Abstract
A substantial body of research suggests that efforts to prevent pediatric obesity may benefit from targeting not just what a child eats, but how they eat. Specifically, child obesity prevention should include a component that addresses reasons why children have differing abilities to start and stop eating in response to internal cues of hunger and satiety, a construct known as eating self‐regulation. This review summarizes current knowledge regarding how caregivers can be an important influence on children's eating self‐regulation during early childhood. First, we discuss the evidence supporting an association between caregiver feeding and child eating self‐regulation. Second, we discuss what implications the current evidence has for actions caregivers may be able to take to support children's eating self‐regulation. Finally, we consider the broader social, economic, and cultural context around the feeding environment relationship and how this intersects with the implementation of any actions. As far as we are aware, this is the first American Heart Association (AHA) scientific statement to focus on a psychobehavioral approach to reducing obesity risk in young children. It is anticipated that the timely information provided in this review can be used not only by caregivers within the immediate and extended family but also by a broad range of community‐based care providers.
Keywords: AHA Scientific Statements, appetite regulation, caregivers, child, preschool, pediatric obesity, satiation
Need for Statement
A healthy body mass index (BMI) is 1 of 7 core factors that the American Heart Association emphasizes as important to ideal cardiovascular health.1 Eight percent of infants (0–2 years of age) and 23% of children (2–5 years of age) in the United States suffer from excess adiposity.2 There is wide recognition that cardiovascular disease prevention should begin in early childhood,3 with a component aimed at reducing obesity.3, 4 Behavioral dimensions of eating (“eating behaviors”), collectively describing what, when, and how much children eat, are robust correlates of childhood weight status (Table),5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53 and child obesity prevention efforts should benefit from a component focused on these. Yet, most interventions54 and/or recommendations3, 55 to reduce child obesity risk only try to manipulate what a child eats. This review has been compiled to discuss the role of caregiver feeding behaviors in shaping child eating behaviors associated with healthy body weight outcomes.
Table 1.
The Association of Appetitive Traits With Child Adiposity/Weight Status
| Appetitive Trait | Definition | Direction of Association | Evidence of Null Associations?a |
|---|---|---|---|
| Traits with consistent evidence across studies | |||
| Eating in the absence of hunger | Eating when having recently consumed a meal to satiation | Positive17, 29, 36, 37, 40, 42 | … |
| Enjoyment of food | The extent to which palatable foods provoke eating | Positive27, 28, 38 | … |
| Restrained eating | How strong attempts to restrain eating are | Inverse23, 25, 26 | |
| Satiety responsiveness | The extent to which children avoid eating, and for how long after, satiation | Positive27, 28, 38, 44 | … |
| Slowness in eating | Fewer bites per minute, usually as a meal progresses | Inverse27, 28, 38 | … |
| Traits with null studies and studies suggesting a consistent direction of association with child adiposity | |||
| Compensation of energy intake | The extent to which energy intake is reduced, following a caloric “preload” | Positive35, 46 | One exception45 |
| Desire to drink | The tendency to carry drinks (often sweetened) | Positive28, 38 | One exception47 |
| Emotional overeating | The extent of a tendency to eat in response to negative emotions | Positive27, 38 | One exception28 |
| Emotional undereating | The extent of a tendency reduce food intake in response to negative emotions | Inverse27 | Yes28, 38 |
| External eating/food responsiveness | Eating in response to external (usually food‐related stimuli) | Positive23, 26, 27, 28, 38, 44 | One exception47 |
| Food fussiness/pickiness | Selectivity regarding which foods are consumed | Positive22, 24, 27, 38, 49 and inverse10, 11, 13, 18, 20, 24, 52 both reported | Yes5, 6, 7, 8, 9, 12, 14, 15, 16, 19, 21, 28, 48, 50, 51, 53 |
To date, to the authors’ knowledge.
Focus of Statement
First, we describe available evidence on how caregiver feeding behaviors influence obesogenic child eating behaviors, adopting a developmental perspective prenatally to childhood, and consider the limitations to this evidence. In the next section, we present evidence‐based actions that caregivers may take to help provide a feeding environment that supports healthy eating behaviors in children. In the final section, we discuss challenges to implementation.
Limitations to Statement
Although a wide variety of caregiver factors may influence child eating behaviors, such as attachment quality,56 this review focuses only on caregiver factors that influence child eating behaviors within the immediate feeding environment. Although such factors also often associate with children's dietary intake, this review does not discuss how caregivers may influence children's dietary composition, quality, or variety. It is beyond the scope of this document to review any mechanisms underlying caregiver feeding and child eating behavior associations.
The Feeding Environment
Conceptual Framework
Feeding children is a reciprocal process that depends on the abilities of the caregiver and the child.56 Early observational data57, 58, 59 indicated that many children inherently vary their food intake in response to the caloric density of foods and energy expenditure to maintain healthy growth. This ability is thought to arise from the “satiety cascade,” which cues children to eat in response to hunger and stop eating in response to satiation, and a biobehavioral mechanism termed eating self‐regulation.60 Some studies refer to “regulation” over relatively short periods (eg, 24 hours, or immediately following a fixed preload meal),61 while other studies consider eating self‐regulation as children's general behavioral responses to hunger, satiation, and satiety, which can be measured over a longer term.62
Under the assumption that eating self‐regulation is present from birth (even in preterm infants63), caregivers are thought to either (1) support children's innate eating self‐regulation tendency or (2) promote a deviation from this tendency. Thus, early feeding research has focused on a didactic relationship between children and caregivers, examining the interrelationship between children's appetite cues, caregiver responsivity to these, and the effect this has on child eating self‐regulation.
At the same time, observational data57, 58, 59, 63 reveal that children vary widely in the extent to which they demonstrate eating self‐regulation, even in controlled settings. The strong heritability underlying child eating behaviors, ranging from 49% to 74% during the first year of life to 62% to 75% in early childhood (see Wood39, 64 for reviews), calls into question whether all children are born with good eating self‐regulation, and highlights the need for research into a more tailored approach to the feeding environment that reflects children's predispositions around eating. Yet it is not possible to infer the importance of environmental influences from heritability estimates. For example, the heritability for child BMI is inversely associated with parental education level65 suggesting the environmental moderation of genetic effects. Changes in the heritability of standardized BMI across childhood (≈40% at 4 years of age and 75% at 19 years of age66), thought to result from factors such as growing child autonomy over their personal food intake within the home, and increasing exposure to the wider obesogenic environment, demonstrate that heritable traits can still be influenced by the environment. When considered alongside decades of developmental science demonstrating that sociocultural context can have a powerful role in shaping a wide range of outcomes for children, including general self‐regulatory skills,67, 68, 69 these findings highlight a core concept underlying this scientific statement, which is that although strong heritability estimates suggest inherent individual differences in child eating self‐regulation, they do not negate the potential for caregivers to shape or moderate the expression of children's eating tendencies.
Caregiver Influences Underlying Child Appetitive Traits
Prenatal Influences
Prepregnancy obesity,70 maternal diet,71 and excess weight gain70 during pregnancy are all associated with increased risk of obesity among offspring. Long‐standing research suggests that what a woman eats during pregnancy not only influences children's taste preferences72, 73, 74 (with effects that can occur across their lifetime75, 76, 77), but may also influence children's growth via effects on appetite. Few human research studies exist on this topic, although higher correlations have been shown between children's protein and fat consumption at 10 years of age with their mother's intake of these macronutrients during pregnancy, than with her postnatal intake.78 However, undernutrition may also be problematic; survivors of the Dutch famine (1944–1945) who experienced caloric restriction during pregnancy saw increased obesity rates in their children up to 30 years after birth.79 Given the challenges of implementing long‐term experimental studies in humans, animal studies, which allow for much greater experimental control of exposure, have been widely used to examine the association between diet and various health and health‐related outcomes.80, 81 In animal studies, offspring of obese (but not lean) dams (female parent) who are subsequently fed a high‐fat diet for 2 to 7 years, including during gestation and lactation, may be more likely to overconsume fat and sucrose,82 be heavier at birth,83 gain more weight,82 and be more susceptible to diet‐induced obesity83 and poor glycemic control.83 Dams who are fed a low‐protein diet for discrete periods of gestation have female offspring who consume lower amounts of fat and show less compensation for changes in the caloric content of foods,84 an effect not seen in males. Animal studies suggest that a prenatal diet impacts offspring neurocircuits involved in satiety85 and alters offspring dopamine signaling.82
The Feeding Environment
After birth, psychobehavioral aspects of the feeding environment become a more important influence on child eating self‐regulation. To maintain good eating self‐regulation in children, current research suggests that a caregiver's overarching goal should be to allow children autonomy over their eating, such that they start and stop eating in response to their hunger and satiation. Yet recognizing the potential role of good dietary quality and variety in healthy growth trajectories for children,86, 87 and the availability of calorically dense, nutrient‐poor foods for many children, caregivers also need to provide structure within the eating environment such that children can be autonomous without compromising a healthy diet. It is important to acknowledge that factors such as cultural practices and beliefs (eg, preference for breastfeeding88 or about ideal body size89) and resources (eg, food insecurity that may limit food options90) can shape caregivers’ methods to achieve these goals. Thus, the challenge for caregivers is to provide structure and boundaries without decreasing children's eating autonomy to the extent that they no longer self‐regulate their eating but instead look to external factors to cue eating.
In describing the behaviors that reflect caregiver goals around child feeding/eating, the literature has made the distinction between caregiver feeding styles and caregiver feeding practices. Feeding styles (Figure) capture the overall emotional climate of meals and are measured along 2 dimensions: responsiveness (represented by warmth, acceptance, and involvement during feeding) and demandingness (represented by parental control and supervision of feeding). Feeding behaviors are often categorized using these dimensions into 4 feeding styles: authoritarian, authoritative, indulgent, and uninvolved,91 which characterize the extent to which a caregiver's overall feeding behaviors reflect responsiveness to the child within the context of boundary setting around food.91 Alternatively, feeding practices describe specific goal‐oriented behaviors and can be organized along higher‐order dimensions of coercive control (eg, pressuring children to eat), structure (eg, limit setting), and autonomy support (eg, praise, active guidance).91, 92
Figure 1.
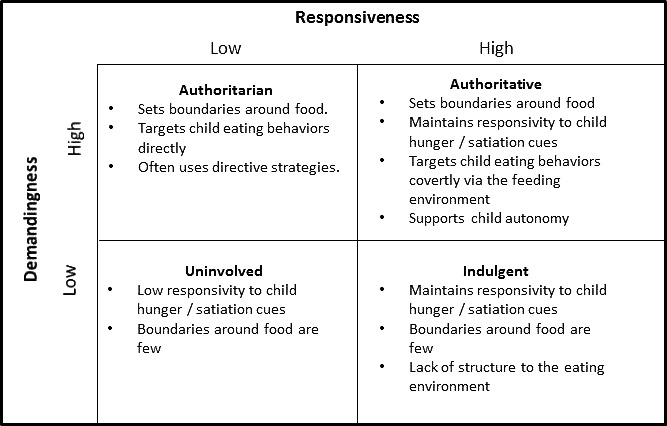
Characteristics of the feeding environments of caregivers with authoritarian, authoritative, uninvolved, and indulgent feeding styles and their relationship to the underlying dimensions of caregiver responsiveness and demandingness according to feeding style typology. 91, 92
Both authoritative and indulgent feeders are considered high in responsiveness; however, they differ in that the indulgent feeding style is low in demandingness (indicating a lack of structure; Figure).91, 93 Of the 2 styles, it is the indulgent feeding style that is associated with higher child adiposity and lower child eating self‐regulation, emphasizing the importance of setting boundaries around food.91, 94 Both authoritative and authoritarian feeders set boundaries around food (Figure),91, 93 but authoritarian parents are considered less responsive and show behaviors aiming to change the child's behavior overtly. Such overt behaviors can include using rewards and/or punishments to control food intake or physically struggling with the child, and are often labeled as directive.94, 95 Authoritative feeders also set boundaries but implement these via more covert nondirective strategies that support the child's autonomy.94, 96 These strategies include reasoning, complimenting, and exerting control over the food environment rather than the child, for example, making the most readily available foods nutrient‐dense options from which the child can make selections, and setting mealtime routines within which the child can decide how much to eat.94 When compared with the authoritarian feeding style, the authoritative style is associated with better child dietary quality.96, 97 As the key difference between these 2 styles lies in the higher responsivity of authoritative feeders to child cues, these findings highlight the need to implement boundaries within a responsive feeding environment.
A strong evidence base suggests that children's eating self‐regulation is best supported when caregivers provide a feeding environment that covertly sets boundaries around food, such as meal timing and the types of foods eaten by children.96, 98 Using overt, directive attempts to control what children eat seems to have “spill‐over” effects on how and/or how much they eat.95, 99 It seems that when children choose foods based on parental directives, they also start and stop eating in response to these and no longer self‐regulate their eating to their appetite cues. The first 5 years of life is a time of rapid development; below, we discuss how each developmental stage during this time (infancy, toddlerhood, and preschool) poses unique challenges to maintaining a structured, yet responsive, feeding environment.
Infancy
Responsive feeding is a reciprocal relationship—children need to communicate their needs for caregivers to respond to these. From infancy, children display a number of external appetite cues. The earliest hunger cues include sucking, opening/closing the mouth repeatedly, smacking and licking the lips, and increased alertness.100 Corresponding fullness cues include turning the head away, increased interest in the environment, decreased activity level, frowning and grimacing, gaze aversion, and putting hand(s) to face.100 Such cues are nonverbal and covert, and an early challenge to responsive feeding is the ability of caregivers to perceive and accurately interpret these cues, which varies considerably.101 By contrast, crying is a late‐stage feeding cue, which is widely recognized by caregivers,102, 103 but which may be confused with nonhunger infant distress. Caregivers endorsing crying as a reliable hunger cue are nearly 3 times as likely to have a pressuring feeding style, perhaps attributable to feeding when the infant is not hungry.102 Infants who are fed to soothe non–hunger‐related distress, which may sometimes be driven by caregivers mistaking distress signals for hunger, are also perceived to have a high responsiveness to food104 and may have a higher BMI in childhood.105 Interventions that have taught caregivers how to discriminate infant cues of hunger from cues of other distress and how to soothe non–hunger‐related fussiness without food have had success in supporting healthy growth.106, 107, 108 Parents of children in neonatal intensive care are more involved in feeding and show better awareness of infant distress cues after discharge when they had social support via an intervention.109
The ability of caregivers to recognize and respond to children's cues of internal hunger/satiation may be influenced by early feeding modality (bottle versus breast). Many studies refute an association between breastfeeding and child obesity risk,110, 111, 112, 113, 114, 115 which it is beyond the scope of this review to discuss. However, some studies have shown that breastfeeding is associated with better child eating self‐regulation,116 including better satiety responsiveness33, 117, 118 and a lower likelihood of emptying a bottle or cup119 than bottle feeding. Contrary findings have also been shown.120, 121 A small randomized study using weighted, opaque bottles that removed external cues to bottle fullness, resulted in less formula intake and greater maternal responsiveness to infant feeding cues compared with a standard bottle.122 This effect was seen particularly in mothers who were less responsive to infant satiation cues (defined as highly pressuring).122 It is theorized that less responsive mothers may be more susceptible to feeding in response to cues other than hunger/satiation from infants and so benefit the most from early interventions.122 In addition, in‐home recorded sessions found that breastfed infants displayed more engagement and disengagement clues than formula‐fed infants,123 perhaps making the hunger/satiation cues from infants fed at the breast easier to “read.”
Toddlerhood
The rapid development of toddlerhood enables children to communicate their appetite more overtly, such as with rudimentary language and reaching for food. Although this may make toddlers’ appetites easier to read, toddlerhood brings new challenges as children strive for autonomy and independence. Striving for autonomy is thought to bring about 2 food‐related behaviors that present a particular challenge to responsive, nondirective feeding: food neophobia (wariness of trying new foods) and food fussiness/“picky” eating (a more general selectivity regarding which foods are consumed).124 Both of these behaviors can be associated with children eating a more limited, often less unhealthy diet, and with weight status (Table).19, 21, 51, 125 Food fussiness and neophobia can involve a disgust response to disliked foods, the rejection of foods on sight, and for some children a contamination response, where disliked foods touching or hidden under liked foods may lead to rejection of the whole meal.126 Although this phase is developmentally normative and typically short‐lived,21, 127, 128 both behaviors also have traitlike dimensions that result in the persistence of these behaviors throughout childhood and adolescence for some children.127, 129 Little is understood about why food neophobia or fussiness persists in some children but not in others.124 This uncertainty, surrounding an eating behavior that is often reported as a significant source of caregiver stress,21, 130 may push caregivers to employ feeding strategies designed to reduce fussiness around food. Parents who perceive their children as more “picky” with food report using more directive attempts to control child intake than do parents who do not perceive their children as picky.21 Picky eating in toddlerhood is associated with controlling feeding practices in caregivers, with mothers who perceive their children as “picky” more likely to report restriction and pressure to eat.21, 125, 131, 132 Not only may directive feeding behaviors pose challenges to child eating self‐regulation, which can disrupt children's ability to respond to internal hunger/fullness cues, thereby contributing to overweight, but they are also associated with increased parental stress at mealtimes.130 Observational data show that stressful feeding encounters are not likely to stimulate a positive response from the child to novel and/or aversive‐tasting foods,133, 134, 135 and overall do not appear to alter children's food acceptance.134, 136, 137 Nondirective strategies such as repeatedly offering foods,52, 138, 139 offering a familiar and accepted food alongside novel or refused foods (such as ketchup140 or other palatable dip141), and having caregivers142, 143, 144 and/or peers145, 146, 147, 148, 149, 150 model eating the food with enjoyment have been demonstrated to increase the consumption of a given food, to support children's liking for a wider variety of healthy foods, and may help maintain responsivity in the feeding environment.
Preschool Period
As the child progresses into the preschool period, food neophobia and food fussiness typically decline, and a wider variety of foods are consumed. Although the increased dietary variety is considered a positive development for health, the preschool period brings more possibilities for autonomy as children can access a greater variety of foods and self‐feed more capably. Research suggests that for good child eating self‐regulation, the preschool period is critical for boundaries around food but without overt control of child eating. Directive approaches that focus on what (or the amount) a child is eating directly, such as pressure to eat certain foods or restricting the types and amount of food consumed are often well intentioned (the goal is usually to improve dietary quality, for example, vegetable intake or overall variety151). However, pressure to eat has been associated with an impaired ability to self‐regulate eating behaviors in preschool152 and poorer energy compensation in childhood.46 By contrast, restrictive feeding practices such as limiting intakes of certain (typically snack) foods, have been associated with higher consumption of food when not hungry,134 energy intake,133 adiposity,134 and likelihood of failing to stop eating when full,46 as well as poorer compensation for the energy density of food153 in early childhood. In preschool, more supportive approaches, such as questions, suggestions, and offering choices within a structured environment that limits the types of food available and the timing of meals rather than places limits on the child's eating behaviors is associated with better eating self‐regulation and growth trajectories.91
Limitations of Research
Much, but not all, of the caregiver feeding research to date is cross sectional, particularly in the preschool age group, which makes it hard to rule out confounding influences such as socioeconomic status. Yet socioeconomic status is positively correlated with rates and duration of breastfeeding in most countries154, 155 and may be inversely correlated with child obesity,156, 157 suggesting it may confound the relationships between breastfeeding and child adiposity outcomes. Similarly, mothers with obesity are less likely to initiate breastfeeding,158, 159, 160, 161 and those who do breastfeed do so for shorter periods than their healthy‐weight counterparts.158, 159, 161, 162 There may also be a confounding role for caregiver characteristics; parents with a high BMI are more likely to use controlling163, 164 and restrictive135 feeding practices. One study in 7‐ to 12‐year‐old siblings discordant for parent feeding did not support a causal role in caregiver feeding control with child obesity risk,164 which highlights the importance of considering factors in addition to caregiver feeding when developing strategies for child obesity prevention.
Even the extant longitudinal studies to date make it difficult to identify the direction of many associations. Evidence has supported directionality from child eating behaviors17, 165, 166 and child BMI53, 167, 168 to controlling feeding practices from caregivers, as well as the reverse.99, 169, 170 Taken together, this and similar evidence suggests a bidirectionality between child eating behaviors and/or adiposity and caregiver feeding behaviors, which some studies have supported.168, 171, 172 Finally, despite a strong theoretical foundation, there is relatively little empirical evidence demonstrating the benefits of approaches that reflect warmth and responsiveness to children's eating cues while providing developmentally appropriate expectations, structure, and involvement, with more focusing on the sequelae of less responsive, more directive behaviors. Relatedly, much of the extant evidence is observational and only a small number of intervention programs have demonstrated evidence of effectiveness at changing caregivers’ food‐related interactions and behaviors.107, 108, 173
Implications for Caregivers
Tremendous progress has been made linking specific aspects of the caregiver‐provided feeding environment with children's ability to self‐regulate their eating behaviors. The associated literature is now substantial and suggests that good eating self‐regulation and lowered obesity risk is supported when:
Prenatal influences on child eating self‐regulation are largely inferred from animal studies that support current advice1 that pregnancies are initiated at a healthy weight; current dietary guidelines for the intake of total calories, fats, and sugars are adhered to throughout pregnancy; and weight gain during pregnancy is kept within guideline levels.
Caregivers have knowledge of infant hunger (such as opening the mouth wide or settling into the feed100) and satiety (such as taking interest in surroundings, decreases in activity level, pulling away abruptly or detaching from the nipple, and falling asleep100) cues and can distinguish these from non–appetite‐related cues.
Caregivers are responsive to children's hunger and fullness cues, paying attention to children's verbal and nonverbal signals and not pressuring children to eat more than they wish. For a child who is not underweight (defined as having a BMI adjusted for age and sex according to published growth reference charts [zBMI] <2 SD from the World Health Organization [WHO] Median174), caregivers should allow children the choice of when to stop eating during a meal and perhaps the choice not to eat at all.
Caregivers do not focus on what or how much a child eats. Rather, a varied diet is encouraged via environmental structure such as the consistent and repeated offering of healthy foods to children, the use of “preferred” foods (such as a dip), and caregivers enthusiastically consuming the food themselves.
An appropriate structure around food is set that focuses not on child behavior specifically, but instead provides rules and limits around children's meals, via consistent snack routines, timing of meals, and selective availability of foods in the home.
Potential Challenges in Implementation
Caregivers should feel empowered to contribute to the development of a healthy eating behavior trajectory in children. However, we recognize that translating these findings into actions can face significant challenges for caregivers.
The Role of Child Development
Most children have developed the motor skills necessary to self‐feed by around 14 months of age.175 During this time, caregivers typically try to socialize children and their eating behaviors to their personal, familial, and cultural values. Such socialization is enabled by children's rapid cognitive development during early childhood, when children learn language comprehension (≈11–12 months of age176), and that others have beliefs, requests, and intentions (≈14 months of age177). However, such cognitive development also enables noncompliance with caregiver requests (the emergency of autonomy; ≈1.5 years178). Physically, height increases linearly until 4 years of age, at which time growth slows.179 However, this pattern may be different for children with a lower birth weight who experience “catch up” growth in early life, which then slows to mirror the expected trajectory.179 BMI typically has a strongly nonlinear growth trajectory, with significant changes in BMI growth rate at ≈7 to 9 months of age (peak)180 and close to 6 years of age (trough).179 Growth changes are often accompanied by changes in food consumption,181 and emerging research shows that parent feeding practices are influenced by child BMI168, 172 and child eating behaviors17 as well as the reverse. And we recognize that there are individual differences with how children transition through developmental periods and growth changes, and there is no one single healthy way. Taken together, this highlights that children's individual differences influence the feeding‐eating relationship and can pose challenges to caregiver attempts to shape healthy eating behaviors in children.
The Role of Child Characteristics
We have already shown that eating behaviors have strong heritabilities. Although a strong heritability does limit the potential for the environment to mediate the expression of child eating behaviors, we acknowledge that the downstream heritable phenotypes, such as temperament, may represent additional challenges to caregivers. There is now emerging evidence for associations between infant temperament, defined as “individual differences in reactivity and self‐regulation that are assumed to have a constitutional basis,”182 and elevated adiposity indices. Adiposity at 6, 9, and 12 months of age associates with early distress to limitations.183, 184 At 6 years of age, BMI associates with early infant low negative affectivity.184, 185 Poorer general self‐regulation and self‐soothing ability at 9 months of age has predicted BMI at ≈4 years of age.184, 186 Temperament may pose a challenge to responsive caregiver feeding practices if food is used to assuage distress105, 187 and may influence the associations of caregiver feeding with child eating behaviors, highlighting the reciprocal nature of the relationship between caregiver feeding and child eating.
The Wider Socioeconomic Context
At a broader level, caregivers who are living in poverty or in underresourced circumstances may face unique challenges to implementing recommended feeding practices. Income and socioeconomic status can influence feeding practices through many interrelated and complex pathways, including the relatively limited access to relatively more expensive healthy foods for many poor families,188 especially when such foods require time, expertise, and facilities to prepare and store.189 In addition, unpredictable job schedules can constrain meal planning and mitigate against regular routines such as family mealtimes.190, 191, 192 Food insecurity may also impact a parent's food options193 and drive caregivers to restrict the range of foods given to children to ensure consumption and avoid waste.194, 195 Living in poverty can increase caregiver stress; caregivers who are under stress have been found to engage in more restrictive feeding practices with their preschool‐aged children.196 An additional stressor that may influence caregiver feeding practices is the pressure to be a “perfect parent.” Although this has not been examined explicitly in regard to feeding, online social comparisons can negatively affect parenting and relationship outcomes, such as parental competence, coparenting relationship quality, and perceived social support.197
These social‐contextual factors shape feeding practices at multiple levels. Mental health issues, such as depression, present challenges in child feeding.197 Differences of opinion on feeding practices between caregiver and partner have been associated with conflict around feeding strategies during early childhood.198, 199 Culture may also shape which individuals are responsible for child feeding (eg, mothers versus fathers,200, 201 the role of grandparents202, 203) and beliefs about the role of restrictive versus indulgent feeding204 in achieving feeding or obesity prevention goals. This statement acknowledges that a single caregiver often does not control the child's entire feeding environment, which may pose a challenge to an individual caregiver's capacity to implement changes in their children's feeding environment. Caregivers may feel particularly frustrated when their feeding goals for their children are disrupted by others who care for the child, for example, grandparents or daycare providers.194 It may be, therefore, helpful to develop advice for caregivers that includes strategies on how to navigate such conflicts, for example, by encouraging them to explain responsive feeding practices to others involved in their child's care and/or identifying ways to respect cultural and/or family‐of‐origin influences on feeding while incorporating other options (eg, healthier preparations of traditional foods).194
Considerations
Any advice given to caregivers regarding their feeding behaviors needs to be offered within the context of implementation challenges. It is important to recognize that:
Infants and caregivers can learn from each other regarding healthy, responsive feeding practices and recognition of hunger and satiety cues, regardless of decisions about what the infant is fed.
Modifying one's feeding behaviors can be harder for some caregivers than others. Caregiver feeding behaviors are not “set” but differ on the basis of the child's temperament205 and the caregiver's psychological well‐being.206, 207 The guilt and judgment some caregivers feel when their child does not conform to their idea of “good eating behaviors”130 can be relinquished, which may ultimately encourage a more responsive partnership between the caregiver and child with feeding.
Optimal feeding strategies may differ depending on a child's genetically influenced behavioral profile, and research has not yet delineated the form this tailoring should take. A caveat to an individually tailored approach to food parenting is that being critiqued for their weight and directly encouraged to lose weight may promote poorer body self‐esteem and disordered eating in children.208 Thus, strategies should likely be adopted for the whole family.209, 210
Conclusions and Future Directions
A substantial body of literature links specific caregiver feeding behaviors to child eating self‐regulation. Overall, the current literature suggests that caregivers focus not on child characteristics (how much the child eats or their adiposity) but on creating a structured environment that inherently limits undesirable behaviors (eg, eating certain foods) without requiring overt control over children. However, such implications should be seen in light of several pressing research needs, perhaps the most pertinent of which is integrating how children's individual differences in temperament, appetite, and adiposity shape parent feeding behaviors and influence their effects on feeding self‐regulation. Caregiver feeding advice will need to be updated as such understanding increases. Further, recognizing the difficulties inherent with implementing change in the feeding environment, we encourage policies that address barriers within the wider socioeconomic context, including the social determinants of health, alongside individual caregiver efforts in child obesity prevention. Although efforts that encourage caregivers to provide a responsive, structured feeding environment could be an important component of reducing obesity and cardiometabolic risk across the life span, it is likely they will be most effective as part of a multilevel, multicomponent prevention strategy.
Disclosures
Writing Group Disclosures
| Writing Group Member | Employment | Research Grant | Other Research Support | Speakers’ Bureau/Honoraria | Expert Witness | Ownership Interest | Consultant/Advisory Board | Other |
|---|---|---|---|---|---|---|---|---|
| Alexis C. Wood | Baylor College of Medicine, Children's Nutrition Research Center | National Institutes of Health (PI/co‐I on several funded grants)†; USDA (PI/co‐I on several funded grants)†; Baylor College of Medicine (biostatistician on several pilot awards)*; Unilever*; American Academy of Pediatrics*; Sabra Dipping Company† | USDA/ARS (Cooperative Agreement 58‐3092‐5‐001)† | None | None | None | None | None |
| Emma Haycraft | Loughborough University SSEHS (United Kingdom) | None | None | None | None | None | None | None |
| Jacqueline M. Blissett | Aston University (United Kingdom) | None | None | None | None | None | None | None |
| Jeffrey M. Brunstrom | University of Bristol School of Experimental Psychology (United Kingdom) | None | None | None | None | None | None | None |
| Susan Carnell | Johns Hopkins University School of Medicine | None | None | None | None | None | None | None |
| Myles S. Faith | University at Buffalo Graduate School of Education‐Counseling and Educational Psychology | NIH contract (subcontract to University at Buffalo—contract #HHSN2752018000021)*; NIH grant (subcontract to University at Buffalo—R01NR016255)* | None | None | None | None | None | None |
| Jennifer O. Fisher | Temple University | NIH (R01 funding on sweet preferences in children)† | None | None | None | None | None | None |
| Laura L. Hayman | UMass Boston College of Nursing and Health Sciences | None | None | None | None | None | None | None |
| Sheryl O. Hughes | Baylor College of Medicine | USDA (PI of a research grant)† | None | None | None | None | None | None |
| Amrik Singh Khalsa | Nationwide Children's Hospital | Center for Innovation in Pediatric Practice at Nationwide Children's Hospital† | National Research Service Award (NRSA) granted to Cincinnati Children's Hospital Medical Center (T32 HP10027)† | None | None | None | Ohio Chapter, American Academy of Pediatrics* | Nationwide Children's Hospital (assistant professor)† |
| Alison L. Miller | University of Michigan, Ann Arbor, Michigan Health Behavior and Health Education School of Public Health | NIH (grant on parenting for children with type 1 diabetes mellitus)* | None | None | None | None | None | None |
| Shabnam R. Momin | Baylor College of Medicine | None | None | None | None | None | None | None |
| Jean A. Welsh | Emory University | None | None | None | None | None | None | None |
| Jessica G. Woo | Cincinnati Children's Hospital Medical Center | None | None | None | None | None | None | None |
This table represents the relationships of writing group members that may be perceived as actual or reasonably perceived conflicts of interest as reported on the Disclosure Questionnaire, which all members of the writing group are required to complete and submit. A relationship is considered to be “significant” if (1) the person receives $10 000 or more during any 12‐month period, or 5% or more of the person's gross income; or (2) the person owns 5% or more of the voting stock or share of the entity or owns $10 000 or more of the fair market value of the entity. A relationship is considered to be “modest” if it is less than “significant” under the preceding definition.
*Modest.
†Significant.
Reviewer Disclosures
| Reviewer | Employment | Research Grant | Other Research Support | Speakers’ Bureau/Honoraria | Expert Witness | Ownership Interest | Consultant/Advisory Board | Other |
|---|---|---|---|---|---|---|---|---|
| Stephen R. Daniels | University of Colorado, Children's Hospital Colorado | None | None | None | None | None | None | None |
| Rachel K. Johnson | University of Vermont | None | None | None | None | None | None | None |
| Tracey Ledoux | University of Houston | University of Houston (PI on study funded by UH to pilot test a wellness program for families with toddler age children)*; USDA (co‐I on project funded by USDA to develop, implement, and assess a child obesity prevention internship for Hispanic college students)*; American Cancer Society (co‐I on a study to test obesity prevention strategies among African American families through faith‐based organizations)*; United Health Foundation (co‐I on grant to deliver obesity prevention programming to an underserved community)* | None | None | None | None | None | None |
| Katherine M. Morrison | McMaster University (Canada) | CIHR (funded grant to evaluate determinants of successful outcomes in pediatric weight management programs)†; CIHR (funded grant to examine the early life influences on the gut microbiota)† | None | None | None | None | None | None |
| Reginald L. Washington | Rocky Mountain Hospital for Children | None | None | None | None | None | None | None |
This table represents the relationships of reviewers that may be perceived as actual or reasonably perceived conflicts of interest as reported on the Disclosure Questionnaire, which all reviewers are required to complete and submit. A relationship is considered to be “significant” if (1) the person receives $10 000 or more during any 12‐month period, or 5% or more of the person's gross income; or (2) the person owns 5% or more of the voting stock or share of the entity, or owns $10 000 or more of the fair market value of the entity. A relationship is considered to be “modest” if it is less than “significant” under the preceding definition.
*Modest.
†Significant.
(J Am Heart Assoc. 2020;9:e014520 DOI: 10.1161/JAHA.119.014520.)
The AHA makes every effort to avoid any actual or potential conflicts of interest that may arise as a result of an outside relationship or a personal, professional, or business interest of a member of the writing panel. Specifically, all members of the writing group are required to complete and submit a Disclosure Questionnaire showing all such relationships that might be perceived as real or potential conflicts of interest.
This statement was approved by the AHA Science Advisory and Coordinating Committee on December 3, 2019, and the AHA Executive Committee on January 31, 2020. A copy of the document is available at https://professional.heart.org/statements by using either “Search for Guidelines & Statements” or the “Browse by Topic” area.
The AHA requests that this document be cited as follows: Wood AC, Blissett JM, Brunstrom JM, Carnell S, Faith MS, Fisher JO, Hayman LL, Khalsa AS, Hughes SO, Miller AL, Momin SR, Welsh JA, Woo JG, Haycraft E; on behalf of the American Heart Association Council on Lifestyle and Cardiometabolic Health; Council on Epidemiology and Prevention; Council on Lifelong Congenital Heart Disease and Heart Health in the Young; Council on Cardiovascular and Stroke Nursing; and Stroke Council. Caregiver influences on eating behaviors in young children: a scientific statement from the American Heart Association. J Am Heart Assoc. 2020;9:e014520. DOI: 10.1161/JAHA.119.014520
The expert peer review of AHA‐commissioned documents (eg, scientific statements, clinical practice guidelines, systematic reviews) is conducted by the AHA Office of Science Operations. For more on AHA statements and guidelines development, visit https://professional.heart.org/statements. Select the “Guidelines & Statements” drop‐down menu, then click “Publication Development.”
References
- 1. Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, Floyd J, Fornage M, Gillespie C, Isasi C. Heart disease and stroke statistics‐2017 update: a report from the American Heart Association. Circulation. 2017;135:e146–e603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311:806–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kumanyika SK, Obarzanek E, Stettler N, Bell R, Field AE, Fortmann SP, Franklin BA, Gillman MW, Lewis CE, Poston WC, et al. Population‐based prevention of obesity: the need for comprehensive promotion of healthful eating, physical activity, and energy balance: a scientific statement from American Heart Association Council on Epidemiology and Prevention, Interdisciplinary Committee for Prevention (formerly the Expert Panel on Population and Prevention Science). Circulation. 2008;118:428–464. [DOI] [PubMed] [Google Scholar]
- 4. Kavey R‐EW, Daniels SR, Lauer RM, Atkins DL, Hayman LL, Taubert K. American Heart Association guidelines for primary prevention of atherosclerotic cardiovascular disease beginning in childhood. Circulation. 2003;107:1562–1566. [DOI] [PubMed] [Google Scholar]
- 5. Wright CM, Parkinson KN, Shipton D, Drewett RF. How do toddler eating problems relate to their eating behavior, food preferences, and growth? Pediatrics. 2007;120:e1069–e1075. [DOI] [PubMed] [Google Scholar]
- 6. Werthmann J, Jansen A, Havermans R, Nederkoorn C, Kremers S, Roefs A. Bits and pieces. Food texture influences food acceptance in young children. Appetite. 2015;84:181–187. [DOI] [PubMed] [Google Scholar]
- 7. Tan CC, Holub SC. Maternal feeding practices associated with food neophobia. Appetite. 2012;59:483–487. [DOI] [PubMed] [Google Scholar]
- 8. Perry RA, Mallan KM, Koo J, Mauch CE, Daniels LA, Magarey AM. Food neophobia and its association with diet quality and weight in children aged 24 months: a cross sectional study. Int J Behav Nutr Phys Act. 2015;12:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Svensson V, Lundborg L, Cao Y, Nowicka P, Marcus C, Sobko T. Obesity related eating behaviour patterns in Swedish preschool children and association with age, gender, relative weight and parental weight‐factorial validation of the children's eating behaviour questionnaire. Int J Behav Nutr Phys Act. 2011;8:134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Jansen PW, Roza SJ, Jaddoe VW, Mackenbach JD, Raat H, Hofman A, Verhulst FC, Tiemeier H. Children's eating behavior, feeding practices of parents and weight problems in early childhood: results from the population‐based Generation R study. Int J Behav Nutr Phys Act. 2012;9:130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Morrison H, Power TG, Nicklas T, Hughes SO. Exploring the effects of maternal eating patterns on maternal feeding and child eating. Appetite. 2013;63:77–83. [DOI] [PubMed] [Google Scholar]
- 12. Moroshko I, Brennan L. Maternal controlling feeding behaviours and child eating in preschool‐aged children. Nut Dietetics. 2013;70:49–53. [Google Scholar]
- 13. Mackenbach JD, Tiemeier H, van der Ende J, Nijs IM, Jaddoe VW, Hofman A, Verhulst FC, Jansen PW. Relation of emotional and behavioral problems with body mass index in preschool children: the Generation R study. J Dev Behav Pediatr. 2012;33:641–648. [DOI] [PubMed] [Google Scholar]
- 14. Lewinsohn PM, Holm‐Denoma JM, Gau JM, Joiner TE Jr, Striegel‐Moore R, Bear P, Lamoureux B. Problematic eating and feeding behaviors of 36‐month‐old children. Int J Eat Disord. 2005;38:208–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Johnson SL, Davies PL, Boles RE, Gavin WJ, Bellows LL. Young children's food neophobia characteristics and sensory behaviors are related to their food intake. J Nutr. 2015;145:2610–2616. [DOI] [PubMed] [Google Scholar]
- 16. Carruth BR, Skinner JD. Revisiting the picky eater phenomenon: neophobic behaviors of young children. J Am Coll Nutr. 2000;19:771–780. [DOI] [PubMed] [Google Scholar]
- 17. Bauer KW, Haines J, Miller AL, Rosenblum K, Appugliese DP, Lumeng JC, Kaciroti NA. Maternal restrictive feeding and eating in the absence of hunger among toddlers: a cohort study. Int J Behav Nutr Phys Act. 2017;14:172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ekstein S, Laniado D, Glick B. Does picky eating affect weight‐for‐length measurements in young children? Clin Pediatr. 2010;49:217–220. [DOI] [PubMed] [Google Scholar]
- 19. Jacobi C, Agras WS, Bryson S, Hammer LD. Behavioral validation, precursors, and concomitants of picky eating in childhood. J Am Acad Child Adolesc Psychiatry. 2003;42:76–84. [DOI] [PubMed] [Google Scholar]
- 20. Antoniou E, Roefs A, Kremers S, Jansen A, Gubbels J, Sleddens E, Thijs C. Picky eating and child weight status development: a longitudinal study. J Hum Nutr Diet. 2016;29:298–307. [DOI] [PubMed] [Google Scholar]
- 21. Mascola AJ, Bryson SW, Agras WS. Picky eating during childhood: a longitudinal study to age 11 years. Eat Behav. 2010;11:253–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Finistrella V, Manco M, Ferrara A, Rustico C, Presaghi F, Morino G. Cross‐sectional exploration of maternal reports of food neophobia and pickiness in preschooler‐mother dyads. J Am Coll Nutr. 2012;31:152–159. [DOI] [PubMed] [Google Scholar]
- 23. Baños R, Cebolla A, Etchemendy E, Felipe S, Rasal P, Botella C. Validation of the Dutch Eating Behavior Questionnaire for Children (DEBQ‐C) for use with Spanish children. Nutr Hosp. 2011;26:890–898. [DOI] [PubMed] [Google Scholar]
- 24. Dubois L, Farmer A, Girard M, Peterson K, Tatone‐Tokuda F. Problem eating behaviors related to social factors and body weight in preschool children: a longitudinal study. Int J Behav Nutr Phys Act. 2007;4:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. van Strien T, Oosterveld P. The children's DEBQ for assessment of restrained, emotional, and external eating in 7‐ to 12‐year‐old children. Int J Eat Disord. 2008;41:72–81. [DOI] [PubMed] [Google Scholar]
- 26. Braet C, Van Strien T. Assessment of emotional, externally induced and restrained eating behaviour in nine to twelve‐year‐old obese and non‐obese children. Behav Res Ther. 1997;35:863–873. [DOI] [PubMed] [Google Scholar]
- 27. Viana V, Sinde S, Saxton JC. Children's eating behaviour questionnaire: associations with BMI in Portuguese children. Br J Nutr. 2008;100:445–450. [DOI] [PubMed] [Google Scholar]
- 28. Sleddens EF, Kremers SP, Thijs C. The children's eating behaviour questionnaire: factorial validity and association with body mass index in Dutch children aged 6‐7. Int J Behav Nutr Phys Act. 2008;5:49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Fisher JO, Cai G, Jaramillo SJ, Cole SA, Comuzzie AG, Butte NF. Heritability of hyperphagic eating behavior and appetite‐related hormones among Hispanic children. Obesity. 2007;15:1484–1495. Available at: 10.1038/oby.2007.177. [DOI] [PubMed] [Google Scholar]
- 30. Santos JL, Ho‐Urriola JA, Gonzalez A, Smalley SV, Dominguez‐Vasquez P, Cataldo R, Obregon AM, Amador P, Weisstaub G, Hodgson MI. Association between eating behavior scores and obesity in Chilean children. Nutr J. 2011;10:108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. van Jaarsveld CH, Boniface D, Llewellyn CH, Wardle J. Appetite and growth: a longitudinal sibling analysis. JAMA Pediatr. 2014;168:345–350. [DOI] [PubMed] [Google Scholar]
- 32. Faith MS, Hittner JB. Infant temperament and eating style predict change in standardized weight status and obesity risk at 6 years of age. Int J Obes (Lond). 2010;34:1515–1523. [DOI] [PubMed] [Google Scholar]
- 33. Reyes M, Hoyos V, Martinez SM, Lozoff B, Castillo M, Burrows R, Blanco E, Gahagan S. Satiety responsiveness and eating behavior among Chilean adolescents and the role of breastfeeding. Int J Obes (Lond). 2014;38:552–557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Remy E, Issanchou S, Chabanet C, Boggio V, Nicklaus S. Impact of adiposity, age, sex and maternal feeding practices on eating in the absence of hunger and caloric compensation in preschool children. Int J Obes. 2015;39:925–930. [DOI] [PubMed] [Google Scholar]
- 35. Kral TV, Allison DB, Birch LL, Stallings VA, Moore RH, Faith MS. Caloric compensation and eating in the absence of hunger in 5‐ to 12‐y‐old weight‐discordant siblings. Am J Clin Nutr. 2012;96:574–583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Faith MS, Berkowitz RI, Stallings VA, Kerns J, Storey M, Stunkard AJ. Eating in the absence of hunger: a genetic marker for childhood obesity in prepubertal boys? Obesity (Silver Spring). 2006;14:131–138. [DOI] [PubMed] [Google Scholar]
- 37. Butte NF, Cai G, Cole SA, Wilson TA, Fisher JO, Zakeri IF, Ellis KJ, Comuzzie AG. Metabolic and behavioral predictors of weight gain in Hispanic children: the viva la familia study. Am J Clin Nutr. 2007;85:1478–1485. [DOI] [PubMed] [Google Scholar]
- 38. Webber L, Hill C, Saxton J, Van Jaarsveld CH, Wardle J. Eating behaviour and weight in children. Int J Obes (Lond). 2009;33:21–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Wood AC. Appetitive traits: Genetic contributions to pediatric eating behaviors In: Lumeng JC, Fisher JO, eds. Pediatric Food Preferences and Eating Behaviors. New York, NY: Elsevier Inc; 2018:127–146. [Google Scholar]
- 40. Fisher JO, Birch LL. Eating in the absence of hunger and overweight in girls from 5 to 7 y of age. Am J Clin Nutr. 2002;76:226–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Croker H, Cooke L, Wardle J. Appetitive behaviours of children attending obesity treatment. Appetite. 2011;57:525–529. [DOI] [PubMed] [Google Scholar]
- 42. Hill C, Llewellyn CH, Saxton J, Webber L, Semmler C, Carnell S, van Jaarsveld CH, Boniface D, Wardle J. Adiposity and “eating in the absence of hunger” in children. Int J Obes (Lond). 2008;32:1499–1505. [DOI] [PubMed] [Google Scholar]
- 43. Carnell S, Wardle J. Appetitive traits in children. New evidence for associations with weight and a common, obesity‐associated genetic variant. Appetite. 2009;53:260–263. [DOI] [PubMed] [Google Scholar]
- 44. Carnell S, Wardle J. Appetite and adiposity in children: evidence for a behavioral susceptibility theory of obesity. Am J Clin Nutr. 2008;88:22–29. [DOI] [PubMed] [Google Scholar]
- 45. Johnson SL, Taylor‐Holloway LA. Non‐Hispanic white and Hispanic elementary school children's self‐regulation of energy intake. Am J Clin Nutr. 2006;83:1276–1282. [DOI] [PubMed] [Google Scholar]
- 46. Johnson SL, Birch LL. Parents’ and children's adiposity and eating style. Pediatrics. 1994;94:653–661. [PubMed] [Google Scholar]
- 47. Powers SW, Chamberlin LA, Schaick KB, Sherman SN, Whitaker RC. Maternal feeding strategies, child eating behaviors, and child BMI in low‐income African‐American preschoolers. Obesity. 2006;14:2026–2033. [DOI] [PubMed] [Google Scholar]
- 48. Rydell A‐M, Dahl M, Sundelin C. Characteristics of school children who are choosy eaters. J Genet Psychol. 1995;156:217–229. [DOI] [PubMed] [Google Scholar]
- 49. Jiang X, Yang X, Zhang Y, Wang B, Sun L, Shang L. Development and preliminary validation of Chinese preschoolers’ eating behavior questionnaire. PLoS One. 2014;9:e88255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Cao Y‐T, Svensson V, Marcus C, Zhang J, Zhang J‐D, Sobko T. Eating behaviour patterns in Chinese children aged 12‐18 months and association with relative weight‐factorial validation of the children's eating behaviour questionnaire. Int J Behav Nutr Phys Act. 2012;9:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Carruth BR, Skinner J, Houck K, Moran J 3rd, Coletta F, Ott D. The phenomenon of “picky eater”: a behavioral marker in eating patterns of toddlers. J Am Coll Nutr. 1998;17:180–186. [DOI] [PubMed] [Google Scholar]
- 52. Carruth BR, Ziegler PJ, Gordon A, Barr SI. Prevalence of picky eaters among infants and toddlers and their caregivers’ decisions about offering a new food. J Am Diet Assoc. 2004;104:57–64. [DOI] [PubMed] [Google Scholar]
- 53. Gregory JE, Paxton SJ, Brozovic AM. Maternal feeding practices, child eating behaviour and body mass index in preschool‐aged children: a prospective analysis. Int J Behav Nutr Phys Act. 2010;7:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Wang Y, Wu Y, Wilson RF, Bleich S, Cheskin L, Weston C, Showell N, Fawole O, Lau B, Segal J. Childhood obesity prevention programs: comparative effectiveness review and meta‐analysis. Database of abstracts of reviews of effects (dare): Quality‐assessed reviews [internet] Centre for Reviews and Dissemination (UK); 2013. [PubMed]
- 55. Williams CL, Hayman LL, Daniels SR, Robinson TN, Steinberger J, Paridon S, Bazzarre T. Cardiovascular health in childhood: a statement for health professionals from the Committee on Atherosclerosis, Hypertension, and Obesity in the Young (AHOY) of the Council on Cardiovascular Disease in the Young, American Heart Association. Circulation. 2002;106:143–160. [DOI] [PubMed] [Google Scholar]
- 56. Satter E. Feeding dynamics: helping children to eat well. J Pediatr Health Care. 1995;9:178–184. [DOI] [PubMed] [Google Scholar]
- 57. Timby N, Hernell O, Lonnerdal B, Domellof M. Parental feeding control in relation to feeding mode and growth pattern during early infancy. Acta Paediatr. 2014;103:1072–1077. [DOI] [PubMed] [Google Scholar]
- 58. Birch LL, Fisher JO. Development of eating behaviors among children and adolescents. Pediatrics. 1998;101:539–549. [PubMed] [Google Scholar]
- 59. Fomon SJ, Filer LJ, Thomas LN, Anderson TA, Nelson SE. Influence of formula concentration on caloric intake and growth of normal infants. Acta Paediatr. 1975;64:172–181. [DOI] [PubMed] [Google Scholar]
- 60. Blundell J, Lawton C, Hill A. Mechanisms of appetite control and their abnormalities in obese patients. Hormone Res Paediatr. 1993;39:72–76. [DOI] [PubMed] [Google Scholar]
- 61. Johnson SL. Improving preschoolers’ self‐regulation of energy intake. Pediatrics. 2000;106:1429–1435. [DOI] [PubMed] [Google Scholar]
- 62. Connell LE, Francis LA. Positive parenting mitigates the effects of poor self‐regulation on body mass index trajectories from ages 4–15 years. Health Psychol. 2014;33:757–764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Saunders RB, Friedman CB, Stramoski PR. Feeding preterm infants: schedule or demand? J Obstet Gynecol Neonatal Nurs. 1991;20:212–220. [DOI] [PubMed] [Google Scholar]
- 64. Wood AC. Gene‐environment interplay in child eating behaviors: what the role of “nature” means for the effects of “nurture.” Curren Nutr Rep. 2018;7:294–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Silventoinen K, Huppertz C, van Beijsterveldt CE, Bartels M, Willemsen G, Boomsma DI. The genetic architecture of body mass index from infancy to adulthood modified by parental education. Obesity. 2016;24:2004–2011. [DOI] [PubMed] [Google Scholar]
- 66. Silventoinen K, Jelenkovic A, Sund R, Hur Y‐M, Yokoyama Y, Honda C, Hjelmborg JV, Möller S, Ooki S, Aaltonen S. Genetic and environmental effects on body mass index from infancy to the onset of adulthood: an individual‐based pooled analysis of 45 twin cohorts participating in the collaborative project of development of anthropometrical measures in twins (CODATwins) study. Am J Clin Nutr. 2016;104:371–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Raver CC. Placing emotional self‐regulation in sociocultural and socioeconomic contexts. Child Dev. 2004;75:346–353. [DOI] [PubMed] [Google Scholar]
- 68. Calkins SD, Hill A. Caregiver influences on emerging emotion regulation: biological and environmental transactions in early development In: Gross JJ, ed. Handbook of Emotion Regulation. New York, NY: The Guilford Press; 2007:229–248. [Google Scholar]
- 69. Bernier A, Carlson SM, Whipple N. From external regulation to self‐regulation: early parenting precursors of young children's executive functioning. Child Dev. 2010;81:326–339. [DOI] [PubMed] [Google Scholar]
- 70. Reynolds RM, Osmond C, Phillips DIW, Godfrey KM. Maternal BMI, parity, and pregnancy weight gain: influences on offspring adiposity in young adulthood. J Clin Endocrinol Metab. 2010;95:5365–5369. [DOI] [PubMed] [Google Scholar]
- 71. Shapiro AL, Kaar JL, Crume TL, Starling AP, Siega‐Riz AM, Ringham BM, Glueck DH, Norris JM, Barbour LA, Friedman J. Maternal diet quality in pregnancy and neonatal adiposity: the healthy start study. Int J Obes. 2016;40:1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Mennella JA, Johnson A, Beauchamp GK. Garlic ingestion by pregnant women alters the odor of amniotic fluid. Chem Senses. 1995;20:207–209. [DOI] [PubMed] [Google Scholar]
- 73. Mennella JA, Jagnow CP, Beauchamp GK. Prenatal and postnatal flavor learning by human infants. Pediatrics. 2001;107:e88–e88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Mennella JA, Beauchamp GK. Understanding the origin of flavor preferences. Chem Senses. 2005;30:i242–i243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Loper HB, La Sala M, Dotson C, Steinle N. Taste perception, associated hormonal modulation, and nutrient intake. Nutr Rev. 2015;73:83–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Zhang G‐H, Chen M‐L, Liu S‐S, Zhan Y‐H, Quan Y, Qin Y‐M, Deng S‐P. Effects of mother's dietary exposure to acesulfame‐K in pregnancy or lactation on the adult offspring's sweet preference. Chem Senses. 2011;36:763–770. [DOI] [PubMed] [Google Scholar]
- 77. Teegarden SL, Scott AN, Bale TL. Early life exposure to a high fat diet promotes long‐term changes in dietary preferences and central reward signaling. Neuroscience. 2009;162:924–932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Brion M‐JA, Ness AR, Rogers I, Emmett P, Cribb V, Davey Smith G, Lawlor DA. Maternal macronutrient and energy intakes in pregnancy and offspring intake at 10 y: exploring parental comparisons and prenatal effects. Am J Clin Nutr. 2010;91:748–756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Roseboom T, de Rooij S, Painter R. The Dutch famine and its long‐term consequences for adult health. Early Hum Dev. 2006;82:485–491. [DOI] [PubMed] [Google Scholar]
- 80. Lai M, Chandrasekera PC, Barnard ND. You are what you eat, or are you? The challenges of translating high‐fat‐fed rodents to human obesity and diabetes. Nutr Diabet. 2014;4:e135–e135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Even PC, Virtue S, Morton NM, Fromentin G, Semple RK. Are rodent models fit for investigation of human obesity and related diseases? Front Nutr. 2017;4:58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Rivera HM, Kievit P, Kirigiti MA, Bauman LA, Baquero K, Blundell P, Dean TA, Valleau JC, Takahashi DL, Frazee T, et al. Maternal high‐fat diet and obesity impact palatable food intake and dopamine signaling in nonhuman primate offspring. Obesity. 2015;23:2157–2164. Available at: 10.1002/oby.21306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Tamashiro KL, Terrillion CE, Hyun J, Koenig JI, Moran TH. Prenatal stress or high‐fat diet increases susceptibility to diet‐induced obesity in rat offspring. Diabetes. 2009;58:1116–1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Bellinger L, Lilley C, Langley‐Evans SC. Prenatal exposure to a maternal low‐protein diet programmes a preference for high‐fat foods in the young adult rat. Br J Nutr. 2004;92:513–520. [DOI] [PubMed] [Google Scholar]
- 85. Bhagat R, Fortna SR, Browning KN. Exposure to a high fat diet during the perinatal period alters vagal motoneurone excitability, even in the absence of obesity. J Physiol. 2015;593:285–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Golley RK, Smithers LG, Mittinty MN, Emmett P, Northstone K, Lynch JW. Diet quality of UK infants is associated with dietary, adiposity, cardiovascular, and cognitive outcomes measured at 7–8 years of age. J Nutr. 2013;143:1611–1617. [DOI] [PubMed] [Google Scholar]
- 87. Okubo H, Crozier SR, Harvey NC, Godfrey KM, Inskip HM, Cooper C, Robinson SM. Diet quality across early childhood and adiposity at 6 years: the Southampton Women's Survey. Int J Obes. 2015;39:1456–1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Reeves EA, Woods‐Giscombé CL. Infant‐feeding practices among African American women: social‐ecological analysis and implications for practice. J Transcult Nurs. 2015;26:219–226. [DOI] [PubMed] [Google Scholar]
- 89. Rosas LG, Harley KG, Guendelman S, Fernald LC, Mejia F, Eskenazi B. Maternal perception of child weight among Mexicans in California and Mexico. Matern Child Health J. 2010;14:886–894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Chen W‐t. From “junk food” to “treats” how poverty shapes family food practices. Food Cult Soc. 2016;19:151–170. [Google Scholar]
- 91. Hughes SO, Power TG, Papaioannou MA, Cross MB, Nicklas TA, Hall SK, Shewchuk RM. Emotional climate, feeding practices, and feeding styles: an observational analysis of the dinner meal in head start families. Int J Behav Nutr Phys Act. 2011;8:60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Vaughn AE, Ward DS, Fisher JO, Faith MS, Hughes SO, Kremers SP, Musher‐Eizenman DR, O'Connor TM, Patrick H, Power TG. Fundamental constructs in food parenting practices: a content map to guide future research. Nutr Rev. 2015;74:98–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Hughes SO, Power TG, Orlet Fisher J, Mueller S, Nicklas TA. Revisiting a neglected construct: parenting styles in a child‐feeding context. Appetite. 2005;44:83–92. [DOI] [PubMed] [Google Scholar]
- 94. Hughes SO, Shewchuk RM, Baskin ML, Nicklas TA, Qu H. Indulgent feeding style and children's weight status in preschool. J Develop Behav Pediatr. 2008;29:403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Loth K, Friend S, Horning M, Neumark‐Sztainer D, Fulkerson J. Directive and non‐directive food‐related parenting practices: associations between an expanded conceptualization of food‐related parenting practices and child dietary intake and weight outcomes. Appetite. 2016;107:188–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Patrick H, Nicklas TA, Hughes SO, Morales M. The benefits of authoritative feeding style: caregiver feeding styles and children's food consumption patterns. Appetite. 2005;44:243–249. [DOI] [PubMed] [Google Scholar]
- 97. Arlinghaus KR, Vollrath K, Hernandez DC, Momin SR, O'Connor TM, Power TG, Hughes SO. Authoritative parent feeding style is associated with better child dietary quality at dinner among low‐income minority families. Am J Clin Nutr. 2018;108:730–736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Brown KA, Ogden J, Vögele C, Gibson EL. The role of parental control practices in explaining children's diet and BMI. Appetite. 2008;50:252–259. [DOI] [PubMed] [Google Scholar]
- 99. Rodgers RF, Paxton SJ, Massey R, Campbell KJ, Wertheim EH, Skouteris H, Gibbons K. Maternal feeding practices predict weight gain and obesogenic eating behaviors in young children: a prospective study. Int J Behav Nutr Phys Act. 2013;10:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Hodges EA, Wasser HM, Colgan BK, Bentley ME. Development of feeding cues during infancy and toddlerhood. MCN Am J Matern Child Nurs. 2016;41:244–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Hodges EA, Hughes SO, Hopkinson J, Fisher JO. Maternal decisions about the initiation and termination of infant feeding. Appetite. 2008;50:333–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Gross RS, Fierman AH, Mendelsohn AL, Chiasson MA, Rosenberg TJ, Scheinmann R, Messito MJ. Maternal perceptions of infant hunger, satiety, and pressuring feeding styles in an urban Latina WIC population. Acad Pediatr. 2010;10:29–35. [DOI] [PubMed] [Google Scholar]
- 103. Pridham KF, Berger Knight C, Stephenson GR. Mothers’ working models of infant feeding: description and influencing factors. J Adv Nurs. 1989;14:1051–1061. [DOI] [PubMed] [Google Scholar]
- 104. Mallan KM, Sullivan SE, Susan J, Daniels LA. The relationship between maternal feeding beliefs and practices and perceptions of infant eating behaviours at 4 months. Appetite. 2016;105:1–7. [DOI] [PubMed] [Google Scholar]
- 105. Stifter CA, Anzman‐Frasca S, Birch LL, Voegtline K. Parent use of food to soothe infant/toddler distress and child weight status. An exploratory study. Appetite. 2011;57:693–699. [DOI] [PubMed] [Google Scholar]
- 106. Paul IM, Savage JS, Anzman SL, Beiler JS, Marini ME, Stokes JL, Birch LL. Preventing obesity during infancy: a pilot study. Obesity. 2011;19:353–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Savage JS, Birch LL, Marini M, Anzman‐Frasca S, Paul IM. Effect of the insight responsive parenting intervention on rapid infant weight gain and overweight status at age 1 year: a randomized clinical trial. JAMA Pediatr. 2016;170:742–749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Hohman EE, Paul IM, Birch LL, Savage JS. Insight responsive parenting intervention is associated with healthier patterns of dietary exposures in infants. Obesity. 2017;25:185–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Olmsted RW, Minde K, Shosenberg N, Marton P, Thompson J, Ripley J, Burns S. Self‐help groups in a premature nursery—a controlled evaluation. J Pediatr. 1980;96:933–940. [DOI] [PubMed] [Google Scholar]
- 110. Brion M‐JA, Lawlor DA, Matijasevich A, Horta B, Anselmi L, Araújo CL, Menezes AMB, Victora CG, Smith GD. What are the causal effects of breastfeeding on IQ, obesity and blood pressure? Evidence from comparing high‐income with middle‐income cohorts. Int J Epidemiol. 2011;40:670–680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Colen CG, Ramey DM. Is breast truly best? Estimating the effects of breastfeeding on long‐term child health and wellbeing in the United States using sibling comparisons. Soc Sci Med. 2014;109:55–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Kramer MS, Guo T, Platt RW, Sevkovskaya Z, Dzikovich I, Collet J‐P, Shapiro S, Chalmers B, Hodnett E, Vanilovich I. Infant growth and health outcomes associated with 3 compared with 6 mo of exclusive breastfeeding. Am J Clin Nutr. 2003;78:291–295. [DOI] [PubMed] [Google Scholar]
- 113. Kramer MS, Matush L, Vanilovich I, Platt RW, Bogdanovich N, Sevkovskaya Z, Dzikovich I, Shishko G, Collet J‐P, Martin RM. Effects of prolonged and exclusive breastfeeding on child height, weight, adiposity, and blood pressure at age 6.5 y: evidence from a large randomized trial. Am J Clin Nutr. 2007;86:1717–1721. [DOI] [PubMed] [Google Scholar]
- 114. Oken E, Patel R, Guthrie LB, Vilchuck K, Bogdanovich N, Sergeichick N, Palmer TM, Kramer MS, Martin RM. Effects of an intervention to promote breastfeeding on maternal adiposity and blood pressure at 11.5 y postpartum: results from the Promotion of Breastfeeding Intervention Trial, a cluster‐randomized controlled trial. Am J Clin Nutr. 2013;98:1048–1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Martin RM, Kramer MS, Patel R, Rifas‐Shiman SL, Thompson J, Yang S, Vilchuck K, Bogdanovich N, Hameza M, Tilling K, et al. Effects of promoting long‐term, exclusive breastfeeding on adolescent adiposity, blood pressure, and growth trajectories: a secondary analysis of a randomized clinical trial. JAMA Pediatr. 2017;171:e170698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. DiSantis KI, Collins BN, Fisher JO, Davey A. Do infants fed directly from the breast have improved appetite regulation and slower growth during early childhood compared with infants fed from a bottle? Int J Behav Nutr Phys Act. 2011;8:89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Brown A, Lee M. Early influences on child satiety‐responsiveness: the role of weaning style. Pediatr Obes. 2015;10:57–66. [DOI] [PubMed] [Google Scholar]
- 118. Brown A, Lee M. Breastfeeding during the first year promotes satiety responsiveness in children aged 18‐24 months. Pediatr Obes. 2012;7:382–390. [DOI] [PubMed] [Google Scholar]
- 119. Li R, Fein SB, Grummer‐Strawn LM. Do infants fed from bottles lack self‐regulation of milk intake compared with directly breastfed infants? Pediatrics. 2010;125:e1386–e1393. [DOI] [PubMed] [Google Scholar]
- 120. Hathcock A, Krause K, Viera AJ, Fuemmeler BF, Lovelady C, Ostbye T. Satiety responsiveness and the relationship between breastfeeding and weight status of toddlers of overweight and obese women. Matern Child Health J. 2014;18:1023–1030. [DOI] [PubMed] [Google Scholar]
- 121. Rogers SL, Blissett J. Breastfeeding duration and its relation to weight gain, eating behaviours and positive maternal feeding practices in infancy. Appetite. 2017;108:399–406. [DOI] [PubMed] [Google Scholar]
- 122. Ventura AK, Pollack Golen R. A pilot study comparing opaque, weighted bottles with conventional, clear bottles for infant feeding. Appetite. 2015;85:178–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Shloim N, Vereijken C, Blundell P, Hetherington MM. Looking for cues—infant communication of hunger and satiation during milk feeding. Appetite. 2017;108:74–82. [DOI] [PubMed] [Google Scholar]
- 124. Dovey TM, Staples PA, Gibson EL, Halford JC. Food neophobia and “picky/fussy” eating in children: a review. Appetite. 2008;50:181–193. [DOI] [PubMed] [Google Scholar]
- 125. Galloway AT, Fiorito L, Lee Y, Birch LL. Parental pressure, dietary patterns, and weight status among girls who are “picky eaters.” J Am Diet Assoc. 2005;105:541–548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Brown S, Harris G. Disliked food acting as a contaminant during infancy. A disgust based motivation for rejection. Appetite. 2012;58:535–538. [DOI] [PubMed] [Google Scholar]
- 127. Hursti U‐KK, Sjödén P‐O. Food and general neophobia and their relationship with self‐reported food choice: familial resemblance in Swedish families with children of ages 7–17 years. Appetite. 1997;29:89–103. [DOI] [PubMed] [Google Scholar]
- 128. McFarlane T, Pliner P. Increasing willingness to taste novel foods: effects of nutrition and taste information. Appetite. 1997;28:227–238. [DOI] [PubMed] [Google Scholar]
- 129. Rigal N, Frelut M‐L, Monneuse M‐O, Hladik C‐M, Simmen B, Pasquet P. Food neophobia in the context of a varied diet induced by a weight reduction program in massively obese adolescents. Appetite. 2006;46:207–214. [DOI] [PubMed] [Google Scholar]
- 130. Harris HA, Ria‐Searle B, Jansen E, Thorpe K. What's the fuss about? Parent presentations of fussy eating to a parenting support helpline. Public Health Nutr. 2018;21:1520–1528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Webber L, Cooke L, Hill C, Wardle J. Associations between children's appetitive traits and maternal feeding practices. J Am Diet Assoc. 2010;110:1718–1722. [DOI] [PubMed] [Google Scholar]
- 132. Harris HA, Fildes A, Mallan KM, Llewellyn CH. Maternal feeding practices and fussy eating in toddlerhood: a discordant twin analysis. Int J Behav Nutr Phys Act. 2016;13:81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. Fisher JO, Birch LL. Restricting access to palatable foods affects children's behavioral response, food selection, and intake. Am J Clin Nutr. 1999;69:1264–1272. [DOI] [PubMed] [Google Scholar]
- 134. Fisher JO, Birch LL. Restricting access to foods and children's eating. Appetite. 1999;32:405–419. [DOI] [PubMed] [Google Scholar]
- 135. Francis LA, Hofer SM, Birch LL. Predictors of maternal child‐feeding style: maternal and child characteristics. Appetite. 2001;37:231–243. [DOI] [PubMed] [Google Scholar]
- 136. Murashima M, Hoerr SL, Hughes SO, Kaplowitz SA. Feeding behaviors of low‐income mothers: directive control relates to a lower BMI in children, and a nondirective control relates to a healthier diet in preschoolers. Am J Clin Nutr. 2012;95:1031–1037. [DOI] [PubMed] [Google Scholar]
- 137. Blissett J. Relationships between parenting style, feeding style and feeding practices and fruit and vegetable consumption in early childhood. Appetite. 2011;57:826–831. [DOI] [PubMed] [Google Scholar]
- 138. Birch LL, McPhee L, Shoba B, Pirok E, Steinberg L. What kind of exposure reduces children's food neophobia? Looking vs. tasting. Appetite. 1987;9:171–178. [DOI] [PubMed] [Google Scholar]
- 139. Sullivan SA, Birch LL. Pass the sugar, pass the salt: experience dictates preference. Dev Psychol. 1990;26:546–551. [Google Scholar]
- 140. Pliner P, Stallberg‐White C. “Pass the ketchup, please”: familiar flavors increase children's willingness to taste novel foods. Appetite. 2000;34:95–103. [DOI] [PubMed] [Google Scholar]
- 141. Fisher JO, Mennella JA, Hughes SO, Liu Y, Mendoza PM, Patrick H. Offering “dip” promotes intake of a moderately‐liked raw vegetable among preschoolers with genetic sensitivity to bitterness. J Acad Nutr Diet. 2012;112:235–245. [DOI] [PubMed] [Google Scholar]
- 142. Pelchat ML, Pliner P. “Try it. You'll like it.” Effects of information on willingness to try novel foods. Appetite. 1995;24:153–165. [DOI] [PubMed] [Google Scholar]
- 143. Jansen A, Tenney N. Seeing mum drinking a “light” product: is social learning a stronger determinant of taste preference acquisition than caloric conditioning? Eur J Clin Nutr. 2001;55:418–422. [DOI] [PubMed] [Google Scholar]
- 144. Palfreyman Z, Haycraft E, Meyer C. Development of the Parental Modelling of Eating Behaviours scale (PARM): links with food intake among children and their mothers. Matern Child Nutr. 2014;10:617–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145. Momin SR, Hughes SO, Elias C, Papaioannou MA, Phan M, Vides D, Wood AC. Observations of toddlers’ sensory‐based exploratory behaviors with a novel food. Appetite. 2018;131:108–116. [DOI] [PubMed] [Google Scholar]
- 146. Luchini V, Musaad S, Lee S‐Y, Donovan SM. Observed differences in child picky eating behavior between home and childcare locations. Appetite. 2017;116:123–131. [DOI] [PubMed] [Google Scholar]
- 147. Horne PJ, Tapper K, Lowe C, Hardman C, Jackson M, Woolner J. Increasing children's fruit and vegetable consumption: a peer‐modelling and rewards‐based intervention. Eur J Clin Nutr. 2004;58:1649–1660. [DOI] [PubMed] [Google Scholar]
- 148. Duncker K. Experimental modification of children's food preferences through social suggestion. J Abnorm Soc Psychol. 1938;33:489. [Google Scholar]
- 149. Birch LL. Effects of peer models’ food choices and eating behaviors on preschoolers’ food preferences. Child Dev. 1980;51:489–496. [Google Scholar]
- 150. Greenhalgh J, Dowey AJ, Horne PJ, Lowe CF, Griffiths JH, Whitaker CJ. Positive‐ and negative peer modelling effects on young children's consumption of novel blue foods. Appetite. 2009;52:646–653. [DOI] [PubMed] [Google Scholar]
- 151. Orrell‐Valente JK, Hill LG, Brechwald WA, Dodge KA, Pettit GS, Bates JE. “Just three more bites”: an observational analysis of parents’ socialization of children's eating at mealtime. Appetite. 2007;48:37–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152. Carper J, Fisher JO, Birch LL. Young girls’ emerging dietary restraint and disinhibition are related to parental control in child feeding. Appetite. 2000;35:121–129. [DOI] [PubMed] [Google Scholar]
- 153. Tripicchio GL, Keller KL, Johnson C, Pietrobelli A, Heo M, Faith MS. Differential maternal feeding practices, eating self‐regulation, and adiposity in young twins. Pediatrics. 2014;134:e1399–e1404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154. Flacking R, Nyqvist KH, Ewald U. Effects of socioeconomic status on breastfeeding duration in mothers of preterm and term infants. Eur J Pub Health. 2007;17:579–584. [DOI] [PubMed] [Google Scholar]
- 155. Amir LH, Donath SM. Socioeconomic status and rates of breastfeeding in Australia: evidence from three recent national health surveys. Med J Aust. 2008;189:254–256. [DOI] [PubMed] [Google Scholar]
- 156. Shrewsbury V, Wardle J. Socioeconomic status and adiposity in childhood: a systematic review of cross‐sectional studies 1990–2005. Obesity. 2008;16:275–284. [DOI] [PubMed] [Google Scholar]
- 157. Sobal J, Stunkard AJ. Socioeconomic status and obesity: a review of the literature. Psychol Bull. 1989;105:260. [DOI] [PubMed] [Google Scholar]
- 158. Wojcicki JM. Maternal prepregnancy body mass index and initiation and duration of breastfeeding: a review of the literature. J Women's Health. 2011;20:341–347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159. Donath S, Amir L. Does maternal obesity adversely affect breastfeeding initiation and duration? J Paediatr Child Health. 2000;36:482–486. [DOI] [PubMed] [Google Scholar]
- 160. Thompson LA, Zhang S, Black E, Das R, Ryngaert M, Sullivan S, Roth J. The association of maternal pre‐pregnancy body mass index with breastfeeding initiation. Matern Child Health J. 2013;17:1842–1851. [DOI] [PubMed] [Google Scholar]
- 161. Donath SM, Amir LH. Maternal obesity and initiation and duration of breastfeeding: data from the longitudinal study of Australian children. Matern Child Nutr. 2008;4:163–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162. Oddy WH, Li J, Landsborough L, Kendall GE, Henderson S, Downie J. The association of maternal overweight and obesity with breastfeeding duration. J Pediatr. 2006;149:185–191. [DOI] [PubMed] [Google Scholar]
- 163. Haycraft EL, Blissett JM. Maternal and paternal controlling feeding practices: reliability and relationships with BMI. Obesity. 2008;16:1552–1558. [DOI] [PubMed] [Google Scholar]
- 164. Saelens BE, Ernst MM, Epstein LH. Maternal child feeding practices and obesity: a discordant sibling analysis. Int J Eat Disord. 2000;27:459–463. [DOI] [PubMed] [Google Scholar]
- 165. Haycraft E, Blissett J. Predictors of paternal and maternal controlling feeding practices with 2‐ to 5‐year‐old children. J Nutr Educ Behav. 2012;44:390–397. [DOI] [PubMed] [Google Scholar]
- 166. Jansen E, Williams KE, Mallan KM, Nicholson JM, Daniels LA. Bidirectional associations between mothers’ feeding practices and child eating behaviours. Int J Behav Nutr Phys Act. 2018;15:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167. Webber L, Cooke L, Hill C, Wardle J. Child adiposity and maternal feeding practices: a longitudinal analysis. Am J Clin Nutr. 2010;92:1423–1428. [DOI] [PubMed] [Google Scholar]
- 168. Jansen PW, Tharner A, Van Der Ende J, Wake M, Raat H, Hofman A, Verhulst FC, Van Ijzendoorn MH, Jaddoe VW, Tiemeier H. Feeding practices and child weight: is the association bidirectional in preschool children? Am J Clin Nutr. 2014;100:1329–1336. [DOI] [PubMed] [Google Scholar]
- 169. Farrow CV, Blissett J. Controlling feeding practices: cause or consequence of early child weight? Pediatrics. 2008;121:e164–e169. [DOI] [PubMed] [Google Scholar]
- 170. Campbell K, Andrianopoulos N, Hesketh K, Ball K, Crawford D, Brennan L, Corsini N, Timperio A. Parental use of restrictive feeding practices and child BMI z‐score. A 3‐year prospective cohort study. Appetite. 2010;55:84–88. [DOI] [PubMed] [Google Scholar]
- 171. Tschann JM, Martinez SM, Penilla C, Gregorich SE, Pasch LA, de Groat CL, Flores E, Deardorff J, Greenspan LC, Butte NF. Parental feeding practices and child weight status in Mexican American families: a longitudinal analysis. Int J Behav Nutr Phys Act. 2015;12:66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172. Afonso L, Lopes C, Severo M, Santos S, Real H, Durão C, Moreira P, Oliveira A. Bidirectional association between parental child‐feeding practices and body mass index at 4 and 7 y of age. Am J Clin Nutr. 2016;103:861–867. [DOI] [PubMed] [Google Scholar]
- 173. Daniels L, Mallan K, Battistutta D, Nicholson J, Perry R, Magarey A. Evaluation of an intervention to promote protective infant feeding practices to prevent childhood obesity: outcomes of the NOURISH RCT at 14 months of age and 6 months post the first of two intervention modules. Int J Obes. 2012;36:1292–1298. [DOI] [PubMed] [Google Scholar]
- 174. World Health Organization . WHO Child Growth Standards: Length/Height for Age, Weight‐for‐Age, Weight‐for‐Length, Weight‐for‐Height and Body Mass Index‐for‐Age, Methods and Development. Geneva, Switzerland: World Health Organization; 2006. [Google Scholar]
- 175. Carruth BR, Skinner JD. Feeding behaviors and other motor development in healthy children (2–24 months). J Am Coll Nutr. 2002;21:88–96. [DOI] [PubMed] [Google Scholar]
- 176. Hallé PA, de Boysson‐Bardies B. Emergence of an early receptive lexicon: infants’ recognition of words. Infant Behav Develop. 1994;17:119–129. [Google Scholar]
- 177. Mitchell P, Lacohée H. Children's early understanding of false belief. Cognition. 1991;39:107–127. [DOI] [PubMed] [Google Scholar]
- 178. Kuczynski L, Kochanska G, Radke‐Yarrow M, Girnius‐Brown O. A developmental interpretation of young children's noncompliance. Dev Psychol. 1987;23:799–806. [Google Scholar]
- 179. Silva IdS, De Stavola BL, Mann V, Kuh D, Hardy R, Wadsworth ME. Prenatal factors, childhood growth trajectories and age at menarche. Int J Epidemiol. 2002;31:405–412. [DOI] [PubMed] [Google Scholar]
- 180. Sun J, Nwaru BI, Hua J, Li X, Wu Z. Infant BMI peak as a predictor of overweight and obesity at age 2 years in a Chinese community‐based cohort. BMJ Open. 2017;7:e015122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181. Monteiro POA, Victora CG. Rapid growth in infancy and childhood and obesity in later life–a systematic review. Obes Rev. 2005;6:143–154. [DOI] [PubMed] [Google Scholar]
- 182. Rothbart MK, Bates JE. Temperament In: Damon W, Eisenberg N, eds. Handbook of Child Psychology. Volume 3: Social, Emotional, and Personality Development. 5th ed. New York, NY: John Wiley & Sons, Inc; 1998:105–176. [Google Scholar]
- 183. Slining MM, Adair L, Goldman BD, Borja J, Bentley M. Infant temperament contributes to early infant growth: a prospective cohort of African American infants. Int J Behav Nutr Phys Act. 2009;6:51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184. Bergmeier H, Skouteris H, Horwood S, Hooley M, Richardson B. Associations between child temperament, maternal feeding practices and child body mass index during the preschool years: a systematic review of the literature. Obes Rev. 2014;15:9–18. [DOI] [PubMed] [Google Scholar]
- 185. Hittner JB, Johnson C, Tripicchio G, Faith MS. Infant emotional distress, maternal restriction at a home meal, and child BMI gain through age 6 years in the Colorado adoption project. Eat Behav. 2016;21:135–141. [DOI] [PubMed] [Google Scholar]
- 186. Peacock‐Chambers E, Radesky JS, Parker SE, Zuckerman B, Lumeng JC, Silverstein M. Infant regulatory problems and obesity in early childhood. Acad Pediatr. 2017;17:523–528. [DOI] [PubMed] [Google Scholar]
- 187. Wasser H, Bentley M, Borja J, Goldman BD, Thompson A, Slining M, Adair L. Infants perceived as “fussy” are more likely to receive complementary foods before 4 months. Pediatrics. 2011;127:229–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188. Horning ML, Fulkerson JA. A systematic review on the affordability of a healthful diet for families in the United States. Public Health Nurs. 2015;32:68–80. [DOI] [PubMed] [Google Scholar]
- 189. Carty SA, Mainvil LA, Coveney JD. Exploring family home food environments: household resources needed to utilise weekly deliveries of free fruits and vegetables. Nutr Dietet. 2017;74:138–146. [DOI] [PubMed] [Google Scholar]
- 190. Devine CM, Jastran M, Jabs J, Wethington E, Farell TJ, Bisogni CA. “A lot of sacrifices:” work–family spillover and the food choice coping strategies of low‐wage employed parents. Soc Sci Med. 2006;63:2591–2603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191. Roy KM, Tubbs CY, Burton LM. Don't have no time: daily rhythms and the organization of time for low‐income families. Fam Relat. 2004;53:168–178. [Google Scholar]
- 192. Jarrett RL, Bahar OS, Kersh RT. “When we do sit down together” family meal times in low‐income African American families with preschoolers. J Fam Issues. 2016;37:1483–1513. [Google Scholar]
- 193. Vedovato GM, Surkan PJ, Jones‐Smith J, Steeves EA, Han E, Trude AC, Kharmats AY, Gittelsohn J. Food insecurity, overweight and obesity among low‐income African‐American families in Baltimore City: associations with food‐related perceptions. Public Health Nutr. 2016;19:1405–1416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194. Mena NZ, Gorman K, Dickin K, Greene G, Tovar A. Contextual and cultural influences on parental feeding practices and involvement in child care centers among Hispanic parents. Child Obes. 2015;11:347–354. [DOI] [PubMed] [Google Scholar]
- 195. Daniel C. Economic constraints on taste formation and the true cost of healthy eating. Soc Sci Med. 2016;148:34–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196. Swyden K, Sisson SB, Morris AS, Lora K, Weedn AE, Copeland KA, DeGrace B. Association between maternal stress, work status, concern about child weight, and restrictive feeding practices in preschool children. Matern Child Health J. 2017;21:1349–1357. [DOI] [PubMed] [Google Scholar]
- 197. Coyne SM, McDaniel BT, Stockdale LA. “Do you dare to compare?” Associations between maternal social comparisons on social networking sites and parenting, mental health, and romantic relationship outcomes. Comput Hum Behav. 2017;70:335–340. [Google Scholar]
- 198. Thullen M, Majee W, Davis AN. Co‐parenting and feeding in early childhood: reflections of parent dyads on how they manage the developmental stages of feeding over the first three years. Appetite. 2016;105:334–343. [DOI] [PubMed] [Google Scholar]
- 199. Khandpur N, Charles J, Blaine RE, Blake C, Davison K. Diversity in fathers’ food parenting practices: a qualitative exploration within a heterogeneous sample. Appetite. 2016;101:134–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200. Galanti G‐A. The Hispanic family and male‐female relationships: an overview. J Transcult Nurs. 2003;14:180–185. [DOI] [PubMed] [Google Scholar]
- 201. O'Connor T, Perez O, Garcia IC, Gallagher M. Engaging Latino fathers in children's eating and other obesity‐related behaviors: a review. Curren Nutr Rep. 2018;7:29–38. [DOI] [PubMed] [Google Scholar]
- 202. Kumanyika SK. Environmental influences on childhood obesity: ethnic and cultural influences in context. Physiol Behav. 2008;94:61–70. [DOI] [PubMed] [Google Scholar]
- 203. Pulgaron ER, Marchante AN, Agosto Y, Lebron CN, Delamater AM. Grandparent involvement and children's health outcomes: the current state of the literature. Fam Syst Health. 2016;34:260–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204. Cardel M, Willig AL, Dulin‐Keita A, Casazza K, Beasley TM, Fernández JR. Parental feeding practices and socioeconomic status are associated with child adiposity in a multi‐ethnic sample of children. Appetite. 2012;58:347–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205. McMeekin S, Jansen E, Mallan K, Nicholson J, Magarey A, Daniels L. Associations between infant temperament and early feeding practices. A cross‐sectional study of Australian mother‐infant dyads from the nourish randomised controlled trial. Appetite. 2013;60:239–245. [DOI] [PubMed] [Google Scholar]
- 206. Haycraft E, Farrow C, Blissett J. Maternal symptoms of depression are related to observations of controlling feeding practices in mothers of young children. J Fam Psychol. 2013;27:159–164. [DOI] [PubMed] [Google Scholar]
- 207. Hurley KM, Black MM, Papas MA, Caufield LE. Maternal symptoms of stress, depression, and anxiety are related to nonresponsive feeding styles in a statewide sample of WIC participants. J Nutr. 2008;138:799–805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208. Gillison FB, Lorenc AB, Sleddens EF, Williams SL, Atkinson L. Can it be harmful for parents to talk to their child about their weight? A meta‐analysis. Prev Med. 2016;93:135–146. [DOI] [PubMed] [Google Scholar]
- 209. Epstein L. Family‐based behavioural intervention for obese children. Int J Obes Relat Metab Disord. 1996;20:S14–S21. [PubMed] [Google Scholar]
- 210. Boutelle KN, Cafri G, Crow SJ. Parent predictors of child weight change in family based behavioral obesity treatment. Obesity. 2012;20:1539–1543. [DOI] [PMC free article] [PubMed] [Google Scholar]


