Abstract
Background
Accurate assessment of cardiac output is critical to the diagnosis and management of various cardiac disease states; however, clinical standards of direct Fick and thermodilution are invasive. Noninvasive alternatives, such as closed‐circuit acetylene (C2H2) rebreathing, warrant validation.
Methods and Results
We analyzed 10 clinical studies and all available cardiopulmonary stress tests performed in our laboratory that included a rebreathing method and direct Fick or thermodilution. Studies included healthy individuals and patients with clinical disease. Simultaneous cardiac output measurements were obtained under normovolemic, hypovolemic, and hypervolemic conditions, along with submaximal and maximal exercise. A total of 3198 measurements in 519 patients were analyzed (mean age, 59 years; 48% women). The C2H2 method was more precise than thermodilution in healthy individuals with half the typical error (TE; 0.34 L/min [r=0.92] and coefficient of variation, 7.2%) versus thermodilution (TE=0.67 [r=0.70] and coefficient of variation, 13.2%). In healthy individuals during supine rest and upright exercise, C2H2 correlated well with thermodilution (supine: r=0.84, TE=1.02; exercise: r=0.82, TE=2.36). In patients with clinical disease during supine rest, C2H2 correlated with thermodilution (r=0.85, TE=1.43). C2H2 was similar to thermodilution and nitrous oxide (N2O) rebreathing technique compared with Fick in healthy adults (C2H2 rest: r=0.85, TE=0.84; C2H2 exercise: r=0.87, TE=2.39; thermodilution rest: r=0.72, TE=1.11; thermodilution exercise: r=0.73, TE=2.87; N2O rest: r=0.82, TE=0.94; N2O exercise: r=0.84, TE=2.18). The accuracy of the C2H2 and N2O methods was excellent (r=0.99, TE=0.58).
Conclusions
The C2H2 rebreathing method is more precise than, and as accurate as, the thermodilution method in a variety of patients, with accuracy similar to an N2O rebreathing method approved by the US Food and Drug Administration.
Keywords: acetylene, cardiac output, exercise, Fick, noninvasive diagnostics, heart failure, thermodilution
Subject Categories: Heart Failure, Exercise, Exercise Testing
Nonstandard Abbreviations and Acronyms
- C2H2
acetylene
- FDA
Food and Drug Administration
- HF
heart failure
- N2O
nitrous oxide
- Qc
cardiac output
- r
Pearson correlation coefficient
- TE
typical error
oxygen uptake
Clinical Perspective
What Is New?
Noninvasive assessment of cardiac output (Qc) by means of inert gas rebreathing techniques, used in physiology laboratories for nearly 100 years, has broad applications for use in clinical patient populations.
In contrast to standard methods of assessing Qc, which are invasive, this technique is safe and easy for patients and staff to use.
Our data demonstrate that assessment of Qc using the inert gas rebreathing technique is as accurate and precise as current clinical gold standards in a wide population of patients.
What Are the Clinical Implications?
The ability to accurately and noninvasively measure Qc represents a major advancement for the field of cardiology, and can be helpful in patients with dyspnea of unclear cause, pulmonary hypertension, valvular heart disease, heart failure, and cardiogenic shock for confirmation and treatment.
The inert gas rebreathing technique allows for the ability to obtain measurements in a variety of locations (clinic and hospital) using a portable device without the risks associated with invasive procedures.
We encourage other investigators and clinicians to consider this technique in studies and patient populations where accurate and precise measurement of Qc would be important.
The accurate assessment of cardiac output (Qc) is critical for the appropriate diagnosis and management of a variety of cardiac diseases. The gold standard for measuring Qc, the direct Fick method, is not routinely performed in clinical settings as it requires specific equipment and expertise that are not readily available. Thus, the thermodilution technique is often used for decision making. Both the direct Fick and thermodilution methods are invasive techniques that require pulmonary artery catheter placement with associated risks including pneumothorax, infection, bleeding, or damage to the vasculature including pulmonary artery rupture. 1 , 2 Additionally, invasive techniques are expensive, time consuming, and require specialized personnel. Importantly, even “gold‐standard” invasive estimates of Qc, which rely on various equations to estimate rather than measure oxygen uptake (), have proven inaccurate. 3 Therefore, an accurate and reliable noninvasive alternative to assess Qc is appealing.
Acetylene (C2H2) is one of several gases used for Qc measurement by the foreign gas rebreathing technique (C2H2 rebreathing). 4 , 5 , 6 C2H2 is an inert, soluble gas that enters the blood stream via pulmonary diffusion but, importantly, does not bind to hemoglobin and thus its concentration decreases during rebreathing at a rate proportional to Qc. In patients without significant lung disease, intracardiac, or intrapulmonary shunting, the estimated pulmonary blood flow to ventilated lung obtained from the closed‐circuit C2H2 rebreathing method is proportional to systemic blood flow. 5
The initial use of C2H2 for measuring Qc was first described by Grollman in the 1920s. 4 , 5 , 6 Since then, inert gas rebreathing methods have been validated against gold standards of dye dilution and the direct Fick method in animal models and healthy patients at rest and during exercise. 7 , 8 , 9 Additionally, the accuracy and feasibility of noninvasive rebreathing methods have been shown in patients with pulmonary hypertension, valvular heart disease, cardiomyopathy (including low Qc states), and pulmonary disease. 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 Importantly, the ease of using commercially available foreign gas rebreathing systems has been demonstrated with exercise stress testing and supports its use in predicting outcomes in patients with heart failure (HF). 18 , 19 , 20 The nitrous oxide (N2O) rebreathing technique is currently approved by the US Food and Drug Administration (FDA) for commercial use and is marketed as the Innocor device (Innovision). This approval was granted given “substantial clinical evidence” for its equivalence to both the thermodilution and direct Fick methods. 21 While these previous investigations provide compelling evidence for the accuracy and feasibility of the inert gas rebreathing technique, most studies relied on small sample sizes and limited age ranges. Additionally, no studies have evaluated the precision and accuracy of the inert gas rebreathing technique in patients over a large range of defined cardiac preload conditions. Therefore, the goals of this study are to assess the precision and accuracy of the closed‐circuit C2H2 rebreathing technique for estimating Qc at rest, over a range of cardiac hemodynamic conditions, and during exercise in a large number of healthy volunteers and clinical patients compared with current clinical standards.
METHODS
The data that support the findings of this study are available from the corresponding author upon reasonable request. The studies included in this analysis were approved by an institutional review committee and the participants gave informed consent.
We retrospectively analyzed 10 clinical research studies and all available invasive cardiopulmonary exercise tests performed in our laboratory using standard measurement protocols (including patient conditions), and using the same equipment, the same techniques, and mostly the same staff over the past decade. These studies included a mixture of healthy individuals and patients with clinical disease recruited from the surrounding community, 4 , 22 , 23 , 24 , 25 , 26 as well as patients referred for evaluation of dyspnea. All study participants underwent invasive hemodynamic assessment with right heart catheterization. The majority of healthy participants were middle‐aged, sedentary adults, and those with clinical disease had HF with preserved ejection fraction as determined by Framingham HF diagnostic criteria and at least 1 prior hospitalization for HF. 10 Patients who were referred for invasive cardiopulmonary exercise testing had a variety of indications including unexplained dyspnea and HF. Studies involving healthy individuals had similar exclusion criteria to those involving patients who had HF with preserved ejection fraction and included inducible coronary artery disease, active or recent tobacco use, significant renal dysfunction (creatinine >2 mg/dL), obesity with a body mass index >35 kg/m2, and poorly controlled diabetes mellitus or hypertension.
The majority of studies were performed with participants at rest in the supine position. Baseline measurements were obtained after 30 minutes of quiet rest. Lower body negative pressure was then used to decrease cardiac filling, as previously published. 25 , 26 Qc measurements were performed after 5 minutes each of −15 and −30 mm Hg lower body negative pressure, which lowered both right atrial (≈−2 and −4 mm Hg) and pulmonary capillary wedge pressure (≈−3 and −6 mm Hg). After a 20‐minute break, repeat measurements were used to confirm a return to steady state. Cardiac filling was then increased by rapid infusion (100–200 mL/min) of warm normal saline. Measurements were repeated after 10 to 15 mL/kg and 20 to 30 mL/kg of saline infusion, which increased right atrial (≈+2 and +4 mm Hg) and pulmonary capillary wedge (≈+3 and +6 mm Hg) pressure, respectively. This protocol provided a large physiological range of pulmonary capillary wedge pressure from ≈4 to 18 mm Hg. For patients who underwent exercise testing, baseline measurements were obtained at rest in the upright position on a cycle ergometer and again during upright exercise under submaximal steady‐state conditions with at least 5 minutes spent at each workload to ensure hemodynamic stability, followed by a maximal effort.
Qc Comparison Methods
Closed‐circuit C2H2 Rebreathing Technique
The modified closed‐circuit C2H2 rebreathing method, with C2H2 as the soluble gas and helium as the insoluble gas, was used for noninvasive Qc assessment and has been previously described. 4 , 6 , 25 , 27 This method assumes that Qc is equal to effective pulmonary blood flow to ventilated lung, which can be assessed by the rate of decay of C2H2 concentration during rebreathing. Adequate mixing of the rebreathing gas in the lung was confirmed by a constant level of helium in all cases. The inspired fraction of C2H2 was calculated from the volume‐weighted integral of C2H2 concentration measured during the first inspiration of a known mixture. The rate of C2H2 absorption into blood was computed from the regression slope of the logarithm of regressed end‐tidal C2H2 fractions. The end‐tidal points were selected by the software based on Sackner criterion, only for breaths where a stable helium concentration had been established. 28 As per the usual laboratory practice in the studies used for this analysis, after a change in posture or prolonged break, the first 2 or 3 C2H2 rebreathing measures are discarded to allow for stabilization of posture‐related distribution of intrathoracic blood volume. No thermodilution measurements are obtained at this time to avoid excessive infusion of saline, and none of these measures were used for accuracy or precision analysis. Occasionally during the course of study, and at the discretion of the study cardiologist, measurements thought to be erroneous at the time of each individual study were excluded from analysis. These values were excluded immediately, in real time, and their exclusion was unrelated to the current comparison study. Common reasons for exclusion included poor inspiratory effort, evidence of inadequate gas mixing, or values obtained that were clearly outside of the achievable physiologic range. After the initial stabilization period (generally ≈15 minutes, and encompassing 2 or 3 measurements) this exclusion occurred rarely, involving no more than 1% to 2% of all measurements.
Thermodilution Technique
Determinations of Qc from thermodilution were based on the temperature changes recorded at the pulmonary artery thermistor after 10 mL of room temperature isotonic saline was injected into the right atrium. All curves were inspected visually, and only curves consistent with the required exponential decay were used for data analysis. Similar to the C2H2 rebreathing technique, <2% of thermodilution measurements were excluded from analysis based on poor temperature/time curves or values that were clearly outside of the achievable physiologic range. As with the C2H2 rebreathing measurements, the decision to exclude values was made at the time of study performance and unrelated to the current analysis.
Direct Fick Technique
Samples of pulmonary artery blood were drawn for determination of mixed venous oxygen content () in the middle of a 3‐minute Douglas bag collection (at rest) and 1‐minute Douglas bag collection (during exercise) for calculation of . Gas concentrations were determined from mass spectrometry and ventilatory volumes from a Tissot spirometer. Hemoglobin concentration and oxyhemoglobin saturation were determined using co‐oximetry (IL 482, Instrument Laboratories).
N2O Technique
This technique has been previously described by Jarvis and colleagues 4 and is essentially the same technique on which the clinically approved Innocor device was based. 29 Qc measurements were determined using the Sackner algorithm. 28
Statistical Analysis
For assessment of reliability (precision), individual measurements over a short period (on average 5 minutes between measurements) under the same condition were used for analysis. The reliability of all 3 methods was quantified by calculating the typical error (TE) of the measurement, retest correlation coefficients, and coefficients of variation (TE expressed as a percentage) for each method. 30
For assessment of accuracy (sensitivity), all patients underwent simultaneous Qc measurements with at least 2 different methods at each time point while either resting or exercising. The average of at least 2 (and up to 4) simultaneous measurements was used for analysis. These measurements were obtained ≈5 minutes apart. The accuracy of the rebreathing method was compared with the direct Fick, thermodilution, and N2O measurements (when available) using Pearson correlation coefficients (r), coefficients of variation, TE of the estimate, and visual presentation of the residuals (y axis) versus the predicted Qc (x axis). The predicted Qc is the practical measure (ie, C2H2, thermodilution or N2O) adjusted for random bias in the sample population using the Hopkins regression method. 30 The resulting plots allow for inspection of possible heteroscedasticity of error in the measurement.
RESULTS
Our study consisted of 3198 measurements in 519 individual encounters (including 34 encounters for patients referred for clinical assessment). Some patients were studied before and after at least a year of intervention or volunteered for a second research protocol. These patients were considered individual encounters as long as there was at least a year between studies. The mean age of the cohort was 59 years (range, 19–89 years) and 48% were women.
Assessment of Precision
The test‐retest reliability for the C2H2 rebreathing method was more precise than thermodilution in healthy patients with nearly half the TE: C2H2 rebreathing r=0.92 and TE 0.34 L/min (0.33–0.36) versus thermodilution r=0.70 and TE 0.67 L/min (0.64–0.71) (Figure 1). For comparison, precision analyses performed in a subset of healthy patients with repeated measurements of direct Fick yielded an excellent correlation (r=1.00) and a low TE of only 0.19 L/min (0.16–0.25).
Figure 1. Reliability of the acetylene (C2H2) rebreathing technique vs thermodilution method for assessment of Qc.
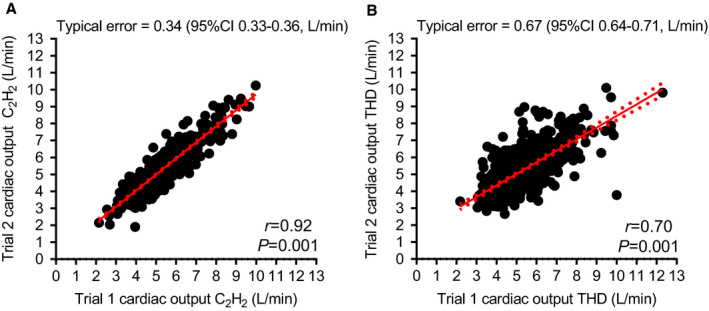
A, Reliability of C2H2 rebreathing for estimation of Qc; (B) Reliability of thermodilution for estimation of Qc. Qc indicates cardiac output.
Assessment of Accuracy
Comparison of Rebreathing and Thermodilution in the Supine Position at Rest
At rest in the supine position, the C2H2 rebreathing method showed excellent agreement with thermodilution (r=0.84) and a clinically acceptable TE of 1.02 L/min (1.00–1.050) (Figure 2). When patients were stratified by loading condition, the TE was lower at normal loading conditions (0.79 L/min [0.76–0.83] versus low (1.0 L/min [0.96–1.05] and high (1.21 L/min [1.16–1.27] preload states) (Table 1). Similarly, the C2H2 rebreathing method showed excellent agreement with thermodilution in patients with clinical disease at rest in the supine condition (r=0.85); however, there was a larger TE of 1.43 L/min (1.24–1.69) as compared with healthy controls.
Figure 2. Comparison of the accuracy of the acetylene (C2H2) rebreathing technique vs thermodilution method for the assessment of Qc in both healthy patients and those with clinical disease in the supine position at rest.
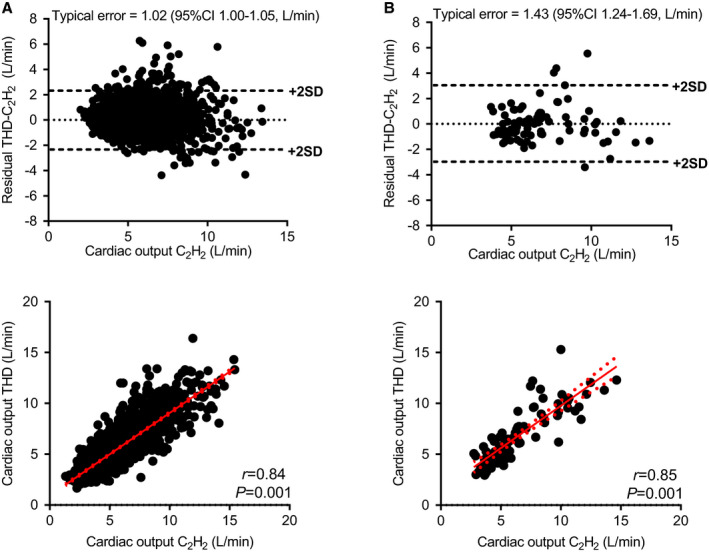
A, Accuracy of C2H2 rebreathing for estimation of Qc vs thermodilution in healthy patients; (B) Accuracy of C2H2 rebreathing for estimation of Qc vs thermodilution in a clinical population. Qc indicates cardiac output.
Table 1.
Assessment of Accuracy Between Various Methods of Qc Measurements
| Patients | Condition | Qc Comparison | No. of Data Points | Qc, Mean (SD) | r | TE | CV |
|---|---|---|---|---|---|---|---|
| Healthy, supine | |||||||
| Rest, all loading conditions | Thermodilution vs C2H2 | 2793 |
Thermodilution 5.5 (1.9) C2H2 5.7 (2.0) |
0.84 (0.83–0.85) | 1.02 (1.00–1.05) | 19.5% (18.9–20.0) | |
| Rest, normal loading/baseline | Thermodilution vs C2H2 | 989 |
Thermodilution 5.4 (1.2) C2H2 5.5 (1.3) |
0.76 (0.73–0.78) | 0.79 (0.76–0.83) | 15.7% (15.0–16.5) | |
| Rest, lower body negative pressure | Thermodilution vs C2H2 | 849 |
Thermodilution 4.8 (1.8) C2H2 4.8 (1.7) |
0.84 (0.82–0.86) | 1.00 (0.96–1.05) | 22.4% (21.3–23.7) | |
| Rest, rapid saline infusion | Thermodilution vs C2H2 | 900 |
Thermodilution 6.5 (2.2) C2H2 6.7 (2.4) |
0.84 (0.82–0.85) | 1.21 (1.16–1.27) | 19.5% (18.6–20.6) | |
| Clinical disease, supine | |||||||
| Rest, all loading conditions | Thermodilution vs C2H2 | 86 |
Thermodilution 6.8 (2.7) C2H2 6.4 (2.7) |
0.85 (0.78–0.90) | 1.43 (1.24–1.69) | 21.7% (18.6–26.0) | |
| Healthy, upright | |||||||
| Rest | Fick vs C2H2 | 117 |
Fick 5.3 (1.5) C2H2 5.6 (1.6) |
0.77 (0.69–0.84) | 0.94 (0.83–1.08) | 20.2% (17.7–23.5) | |
| Exercise | Fick vs C2H2 | 114 |
Fick 15.4 (4.8) C2H2 13.5 (3.7) |
0.87 (0.81–0.91) | 2.39 (2.12–2.75) | 16.5% (14.5–19.2) | |
| Rest | Fick vs Thermodilution | 109 |
Fick 5.3 (1.5) Thermodilution 5.6 (1.5) |
0.81 (0.74–0.87) | 0.88 (0.78–1.02) | 17.6% (15.3–20.5) | |
| Exercise | Fick vs Thermodilution | 87 |
Fick 14.7 (4.2) Thermodilution 14.0 (3.3) |
0.73 (0.61–0.82) | 2.87 (2.50–3.38) | 20.5% (17.6–24.5) | |
| Exercise | Thermodilution vs C2H2 | 98 |
Thermodilution 15.0 (4.1) C2H2 13.3 (3.2) |
0.82 (0.75–0.88) | 2.36 (2.06–2.74) | 16.5% (14.3–19.4) | |
| Clinical disease, upright | |||||||
| Exercise | Fick vs C2H2 | 44 |
Fick 8.2 (2.5) C2H2 8.2 (2.5) |
0.89 (0.81–0.94) | 1.14 (0.94–1.45) | 13.4% (11.0–17.4) | |
C2H2 indicates acetylene; CV, coefficient of variation; Qc, cardiac output; r, Pearson correlation coefficient; and TE, typical error.
Comparison of Rebreathing and Thermodilution in the Upright Position at Rest and With Exercise
In healthy individuals during upright exercise, the agreement between the C2H2 rebreathing and thermodilution methods remained excellent (r=0.82). As expected, there was a larger TE at higher Qc of 2.36 L/min (2.13–2.98). However, when expressed as a percentage, the variation in TE was similar to that observed for direct Fick versus C2H2 rebreathing. We did not have a significant number of patients who had simultaneous rebreathing and thermodilution measured with upright exercise in our cohort of patients with clinical disease for comparison.
Comparison of Rebreathing and Thermodilution Versus Direct Fick During Supine Rest, Upright Rest, and Upright Exercise: Sensitivity Analyses
We studied a subset of patients who underwent simultaneous measurement of direct Fick and either the C2H2 rebreathing or thermodilution method (Figures 3 and 4). In healthy patients at rest in the supine position, the C2H2 rebreathing method had better agreement than thermodilution when compared with direct Fick (C2H2 rebreathing r=0.85 versus thermodilution r=0.72) with a lower TE (C2H2 rebreathing TE=0.84 L/min [0.51–0.86] versus thermodilution TE=1.11 L/min [0.93–1.39]). In healthy patients at rest in the upright position, the C2H2 rebreathing method had a similar correlation (C2H2 rebreathing r=0.77 versus thermodilution r=0.81) and TE (C2H2 rebreathing TE=0.94 L/min (0.83–1.08) versus thermodilution TE=0.88 L/min [0.78–1.02]) as thermodilution when compared with the direct Fick method.
Figure 3. Comparison of the accuracy of the acetylene (C2H2) rebreathing technique and thermodilution method vs the direct Fick method for assessment of Qc in healthy patients in both the supine and upright positions at rest.
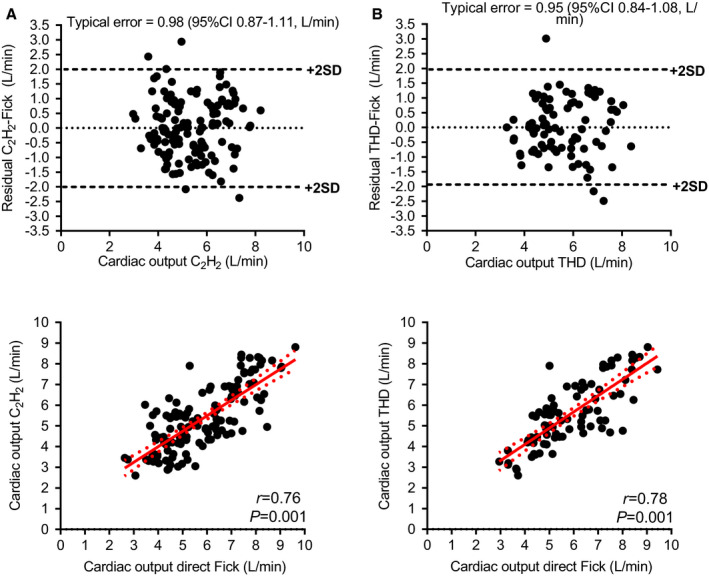
A, Accuracy of C2H2 rebreathing for estimation of Qc at rest; (B) Accuracy of thermodilution for estimation of Qc at rest. Qc indicates cardiac output.
Figure 4. Comparison of the accuracy of the acetylene (C2H2) rebreathing technique and thermodilution method vs the direct Fick method for assessment of Qc during upright exercise in healthy patients and those with clinical disease.
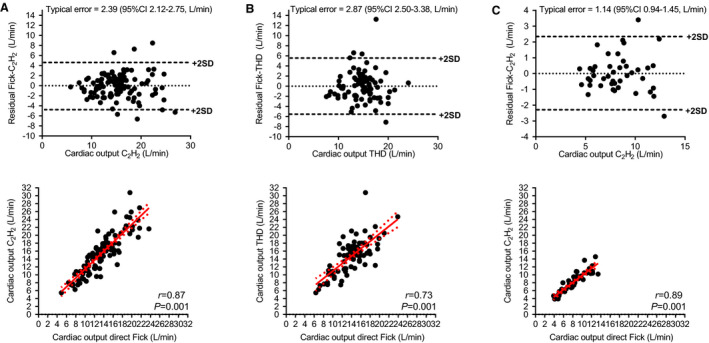
A, Accuracy of C2H2 rebreathing for estimation of Qc during exercise in healthy patients; (B) Accuracy of thermodilution for estimation of Qc during exercise in healthy patients; and (C) Accuracy of C2H2 rebreathing for estimation of Qc during exercise in clinical populations. Qc indicates cardiac output.
During exercise, the C2H2 rebreathing method correlated better with a lower TE when compared with the direct Fick than the thermodilution method (C2H2 rebreathing r=0.87 versus thermodilution r=0.73; C2H2 rebreathing TE=2.39 L/min [2.12–2.75] versus thermodilution TE=2.87 L/min [2.50–3.38]). In our clinical cohort of patients during exercise, the C2H2 rebreathing method correlated significantly with the direct Fick method (r=0.89) and had a very good TE of only 1.14 L/min (0.94–1.45).
Comparison of Direct Fick and Thermodilution to the C2H2 and N2O Rebreathing Techniques
Direct Fick and thermodilution Qc measurements, along with both C2H2 rebreathing and N2O rebreathing estimates of Qc, were obtained in 14 young, healthy patients in the supine and upright resting positions as well as during upright exercise. When compared with both the direct Fick and thermodilution methods, the C2H2 rebreathing technique appeared at least as good as, if not better than, the N2O rebreathing technique with respect to the degree of correlation and TE (Table 2 and Figure 5).
Table 2.
Assessment of Accuracy Between 2 Inert Gas Rebreathing Methods
| Patients | Condition | Qc Comparison | No. of Data Points | Qc, Mean (SD) | r | TE | CV |
|---|---|---|---|---|---|---|---|
| Healthy, supine | |||||||
| Rest | Fick vs N2O | 52 |
Fick 6.4 (1.6) N2O 6.6 (1.0) |
0.82 (0.71–0.89) | 0.94 (0.79–1.17) | 16.5 (13.9–20.9) | |
| Rest | Fick vs C2H2 | 51 |
Fick 6.3 (1.6) Rebreathing 7.2 (1.0) |
0.85 (0.76–0.91) | 0.84 (0.70–1.05) | 14.5% (12.0–18.3) | |
| Rest | Thermodilution vs N2O | 56 |
Thermodilution 7.2 (1.2) N2O 6.6 (1.0) |
0.65 (0.46–0.78) | 0.90 (0.76–1.11) | 14.1 (11.8–17.7) | |
| Rest, all loading conditions | Thermodilution vs C2H2 | 2793 |
Thermodilution 5.5 (1.9) Rebreathing 5.7 (2.0) |
0.84 (0.83–0.85) | 1.02 (1.00–1.05) | 19.5% (18.9–20.0) | |
| Healthy, upright | |||||||
| Rest | Fick vs N2O | 54 |
Fick 4.5 (0.9) N2O 4.1 (1.0) |
0.44 (0.19–0.63) | 0.82 (0.69–1.01) | 19.8 (16.3–25.0) | |
| Exercise | Fick vs N2O | 57 |
Fick 16.9 (3.9) N2O 11.8 (2.4) |
0.84 (0.74–0.90) | 2.18 (1.84–2.68) | 13.9 (11.6–17.3) | |
| Rest | Fick vs C2H2 | 117 |
Fick 5.3 (1.5) Rebreathing 5.6 (1.5) |
0.77 (0.69–0.84) | 0.94 (0.83–1.08) | 20.2% (17.7–23.5) | |
| Exercise | Fick vs C2H2 | 114 |
Fick 15.4 (4.8) Rebreathing 13.5 (3.7) |
0.87 (0.81–0.91) | 2.39 (2.12–2.75) | 16.5% (14.5–19.2) | |
| Rest | Thermodilution vs N2O | 54 |
Thermodilution 4.8 (0.9) N2O 4.1 (1.0) |
0.73 (0.57–0.83) | 0.64 (0.54–0.80) | 14.5 (12.0–18.2) | |
| Exercise | Thermodilution vs N2O | 62 | Thermodilution 15.8 (3.9) N2O 12.1 (2.3) | 0.82 (0.72–0.89) | 2.21 (1.88–2.69) | 15.0 (12.6–18.6) | |
| Exercise | Thermodilution vs C2H2 | 98 |
Thermodilution 15.0 (4.1) Rebreathing 13.3 (3.2) |
0.82 (0.75–0.88) | 2.36 (2.06–2.74) | 16.5% (14.3–19.4) | |
| Healthy, supine/upright rest and upright exercise | N2O vs C2H2 | 172 |
N2O 7.9 (3.8) Rebreathing 8.9 (4.2) |
0.99 (0.98–0.99) | 0.58 (0.52–0.65) | 89 (8.1–10.1) | |
C2H2 indicates acetylene; CV, coefficient of variation; N2O, nitrous oxide; Qc, cardiac output; r, Pearson correlation coefficient; and TE, typical error.
Figure 5. Comparison of the accuracy of the acetylene (C2H2) and nitrous oxide (N2O) rebreathing techniques vs the direct Fick method for assessment of Qc in healthy patients during supine rest and upright exercise.

A, Accuracy of N2O rebreathing for estimation of Qc during supine rest in healthy patients; (B) Accuracy of C2H2 rebreathing for estimation of Qc during supine rest in healthy patients; (C) Accuracy of N2O rebreathing for estimation of Qc during exercise in healthy patients; and (D) Accuracy of C2H2 rebreathing for estimation of Qc during exercise in healthy patients. Qc indicates cardiac output.
Comparison of C2H2 to N2O Rebreathing Technique
The C2H2 rebreathing and N2O rebreathing methods from the cohort of 14 young, healthy patients in the supine and upright resting positions, as well as during upright exercise, were directly compared. There was excellent agreement between the 2 with an r of 0.99 and a low TE of only 0.58 L/min (0.52–0.65) under all conditions (Table 2 and Figure 6).
Figure 6. Agreement between the (A) acetylene (C2H2) rebreathing and (B) nitrous oxide (N2O) techniques for assessment of Qc.
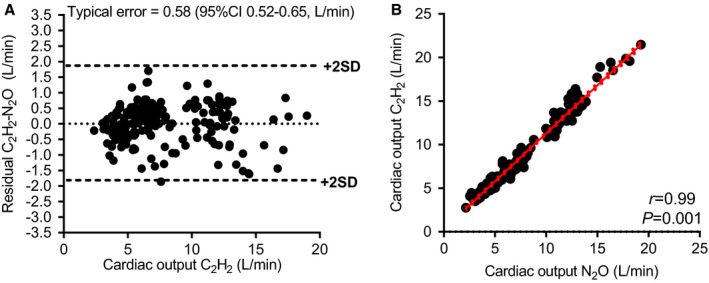
Qc indicates cardiac output.
DISCUSSION
In this study, we assessed the precision and accuracy of the C2H2 rebreathing method for estimation of Qc in a large cohort of individuals and found it to be much more precise than, and at least as accurate as, thermodilution—the most commonly used invasive method. To the best of our knowledge, this is the largest reported study to analyze methods for Qc comparison both simultaneously and under a variety of hemodynamic conditions, including both men and women across a wide age range.
Patients are referred for Qc assessment at rest and with exercise for a variety of indications (shock, dyspnea, pulmonary hypertension, HF), and important clinical decisions, including when to refer for heart transplant evaluation, rely heavily on the correct assessment of Qc. 31 The noninvasive method of assessment of Qc in our laboratory using the C2H2 rebreathing technique has a number of advantages over other available techniques that could facilitate its use: (1) the ease of use for both patients and staff (patients need to simply breathe through a mouthpiece, at a regular pace, for several breaths as instructed by easily trained staff); (2) the ability to obtain measurements in a variety of locations (ie, in a regular clinic setting or anywhere in the hospital) using a portable device without the risks associated with invasive procedures; and (3) substantially reduced overall cost compared with other available foreign gas rebreathing techniques (C2H2 gas is less expensive than other inert gasses such as N2O and sulfur hexafluoride). Moreover, the technical modification to allow the patient to determine their own inspiratory volume, which is measured at the mouthpiece, ensures a smooth and patient‐specific bag volume allowing improved rebreathing technique. Disadvantages to this technique include the need for patients to cooperate with rebreathing including the ability to tolerate a mouthpiece and additional limitations in use with patients who have significant underlying lung disease or shunt physiology.
Our data show that the C2H2 rebreathing method is much more precise than thermodilution and is comparable to the precision of the direct Fick measurement. This is likely a result of less susceptibility of the rebreathing method to measurement errors inherent to thermodilution including operator inconsistency in the rate of injection of saline, variability in the temperature of saline used, and the presence of underlying cardiac pathology (such as tricuspid regurgitation) in the patients.
Our results also demonstrate that the C2H2 rebreathing method is at least as accurate as the thermodilution method under a variety of preload and exercise conditions as evidenced by excellent correlation when the C2H2 rebreathing method is compared directly with the thermodilution method. There is a larger TE with exercise, related to higher Qc, as compared with measurements in the resting position without a significant difference in the coefficients of variation when comparing the true gold standard of the direct Fick method with the rebreathing method. In clinical practice, Qc measurements are most often assessed at rest and the variability in the rebreathing method of ≈1 L/min is acceptable. Importantly, sensitivity analyses performed in healthy patients at rest and with exercise in the upright position show that the C2H2 rebreathing method, as compared with the direct Fick method, was at least comparable to that of thermodilution. Notably, with exercise, the C2H2 rebreathing method is more accurate than thermodilution when compared with the direct Fick method, as demonstrated by a higher correlation coefficient, lower TE (nearly 10%), and smaller coefficients of variation. Additionally, we analyzed a subset of patients with clinical disease undergoing exercise in the upright position. The C2H2 rebreathing method was highly correlated with the direct Fick method with a clinically acceptable TE of just over 1 L/min (similar to that found in healthy patients at rest) even though the average Qc with exercise in our cohort of HF with preserved ejection fraction was >8 L/min.
The overall agreement between the C2H2 rebreathing method and the current clinical standards based on linear correlation is excellent, although the variability in measurements between the 2 methods ranges from 13.4% to 22.9%. This variation is multifactorial and caused by both technical sources of error inherent to each method and biologic variability of the patients based on age, sex, and medical comorbidities. Importantly, the variability of measurements between the rebreathing method and current clinical standards is not larger than those reported in prior studies involving healthy individuals and patients with clinical disease, which was up to 30%. 16 Notably, the C2H2 rebreathing technique is as accurate as the FDA‐approved N2O rebreathing technique both at rest and during exercise in our cohort of healthy patients when compared with direct Fick, thermodilution, and N2O rebreathing techniques. This close relationship should be no surprise since they are essentially the same biological technique, just using different soluble and insoluble gases. Our data suggesting similarity in accuracy and precision between various inert gasses should encourage other investigators, clinicians, and perhaps industry to consider noninvasive rebreathing techniques for assessment of Qc.
Several strengths of our study include the assessment of an ample number of men and women under a variety of loading conditions, the evaluation of patients with clinical cardiac or pulmonary disease at rest and with exercise, and the inclusion of simultaneously derived Qc data for optimal comparison with current clinical standards as well as an inert gas rebreathing method that is approved for clinical use. 13 , 17 There are also pertinent limitations to our study. The surrogate “clinical” gold standard of thermodilution was used for the majority of comparisons with the rebreathing method as the majority of our patients did not have simultaneous direct Fick measurements for analysis. Although not considered the true gold standard of the direct Fick method, the thermodilution method showed clinical utility in predicting mortality in 2 large clinical cohorts. 32
As previously noted, there are several technical sources of error inherent to the thermodilution method. However, in the subset of patients for whom we did have direct Fick measurement for comparison, there remains good correlation with thermodilution. Given this information, and the fact that thermodilution is used routinely in clinical practice, we felt that this was a valuable comparison to make. Room‐temperature saline was used as the injectate for thermodilution, which could have contributed to less precision when comparing sequential trials. 33 , 34 However, this approach mimics the technique that is used most frequently in clinical settings such as the cardiac catheterization laboratory or intensive care unit. As a matter of policy and good experimental technique, we often excluded the first few C2H2 rebreathing measurements obtained during baseline assessments in our studies as previously discussed. Importantly, this was performed at the time of each individual study as a part of the study protocol and not for the purposes of this analysis. The initial measurements were often discarded because of patient factors (inadequate breath size) and technical considerations (saturation of the mass spectrometer C2H2) and were similar to the ≈1% to 2% of the thermodilution values that were excluded from analysis for reasons such as inadequate thermodilution curves. Additionally, patients had generally practiced C2H2 rebreathing measurements for various other components of our studies before undergoing the measurements used in this analysis, which could have improved the precision of this technique under laboratory conditions.
Currently, there is not universal use of inert gas rebreathing techniques for Qc assessment. Previous, smaller studies have supported the use of inert gas rebreathing techniques in predicting clinical outcomes. 18 , 19 , 20 , 21 Given our data, we encourage other investigators and clinicians to consider this technique in studies and patient populations where accurate and precise measurement of Qc would be important (such as in patients with dyspnea of unclear cause, pulmonary hypertension, valvular heart disease, HF for risk stratification, and cardiogenic shock for confirmation and treatment). Increased use and standardization of inert gas rebreathing techniques is important as it would allow for analysis of data from larger and broader patient populations and could have strong implications for assessing prognosis in health outcomes studies.
Conclusions
The C2H2 rebreathing method is much more precise than, and at least as accurate as, the thermodilution method under a variety of conditions in healthy patients and those with clinical disease. It has an accuracy that parallels that of a commercially available, FDA‐approved N2O rebreathing technique that is currently in clinical use. Our data suggest that inert gas rebreathing techniques can be employed in Qc assessment with similar diagnostic accuracy as compared with current clinical standards. Although this study is retrospective in nature, it has allowed us to demonstrate the utility of this technique in a large number of healthy individuals and a variety of patient populations, across a broad range of age and sex, and under diverse conditions. By means of presenting these robust validation data, we hope to inspire increased confidence from the scientific community that the inert gas rebreathing technique used by our laboratory and others is reliable and valid. Our data support the use of the C2H2 rebreathing method as a precise and accurate way to noninvasively measure Qc in healthy individuals and patients with clinical disease at rest and during exercise.
Sources of Funding
Our research was supported in part by grants from the American Heart Association and the National Aeronautics and Space Administration.
Disclosures
None.
(J Am Heart Assoc. 2020;9:e015794 DOI: 10.1161/JAHA.120.015794.)
For Sources of Funding and Disclosures, see page 11.
References
- 1. Patel C, Laboy V, Venus B, Mathru M, Wier D. Acute complications of pulmonary artery catheter insertion in critically ill patients. Crit Care Med. 1986;14:195–197. [DOI] [PubMed] [Google Scholar]
- 2. Simmons R, Shephard RJ. Measurements of cardiac output in maximum exercise. Application of an acetylene rebreathing method to arm and leg exercise. Int Z Angew Physiol. 1971;29:159–172. [DOI] [PubMed] [Google Scholar]
- 3. Narang N, Thibodeau JT, Levine BD, Gore MO, Ayers CR, Lange RA, Cigarroa JE, Turer AT, de Lemos JA, McGuire DK. Inaccuracy of estimated resting oxygen uptake in the clinical setting. Circulation. 2014;129:203–210. [DOI] [PubMed] [Google Scholar]
- 4. Jarvis SS, Levine BD, Prisk GK, Shykoff BE, Elliott AR, Rosow E, Blomqvist CG, Pawelczyk JA. Simultaneous determination of the accuracy and precision of closed‐circuit cardiac output rebreathing techniques. J Appl Physiol (1985). 2007;103:867–874. [DOI] [PubMed] [Google Scholar]
- 5. Warburton DE, Haykowsky MJ, Quinney HA, Humen DP, Teo KK. Reliability and validity of measures of cardiac output during incremental to maximal aerobic exercise. Part I: conventional techniques. Sports Med. 1999;27:23–41. [DOI] [PubMed] [Google Scholar]
- 6. Laszlo G. Respiratory measurements of cardiac output: from elegant idea to useful test. J Appl Physiol (1985). 2004;96:428–437. [DOI] [PubMed] [Google Scholar]
- 7. Hsia CC, Herazo LF, Ramanathan M, Johnson RL Jr. Cardiac output during exercise measured by acetylene rebreathing, thermodilution, and Fick techniques. J Appl Physiol (1985). 1995;78:1612–1616. [DOI] [PubMed] [Google Scholar]
- 8. Triebwasser JH, Johnson RL, Burpo RP, Campbell JC, Reardon WC, Blomqvist CG. Noninvasive determination of cardiac output by a modified acetylene rebreathing procedure utilizing mass spectrometer measurements. Aviat Space Environ Med. 1977;48:203–209. [PubMed] [Google Scholar]
- 9. Liu Y, Menold E, Dullenkopf A, Reibnecker S, Lormes W, Lehmann M, Steinacker JM. Validation of the acetylene rebreathing method for measurement of cardiac output at rest and during high-intensity exercise. Clin Physiol. 1997;17:171–182. [DOI] [PubMed] [Google Scholar]
- 10. Zenger MR, Brenner M, Haruno M, Mahon D, Wilson AF. Measurement of cardiac output by automated single-breath technique, and comparison with thermodilution and Fick methods in patients with cardiac disease. Am J Cardiol. 1993;71:105–109. [DOI] [PubMed] [Google Scholar]
- 11. Gabrielsen A, Videbaek R, Schou M, Damgaard M, Kastrup J, Norsk P. Non-invasive measurement of cardiac output in heart failure patients using a new foreign gas rebreathing technique. Clin Sci (Lond). 2002;102:247–252. [PubMed] [Google Scholar]
- 12. Kallay MC, Hyde RW, Smith RJ, Rothbard RL, Schreiner BF. Cardiac output by rebreathing in patients with cardiopulmonary diseases. J Appl Physiol (1985). 1987;63:201–210. [DOI] [PubMed] [Google Scholar]
- 13. Sadeh JS, Miller A, Kukin ML. Noninvasive measurement of cardiac output by an acetylene uptake technique and simultaneous comparison with thermodilution in ICU patients. Chest. 1997;111:1295–1300. [DOI] [PubMed] [Google Scholar]
- 14. Agostoni P, Cattadori G, Apostolo A, Contini M, Palermo P, Marenzi G, Wasserman K. Noninvasive measurement of cardiac output during exercise by inert gas rebreathing technique: a new tool for heart failure evaluation. J Am Coll Cardiol. 2005;46:1779–1781. [DOI] [PubMed] [Google Scholar]
- 15. Corte TJ, Wells AU, Gatzoulis MA, Cramer D, Ward S, Macdonald RS, Dimopoulos K, Wort SJ. Non-invasive assessment of pulmonary blood flow using an inert gas rebreathing device in fibrotic lung disease. Thorax. 2010;65:341–345. [DOI] [PubMed] [Google Scholar]
- 16. Hoeper MM, Maier R, Tongers J, Niedermeyer J, Hohlfeld JM, Hamm M, Fabel H. Determination of cardiac output by the Fick method, thermodilution, and acetylene rebreathing in pulmonary hypertension. Am J Respir Crit Care Med. 1999;160:535–541. [DOI] [PubMed] [Google Scholar]
- 17. Hassan M, Wagdy K, Kharabish A, Selwanos PP, Nabil A, Elguindy A, ElFaramawy A, Elmahdy MF, Mahmoud H, Yacoub MH. Validation of noninvasive measurement of cardiac output using inert gas rebreathing in a cohort of patients with heart failure and reduced ejection fraction. Circ Heart Fail. 2017;10:e003592 DOI: 10.1161/CIRCHEARTFAILURE.116.003592. [DOI] [PubMed] [Google Scholar]
- 18. Goda A, Lang CC, Williams P, Jones M, Farr MJ, Mancini DM. Usefulness of non-invasive measurement of cardiac output during sub-maximal exercise to predict outcome in patients with chronic heart failure. Am J Cardiol. 2009;104:1556–1560. [DOI] [PubMed] [Google Scholar]
- 19. Lang CC, Karlin P, Haythe J, Lim TK, Mancini DM. Peak cardiac power output, measured noninvasively, is a powerful predictor of outcome in chronic heart failure. Circ Heart Fail. 2009;2:33–38. [DOI] [PubMed] [Google Scholar]
- 20. Lang CC, Karlin P, Haythe J, Tsao L, Mancini DM. Ease of noninvasive measurement of cardiac output coupled with peak VO2 determination at rest and during exercise in patients with heart failure. Am J Cardiol. 2007;99:404–405. [DOI] [PubMed] [Google Scholar]
- 21. Food and Drug Administration . Summary of substantial equivalence for Innocor™. Available at: https://www.accessdata.fda.gov/cdrh_docs/pdf5/K051907.pdf. Accessed April 30, 2018.
- 22. Bhella PS, Hastings JL, Fujimoto N, Shibata S, Carrick-Ranson G, Palmer MD, Boyd KN, Adams-Huet B, Levine BD. Impact of lifelong exercise "dose" on left ventricular compliance and distensibility. J Am Coll Cardiol. 2014;64:1257–1266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Fujimoto N, Hastings JL, Bhella PS, Shibata S, Gandhi NK, Carrick-Ranson G, Palmer D, Levine BD. Effect of ageing on left ventricular compliance and distensibility in healthy sedentary humans. J Physiol. 2012;590:1871–1880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Fujimoto N, Hastings JL, Carrick-Ranson G, Shafer KM, Shibata S, Bhella PS, Abdullah SM, Barkley KW, Adams-Huet B, Boyd KN, et al. Cardiovascular effects of 1 year of alagebrium and endurance exercise training in healthy older individuals. Circ Heart Fail. 2013;6:1155–1164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Fujimoto N, Prasad A, Hastings JL, Arbab-Zadeh A, Bhella PS, Shibata S, Palmer D, Levine BD. Cardiovascular effects of 1 year of progressive and vigorous exercise training in previously sedentary individuals older than 65 years of age. Circulation. 2010;122:1797–1805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Arbab-Zadeh A, Dijk E, Prasad A, Fu Q, Torres P, Zhang R, Thomas JD, Palmer D, Levine BD. Effect of aging and physical activity on left ventricular compliance. Circulation. 2004;110:1799–1805. [DOI] [PubMed] [Google Scholar]
- 27. Pawelczyk JA, Zuckerman JH, Blomqvist CG, Levine BD. Regulation of muscle sympathetic nerve activity after bed rest deconditioning. Am J Physiol Heart Circ Physiol. 2001;280:H2230–H2239. [DOI] [PubMed] [Google Scholar]
- 28. Sackner MA, Markwell G, Atkins N, Birch SJ, Fernandez RJ. Rebreathing techniques for pulmonary capillary blood flow and tissue volume. J Appl Physiol Respir Environ Exerc Physiol. 1980;49:910–915. [DOI] [PubMed] [Google Scholar]
- 29. Peyton PJ, Thompson B. Agreement of an inert gas rebreathing device with thermodilution and the direct oxygen Fick method in measurement of pulmonary blood flow. J Clin Monit Comput. 2004;18:373–378. [DOI] [PubMed] [Google Scholar]
- 30. Hopkins WG. A new view of statistics. Internet Society for Sport Science. 2016. Available at: http://www.sportsci.org/resource/stats/index.html. [Google Scholar]
- 31. Chomsky DB, Lang CC, Rayos GH, Shyr Y, Yeoh TK, Pierson RN, Davis SF, Wilson JR. Hemodynamic exercise testing. A valuable tool in the selection of cardiac transplantation candidates. Ciculation. 1996;94:3176–3183. [DOI] [PubMed] [Google Scholar]
- 32. Opotowsky AR, Hess E, Maron BA, Brittain EL, Baron AE, Maddox TM, Alshawabkeh LI, Wertheim BM, Xu M, Assad TR, et al. Thermodilution vs estimated Fick cardiac output measurement in clinical practice: an analysis of mortality from the Veterans Affairs Clinical Assessment, Reporting, and Tracking (VA CART) Program and Vanderbilt University. JAMA Cardiol. 2017;10:1090–1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Nishikawa T, Dohi S. Errors in the measurement of cardiac output by thermodilution. Can J Anaesth. 1993;40:142–153. [DOI] [PubMed] [Google Scholar]
- 34. Berthelsen PG, Eldrup N, Nilsson LB, Rasmussen JP. Thermodilution cardiac output. Cold vs room temperature injectate and the importance of measuring the injectate temperature in the right atrium. Acta Anaesthesiol Scand. 2002;46:1103–1110. [DOI] [PubMed] [Google Scholar]


