Abstract
Background
Referring patients to specialty care is an inefficient and error-prone process. Gaps in the referral process lead to delays in patients’ access to care, negative patient experience, worse health outcomes, and increased operational costs. While implementation of standards-based electronic referral options can alleviate some of these inefficiencies, many referrals to tertiary and quaternary care centers continue to be sent via fax.
Objective
We describe the design process and architecture for a software application that has been developed and deployed to optimize the referrals intake process by automating the processing and digitization of incoming specialty referral faxes, extracting key data elements and integrating them into the electronic health record (EHR), and organizing referrals.
Methods
A human-centered design approach was used to identify and describe the inefficiencies in the external referral process at our large, urban tertiary care center. Referrals Automation, an application to convert referral faxes to digital referrals in the EHR, was conceptualized based on key stakeholder interviews and time and motion studies. This application was designed using Substitutable Medical Applications and Reusable Technologies (SMART) and Fast Healthcare Interoperability Resource (FHIR) platforms to allow for adaptability into other healthcare organizations.
Results
Referrals Automation software was developed as a healthcare information technology solution to streamline the fax to referral process. The application was implemented into several specialty clinics. Metrics were built-in to the applications to evaluate and guide the further iteration of these features.
Conclusions
Referrals Automation will enhance the referrals process by further streamlining and organizing the patient referral process.
Keywords: access to care, application programming interface, HL7 FHIR, referral, user-centered design
INTRODUCTION
From 1999 to 2009, the number of patient referrals to specialty care in the United States increased from 40.6 million to 105 million.1 Patient referrals are a crucial component of the healthcare system linking primary care to specialty care, where efficient communication is essential for appropriate escalation of patient care. Despite the importance of escalation of care, unclear referral procedures, uncertainty in staff responsibilities, and inadequate tools and resources to fulfill referral requests,2–4 contribute to a referral process that is inefficient and confounding for providers and patients. Breakdowns in referral communication lead to worse health outcomes, increased cost, and appointment delays.5
With the adoption of standards such as Direct and the Consolidated Clinical Document Architecture, health organizations have begun to shift toward use of electronic referrals (eReferrals) to streamline the referral process.3,5–8 Adoption of this new technology is associated with greater provider satisfaction, improved transmission of key referral information, and reduction in healthcare spending.9,10 However, external eReferrals only work if the participating health systems integrate their electronic health record (EHR) systems. As a result, a large proportion of external referrals continue to rely heavily on faxed documents. At our own institution, 47% of annual incoming consult referrals continue to be received via fax. The poor data quality from faxed documents and underdeveloped use of eReferrals within and between different healthcare systems are cited as sources of continued inefficiencies in the referral process.11,12 To address these issues, healthcare systems and health information technology (IT) experts recommend utilizing additional health IT strategies to further automate and streamline the eReferral process.6 However, there are few described examples of production systems that address this need.6,13
With the majority of referrals continuing to be sent via fax, the referrals intake process remains highly manual and cumbersome. Current workflows commonplace at large academic medical centers involve dozens of staff typing in data from a faxed document into the EHR. This results in high referral processing costs, more than 40% of referrals never scheduled at all, and increased patient suffering from delays and poor communication.14–17 Clinic administrative staff experience the burden of significant manual data entry and providers experience inefficient use of appointment slots and frustration with delays in patient care. Health systems may be unable to accurately measure referral turnaround times and access outcomes due to manual processes.
We developed a software tool called Referrals Automation that helps receiving practice staff process faxed referrals, book specialty clinical appointments more efficiently, and monitor referral progress. This application automates the receipt, digitization, information extraction, and creation of a structured referral object within the EHR, nearly eliminating the manual entry of data from inbound referral sources such as faxes. Referrals Automation was developed using Substitutable Medical Applications and Reusable Technologies (SMART) and Fast Healthcare Interoperability Resource (FHIR) toolkits.18,19 We describe the development process and the components of the Referrals Automation application.
METHODS
The Referrals Automation software was developed by the Center for Digital Health Innovation (CDHI) at the University of California, San Francisco (UCSF). The CDHI is a multidisciplinary center founded in 2013 by UCSF to develop, advance, and implement digital health technologies to transform the delivery of healthcare, internally and externally.20
Conception and problem identification
In collaboration with Gestalt Design, Inc. (San Francisco, CA, USA), a human-centered healthcare design consulting group, semi-structured interviews were conducted with external referring providers, clinic staff, and internal providers to develop process maps, better understand their unique perspectives, and identify opportunities for improvement. Patients who were referred to UCSF for specialty care were also interviewed to better understand their experience with the referral and appointment scheduling process. The results of these interviews were condensed into personas to drive product conception.
Time and motion studies
Time and motion studies were performed at the Pediatric Access Center (PAC), a centralized patient access center, to understand the end-to-end referral process, and to identify bottlenecks and opportunities for improvement. The research team observed new patient navigators as they performed referral intake, patient registration, referral creation, and appointment scheduling. All actions taken were identified and timed in seconds over multiple observations. Findings from the interviews and time and motion studies were discussed with the design team and engineering team.
Product design, user feedback, and iteration
After synthesizing the results of the key stakeholder interviews and time and motion studies, we identified a significant need to improve the referral processing experience. We conceptualized a fax to referral automation application. The application, Referrals Automation, was designed to automatically extract referral information from incoming referral faxes, correct transcription errors, update patient demographic information, and create the referral object in the EHR. Wireframes for the application were designed by the development team and reviewed by the key stakeholders. The user workflow and touchpoints for the Referrals Automation application were mapped. A development timeline was established and included weekly user feedback sessions with PAC team members, which allowed for continuous product iteration throughout the development cycle. Data logs of time spent on each screen, processing time per referral, number of referrals processed per day and hour, time taken for system performed activities (ie file upload time, page load time) and application programming interface (API) response times were used to understand usage of the application and improve usability.
RESULTS
Key stakeholder interviews
Four referring provider administrators, six patients, and one specialty care administrator were interviewed. The results of the key stakeholder interviews are summarized in Table 1. Patients, referring provider administrators, and specialty care administrators demonstrated different, but overlapping needs that centered around greater transparency and streamlined referral processing.
Table 1.
Summary of semi-structured interviews with patients, referring provider administrators, and specialty care administrators
| Patients | Key points from interview |
| “Then two weeks passed before I realized, there is this outstanding appointment that I need to schedule. I called back and they said there is nothing in the system.” | Patients want more transparency on what to expect when referred to another provider (ie the office will call them in 3 days). |
| “It would be comforting to know when the referral has been received…and how long it’s taking in case something goes wrong. It’s like when you purchase something online.” | |
| “I had to cancel two weeks in advance because we were going out of town. Someone did not note that I canceled…They said I was a no show” | Administrative delays and communication errors contribute to delays in appointment scheduling and patient uncertainty. |
| Referring provider administrators | Key points from interview |
| “There is an option to upload a referral. Traditionally, we have not done that. We do not know what the workflow is on the other end… Each [specialty] department has their own system.” | Clinics refer to multiple specialty care institutions and find it challenging to manage multiple portals when each specialty care center has its own unique referral portal. |
| “We [nurses] send our referrals as faxes. The front desk staff are the only ones that receive faxes, so they would be the ones to get any notifications UC might send about patient status. They either stack them in the “To Do” basket or shred them. So, I’m not sure if UC sends us receipt notices or not. We don’t get them. I don’t think they do.” | PCP administrators face external and internal processes. The tools they utilize should accommodate local workflows and preferences. |
| “It takes forever if you try to upload anything to [EHR vendor referral portal]. We’ll maybe use it if it’s only one or two pages, otherwise we’ll send it by fax” | Information transfer with specialty care needs to be one touch, skimmable, readily accessible. |
| “Patients call and say ‘hey, I have not heard anything’. We call the access center. Most of the time they got it, but we haven’t heard from them.” | Improved communication and closing the loop between specialty clinics, referring providers and administrators, and patients is desired. |
| “Some primary care physicians want to see the visit summary of the patient’s visit to the specialist. It is useful for us to get an email to let us know a patient has been seen.” | |
| Specialty care administrators | Key points from interview |
| “We need technology, because [we] can't hire enough [full time employees] for their volume… [the current referral work queue is 450] and creeping up…Managing these, including calling/scheduling the patient the rate is 30 referrals per 8 h per full-time employee…. They don't have dedicated staff but probably 2–3 FTE.” | Technology-driven solutions are necessary to increase referral processing efficiency in the setting of limited employee bandwidth. |
Patients desired more transparency about the patient referral process and updates on the status of referrals, stating that “it would be comforting to know when the referral has been received…and how long it’s taking in case something goes wrong.” Breakdowns in patient-specialty clinic communication contributed greatly to referral delays and patients felt the frustrations of scheduling delays as they attempted to schedule their referrals. “Then two weeks passed before I realized, there is this outstanding appointment that I need to schedule.”
Referring clinic administrators are challenged by external, as well as, internal processes as they manage and facilitate the process of sending their own patients’ referrals. They are simultaneously managing patients, insurance companies, hundreds of referrals, and physician requests. Information transfer to specialty care needs to be fast and readily accessible. “It takes forever if you try to upload anything to [the existing external referral portal]. We’ll maybe use it if it’s only one or two pages, otherwise we’ll send it by fax.” Of note, interviews with referring clinic administrators highlighted that it was not feasible to transition hundreds of external referring physicians with unique workflows and IT systems to a single, integrated solution so that our center could easily receive standardized referrals. As a result, they often relied on sending documents to specialty clinics by fax rather than using the existing external referral portal (provided by our EHR vendor, Epic Systems), which further supported the need to build a tool around automating the receipt of faxes rather than forcing external partners to use our electronic referral portal that was foreign to their native workflow. They expected tools they use to accommodate their existing individual workflows and preferences. In addition, closed-loop communication between referring clinics and specialty clinics is desired but often not accomplished. “We call the access center. Most of the time they got it, but we haven’t heard from them….” Lastly, technology-driven solutions are necessary to increase referral processing efficiency in the setting of limited resources, such as limited employee bandwidth and inability to hire additional staff. “We need technology, because [we] can’t hire enough [full time employees] for their volume.”
Time and motion studies
Seven PAC staff members participated in the time and motion study to map out the referral intake process. The process description and recommendations to optimize are summarized in Table 2. Time and Motion studies showed that these cumulative tasks took 719 ± 48 s per referral. Some of the most time-consuming steps identified by the time motion study involved insufficient information transfer, such as calling the referring provider to obtain missing information. These problems were not readily addressable, involving coordination among different referring provider clinics with unique referral placement processes. Key areas for improvement identified included the processing of faxed referrals, looking up the patient in the EHR, entry of demographic information, updating insurance and coverage, creating the referral, finding patient information, calling the patient, and logging the referral. Collectively, automation of these steps would nearly eliminate manual entry of patient information by staff, leading to greater efficiency in the processing of faxed referrals.
Table 2.
Time and motion study for manual referrals processing
| Task | Observations (n) | Time spent (s), mean ± SD | How is this optimized by Referrals Automation? |
|---|---|---|---|
| Move a fax to folder and open it | 28 | 8 ± 6 | Automate and avoid duplication of effort |
| Look up patient in EHR | 29 | 16 ± 13 | |
| Review required information | 17 | 39 ± 27 | |
| Missing info: call referring provider | 2 | 226 ± 106 | Not currently addressed |
| Update demographics, primary care physician, and emergency contacts | 20 | 77 ± 35 | Auto-fill information, system-assisted |
| Update guarantor, insurance, coverage | 19 | 65 ± 48 | |
| Verify insurance | 15 | 21 ± 27 | |
| Update missing insurance details | 5 | 28 ± 35 | Not currently addressed |
| Create referral object in EHR | 25 | 59 ± 19 | Auto-fill information, system-assisted |
| Add relevant patient visit notes | 25 | 21 ± 24 | Not currently addressed |
| Set scheduling status | 12 | 17 ± 15 | Not currently addressed |
| For external referral (notify department, flag, fax referring provider) | 5 | 90 ± 55 | Not currently addressed |
| Find patient info and call patient | 17 | 175 ± 148 | Smart scheduling with patient input |
| Send fax to referral provider | 6 | 16 ± 6 | Not currently addressed |
| Log referral in EHR | 14 | 14 ± 6 | Automate |
| Other miscellaneous administrative tasks | 13 | 73 ± 48 | Not currently addressed |
| Cumulative mean time | 719 ± 48 |
Workflow and components of the Referrals Automation application
We worked with some of our highest volume referring providers and found a significant resistance to using a distinct referral application from their native EHR, even if connected via FHIR. We have instead connected these top referring providers to our EHR via direct protocol referrals. We decided that given the workflow issues, and the fact that hundreds of thousands of referral faxes would continue to arrive annually from smaller practices (many of whose EHRs would not support FHIR), that it was most practical to focus our efforts on the receiving end rather than the sending end. After synthesizing the results of the key stakeholder interviews and time and motion studies, Referrals Automation, a fax to referral automation application, was conceptualized and developed (see Methods section for description of development).
The application uses SMART-on-FHIR for authenticating the user and passing information from the EHR to the application (Figure 1). Incoming faxes are converted to PDF documents using a digitization service, RightFax (Advantage Technologies, Inc., New York, NY, USA) and stored in a fax file server. UCSF’s Health Data Kit (HDK) transmits these files to the optical character recognition (OCR) service hosted on Amazon Web Services (AWS). Commercial OCR software from Nuance (Irvine, CA, USA) was integrated to recognize and extract the demographic and referral information required to create a digital referral object in the EHR (Epic, Verona, WI, USA). Nuance’s software provides confidence values for each extracted data element, which when combined with manual data correction event logs, allowed us to define thresholds to reject values with errors and select values with highest confidence.
Figure 1.
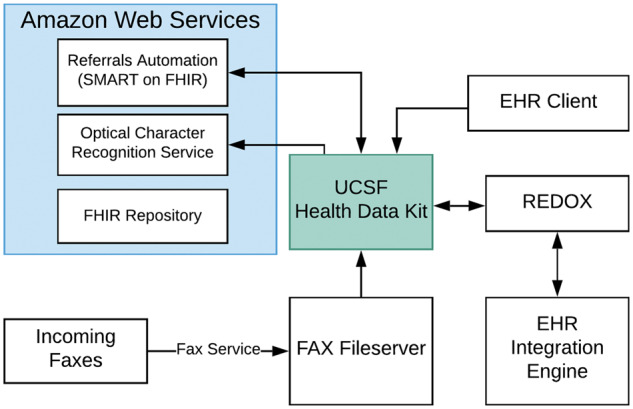
Referrals Automation architecture diagram. Arrows represent data flows between modules. All modules within the Amazon Web Services (AWS) container have bidirectional data flow with each other.
The application uses a mix of integration methods to connect to the EHR: an HL7 FHIR API is used to look up patient and practitioner details from the EHR, EHR-native APIs are used to look up information such as the target referral department, while Health Level 7 version 2 (HL7 v2) interfaces were used to update patient data and create the referral objects in the EHR. The data model centers around the FHIR R3 ReferralRequest resource with references to the EHR’s core FHIR resources: Patient and Practitioner. To model the referring physician office’s coordinator and location, these are represented as contained Person and Location in the ReferralRequest.supportingInfo field, respectively. The ReferralRequest captures the patient’s journey throughout the workflow process so when appointments are scheduled and an actual visit is made, these are represented as Appointment and Encounter, respectively. At the time of implementation, the EHR only supported a handful of read-only FHIR (STU3) resources such as Patient and Practitioner but a writable ReferralRequest resource was required. This gap was addressed by use of a third-party API platform (MuleSoft, San Francisco, CA, USA) to transform the FHIR ReferralRequest data into an HL7v2 format acceptable by the EHR interface and orchestrate consumption of both FHIR and non-FHIR APIs to update the Referral data once in the EHR. These resources are linked to the ReferralRequest as ReferralRequest.supportingInfo and are derived from HL7v2 messages: SIU_S01/S02/S04, ADT_A04.
Redox (Redox, Madison, WI, USA) is used to bidirectionally integrate data from the EHR integration engine into the HDK tool. Redox was utilized so that this program could be expanded into future EHRs. It abstracts the complexity of the health system’s data API and other integrations and provides consistent APIs that can be leveraged across multiple health systems. The application is Health Insurance Portability and Accountability Act compliant and hosted on AWS to allow for rapid application development, deployment, scaling, and support. The Referrals Automation application was also designed to log the details of extracted information so we can track metrics such as number of data elements extracted per referral and error rate of extracted information. The logs will also be used to improve the information extraction engine and create training data sets for future machine-learning and artificial intelligence-based optimizations.
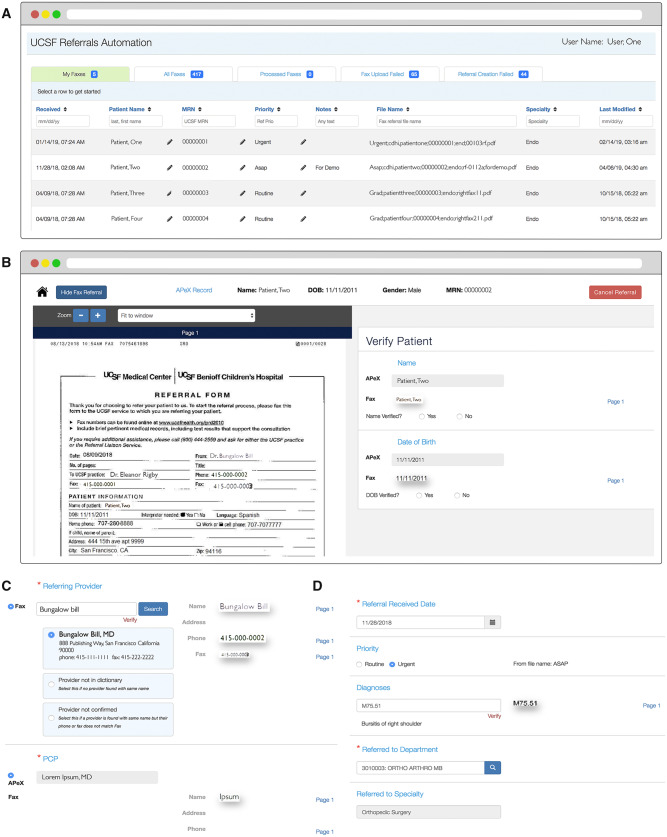
To use the application, a referral coordinator launches the Referrals Automation application from the EHR into an external web browser, allowing the user a side-by-side use of the two applications (Figure 2). In the background, the OCR Service running in AWS automatically processes all the uploaded files, extracts the demographics and referral information, and keeps them ready for a referral coordinator to begin work processing referrals. The first screen (Figure 2A) demonstrates how faxes are organized into different tabs. The My Faxes tab allows the user to visualize the faxes they are assigned to process. The faxes in the My Faxes tab can be organized by receipt date, priority, and specialty. After the referral is processed, they get transitioned into the Processed Faxes tab. Next, the system matches the patient with the medical record number and the referral coordinator verifies that the patient’s name and date of birth in the EHR matches with the values extracted from the fax. The next screen (Figure 2B) allows the referral coordinator to visualize the scanned document and review the patient information that was extracted. This step automates the manual entry of patient information and demographic information. The application checks the EHR for available patient information and allows the coordinator to use the available information from the EHR when appropriate. The referring provider information is also extracted and verified against a database for contact information and location (Figure 2C). Lastly, the referral date, priority, diagnosis, and specialty of referral are extracted for the coordinator for review (Figure 2D). After the data elements are verified, the referral object is created in the EHR allowing the referral coordinator to complete the rest of the process from the work queue.
Figure 2.
Screenshots and workflow of the Referrals Automation application. (A) The home screen of Referrals Automation for new patient navigators. Each row represents an individual referral. (B) The scanned referral and extracted patient information. This step allows the new patient navigator to verify the information. (C) The referring provider and primary care provider information are also extracted from the document and verified using a master provider index. (D) Lastly, the referral priority, diagnosis, and referral department information extracted and verified. All identifiers depicted in the figures are fabricated and do not represent real data.
Implementation of the Referrals Automation program
Access to the application in AWS is restricted to the medical center’s internet protocol addresses. Referrals Automation is a web application and hence does not require installation on any end users’ computers. It was built and tested for Google Chrome, which is the default browser on employee computers. Implementation was completed in a stepwise fashion. Approvals for API connectivity occurred through our local institutional “Digital Diagnostics & Therapeutics Committee,” responsible for review and approvals of all API-connected applications at our institution, and through our EHR vendor’s approval process, which involved the registration of the application and defining its subscription to a list of APIs and scoping its usage for internal-use only.21 To date, Referrals Automation has been implemented in four areas: two centralized access centers which each process referrals for a large number of specialties (PAC and Cancer Services Referral Center) and two specialty practices (Orthopedic Surgery and Urology). The application now processes over 20% of all incoming faxed referrals to UCSF.
DISCUSSION
The human-centered design process described in this manuscript identified and quantified steps related to the referral process that delay patient access to specialty care. Tasks such as the manual entry of information from an incoming fax emerged as immensely time-consuming, tedious, error-prone, and well-suited to automation. From a methodology and technological standpoint, this application yields several advantages. First, the application aims to improve the turnaround time from referral receipt to a scheduled appointment by automating key steps in the patient referral workflow. Second, the referrals user interface promotes greater organization and accountability to complete scheduling of patient referrals. Third, the application was built using the SMART on FHIR standard, allowing for adaptability and future use by other healthcare organizations. Lastly, the current literature on technological solutions for improving the referrals process is limited to survey and questionnaire data.5 The Referrals Automation application was designed with analytics in mind, allowing for easy access to usage data, such as user action logs, to help drive both further product iteration and evaluation as well as identify opportunities for operational and process improvements.
Despite the increased adoption of EHRs and eReferrals tools, faxed referrals for specialty care remain highly prevalent.3,5–8 Smaller practices refer to a wide variety of specialty providers, and they lack technological infrastructure to develop custom integrations with each partner. While the EHR gives much needed structure to diverse clinical data, poor EHR interoperability is a major barrier to eliminating faxes from the workflow.22,23 A national survey of healthcare organizations found that only 30% of hospitals and 10% of ambulatory clinics engage in health information exchange, citing financial sustainability and regulatory restraints as key impediments.24 The 21st Century Cures Act describes rules that support interoperability, API use and restrictions on information blocking, and sets the stage for health IT developers to tackle this problem with more generalizable solutions.25 Until then, the continued utilization of faxed referrals is a reality that many healthcare organizations grapple with and Referrals Automation aims to address the inefficiencies of this dated but widespread method of information exchange.
Of note, there were inherent limitations in the FHIR-based APIs themselves and their implementation in our EHR, requiring a hybrid approach. We found that the EHR FHIR resources implementation met the minimum information needed as set by policy, but it was insufficient for supporting the health systems’ operational needs. For example, the 2015 Edition Certified EHR Technology (2015 CEHRT) does not require use of FHIR Write APIs, and our current EHR implementation does not support them. As a result, we leveraged an HL7 v2 message to write the Referral data back to our EHR instead of the FHIR Write API. The core data was further augmented by a custom API that set the Referral’s priority, referred-to Specialty, and timestamp of the inbound Fax as received into the health system, which is not available in the existing specification. Also, we could not use the FHIR ServiceRequest because it was not in the current FHIR STU3 specifications at time of implementation and our EHR did not have write APIs for the referral resource. We persisted the data in a third-party FHIR repository which was FHIR STU3 compliant.
There are a few limitations to this tool. First, this technology is built around the current state in which the majority of specialty referrals are still sent by fax. We hope to see further uptake of standardized electronic referrals, which would limit the need for this tool. Second, despite automating several steps in the referral process, key steps still require human intervention, such as approval of each suggestion from the software to reduce the risk of creating an erroneous referral record. In addition, this technology is unable to address significant interpersonal and structural inefficiencies such as reconciling patient or insurance information missing from the fax. Another limitation of the technology is the reliance on traditional OCR methods for automating text ingestion, meaning that templates must be created to show the OCR software where to look on each page for the required text. New types of incoming faxes require creation of a new template. Making referral communication more efficient requires a sociotechnical approach that involves not only the implementation of new technology to improve workflow but also good clinical practices such as communication and collaboration between internal and external healthcare workers.6
Despite these limitations, by speeding up one of the steps in a complex referral process, the protocols and applications described here have the potential to enable more efficient processing of patient referrals to specialty care. The team plans to further evaluate and expand the functionality. Key features in the development pipeline include using machine learning and artificial intelligence to improve information extraction and prioritize referrals based on clinical complexity and urgency. Lastly, a recent scoping review of the literature highlighted the lack of quantitative data on the efficacy of health IT solutions to improve the patient referral process.5 Referrals Automation was designed to allow institutions to track metrics such as the elements extracted, error rates, and time stamps. These data will allow institutions to rigorously evaluate and iterate the application.
CONCLUSION
We describe the design and technical infrastructure of Referrals Automation, an EHR-integrated SMART on FHIR application to expedite the processing of faxed referrals by automating the receipt, information extraction, digitization, and creation of a digital referral record in the EHR. This application has been deployed widely at our large tertiary and quaternary care institution, minimizing the manual entry of faxed data and streamlining the intake process for incoming referrals. In addition, the SMART on FHIR framework allows other healthcare systems to more easily implement the application.
FUNDING
The development, design, and evaluation of Referrals Automation was funded by the UCSF Center for Digital Health Innovation.
AUTHOR CONTRIBUTIONS
All authors except H.L. contributed to the design and development of Referrals Automation. All authors contributed to the analysis of data and drafting of the manuscript. All authors approved the final version of the manuscript.
CONFLICT OF INTEREST STATEMENT
None declared.
DISCLOSURES
A.N. has received research support from Cisco Systems, Inc.; has received consulting fees from Nokia Growth Partners and Grand Rounds; serves as advisor to Steady Health (received stock options); has received speaking honoraria from Academy Health and Symposia Medicus; has written for WebMD (receives compensation); and is a medical advisor and co-founder of Tidepool (for which he has received no compensation).
REFERENCES
- 1. Barnett ML, Song Z, Landon BE. Trends in physician referrals in the United States, 1999-2009. Arch Intern Med 2012; 172 (2): 163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hysong SJ, Esquivel A, Sittig DF, et al. Towards successful coordination of electronic health record based-referrals: a qualitative analysis. Implement Sci 2011; 6 (1): 84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Joschko J, Keely E, Grant R, et al. Electronic consultation services worldwide: environmental scan. J Med Internet Res 2018; 20 (12): e11112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kim Y, Chen AH, Keith E, et al. Not perfect, but better: primary care providers’ experiences with electronic referrals in a safety net health system. J Gen Intern Med 2009; 24 (5): 614–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Azamar-Alonso A, Costa AP, Huebner L-A, Tarride J-E. Electronic referral systems in health care: a scoping review. Clin Outcomes Res 2019; 11: 325–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Esquivel A, Sittig DF, Murphy DR, et al. Improving the effectiveness of electronic health record-based referral processes. BMC Med Inform Decis Mak 2012; 12 (1): 107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.HL7 Contributers. C-CDA (HL7 CDA® R2 Implementation Guide: Consolidated CDA Templates for Clinical Notes - US Realm). HL7 Int. 2019.
- 8.Direct Project contributors. Welcome to the Direct Project’s Implementation Group [Internet]. http://wiki.directproject.org/Main_Page Accessed April 21, 2020.
- 9. Doumouras AG, Anvari S, Breau R, et al. The effect of an online referral system on referrals to bariatric surgery. Surg Endosc 2017; 31 (12): 5127–34. [DOI] [PubMed] [Google Scholar]
- 10. Cannaby S, Wanscher MCE, Pedersen MCD, et al. The cost benefit of electronic patient referrals in Denmark—summary report. Stud Health Technol Inform 2004; 100: 238–45. [PubMed] [Google Scholar]
- 11. Hughes CA, Allen P, Bentley M. eReferrals: why are we still faxing? Aust J Gen Pract 2018; 47 (1–2): 51–6. [DOI] [PubMed] [Google Scholar]
- 12. Warren J, White S, Day KJ, et al. Introduction of electronic referral from community associated with more timely review by secondary services. Appl Clin Inform 2011; 02 (04): 546–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ramelson H, Nederlof A, Karmiy S, et al. Closing the loop with an enhanced referral management system. J Am Med Inform Assoc 2018; 25 (6): 715–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Forrest CB, Shadmi E, Nutting PA, et al. Specialty referral completion among primary care patients: results from the ASPN referral study. Ann Fam Med 2007; 5 (4): 361–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Mehrotra A, Forrest CB, Lin CY. Dropping the Baton: specialty referrals in the United States: specialty referrals in the United States. Milbank Q 2011; 89 (1): 39–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. O’Malley AS, Reschovsky JD. Referral and consultation communication between primary care and specialist physicians: finding common ground. Arch Intern Med 2011; 171 (1): 56–65. [DOI] [PubMed] [Google Scholar]
- 17. Stille CJ, McLaughlin TJ, Primack WA, et al. Determinants and impact of generalist-specialist communication about pediatric outpatient referrals. Pediatrics 2006; 118 (4): 1341–9. [DOI] [PubMed] [Google Scholar]
- 18. Mandel JC, Kreda DA, Mandl KD, et al. SMART on FHIR: a standards-based, interoperable apps platform for electronic health records. J Am Med Inform Assoc 2016; 23 (5): 899–908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Mandl KD, Mandel JC, Murphy SN, et al. The SMART Platform: early experience enabling substitutable applications for electronic health records. J Am Med Inform Assoc 2012; 19 (4): 597–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Center for Digital Health Innovation [Internet]. Center for Digital Health Innovation. https://www.centerfordigitalhealthinnovation.org Accessed April 21, 2020.
- 21. Auerbach AD, Neinstein A, Khanna R. Balancing innovation and safety when integrating digital tools into health care. Ann Intern Med 2018; 168 (10): 733–4. [DOI] [PubMed] [Google Scholar]
- 22. Kruse CS, Kristof C, Jones B, Mitchell E, Martinez A. Barriers to electronic health record adoption: a systematic literature review. J Med Syst 2016; 40 (12): 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Meigs SL, Electronic SM. Electronic health record use a bitter pill for many physicians. Perspect Health Inf Manag 2016; 13: 1d. [PMC free article] [PubMed] [Google Scholar]
- 24. Adler-Milstein J, Bates DW, Jha AK. Operational health information exchanges show substantial growth, but long-term funding remains a concern. Health Aff 2013; 32 (8): 1486–92. [DOI] [PubMed] [Google Scholar]
- 25. Barlas S. The 21st Century Cures Act: FDA implementation one year later, some action, some results, some questions. P T 2018; 43 (3): 149–51, 179. [PMC free article] [PubMed] [Google Scholar]