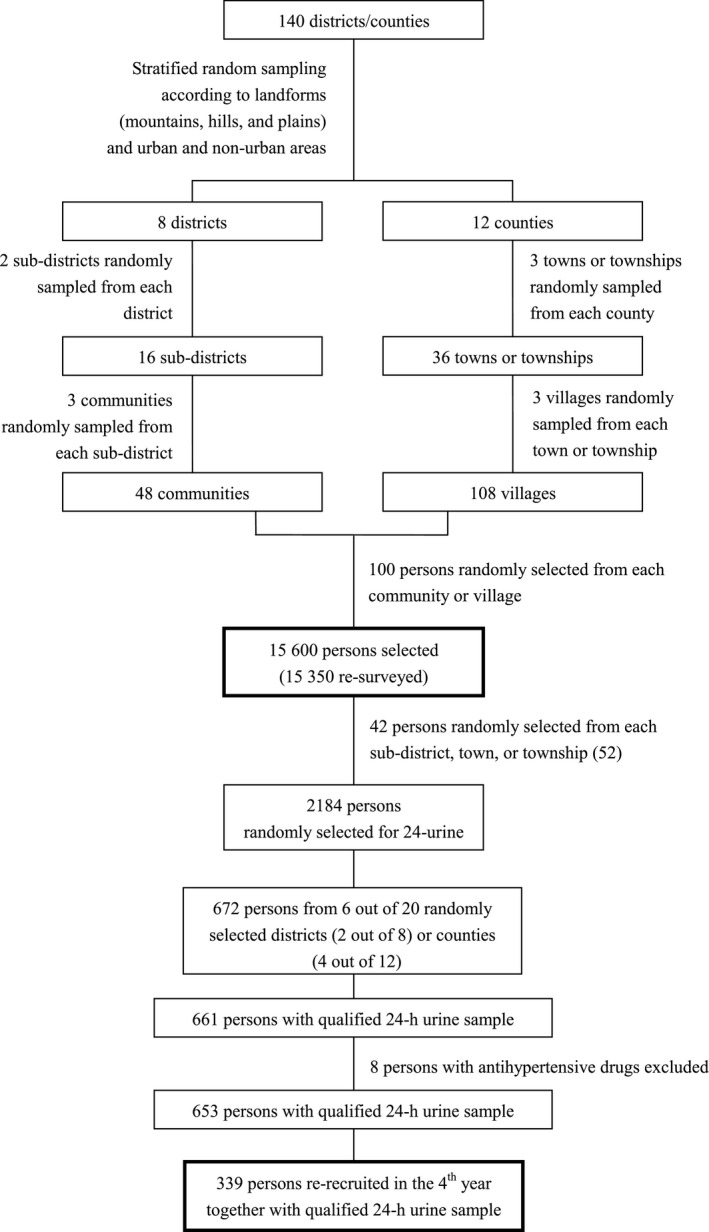
Figure 2. Distribution of areas and population.

Table 1.
Comparison of Baseline Characteristics Between the Study and Background Population
| Resurveyed (n=339) | Total (n=15 350) | |
|---|---|---|
| Women, % | 50.4 | 50.0 |
| Age, y | 43.6 (14.0) | 41.4 (14.1) |
| Rural people, % | 63.4 | 68.7 |
| Middle school or higher, % | ||
| Primary school or lower | 41.4 | 33.5 |
| Middle school | 39.1 | 43.2 |
| High school | 13.0 | 15.5 |
| College or higher | 6.5 | 7.8 |
| Smoking, % | 26.6 | 26.7 |
| Alcohol intake, % | 35.5 | 39.5 |
| BMI, kg/m2 | 24.8 (3.7) | 24.4 (4.0) |
| Systolic BP, mm Hg | 124.4 (19.7) | 121.5 (18.6) |
| Diastolic BP, mm Hg | 79.9 (11.0) | 79.2 (11.7) |
| Hypertension, % | 21.2 | 23.7 |
| Diabetes mellitus, % | 5.6 | 2.8 |
Data of age, BMI, and BP are means (standard deviations). BMI indicates body mass index; and BP, blood pressure.
Acquisition of Salt‐Intake Data
A face‐to‐face interview was conducted to complete a standardized questionnaire with trained public health professionals at baseline and follow‐up. In summary, participants were required to answer questions regarding their knowledge, attitude, and behavior on salt reduction such as using a salt‐restriction spoon for cooking and the use of low‐sodium salt. Additional details regarding this questionnaire have been described elsewhere.19
Measurements of Urinary Na+/K+ Ratios and Blood Pressure
Timed urine samples were obtained over at least a 24‐hours period after discarding urine obtained immediately before the collection period. Then, a 20‐mL aliquot of mixed urine was stored at −20°C. Urinary sodium, potassium, and creatinine concentrations were measured, and the 24‐hour urinary Na+/K+ ratio (mmol/mmol) was calculated from the urinary electrolyte concentration measured with an ion selective electrode method (AU5800, Beckman Coulter, USA). Individuals with urinary creatinine levels of ≤6 mmol/d or less, together with a urine volume of <300 mL/d, were excluded from the study. Trained researchers measured BP in the morning fasting in a quiet room using a validated automatic BP monitor (HEM‐7071, Omron Corporation, Kyoto, Japan) with an appropriately sized cuff. After participants had rested for at least 5 minutes, 3 readings were taken in the left upper arm at 1‐minute intervals with the participants in the sitting position and the arm supported at heart level. Systolic and diastolic BPs were obtained from the mean values of 3 BP readings.
Definitions Related to This Study
In the SMASH project, the public across Shandong Province were promoted to follow commendations from the Chinese Nutrition Society, that is, salt intake <6 g/person per day as determined using a measuring spoon (2, 3, or 6 g salt per spoon) when preparing food. We defined normal, high normal, and hypertension at baseline as systolic BP (SBP) <120 mm Hg and diastolic BP (DBP) <80 mm Hg, SBP=120 to 139 mm Hg or DBP=80 to 89 mm Hg, and SBP ≥140 mm Hg or DBP ≥90 mm Hg, respectively.20 Diabetes mellitus was defined as a fasting plasma glucose ≥7.0 mmol/L or the use of hypoglycemic medications within the past 2 weeks. Also, we calculated body mass index according to height and body weight.
Statistical Analysis
For practice, ratio decrease for quartiles 1 to 4 of Na+/K+ were approximately defined as <0, 0 to 1.9, 2.0 to 3.9, and ≥4.0. We used a paired Student's t test for examining intraindividual differences in Na+/K+ ratio during the 3‐year implementation of the SMASH project. We employed an ANCOVA for comparing a change in the Na+/K+ ratio and BP within 3 years among groups and subgroups taking antihypertensive drugs of follow‐ups and baseline BP stages; the dependent and independent variables in the ANCOVA model were the change in the Na+/K+ ratio or BP and grouping variables studied, respectively. Finally, we used a multiple linear regression with a quantitative Na+/K+ ratio change as independent variable for conducting a trend test after adjustments for confounding factors such as sex, age, education, smoking, alcohol intake, body mass index, baseline diabetes mellitus history, and use of antihypertensive drugs at follow‐up (if applicable). All analyses were performed using the SAS 9.2 statistical software package (SAS Institute, Cary, NC, USA). All P values were 2‐sided except for the P‐trend tests, in which 1‐sided P values were used. A P value <0.05 was considered statistically significant.
Results
Compared with the baseline measurements, the urinary Na+/K+ ratio in the analyzed population decreased by 32.2% (interquartile range, 5.0%–54.3%); the average change in ratio was 2.39 (95% CI, 2.17–2.61) from 6.81 (95% CI, 6.41–7.21) at baseline to 4.41 (95% CI, 4.18–4.64) during the resurvey. This finding was highly consistent in all subgroups with different baseline characteristics (Table S1), but this reduction was relatively small in people who were 40 to 59 years old. Individuals with a higher baseline BP category showed a greater reduction in Na+/K+ ratio (P for trend <0.001). Despite a decrease in Na+/K+ ratio, an overall increase in BP over time was observed; however, this BP change was reversely associated with a change of Na+/K+ ratio after adjustment for confounders (Table 2). Specifically, the average increases were 10.9 (95% CI, 8.9–12.9), 9.2 (95% CI, 6.9–11.5), 6.3 (95% CI, 4.0–8.6), and 5.3 (95% CI, 2.9–7.7) mm Hg for systolic BP and 3.8 (95% CI, 2.4–5.2), 2.9 (95% CI, 1.7–4.2), 1.6 (95% CI, 0.4–2.8), and −0.3 (95% CI, −1.4–0.8) mm Hg for diastolic BP, following a reduction from low to high quartiles in Na+/K+ ratio, <0, 0 to 1.9, 2.0 to 3.9, and ≥4.0, within these 3 years, respectively. The decreasing trends of BP increases associated with salt reduction, as shown in Figure 3A, were statistically significant for both SBP (P for trend=0.019) and DBP (P for trend=0.002); this association was consistent in individuals who did or did not take antihypertensive medicine within 2 weeks of follow‐up and especially evident in individuals with high baseline BP (Figure 3B through 3E). Of note, compared with individuals who exhibited no reduction in the Na+/K+ ratio (ie, the lowest quartile), a reduction in the Na+/K+ ratio of ≥2 (ie, the second‐highest quartile) led to a reduced BP increase by 42.2% for SBP and 57.9% for DBP; this effect was 51.4% for SBP, and there was no increase in DBP in individuals with a reduction in the Na+/K+ ratio of >4 (ie, the highest quartile). A total of 29.5% of our study population reached 50% of reduction in Na+/K+ ratio and, following this reduction, obtained a large blunting of BP deterioration.
Table 2.
Relationship Between Changes in the 24‐Hour Urinary Na+/K+ Ratio and Blood Pressure Within 3 y
| Decrease of Na+/K+ Ratio (mmol/mmol) | Systolic BP (mm Hg) | Diastolic BP (mm Hg) | ||||
|---|---|---|---|---|---|---|
| At. Baseline | After 3 y | Increase | At. Baseline | After 3 y | Increase | |
| First quartile (73 people) | 120.7 (15.5) | 131.6 (18.7) | 10.9 (8.9–12.9) | 77.4 (9.8) | 81.2 (11.9) | 3.8 (2.4–5.2) |
| Second quartile (99 people) | 125.1 (19.3) | 134.4 (20.2) | 9.2 (6.9–11.5) | 80.2 (10.3) | 83.1 (11.9) | 2.9 (1.7–4.2) |
| Third quartile (82 people) | 122.8 (22.1) | 129.1 (19.7) | 6.3 (4.0–8.6) | 78.5 (11.3) | 80.1 (9.9) | 1.6 (0.4–2.8) |
| Fourth quartile (85 people) | 128.4 (20.6) | 133.7 (20.5) | 5.3 (2.9–7.7) | 83.5 (11.9) | 83.2 (10.0) | −0.3 (−1.4–0.8) |
| P for trenda | … | … | 0.023 | … | … | 0.001 |
| Total (339 people) | 124.5 (16.4) | 132.3 (19.9) | 7.9 (21.1) | 79.9 (11.0) | 82.0 (11.0) | 2.0 (11.5) |
Quartiles 1–4 of Na+/K+ ratio decrease were defined as <0, 0–1.9, 2.0–3.9, and ≥4.0. An increase of BP after 3 years compared with baseline BP was a mean of BP changes within the study duration for each person. Data are means (standard deviations) unless an increase indicated by means with 95% CIs. BP indicates blood pressure.
Adjusted for sex, age, education, smoking, alcohol intake, body mass index, and diabetes mellitus at baseline.
Figure 3. Relationship between changes in 24‐hours urinary Na+/K+ ratio and BP within 3 years.
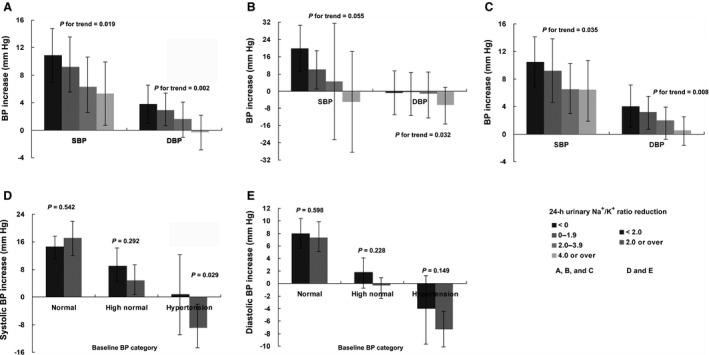
A, Overall trend for the increase in BP and decrease in the 24‐hour urinary Na+/K+ ratio. B and C, Trend for the increase in BP and decrease in the 24‐hour urinary Na+/K+ ratio in individuals with antihypertensive medications at the re‐survey or not. D and E, Increase in BP and decrease in the 24‐hour urinary Na+/K+ ratio in each BP category. Multiple linear regression models (stepwise method) were employed with BP increase as dependent variable and Na+/K+ ratio as continuous independent variable after the adjustment for age, sex, education level, smoking, body mass index, and diabetes mellitus at baseline, as well as the use of antihypertensive medications within the past 2 weeks at the resurvey (if applicable). BP indicates blood pressure; DBP, diastolic blood pressure; and SBP, systolic blood pressure.
We further observed factors associated with a reduction in urinary Na+/K+ ratio. Table 3 shows that in the study population, individuals answering “Yes” to any indicator related to salt reduction had significantly higher Na+/K+ ratios during the resurvey compared with baseline. In terms of knowledge level, the percentage of individuals receiving knowledge from publicity campaigns increased from 34.0% in 2011 to 50.7% in 2014 through the implementation of this project. Compared with 2.4% and 12.7% at baseline, 18.0% and 33.5% of individuals, respectively, knew about use of a salt‐restriction spoon during cooking and were familiar with low‐sodium salt in the resurvey. For behaviors, when comparing the resurvey to baseline, more individuals used less cooking salt (46.9% versus 15.3%, respectively). In particular, the percentages of those using a salt‐restriction spoon and low‐sodium salt changed from a much lower level (both 3.2%) to 22.7% and 25.1%, respectively. These indicators of knowledge and behavior were partly translated to a reduction in the Na+/K+ ratio.
Table 3.
Effect of Methods for Salt Reduction on Sodium Intake
| Indicators Related to Methods of Salt Reduction | Answer “Yes” (%) in 15 350 vs 339 People | Changes of 24 Urinary Na+/K+ Ratio After 3 yb | |||
|---|---|---|---|---|---|
| At Baseline | After 3 ya | Answer “Yes” or “No” at the 3‐y Follow‐Up | P Value Between “Yes” and “No” Groupsc | ||
| Yes | No | ||||
| Receive knowledge from publicity campaign | 34.0 | 50.7 | −2.64 (−3.27 to −2.01) | −2.13 (−2.70 to −1.56) | 0.155 |
| Knowledge of use of salt‐restriction spoon | 2.4 | 18.0 | −3.20 (−4.40 to −2.00) | −2.22 (−2.66 to −1.78) | 0.052 |
| Knowledge of low‐sodium salt | 12.7 | 33.5 | −2.51 (−3.47 to −1.63) | −2.09 (−2.47 to −1.69) | 0.131 |
| Use less cooking salt | 15.3 | 46.9 | −2.35 (−2.98 to −1.72) | −2.43 (−3.01 to −1.85) | 0.820 |
| Use salt‐restriction spoon | 3.2 | 22.7 | −3.05 (−4.14 to −1.96) | −2.22 (−2.67 to −1.77) | 0.053 |
| 2 g | 0.9 | 9.7 | −3.49 (−5.31 to −1.67) | −2.22 (−2.67 to −1.77) | 0.027 |
| 3 g | 0.9 | 4.7 | −2.66 (−4.62 to −0.70) | −2.22 (−2.67 to −1.77) | 0.654 |
| 6 g | 0.9 | 6.8 | −2.70 (−4.51 to −0.89) | −2.22 (−2.67 to −1.77) | 0.425 |
| Know usage of salt‐restriction spoon and use it | 0 | 16.5 | −3.39 (−4.65 to −2.13) | −2.20 (−2.64 to −1.76) | 0.022 |
| Know usage of salt‐restriction spoon and use less cooking salt | 0.3 | 13.6 | −3.41 (−4.84 to −1.98) | −2.23 (−2.66 to −1.80) | 0.038 |
| Use low‐sodium salt | 3.2 | 25.1 | −2.55 (−3.55 to −1.55) | −2.34 (−3.04 to −1.64) | 0.467 |
Change is indicated by means with 95% CIs.
Grouping indicator.
All Ps<0.01 for self‐comparisons of subgroups within 3 years.
Adjusted for sex, age, residence, education, smoking, and alcohol intake.
We found that some indicators of a salt‐restriction spoon were associated with a reduction in the Na+/K+ ratio. For example, although the baseline mean Na+/K+ ratio was non‐statistically higher among the groups using the salt‐restriction spoon approach in comparison to non‐users (7.4, 7.9, 7.3, 7.1, and 6.6 for all users, users with 2‐g, 3‐g, and 6‐g spoon, and nonusers, respectively), individuals using a 2‐g salt‐restriction spoon had a significantly greater reduction in the Na+/K+ ratio compared with those reporting no use of any salt‐restriction spoon (−3.49 versus −2.22; P=0.027) after adjustment of confounders, and this resulted in an overall marginal effect for using any salt‐restriction spoon (−3.05 versus −2.22; P=0.053). Combining knowledge with behaviors was substantial for salt‐restriction spoons. Compared with the controls, those aware of the use of salt‐restriction spoons obtained a greater reduction in Na+/K+ ratios using the spoon (−3.39 versus −2.20; P=0.022) or using less cooking salt (−3.41 versus −2.23; P=0.038). Contrary to the results of salt‐restriction spoons, we did not observe an association between using low‐sodium salt and the Na+/K+ ratio.
Discussion
To the best of our knowledge, this study provides the first evidence indicating an association between long‐term changes in 24‐hour urinary Na+/K+ ratios and BP in a real‐world population. This study is also the first to indicate that the use of a salt‐restriction spoon may be an important strategy for population‐based salt reduction for blunting BP deterioration.
Although the Health ABC (Health, Aging, and Body Composition) study and the PURE study have resulted in controversies on the association of salt intake with hypertension and cardiovascular risk,8, 9 the present study indicated that a reduction in the 24‐hour urinary Na+/K+ ratio attributable to salt restriction resulted in a blunted deterioration of BP. Our study differs in many ways from previous studies. For example, our findings on the association between the 24‐hour urinary Na+/K+ ratio and BP were obtained in the context of salt‐reduction intervention, which was applied to nearly 100 million people in the Shandong Province. Moreover, the association we observed was between changes over time in both salt intake and BP in the real world. We found that a large proportion of the population could obtain a substantial reduction in the 24‐hour urinary Na+/K+ ratio within 3 years, and thereafter, a significant blunting of BP deterioration despite increasing age and use of drugs. This long‐term and practical BP improvement should be compared with a meta‐analysis based on short‐term and idealistic randomized controlled trials, although there was a greater effect associated with higher‐baseline BP in these 2 studies.21 Nevertheless, our results provide new evidence for supporting an etiological relationship between salt intake and BP in a large‐scale background population that received policy‐based salt‐restriction interventions.
Our study revealed an effect of a 2‐g salt‐restriction spoon on reducing the 24‐hour urinary Na+/K+ ratio. This result should be compared with a previous intervention study that was conducted for 6 months.16 In this previous study, also conducted with Chinese community‐based people, the use of a 2‐g salt‐restriction spoon reduced daily salt intake as measured in dietary records (1.42 versus 0.28 g; P<0.001) but failed to reduce 24‐hour urinary sodium (34.8 versus 33.7 mmol; P=0.870) when compared with that of the intervention or control group. A long‐term habit, especially in favor of salt, was difficult to change by a short‐term intervention in the real world, as suggested by a systematic review,22 and a reduction of salt added in home cooking could receive compensation by the addition of condiments such as soy sauce or eating other food with salt that was not easy to measure. This could also result in the same effect on the 24‐hour urinary Na+/K+ ratio as that of using low‐sodium salt, which is usually less salty than normal‐sodium salt, but was not indicated in our population. In the current study, we failed to find an association between using salt‐restriction spoons and BP. This strengthened our knowledge that in this salt‐reduction campaign, BP benefited from a reduction in salt intake, as measured via the 24‐hour urinary Na+/K+ ratio, following the implementation of salt‐restriction actions for the population.23
Of interest, our study suggests the use of a salt‐restriction spoon–based strategy in countries in which there is a dietary culture of high sodium intake mainly from salt added to home‐cooked foods. This strategy should include the following: public education of the influence of salt on health, an increased number of families with a salt‐restriction spoon, an increased rate of using a salt‐restriction spoon, and using less cooking salt in combination with the use of a salt‐restriction spoon. As indicated by the present study, approximately 50% of the people of Shandong received public education related to salt restriction despite mass media such as television, broadcasting, Internet, and public‐service announcements advertising the SMASH project during these 3 years.
In Shandong Province, although residents are eligible to receive a free salt‐restriction spoon with instructions for its use from healthcare centers and from the Centers for Disease Control and Prevention, this has not guaranteed that each individual or family will own and use this spoon. In our present study, <25% of the people used a salt‐restriction spoon and <20% understood proper usage. Even so, salt‐restriction spoons are still recommended as a long‐term method of salt reduction. As supported by some studies, most people who are given salt‐restriction spoons do not or cannot use them correctly, such that they are not willing to abandon their high‐sodium diet and fail to observe an association between knowledge, attitudes, and behaviors toward salt and actual salt consumption indicated by 24‐hour urinary salt excretion, as suggested by a cross‐sectional study.23, 24, 25 This phenomenon was also observed in our present study, in which a lower salt intake was observed, particularly in people who understood the use of salt‐restriction spoons and practiced a low‐sodium diet (using salt‐restriction spoons, by reducing salt intake, or both).
Our present study implied that this salt‐restriction strategy was likely more effective on higher baseline sodium intake and BP. This is important when adding salt restriction to follow‐ups for patients with BP categories of normal‐high BP or hypertension receiving the National Primary Public Health Services by primary healthcare sites, where effective nondrug interventions are lacking.26 Despite a practical salt‐restriction strategy, we found that its effect on people who were 40 to 59 years old was minimal, and this was partly explained by poor compliance with salt restriction and outdoor dining of this population. This result also indicated involvement of other salt‐restriction strategies, such as intervention of the food and catering industry.
The present study has a few specific strengths. This study was based on a high‐quality design, including a multiple‐stage random sampling across Shandong, which is a typical province of China characterized by high‐sodium diets.27 Also, this was a long‐term cohort study in the context of the real world where we not only established temporality of the cohort study but also observed the dynamic relationship between long‐term changes in salt intake and BP for up to 3 years. Additionally, assessment of salt intake by spot urine produced many controversies and criticisms of results, but the 24‐hour urine collection method in this 3‐year follow‐up study is the gold standard for assessing salt intake and means a narrow range of measurements that is remarkably reproducible over at least 5 decades and across 45 societies and their unique dietary practices.28, 29 Moreover, the balance of sodium‐potassium is an overall reflection of the high sodium and low potassium intake of Chinese people, and the Na+/K+ ratio appears to be more strongly associated with BP outcomes than either sodium or potassium alone.18 More importantly, before intervention for this largest population of the salt‐restriction world, Chinese people across China, similar to Shandong, had extremely low rates of use of a salt‐restriction spoon and a high urinary Na+/K+ ratio of >6. Thus, our results are relevant for policy making to reduce future salt consumption in China.
This study also has some potential limitations. First, the flow from 15 350 to 339 individuals resulted in selection bias that reduced population representation on some indicators such as age, education, and history of diabetes mellitus, although there were similar baseline characteristics for the analyzed sample and sampled population, particularly for our primary indicators, that is, using a salt‐restriction spoon (15.3% versus 14.6%) and the mean 24‐hour urinary Na+/K+ ratio (6.81 versus 6.8).30, 31 Second, BP is not determined solely by salt. Therefore, we required information on antihypertensive drugs at follow‐up in spite of no patients using antihypertensive drugs at baseline, but these medications unchanged our findings. Also, the resurveyed individuals were older and have lower levels of education than the background population, and this likely resulted in an underestimation of the effect from various exposures such as the use of salt‐restriction spoons. Third, our sample size appeared to be small, but because of random sampling and 24‐hour urine collection, this sample could produce more plausible results than some large‐sample‐size studies such as the PURE study, which was conducted with a nonrandom sample and used spot urine tests.6, 9 Fourth, 24‐hour ambulatory BP monitoring and multiple 24‐hour urine collection were not performed, although we followed guidelines to conduct measurements and single 24‐hour urine collection has been validated.28 Finally, we failed to observe the effect of using low‐sodium salt in cooking, but salt‐restriction spoons for cooking such as those in our study could prevent 183 000 fewer cases of cardiovascular diseases and avoid $1.4 billion in the annual cardiovascular disease treatment costs across China, as indicated by a modeling study.23 Additionally, our study included a before‐versus‐after comparison within a single group of people. Though less likely, the observed changes could also be attributable to time difference.
In sum, our study revealed that a salt‐restriction spoon could be associated with a reduced salt intake that led to the blunting of BP deterioration. This finding further strengthens the use of a salt‐restriction spoon–based strategy for a population in which salt intake is mainly derived from homemade cooking and supports the use of salt‐restriction spoons to the National Primary Public Health Services of China for hypertension control and prevention. Considering a reduction of salt intake within 3 years in this study, the salt‐restriction spoon–based strategy could be important for achieving the World Health Organization goal by 2025, especially in Chinese people and other populations with similar dietary cultures.
Sources of Funding
This work, including analysis, decision to publish, and preparation of the manuscript, was supported by the SMASH Project and Shandong Provincial Technical Development Plan Grant (2012GSF11828). We acknowledge the following institutions that supported this work within their own administrative areas: the Fushan (Yantai City) Center for Disease Control and Prevention, Gaotang (Liaocheng City) Center for Disease Control and Prevention, Laicheng (Laiwu City) Center for Disease Control and Prevention, Gaomi (Weifang City) Center for Disease Control and Prevention, Junan (Linyi City) Center for Disease Control and Prevention, and Zoucheng (Jining City) Center for Disease Control and Prevention. We thank Prof. Yu Wang, Prof. Linhong Wang, Prof. Zhenqiang Bi, Prof. Yuling Hong, Prof. Quanhe Yang, Mr. Hai Xu, Dr Hao Liang, Dr Jing Dong, Dr Jianwei Xu, Dr Xiaorong Chen, Dr Zeng Ge, and Dr Congcong Gao. The local governments and many doctors, nurses, and other field workers provided their support to this project.
Disclosures
None.
Supporting information
Table S1
Acknowledgments
Author contributions: Drs Hou, Guo, and Zhang drafted the manuscript. Drs Hou, Guo, Zhang, Chen, Yan, Cai, Tang, and Xu performed the field survey. All authors were involved in acquisition, analysis, and interpretation of the data. Dr Hou conceived the hypothesis and analysis plan of this study. Drs Wu, Ma, and Xu were the guarantors of this work.
(J Am Heart Assoc. 2020;9:e014897 DOI: 10.1161/JAHA.119.014897.)
For Sources of Funding and Disclosures, see page 9.
Contributor Information
Jing Wu, Email: wujing@chinacdc.cn.
Jixiang Ma, Email: majix@163.com.
References
- 1. Mozaffarian D, Fahimi S, Singh GM, Micha R, Khatibzadeh S, Engell RE, Lim S, Danaei G, Ezzati M, Powles J. Global sodium consumption and death from cardiovascular causes. N Engl J Med. 2014;371:624–634. [DOI] [PubMed] [Google Scholar]
- 2. He FJ, Brinsden HC, MacGregor GA. Salt reduction in the United Kingdom: a successful experiment in public health. J Hum Hypertens. 2014;28:345–352. [DOI] [PubMed] [Google Scholar]
- 3. Bibbins‐Domingo K, Chertow GM, Coxson PG, Moran A, Lightwood JM, Pletcher MJ, Goldman L. Projected effect of dietary salt reductions on future cardiovascular disease. N Engl J Med. 2010;362:590–599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Vogel L. Health Canada sidesteps commitment to new salt reduction strategy. CMAJ. 2010;182:E571–E572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bi Z, Liang X, Xu A, Wang L, Shi X, Zhao W, Ma J, Guo X, Zhang X, Zhang J, et al Hypertension prevalence, awareness, treatment, and control and sodium intake in Shandong Province, China: baseline results from Shandong‐Ministry of Health Action on Salt Reduction and Hypertension (SMASH), 2011. Prev Chronic Dis. 2014;11:E88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. He FJ, MacGregor GA. Role of salt intake in prevention of cardiovascular disease: controversies and challenges. Nat Rev Cardiol. 2018;15:371–377. [DOI] [PubMed] [Google Scholar]
- 7. Tan M, He FJ, MacGregor GA. Salt and cardiovascular disease in PURE: a large sample size cannot make up for erroneous estimations. J Renin Angiotensin Aldosterone Syst. 2018;19:1470320318810015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kalogeropoulos AP, Georgiopoulou VV, Murphy RA, Newman AB, Bauer DC, Harris TB, Yang Z, Applegate WB, Kritchevsky SB. Dietary sodium content, mortality, and risk for cardiovascular events in older adults: the Health, Aging, and Body Composition (Health ABC) Study. JAMA Intern Med. 2015;175:410–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Mente A, O'Donnell MJ, Rangarajan S, McQueen MJ, Poirier P, Wielgosz A, Morrison H, Li W, Wang X, Di C, et al Association of urinary sodium and potassium excretion with blood pressure. N Engl J Med. 2014;371:601–611. [DOI] [PubMed] [Google Scholar]
- 10. Cappuccio FP, Campbell NR. Population dietary salt reduction and the risk of cardiovascular disease: a commentary on recent evidence. J Clin Hypertens (Greenwich). 2017;19:4–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Mente A, O'Donnell M, Rangarajan S, Dagenais G, Lear S, McQueen M, Diaz R, Avezum A, Lopez‐Jaramillo P, Lanas F, et al Associations of urinary sodium excretion with cardiovascular events in individuals with and without hypertension: a pooled analysis of data from four studies. Lancet. 2016;388:465–475. [DOI] [PubMed] [Google Scholar]
- 12. World Health Organization . Second consultation on a comprehensive global monitoring framework, including indicators, and a set of voluntary global targets for the prevention and control of NCDs. March 22, 2012. Available at: http://www.who.int/nmh/events/2012/consultation_april_2012/en/. Accessed June 1, 2019.
- 13. He FJ, Li J, Macgregor GA. Effect of longer‐term modest salt reduction on blood pressure. Cochrane Database Syst Rev. 2013;CD004937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. He FJ, Marciniak M, Visagie E, Markandu ND, Anand V, Dalton RN, MacGregor GA. Effect of modest salt reduction on blood pressure, urinary albumin, and pulse wave velocity in white, black, and Asian mild hypertensives. Hypertension. 2009;54:482–488. [DOI] [PubMed] [Google Scholar]
- 15. Anderson CA, Appel LJ, Okuda N, Brown IJ, Chan Q, Zhao L, Ueshima H, Kesteloot H, Miura K, Curb JD, et al Dietary sources of sodium in China, Japan, the United Kingdom, and the United States, women and men aged 40 to 59 years: the INTERMAP study. J Am Diet Assoc. 2010;110:736–745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Chen J, Tian Y, Liao Y, Yang S, Li Z, He C, Tu D, Sun X. Salt‐restriction‐spoon improved the salt intake among residents in China. PLoS ONE. 2013;8:e78963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. National Health and Family Planning Commission of China . 2017 [Norm of National Primary Public Health Services; 2017]. Available at: http://www.nhfpc.gov.cn/jws/s3578/201703/d20c37e23e1f4c7db7b8e25f34473e1b.shtml. Accessed January 26, 2019. Chinese.
- 18. Perez V, Chang ET. Sodium‐to‐potassium ratio and blood pressure, hypertension, and related factors. Adv Nutr. 2014;5:712–741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Zhang J, Xu AQ, Ma JX, Shi XM, Guo XL, Engelgau M, Yan LX, Li Y, Li YC, Wang HC, et al Dietary sodium intake: knowledge, attitudes and practices in Shandong Province, China, 2011. PLoS ONE. 2013;8:e58973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Revision Committee of Chinese Guidelines for the Prevention and Treatment of Hypertension . Chinese Guidelines for the Prevention and Treatment of Hypertension: Revised Edition 2018. Beijing: China Medical Science and Technology Publishing House; 2018. Chinese. [Google Scholar]
- 21. Graudal NA, Hubeck‐Graudal T, Jurgens G. Effects of low sodium diet versus high sodium diet on blood pressure, renin, aldosterone, catecholamines, cholesterol, and triglyceride. Cochrane Database Syst Rev. 2017;4:CD004022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Trieu K, McMahon E, Santos JA, Bauman A, Jolly KA, Bolam B, Webster J. Review of behaviour change interventions to reduce population salt intake. Int J Behav Nutr Phys Act. 2017;14:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wang M, Moran AE, Liu J, Coxson PG, Penko J, Goldman L, Bibbins‐Domingo K, Zhao D. Projected impact of salt restriction on prevention of cardiovascular disease in China: a modeling study. PLoS ONE. 2016;11:e0146820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Land MA, Webster J, Christoforou A, Johnson C, Trevena H, Hodgins F, Chalmers J, Woodward M, Barzi F, Smith W, et al The association of knowledge, attitudes and behaviours related to salt with 24‐hour urinary sodium excretion. Int J Behav Nutr Phys Act. 2014;11:47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Dong W, Lv W, Kang M, Du Y, Ma H, Zhang L, Zeng G. Survey on the situation of salt‐restriction‐spoon using among urban residents in Beijing in 2011. Chin J Prev Med. 2011;10:952–953. [Google Scholar]
- 26. Hou L, Chen X, Chen B, Liu L, Sun X, Zou Y, Liu H, Guo H, Zhang J, Ma J. Pharmacological therapy and blood pressure control in primary health care sites in China: data from 254,848 hypertensive patients. Clin Epidemiol. 2018;10:1467–1478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Zhang J, Guo X, Lu Z, Tang J, Li Y, Xu A, Liu S. Cardiovascular diseases deaths attributable to high sodium intake in Shandong province, China. J Am Heart Assoc. 2019;8:e010737 DOI: 10.1161/JAHA.118.010737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Cobb LK, Anderson CA, Elliott P, Hu FB, Liu K, Neaton JD, Whelton PK, Woodward M, Appel LJ. Methodological issues in cohort studies that relate sodium intake to cardiovascular disease outcomes: a science advisory from the American Heart Association. Circulation. 2014;129:1173–1186. [DOI] [PubMed] [Google Scholar]
- 29. McCarron DA, Kazaks AG, Geerling JC, Stern JS, Graudal NA. Normal range of human dietary sodium intake: a perspective based on 24‐hour urinary sodium excretion worldwide. Am J Hypertens. 2013;26:1218–1223. [DOI] [PubMed] [Google Scholar]
- 30. Zhang JY, Yan LX, Tang JL, Ma JX, Guo XL, Zhao WH, Zhang XF, Li JH, Chu J, Bi ZQ. Estimating daily salt intake based on 24 h urinary sodium excretion in adults aged 18‐69 years in Shandong, China. BMJ Open. 2014;4:e005089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Bi Z, Wang L, Zong L, Xu A. 2011 Baseline Report on the Shandong‐Ministry of Health Action on Salt Reduction and Hypertension. Ji'nan: Shandong Science and Technology Press; 2013. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1


