Abstract
Background
Home‐time, defined as the time spent alive outside of a healthcare institution, has emerged as a patient‐centered health outcome. The discharge locations and distribution of home‐time after a type 2 myocardial infarction are unknown.
Methods and Results
Patients with a type 2 myocardial infarction between October 2017 and May 2018 at Massachusetts General Hospital were included. Patients discharged to hospice or without follow‐up data were excluded. Our primary outcome was home‐time defined as the number of days lived outside of a hospital, long‐term acute care facility, skilled nursing facility, or rehabilitation facility. We identified 359 patients with type 2 myocardial infarction over the study period. Of those discharged alive (N=321), 62.9% were discharged home, and the remainder went to a facility or hospice. Among those with available follow‐up data (N=289), the median home‐time was 30 (interquartile range [IQR], 16–30) days at 30 days, 171 (IQR, 133–180) days at 180 days, and 347 (IQR, 203–362) days at 365 days. At 1 year, 29 patients (10%) with type 2 myocardial infarction had spent no time at home and only 57 patients (19.7%) spent the entire year alive and at home. At 1 year, postdischarge all‐cause mortality was 23.2%, all‐cause readmission was 69.2%, and major adverse cardiovascular events (composite of all‐cause mortality, recurrent myocardial infarction, or stroke) was 34.9%. Home‐time through 1 year correlated strongly with time‐to‐event all‐cause mortality (τ=0.54, P<0.001) and major adverse cardiovascular events (τ=0.52, P<0.001) and modestly with a composite of all‐cause mortality or readmission (τ=0.44, P<0.001).
Conclusions
Home‐time is low after a hospitalization for type 2 myocardial infarction and correlates strongly with mortality and major adverse cardiovascular events.
Keywords: home‐time, patient‐centered health outcome, type 2 myocardial infarction
Subject Categories: Quality and Outcomes
Nonstandard Abbreviations and Acronyms
- GRACE
Global Registry of Acute Coronary Events
- IQR
interquartile range
- MACE
major adverse cardiovascular events
- MI
myocardial infarction
- OR
odds ratio
- SNF
skilled nursing facility
- TIMI
Thrombolysis in Myocardial Infarction
- T1MI
type 1 myocardial infarction
- T2MI
type 2 myocardial infarction
Clinical Perspective
What Is New?
Approximately one third of type 2 myocardial infarction patients discharged alive from the hospital were discharged to a facility, and the median home‐time at 1 year after a type 2 myocardial infarction was 347 days; 10% of patients spent no time at home and only 19.7% spent the entire year alive and at home.
Patients with a home‐time below the median at 1 year were older and had a higher prevalence of heart failure, atrial fibrillation, chronic kidney disease, and GRACE (Global Registry of Acute Coronary Events) scores >140.
Home‐time through 1 year correlated strongly with time‐to‐event all‐cause mortality and major adverse cardiovascular events, and modestly with a composite of all‐cause mortality or readmission.
What Are the Clinical Implications?
As efforts to identify evidence‐based therapies for type 2 myocardial infarction are explored, home‐time may serve as an important patient‐centered outcome that: (1) captures total recurrent nonfatal events and death; (2) accounts for time spent in postacute care facilities; and (3) summarizes individual patient experience and provides an alternative approach to communicating prognosis and anticipated course with patients.
Introduction
Type 2 myocardial infarction (T2MI) is now recognized as a common subtype of MI with a sobering prognosis.1, 2 As there are currently no evidence‐based therapies for patients with T2MI, there is a substantial unmet need to improve patient outcomes. All‐cause mortality and hospital readmission are frequently used as outcomes in randomized clinical trials; however, these outcomes fail to capture the total time patients spend in hospitals or in healthcare facilities; both have a significant influence on patient's quality of life and longer term outcome. Over the past 35 years, although hospital length of stay for Medicare patients has halved, discharges to skilled nursing facilities (SNFs) have quadrupled.3 Thus, more comprehensive, meaningful patient‐centered measures that incorporate such secular trends are needed.
Home‐time, defined as the time a patient lives out of a healthcare institution, has recently emerged as a novel patient‐centered health outcome. Home‐time has correlated with functional and quality‐of‐life outcomes among stroke survivors,4, 5, 6 and with mortality and readmission after hospitalization for heart failure.7 The type of discharge locations and distribution of home‐time patients experience after a hospitalization for T2MI have yet to be described and may serve as an important patient‐centered end point in future clinical trials.
Accordingly, we sought to examine the discharge locations and home‐time after a hospitalization for T2MI. Furthermore, we investigated whether home‐time after a T2MI correlated with traditional end points such as all‐cause mortality, all‐cause readmission or mortality, and major adverse cardiovascular events (MACE). We hypothesized home‐time would be inversely associated with deleterious outcomes in those with T2MI.
Methods
The data, analytic methods, and study materials will not be made available to other researchers for purposes of reproducing the results.
Study Population
We identified patients coded as T2MI (International Classification of Diseases, Tenth Revision (ICD‐10), code I21.A1) between October 1, 2017 and May 31, 2018 at Massachusetts General Hospital, a large tertiary care hospital in Boston, Massachusetts. Strict adjudication with physician chart reviewers using the 4th Universal Definition of MI was then applied to confirm the diagnosis using methods described elsewhere.8, 9 An MI was defined as a rising/or falling elevation in cardiac troponin (conventional or high sensitivity) >99th percentile and at least one of the following: (1) symptoms of ischemia; (2) new electrocardiographic evidence of ischemia; (3) new pathologic Q waves; (4) new regional wall motions on imaging in an ischemic territory; or (5) coronary thrombus on angiography. At our institution, a cardiac troponin T concentration ≥0.03 ng/L (10% coefficient of variation) or a fifth generation high‐sensitivity cardiac troponin T concentration of ≥10 ng/L for women or ≥15 ng/L for men were diagnostic of myocardial injury. T2MI was defined as an MI with an identifiable preceding imbalance between myocardial oxygen supply and demand unrelated to coronary thrombus. To ensure consistency with the diagnoses, uncertain cases were reviewed by a physician (C.M.C.).
Outcomes
The primary outcome of interest was postdischarge home‐time; calculated for each patient as the number of days lived outside of an acute care hospital, long‐term acute care facility, SNF, or acute rehabilitation facility. Dates in facilities were obtained from discharge summaries, case management notes, primary care physician office visit notes, and telephone encounters in the electronic health records. Hospital days from the index T2MI hospitalization were not included in the home‐time calculations. Patients who were discharged to hospice or who did not have clear follow‐up data (including dates residing in facilities) beyond their index T2MI hospitalization were excluded from the home‐time analyses.
Secondary outcomes recorded included all‐cause mortality, all‐cause readmission or mortality, and MACE (composite of all‐cause mortality, MI, and stroke) at 30, 180, and 365 days postdischarge. All‐cause mortality was used in our MACE composite outcome instead of cardiovascular death to account for the competing risk of noncardiovascular death.
Statistical Analysis
Mean, standard deviation, median, and quartiles of home‐time were calculated at 30, 180, and 365 days. Baseline characteristics including GRACE (Global Registry of Acute Coronary Events) and Thrombolysis in Myocardial Infarction (TIMI) scores, diagnostic testing, treatment strategies, and discharge locations were compared among T2MI patients with home‐time below versus above/equal to the median using the chi‐square or Fisher exact test for dichotomous variables and the Welch two‐sample t test for continuous variables.
To demonstrate and capture nonlinearity, we divided home‐time into sextiles. Due to clustering of home‐time at each end of the non‐normal distribution, we then performed ordinal logistic regression using home‐time divided into sextiles to assess the association of baseline participant characteristics, in‐hospital treatment strategies, and discharge medications with home‐time at 1 year with bidirectional variable selection for identifying the best subset of predictors that related to the outcome variable. Models were structured hierarchically first including baseline patient characteristics (model 1), followed by addition of in‐hospital MI‐related treatments (model 2), and discharge medications (model 3).
The correlation between home‐time and days free from each secondary outcome were determined using Kendall's tau b correlation coefficients. The timepoints for each outcome began on the date of index discharge through to the 365 days postdischarge date. All statistical tests were two‐sided, with P<0.05 considered statistically significant. All analyses were performed using R software. This study was approved by the institutional review board of Partners Healthcare. Informed consent was waived.
Results
Patient Characteristics and Discharge Locations After T2MI
We identified 633 patients coded as T2MI and adjudicated 359 patients to have T2MI over the study period, as described elsewhere (Figure 1).9 The precipitants of T2MI were heart failure (N=78; 21.7%), respiratory failure (N=69; 19.2%), sepsis (N=51; 14.2%), arrhythmias (N=52; 14.5%), hypertensive urgency (N=38; 10.6%), bleeding (N=19; 5.3%), anemia unrelated to active bleeding (N=14; 3.9%), hypotension (N=14; 3.9%), surgery (N=10; 2.8%), coronary artery dissection (N=1; 0.3%), and other causes (N=13; 3.6%). Of those adjudicated to have T2MI (N=359), 38 patients died in hospital (10.6%) and 321 (89.4%) patients were discharged alive. Of those 321 discharged alive, 202 (62.9%) were discharged home, 67 (20.9%) to SNFs, 37 (11.5%) to acute rehabilitation facilities, 10 (3.1%) to long‐term acute care facilities, and 5 (1.6%) to hospice (Figure 2). Among those discharged alive and not to hospice (N=316), follow‐up data pertaining to home‐time were available for 289 patients (Figure 1). Of the final cohort included in our study for our home‐time analysis (N=289), 40 underwent coronary angiogram and only 5 underwent percutaneous coronary intervention and 3 underwent coronary artery bypass grafting during their index hospitalization.
Figure 1. Flow diagram illustrating T2MI patients who were included in this study.
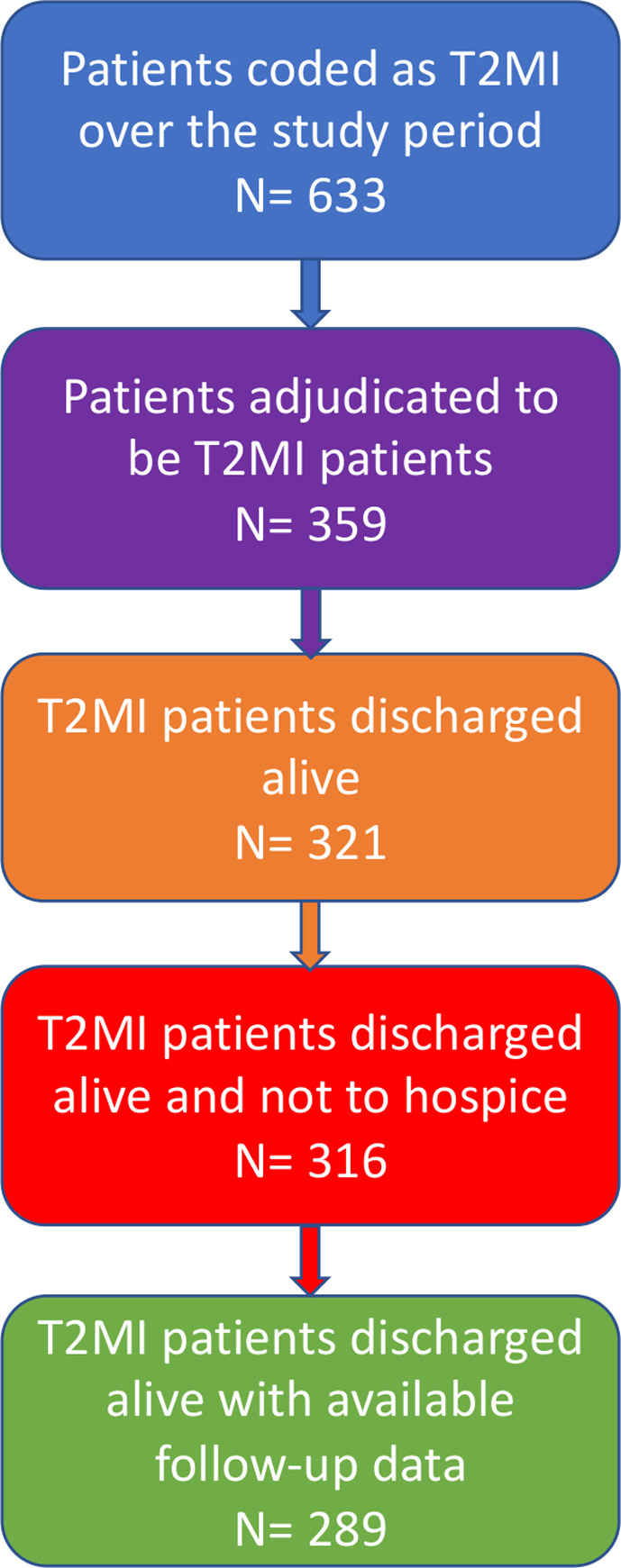
T2MI, type 2 myocardial infarction.
Figure 2.
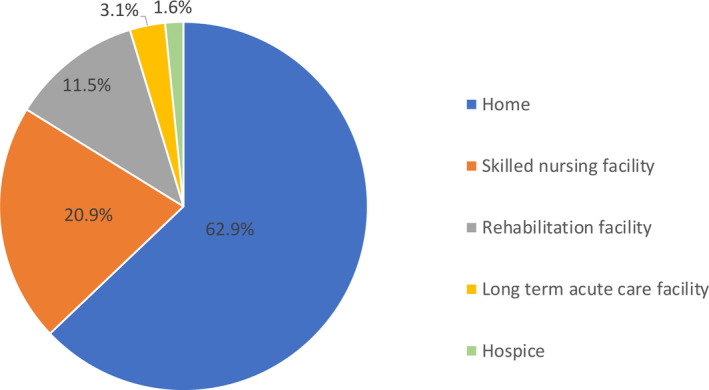
Pie chart showing the distribution of surviving patients' discharge location after a hospitalization complicated by type 2 myocardial infarction.
Distribution of Home‐Time After a T2MI
Among those with available follow‐up data (N=289), the median home‐time was 30 (interquartile range [IQR], 16–30) days at 30 days, 171 (IQR, 133–180) days at 180 days, and 347 (IQR, 203–362) days at 365 days. The distribution of home‐time at 30, 180, and 365 days is illustrated in Figure 3. Patients with a home‐time below the median at 1‐year were significantly older (P=0.01) and had a higher prevalence of heart failure (P=0.004), atrial fibrillation (P=0.02), chronic kidney disease (P=0.03), and GRACE scores >140 (P<0.001; Table 1). The mean home‐time was 21.57±11.72 days at 30 days, 138.00±62.52 days at 180 days, and 270.10±133.53 days at 365 days. At 1 year, 29 patients with T2MI (10.0%) had spent no time at home and only 57 (19.7%) spent the full year alive and at home (Table 2).
Figure 3.
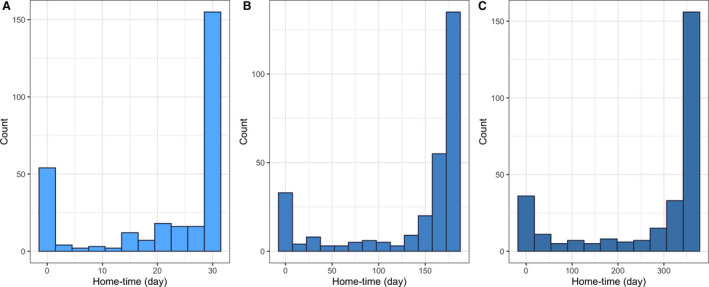
Histograms illustrating distribution of home‐time at 30 days (A), 180 days (B), and 365 days (C) among 289 patients for each time period.
Table 1.
Characteristics of Type 2 MI Patients Stratified by Median Home‐Time at 1 Year (N=289)
| Home‐Time Below Mediana (n=144) | Home‐Time Equal to or Above the Mediana (n=145) | |
|---|---|---|
| Demographics | ||
| Age, mean (SD) | 75.8 (13.4) | 72.0 (13.2) |
| Men | 81 (56.2%) | 84 (57.9%) |
| Race | ||
| White | 126 (87.5%) | 115 (79.3%) |
| Black | 13 (9.0%) | 17 (11.7%) |
| Other | 5 (3.5%) | 13 (9.0%) |
| Past medical history | ||
| Diabetes mellitus | 68 (47.2%) | 56 (38.6%) |
| Smoker | 16 (11.1%) | 17 (11.7%) |
| COPD | 35 (24.3%) | 26 (17.9%) |
| Hypertension | 114 (79.2%) | 119 (82.1%) |
| Hyperlipidemia | 88 (61.1%) | 92 (63.4%) |
| Previous MI | 35 (24.3%) | 29 (20%) |
| Previous PCI | 29 (20.1%) | 22 (15.2%) |
| Previous CABG | 21 (14.6%) | 26 (17.9%) |
| Heart failure | 87 (60.4%) | 62 (42.8%) |
| Known CAD | 74 (51.4%) | 77 (53.1%) |
| Atrial fibrillation | 55 (38.2%) | 36 (24.8%) |
| Previous stroke or TIA | 27 (18.8%) | 30 (20.7%) |
| PAD | 39 (27.1%) | 28 (19.3%) |
| Cancer history | 33 (22.9%) | 26 (17.9%) |
| CKD | 79 (54.9%) | 60 (41.4%) |
| Dialysis | 19 (13.2%) | 14 (9.7%) |
| Liver cirrhosis | 7 (4.9%) | 4 (2.8%) |
| Prior GI bleed | 13 (9.0%) | 12 (8.3%) |
| Diagnostic work‐up | ||
| Ejection fraction (N=99), mean % (SD) | 53.1% (17.4) | 54.1% (15.7) |
| Positive stress test/number performed (%) | 4/13 (30.8%) | 6/18 (33.3%) |
| Coronary angiography with obstructive disease/number performed (%) | 6/12 (50%) | 13/28 (46.4%) |
| HbA1c level (N=189) (SD) | 6.4% (2.1) | 6.5% (2.2) |
| LDL‐C level (N=212), mean mg/dL (SD) | 61.9 (21) | 81.8 (47.5) |
| Initial conventional troponin concentration (N=86), mean ng/mL (SD) | 0.17 (0.2) | 0.15 (0.2) |
| Peak conventional troponin concentration (N=86), mean ng/mL (SD) | 0.41 (0.7) | 0.40 (0.2) |
| Initial hs troponin concentration (N=203), mean ng/L (SD) | 128.1 (253.2) | 58.1 (64.1) |
| Peak hs troponin concentration (N=203), mean ng/L (SD) | 282.2 (579.9) | 150.6 (304.4) |
| GRACE score | ||
| 1–109 | 21 (14.6%) | 28 (19.3%) |
| 110–140 | 33 (22.9%) | 61 (42.1%) |
| >140 | 90 (62.5%) | 55 (37.9%) |
| TIMI score | ||
| 1 | 12 (8.3%) | 9 (6.2%) |
| 2 | 18 (12.5%) | 30 (20.7) |
| 3 | 31 (21.5%) | 29 (20%) |
| 4 | 36 (25%) | 33 (22.8%) |
| 5 | 32 (22.2%) | 34 (23.4%) |
| 6 | 12 (8.3%) | 7 (4.8%) |
| 7 | 3 (2.1%) | 3 (2.1%) |
| In‐hospital treatment | ||
| Aspirin | 109 (75.7%) | 123 (84.8%) |
| Clopidogrel | 20 (13.9%) | 14 (9.7%) |
| β‐blocker | 103 (72%) | 98 (69.5%) |
| ACEi/ARB | 36 (25%) | 46 (31.7%) |
| Statin | 119 (82.6%) | 112 (77.2%) |
| PCI | 2 (1.4%) | 3 (2.1%) |
| CABG | 2 (1.4%) | 1 (0.7%) |
| Discharge medications | ||
| Aspirin | 107 (74.3%) | 120 (82.8%) |
| Clopidogrel | 18 (12.5%) | 18 (12.4%) |
| Ticagrelor | 1 (0.7%) | 1 (0.7%) |
| ACEi/ARB | 41 (28.5%) | 56 (38.6%) |
| Statin | 119 (82.6%) | 111 (76.6%) |
| β‐blocker | 104 (72.2%) | 109 (75.2%) |
ACEi indicates angiotensin‐converting enzyme inhibitor; ARB, angiotensin II receptor blocker; CABG, coronary artery bypass grafting; CAD, coronary artery disease; CKD, chronic kidney disease; COPD, chronic obstructive pulmonary disease; GI, gastrointestinal; GRACE, Global Registry of Acute Coronary Events; hs, high sensitivity, LDL‐C, low‐density lipoprotein‐cholesterol; MI, myocardial infarction; PAD, peripheral arterial disease; PCI, percutaneous coronary intervention; TIA, transient ischemic attack; and TIMI, Thrombolysis in Myocardial Infarction.
Median home‐time 347 (interquartile range, 203–362) days.
Table 2.
Postdischarge Outcomes Among Patients With Type 2 MI (N=289)
| Outcome | 30 Days | 180 Days | 365 Days |
|---|---|---|---|
| Traditional outcomes | |||
| All‐cause mortality, N (%) | 11 (3.8%) | 46 (15.9%) | 67 (23.2%) |
| Cardiovascular death, N (%) | 2 (0.7%) | 14 (4.8%) | 24 (8.3%) |
| Time‐to‐event all‐cause mortality, mean (SD) | 29.5 (3.0) | 163.7 (42.9) | 312.7 (108.2) |
| All‐cause rehospitalization, N (%) | 75 (26.0%) | 162 (56.1%) | 200 (69.2%) |
| Time‐to‐event all‐cause rehospitalization, mean (SD) | 25.3 (9.0) | 108.3 (73.8) | 174.0 (148.6) |
| All‐cause mortality or readmission, N (%) | 79 (27.3%) | 175 (60.6%) | 215 (74.4%) |
| Time‐to‐event all‐cause mortality or readmission, mean (SD) | 25.1 (9.1) | 103.7 (73.4) | 160.3 (143.7) |
| MACE (all‐cause mortality, MI, or stroke), N (%) | 24 (8.3%) | 75 (26.0%) | 101 (34.9%) |
| Time‐to‐event MACE (all‐cause mortality, MI, or stroke), mean (SD) | 28.5 (5.2) | 150.0 (57.1) | 277.9 (133.2) |
| Home‐time | |||
| Home‐time, mean days (SD) | 21.6 (11.7) | 138.0 (62.5) | 270.1 (133.5) |
| Home‐time, median days (IQR) | 30 (16–30) | 171 (133–180) | 347 (203–362) |
| 0% home‐time, N (%) | 53 (18.3%) | 29 (10.0%) | 29 (10.0%) |
| 100% home‐time, N (%) | 150 (51.9%) | 87 (30.1%) | 57 (19.7%) |
IQR indicates interquartile range; MACE, major adverse cardiovascular event; MI, myocardial infarction; N, number; and SD, standard deviation.
Predictors of Home‐Time
In multivariable logistic regression analysis including baseline characteristics, in‐hospital treatment, and discharge medications, several variables were associated with a reduction in home‐time (Table 3), including diabetes mellitus (proportional odds ratio [OR], 0.42; 95% CI, 0.24–0.83), chronic obstructive pulmonary disease (proportional OR, 0.44; 95% CI, 0.24–0.83), before percutaneous coronary intervention or angioplasty (proportional OR: 0.44; 95% CI, 0.22–0.88), chronic kidney disease (proportional OR, 0.56; 95% CI, 0.32–0.98), previous gastrointestinal bleed (proportional OR, 0.36; 95% CI, 0.14–0.90), and GRACE score >140 (proportional OR, 0.33; 95% CI, 0.14–0.71). Hyperlipidemia (proportional OR, 2.08; 95% CI, 1.16–3.78), aspirin (proportional OR, 2.61; 95% CI, 1.36–5.01), and β‐blocker prescriptions on discharge (proportional OR, 2.02; 95% CI, 1.08–3.80) were associated with higher home‐time (Table 3).
Table 3.
Ordinal Logistic Regression Analysis Assessing the Association Between Baseline Characteristics, In‐Hospital Treatments, and Discharge Medications With Home‐Time Stratified Into Sextiles
| Variable | Model 1 | Model 2 | Model 3 | |||
|---|---|---|---|---|---|---|
| Proportional OR (95% CI) | P Value | Proportional OR (95% CI) | P Value | Proportional OR (95% CI) | P Value | |
| Demographics | ||||||
| Age | 0.97 (0.94–1.002) | 0.07 | 0.97 (0.95–1.002) | 0.07 | … | … |
| Diabetes mellitus | 0.36 (0.19–0.65) | <0.001 | 0.38 (0.20–0.71) | 0.003 | 0.42 (0.24–0.83) | 0.004 |
| COPD | 0.49 (0.26–0.93) | 0.03 | 0.48 (0.26–0.91) | 0.02 | 0.44 (0.24–0.83) | 0.01 |
| Hypertension | 1.67 (0.83–3.34) | 0.15 | … | … | … | … |
| Hyperlipidemia | 2.34 (1.28–4.35) | 0.006 | 2.48 (1.36–4.60) | 0.003 | 2.08 (1.16–3.78) | 0.01 |
| Prior PTCA or PCI | 0.48 (0.23–0.99) | 0.05 | 0.49 (0.23–1.04) | 0.06 | 0.44 (0.22–0.88) | 0.02 |
| History of malignancy | 0.56 (0.30–1.05) | 0.07 | … | … | 0.56 (0.30–1.05) | 0.07 |
| CKD | 0.54 (0.30–0.94) | 0.03 | 0.58 (0.33–1.03) | 0.06 | 0.56 (0.32–0.98) | 0.04 |
| Prior GI bleed | 0.31 (0.13–0.78) | 0.01 | 0.32 (0.13–0.80) | 0.01 | 0.36 (0.14–0.90) | 0.03 |
| Previous MI | … | … | 0.48 (0.24–0.96) | 0.04 | … | … |
| PAD | 0.63 (0.33–1.20) | 0.15 | … | … | … | … |
| TIMI score | 1.33 (1.03–1.73) | 0.03 | 1.25 (0.95–1.66) | 0.11 | … | … |
| GRACE score 110–140 | 1.28 (0.50–3.19) | 0.60 | 1.36 (0.53–3.45) | 0.51 | 1.23 (0.51–2.88) | 0.63 |
| GRACE score >140 | 0.50 (0.17–1.37) | 0.18 | 0.53 (0.18–1.44) | 0.22 | 0.33 (0.14–0.71) | 0.006 |
| In‐hospital treatment | ||||||
| Aspirin | … | … | 2.01 (1.00–4.02) | 0.05 | … | … |
| β‐blocker | … | … | 1.81 (0.99–3.31) | 0.05 | … | … |
| Discharge medications | ||||||
| Aspirin | … | … | … | … | 2.61 (1.36–5.01) | 0.004 |
| β‐blocker | … | … | … | … | 2.02 (1.08–3.80) | 0.03 |
| Deviation | 562.20 | 554.47 | 554.08 | |||
| AIC | 598.20 | 590.47 | 586.08 | |||
Models were structured hierarchically first including baseline patient characteristics (model 1), followed by addition of in‐hospital MI‐related treatments (model 2), and discharge medications (model 3). AIC, Akaike information criterion; CKD, chronic kidney disease; COPD, chronic obstructive pulmonary disease; GI, gastrointestinal; MI, myocardial infarction; OR, odds ratio; PAD, peripheral artery disease; PCI, percutaneous coronary intervention; and PTCA, percutaneous transluminal coronary angioplasty.
Correlation of Home‐Time With Traditional Outcomes
At 1 year, postdischarge all‐cause mortality was 23.2%, cardiovascular death was 8.3%, all‐cause readmission was 69.2%, all‐cause readmission or mortality was 74.4%, and MACE was 34.9% (Table 2). Home‐time correlated strongly with time‐to‐event all‐cause mortality (τ=0.54, P<0.001) and MACE (τ=0.52, P<0.001) and modestly with a composite end point of all‐cause mortality or readmission (τ=0.44, P<0.001) through 1 year (Figure 4).
Figure 4. Association between home‐time and days free from death (A), days free from readmission or death (B), and days free from MACE (C) at 365 days.
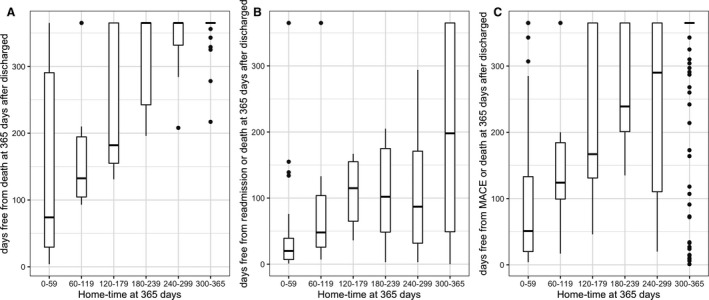
MACE, composite of death, recurrent myocardial infarction, or stroke.
Discussion
In this first study to examine discharge locations and the distribution of home‐time after a hospitalization complicated by T2MI, we report several noteworthy findings. We found that ≈1 in 10 patients with T2MI will not survive their hospitalization. For those patients discharged alive, one third will be discharged to a facility, most commonly, an SNF. This discharge rate to postacute care facilities is higher than the estimated national average among all Medicare patients10 and likely reflects the medical complexity and high‐risk nature of T2MI patients. Similarly, postacute facility utilization is ≈4‐fold higher than those with type 1 MI (T1MI). Among 633 737 patients with acute MI included in the National Cardiovascular Data Registry's ACTION Registry (now renamed the Chest Pain/MI registry), only 7.8% were discharged to a postacute facility.11 Recognition of the high rates of postacute care facility utilization among patients with T2MI can be useful both for hospital administration and for patients and their families in discharge planning.
After a hospitalization for T2MI, we found patient home‐time to be low. On average, patients with T2MI will only spend 9 months at home in the year after their hospitalization. One in 10 patients will spend no time at home, and only 1 in 5 will spend the full year at home. We found this low observed home‐time to be similar to that previously reported among postacute heart failure patients.7 Notably, similar to those with heart failure, medical complexity strongly influences the course of T2MI: patients with diabetes mellitus, chronic obstructive pulmonary disease, previous gastrointestinal bleed, previous coronary intervention, chronic kidney disease, and GRACE scores >140 were at higher risk of reduced home‐time. Identifying T2MI patients with these comorbidities may be helpful to physicians in discharge planning. Patients discharged on aspirin or β‐blockers had a higher likelihood of increased home‐time. However, it is plausible that this finding is related to selection bias in that these patients may have had favorable hemodynamics and health status sufficient to tolerate more aggressive medical management.
Consistent with previous studies,1, 12 patients with T2MI had high 1‐year mortality rates (23.2%). Furthermore, we demonstrated that all‐cause readmission (69.2%) and MACE (34.9%) rates are extremely high over the same period among this population. These rates again highlight the urgent need to identify evidence‐based therapies for this cohort.13 It is clear that T2MI is a highly prevalent and considerably complicated cardiovascular condition. However, despite being recognized as common and accompanied by considerable medical complexity and poor outcomes,2 means to improve outcomes in those with acute T2MI remain limited. Our analysis could not assess whether T2MI is causative of this prognosis or, alternatively, whether the prognosis is related to the prevalent coexisting cardiovascular and noncardiovascular comorbidities in this patient population. Studies focused on improved recognition, phenotyping, and multidisciplinary treatment of those with T2MI are needed.
Importantly, home‐time at 1 year correlated strongly with time to all‐cause mortality and MACE and correlated modestly with time to a composite end point of all‐cause mortality and readmission. These correlations are important if home‐time is to be considered as an end point in clinical trials. Home‐time has distinct advantages over traditional time to first end points and appears attractive in therapeutic development in this space: (1) the metric summarizes individual patient experience and provides an alternative approach to communicating prognosis and anticipated course with patients; (2) it may possess greater power in integrating total recurrent nonfatal events and death, frequently occurring in high‐risk cardiovascular populations; (3) it aligns with regulatory calls for consideration of new, patient‐oriented end points for other chronic cardiovascular conditions14; and (4) it accounts for time spent in postacute care facilities, which appears especially prevalent in this high‐risk cohort.
Limitations
This study has some limitations. As patients were identified using the T2MI code from the International Classification of Diseases, Tenth Revision (ICD‐10), it is possible that some T2MI patients who were not coded or miscoded were missed in this analysis. Furthermore, patients with T2MI were adjudicated and differentiated from T1MI based on the clinical scenario and as rates of coronary angiogram were relatively low among adjudicated T2MI patients (≈14%), definitive angiographic exclusion of coronary thrombus could not be made in the majority of cases. Dates during which patients resided in facilities were obtained from discharge summaries and documentation in the electronic health record and those without clear documentation were excluded. Therefore, some patients who resided in facilities were not included in the analyses due to uncertainty regarding their home‐time, thus the estimated home‐time rates may be under‐ or overestimated. Readmissions to outside facilities may not have been captured in our medical record system. We attempted to address this source of bias by excluding patients without follow‐up within our electronic medical record system. However, estimated home‐times may actually be lower than reported. Kendall's tau correlation coefficients were used for correlation analyses; however, this method may not account for censoring in the data and does not adjust for potential confounders. These findings may not be generalizable to other hospitals with differing healthcare practices, mixes of patients, or availability of resources. Last, as patient insurance data were not recorded, it is uncertain how types of insurance may impact home‐time, particularly time in facilities.
Conclusions
Home‐time is low after a hospitalization for T2MI and correlates strongly with time‐to‐event mortality and MACE. These results add to evidence illustrating the sobering prognosis of T2MI. As efforts to identify evidence‐based therapies for T2MI are explored, home‐time may serve as an important patient‐centered outcome.
Sources of Funding
This work was funded in part from grants from the American Heart Association (18 CDA 34110215) and the Massachusetts General Hospital Corrigan Minehan Heart Center SPARK program, both awarded to Dr. Wasfy.
Disclosures
M.V. is supported by the KL2/Catalyst Medical Research Investigator Training award from Harvard Catalyst (NIH/NCATS Award UL 1TR002541), serves on advisory boards for Amgen, AstraZeneca, Baxter Healthcare, Bayer AG, and Boehringer Ingelheim, and participates on clinical end point committees for studies sponsored by Novartis and the NIH. J.H.W. reports a grant from the American Heart Association (18 CDA 34110215). J.L.J. is supported by the Hutter Family Professorship; is a Trustee of the American College of Cardiology; has received grant support from Novartis Pharmaceuticals, Roche Diagnostics, Abbott, Singulex, and Prevencio, and consulting income from Abbott, Janssen, Novartis, Pfizer, Merck, and Roche Diagnostics; and participates in clinical end‐point committees/data safety monitoring boards for Abbott, AbbVie, Amgen, Boehringer‐Ingelheim, Janssen, and Takeda. The remaining authors have no disclosures to report.
(J Am Heart Assoc. 2020;9:e015978 DOI: 10.1161/JAHA.119.015978.)
For Sources of Funding and Disclosures, see page 9.
References
- 1. Chapman AR, Shah ASV, Lee KK, Anand A, Francis O, Adamson P, McAllister DA, Strachan FE, Newby DE, Mills NL. Long‐term outcomes in patients with type 2 myocardial infarction and myocardial injury. Circulation. 2018;137:1236–1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Gaggin HK, Liu Y, Lyass A, van Kimmenade RR, Motiwala SR, Kelly NP, Mallick A, Gandhi PU, Ibrahim NE, Simon ML, et al. Incident type 2 myocardial infarction in a cohort of patients undergoing coronary or peripheral arterial angiography. Circulation. 2017;135:116–127. [DOI] [PubMed] [Google Scholar]
- 3. Barnett ML, Grabowski DC, Mehrotra A. Home‐to‐home time—measuring what matters to patients and payers. N Engl J Med. 2017;377:4–6. [DOI] [PubMed] [Google Scholar]
- 4. McDermid I, Barber M, Dennis M, Langhorne P, Macleod MJ, McAlpine CH, Quinn TJ. Home‐time is a feasible and valid stroke outcome measure in national datasets. Stroke. 2019;50:1282–1285. [DOI] [PubMed] [Google Scholar]
- 5. Stienen MN, Smoll NR, Fung C, Goldberg J, Bervini D, Maduri R, Chiappini A, Robert T, May A, Bijlenga P, et al. Home‐time as a surrogate marker for functional outcome after aneurysmal subarachnoid hemorrhage. Stroke. 2018;49:3081–3084. [DOI] [PubMed] [Google Scholar]
- 6. Fonarow GC, Liang L, Thomas L, Xian Y, Saver JL, Smith EE, Schwamm LH, Peterson ED, Hernandez AF, Duncan PW, et al. Assessment of home‐time after acute ischemic stroke in Medicare beneficiaries. Stroke. 2016;47:836–842. [DOI] [PubMed] [Google Scholar]
- 7. Greene SJ, O'Brien EC, Mentz RJ, Luo N, Hardy NC, Laskey WK, Heidenreich PA, Chang CL, Turner SJ, Yancy CW, et al. Home‐time after discharge among patients hospitalized with heart failure. J Am Coll Cardiol. 2018;71:2643–2652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, White HD. Fourth universal definition of myocardial infarction (2018). J Am Coll Cardiol. 2018;72:2231–2264. [DOI] [PubMed] [Google Scholar]
- 9. McCarthy C, Murphy S, Cohen JA, Rehman S, Jones‐O'Connor M, Olshan DS, Singh A, Vaduganathan M, Januzzi JL Jr, Wasfy JH. Misclassification of myocardial injury as myocardial infarction: implications for assessing outcomes in value‐based programs. JAMA Cardiol. 2019;4:460–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Werner RM, Konetzka RT. Trends in post‐acute care use among Medicare beneficiaries: 2000 to 2015. JAMA. 2018;319:1616–1617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wasfy JH, Kennedy KF, Masoudi FA, Ferris TG, Arnold SV, Kini V, Peterson P, Curtis JP, Amin AP, Bradley SM, et al. Predicting length of stay and the need for postacute care after acute myocardial infarction to improve healthcare efficiency. Circ Cardiovasc Qual Outcomes. 2018;11:e004635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Stein GY, Herscovici G, Korenfeld R, Matetzky S, Gottlieb S, Alon D, Gevrielov‐Yusim N, Iakobishvili Z, Fuchs S. Type‐II myocardial infarction―patient characteristics, management and outcomes. PLoS One. 2014;9:e84285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. McCarthy CP, Vaduganathan M, Januzzi JL Jr. Type 2 myocardial infarction―diagnosis, prognosis, and treatment. JAMA. 2018;320:433–434. [DOI] [PubMed] [Google Scholar]
- 14. US Food and Drug Administration . Treatment for heart failure: endpoints for drug development. Available at: https://www.fda.gov/media/128372/download. Accessed August 5, 2019.


