Abstract
Background
Atherosclerotic cardiovascular disease (ASCVD) has a strong association with diabetes mellitus (DM), accounting for approximately two thirds of deaths in this patient population. Many individuals with ASCVD and DM are vulnerable to financial hardship associated with treatment‐related expenses. Therefore, we examined the burden of financial hardship from medical bills across the spectrum of ASCVD status with and without DM.
Methods and Results
Using data from the National Health Interview Survey from 2013 to 2017, we used logistic regression analysis to examine the association of ASCVD and DM status with financial hardship and an inability to pay medical bills from a representative sample of non‐elderly adults in the United States. Our study population consisted of 121 672 individuals. Approximately 3.1% of the weighted population had ASCVD, 5.6% had DM, and 1.3% had both ASCVD and DM. Nearly 50% of individuals with ASCVD and DM reported financial hardship from medical bills (23% being unable to pay medical bills at all), whereas ≈28% of those with neither ASCVD nor DM reported financial hardship from medical bills (8% being unable to pay medical bills at all). Individuals with concurrent ASCVD and DM had the highest relative odds of expressing an inability to pay at all when compared with those with neither condition (odds ratio, 2.69; 95% CI, 2.21–3.28).
Conclusions
Individuals with concurrent ASCVD and DM are at a disproportionately high risk of being unable to pay their medical bills. The findings provide strong evidence for developing more effective public health policies that protect vulnerable populations from financial hardship.
Keywords: atherosclerotic cardiovascular disease, diabetes mellitus, financial hardship, medical bills, outcomes
Subject Categories: Quality and Outcomes
Nonstandard Abbreviations and Acronyms
- ASCVD
atherosclerotic cardiovascular disease
- DM
diabetes mellitus
- NHIS
National Health Interview Survey
Clinical Perspective
What Is New?
In a nationally representative sample of non‐elderly adults in the United States, ≈1‐in‐2 individuals with concurrent atherosclerotic cardiovascular disease and diabetes mellitus reported financial hardship from medical bills.
Among patients with both atherosclerotic cardiovascular disease and diabetes mellitus, representing >2.3 million individuals in the United States, nearly 1‐in‐4 were unable to pay their medical bills at all.
What Are the Clinical Implications?
Considering significant financial burden experienced by individuals with atherosclerotic cardiovascular disease and diabetes mellitus, shared decision‐making processes should leverage patients' insurance coverage and financial circumstances.
Atherosclerotic cardiovascular disease (ASCVD) is the leading cause of morbidity and mortality among individuals with diabetes mellitus (DM) and the largest contributor to direct and indirect healthcare costs associated with DM. Individuals with DM have a 2‐ to 3‐fold increased risk for ASCVD.1, 2 Despite a national healthcare system with access to statins and other lipid‐lowering medications, along with anti‐hypertensive and anti‐hyperglycemic therapies, adverse cardiovascular events rates remain higher for patients with DM than for those without DM.3, 4 With nearly 1‐in‐4 non‐elderly individuals devoting more than half of their total out‐of‐pocket healthcare spending to prescription drugs,5 this high resource utilization may translate into higher financial burden among patients with ASCVD and DM as concurrent chronic diseases.
Recent research has shown that patients with either ASCVD or DM have high medical‐related expenses that can put them at risk for financial toxicity.6 Even among those with adequate health insurance, individuals with ASCVD are inadequately protected from financial hardship because of insurance‐ and treatment‐related expenses.7 More than 45% of non‐elderly adults, or 3.9 million individuals, with ASCVD have reported financial hardship from medical bills with nearly 19% being unable to pay their medical bills at all.6 In terms of DM, the estimated national cost of DM in 2017 was ≈$327 billion, of which 73% represented direct healthcare expenditures attributable to DM.8 On average, people with diagnosed DM have medical expenditures ≈2.3 times higher than what they would be in the absence of DM or an average out‐of‐pocket expenditure of over $1800 per year.8, 9 Nearly 25% of individuals with DM are part of a family that spends >10% on health‐related expenses10 and 41% of DM patients reporting living in families with financial hardship from medical bills (15.6% being unable to pay medical bills at all).11 Individuals with DM who report financial hardship from medical bills have recently been shown to express higher rates of high financial distress, food insecurity, cost‐related medication non‐adherence, and foregone or delayed care.11
Although healthcare costs and resource utilization have been shown to be highest among individuals diagnosed with concurrent DM and ASCVD,12 the cumulative burden of financial hardship from medical bills reported by individuals with both chronic conditions remains unknown. With more than one quarter of adults having multiple chronic conditions, understanding current trends in a nationally representative sample of non‐elderly adults in the United States may provide insight into the prevalence of financial burden and its consequences, including cost‐related medication nonadherence.13, 14 Therefore, using data from the National Health Interview Survey (NHIS), we compared the prevalence of financial hardship and an inability to pay medical bills among individuals with and without ASCVD and DM.
Methods
All NHIS data and materials have been made publicly available by the Centers of Disease Control and Prevention and can be accessed at https://www.cdc.gov/nchs/nhis/index.htm.
Study Design
We used 5 years (2013–2017) of pooled data from the NHIS. The NHIS is led by the National Center for Health Statistics/Centers for Disease Control and Prevention database and is developed from annual cross‐sectional surveys disseminated nationwide.15 These surveys incorporate multi‐stage sampling to provide estimates on the population of the United States. The NHIS questionnaire is distributed into 4 central sections: Household Composition, Family Core, Sample Child Core, and Sample Adult Core. The Household Composition file contains data pertaining to basic and relationship characteristics about all individuals included in the given household. Additionally, the Family Core file collects various sociodemographic information along with fundamental markers of health status, health insurance coverage, and access to healthcare services. One child and one adult are ultimately selected at random from each family to collect more detailed information contributing to the Sample Child Core and Sample Adult Core files, respectively. In this study, we used the in‐depth data from the Sample Adult Core file, supplemented with covariates collected in other files, to analyze factors associated with financial hardship from medical bills in the US adult population. Since NHIS data are publicly available as de‐identified records, this study was exempt from review by the Yale University Institutional Review Board Committee.16
Study Population
To classify individuals with an ASCVD status, we used a self‐reported diagnosis of coronary or cerebrovascular disease. Individuals were included if they reported having coronary artery disease (“Yes” to any of the following questions: “Have you ever been told by a doctor or other health professional that you had … coronary heart disease?”, “… angina, also called angina pectoris?”, “… a heart attack (also called a myocardial infarction)?”, and/or “… stroke”). Additionally, we used self‐reported measures to determine individuals with DM. Specifically, individuals were included if they reported having DM (“Yes” to the following questions: Other than during pregnancy, have you ever been told by a doctor or other health professional that you have diabetes or sugar diabetes?”). We limited our study to focus on non‐elderly (18–64 years of age) adults with ASCVD and/or DM to analyze the financial hardship experienced by those who lack financial protections from public insurance.
Outcome Variables
Individuals who responded “Yes” to any of the following questions were classified as having financial hardship from medical bills: “In the past 12 months did you/anyone in your family have problems paying or were unable to pay any medical bills? Include bills for doctors, dentists, hospitals, therapists, medication, equipment, nursing home or home care”, and “Do you/anyone in your family currently have any medical bills that are being paid off over time? This could include medical bills being paid off with a credit card, through personal loans, or bill paying arrangements with hospitals or other providers. The bills can be from earlier years as well as this year”. Additionally, to establish the severity of the financial burden, those who answered “Yes” to the following follow‐up question were then classified as “Unable to pay medical bills at all”, what we considered to be the highest degree of financial hardship from medical bills: “Do you/Does anyone in your family currently have any medical bills that you are unable to pay at all?”, while the rest of them were classified as “financial hardship from medical bills but able to pay”.
Covariates
Covariates included in this study were age (18–39 and 40–64 years), sex, family income (middle/high income (≥200% federal poverty limit) and poor/low‐income (<200% federal poverty limit)), race/ethnicity (non‐Hispanic white, non‐Hispanic black, non‐Hispanic Asian, and Hispanic), insurance status (public, private, and uninsured), education (at least some college education and less than college education), family size (1, 2, and ≥3), region (Northeast, Midwest, South, and West), and number of chronic comorbidities. Chronic comorbidities included emphysema, chronic obstructive pulmonary disease, asthma, gastrointestinal ulcer, cancers, arthritis, and any kind of liver condition or “weak/failing” kidneys, and were categorized as having 0, 1, or ≥2.
Statistical Analysis
We used data from the Integrated Public Use Microdata Series (http://www.ipums.org) to correctly calculate variance estimation for nationally representative results, since 5 years of pooled data were used for analysis.17 Weighted proportions were used to study the prevalence of the baseline characteristics of the study population and the outcomes of interest which were compared using χ2 analysis across DM and ASCVD status. Unadjusted and adjusted logistic regressions were used to calculated odds ratios (ORs) and 95% CI to evaluate the association of financial hardship from medical bills and inability to pay bills across DM and ASCVD status. For all statistical analyses, P value of <0.05 was considered statistically significant. All analyses were conducted using Stata, version 15.1 (StataCorp, LP, College Station, Texas, USA).
Results
Our study population consisted of 121 672 individuals (aged 18–64 years), 74% of the total cohort surveyed by NHIS from 2013 to 2017. This sample represented the 193 million non‐elderly adults in the United States (Table 1). The mean age of the sample was 42±13.4 years and nearly 51% were women. Overall, 6.9% of the weighted study population had DM and 4.4% had ASCVD. On further stratification, 3.1% had ASCVD alone, 5.6% had diabetes mellitus alone, and 1.3% of the study population had both ASCVD and DM. Individuals with neither condition accounted for the remaining 90% of the study population. When comparing individuals with DM and ASCVD alone, a greater proportion of those with ASCVD reported poor/low family income and ≥2 comorbid conditions, whereas a greater proportion of those with DM reported having ≥3 family members in the household.
Table 1.
General Characteristics Among Non‐Elderly Adults by DM and ASCVD Status, From the National Health Interview Survey, 2013 to 2017
| Total | DM (−), ASCVD (−) | DM (+), ASCVD (−) | DM (−), ASCVD (+) | DM (+), ASCVD (+) | P Value | |
|---|---|---|---|---|---|---|
| Sample, N | 121 672 | 108 516 | 7251 | 4189 | 1716 | |
| Weighted sample, n (weighted %) | 192 524 324 | 173 490 379 (90%) | 10 709 141 (5.6%) | 5 905 548 (3.1%) | 2 419 256 (1.3%) | |
| Age category, n (weighted %) | <0.001 | |||||
| 18 to 39 y | 55 252 (47.7) | 53 541 (51.4) | 1051 (15.2) | 599 (15.7) | 61 (4.8) | |
| 40 to 64 y | 66 420 (52.3) | 54 975 (48.6) | 6200 (84.8) | 3590 (84.3) | 1655 (95.2) | |
| Sex, n (weighted %) | <0.001 | |||||
| Men | 56 203 (49.1) | 49 749 (48.7) | 3275 (49.5) | 2253 (57.6) | 926 (57.1) | |
| Women | 65 469 (50.9) | 58 767 (51.3) | 3976 (50.5) | 1936 (42.3) | 790 (42.9) | |
| Race/ethnicity, n (weighted %) | <0.001 | |||||
| Non‐Hispanic white | 75 156 (63.4) | 67 405 (63.6) | 3960 (57.7) | 2797 (70.4) | 994 (60.0) | |
| Non‐Hispanic black | 16 647 (13.0) | 14 176 (12.5) | 1399 (17.3) | 690 (14.8) | 382 (19.9) | |
| Non‐Hispanic Asian | 7337 (6.1) | 6870 (6.4) | 317 (5.3) | 102 (2.6) | 48 (3.3) | |
| Hispanic | 20 845 (17.5) | 18 701 (17.5) | 1380 (19.7) | 516 (12.2) | 248 (16.8) | |
| Family size, n (weighted %) | <0.001 | |||||
| 1 | 36 803 (17.1) | 32 082 (16.8) | 2408 (18.1) | 1596 (22.2) | 717 (24.5) | |
| 2 | 34 504 (28.8) | 30 117 (27.9) | 2373 (35.0) | 1415 (38.3) | 599 (38.0) | |
| ≥3 | 50 365 (54.1) | 46 317 (55.3) | 2470 (46.9) | 1178 (39.5) | 400 (37.5) | |
| Family income, n (weighted %) | <0.001 | |||||
| Middle/high‐income | 72 493 (68.5) | 66 119 (69.7) | 3796 (60.8) | 1915 (55.6) | 663 (48.7) | |
| Poor/low‐income | 41 842 (31.5) | 35 773 (30.3) | 3063 (39.2) | 2048 (44.4) | 958 (51.3) | |
| Insurance status, n (weighted %) | <0.001 | |||||
| Insured | 102 348 (85.4) | 90 830 (85.2) | 6347 (87.6) | 3587 (86.5) | 1584 (91.5) | |
| Uninsured | 18 732 (14.6) | 17 137 (14.8) | 882 (12.4) | 584 (13.5) | 129 (8.5) | |
| Education, n (weighted %) | <0.001 | |||||
| Some college or higher | 77 769 (64.1) | 71 016 (65.4) | 3830 (53.4) | 2122 (51.8) | 801 (48.1) | |
| HS/GED or less than HS | 43 479 (35.9) | 37 132 (34.6) | 3385 (46.6) | 2053 (48.2) | 909 (51.9) | |
| Region, n (weighted %) | <0.001 | |||||
| Northeast | 19 285 (17.4) | 17 353 (17.6) | 1067 (16.0) | 621 (15.4) | 244 (14.9) | |
| Midwest | 26 289 (22.5) | 23 422 (22.3) | 1553 (22.7) | 945 (24.3) | 369 (24.6) | |
| South | 43 400 (36.5) | 38 066 (36.1) | 2843 (39.6) | 1712 (41.4) | 779 (44.9) | |
| West | 32 698 (23.6) | 29 675 (24.0) | 1788 (21.7) | 911 (18.9) | 324 (15.6) | |
| Comorbidities, n (weighted %) | <0.001 | |||||
| 0 | 78 516 (66.3) | 73 616 (69.3) | 3078 (44.2) | 1439 (36.2) | 383 (24.8) | |
| 1 | 29 933 (24.0) | 25 732 (23.1) | 2413 (33.8) | 1284 (34.5) | 504 (30.3) | |
| ≥2 | 13 223 (9.6) | 9168 (7.6) | 1760 (22.0) | 1466 (32.3) | 829 (44.9) |
ASCVD indicates atherosclerotic cardiovascular disease; CRF, cardiovascular risk factor; HS, high school; and GED, general equivalency diploma.
Individuals with DM alone reported lower, but not statistically significant, rates of financial hardship from medical bills and an inability to pay bills at all when compared with individuals with ASCVD alone (financial hardship from medical bills but able to pay: 39.1% versus 43.2% and unable to pay at all: 13.9% versus 17.2%). Furthermore, 49.9% of individuals with both ASCVD and DM reported having financial hardship from medical bills (23% being unable to pay medical bills at all), whereas 28.1% of those without both ASCVD and DM reported financial hardship from medical bills (8% being unable to pay medical bills at all) (Figure 1). There were significant but minimal differences in the prevalence of financial hardship from medical bills but able to pay across DM and ASCVD status.
Figure 1. Proportion of financial hardship from medical bills and inability to pay at all by diabetes mellitus and atherosclerotic cardiovascular disease status among non‐elderly adults, from the National Health Interview Survey, 2013 to 2017.
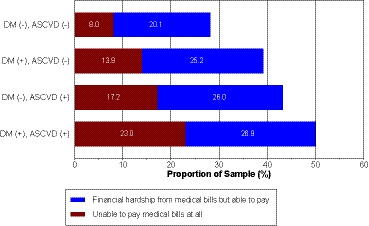
ASCVD indicates atherosclerotic cardiovascular disease; and DM, diabetes mellitus.
Table 2 depicts the prevalence of financial hardship from medical bills among the covariates across DM and ASCVD status. A notably higher prevalence of both financial hardship from medical bills was demonstrated among individuals between aged 18 and 39 years, without insurance, and with poor/low family income, ≥3 family members in the household, or ≥2 comorbid conditions. Similarly, the prevalence of being unable to pay at all was much higher among the above mentioned characteristics (Table 3). In regard to sociodemographic variations among individuals with both conditions, we found that 29.7% of non‐Hispanic black individuals with concurrent DM and ASCVD reported an inability to pay their medical bills at all, compared with 22.4% of non‐Hispanic white individuals. Moreover, our findings showed that 52.8% of uninsured individuals with both ASCVD and DM were unable to pay their medical bills at all, compared with 20.2% among individuals with insurance coverage.
Table 2.
Prevalence of Overall Financial Hardship, Among Non‐Elderly Adults by DM and ASCVD Status, From the National Health Interview Survey, 2013 to 2017
| Total | DM (−), ASCVD (−) | DM (+), ASCVD (−) | DM (−), ASCVD (+) | DM (+), ASCVD (+) | P Value | |
|---|---|---|---|---|---|---|
| Sample, n | 121 672 | 108 516 | 7251 | 4189 | 1716 | |
| Weighted sample, (weighted %) | 192 524 324 | 173 490 379 (90%) | 10 709 141 (5.6%) | 5 905 548 (3.1%) | 2 419 256 (1.3%) | |
| Age category, n (weighted %) | ||||||
| 18 to 39 y | 15 588 (30.1) | 14 903 (29.5) | 480 (44.9) | 274 (45.0) | 31 (64.1) | <0.001 |
| 40 to 64 y | 19 190 (29.2) | 14 561 (26.7) | 2312 (38.1) | 1527 (42.8) | 790 (49.2) | <0.001 |
| Sex, n (weighted %) | ||||||
| Men | 14 676 (27.9) | 12 157 (26.4) | 1178 (36.3) | 907 (41.1) | 434 (47.2) | <0.001 |
| Women | 20 102 (31.3) | 17 207 (29.7) | 1614 (41.9) | 894 (46.0) | 387 (53.5) | <0.001 |
| Race/Ethnicity, n (weighted %) | ||||||
| Non‐Hispanic white | 21 371 (29.3) | 18 122 (27.8) | 1534 (39.5) | 1236 (44.3) | 479 (50.3) | <0.001 |
| Non‐Hispanic black | 5759 (36.2) | 4657 (34.6) | 606 (45.1) | 303 (45.2) | 193 (51.9) | <0.001 |
| Non‐Hispanic Asian | 956 (14.3) | 840 (13.1) | 70 (18.6) | 26 (30.3) | 20 (54.8) | <0.001 |
| Hispanic | 6149 (31.0) | 5326 (30.0) | 519 (39.2) | 195 (35.9) | 109 (45.2) | <0.001 |
| Family size, n (weighted %) | ||||||
| 1 | 8187 (21.3) | 6382 (18.8) | 855 (35.5) | 642 (39.6) | 308 (42.8) | <0.001 |
| 2 | 9528 (26.6) | 7727 (24.6) | 908 (36.6) | 601 (41.4) | 292 (46.0) | <0.001 |
| ≥3 | 17 063 (33.9) | 15 255 (32.7) | 1029 (42.5) | 558 (46.8) | 221 (58.5) | <0.001 |
| Family income, n (weighted %) | ||||||
| Middle/high‐income | 18 781 (27.0) | 16 399 (25.9) | 1347 (35.7) | 730 (38.1) | 305 (47.9) | <0.001 |
| Poor/low‐income | 14 360 (36.5) | 11 571 (34.5) | 1320 (45.7) | 993 (50.7) | 476 (53.0) | <0.001 |
| Insurance status, n (weighted %) | ||||||
| Insured | 27 138 (27.6) | 22 668 (26.0) | 2294 (36.6) | 1451 (41.2) | 725 (48.1) | <0.001 |
| Uninsured | 7523 (42.0) | 6593 (40.4) | 491 (57.8) | 345 (56.5) | 94 (69.0) | <0.001 |
| Education, n (weighted %) | ||||||
| Some college or higher | 20 271 (26.8) | 17 570 (25.5) | 1458 (37.9) | 872 (40.6) | 371 (47.4) | <0.001 |
| HS/GED or less than HS | 14 401 (34.5) | 11 709 (33.0) | 1324 (40.5) | 922 (46.0) | 446 (52.0) | <0.001 |
| Region, n (weighted %) | ||||||
| Northeast | 4620 (22.7) | 3927 (21.6) | 347 (30.0) | 245 (34.7) | 101 (46.2) | <0.001 |
| Midwest | 8204 (33.5) | 6933 (31.8) | 680 (47.2) | 402 (44.3) | 189 (52.0) | <0.001 |
| South | 13 679 (33.7) | 11 273 (31.9) | 1191 (42.7) | 809 (48.8) | 406 (55.8) | <0.001 |
| West | 8275 (24.7) | 7231 (23.8) | 574 (30.9) | 345 (36.2) | 125 (33.3) | <0.001 |
| Comorbidities, n (weighted %) | ||||||
| 0 | 19 053 (25.9) | 17 373 (25.2) | 1023 (33.5) | 495 (35.3) | 162 (45.3) | <0.001 |
| 1 | 9871 (33.6) | 8115 (32.0) | 947 (41.2) | 560 (42.8) | 249 (51.7) | <0.001 |
| ≥2 | 5854 (44.9) | 3876 (42.5) | 822 (47.4) | 746 (52.3) | 410 (51.3) | <0.001 |
ASCVD indicates atherosclerotic cardiovascular disease; CRF, cardiovascular risk factor; HS, high school; and GED, general equivalency diploma.
Table 3.
Prevalence of an Inability to Pay Medical Bills Among Non‐Elderly Adults by DM and ASCVD Status, From the National Health Interview Survey, 2013–2017
| Total | DM (−), ASCVD (−) | DM (+), ASCVD (−) | DM (−), ASCVD (+) | DM (+), ASCVD (+) | P Value | |
|---|---|---|---|---|---|---|
| Sample, n | 121 672 | 108 516 | 7251 | 4189 | 1716 | |
| Weighted sample, (weighted %) | 192 524 324 | 173 490 379 (90%) | 10 709 141 (5.6%) | 5 905 548 (3.1%) | 2 419 256 (1.3%) | |
| Age category, n (weighted %) | ||||||
| 18 to 39 y | 4943 (9.4) | 4578 (9.0) | 241 (20.0) | 133 (19.6) | 18 (39.3) | <0.001 |
| 40 to 64 y | 5836 (8.4) | 3970 (6.9) | 840 (12.8) | 657 (16.8) | 369 (22.2) | <0.001 |
| Sex, n (weighted %) | ||||||
| Men | 4352 (8.0) | 3359 (7.2) | 435 (12.6) | 370 (15.5) | 188 (19.2) | <0.001 |
| Women | 6427 (9.7) | 5189 (8.7) | 619 (15.2) | 420 (19.6) | 199 (28.1) | <0.001 |
| Race/Ethnicity, n (weighted %) | ||||||
| Non‐Hispanic white | 5694 (7.6) | 4498 (6.8) | 498 (12.3) | 488 (15.4) | 210 (22.4) | <0.001 |
| Non‐Hispanic black | 2575 (15.9) | 1977 (14.6) | 301 (21.7) | 186 (27.7) | 111 (29.7) | <0.001 |
| Non‐Hispanic Asian | 209 (2.8) | 172 (2.5) | 17 (3.0) | 13 (11.2) | 7 (23.6) | <0.001 |
| Hispanic | 2093 (10.1) | 1749 (9.5) | 206 (14.7) | 88 (15.7) | 50 (17.5) | <0.001 |
| Family size, n (weighted %) | ||||||
| 1 | 2841 (7.2) | 2018 (5.8) | 351 (14.5) | 318 (18.6) | 154 (21.7) | <0.001 |
| 2 | 2870 (7.8) | 2184 (6.7) | 322 (12.7) | 234 (15.1) | 130 (21.2) | <0.001 |
| ≥3 | 5068 (10.0) | 4346 (9.3) | 381 (14.7) | 238 (18.4) | 103 (25.8) | <0.001 |
| Family income, n (weighted %) | ||||||
| Middle/high‐income | 3648 (5.3) | 3027 (4.8) | 312 (8.0) | 208 (9.7) | 101 (17.8) | <0.001 |
| Poor/low‐income | 6649 (17.1) | 5139 (15.7) | 691 (23.7) | 552 (27.3) | 267 (29.1) | <0.001 |
| Insurance status, n (weighted %) | ||||||
| Insured | 7093 (6.9) | 5431 (6.1) | 774 (11.6) | 572 (14.6) | 316 (20.2) | <0.001 |
| Uninsured | 3646 (20.2) | 3082 (18.9) | 277 (30.7) | 217 (34.4) | 70 (52.8) | <0.001 |
| Education, n (weighted %) | ||||||
| Some college or higher | 5275 (6.7) | 4293 (6.0) | 478 (11.8) | 353 (14.8) | 151 (19.5) | <0.001 |
| HS/GED or less than HS | 5474 (12.7) | 4232 (11.7) | 573 (16.5) | 435 (19.8) | 234 (26.3) | <0.001 |
| Region, n (weighted %) | ||||||
| Northeast | 1368 (6.5) | 1101 (6.0) | 121 (9.1) | 96 (11.6) | 50 (22.1) | <0.001 |
| Midwest | 2223 (8.6) | 1779 (7.8) | 226 (15.4) | 151 (14.7) | 67 (18.6) | <0.001 |
| South | 4949 (11.8) | 3829 (10.7) | 501 (16.8) | 396 (22.4) | 223 (29.2) | <0.001 |
| West | 2239 (6.2) | 1839 (5.6) | 206 (10.6) | 147 (13.5) | 47 (13.2) | <0.001 |
| Comorbidities, n (weighted %) | ||||||
| 0 | 5253 (6.9) | 4661 (6.6) | 337 (10.0) | 187 (13.6) | 68 (18.8) | <0.001 |
| 1 | 3136 (10.5) | 2443 (9.5) | 359 (15.7) | 231 (15.3) | 103 (21.4) | <0.001 |
| ≥2 | 2390 (17.7) | 1444 (15.6) | 358 (19.1) | 372 (24.2) | 216 (26.5) | <0.001 |
ASCVD indicates atherosclerotic cardiovascular disease; CRF, cardiovascular risk factor; HS, high school; and GED, general equivalency diploma.
After adjusting for known covariates, individuals with concurrent ASCVD and DM had the highest relative odds of expressing an inability to pay at all when compared with those with neither condition (OR, 2.69; 95% CI, 2.21–3.28). Additionally, individuals with either ASCVD or DM had higher odds of being unable to pay when compared with those with neither condition (ASCVD: OR, 1.97; 95% CI, 1.72–2.25; DM: OR, 1.70; 95% CI, 1.52–1.91) (Figure 2). On stratified analysis to control for effect‐modification, similar trends were seen in the odds of financial hardship from medical bills and inability to pay medical bills (Tables S1 and S2).
Figure 2. Odds ratios of financial hardship from medical bills by diabetes mellitus and atherosclerotic cardiovascular disease status among non‐elderly adults in the United States, from the National Health Interview Survey, 2013 to 2017.
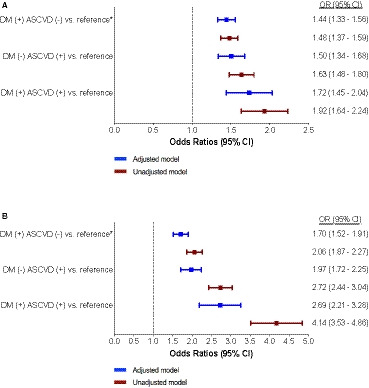
A, Odds ratios represent financial hardship from medical bills, but able to pay. B, Odds ratios represent an inability to pay medical bills at all. Adjusted models take into account age, sex, race/ethnicity, geographic region, comorbidities, family size, family income, education, and insurance status. *Reference group includes non‐elderly adults without either ASCVD or DM. ASCVD indicates atherosclerotic cardiovascular disease; DM, diabetes mellitus; OR, odds ratio.
Discussion
In a nationally representative sample of non‐elderly adults in the United States, we found that individuals with both ASCVD and DM experienced nearly a 3‐fold increase in the adjusted odds of reporting an inability to pay their medical bills at all when compared with individuals with neither ASCVD nor DM. Additionally, those with either ASCVD or DM were found to express higher relative levels of financial hardship from medical bills when compared with those with neither condition. A higher prevalence of both financial hardship and an inability to pay medical bills at all were demonstrated among individuals with a low family income as well as those without insurance coverage.
Because of rising healthcare costs, the financial burden sustained by patients and their families from medical bills has gained considerable attention nationwide. Financial hardship has been reported in various chronic conditions,18, 19 particularly with regards to cancer.20, 21, 22 Several recent studies, however, have assessed trends in financial hardship and its consequences among individuals with ASCVD.6, 17, 23, 24 Khera and colleagues, for instance, reported that among families with low‐income and a member that has ASCVD, 1‐in‐4 suffer from high financial burden, while 1‐in‐10 suffer from catastrophic financial burden, defined as expenses beyond financial means.25 Additionally, research from Valero‐Elizondo et al found that >45% of non‐elderly adults, or 3.9 million individuals, with ASCVD report financial hardship from medical bills and nearly 19% have reported being unable to pay their medical bills at all.6 These results, also using NHIS data, correspond with our findings that 43.2% of individuals with ASCVD alone report financial hardship from medical bills, and that this burden disproportionately affects racial/ethnic minorities along with uninsured individuals, and those with a lower relative family income and education status.
To our knowledge, this is the first study that has examined self‐reported financial hardship from medical bills and an inability to pay medical bills across the spectrum of ASCVD and DM status as concurrent chronic conditions. Results from our study also coincide with recent literature that has assessed the burden and consequences of financial toxicity among non‐elderly adults with DM. Caraballo and colleagues found that, among their sample of nearly 9000 individuals with DM, representing 13.1 million people annually across the United States, that 41.1% were part of families facing financial hardship from medical bills where 15.6% were unable to pay their bills at all.11 In our study, 39.1% of non‐elderly adults with DM alone faced financial hardship from medical bills. Our findings also align with the outcomes reported by Feldman and colleagues, who demonstrated that the diagnosis of DM yields significantly lower healthcare expenditures and resource utilization when compared with ASCVD and that the highest expenditure rates were among individuals with concurrent ASCVD and DM.12 Though not statistically significant, we found that individuals with ASCVD alone experienced greater financial hardship along with an inability to pay their medical bills at all than those with DM alone, when compared with the reference.
Lack of health insurance and lower family income are determinants of health accepted to predispose an individual or household to financial hardship from medical bills.7, 25 Poor overall health with greater comorbidities, lower income, and lack of health insurance have been shown to contribute to difficulty paying for health care among non‐elderly adults in the United States.26 Among individuals with ASCVD, a recent study found associations between health‐related quality of life, psychological distress, risk of depression, and self‐perception of health from the financial burden.23 In our study, we exhibited that a higher prevalence of financial hardship and an inability to pay medical bills among low income and uninsured individuals were consistent across the spectrum of ASCVD and DM status. However, it is worthwhile to note that even among those with adequate health insurance, many individuals were inadequately safeguarded from the financial hardship associated with insurance‐ and treatment‐related expenses from these conditions both together and on their own. This study affirms the need to mitigate the long‐term effects of financial toxicity, especially among those with a low income or who are uninsured.
Future studies are needed to assess the underlying differences in financial burden between ASCVD and DM and may further stratify financial hardship status by healthcare expenditures including outpatient and institutional care as well as by medications such as insulin for DM. Moreover, additional research is needed to further explore potential explanations for these trends and their consequences, particularly regarding financial toxicity among younger adults aged 18 to 39 years with concurrent chronic conditions. Though our results affirm that insurance coverage may be insufficient in protecting an individual and his or her family from financial toxicity, lower relative rates of insurance coverage among younger adults may, at least in part, help explain the observed differences in reported financial hardship and an inability to pay medical bills among those aged 18 to 39 years.27
The results of our study should be interpreted considering certain limitations. First, information pertaining to the study variables was obtained through self‐reported surveys, opening the potentiality for recall bias. Though objective questions and alternative framing methods could have added reliability to measures of financial hardship, self‐reported measures of financial burden have been used extensively in previous studies and have been shown to correspond to objective measures of out‐of‐pocket expenditures.28 Second, the diagnoses of ASCVD and DM were based on self‐report and were not validated with medical records, thus our results and weighted disease prevalence measures may be subject to misclassification bias. An underestimation of the true national prevalence of DM and ASCVD status is plausible. However, despite self‐reported ASCVD and DM, our findings are similar to other previously reported national estimates.29, 30 Lastly, because of the cross‐sectional nature of the NHIS, causality cannot be established with a plausible reverse causation and the risk for residual confounding, even after adjusting for all known confounders, cannot be disregarded.
Conclusions
Individuals with concurrent ASCVD and DM are at an elevated risk of experiencing financial hardship from medical bills, including being unable able to pay medical bills at all when compared to those with ASCVD or DM or neither. Our findings provide strong evidence for clinicians to prevent and manage DM and ASCVD concurrently while leveraging patients' financial circumstances in shared decision making processes, highlights the need for effective public health policies that protect vulnerable populations from financial hardship, and strengthens the notion that insurance coverage may not be sufficient in protecting an individual and their family from financial toxicity.
Sources of Funding
None.
Disclosures
Dr Khera is supported by the National Heart, Lung, and Blood Institute (grant 5T32HL12524702) and the National Center for Advancing Translational Sciences (grant UL1TR001105) of the National Institutes of Health. Dr Virani has received research grants from the Department of Veterans Affairs, American Heart Association, American Diabetes Association, and World Heart Federation; and has received honoraria from the American College of Cardiology (Associate Editor for Innovations, acc.org). Dr Desai is supported by grant K12 HS023000‐01 from the Agency for Healthcare Research and Quality; has received research funding from the Centers for Medicare & Medicaid Services to develop and maintain performance measures that are used for public reporting; and support from Johnson & Johnson and Medtronic, through Yale University, to develop methods of clinical trial data sharing. The remaining authors have no disclosures to report. Additionally, Dr. Nasir is supported by the Katz Academy of Translational Research.
Supporting information
Tables S1–S2
(J Am Heart Assoc. 2020;9:e015523 DOI: 10.1161/JAHA.119.015523.)
For Sources of Funding and Disclosures, see page 9.
References
- 1. Booth GL, Kapral MK, Fung K, Tu JV. Relation between age and cardiovascular disease in men and women with diabetes compared with non‐diabetic people: a population‐based retrospective cohort study. Lancet. 2006;368:29–36. [DOI] [PubMed] [Google Scholar]
- 2. Preis SR, Pencina MJ, Hwang SJ, D'Agostino RB Sr, Savage PJ, Levy D, Fox CS. Trends in cardiovascular disease risk factors in individuals with and without diabetes mellitus in the Framingham Heart Study. Circulation. 2009;120:212–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Low Wang CC, Hess CN, Hiatt WR, Goldfine AB. Clinical update: cardiovascular disease in diabetes mellitus: atherosclerotic cardiovascular disease and heart failure in type 2 diabetes mellitus—mechanisms, management, and clinical considerations. Circulation. 2016;133:2459–2502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gortmaker SL, Wang YC, Long MW, Giles CM, Ward ZJ, Barrett JL, Kenney EL, Sonneville KR, Afzal AS, Resch SC, et al. Three interventions that reduce childhood obesity are projected to save more than they cost to implement. Health Aff (Millwood). 2015;34:1932–1939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gellad WF, Donohue JM, Zhao X, Zhang Y, Banthin JS. The financial burden from prescription drugs has declined recently for the nonelderly, although it is still high for many. Health Aff (Millwood). 2012;31:408–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Valero‐Elizondo J, Khera R, Saxena A, Grandhi GR, Virani SS, Butler J, Samad Z, Desai NR, Krumholz HM, Nasir K. Financial hardship from medical bills among nonelderly U.S. adults with atherosclerotic cardiovascular disease. J Am Coll Cardiol. 2019;73:727–732. [DOI] [PubMed] [Google Scholar]
- 7. Khera R, Valero‐Elizondo J, Okunrintemi V, Saxena A, Das SR, de Lemos JA, Krumholz HM, Nasir K. Association of out‐of‐pocket annual health expenditures with financial hardship in low‐income adults with atherosclerotic cardiovascular disease in the United States. JAMA Cardiol. 2018;3:729–738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. American Diabetes A . Economic costs of diabetes in the U.S. in 2017. Diabetes Care. 2018;41:917–928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Zhuo X, Zhang P, Barker L, Albright A, Thompson TJ, Gregg E. The lifetime cost of diabetes and its implications for diabetes prevention. Diabetes Care. 2014;37:2557–2564. [DOI] [PubMed] [Google Scholar]
- 10. Li R, Barker LE, Shrestha S, Zhang P, Duru OK, Pearson‐Clarke T, Gregg EW. Changes over time in high out‐of‐pocket health care burden in U.S. adults with diabetes, 2001–2011. Diabetes Care. 2014;37:1629–1635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Caraballo C, Valero‐Elizondo J, Khera R, Mahajan S, Grandhi GR, Virani SS, Mszar R, Krumholz HM, Nasir K. Burden and consequences of financial hardship from medical bills among nonelderly adults with diabetes mellitus in the United States. Circ Cardiovasc Qual Outcomes. 2020;13:e006139. [DOI] [PubMed] [Google Scholar]
- 12. Feldman DI, Valero‐Elizondo J, Salamib JA, Rana JS, Ogunmoroti O, Okunrintemi V, Osondub CU, Spatz ES, Virani SS, Blankstein R, et al. Is diabetes mellitus equivalent to atherosclerotic cardiovascular disease from a healthcare cost perspective? Insights from the Medical Expenditure Panel Survey: 2010–2013. Cardiovasc Endocrinol Metab. 2018;7:64–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Khera R, Valero‐Elizondo J, Das SR, Virani SS, Kash BA, de Lemos JA, Krumholz HM, Nasir K. Cost‐related medication nonadherence in adults with atherosclerotic cardiovascular disease in the United States, 2013 to 2017. Circulation. 2019;140:2067–2075. [DOI] [PubMed] [Google Scholar]
- 14. Ward BW. Barriers to health care for adults with multiple chronic conditions: United States, 2012–2015. NCHS Data Brief. 2017;275:1–8. [PubMed] [Google Scholar]
- 15. NHIS Data, Questionnaires and Related Documentation. Centers for Disease Control and Prevention; Available at: https://www.cdc.gov/nchs/nhis/data-questionnaires-documentation.htm. Accessed October 6, 2018. [Google Scholar]
- 16. IRB Exemption. Available at: http://www.hhs.gov/ohrp/regulations-and-policy/decision-trees/. Accessed October 20, 2018.
- 17. Blewett L, Rivera Drew JA, Griffin R, King M, Williams K. IPUMS Health Surveys: National Health Interview Survey. Vol 6.2. Minneapolis: University of Minnesota; 2016. [Google Scholar]
- 18. Arsenijevic J, Pavlova M, Rechel B, Groot W. Catastrophic health care expenditure among older people with chronic diseases in 15 European countries. PLoS One. 2016;11:e0157765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Choi S. Experiencing financial hardship associated with medical bills and its effects on health care behavior: a 2‐year panel study. Health Educ Behav. 2018;45:616–624. [DOI] [PubMed] [Google Scholar]
- 20. Gilligan AM, Alberts DS, Roe DJ, Skrepnek GH. Death or debt? National estimates of financial toxicity in persons with newly‐diagnosed cancer. Am J Med. 2018;131:1187–1199.e1185. [DOI] [PubMed] [Google Scholar]
- 21. Cagle JG, Carr DC, Hong S, Zimmerman S. Financial burden among US households affected by cancer at the end of life. Psychooncology. 2016;25:919–926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Yabroff KR, Dowling EC, Guy GP Jr, Banegas MP, Davidoff A, Han X, Virgo KS, McNeel TS, Chawla N, Blanch‐Hartigan D, et al. Financial hardship associated with cancer in the United States: findings from a population‐based sample of adult cancer survivors. J Clin Oncol. 2016;34:259–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Annapureddy A, Valero‐Elizondo J, Khera R, Grandhi GR, Spatz ES, Dreyer RP, Desai NR, Krumholz HM, Nasir K. Association between financial burden, quality of life, and mental health among those with atherosclerotic cardiovascular disease in the United States. Circ Cardiovasc Qual Outcomes. 2018;11:e005180. [DOI] [PubMed] [Google Scholar]
- 24. Georgiou D, Budoff MJ, Kaufer E, Kennedy JM, Lu B, Brundage BH. Screening patients with chest pain in the emergency department using electron beam tomography: a follow‐up study. J Am Coll Cardiol. 2001;38:105–110. [DOI] [PubMed] [Google Scholar]
- 25. Khera R, Hong JC, Saxena A, Arrieta A, Virani SS, Blankstein R, de Lemos JA, Krumholz HM, Nasir K. Burden of catastrophic health expenditures for acute myocardial infarction and stroke among uninsured in the United States. Circulation. 2018;137:408–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Richman IB, Brodie M. A national study of burdensome health care costs among non‐elderly Americans. BMC Health Serv Res. 2014;14:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Berchick ER, Hood E, Barnett JC. Health insurance coverage in the United States: 2017. Current Population Reports Washington, DC: US Government Printing Office; 2018:60–264. [Google Scholar]
- 28. Chen JE, Lou VW, Jian H, Zhou Z, Yan M, Zhu J, Li G, He Y. Objective and subjective financial burden and its associations with health‐related quality of life among lung cancer patients. Support Care Cancer. 2018;26:1265–1272. [DOI] [PubMed] [Google Scholar]
- 29. Menke A, Casagrande S, Geiss L, Cowie CC. Prevalence of and trends in diabetes among adults in the United States, 1988–2012. JAMA. 2015;314:1021–1029. [DOI] [PubMed] [Google Scholar]
- 30. Geiss LS, Wang J, Cheng YJ, Thompson TJ, Barker L, Li Y, Albright AL, Gregg EW. Prevalence and incidence trends for diagnosed diabetes among adults aged 20 to 79 years, United States, 1980–2012. JAMA. 2014;312:1218–1226. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Tables S1–S2


