Meningeal melanocytoma is a rare primary pigmented lesion that arises from the central nervous system (CNS). It was first described by Limas and Tio in 1972 as a primary melanocytic tumor of the CNS with a prolonged clinical course and benign histological features1). It was previously reported to originate from the leptomeningeal melanocytes and usually presents as an intradural extramedullary mass. We herein report a case of meningeal melanocytoma arising at the epidural region.
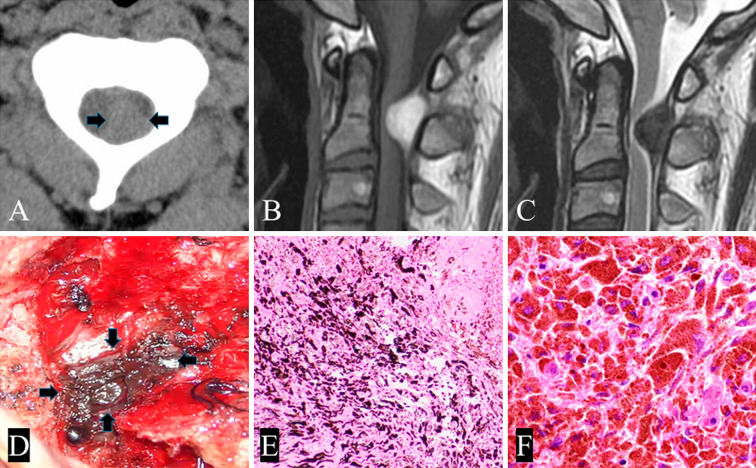
A 27-year-old previously healthy man presented with a 2-year history of increasing posterior neck pain. No neurological abnormalities were observed. Examinations of the skin and the fundus of the eye did not reveal any melanotic lesions. Computed tomography demonstrated a well-defined mass on the left side of the spinal canal at the C1C2 level (Fig. 1A). Cervical spine magnetic resonance imaging (MRI) revealed an extradural mass that was hyperintense on T1-weighted imaging (T1WI) and hypointense on T2-weighted imaging (T2WI), and the spinal cord was displaced and compressed by the epidural mass (Fig. 1B, C). Tumor resection was planned for a definitive diagnosis.
Figure 1.
A) Computed tomography scans showing a mass lesion at the C2 level. B) Hyperintense lesion on T1-weighted imaging. C) Hypointense lesion on T2-weighted imaging. D) Intraoperative photograph showing a blackish tumor. E) Epithelioid and spindle-shaped tumor as cells arranged in whorls and nests with black pigmentation (×100). Hematoxylin and Eosin (H & E) staining of the resected meningeal melanocytoma. F) Melanin-containing macrophages (×400). H & E staining.
A gross examination revealed a black, discolored mass on the dura mater (Fig. 1D). Near-total excision of the tumor, including the tumor membrane, was performed, and light-black spots were found on the dura mater. A pathological examination showed tumor cells with slightly enlarged nuclei containing melanin granules. The mass was judged to be a melanocyte tumor on immunostaining (Fig. 1E, F). Because there were no malignant findings, the tumor was diagnosed as benign.
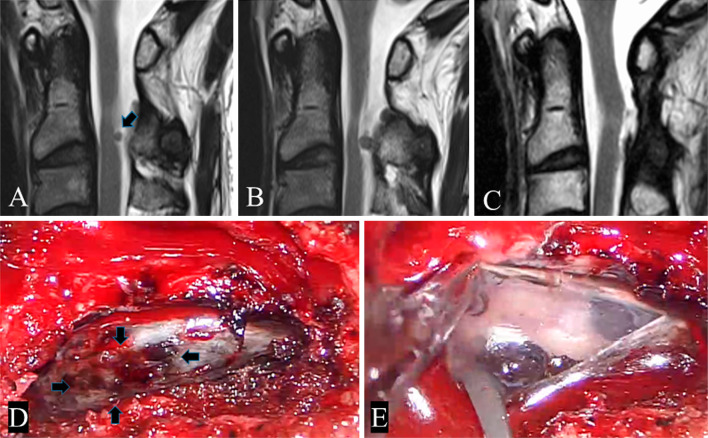
One year after the operation, follow-up MRI revealed a tumor arising in the intradural extramedullary lesion (Fig. 2A). One and a half years later, the tumor had expanded and compressed the spinal cord (Fig. 2B), so we considered a second operation for the benign tumor. At the second surgery, hard, black pigmentation was observed on the dural surface (Fig. 2D). After the dura was dissected, a black mass was found beneath the dura and attached to the dorsal aspect of the arachnoid (Fig. 2E). The tumor had a well-defined margin. The tumor was resected along with the invaded dura matter. At the dural defect site, dural reconstruction was performed using artificial dura mater. A pathological examination of the tumor and the dura mater revealed the same findings as the initial surgery. Because of the possibility of recurrence, postoperative radiation therapy was performed. There were no neurological abnormalities. Two years have passed since the operation, with no recurrence noted on MRI (Fig. 2C).
Figure 2.
A) Hypointense lesion on T2-weighted imaging. B) The tumor had expanded further after 1.5 years. C) Postoperative magnetic resonance imaging showing gross total resection of the lesion. D) Intraoperative photograph showing the pigmented lesion on the dura. E) The intradural main lesion was exposed.
Meningeal melanocytoma in the spinal region has rarely been reported. The MRI findings include a high signal intensity on T1WI and low intensity on T2WI2). Hemosiderin deposits can be seen on T2WI in the form of a low-intensity rim. In many cases, meningeal melanocytoma is reported intradurally, but it developed in the epidural area in the present case. Despite a thorough search, no references describing a tumor originating from the epidural area were found. We suspect that the tumor arising from the dura mater spread epidurally and intradurally initially, with the main tumor ultimately progressing to an extradural location. Meningeal melanocytomas are biologically benign and can be cured by complete surgical resection, although local recurrence has been reported despite gross total resection3). Rades et al. said that if the tumor can only be subtotally resected, postoperative radiotherapy should be administered4). In our case, the patient's course has progressed over 2 years without recurrence following radiotherapy (total dose 45 Gy). However, careful follow-up is required, as the possibility of tumor recurrence remains.
Conflicts of Interest: The authors declare that there are no relevant conflicts of interest.
Ethical Approval: There was no invasive research, and magnetic resonance imaging was performed for follow-up purposes. The anonymity of the patient is protected.
Informed Consent: The patient and his family were informed that the data from his case would be submitted for publication, and all gave their consent.
References
- 1.Limas C, Tio FO. Meningeal melanocytoma (“melanotic meningioma”). Its melanotic orgin as revealed by electron microscopy. Cancer. 1972;30:1286-94. [DOI] [PubMed] [Google Scholar]
- 2.EJ Czarnecki, R Silbergleit, JA Gutierrez. MR of Spinal Meningeal Melanocytoma. American Society of Neuroragiology. 1997;18:180-2. [PMC free article] [PubMed] [Google Scholar]
- 3.Yang C, Fang J, Li G. Spinal meningeal melanocytomas: clinical manifestations, radiological and pathological characteristics, and surgical outcomes. J Neurooncol. 2016;127:279-86. [DOI] [PubMed] [Google Scholar]
- 4.D Rades 1, F Heidenreich, M Tatagiba. Therapeutic options for meningeal melanocytoma. J Neurosurg (Spine 2). 2001;95:225-31. [DOI] [PubMed] [Google Scholar]