Abstract
Background
This exploratory study investigated the time-course of lectin complement pathway (LCP) initiators in cerebrospinal fluid (CSF) and plasma in patients with subarachnoid hemorrhage (SAH), as well as their relationship to delayed cerebral ischemia (DCI) and functional outcome.
Methods
Concentrations of ficolin-1, ficolin-2, ficolin-3, and mannose-binding lectin (MBL) were analyzed in CSF and plasma from patients with SAH. Samples were collected daily from admission until day 9 (CSF; N_PATIENTS = 63, n_SAMPLES = 399) and day 8 (plasma; N_PATIENTS = 50, n_SAMPLES = 358), respectively. Twelve neurologically healthy patients undergoing spinal anesthesia and 12 healthy blood donors served as controls. The development of DCI during hospitalization and functional outcome at 3 months (modified Rankin Scale) were registered for patients.
Results
On admission, CSF levels of all LCP initiators were increased in SAH patients compared with healthy controls. Levels declined gradually over days in patients; however, a biphasic course was observed for ficolin-1. Increased CSF levels of all LCP initiators were associated with a poor functional outcome in univariate analyses. This relationship persisted for ficolin-1 and MBL in multivariate analysis after adjustments for confounders (age, sex, clinical severity, distribution and amount of blood on CT-imaging) and multiple testing (1.87 ng/mL higher in average, 95% CI, 1.17 to 2.99 and 1.69 ng/mL higher in average, 95% CI, 1.09 to 2.63, respectively). In patients who developed DCI compared with those without DCI, CSF levels of ficolin-1 and MBL tended to increase slightly more over time (p_interaction = 0.021 and 0.033, respectively); however, no association was found after adjustments for confounders and multiple testing (p-adj_interaction = 0.086 and 0.098, respectively). Plasma ficolin-1 and ficolin-3 were lower in SAH patients compared with healthy controls on all days. DCI and functional outcome were not associated with LCP initiator levels in plasma.
Conclusion
Patients with SAH displayed elevated CSF levels of ficolin-1, ficolin-2, ficolin-3, and MBL. Increased CSF levels of ficolin-1 and MBL were associated with a poor functional outcome.
Trial registration
This study was a retrospective analysis of samples, which had been prospectively sampled and stored in a biobank. Registered at clinicaltrials.gov (NCT01791257, February 13, 2013, and NCT02320539, December 19, 2014).
Supplementary Information
The online version contains supplementary material available at 10.1186/s12974-020-01979-y.
Keywords: Ficolin, Lectin complement pathway, Subarachnoid hemorrhage, Delayed cerebral ischemia, Functional outcome
Background
Aneurismal subarachnoid hemorrhage (SAH) is a life-threatening condition accounting for ~5% of all stroke cases. Despite low annual incidence rates [1], the total loss of productive life years in the SAH patients is similar to more common types of stroke [2], due to a high mortality rate [1] and a low chance that survivors return to the labor market [2, 3].
Delayed cerebral ischemia (DCI) is a main contributor to a poor functional outcome in patients surviving SAH [4, 5]. The pathogenesis and pathophysiology of DCI are still incompletely understood. Previously, DCI has been attributed to cerebral vasospasm [6], but recent research suggests a multifactorial origin, including neuroinflammation as a central causal factor [7, 8].
The complement system is part of the innate immune system, which comprises a first-line defense against invading microorganisms, enabling clearance of dying cells, and amplifying adaptive and inflammatory immune responses upon stimulation [9]. Three pathways activate the complement system, i.e., the classical, the alternative, and the lectin complement pathway (LCP) [10]. The initiators of the LCP, comprising ficolin-1, ficolin-2, and ficolin-3, mannose-binding lectin (MBL), and collectin-10 and collectin-11, induce down-streams activation upon binding to specific carbohydrate structures on injured cells and microorganisms [11, 12].
Recent studies have reported an association between LCP initiators in plasma and functional outcome in ischemic stroke patients [13–16]. LCP initiators have previously been investigated in SAH patients but with conflicting results [17–20].
We aimed to investigate the time-course of LCP initiator levels in CSF and plasma after SAH and to describe their potential relationship to DCI and functional outcome.
Methods
Standard protocol approvals, registrations, and patient consents
This study was a retrospective analysis of samples from CSF and plasma, which had been prospectively sampled and stored in a biobank, and some of which were included in a prospective observational cohort study of microRNAs [21]. Protocols were approved by the Danish Scientific Ethics Committee of the Capital Region (H-3-2013-009 and H-3-2014-073) including amendments for the present study (H-3-2013-009 and H-6-2014-073) and the Danish Data Protection Agency (I-suite # 02116 and 03279) and registered at clinicaltrials.gov (NCT01791257 and NCT02320539). Informed consent was obtained from the next of kin, the general practitioner and, when possible, from the patient.
This manuscript adheres to requirements set by the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) statement.
Study participants
Patients with spontaneous aneurysmal subarachnoid hemorrhage (SAH) as diagnosed by computed tomography (CT) and CT angiography who were admitted to the Neurointensive Care Unit at Rigshospitalet (Copenhagen, Denmark) were assessed for eligibility. Inclusion criteria were >18 years of age. Exclusion criteria were more than 24 h uncertainty of the time of ictus, as well as the inability to speak and understand Danish.
Neurologically healthy patients >18 years of age with an American Society of Anesthesiologists physical status classification ≤2, who had spinal anesthesia before lower limb orthopedic surgery at Frederiksberg Hospital, were included and served as the control group for the CSF analyses.
Neurologically healthy blood donors >18 years of age were included from the National Donor Registry (Copenhagen, Denmark) and served as the control group for the plasma analyses.
Clinical definitions and outcome measures
The clinical severity of SAH was assessed using the World Federation of Neurosurgical Societies (WFNS) grading scale, which categorizes patients from 1 to 5; 1 indicating the lowest and 5 indicating the highest disease severity [22]. The extent of intracranial hemorrhage on admission CT was registered by the Fisher grading scale, which rates the severity of SAH from 1 to 4 based on the distribution and amount of blood on CT scans of the head [23].
Clinical deterioration due to DCI was defined according to Vergouwen et al. as the development of a new neurological deficit or a decrease of at least 2 points in GCS, persisting for at least 1 h, and which was not explained by any other potential cause [5]. Two clinicians independently reviewed all patient data obtained in the medical journal within 3 weeks from ictus and allocated the patients to five subgroups regarding the diagnostic certainty of DCI (definite DCI, probably DCI, possible DCI, probably not DCI, and definitely not DCI). To increase the chance of detecting a difference between groups, only patients from the groups, ‘definite DCI’ and ‘definitely not DCI’ were compared.
Functional outcome at 3-months follow-up was based on the modified ranking scale (mRS) [24], which measures the degree of disability (i.e., dependence in daily activities) after a stroke ranging from a mRS score of 0 (no disability symptoms) to 6 (death). This outcome was subsequently dichotomized into good functional outcome, defined as independence or minor disability (mRS 0–2), and poor functional outcome, defined as being dependent or dead (mRS 3–6).
CSF samples
From patients with an external ventricular drain (EVD), CSF was collected immediately after placement with a sterile procedure, and once daily using an aseptic procedure the following 7 days. From neurologically healthy patients, one CSF sample was collected using a sterile procedure immediately before spinal anesthesia for orthopedic lower limb surgery. CSF samples were immediately put on ice and spun within 15 min at 500 g for 10 min, and the supernatant was stored at −80 °C.
Plasma samples
Blood was collected from an arterial catheter from SAH patients upon admission and once daily the following 7 days. If no arterial catheter was present, sampling was done from a central venous catheter. From healthy volunteers, blood was sampled once during a blood donation. Blood samples were immediately put on ice and spun within 15 min at 2000 g for 10 min, and the plasma samples were stored at −80 °C. Both plasma and CSF samples were collected at the same time of the morning each day.
Protein quantification
The concentration of LCP initiators (ficolin-1, ficolin-2, ficolin-3, and MBL) in CSF and plasma was determined using sandwich enzyme-linked immunosorbent assay (ELISA) developed in the Laboratory of Molecular Medicine, Rigshospitalet, according to previously described procedures [25–28]. Briefly, microtiter plates (Nunc Immuno Plates, F384 Maxisorp) were coated with one of the following monoclonal antibodies against ficolin-1 (HP9039; Hycult Biotech, Uden, Nederlands) and in-house produced biotinylated antibodies against ficolin-2 (anti-ficolin 2 ficolin-219), ficolin-3 (anti-ficolin 3 ficolin-334), and MBL (anti-MBL Hyb-131-1) and diluted in phosphate-buffered saline +0.05% Tween-20 (PBS-T), and incubated overnight. Samples were diluted 1:200 and run in triplicates and parallel to a standard pool with a known concentration. Subsequently, polyclonal donkey anti-rapid antibody (ficolin-1) or streptavidin-horseradish peroxidase conjugate (ficolin-2, ficolin-3, and MBL) was applied and plates were developed using o-phenylenediamine dihydrochloride substrate and stopped by adding H2SO4. Assays were optimized for automated analysis in a 384-well format using the Biomek FX platform (Beckman Coulter, Fullerton, California, USA) for pipetting followed by a DTX880 Multimode detector system where assays were analyzed at 490 nm.
The lower detection limit was as follows in plasma: 5 ng/ml for ficolin-1, 0.005 μg/ml (5 ng/ml) for ficolin-2, 1 ng/ml for ficolin-3, and 20 ng/ml for MBL; it was 0.4 ng/ml in CSF for all four biomarkers. We obtained the following coefficients of variation as calculated from the raw triplicate measurements: Ficolin-1: CSF 9.3%, plasma 7.1%; ficolin-2: CSF 20.2%, plasma 10.6%; ficolin-3: CSF 18.1%, plasma 9.6%, MBL: CSF 9.2%, plasma 7.7%.
Statistical analysis
Plasma and CSF levels of LCP initiators on admission and specific days after the initial bleeding in SAH patients were compared with those of neurologically healthy individuals using Wilcoxon’s rank-sum test. Within SAH patients, levels were compared between the groups, ‘definitely DCI’ vs ‘definitely not DCI’ and ‘poor functional outcome’ vs ‘good functional outcome’, using a linear mixed model with subgroup (DCI or functional outcome) and day as fixed effects, and patients as a random effect. Crude comparison was done without including any further covariates (univariate analyses), whereas adjusted analyses included sex, age, and WFNS and Fisher scores as covariates (multivariate analyses). The linear mixed model was applied twice: (1) Assuming no interaction (i.e., assuming that LCP initiator levels did not develop differently over time between groups) thereby evaluating the overall difference in concentrations (p), and (2) including the group*day interaction to explore potentially different time developments between groups (p_interaction). Goodness of fit was assessed by residual plots. Due to substantial skewness, CSF levels were log-transformed prior to analysis and results were expressed accordingly (i.e., as percentwise differences in medians). P values were corrected for multiple testing using the Benjamini-Hochberg procedure.
All statistical analysis was performed using Statistical Analysis System v.9.4 (SAS Institute Inc., Cary, NC).
Results
In total, 82 patients were recruited for this study and included in the CSF study alone (N = 32), the plasma study alone (N = 19), or both (N = 31) (Table 1). The 63 SAH patients in the CSF study all underwent placement of an EVD for clinical reasons and had a total of 402 CSF samples collected (Sup. Fig. 1), of which 399 were used for final analysis. Of these 63 patients, 39 (62%) were in a poor condition on admission (WFNS grade 4 or 5) and 13 (21%) had a Fisher grade of 4 (i.e., intraventricular hemorrhage or intracerebral hemorrhage). Thirty-six were assessable for development of DCI; of these, 18 were categorized as ‘definite’ and 18 as ‘definitely not DCI’. Clinical deterioration due to DCI typically occurred between day 6 and day 7 (mean = 6.5 days, SD = 1.5). At the 3-month follow-up, all 63 SAH patients were assessable for a functional outcome, of whom 29 (46%) had a poor (mRS 3–6) and 34 (54%) had a good functional outcome (mRS 0–2), respectively. Twelve CSF samples were collected from 12 neurologically healthy patients.
Table 1.
Demographic data of the SAH patients and related control groups
| CSF control group (n = 12) |
CSF (n = 63) |
Plasma Control Group (n = 12) |
Plasma (n = 50) |
|
|---|---|---|---|---|
| Age, mean years (SD) | 69 (± 9) | 59 (±11) | 55 (±7) | 61 (± 11) |
| Sex, n (%) | ||||
| Men | 8 (66.7) | 14 (22.2) | 4 (33.3) | 5 (10) |
| Women | 4 (33.3) | 49 (77.8) | 8 (66,7) | 45 (90) |
| WFNS, n (%) | ||||
| 1 | 8 (12.7) | 17 (34.0) | ||
| 2 | 12 (19.0) | 8 (16.0) | ||
| 3 | 4 (6.3) | 5 (10.0) | ||
| 4 | 21 (33.3) | 10 (20.0) | ||
| 5 | 18 (28.6) | 10 (20.0) | ||
| Fisher score, n (%) | ||||
| 1 | 0 (0) | 0 (0) | ||
| 2 | 1 (1.6) | 4 (8.0) | ||
| 3 | 48 (77.4) | 37 (74.0) | ||
| 4 | 13 (21.0) | 9 (18.0) | ||
| Definite DCI, n (%) | 18 (28.6) | 13 (26.0) | ||
| Definitely not DCI, n (%) | 18 (28.6) | 20 (40.0) | ||
| Days from ictus to DCI, mean (SD) | 6.5 (±1.5) | 7.2 (±2.2) | ||
| mRS, n (%) | ||||
| 0–2 | 34 (54.0) | 35 (70.0) | ||
| 3–6 (poor functional outcome) | 29 (46.0) | 15 (30.0) | ||
| Aneurysm location, n (%) | ||||
| Anterior cerebral artery | 25 (39.7) | 16 (32.0) | ||
| Middle cerebral artery | 13 (20.6) | 10 (20.0) | ||
| Posterior cerebral artery | 16 (25.4) | 18 (36.0 | ||
| Internal carotid artery | 9 (14.3) | 6 (12.0) | ||
| Technique for securing aneurysm, n (%) | ||||
| Coil | 42 (66.7) | 35 (71.4 | ||
| Clip | 21 (33.3) | 14 (28.6) | ||
| Vasospasm, n (%) | ||||
| Yes | 28 (73.7) | 17 (70.8) | ||
| No | 10 (26.3) | 7 (29.2) | ||
CSF cerebrospinal fluid, WFNS World Federation of Neurological Surgeons scale, EBI early brain injury, DCI delayed cerebral ischemia, mRS Modified ranking scale
From the 50 patients in the plasma study, 359 plasma samples were collected (Sup. Fig. 2), of which 358 were used for final analysis. Of these 50 SAH patients, 20 (40%) were in a clinically poor condition (WFNS 4–5) on admission and 9 (18%) had a Fisher grade of 4 (i.e., intraventricular hemorrhage or intracerebral hemorrhage). Thirty-three SAH patients were assessable for the development of DCI, of which 13 patients were categorized as ‘definite’ and 20 patients as ‘definitely not’ DCI. On average, clinical deterioration due to DCI occurred on day 7 (mean = 7.2, SD = 2.2). At the 3-month follow-up, all 50 SAH patients were assessable for the functional outcome, of whom 15 (30%) had a poor and 35 (70%) had a good functional outcome, respectively. Twelve plasma samples were collected from 12 healthy volunteers.
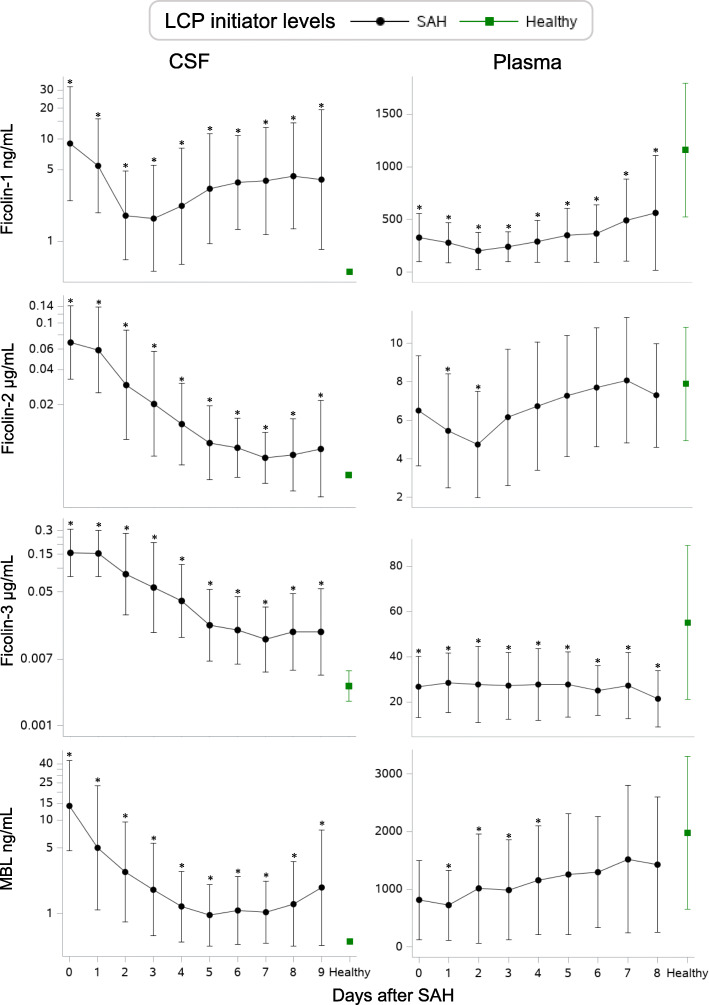
LCP initiator concentrations in SAH patients vs healthy controls (Fig. 1)
Fig. 1.
Daily levels of LCP initiators. Daily levels of ficolin-1, ficolin-2, ficolin-3, and MBL in CSF (left) and plasma (right) in patients with SAH (black) and neurologically healthy patients (green). The daily levels are presented as medians in CSF and as means in plasma. Error bars show ±1 SD. Asterisks (*) indicate significance on specific days after SAH compared to control patients (p < 0.05) using Wilcoxon’s rank-sum test. Each LCP initiator graph is based on a total number of 399 CSF samples from 63 SAH patients (mean number of samples per patient, 7; range, 6–8), 358 plasma samples from 50 SAH patients (mean number of samples per patient, 7; range, 6–8), and 12 control samples from 12 neurologically healthy patients. MBL: Mannose-binding lectin, CSF: Cerebrospinal fluid, SAH: Subarachnoid hemorrhage
Ficolin-1, ficolin-2, and MBL were not detected in CSF from neurologically healthy patients and ficolin-3 concentrations in CSF were low compared with SAH patients. Median levels of ficolin-1, ficolin-2, and ficolin-3, and MBL were elevated in CSF on all days after SAH compared with neurologically healthy patients; concentrations were high on admission followed by a gradual decline towards normal levels on day 7 to 9. In contrast, ficolin-1 showed a biphasic slope with a second peak between day 3 and 9.
Average plasma concentrations of all LCP initiators in SAH patients were lower than or comparable to the levels of neurologically healthy individuals. Ficolin-1 and ficolin-3 were lower on all days after SAH, whereas ficolin-2 and MBL were lower only on days 1–2 and 1–4, respectively. Ficolin-2 showed a biphasic slope with a second peak from day 2. Ficolin-1 showed a minor decline between day 0 and day 2 followed by a gradual day-by-day increase. MBL showed a gradual increase over time, reaching normal levels from day 5. Ficolin-3 remained low on all days.
Daily levels of the LCP initiators in SAH and neurologically healthy patients are shown in Fig. 1.
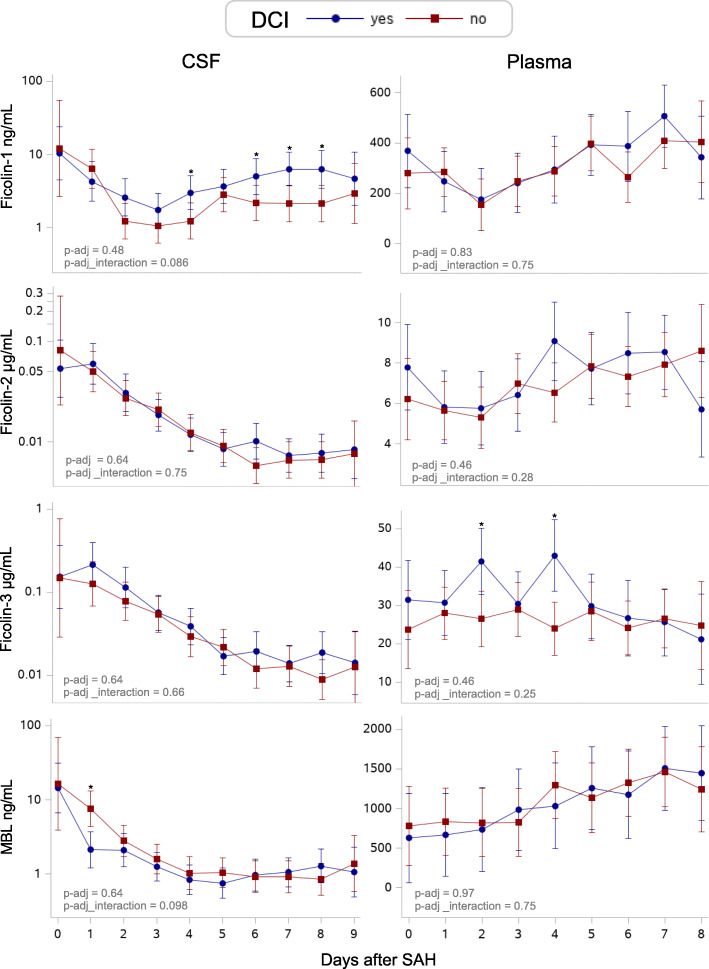
DCI — longitudinal analysis (Fig. 2 and Table 2)
Fig. 2.
Predicted daily LCP initiator levels in SAH patients with or without the development of DCI. Predicted daily levels of ficolin-1, ficolin-2, ficolin-3, and MBL in CSF (left) and in plasma (right) in patients with (blue) or without (red) the development of DCI. The predicted daily levels are presented as medians in CSF and as means in plasma. Error bars show 95% confidence intervals. P values shown in the bottom left of each graph are adjusted for confounders (age, sex, WFNS, and Fisher score) and multiple testing (Benjamini-Hochberg procedure) and represent the overall difference in concentration between groups (p-adj) and overall different development over time (p-adj_interaction) for each LCP initiator. Asterisks indicate (*) significant levels on specific days <0.05. Each LCP initiator graph is based on a total number of 241 CSF samples from 36 SAH patients (mean number of samples per patient, 7; range, 6–8) and 233 plasma samples from 33 SAH patients (mean number of samples per patient, 7; range, 6–8). LCP: Lectin complement pathway, MBL: Mannose-binding lectin, CSF: Cerebrospinal fluid, CT: Computed tomography, DCI: Delayed cerebral ischemia, SAH: Subarachnoid hemorrhage
Table 2.
Overall difference in CSF levels of each LCP initiator in SAH subgroups (DCI and functional outcome)
| Univariate analyses | Multivariate analyses (age, sex, WFNS, Fisher) |
|||||
|---|---|---|---|---|---|---|
| CSF-levels | Estimate (95% CI) |
p | p-adj | Estimate (95% CI) |
p | p-adj |
| DCI | ||||||
|
Ficolin-1 (ng/mL) |
1.87 (0.99, 3.53) | 0.052 | 0.20 | 1.72 (0.85, 3.48) | 0.12 | 0.48 |
|
Ficolin-2 (μg/mL) |
1.08 (0.73, 1.60) | 0.69 | 0.69 | 1.11 (0.70, 1.78) | 0.64 | 0.64 |
|
Ficolin-3 (μg/mL) |
1.26 (0.75, 2.13) | 0.37 | 0.61 | 1.20 (0.65, 2.23) | 0.55 | 0.64 |
|
MBL (ng/mL) |
1.21 (0.49, 1.39) | 0.46 | 0.61 | 0.78 (0.42, 1.47) | 0.43 | 0.64 |
| Functional outcome | ||||||
|
Ficolin-1 (ng/mL) |
1.85 (1.12, 3.05) | 0.017* | 0.022* | 1.87 (1.17, 2.99) | 0.010* | 0.040* |
|
Ficolin-2 (μg/mL) |
1.47 (1.08, 2.01) | 0.015* | 0.022* | 1.33 (0.96, 1,83) | 0.079 | 0.10 |
|
Ficolin-3 (μg/mL) |
1.54 (1.01, 2.36) | 0.043* | 0.043* | 1.45 (0.92, 2.27) | 0.10 | 0.10 |
|
MBL (ng/mL) |
1.69 (1.13, 2.52) | 0.012* | 0.022* | 1.69 (1.09, 2.63) | 0.020* | 0.040* |
Estimates represent the relative overall difference in CSF concentration (relative ∆medians) of each LCP initiator in patients with DCI versus without DCI (reference) and in patients with a poor versus good (reference) functional outcome, respectively. Both univariate linear mixed model analyses (left) and multivariate analyses (right) with adjustment for confounders are shown in the table.
P values (p) represent the overall difference in CSF concentrations between groups (assuming no interaction). p-adj represent p values corrected for multiple testing using Benjamini-Hochberg’s procedure. Asterisks indicate significance levels <0.05.
∆: Difference; CI confidence interval, CSF cerebrospinal fluid, Fisher: extent and location of the intracranial hemorrhage, LCP lectin pathway initiators, MBL mannose-binding lectin; WFNS: clinical severity on admission
For the 36 patients in the CSF study who were diagnosed as either ‘definitely DCI’ or ‘definitely not DCI’, 241 CSF samples were available.
In univariate analysis, the CSF level of ficolin-1 seemed elevated in patients with DCI versus patients without DCI (1.87 ng/mL higher in average, 95% confidence interval [CI], 0.99 to 3.53, p = 0.052), although insignificant. However, after adjustment for multiple testing, the association was no longer found (p-adj = 0.20). In multivariate analysis adjusted for sex, age, WFNS, and Fisher score no association was found.
Ficolin-1 and MBL increased slightly more over time in patients with DCI versus without DCI, i.e., a different slope was present (p_interaction = 0.021 and 0.033, respectively; data not shown). Adjusted for confounders (sex, age, WFNS, and Fisher score), the increase over time for ficolin-1 and MBL remained significant, but with further adjustment for multiple testing, the increase over time became non-significant (p-adj_interaction = 0.086 and 0.098, respectively, Fig. 2).
Ficolin-2 and ficolin-3 in CSF did not differ between patients with and without DCI.
For the 33 patients who were diagnosed with either ‘definitely DCI’ or ‘definitely not DCI’, 233 plasma samples were available. Neither overall difference in plasma concentrations (Sup. Table 1) nor overall changes over time was observed for any of the LCP initiators (ficolin-1, ficolin-2, ficolin-3, and MBL) in patients with or without DCI (Fig. 2).
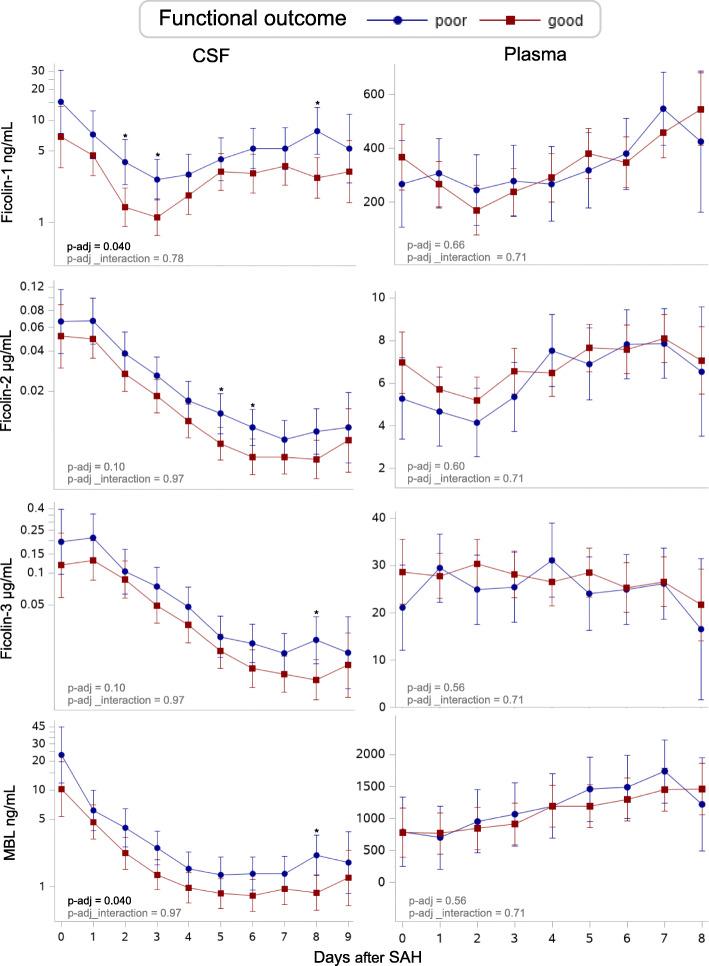
Functional outcome — longitudinal analysis (Fig. 3 and Table 2)
Fig. 3.
Predicted daily levels of LCP initiators in SAH patients with poor versus good functional outcome. Predicted daily levels of ficolin-1, ficolin-2, ficolin-3, and MBL in CSF (left) and in plasma (right) in patients with a poor (blue) and good (red) functional outcome. The predicted daily levels are presented as medians in CSF and as means in plasma. Error bars show 95% confidence intervals. P values shown in the bottom left of each graph are adjusted for confounders (age, sex, WFNS, and Fisher score) and multiple testing (Benjamini-Hochberg procedure) and represent the overall difference in concentration between groups (p-adj) and overall different development over time (p-adj_interaction) for each LCP initiator. Asterisks (*) indicate significant levels on specific days <0.05. Each LCP initiator graph is based on a total number of 399 CSF samples from 63 SAH patients (mean number of samples per patient, 7; range, 6–8) and 358 plasma samples from 50 SAH patients (mean number of samples per patient, 7; range, 6–8). MBL: Mannan-binding lectin, CSF: Cerebrospinal fluid, SAH = subarachnoid hemorrhage
All 399 CSF samples and all 358 plasma samples were entered into these analyses.
In univariate analyses, CSF levels of ficolin-1, ficolin-2, ficolin-3, and MBL were higher in patients with a poor functional outcome compared with those with a good functional outcome. In multivariate analyses adjusting for sex, age, WFNS, and Fisher score as well as for multiple testing, ficolin-1 and MBL levels remained higher in patients with a poor functional outcome (1.87 ng/mL higher in average, 95% CI, 1.17 to 2.99, p = 0.040) and 1.69 ng/mL higher in average, 95% CI, 1.09 to 2.63, p = 0.040).
No change over time was detected between groups, indicating that the slopes were parallel (p_interaction >0.05, data not shown).
In contrast, LCP initiators in plasma did not differ between patients with good and those with poor functional outcomes either overall or by time (Fig. 3 and Sup. Table 1).
Discussion
We investigated the day-by-day changes of LCP initiators in both CSF and plasma after SAH. Our study revealed three major findings. First, CSF concentrations of LCP initiators were increased throughout the first week following SAH, followed by a gradual decline over time. Second, increased CSF levels of all investigated LCP initiators, especially ficolin-1 and MBL, were associated with a poor functional outcome in SAH patients. Third, in univariate analysis, patients with DCI compared with those without DCI, no association was found between DCI and overall LCP initiator levels in CSF. However, ficolin-1 tended to increase slightly more over time in patients with DCI than without (i.e., slopes showing CSF levels increased more over time in the DCI group versus the group without DCI), but the increase was not significant after adjustment for multiple testing (p-adj_interaction = 0.086, Fig. 2).
The present design does not allow us to conclude whether the increased CSF concentration of LCP initiators in the present study is due to local synthesis or simply to a spill-over from the systemic circulation, e.g., due to blood-brain barrier (BBB) dysfunction after SAH. In favor of spill-over from plasma, invasion of complement and inflammatory cells over the disrupted BBB has been proposed as a major contributor to the BBB pathology in other neuroinflammatory central nervous system (CNS) disorders, such as traumatic brain injury, bacterial meningitis, and cerebral malaria [29]. However, this suggestion was based on experimental findings rather than clinical data. Our reported median CSF level of MBL of 15 ng/ml is slightly lower than the median level of approximately 25 ng/ml in patients with pneumococcal meningitis and no MBL deficiency reported in a study evaluating CSF levels of MBL in relation to pneumococcal meningitis, but slightly higher than in such patients with MBL deficiency (<5–15 ng/ml depending on genotype) [30]. Furthermore, another study reported a mean CSF MBL level of 5.11 ng/ml in patients with non-HIV-associated cryptococcal meningitis [31]. To our knowledge, nobody has reported CSF levels of ficolins in pneumococcal meningitis, nor CSF levels of MBL or ficolins in patients with cerebral malaria or traumatic brain injury. In favor of local production of complement proteins, production of initiators and down-stream mediators of the classical and the alternative pathway does occur in the healthy brain [32, 33]. Most LCP initiators (ficolin-2, ficolin-3, and MBL) are primarily produced by hepatocytes in the liver, after which they enter the systemic circulation, forming complexes with mannose-associated serine proteases (MASPs) [34]. Ficolin-1, in contrast, acts as a secretory protein and is mainly produced by the myeloid cell line. Ficolin-1 is found in secretory granules in neutrophils and monocytes, where it can be exocytosed into extracellular environments upon stimulation [35]. We speculate that ficolin-1 is released by immune cells locally within the brain, whereas the remaining LCP initiators enter the intrathecal space from the blood. This hypothesis is supported by the finding that CSF ficolin-1 increased again after an initial decline. Although a concomitant increase in plasma levels could also have facilitated a larger passive influx, the plasma level of ficolin-2 increased in parallel with ficolin-1 but was not associated with an increase in CSF.
One other study has looked at LCP initiator levels in CSF after SAH [17]. The authors reported a tendency towards lower ficolin-1 levels in CSF after 24 h in 18 SAH patients with angiographic vasospasm but did not find any association with the cerebral ischemic lesions. We were not able to directly compare the predicted concentrations in CSF in our study with the previous one because the outcome variables differed (cerebral ischemic lesions versus DCI). However, the previous study found a considerably higher median concentration of ficolin-1 in CSF from patients with cerebral ischemic lesions (51 ng/mL (30–102)) compared with patients with DCI in our study (4 ng/mL (2–8) on day 1). Notably, this could be explained by a different distribution of patients with intraventricular hemorrhage; as many as 84% had intraventricular hemorrhage (i.e., original Fisher scale with grade 4) compared with 21% in the present study, indicating less contamination by blood in our CSF samples. Additionally, the studies used different protein quantification assays.
A study assessing the involvement of the LCP initiators in contused human brain tissue from patients with head trauma found that the LCP initiators were present inside and outside of brain vessels in all contusions examined [36]. Only ficolin-1 was found in normal brain tissue from control patients. In contrast, we were not able to detect ficolin-1 in CSF from neurologically healthy patients. One explanation to this may be that ficolin-1 acts as a secretory protein in the brain, which is only released into the extracellular compartment in response to inflammatory stimulation.
Another study examining brain samples in patients with acute ischemic stroke showed that certain complement proteins, including MBL, were deposited in ischemic lesions in the brain [37]. The authors suggested that increased complement deposition in the brain combined with decreased expression of complement regulators may be a possible mechanism of tissue damage during ischemia. Our findings of increased levels of LCP initiators in CSF associated with SAH and with poor functional outcome appear to support these findings. In line with this, experimental stroke models have reported that complement proteins mediate inflammation after cerebral ischemic injury and that inhibition of complement activation conferred neuronal protection and reduced stroke volume [38–41]. Our findings of increased levels of ficolin-1 and MBL associated with a poor functional outcome may support this notion; however, we have observed an association only and are unable to shed further light on these hypotheses.
Plasma levels of all investigated LCP initiators were lower or comparable in SAH patients compared with healthy individuals, and ficolin-1 and ficolin-3 were lower in both the hyperacute, acute, and the intermediate phase after SAH. Also, circulating LCP initiators were associated neither to DCI nor to functional outcome.
Few research groups have examined the changes of LCP initiators in plasma after SAH, and conflicting results have been reported [14, 17, 18, 20]. As a common denominator, the focus has primarily been on the hyperacute phase of SAH (i.e., hours after ictus). The studies used different approaches (e.g., regarding time from SAH to sampling, definition of DCI, techniques of protein quantification, etc.), which limits the comparability with our study.
This study is the first to provide information about the day-by-day changes of LCP initiators after SAH. The high number of consecutive samples of both CSF and plasma from each patient yielded a higher resolution than previous studies, conferring improved robustness and precision of the natural course of LCP initiators after SAH.
Furthermore, our study complies with the recent reporting recommendations in cellular and molecular SAH studies using recommended methods of sample acquisition, use of collection tubes, biospecimen processing and storage, inclusion of a neurologically healthy control group for both CSF and plasma, as well as using functional outcome and DCI as outcome measures [42]. This way, we hope to contribute to increased homogeneity across studies, which is essential for future biomarker validation to improve risk prediction and optimize treatment. Despite the retrospective study design, patients were thoroughly evaluated for the occurrence of DCI, as well as for their functional outcome 3 months after SAH.
However, this study also has noteworthy limitations. First, we evaluated multiple outcome measures (ficolin-1, ficolin-2, ficolin-3, and MBL) which increase the risk of chance findings. We reduced this risk by correcting for multiple testing.
Due to the post hoc nature of this study, we cannot exclude a potential risk of selection bias as well as a risk of analytical variation due to the chosen method to detect LCP initiators. Furthermore, the retrospective design of the study rendered us unable to measure the actual activity of the LCP system and establish any potential causal relationship with the levels of LCP initiators. However, another study found plasma ficolin-3 and ficolin-3-mediated functional LCP activity to be well correlated [19]. Similarly, a causal relationship between LCP initiators and brain damage is not possible to determine in our study. Experimental studies are needed to address this aspect.
CSF samples were collected from patients treated with an EVD; thus, our CSF findings mainly is related to this selected subgroup of SAH patients. In addition, SAH patients with intraventricular blood (Fisher grade of IV) could conceivably experience variation in the CSF composition depending on positioning and other manipulations affecting cerebrospinal fluid compartments.
All included patients were treated with tranexamic acid (TXA) (an antifibrinolytic) based on the Danish National Guidelines, which might have an impact on complement activity. Many fibrinolytic compounds work as natural C3 and C5 convertases, thus generating C3a and C5a (active anaphylatoxins) [43]. The use of TXA in SAH patients could potentially influence the LCP initiator levels as well as the activity of the complement system.
In our study, we did not control for the presence of intercurrent infection; neither did we measure other markers of inflammation in plasma or CSF. Although SAH is associated with a marked systemic inflammatory response [44, 45], infection, such as pneumonia in mechanically ventilated patients, could also contribute to inflammation and potentially affect the relationship between plasma LCP initiator levels, DCI, and functional outcome. By contrast, the CSF levels of LCP initiators probably represented the true inflammatory response to SAH in and of itself since ventriculostomy-related infection is rare during the first week after insertion [46].
Additionally, a longitudinal analytical approach results in a high-resolution due to frequent repeated measures, which eases the process of visualizing on which time point (day) potential differences between groups occur. However, this analytical approach limits the likelihood of finding significant differences between groups on a specific day. Thus, in our study p values for individual days are less important than the visualization of the dynamic changes over time.
Finally, this is still a novel investigation field in which our exploratory and retrospective study design was not able to include all potential laboratory and clinical confounders, which may alter LCP profiles in plasma and CSF. Future studies should investigate comorbidities, in particular on-going inflammatory/infectious diseases, neoplastic, paraneoplastic and demyelinating conditions, premorbid hypertension as stated in recent recommendations as well as other potential confounders [42, 47].
Conclusion
Our study revealed that SAH patients treated with external ventricular drain had elevated levels of LCP initiators in CSF compared with neurologically healthy patients. Intrathecal ficolin-1 and MBL were increased in SAH patients with a poor functional outcome. No association was found between DCI and overall CSF levels of LCP initiators. Future studies should clarify the pathophysiological mechanism behind ficolin-1 in the central nervous system and determine the potential of ficolin-1 as a prognostic marker of functional outcome.
Supplementary Information
Additional file 1. Supplementary Table 1
Acknowledgements
We are grateful to Mr. Jesper Andresen for laboratory assistance.
Abbreviations
- BBB
Blood-brain barrier
- CNS
Central nervous system
- CSF
Cerebrospinal fluid
- CT
Computed tomography
- DCI
Delayed cerebral ischemia
- EBI
Early brain injury
- ELISA
Enzyme-linked immunosorbent assay
- EVD
External ventricular drain
- LCP
Lectin complement pathway
- MASP
Mannose-binding lectin associated serine protease
- MBL
Mannose-binding lectin
- mRS
Modified ranking scale
- SAH
Subarachnoid hemorrhage
- WFNS
World Federation of Neurosurgical Societies
Authors’ contributions
JSM and SB had access to all data used in the study and take full responsibility for the integrity of the data. JSM, JLF, and SB take responsibility for the accuracy of the statistical analysis. JSM analyzed data, drafted the manuscript, and revised it critically for intellectual content. CLK collected data and revised the manuscript critically for intellectual content. JLF analyzed data and revised the manuscript critically for intellectual content. PG conceived the study, analyzed laboratory data and revised the manuscript critically for intellectual content, handled funding and supervision. KM conceived and designed the study, revised the manuscript critically for intellectual content, handled funding and supervision. SB conceived and designed the study, collected data, analyzed data, revised the manuscript critically for intellectual content, handled funding and supervision. The authors read and approved the final manuscript.
Funding
J.S.M. was supported by a 6-month research scholarship by the University Hospital of Copenhagen/Rigshospitalet. C.L.K. received funding from the Ehrenreich Foundation. P.G. was supported by The Danish Research Foundation of Independent Research [DFF-6110-00489], The Svend Andersen Research Foundation and the Novo Nordisk Research Foundation. S.B. received grants from the Research Board at Rigshospitalet, Copenhagen, Denmark and Lundbeckfonden (R212-2015-1987). J.L.F and K.M. report no disclosures.
Availability of data and materials
The datasets generated and analyzed during the current study are available from the authors on reasonable request and provided a Data Sharing Agreement approved by the Danish Data Protection Agency.
Ethics approval and consent to participate
Protocols were approved by the Danish Scientific Ethics Committee of the Capital Region (H-3-2013-009 and H-3-2014-073) including amendments for the present study (H-3-2013-009 and H-6-2014-073), and the Danish Data Protection Agency (I-suite # 02116 and 03279), and registered at clinicaltrials.gov (NCT01791257 and NCT02320539). Informed consent was obtained from the next of kin, the general practitioner and when possible, from the patient.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interest and no conflict of interest with respect to the research, authorship, and publication.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ingall T, Asplund K, Mahonen M, Bonita R. A multinational comparison of subarachnoid hemorrhage epidemiology in the WHO MONICA stroke study. Stroke. 2000;31:1054–1061. doi: 10.1161/01.STR.31.5.1054. [DOI] [PubMed] [Google Scholar]
- 2.Johnston SC, Selvin S, Gress DR. The burden, trends, and demographics of mortality from subarachnoid hemorrhage. Neurology. 1998;50:1413–1418. doi: 10.1212/WNL.50.5.1413. [DOI] [PubMed] [Google Scholar]
- 3.de Rooij NK, Linn FH, van der Plas JA, Algra A, Rinkel GJ. Incidence of subarachnoid haemorrhage: a systematic review with emphasis on region, age, gender and time trends. J Neurol Neurosurg Psychiatry. 2007;78:1365–1372. doi: 10.1136/jnnp.2007.117655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rowland MJ, Hadjipavlou G, Kelly M, Westbrook J, Pattinson KT. Delayed cerebral ischaemia after subarachnoid haemorrhage: looking beyond vasospasm. Br J Anaesth. 2012;109:315–329. doi: 10.1093/bja/aes264. [DOI] [PubMed] [Google Scholar]
- 5.Vergouwen MD, Vermeulen M, van Gijn J, et al. Definition of delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage as an outcome event in clinical trials and observational studies: proposal of a multidisciplinary research group. Stroke. 2010;41:2391–2395. doi: 10.1161/STROKEAHA.110.589275. [DOI] [PubMed] [Google Scholar]
- 6.Adams HP., Jr Early management of the patient with recent aneurysmal subarachnoid hemorrhage. Stroke. 1986;17:1068–1070. doi: 10.1161/01.STR.17.6.1068. [DOI] [PubMed] [Google Scholar]
- 7.Foreman B. The Pathophysiology of Delayed Cerebral Ischemia. J Clin Neurophysiol. 2016;33:174–182. doi: 10.1097/WNP.0000000000000273. [DOI] [PubMed] [Google Scholar]
- 8.Geraghty JR, Testai FD. Delayed cerebral ischemia after subarachnoid hemorrhage: beyond vasospasm and towards a multifactorial pathophysiology. Current atherosclerosis reports. 2017;19:50. doi: 10.1007/s11883-017-0690-x. [DOI] [PubMed] [Google Scholar]
- 9.Bajic G, Degn SE, Thiel S, Andersen GR. Complement activation, regulation, and molecular basis for complement-related diseases. Embo j. 2015;34:2735–2757. doi: 10.15252/embj.201591881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Degn SE, Thiel S. Humoral pattern recognition and the complement system. Scand J Immunol. 2013;78:181–193. doi: 10.1111/sji.12070. [DOI] [PubMed] [Google Scholar]
- 11.Garred P, Genster N, Pilely K, et al. A journey through the lectin pathway of complement-MBL and beyond. Immunol Rev. 2016;274:74–97. doi: 10.1111/imr.12468. [DOI] [PubMed] [Google Scholar]
- 12.Degn SE, Hansen AG, Steffensen R, Jacobsen C, Jensenius JC, Thiel S. MAp44, a human protein associated with pattern recognition molecules of the complement system and regulating the lectin pathway of complement activation. J Immunol. 2009;183:7371–7378. doi: 10.4049/jimmunol.0902388. [DOI] [PubMed] [Google Scholar]
- 13.Fust G, Munthe-Fog L, Illes Z, et al. Low ficolin-3 levels in early follow-up serum samples are associated with the severity and unfavorable outcome of acute ischemic stroke. J Neuroinflammation. 2011;8:185. doi: 10.1186/1742-2094-8-185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zangari R, Zanier ER, Torgano G, et al. Early ficolin-1 is a sensitive prognostic marker for functional outcome in ischemic stroke. J Neuroinflammation. 2016;13:16. doi: 10.1186/s12974-016-0481-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang ZY, Sun ZR, Zhang LM. The relationship between serum mannose-binding lectin levels and acute ischemic stroke risk. Neurochem Res. 2014;39:248–253. doi: 10.1007/s11064-013-1214-x. [DOI] [PubMed] [Google Scholar]
- 16.Zhang ZG, Wang C, Wang J, et al. Prognostic value of mannose-binding lectin: 90-day outcome in patients with acute ischemic stroke. Mol Neurobiol. 2015;51:230–239. doi: 10.1007/s12035-014-8682-0. [DOI] [PubMed] [Google Scholar]
- 17.Llull L, Thiel S, Amaro S, Cervera A, Planas AM, Chamorro A. Ficolin-1 levels in patients developing vasospasm and cerebral ischemia after spontaneous subarachnoid hemorrhage. Mol Neurobiol. 2017;54:6572–6580. doi: 10.1007/s12035-016-0180-0. [DOI] [PubMed] [Google Scholar]
- 18.Sandgaard E, Troldborg A, Lauridsen SV, Gyldenholm T, Thiel S, Hvas AM. Changes in the lectin pathway following intracerebral or spontaneous subarachnoid hemorrhage. Mol Neurobiol. 2019;56:78–87. doi: 10.1007/s12035-018-1066-0. [DOI] [PubMed] [Google Scholar]
- 19.Zanier ER, Zangari R, Munthe-Fog L, et al. Ficolin-3-mediated lectin complement pathway activation in patients with subarachnoid hemorrhage. Neurology. 2014;82:126–134. doi: 10.1212/WNL.0000000000000020. [DOI] [PubMed] [Google Scholar]
- 20.Cai JY, Sun J, Yu ZQ. Serum mannose-binding lectin levels after aneurysmal subarachnoid hemorrhage. Acta Neurol Scand. 2016;134:360–367. doi: 10.1111/ane.12552. [DOI] [PubMed] [Google Scholar]
- 21.Bache S, Rasmussen R, Rossing M, Laigaard FP, Nielsen FC, Moller K. MicroRNA Changes in Cerebrospinal Fluid After Subarachnoid Hemorrhage. Stroke. 2017;48:2391–2398. doi: 10.1161/STROKEAHA.117.017804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Teasdale GM, Drake CG, Hunt W, et al. A universal subarachnoid hemorrhage scale: report of a committee of the World Federation of Neurosurgical Societies. J Neurol Neurosurg Psychiatry. 1988;51:1457. doi: 10.1136/jnnp.51.11.1457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fisher CM, Kistler JP, Davis JM. Relation of cerebral vasospasm to subarachnoid hemorrhage visualized by computerized tomographic scanning. Neurosurgery. 1980;6:1–9. doi: 10.1227/00006123-198001000-00001. [DOI] [PubMed] [Google Scholar]
- 24.van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke. 1988;19:604–607. doi: 10.1161/01.STR.19.5.604. [DOI] [PubMed] [Google Scholar]
- 25.Munthe-Fog L, Hummelshoj T, Honore C, et al. Variation in FCN1 affects biosynthesis of ficolin-1 and is associated with outcome of systemic inflammation. Genes Immun. 2012;13:515–522. doi: 10.1038/gene.2012.27. [DOI] [PubMed] [Google Scholar]
- 26.Munthe-Fog L, Hummelshoj T, Hansen BE, et al. The impact of FCN2 polymorphisms and haplotypes on the Ficolin-2 serum levels. Scand J Immunol. 2007;65:383–392. doi: 10.1111/j.1365-3083.2007.01915.x. [DOI] [PubMed] [Google Scholar]
- 27.Munthe-Fog L, Hummelshoj T, Ma YJ, et al. Characterization of a polymorphism in the coding sequence of FCN3 resulting in a Ficolin-3 (Hakata antigen) deficiency state. Mol Immunol. 2008;45:2660–2666. doi: 10.1016/j.molimm.2007.12.012. [DOI] [PubMed] [Google Scholar]
- 28.Garred P, Madsen HO, Kurtzhals JA, et al. Diallelic polymorphism may explain variations of the blood concentration of mannan-binding protein in Eskimos, but not in black Africans. Eur J Immunogenet. 1992;19:403–412. doi: 10.1111/j.1744-313X.1992.tb00083.x. [DOI] [PubMed] [Google Scholar]
- 29.Jacob A, Alexander JJ. Complement and blood-brain barrier integrity. Mol Immunol. 2014;61:149–152. doi: 10.1016/j.molimm.2014.06.039. [DOI] [PubMed] [Google Scholar]
- 30.Brouwer MC, Baas F, van der Ende A, van de Beek D. Genetic variation and cerebrospinal fluid levels of mannose binding lectin in pneumococcal meningitis patients. PLoS One. 2013;8:e65151. doi: 10.1371/journal.pone.0065151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shen L, Zheng J, Wang Y, et al. Increased activity of the complement system in cerebrospinal fluid of the patients with Non-HIV Cryptococcal meningitis. BMC Infect Dis. 2017;17:7. doi: 10.1186/s12879-016-2107-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kjaeldgaard AL, Pilely K, Olsen KS, et al. Amyotrophic lateral sclerosis: The complement and inflammatory hypothesis. Mol Immunol. 2018;102:14–25. doi: 10.1016/j.molimm.2018.06.007. [DOI] [PubMed] [Google Scholar]
- 33.Alexander JJ. Blood-brain barrier (BBB) and the complement landscape. Mol Immunol. 2018;102:26–31. doi: 10.1016/j.molimm.2018.06.267. [DOI] [PubMed] [Google Scholar]
- 34.Runza VL, Schwaeble W, Mannel DN. Ficolins: novel pattern recognition molecules of the innate immune response. Immunobiology. 2008;213:297–306. doi: 10.1016/j.imbio.2007.10.009. [DOI] [PubMed] [Google Scholar]
- 35.Honore C, Rorvig S, Munthe-Fog L, et al. The innate pattern recognition molecule Ficolin-1 is secreted by monocytes/macrophages and is circulating in human plasma. Mol Immunol. 2008;45:2782–2789. doi: 10.1016/j.molimm.2008.02.005. [DOI] [PubMed] [Google Scholar]
- 36.De Blasio D, Fumagalli S, Orsini F, et al. Human brain trauma severity is associated with lectin complement pathway activation. J Cereb Blood Flow Metab. 2019;39:794–807. doi: 10.1177/0271678X18758881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pedersen ED, Loberg EM, Vege E, Daha MR, Maehlen J, Mollnes TE. In situ deposition of complement in human acute brain ischaemia. Scand J Immunol. 2009;69:555–562. doi: 10.1111/j.1365-3083.2009.02253.x. [DOI] [PubMed] [Google Scholar]
- 38.Huang J, Kim LJ, Mealey R, et al. Neuronal protection in stroke by an sLex-glycosylated complement inhibitory protein. Science. 1999;285:595–599. doi: 10.1126/science.285.5427.595. [DOI] [PubMed] [Google Scholar]
- 39.Mocco J, Mack WJ, Ducruet AF, et al. Complement component C3 mediates inflammatory injury following focal cerebral ischemia. Circ Res. 2006;99:209–217. doi: 10.1161/01.RES.0000232544.90675.42. [DOI] [PubMed] [Google Scholar]
- 40.Imm MD, Feldhoff PW, Feldhoff RC, Lassiter HA. The administration of complement component C9 augments post-ischemic cerebral infarction volume in neonatal rats. Neurosci Lett. 2002;325:175–178. doi: 10.1016/S0304-3940(02)00271-9. [DOI] [PubMed] [Google Scholar]
- 41.Orsini F, Fumagalli S, Csaszar E, et al. Mannose-binding lectin drives platelet inflammatory phenotype and vascular damage after cerebral ischemia in mice via IL (Interleukin)-1alpha. Arterioscler Thromb Vasc Biol. 2018;38:2678–2690. doi: 10.1161/ATVBAHA.118.311058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chou SH, Macdonald RL, Keller E, Unruptured Intracranial A, Investigators SCP. Biospecimens and molecular and cellular biomarkers in aneurysmal subarachnoid hemorrhage studies: common data elements and standard reporting recommendations. Neurocrit Care. 2019;30:46–59. doi: 10.1007/s12028-019-00725-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Amara U, Flierl MA, Rittirsch D, et al. Molecular intercommunication between the complement and coagulation systems. J Immunol. 2010;185:5628–5636. doi: 10.4049/jimmunol.0903678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Krzyzewski RM, Klis KM, Kwinta BM, Stachura K, Guzik TJ, Gasowski J. High Leukocyte Count and Risk of Poor Outcome After Subarachnoid Hemorrhage: A Meta-Analysis. World Neurosurg. 2020;135:e541–e547. doi: 10.1016/j.wneu.2019.12.056. [DOI] [PubMed] [Google Scholar]
- 45.Schuss P, Hadjiathanasiou A, Brandecker S, Guresir A, Vatter H, Guresir E. Elevated C-reactive protein and white blood cell count at admission predict functional outcome after non-aneurysmal subarachnoid hemorrhage. J Neurol. 2018;265:2944–2948. doi: 10.1007/s00415-018-9091-5. [DOI] [PubMed] [Google Scholar]
- 46.Mounier R, Birnbaum R, Cook F, et al. Natural history of ventriculostomy-related infection under appropriate treatment and risk factors of poor outcome: a retrospective study. J Neurosurg. 2018:1–10. [DOI] [PubMed]
- 47.Jaja BNR, Saposnik G. Lingsma HF, et al. Development and validation of outcome prediction models for aneurysmal subarachnoid haemorrhage: the SAHIT multinational cohort study. 2018;360:j5745. doi: 10.1136/bmj.j5745. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Supplementary Table 1
Data Availability Statement
The datasets generated and analyzed during the current study are available from the authors on reasonable request and provided a Data Sharing Agreement approved by the Danish Data Protection Agency.