Abstract
Objective
Healthcare systems have adopted electronic health records (EHRs) to support clinical care. Providing patient-centered care (PCC) is a goal of many healthcare systems. In this study, we sought to explore how existing EHR systems support PCC; defined as understanding the patient as a whole person, building relational connections between the clinician and patient, and supporting patients in health self-management.
Materials and Methods
We assessed availability of EHR functions consistent with providing PCC including patient goals and preferences, integrated care plans, and contextual and patient-generated data. We surveyed and then interviewed technical representatives and expert clinical users of 6 leading EHR systems. Questions focused on the availability of specific data and functions related to PCC (for technical representatives) and the clinical usefulness of PCC functions (for clinicians) in their EHR.
Results
Technical representatives (n = 6) reported that patient communication preferences, personalized indications for medications, and end of life preferences were functions implemented across 6 systems. Clinician users (n = 10) reported moderate usefulness of PCC functions (medians of 2–4 on a 5-pointy -35t scale), suggesting the potential for improvement across systems. Interviews revealed that clinicians do not have a shared conception of PCC. In many cases, data needed to deliver PCC was available in the EHR only in unstructured form. Data systems and functionality to support PCC are under development in these EHRs.
Discussion and Conclusion
There are current gaps in PCC functionality in EHRs and opportunities to support the practice of PCC through EHR redesign.
Keywords: patient-centered care, electronic health records, patient-generated data
LAY SUMMARY
Patient-centered care (PCC) is healthcare that treats the whole patient, not just the patient’s problem. This shift requires that healthcare decisions incorporate what matters to patients, including patients’ values, preferences, and goals. PCC should include developing trusting relationships, sharing decisions about treatment, and listening to information from patients about their behavior and environment. Healthcare systems nationwide are now using electronic health records (EHRs). To learn about how well the EHRs support PCC, we recruited technical representatives who worked with, and clinicians who used, 6 major EHRs. We surveyed the technical representatives about what functions are available in their specific EHR to support PCC. We surveyed clinicians about how useful the PCC functions available in their EHR are for supporting PCC. We also conducted follow-up interviews to find out more about PCC and the EHR. Technical representatives reported all 6 systems included functionality for communication and end of life preferences. Clinician users reported that the PCC functions were moderately useful. Our results showed that PCC is beginning to be supported by EHRs, and there is room for improvement in supporting PCC by working to improve EHR design.
BACKGROUND AND SIGNIFICANCE
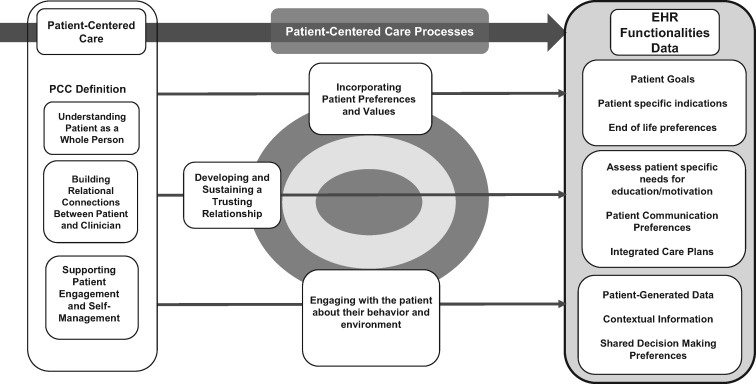
Patient-centered care (PCC) is an ethical imperative that shifts the approach to healthcare from disease- to person-centric. The National Academy of Medicine defines PCC as “providing care that is respectful of, and responsive to, individual patient preferences, needs, and values, and ensuring the patient's values guide all clinical decisions.”1 We propose that PCC involves (1) understanding the patient as a whole person by incorporating patient preferences and values, (2) building relational connections between the clinician and patient by developing and sustaining a trusting relationship, and (3) supporting patients in actions that promote self-management of their health by engaging with them about their environment and behavior.2,3
PCC is being proposed and implemented in healthcare systems and health information technology (health IT) is critical to support these processes.4,5 One PCC approach is Age-Friendly Health Systems, centered on “what matters” to the patient and including incorporating patient goals in the development of comprehensive care plans.6,7 Another is the Veterans Health Administration’s Whole Health program, supported by the Office of Patient Centered-Care and Cultural Transformation. Whole health is characterized by relationship-building between Veterans and their care teams, patient self-management focused on well-being, and traditional as well as complementary and integrative health options.8,9 PCC implementation is also beginning to incorporate contextual data—information about patients’ beliefs, behavior, or environment into clinical care10 and into the electronic health record (EHR). Patient-generated data (PGD; closely related to contextual data) encompasses many types of data provided by the patient, including outcomes, activity, or behavior tracking via output from wearable devices. PGD may also include patient-reported goals, values, and preferences.11–15 PCC approaches may require integrating contextual and PGD into clinician facing views, which could effectively summarize the patient’s environment including social history, and current health behaviors.16–20
Despite the imperative of PCC and the emerging frameworks to support it, health IT does not fully support this focus shift. Clinicians using EHRs spend more time documenting with less time for face to face patient care, hindering communication21 in the patient encounter.22 Extensive coordination among the care team is required for some EHR interactions and for decisions about what information to access or input to a patient’s electronic record. This communication coordination creates barriers to processing patient information like patient portal messages.23,24 Despite these challenges, PCC functions in the EHR are being recognized as crucial. Documenting PCC information and capturing patient preferences is necessary to realize the vision of personalized precision medicine,25,26 and the EHR should support effective workflow to optimize PCC processes.27,28 Figure 1 illustrates the links among PCC definitions, processes, and EHR functions, depicting how EHR solutions for PCC should reinforce the processes central to PCC.
Figure 1.
Patient-centered care definitions and processes mapped to electronic health record functionalities. Abbreviations: EHR: electronic health record; PCC: patient-centered care.
OBJECTIVE
We used surveys and semi-structured interviews to explore how existing EHRs support PCC by assessing (1) technical representatives’ perceptions of the availability of PCC functions in EHRs and (2) clinician users’ perceptions of the capacity of their specific EHR to support PCC.
MATERIALS AND METHODS
Study design
In our mixed-methods exploratory study, surveys were administered to technical representatives and clinician users of 6 leading EHRs. Follow-up semi-structured interviews explored further details of survey responses. The project was designated a quality improvement study by Veterans Affairs Research and Development and approved by the University of Utah IRB.
Study sample
We approached technical representatives from 7 highly rated EHR systems.29 We expected that these representatives, although not designers, would be generally aware of current and future EHR functionalities. Technical representatives from 6 of the 7 EHR systems agreed and this determined the EHR systems explored in our study. We recruited 10 clinician users from those 6 systems by email and word of mouth. Five of the EHR systems are commercial systems which together account for over 75% of market share. One is a government-based system. To ensure participant privacy and promote candid responses, we informed participants that we would not link specific EHRs to survey results.
Survey and telephone interviews
Surveys were completed online using Qualtrics software30 and queried technical representatives about the current functionalities of their particular EHR system (eg, Is functionality available for the EHR to collect and display patient’s treatment-related preferences—yes or no?). A parallel adapted survey queried clinicians about the usefulness of their system’s current PCC functions for clinical care (eg, How useful is your EHR support for documenting and reviewing patients’ treatment-related preferences) with responses rated on a 5-point Likert scale from “not at all useful” to “extremely useful.”
Follow-up telephone interviews revealed additional details complementary to survey results about current implementation and future plans. Telephone interviews were recorded, de-identified, and transcribed by the Veterans Affairs Centralized Transcription Services Program.31
Analytic approach
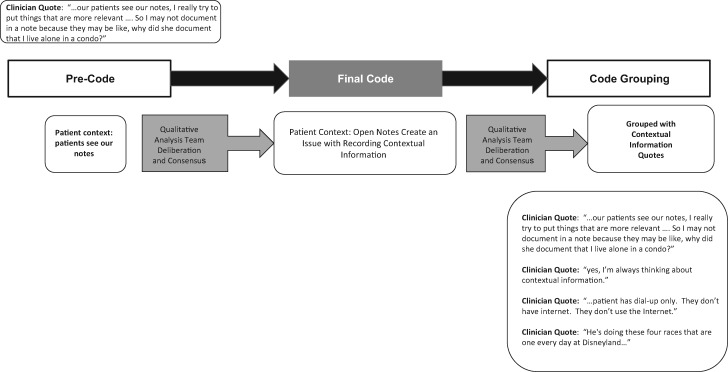
We conducted descriptive analyses of survey data by participant category (technical representative or clinician user) and EHR system. The study team’s health psychologist, informaticist, and research staff member, all of whom have extensive experience with qualitative research, conducted qualitative thematic analyses using the software program ATLAS.ti.32–34 We reviewed the transcripts and assigned precodes—general categorizations drawn directly from participants’ words (eg, see Figure 2). We iteratively reviewed these precodes and consolidated them into similar groups, resolving any disagreements among coders using a consensus approach. We combined codes into groupings with similar codes and then developed themes reflecting participants’ perspectives about the specific EHR system.
Figure 2.
Coding process specific example.
RESULTS
Survey results
One technical representative and up to 3 clinician users from each of the 6 represented EHR systems reported (see Table 1). Survey results of technical representatives showed that all 6 EHRs included some functionality to record and display patient goals and preferences, goals related to personalized indications for medications, and end of life preferences (see Table 2). The other PCC functions we assessed were supported by some EHRs but not all. The PCC functions identified as least available in the 6 EHR systems were the ability to record and display patient-specific needs for education and health-related motivation, which could include assessments of health literacy35 or patient activation.36
Table 1.
Demographics of EHR technical representatives and clinician users
| Demographics | Technical representatives (n = 6) | Clinician users (n = 10) | ||
|---|---|---|---|---|
| n | % | n | % | |
| Sex | ||||
| Male | 4 | 66.7 | 7 | 70 |
| Female | 2 | 33.3 | 3 | 30 |
| Mean (R) | Mean (R) | |||
| Age | ||||
| Mean age | 43 (29–59) | 54 (39–64) | ||
| Years working with EHR system | ||||
| Mean years | 12 (6–20) | 12 (6–23) | ||
Abbreviation: EHR: electronic health record.
Table 2.
EHR functionality and user ratings of usefulness for supporting patient-centered carea
| Functionality exists in EHR |
Usefulness of functionality in EHR |
|||||
|---|---|---|---|---|---|---|
| Technical representatives (n = 6) |
Clinician users (n = 10) |
|||||
| Mean/median usefulness ratingb | Range of responses | Users who rated function “very or extremely useful” |
||||
| n | % | n | % | |||
| Understanding the patient as a whole person | ||||||
| Patient goals | ||||||
| Patient goals and preferences | 6 | 100 | 1.8/2 | 1–5 | 2 | 20 |
| Patient treatment-related preferences | 3 | 50 | 1.53/2 | 1–4 | 2 | 20 |
| Patient treatment-related goals | 5 | 83.3 | 1.93/3.5 | 1–5 | 5 | 50 |
| Patient life goals | 4 | 66.7 | 1.73/2.5 | 1–5 | 2 | 20 |
| End of life preferences | 6 | 100 | 2.13/3.5 | 2–5 | 5 | 50 |
| Patient specific goals | ||||||
| Goals related to indications for medications | 6 | 100 | 2.33/4 | 1–5 | 6 | 60 |
| Goals related to monitoring (labs) | 5 | 83.3 | 2/3 | 1–5 | 3 | 30 |
| Building a relationship with the patient | ||||||
| Integrated care plan | 5 | 83.3 | 1.53/3 | 1–5 | 3 | 30 |
| Assessing patient specific needs for education/motivation | 3 | 50 | 1.6/2 | 1–5 | 1 | 10 |
| Patient communication preferences | 6 | 100 | 1.8/2 | 1–5 | 2 | 20 |
| Supporting patient self-management behaviors | ||||||
| Patient-generated data | 5 | 83.3 | 1.8/3.5 | 1–5 | 5 | 50 |
| Contextual information about the patient | 5 | 83.3 | 1.87/3 | 1–5 | 2 | 20 |
| Shared decision-making preferences | 5 | 83.3 | 2.33/2 | 1–4 | 2 | 20 |
Abbreviation: EHR: electronic health record.
Most functions result in unstructured data.
Range 1–5 where 1 = not useful, 3 = moderately useful, 5 = very useful.
Clinician users reported on the usefulness of the PCC function within their EHR (see Table 2). Median usefulness ratings are reported on a 5-point Likert scale with 5 representing “extremely useful.” Medians ranged from 2.0 (for patient preferences related to communication, treatment, and shared decision-making and information about patient needs for education or motivation) to 4.0 (for goals related to personalized indications for medications).
Interview results
A total of 12 participants (4 technical representatives and 8 clinicians) completed the follow-up interview; declines cited lack of time. The themes resulting from our qualitative analysis are described in Table 3. We also provide illustrative quotes from each theme below. Clinician responses are overrepresented in quotes for space because technical representatives generally described data locations or entry methods. Technical representative responses are noted below.
Table 3.
Identified themes and description
| Identified themes | Explanation and description details |
|---|---|
| When there is not a shared conception of PCC it is difficult to have a shared perspective on EHR functions |
|
| The documentation of goals does not match the construct of goals and patient contextual data is valuable, but not systematically documented in the EHR |
|
| There is a collective challenge in representing the patient and the patient’s needs in an integrated way |
|
| PGD is an emerging function in EHRs |
|
Abbreviations: EHR: electronic health record; PCC: patient-centered care; PGD: patient-generated data.
Theme 1: When there is not a shared conception of PCC, it is difficult to have a shared perception of EHR functions
The clinician views of PCC that emerged from our interviews indicated that there was not a clear consensus about what PCC is and what comprises PCC information. For example:
“I’m thinking of patients who are fine taking medications and then I have patients who are really …[saying] I do not want to be on anything I don’t need to be on….[not recording this in the EHR] wouldn’t be something I would say is a short coming of our EMR at all.”
For some EHRs, notes on communication and other preferences are available in a central location:
“We do have a summary page on each patient that, an overview of their care and it pulls in… there’s also a portion on there with communications between providers…I’ll mark it as [an electronic] sticky note where I could type in patient’s daughter phone number, call her first. And then maybe nursing could type it into the box, patient does not want… breakfast at seven AM, they want it at nine AM.”
The preference for breakfast time represents a different level of what matters to a patient: convenience rather than patient values.
Clinicians perceived that EHR functions that allowed them to record patient personalized lab or medication goals, and reasons for referral to other services were valuable:
“I think [it’s] important because there’s any number of reasons why you might send someone to cardiology. And there’s nothing that (cardiology) hate(s) more than just getting a referral and they don’t know …. why are you sending me this patient?”
In other words, team communication is enhanced when the EHR enables communicating a personalized reason.
One clinician addressed the value of recording personalized goals for lab and ranges for guideline consistent clinical care.
“…. if the patient did meet criteria like being over 80 years old it might be nice to know, ….I’ve got a…[guideline that] permissibly allows this person to have a little bit higher blood sugars or high blood pressures.”
Treatment-related end of life preferences were systematically documented. In the 2 examples below, clinicians described preferences as valuable, available, and shared with the patient. A Physicians Order for Life for Life-Sustaining Treatment (POLST) form facilitates patient wishes in the form of physician’s orders to support patients and clinicians in delivering care that is consistent with a patient’s end of life preferences.
“Whether or not they want aggressive treatment, CPR, that kind of thing, placed on a ventilator. That to me is very important.”
“So we can document the findings with the initial conversation in the assessment and plan and I might even do a POLST form right there in the room so that I have a copy and give them the originals.”
For clinicians the purpose, the mechanisms, and the functionality for end of life preferences were of clear use in clinical care.
One clinician was not sure where to find these data within their specific EHR system.
“I don’t think it’s common knowledge about where to find that information (end of life wishes). If this is an unconscious person I don’t know where I would find that information.”
A technical representative’s response about end of life preferences data location indicated that even when available, these preferences may not be particularly convenient to access.
“So there’s … a scanned copy of the document … stored as part of the patient’s record. And then, within the demographics field you enter … an advanced directive and you choose, like you can choose family trust set up, you can choose DNI [do not intubate], DNR [do not resuscitate].”
Overall, clinicians were not in uniform agreement about what PCC is, but in an area in which PCC concepts were more clearly defined, the relevance to clinical care was obvious.
Theme 2: The documentation of goals does not match the construct of goals and patient contextual data is valuable, but not systematically documented in the EHR
Simply capturing the goals was not considered “enough.” Clinicians highlighted the importance of engaging with patients about their goals and monitoring the goals.
“I would say generally, any care planning component, …. the diagnosis, goal, and objective, and interventions, (such as) medications, or lab studies, or physical therapy…. Any of those things that we do for patients as providers, we need to engage with the patient about …. achieving those goals, objectives, and interventions, and what their preferences are for those.”
This clinician went on to say that engaging with patients about goal progress is not generally part of clinical workflow:
“Today, we providers just assume the patients are going to do these things… But there is no back and forth dialogue about whether or not it gets done. And that’s why patient compliance is so bad, patient literacy is so bad… we’re not truly engaging with patients on these things… I would say the most important thing we can do next in health care delivery in the world is to engage patients on all of those preferences, all of those literacy issues, all of those factors that play into whether or not… they’re compliant.”
Another clinician stated:
“[Goal progress is] important from a quantitative perspective, but the most important thing is the patient’s perception of their improvement. And so a patient reported outcome actually has a very valid place in understanding quality and outcomes in a value based system…. if you are going to move into a value based system you have to factor in what is perceived and valued by the patient regarding quality and cost.”
Goal achievement is generally not tracked, presumably limiting the value of goals related data as a tool for enhancing care.
“Well, I guess that’s the salient point here… there’s no event driven technology to know the status of whether or not a goal is being achieved.”
Goal related information was perceived as difficult to store and access:
“You can dig around in the EHR and find out what providers have put in their notes, or put in their orders. There’s no uniform way to identify patient goals.”
Clinician respondents also highlighted their practices for eliciting goals:
“Oh it’s always part of my conversation like what, between now and when I see you again, what you know, let’s make a plan. It’s definitely part of my clinic, and part of my work flow but… documenting I would say is not done, unfortunately.”
A distinction was drawn between types of goals (life and personal) which potentially could be stored in different ways:
“So, lifestyle, we have lifestyle goals we kinda have, oh gosh there’s maybe fifteen or twenty that vary from go to AA meetings to exercise.”
“I don’t know about their personal goals about like seeing their daughter graduate or being able to do a marathon. I don’t know if there’s a discrete place where I would know to look to see what this person’s goals are.”
Additionally, clinicians noted that goals might differ based on personalized patient factors:
“the patient that has a short-term life expectancy their goals are gonna be different than the one who has a longer life expectancy. So I think it’s kind of important to know those so that you can be realistic in addressing and helping them to achieve those goals.”
EHR functions that allowed clinicians to record a patient’s goals were cited as important but concerns were raised about how this information is handled in the EHR, how it might be used, and whether its inclusion would be a critical component in the EHR.
Contextual information about a patient’s life was perceived as highly valuable as in the examples below:
“I’m always thinking about contextual information.”
“You know if they can’t get up here for blood draws…or if they’re financially in a situation where they’re having trouble getting all their medications and appropriate amount of food and that kind of thing, it’s nice to know”
The contextual information was not systematically captured within the EHR, sometimes due to clinician failure to log:
“marital status. So, like the spouse’s name and how many kids they have and how many years of college they have, those fields are there…. I don’t know that I’ve ever really filled them out.”
In some cases, clinicians could flag information to use later in conversation with patients:
“…she broke up with her boyfriend… or, walks her dog every day for exercise, I might put that in my note. But I would probably put in [an electronic] sticky note too cause it’s there. And I can say…, how’s Jax? Are you still walking him every day?”
The quotes above demonstrate the challenges of moving to a PCC-based healthcare system and of determining what the patient outcomes of such a values-based system should be.
Theme 3: There is a collective challenge in representing the patient and the patient’s needs in an integrated way
Integrated plans with multiple stakeholders were rated of moderate usefulness by clinicians in our survey (3 on the 5 point scale). The qualitative data revealed some of the difficulties with achieving useful plans including problems with prioritization, communication, and complexity of documentation:
“Well it’s really critical because you can have….multiple providers taking care of multiple problems that a patient has, and the goals, objectives and interventions can be in direct conflict.”
In other words, integration itself is a more complex issue than is often addressable given at times competing goals. Another respondent spoke to the complexity of a multi-stakeholder environment:
“care is not just going to see a single physician, there’s a whole spectrum of people that are going to be involved… and having all of that function as one is definitely going to be the most important part of having patient focus or patient-centered care.”
Participants addressed the difficulties of retaining values-based data in the EHR in a multi-stakeholder environment:
“we have one chart and we have one problem list, and we have one past medical history… And you’re managing her heart disease, you don’t care about her recurring UTIs, that’s not relevant to you. ….Still specialists will complain about having to see problems that they don’t care about to the point that they’ll delete them.”
In essence, across the spectrum of multiple stakeholders, the perceived value of PCC and integrated care is not consistent. Specialty care providers may even object to inclusion of PCC information displays.
Theme 4: Patient-generated data is an emergent feature in EHR systems
Technical representatives indicated that for many of the 6 represented systems PGD was going to be an available function in the future:
“They’re working on device integration with like Fitbits and pulse ox and you know your scale for patients with congestive heart failure, and glucose and blood pressure monitors. So they are looking at device integration, and that’s coming, but we don’t have that now.”
“we fully support device integration. We have capital technology for that….a lot of times we’ll go ahead and send the patients home with specific Bluetooth enabled devices, like the glucometer, like the blood pressure cuff, like a scale and we’re monitoring weight, and that information is automatically transmitted to their personal health record in recordings.”
Indications are that these data are emergent as clinicians in our sample had not seen this PGD device data:
“I’m trying to think. Gosh, I don’t think I’ve had anybody come in with their Fitbit data yet.”
One clinician highlighted patient editing capacities for PGD beyond devices, such as medical history and social information.
“we actually allow patients, to ahead of time, enter and modify their … past medical history, social history, family history, surgical history, they can also edit … some of their social history that can be there, substance use, sexual history, all of that.”
A technical representative described where PGD could be found.
“Within the progress note they can download it and view it just when they’re seeing the patient or they can go in ahead of time and look at it.”
PGD was often conceptualized as device integration and is being increasingly recognized as a broader concept integrated with contextual data. Data storage descriptions suggested access may not be particularly seamless.
DISCUSSION
The development of EHR solutions promoting PCC has been characterized as an ethical necessity.37 We used an exploratory mixed-methods approach to advance the understanding of current EHR functionality relevant to PCC. We assessed 13 EHR functions consistent with PCC implemented across 6 EHRs. Those PCC functions least commonly implemented in the EHR relate to patient goals or building a relationship with the patient (patient treatment-related goals, patient life goals, and patient needs for education/motivation; rated middling in terms of usefulness). This may reflect challenges with data access and uncertainty about how to integrate this data into clinical care.
Our results suggest clinician confusion about what PCC should look like at the point of care. Contextual, goal-related, and values-based information was discussed by respondents as a valuable part of clinical care, but clinicians expressed concerns about how this information could be recorded and accessed. PCC is dynamic, complex, and relationship-based whereas the EHR is organized as a tightly structured system. Thus, EHR design will be complemented by continued study of PCC so that constructs and optimal processes can be mapped to EHR design with more precision.
Our results indicate that capturing contextual information about patients16 supports clinicians in understanding patient needs. Clinicians described using contextual information to build rapport (eg, awareness of a patient’s dog walking or boyfriend breakup) or to identify preferred inpatient breakfast times. Patient preferences for breakfast time and communication by phone call are important. However, such preferences are relatively narrow in the spectrum of patient preferences,38 which often address more consequential preferences such as treatment for prostate cancer39 or care at the end of life.40 Contextual data are just beginning to be recognized and included in clinical care and care must be taken to determine optimal ways to present these data.10
Implications for EHR design
The results of this study suggest that EHR systems are building PCC capacity. Additional probing of EHR technical representatives and clinician users demonstrates that PCC tasks are complex from both the clinical care and health IT perspectives. Clinician respondents endorsed the importance of PCC processes that include tracking patient goals across broad dimensions, allow sharing information across care plans, and including contextual information. This is encouraging from the perspective of promoting PCC, as some PCC-related tasks have been found by other teams to be distracting when integrated within the EHR.41
We identified gaps in usefulness of emerging PCC functions. These gaps are similar to other deficits in EHR functioning such as difficulty accessing PCC information like patient preferences.26 In addition, our findings are similar to findings related to studies of patient-reported outcomes (PROs) in which clinicians were enthusiastic about the overall value of PROs but also highlighted challenges in incorporating PROs into care decisions, particularly without incentives.41,42
Our study highlights the need for additional PCC functions within the EHR such as event driven tracking so that clinicians can view progress toward goals. This demonstrates a challenge of incorporating PCC tasks into the EHR—the complexity of recording and tracking information that is crucial for personalized care. New ways to integrate with patient portals to incorporate contextual information and PGD into care may be necessary to realize the potential of PCC in clinical care. Our findings suggest that summarization and display of contextual information and PGD could support PCC.
The importance of regulation to support PCC documentation is highlighted by the near universal availability of end of life preference capacity in the EHR systems surveyed.42 For prioritization of PCC to support the evolution of the EHR policies and incentives related to other data types may be needed. Ultimately, the gaps between the available EHR capacity and seamlessly using these PCC functions at the point of care will need to be closed to promote PCC as a critical imperative.
Limitations and strengths
This is a small exploratory study of technical representatives and clinical users from 6 EHR systems. Although the clinicians queried are long-term users, their usefulness ratings are not representative of all users working with the chosen EHRs. Technical representatives may not have been aware of all future development plans. Because we were focused on the process of PCC from the perspective of interaction with the EHR, we did not include patients in this study. Assessing patient perspectives will be important in future work. We did not include functions specifically related to social determinants of health.13 This is one of the first studies to examine EHR function and PCC across systems using a mixed-methods approach. Implementing EHR functions that support PCC may enable healthcare systems to more precisely understand the impact of PCC processes on health.
CONCLUSIONS
Institutions are prioritizing PCC in varied ways. Increased documentation transparency (eg, open notes) and patient advisory councils have been widely adopted to increase respectful care.43 As these efforts mature, consensus around PCC will need to coalesce and technology support will need to increase, requiring designs that support such PCC principles as optimized communication, the incorporation of patient goals, and allow clinicians to prioritize PCC.37
AUTHOR CONTRIBUTIONS
All authors contributed substantially to the conception or design of the work or to the acquisition and analyses of data. All authors drafted or revised the manuscript critically for important intellectual content. All authors issued final approval of the version to be published. All authors are accountable for aspects of the work including accuracy and integrity.
ACKNOWLEDGEMENTS
The authors wish to acknowledge Carrie Edlund for her edit of the manuscript.
DISCLAIMER
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Veterans Health Administration.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1.Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001. [PubMed] [Google Scholar]
- 2. Greene J, Hibbard JH. Why does patient activation matter? An examination of the relationships between patient activation and health-related outcomes. J Gen Intern Med 2012; 27 (5): 520–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Stewart M, Brown JB, Donner A, et al. The impact of patient-centered care on outcomes. J Fam Pract 2000; 49 (9): 796–804. [PubMed] [Google Scholar]
- 4. Steichen O, Gregg W; Section Editors for the IMIA Yearbook Section on Patient-centered Care Coordination. Health information technology coordination to support patient-centered care coordination. Yearb Med Inform 2015; 24 (1): 34–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Demiris G, Kneale L. Informatics systems and tools to facilitate patient-centered care coordination. Yearb Med Inform 2015; 24 (1): 15–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Tinetti ME, Naik AD, Dodson JA. Moving from disease-centered to patient goals-directed care for patients with multiple chronic conditions: patient value-based care. JAMA Cardiol 2016; 1 (1): 9–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Institute for Healthcare Improvement. Age-Friendly Health Systems: Guide to Using the 4Ms in the Care of Older Adults Boston, MA: Institute for Healthcare Improvement; 2019. [Google Scholar]
- 8. Krejci LP, Carter K, Gaudet T. Whole health: the vision and implementation of personalized, proactive, patient-driven health care for veterans. Med Care 2014; 52(12 Suppl 5): S5–8. [DOI] [PubMed] [Google Scholar]
- 9. Woods S, Evans N, Frisbee K. Integrating patient voices into health information for self-care and patient-clinician partnerships: veterans affairs design recommendations for patient-generated data applications. J Am Med Inform Assoc 2016; 23 (3): 491–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Holt JM, Cusatis R, Asan O, et al. Incorporating patient-generated contextual data into care: clinician perspectives using the consolidated framework for implementation science. Healthc (Amst) 2020; 8 (1): 100369. [DOI] [PubMed] [Google Scholar]
- 11. Cusatis R, Holt JM, Williams J, et al. The impact of patient-generated contextual data on communication in clinical practice: a qualitative assessment of patient and clinician perspectives. Patient Educ Couns 2020; 103 (4): 734–40. [DOI] [PubMed] [Google Scholar]
- 12. Wang J, Wongvibulsin S, Henry K, Fujita S. Quantifying and visualizing medication adherence in patients following acute myocardial infarction. AMIA Annu Symp Proc 2017; 2017: 2299–303. [PMC free article] [PubMed] [Google Scholar]
- 13. Deferio JJ, Breitinger S, Khullar D, Sheth A, Pathak J. Social determinants of health in mental health care and research: a case for greater inclusion. J Am Med Inform Assoc 2019; 26 (8–9): 895–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Estabrooks PA, Boyle M, Emmons KM, et al. Harmonized patient-reported data elements in the electronic health record: supporting meaningful use by primary care action on health behaviors and key psychosocial factors. J Am Med Inform Assoc 2012; 19 (4): 575–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Weiner SJ, Schwartz A, Weaver F, et al. Contextual errors and failures in individualizing patient care: a multicenter study. Ann Intern Med 2010; 153 (2): 69–75. [DOI] [PubMed] [Google Scholar]
- 16. Glasgow RE, Kaplan RM, Ockene JK, Fisher EB, Emmons KM. Patient-reported measures of psychosocial issues and health behavior should be added to electronic health records. Health Aff (Millwood) 2012; 31 (3): 497–504. [DOI] [PubMed] [Google Scholar]
- 17. O’Malley AS, Draper K, Gourevitch R, Cross DA, Scholle SH. Electronic health records and support for primary care teamwork. J Am Med Inform Assoc 2015; 22 (2): 426–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kuo AM, Thavalathil B, Elwyn G, Nemeth Z, Dang S. The promise of electronic health records to promote shared decision making: a narrative review and a look ahead. Med Decis Making 2018; 38 (8): 1040–5. [DOI] [PubMed] [Google Scholar]
- 19. Lenert L, Dunlea R, Del Fiol G, Hall LK. A model to support shared decision making in electronic health records systems. Med Decis Making 2014; 34 (8): 987–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Fossa AJ, Bell SK, DesRoches C. OpenNotes and shared decision making: a growing practice in clinical transparency and how it can support patient-centered care. J Am Med Inform Assoc 2018; 25 (9): 1153–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Joukes E, Abu-Hanna A, Cornet R, de Keizer NF. Time spent on dedicated patient care and documentation tasks before and after the introduction of a structured and standardized electronic health record. Appl Clin Inform 2018; 9 (1): 46–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lown BA, Rodriguez D. Commentary: lost in translation? How electronic health records structure communication, relationships, and meaning. Acad Med 2012; 87 (4): 392–4. [DOI] [PubMed] [Google Scholar]
- 23. Murphy DR, Satterly T, Giardina TD, Sittig DF, Singh H. Practicing clinicians' recommendations to reduce burden from the electronic health record inbox: a mixed-methods study. J Gen Intern Med 2019; 34 (9): 1825–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Cohen GR, Friedman CP, Ryan AM, Richardson CR, Adler-Milstein J. Variation in physicians' electronic health record documentation and potential patient harm from that variation. J Gen Intern Med 2019; 34 (11): 2355–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Office of the National Coordinator for Health Information Technology. Conceptualizing a Data Infrastructure for the Capture, Use, and Sharing of Patient-Generated Health Data in Care Delivery and Research through 2024: White Paper. Washington, DC: Office of the National Coordinator for Information Technology; 2018.
- 26. Glasgow RE, Kwan BM, Matlock DD. Realizing the full potential of precision health: the need to include patient-reported health behavior, mental health, social determinants, and patient preferences data. J Clin Trans Sci 2018; 2 (3): 183–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Street RL, Liu L, Farber NJ, et al. Provider interaction with the electronic health record: the effects on patient-centered communication in medical encounters. Patient Educ Couns 2014; 96 (3): 315–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Zulman DM, Haverfield MC, Shaw JG, et al. Practices to foster physician presence and connection with patients in the clinical encounter. JAMA 2020; 323 (1): 70–81. [DOI] [PubMed] [Google Scholar]
- 29. Peckham C. Medscape EHR Report 2016: Physicians Rate Top EHRs New York, NY: Medscape; 2016.
- 30.Qualtrics. Qualtrics Software. 2019 ed. Provo, UT; 2019.
- 31.Department of Veterans Affairs Health Services Research and Development. Centralized Transcription Service Program. https://www.hsrd.research.va.gov/centers/resource_centers.cfm#ctsp Accessed September 6, 2019.
- 32. Patton MQ. Qualitative Research & Evaluation Methods. 3rd ed Thousand Oaks, CA: Sage Publications, Inc.; 2002. [Google Scholar]
- 33. Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology 2006; 3 (2): 77–101. [Google Scholar]
- 34.ATLAS. ATLAS.ti. 2019. Qualitative Data Analysis Software.
- 35. Altin SV, Finke I, Kautz-Freimuth S, Stock S. The evolution of health literacy assessment tools: a systematic review. BMC Public Health 2014; 14 (1): 1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the Patient Activation Measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv Res 2004; 39 (4p1): 1005–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Sulmasy LS, Bledsoe TA; for the ACP Ethics, Professionalism and Human Rights Committee. American College of Physicians Ethics Manual: Seventh Edition. Ann Intern Med 2019; 170 (2_Suppl): S1–32. [DOI] [PubMed] [Google Scholar]
- 38. Knight SJ. Bridging the gap at the center of patient centeredness: individual patient preferences in health care decision making. JAMA Intern Med 2013; 173 (5): 369–70. [DOI] [PubMed] [Google Scholar]
- 39. Pignone MP, Howard K, Brenner AT, et al. Comparing 3 techniques for eliciting patient values for decision making about prostate-specific antigen screening: a randomized controlled trial. JAMA Intern Med 2013; 173 (5): 362–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Sudore RL, Schillinger D, Knight SJ, Fried TR. Uncertainty about advance care planning treatment preferences among diverse older adults. J Health Commun 2010; 15 (Suppl 2): 159–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Zhang R, Burgess ER, Reddy MC, et al. Provider perspectives on the integration of patient-reported outcomes in an electronic health record. JAMIA Open 2019; 2 (1): 73–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Turley M, Wang S, Meng D, Kanter MH, Garrido T. An information model for automated assessment of concordance between advance care preferences and care delivered near the end of life. J Am Med Inform Assoc 2016; 23 (e1): e118–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Litman K. Patient Centered Care Bethesda, MD: Insitute for Patient- and Family-Centered Care; 2017.