Abstract
Background
Excessive generation of reactive oxygen species (ROS) in the presence of a defective antioxidant system can induce cellular damage and disrupt normal physiological functions. Several studies have revealed the unfavorable role of ROS in promoting the growth, proliferation, migration, and survival of leukemia cells. In this review study, we summarize the mechanisms of ROS production and its role in leukemogenesis, counteractive effects of antioxidants, and implicate the current ROS-dependent anticancer therapies in acute myeloid leukemia.
Body
The dysregulation of the redox system is known to play a significant role in the pathogenesis of leukemia. Leukemia cells generate high levels of ROS, which further increases the levels through extra pathways, including mitochondrial deoxyribonucleic mutation, leukemic oncogene activation, increased nicotinamide adenine phosphate hydrogen (NADPH), and cytochrome P450 activities. Aforementioned pathways once activated have shown to promote genomic instability, induce drug resistance to leukemia medical therapy, disease relapse and reduce survival period. The current standard of treatment with chemotherapy employs the pro-oxidant approach to induce apoptosis and promote tumor regression. However, this approach retains several deleterious effects on the subject resulting in degradation of the quality of life. Nevertheless, the addition of an antioxidant as an adjuvant drug to chemotherapy alleviates treatment-related toxicity, increases chemotherapeutic efficacy, and improves survival rates of a patient.
Conclusion
Acute myeloid leukemia remains a daunting challenge to clinicians. The desire to achieve the maximum benefit of chemotherapy but also improve patient outcomes is investigated. ROS generated through several pathways promotes leukemogenesis, drug resistance, and disease relapse. Chemotherapy, the mainstay of treatment, further upregulates ROS levels. Therefore, the addition of an antioxidant to leukemia medical therapy alleviates toxicity and improves patient outcomes.
Keywords: Acute myeloid leukemia, Reactive oxygen species, Oxidative stress, Oncogene mutations, Jab1/COPS5, Antioxidants
Introduction
Reactive Oxygen Species (ROS) is a variety of chemically-active and oxygen-containing molecules that are naturally produced during cellular metabolism [1] and are involved in regulating normal biological cell functions, cell signaling, and homeostasis [2, 3]. They play critical roles in promoting health and longevity, and antimicrobial phagocytosis by cells of the innate immune system [4]. ROS in low concentrations is beneficial to supporting cell proliferation and continuity of pathways, whereas high concentration leads to the damage of deoxyribonucleic acid (DNA), proteins and lipids in normal or precancerous cells and promotes malignancy transformation. Therefore, the dynamic regulation of ROS in the redox microenvironment is critical to cell survival and function.
Typically, an intracellular balance between the generation and elimination of ROS is maintained by antioxidants or specific regulatory pathways, with the major players being Glutathione and Thioredoxin. In hematological malignancies distinctly, ROS perform a double role in tumorigenicity [5]. At high levels, ROS suppress tumor growth and induce apoptosis, which is the primary mode of action of chemotherapeutic agents [6]. In contrast, at low levels, ROS protect the cell from apoptosis and promote cell survival, growth, proliferation, migration, and drug resistance.
A pervasive condition in which an imbalance between ROS production and the response of endogenous antioxidant defense systems resulting in ROS accumulation is known as oxidative stress (OS) [7]. OS is implicated in several acute and chronic diseases, including hematological malignancies such as acute myeloid leukemia (AML), chronic myeloid leukemia (CML), acute lymphoblastic leukemia (ALL), and myelodysplastic syndromes. AML is a highly aggressive hematopoietic malignancy characterized by highly proliferative blast cells. It is the most common acute leukemia in adults with an increasing incidence with age and high relapse rates [8]. Despite current advancement in the treatment of AML, refractory disease remains prevalent, with disease relapse being the major cause of treatment failure [9]. The current AML management guidelines largely rely on high-dose chemotherapy with cytarabine- and anthracycline-based regimes, and allogeneic hematopoietic stem cell transplant (HSCT) [10].
The use of intensive chemotherapy leads to increased ROS generation and ROS-induced cytotoxicity. Elevated ROS levels and other molecular mechanisms of ROS production, including nicotinamide adenine dinucleotide phosphate (NADPH) oxidase, mitochondrial electron transport chain (mtETC), leukemic oncogene activity, xanthine oxidase, and cytochrome P450, are the key feature of leukemia cells [11]. AML is associated with an inadequate antioxidant status resulting in an imbalance in the redox microenvironment leading to OS. Antioxidants control the OS state and provide a major defense line in blocking the harmful effects of ROS [12]. Several studies support the application of antioxidants in leukemia treatment to improve patient outcomes. This review study aims at summarizing the mechanisms of ROS production and its role in leukemogenesis, counteractive effects of antioxidants and implicate the current ROS-dependent anticancer therapies in AML.
ROS and the mechanisms of ROS production
ROS are a heterogenous group of small molecules and free radicles, which include hydrogen peroxide, superoxide anions, ozone, singlet oxygen, organic peroxides and hypochlorous acids [13]. In hematopoietic stem cells (HSCs), ROS are generated in the mitochondria through NADPH oxidases and other ROS-related metabolic pathways such as polyamine metabolism, cytochrome P450, and xanthine oxidase [14]. Overproduction of ROS without adequate counteraction by antioxidants results in OS, which mediates the damage of cell structure and membranes, DNA, lipids, and proteins [15]. In hematological malignancies, OS is generated from chemotherapy and radiotherapy use. The effect of OS on cells can be acute or chronic. OS’ chronic effect is associated with little oxidative damage, accumulating over time in the life cycle of a cell, eventually interrupting normal cellular function and promoting cancerous changes. Acute OS is implicated in acute illness such as sepsis, cardiovascular accidents, myocardial infarction and is a useful measurement in evaluating acute illness [16].
ROS source can be either endogenous or exogenous. Cellular metabolism gives rise to endogenous ROS through mitochondria-catalyzed transport reactions, cytochrome P450 metabolism, and inflammatory activities involving neutrophils, eosinophils, peroxisomes, and macrophages [17]. Mitochondria are the primary source of free radicals in living organisms, generating an estimated 2–3 nmol of superoxide/min per mg of protein. Evidence shows that complex III of the mitochondria is the main site of ROS production in normal metabolism. Cytochrome P450 enzyme induces the production of superoxide anion and hydrogen peroxide after the breakdown of the P450 catalytic cycle [18]. Macrophage activation during inflammation may increase oxygen uptake, leading to increased superoxide anion, nitric oxide, and hydrogen peroxide [19]. The conversion of hypoxanthine to xanthine and its subsequent transformation into uric acid is catalyzed by xanthine oxidase with superoxide anion as a by-product [20].
Exogenous sources include cigarette smoke, which naturally contains free radicals and organic compounds like superoxide and nitric oxide, which activate endogenous mechanisms and lead to an accumulation of neutrophils and macrophages, worsening oxidant injury [21]. Exposure to ozone may cause lipid peroxidation and induce airway invasion by neutrophils and compromise lung function even in healthy individuals. Hyperoxia is a condition of high oxygen levels than the average partial pressure of oxygen in the lungs or other tissues, results in increased production of reactive oxygen and nitrogen species [22]. Exposure to radiation, xenobiotics, barbiturates, chlorinated compounds, air and water pollution, alcohol, and heavy metals are implicated in ROS production [23].
Oxidative stress-induced cellular injury
OS, as defined, occurs when intracellular antioxidants are unable to counteract the pro-oxidants, causing damage to various cell components and triggering activation of specific pathways [24]. The three main pathways by which OS causes cellular injury are lipid peroxidation of membranes, oxidative modification of proteins, and DNA damage [25]. In lipid peroxidation, damage to the cell membrane and other lipid-containing structures gives rise to primary products known as lipid hydroperoxides which alter membrane structure and endanger the cell [26]. The secondary products of lipid peroxidation, aldehydes, have a ‘no-charge’ property which allow them easily to permeate through the membranes into cytosol and cause extensive damage both inside and outside the cell. Amongst the aldehydes, malondialdehyde is highly mutagenic, and 4-hydroxynonenal is highly toxic [27].
Oxidative modification of proteins results in the formation of protein carbonyl derivatives which together with advanced oxidation protein products, advanced glycation end products, and S-nitrosylated proteins serve as markers for ROS-mediated protein damage [28]. The secondary products of lipid peroxidation, malondialdehyde and 4-hydroxynonenal, react with and modify proteins at several amino acid side chains leading to a formation of stable adducts and a change in the function and fate of that protein [25, 29]. The aldehyde protein-adducts play a vital role in physiological processes but are associated with disease pathogenesis, and influence the aging process and cellular senescence [30].
Studies have shown that ROS and lipid peroxidation products affect genomic and mitochondrial DNA (mtDNA), inducing DNA damage to nuclear and mitochondrial compartments. Furthermore, the replication of damaged DNA before repair leads to DNA mutations and genomic instability [31]. DNA double-strand breaks are the most destructive impairment compared to single-strand breaks. They cause severe genetic mutations leading to oncogene activation or tumor suppressor gene inactivation, gene expression modification and tumor development [32]. Though not harmful, single-strand breaks can result in serious lesions if not repaired early [33]. 8-oxoGuanine (8-OHG), an oxidation product generated in DNA through deoxyguanosine (dG) oxidation, and its nucleoside form 8-oxo-2′-deoxyguanosine (8-OHdG), are useful markers of oxidative DNA damage both in vivo and in vitro [34]. The formation of 8-OHG/8-OHdG, DNA lesions is responsible for mutagenesis and carcinogenesis [35, 36]. Products of lipid, protein, and DNA damage have been investigated and extensively studied as biomarkers of OS in leukemia by earlier pioneers [28, 37–39], as illustrated in (Table 1).
Table 1.
Extensively studied biomarkers of oxidative stress in patients with leukemia
| Biomarkers | Clinical Significance | Pioneer(S) |
|---|---|---|
| MDA,TAC | To determine the involvement of OS in AML development and implicate biomarkers of OS in disease diagnosis and prognosis | Tsamesidis et al. 2019 |
| PC,TBARS,LOOH | To evaluate and quantify products of protein carbonylation and lipid peroxidation as valuable indicators for OS and disease progression in CML | Singh et al. 2009 |
| MDA | To estimate MDA concentration as a marker of OS in AML patients receiving treatment | A. Hlavackova et al. 2019 |
| TBARS, PC | To determine oxidative damage from increased OS and decreased antioxidant defense in ALL patients | Battisti et al. 2008 |
Abbreviations: OS Oxidative stress, MDA Malondialdehyde, TAC Total antioxidant capacity, PC Protein carbonyl, TBARS Thiobarbituric acid reactive substances, LOOH Lipid hydroperoxide, AML Acute myeloid leukemia, CML Chronic myeloid leukemia, ALL Acute lymphoblastic leukemia
ROS in myeloid leukemia
Leukemogenesis is a multistep process caused by mutations in DNA repair genes, oncogenes, and tumor suppressor genes. Thus, it is difficult to identify a single driving force as to the cause of leukemogenesis. ROS are implicated in the pathogenesis of hematological malignancies [40, 41]. Increased ROS production remains a key feature of human tumor cells, of which leukemic cells are no exception. In leukemia, an increase in ROS and antioxidants, as an adaptive protective defense, is indicative of OS, resulting in genetic mutations, chromosomal alternations and contributes to carcinogenesis [42]. It has long been known that ROS have a crucial role in regulating the balance between self-renewal and myeloid differentiation of HSCs. Generally, ROS exist at low levels in HSCs to maintain pluripotency. Several theories support the mechanisms that promote leukemogenesis.
Primary ROS production in leukemia
NADPH oxidases (NOX) are an important primary source of ROS in leukemia. Studies have shown that over 60% of primary AML blasts produce high levels of NOX-derived ROS, promoting cell proliferation and survival in AML [41]. The increased ROS levels are associated with reduced GSH levels and depletion of antioxidant defense proteins, mtDNA and peroxiredoxin [43], demonstrating that NOX-derived ROS develop adaptative mechanisms to suppress stress signaling that would normally limit this response. The mtETC complex is another major source of endogenous ROS in any known cell type, and through oxidative phosphorylation, the mitochondria provide adenosine triphosphate. Mutations in mtDNA in leukemia cells lead to alternations in the mtETC, enhancing ROS production. In chronic lymphocytic leukemia (CLL), mitochondrial ROS are implicated in promoting genetic instability and drug resistance [44].
Leukemic blasts continuously generate excessive ROS involved in the regulation of intracellular signaling pathways and modulation of cells in the microenvironment, thereby promoting leukemogenesis [45]. In the leukemic bone marrow microenvironment, NADPH oxidase-2 derived ROS drive mitochondrial transfer between leukemic cells and bone marrow mesenchymal stromal cells through tunneling nanotubules enhancing metabolic activity in AML cells [46]. In addition to leukemic cells, immune cells such as neutrophils, eosinophils, mononuclear phagocytes, tumor-associated macrophages, regulatory T cells and myeloid-derived suppressor cells are implicated in ROS production in the microenvironment, facilitating tumor growth [47].
Metabolic pathways of ROS production
Xanthine oxidase/dehydrogenase has been implicated in several diseases, though its involvement in leukemia has not been adequately researched. It has been reported that increased xanthine oxidase activity and uric acid production is induced in myeloid leukemia cells. Activator protein-1 and hypoxia-inducible factor 1 transcription complexes are implicated in ligand-induced xanthine oxidase upregulation [48]. In relapsed AML, elevations in xanthine oxidase activity are found, contributing to increased ROS levels [49]. Cyclooxygenases and lipoxygenases, enzymes produced by tumor cells, are proved to promote tumorigenesis by directly promoting and enhancing cell proliferation, migration, and survival. The expression of cyclooxygenase-2 is highly elevated in CML and CLL and is associated with poor prognosis and enhancement of survival and proliferation of malignant cells [50].
Genetic polymorphisms of cytochrome P450 promote ROS generation in leukemia, though more investigation is required to clarify this theory. The bone marrow microenvironment is demonstrated to contribute to drug resistance, and this is associated with the expression of cytochrome P450 enzymes. In AML, fms-like receptor tyrosine kinase 3 (FLT3) mutations are among the most common genetic alterations. The introduction of FLT3 tyrosine kinase inhibitors (TKIs) to target AMLs with mutant FLT3 yields promising results. Still, it fails to achieve durable responses due to minimal residual disease resulting in disease relapse associated with resistance to FLT3 TKIs [51]. Cytochrome P450 enzymes contribute to bone marrow-mediated FLT3-AML protection from FLT3 inhibitors [52].
Oncogene activity-induced ROS production
Alternations in leukemic ‘driver’ oncogenes caused by chromosomal translocations and mutations are found in all forms of leukemia. Breakpoint cluster region-Abelson (BCR-ABL) mutation caused by a chromosomal translocation between chromosomes 9 and 22 is commonly found in CML and a subtype of ALL. It regulates proliferation and survival signaling in leukemia. Studies have shown that BCR-ABL expression can induce elevated ROS production, contributing to genomic instability and progression to blast-crisis in CML [53]. Mutations such as M244I, E255K, and T315I, caused by BCR-ABL induced ROS within the BCR-ABL kinase domain itself, promote resistance to BCR-ABL TKIs [54]. The idea that BCR-ABL oncogene induces ROS production responsible for the aberrant proliferation, cellular signaling, and resistance to TKIs can be validated.
FLT3-ITD (fms-like receptor tyrosine kinase 3-internal tandem duplication), Ras, and c-Kit are driver leukemic-oncogenes activated by mutations. FLT3-ITD is the most prevalent mutation in acute leukemia and is expressed in about 30% of AML patients [55]. FLT3-ITD mutation induces ROS elevation through NADPH oxidases, and its constitutive activity promotes proliferation and survival signaling in AML cells [56]. Ras mutations, found prevalent in about 20% of AML cases cause cell transformation through NADPH oxidase driven ROS, thereby promoting survival and growth factor-independent proliferation in human CD34+ cells [57]. C-Kit, much like Ras, has a role in ROS production by regulating NOX activity [58]. B-cell lymphoma 2 (Bcl-2) functions as an oncogene in AML, ALL, and CLL. Though previous studies demonstrated the inhibition potential of Bcl-2 by inducing antioxidant proteins in cancer cells [59], recent research has shown that Bcl-2 can promote ROS production in human leukemia cell lines, particularly. Bcl-2 family proteins regulate cancer cell migration, invasion, and metastases [60].
Recently, mutations in the Isocitrate dehydrogenase 1 and 2 (IDH1 and IDH2) genes have been reported common in AML, myelodysplastic syndromes, and angioimmunoblastic T-cell lymphomas [61]. When a mutation occurs, IDH1 and IDH2 convert α-ketoglutarate (α-KG) to 2-hydroxyglutarate (2-HG) while consuming NADPH instead of their normal function of converting isocitrate to α-KG. 2-HG accumulates to high levels in cancer cells inhibiting α-ketoglutarate-dependent dioxygenase enzymes, thereby expressing mutant IDH1 or IDH2 [62]. IDH mutations alter redox homeostasis by diminishing cellular NADPH, and through 2-HG, which acts as an ‘oncometabolite’ and contributes to leukemia transformation and progression [63].
In summary, mtETC and NOX complex are major sources of ROS in leukemic cells. Alternations in leukemic oncogene activity control several NOX components and induce elevated NADPH levels, resulting in amplified ROS production. The metabolic/detoxification enzymes, xanthine oxidase/dehydrogenase and cytochrome P450 also contribute to ROS production in leukemia cells. The mentioned pathways are implicated in leukemogenesis and leukemia progression, either by promoting genomic instability, cell proliferation, and survival, or creating drug resistance. Understanding the role of each ROS-producing pathway in leukemogenesis makes them potential targets for research in AML treatment.
Oncogene Jab1/COPS5 in myeloid leukemia
Recent research demonstrates the role of Jab1/COPS5 overexpression in tumorigenesis, signaling pathways and the development of oncogene inhibitors [64]. C-Jun activation domain-binding protein-1 (Jab1), which was initially identified as a c-Jun coactivator, is known to modulate cell proliferation, cell cycle, and apoptosis. Additionally, it regulates genomic instability, DNA damage response, and affects intracellular signaling through its existence as a member of the COP9 signalosome complex fifth subunit (COPS5, CSN5) [64, 65]. As a multifunctional complex, dysregulation of Jab1/COPS5 deactivates several tumor suppressors, and activates oncogenes, promoting oncogenesis. Furthermore, Jab1 stabilizes hypoxia-inducible factor-1alpha and c-Jun and acts as a transcription co-factor for MYC, regulating transcriptional activation of genes involved in cell proliferation, angiogenesis, and invasion [66]. As an oncogene, Jab1/COPS5 is aberrantly overexpressed in several human cancers and implicated in facilitating carcinogenesis.
In cancer, dysregulation of Jab1/COPS5 expression may originate from three regulatory mechanisms: gene amplification, microRNAs, and other signaling transduction pathways such as IL6-Stat3 (signal transducer and activator of transcription 3) signaling, HER2-AKT (human epidermal growth factor receptor 2-protein kinase B) signaling, and BCR-ABL signaling. However, more investigation is required to validate them [67]. A recent study was undertaken to investigate the role of ROS and OS on gene expression in the development and relapse of acute monocytic leukemia. In this study, blood samples obtained from AML patients at initial diagnosis were compared with AML cells from the same patients obtained at relapse. Collective data demonstrated that at both diagnosis and disease relapse, increased ROS production and low capacity of antioxidant enzymes were characteristics of AML-M5. High gene expression levels of Jab1 and Trx were associated with disease progression and poor prognosis in relapsed AML-M5, showing that increased levels of ROS stimulate aberrant gene expression and promote the proliferation of leukemic blasts. Jab1 is a new target in the ROS pathway and plays a critical role in the pathogenesis of AML-M5 through its interaction and positive regulation of Trx expression [68].
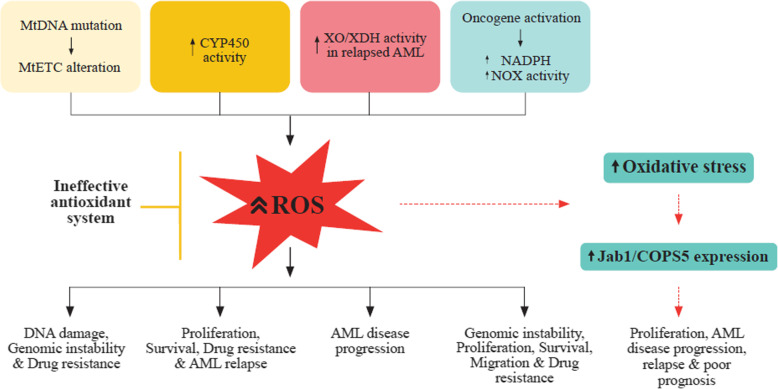
A summary of the different ROS generation mechanisms in leukemia cells and their role in leukemogenesis are shown (Fig. 1).
Fig. 1.
The different mechanisms of ROS generation in leukemia cells and their role in leukemogenesis. (1) MtDNA mutations lead to alternations in the mtETC, resulting in increased ROS production promoting DNA damage, genomic instability, and drug resistance in AML. (2) Activated genetic polymorphisms of CYP450 in AML, ALL, and CLL, generate high ROS levels contributing to cell proliferation, survival, drug resistance, and disease relapse. (3) Elevated XO/XDH activity leads to increased ROS & OS attributed to AML relapse and progression. (4) Leukemic oncogene activity (BCR/ABL, Flt3-ITD, Ras, c-Kit, JAK2 V617F) induce NADPH elevation and increased NOX activity resulting in elevated ROS levels which promote DNA damage, genetic instability, proliferation, survival, migration, and drug resistance in leukemic cells. (5) Increased ROS generated from leukemic cells, oncogene mutations, abnormal metabolism with an ineffective antioxidant system results in increased OS which aberrantly expresses Jab1/COPS5 leading to AML proliferation, progression, and relapse. Abbreviations: mitochondrial ETC, electron transport chain; CYP450, cytochrome P450; XO, xanthine oxidase; XDH, xanthine dehydrogenase; AML, acute myeloid leukemia; BCR/ABL, Breakpoint cluster region-Abelson leukemia virus; Flt3-FTD, FMS-like tyrosine kinase 3-internal tandem duplication; c-Kit, receptor tyrosine kinase; JAK2 V617F, Janus kinase 2 V617F; Jab1/COPS5, c-Jun activation domain-binding protein-1
Cellular antioxidants in myeloid leukemia
Antioxidants can either be upregulated or downregulated in leukemia cells. The upregulation of antioxidants is observed in acute leukemia, in which expression of superoxide dismutase (SOD), GSH, Trx, Peroxiredoxin is increased. Dysregulation of antioxidants alters redox homeostasis and may have beneficial or detrimental effects on leukemic cells. Upregulation of antioxidant activity increases the resistance of leukemic cells to deleterious ROS effects. Downregulation of antioxidant activity has been reported in lymphocytes from ALL [69] and CLL [70] patients in which both SOD and catalase (CAT) activity was reduced.
Heme oxygenase (HO) has defense properties against ROS in leukemia and is implicated in AML and CML. HO neutralizes the highly cytotoxic, free-radical producing heme that controls diverse molecular and cellular processes [71]. Of its multiple isoforms, HO-1 is predominantly involved in redox biology and catalyzes the oxidative degradation of cellular heme into free iron, carbon monoxide, and biliverdin, which is immediately converted into bilirubin. HO-1 has shown to exhibit antioxidant, antiapoptotic, and immune-modulating effects by removing pro-oxidant heme and catabolic end-products, thereby providing a cytoprotective and beneficial function to cells. Contradicting evidence shows that HO-1 may promote carcinogenesis and drug-resistance in AML upon induction with chemotherapeutic drugs [72]. Similarly, in CML, HO-1 expression correlates with cell survival, proliferation, and drug resistance [73].
Superoxide dismutase (SOD) catalyzes the conversion of superoxide to molecular oxygen and hydrogen peroxide, further processed into water and molecular oxygen by CAT. In leukemia, however, the activity of SOD remains debatable. Different expression of SOD in leukemia blasts and serum have been noted. For instance, SOD activity was decreased in lymphocytes from ALL [39] and CLL [70] patients, whereas protein expression of SOD, was increased in the serum collected from acute leukemia patients and the decrease in the SOD2 was linked to disease regression [74]. Analyses of SOD in both leukemic blasts and serum from patients could explain the inconsistency in SOD elevation or reduction in leukemia. SOD inhibition has shown to induce apoptosis by the elevation of superoxide and free-radical mediated mitochondrial damage in all four subtypes of leukemia [75].
Catalase (CAT) catalyzes the conversion of hydrogen peroxide into water and molecular oxygen. Overexpression of CAT is cytoprotective to cells, as it increases life span and decreases ROS-induced injury. However, in leukemia, alteration of CAT may lead to increased proliferation, genomic instability, and drug resistance. The increase or decrease in catalase activity has different implications on both myeloid and lymphocytic type leukemias. In AML cell lines and CML samples, an elevation in CAT activity was observed compared to normal granulocytes [76]. Increased CAT activity results in lowered ROS levels, which promote proliferation and resistance to chemotherapeutics [77]. Contrarily, decreased CAT activity results in elevated ROS levels associated with lipid, DNA damage, and genomic instability.
Glutathione (GSH) is the most abundant antioxidant present within the cells and is consumed in the cells to restore other antioxidants and remove OS. Glutathione peroxidase catalyzes the conversion of GSH to oxidized glutathione disulfide (GSSG). When cellular GSH is low, GSSG is reduced back to GSH through a reaction that utilizes NADPH, thereby forming a redox cycle. A depletion in GSH or reduced GSH/GSSH ratio leads to OS, implicated in cancer progression. In contrast, elevated GSH levels increase the antioxidant capacity resulting in resistance to OS in cancer cells. GSH elevation has been observed in hematological malignancies and is associated with chemoresistance. Study shows that elevated GSH levels in leukemic blasts of children and adults with ALL were associated with increased resistance to melphalan, daunorubicin, and prednisolone [78].
Thioredoxin (Trx) system regulates cellular ROS levels and helps maintain redox homeostasis of leukemia cells. The elimination of hydrogen peroxide processed from superoxide anion involves Trx, thioredoxin reductase, and NADPH. Peroxiredoxin reduces hydrogen peroxide, and the oxidized peroxiredoxin is, in turn, reduced by Trx. Furthermore, oxidized Trx is recycled by thioredoxin reductase using NADPH [79]. In the presence of thioredoxin reductase, Trx takes electrons from NADPH, transfers them to the active site of Trx, then uses the electrons to decrease protein disulfides [80]. The Trx system has been implicated in carcinogenesis by promoting cell proliferation, angiogenesis, metastasis, and inhibiting apoptosis signal-regulating kinase 1. In hematological malignancies, upregulation of Trx expression is associated with aggressive disease and shorter relapse interval, as observed in samples from patients with primary and relapsed AML and ALL [49].
ROS modulated therapy in AML
The pro-oxidant approach
Leukemia cells are known to generate high ROS levels, and chemotherapy, which is the mainstay treatment in leukemia, is associated with elevated ROS levels. The purine analog, cytarabine, effectively induces remission in AML, although it has high toxicity profiles and a short duration of clinical response with a 5-year event-free survival [81]. Cytarabine induces ROS elevation in both leukemia cells and nonproliferating cells and alters the antioxidant levels in these cells. The early induction of ROS and altered antioxidant expression contribute to OS and eventually lead to apoptotic death [82]. Vincristine, a mitotic inhibitor, has successfully treated ALL when combined with anthracyclines, steroids, or asparaginase, though with early relapse of 15 months. Much like cytarabine, an early elevation in ROS is seen with the initiation of treatment with vincristine [83].
Daunorubicin, idarubicin, and mitoxantrone are anthracyclines which, when in their semiquinone free radical form, can induce direct DNA damage or promote ROS production by interacting with molecular oxygen [84]. Furthermore, anthracyclines complex with free iron in cells, leading to a Fenton reaction in which the combination of iron and hydrogen peroxide results in a further upregulation of ROS. Arsenic trioxide, an anti-leukemic agent that has shown encouraging results in treating relapsed acute promyelocytic leukemia, induces ROS production through Trx inhibition and NOX activation [85]. In a recent study, the pro-oxidant approach of high-dose ascorbate in combination with arsenic trioxide in AML and acute promyelocytic leukemia was evaluated and proved that leukemic cell apoptosis was related to increased ROS and OS [86].
Histone deacetylase inhibitors (HDACi) induce ROS production as part of their cytotoxic mechanism by elevating NOX2 expression and increasing the thioredoxin-binding protein-2 (TBP-2) gene expression and promoting the expression of the Bcl-2 family member Bid. Vorinostat, an HDACi, was reported to induce ROS, DNA damage, and eventually apoptosis in leukemic cell lines [87]. The combination of HDACi with standard chemotherapy agents could potentiate their effectiveness in clinical outcomes [11]. The relation between Proteasome Inhibitors and ROS production is better established in hematological malignancies than in solid tumors. Bortezomib, the first proteosome inhibitor approved by the FDA, has shown promising clinical outcomes in mantle cell lymphoma and myeloma and may have therapeutic benefits in leukemia. In vitro studies have indicated that bortezomib inhibits proliferation in AML blasts and enhances apoptosis [88].
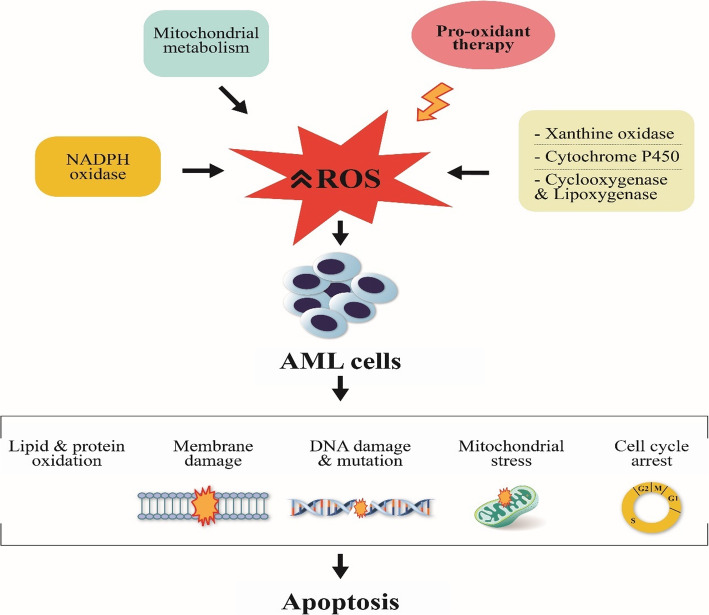
The pro-oxidant approach has been preferred over the past years due to the hypothesis that amplification of ROS levels by chemotherapy and other ROS-producing agents induces apoptotic death and leads to tumor regression. Apart from increasing ROS, this approach can lead to damage of lipids, proteins, and DNA, mutations, mitochondrial stress, reduced antioxidant capacity, and cell cycle arrest, all of which have been implicated in cell injury and cell death (Fig. 2). However, prolonged exposure to chemotherapy-induced ROS may induce chemoresistance and lead to increased genetic instability in cancer cells due to ROS-induced mutations [56, 89]. In conclusion, chemotherapy-induced ROS may inhibit the antioxidant defense system leading to further upregulation of ROS and eventually apoptotic death of AML cells [90].
Fig. 2.
Mechanisms by which the pro-oxidant approach induces cell death in leukemia treatment
The antioxidant approach
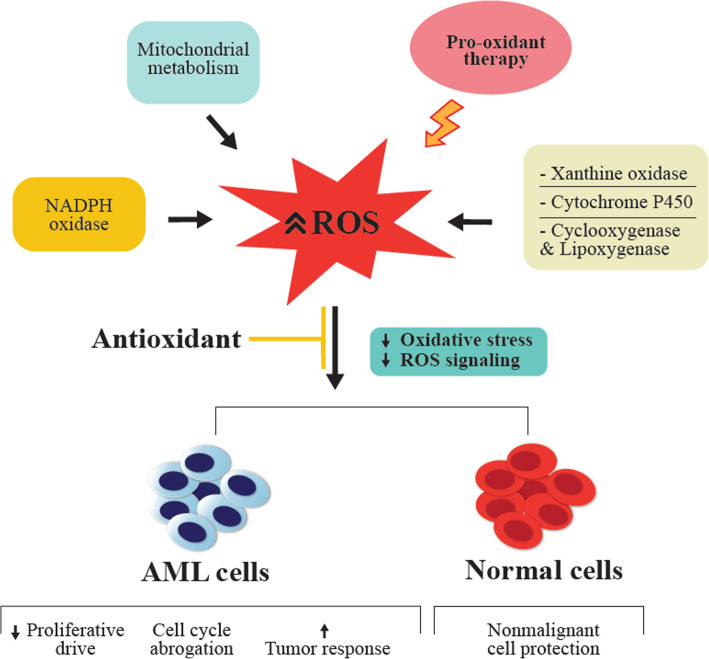
Antioxidant use to counteract the deleterious effects of ROS or cytotoxicity induced by chemotherapy/radiotherapy in several diseases, including leukemia, was previously frowned upon in clinical practice. Several studies argue that antioxidants may reduce the effectiveness of these agents by protecting not only healthy cells but also malignant cells [91]. To balance the deleterious effects of pro-oxidant therapy, antioxidants reduce ROS signaling, decrease proliferative drive and abrogate the cell cycle, and through these mechanisms, may reduce tumor burden and protect healthy cells from oxidative damage (Fig. 3) [92]. Nutrient antioxidants which are exogenous sources of antioxidants obtained from food supplements are vitamins A, C, E, carotenoids, flavonoids, trace elements, polyphenols, melatonin, to mention a few, with vitamin C being the most widely used supplement.
Fig. 3.
Mechanisms by which antioxidants counteract deleterious effects of pro-oxidant therapy. Antioxidant application to pro-oxidant therapy reduces OS, ROS signaling, and proliferative drive. Furthermore, it induces cell cycle suppression, increases tumor response of AML cells, and protects nonmalignant cells
Evidence shows that when antioxidants are administered concurrently with chemotherapy, they enhance the cytotoxicity of chemotherapy against malignant cells, protect healthy cells and tissue against treatment-related toxicities, increase patient survival and treatment response, and do not interfere with chemotherapy [93, 94]. In addition to this, supplementation with antioxidants and other nutrients may restore the body’s’ natural antioxidant vitamins and minerals depleted during chemotherapy, which may enhance the patients’ health status. In AML and CML patients, who are reported to have reduced antioxidant capacity, antioxidants have shown to inhibit both the initiation and promotion of carcinogenesis [7]. With antioxidant application in cancer therapy, the challenge is determining which dose intensity to apply: the preventive dose (low dose), which protects both normal and tumor cells or therapeutic dose (high dose), which inhibits the growth of tumor cells but not normal cells.
Studies, both in vitro and in vivo, have shown that combining antioxidants with specific chemotherapeutic agents provides positive benefits and enhances patients’ survival [95]. In a systematic review conducted by Nakayama et al. on the concurrent use of dietary antioxidants with chemotherapy/radiotherapy, it was reported that GSH, vitamin E and N-acetylcysteine (NAC) were the most frequently used in different types of cancers, including leukemia [96], with GSH being the most studied [94]. The effect of antioxidants and a healthy lifestyle of fruit, vegetables, nuts, and seeds were explored to reduce the risk of infectious complications in CLL. Results suggested that antioxidants stimulated immune response and lowered the incidence of infectious complications in CLL patients [97]. Compound kushen injection (CKI), studied as a promising prospect for the treatment of AML, showed the potential of regulating ROS levels to prevent AML relapse as an antioxidant. This study showed that CKI inhibited the proliferation of both hyperleukocytic and non-hyperleukocytic AML cells, and promoted apoptosis of AML cells. Additionally, CKI inhibited intracellular ROS levels by increasing peroxiredoxin 2 and peroxiredoxin 3 expression and decreasing Trx1 expression [98].
The PI, Ixazomib, was evaluated for use in human AML cell lines expressing the mutated nucleophosmin-1 gene. Superoxide induction after ixazomib treatment enhanced apoptosis and cytotoxicity that was reduced by treatment with NAC. The study proved that antioxidants could reduce the toxicity of pro-oxidant drugs [99]. NAC administration elevated antioxidant activity and showed potential in preventing leukemia initiation and reducing DNA damage induced by HL-60 leukemia cells [100]. In children with ALL on chemotherapy, adequate supplementation with Vitamin C and E and β-carotene was associated with a decreased risk of chemotherapy-related toxicity and a lower incidence of infections. In contrast, a lower intake of antioxidants was associated with increased adverse effects [101]. Because several antioxidants stimulate apoptotic pathways and chemotherapy also induces apoptosis by harming DNA, complementary effects between chemotherapeutics and antioxidants exist [94]. The polyphenols, resveratrol, and curcumin exhibit pro-oxidant and antioxidant effects, whether in combination with other natural antioxidants or classical chemotherapy and may be promising future strategies in chemoprevention and chemotherapy of hematological malignancies [102, 103].
In summary, to obtain the desired beneficial results from chemotherapy in AML patients, it may be necessary to supplement treatment with nutritional antioxidants. Targeted nutritional therapies with antioxidants may enhance the patients’ health status, reduce treatment-related toxicities, and increase chemotherapeutic efficiency, thereby improving AML patients’ outcomes.
Conclusion
AML remains a daunting challenge with high relapse rates and poor patient outcomes despite the current treatment advancements. ROS and OS have been implicated in cellular injury and leukemogenesis. Leukemia cells exhibit elevated ROS levels, of which several identified pathways further increase ROS generation. Alterations in mitochondrial metabolism, cytochrome P450, leukemic oncogenes, expression of metabolic enzymes, and a defective antioxidant capacity play a role in leukemogenesis. The oncogene Jab1/COPS5 is aberrantly expressed in several malignancies, including leukemia. Overexpression of Jab1 and Trx was associated with disease progression and poor prognosis in relapsed AML-M5, thereby presenting a new target in the ROS pathway.
In recent years, pro-oxidant therapy has been preferred for front-line treatment as chemotherapy induces apoptosis and tumor regression through ROS elevation. Antioxidant use to minimize oxidative damage and alleviate chemotherapy-induced toxicity has been frowned upon by clinical oncologists owing to controversies on reduced chemotherapy efficacy with antioxidant use. However, many studies support the use of supplemental antioxidants with chemotherapy to enhance the cytotoxicity of chemotherapy against malignant cells, reduce treatment-related toxicities, boost the patients’ health status, and improve treatment response. Therefore, antioxidant supplements should be administered during chemotherapy in AML patients to improve the efficiency of therapy, treatment outcome, and patient survival.
Acknowledgements
We thank Barbara K. Luhila for her graphic expertise and assistance in formatting the figures included in the review.
Abbreviations
- AML
Acute myeloid leukemia
- ALL
Acute lymphoblastic leukemia
- BCR-ABL
Breakpoint cluster region-Abelson
- Bcl-2
B-cell lymphoma 2
- CAT
Catalase
- JAB1/COPS5
C-Jun activation domain-binding protein-1
- CML
Chronic myeloid leukemia
- CKI
Compound kushen injection
- GSH
Glutathione
- HSCs
Hematopoietic stem cells
- HO
Heme oxygenase
- IDH
Isocitrate dehydrogenase
- MtETC
Mitochondrial electron transport chain
- NAC
N-acetylcysteine
- NADPH
Nicotinamide adenine dinucleotide phosphate
- NOX
NADPH oxidase
- OS
Oxidative stress
- ROS
Reactive oxygen species
- SOD
Superoxide dismutase
- Trx
Thioredoxin
- 8-OHG
8-oxoGuanine
Authors’ contributions
NMK performed literature research and review and wrote the final manuscript. SZ conducted literature review and critical review of the manuscript. GJC revised the final manuscript. FZ conceived and revised the final manuscript. The authors read and approved the final manuscript.
Funding
This project was funded by the National Natural Science Foundation of China [grant numbers: 81270597 and 81770179] for leukemia research.
Availability of data and materials
Not applicable.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Take home: Reactive Oxygen Species and Antioxidants are crucial to the pathogenesis and treatment of leukemia. Pro-oxidants induce cell death, whereas antioxidants counteract.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Lau ATY, Wang Y, Chiu J-F. Reactive oxygen species: current knowledge and applications in cancer research and therapeutic. J Cell Biochem. 2008;104(2):657–667. doi: 10.1002/jcb.21655. [DOI] [PubMed] [Google Scholar]
- 2.Zhou F, Shen Q, Claret FX. Novel roles of reactive oxygen species in the pathogenesis of acute myeloid leukemia. J Leukoc Biol. 2013;94(3):423–429. doi: 10.1189/jlb.0113006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Finkel T. Oxidant signals and oxidative stress. Curr Opin Cell Biol. 2003;15(2):247–254. doi: 10.1016/S0955-0674(03)00002-4. [DOI] [PubMed] [Google Scholar]
- 4.Valko M, Leibfritz D, Moncol J, Cronin MTD, Mazur M, Telser J. Free radicals and antioxidants in normal physiological functions and human disease. Int J Biochem Cell Biol. 2007;39(1):44–84. doi: 10.1016/j.biocel.2006.07.001. [DOI] [PubMed] [Google Scholar]
- 5.Udensi UK, Tchounwou PB. Dual effect of oxidative stress on leukemia cancer induction and treatment. J Exp Clin Cancer Res. 2014;33:106. doi: 10.1186/s13046-014-0106-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khoshtabiat L, Mahdavi M, Dehghan G, Rashidi MR. Oxidative stress-induced apoptosis in chronic Myelogenous leukemia K562 cells by an active compound from the Dithio- Carbamate family. Asian Pac J Cancer Prev. 2016;17(9):4267–4273. [PubMed] [Google Scholar]
- 7.Rajeshwari U, Shobha I, Raghunatha R, Andallu B. Oxidative stress and antioxidant status in acute and chronic myeloid Leukemia patients. Open J Blood Dis. 2013;03(03):17–22. doi: 10.4236/ojbd.2013.33A004. [DOI] [Google Scholar]
- 8.De Kouchkovsky I, Abdul-Hay M. Acute myeloid leukemia: a comprehensive review and 2016 update. Blood Cancer J. 2016;6(7):e441. doi: 10.1038/bcj.2016.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Döhner H, Weisdorf DJ, Bloomfield CD. Acute myeloid Leukemia. N Engl J Med. 2015;373(12):1136–1152. doi: 10.1056/NEJMra1406184. [DOI] [PubMed] [Google Scholar]
- 10.Dombret H, Gardin C. An update of current treatments for adult acute myeloid leukemia. Blood. 2016;127(1):53–61. doi: 10.1182/blood-2015-08-604520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Irwin ME, Rivera-Del Valle N, Chandra J. Redox control of leukemia: from molecular mechanisms to therapeutic opportunities. Antioxid Redox Signal. 2013;18(11):1349–1383. doi: 10.1089/ars.2011.4258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Birben E, Sahiner UM, Sackesen C, Erzurum S, Kalayci O. Oxidative stress and antioxidant defense. World Allergy Organ J. 2012;5(1):9–19. doi: 10.1097/WOX.0b013e3182439613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang H, Fang H, Wang K. Reactive oxygen species in eradicating acute myeloid leukemic stem cells. Stem Cell Investig. 2014;1:13. doi: 10.3978/j.issn.2306-9759.2014.04.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Murphy MP. How mitochondria produce reactive oxygen species. Biochem J. 2009;417(1):1–13. doi: 10.1042/BJ20081386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stadtman ER. Role of oxidant species in aging. Curr Med Chem. 2004;11(9):1105–1112. doi: 10.2174/0929867043365341. [DOI] [PubMed] [Google Scholar]
- 16.Bar-Or D, Bar-Or R, Rael LT, Brody EN. Oxidative stress in severe acute illness. Redox Biol. 2015;4:340–345. doi: 10.1016/j.redox.2015.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Inoue M, Sato EF, Nishikawa M, Park A-M, Kira Y, Imada I, et al. Mitochondrial generation of reactive oxygen species and its role in aerobic life. Curr Med Chem. 2003;10(23):2495–2505. doi: 10.2174/0929867033456477. [DOI] [PubMed] [Google Scholar]
- 18.Ames BN, Shigenaga MK, Hagen TM. Oxidants, antioxidants, and the degenerative diseases of aging. Proc Natl Acad Sci U S A. 1993;90(17):7915. doi: 10.1073/pnas.90.17.7915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Conner EM, Grisham MB. Inflammation, free radicals, and antioxidants. Nutrition. 1996;12(4):274–277. doi: 10.1016/S0899-9007(96)00000-8. [DOI] [PubMed] [Google Scholar]
- 20.Valko M, Izakovic M, Mazur M, Rhodes CJ, Telser J. Role of oxygen radicals in DNA damage and cancer incidence. Mol Cell Biochem. 2004;266(1–2):37–56. doi: 10.1023/B:MCBI.0000049134.69131.89. [DOI] [PubMed] [Google Scholar]
- 21.Church DF, Pryor WA. Free-radical chemistry of cigarette smoke and its toxicological implications. Environ Health Perspect. 1985;64:111–126. doi: 10.1289/ehp.8564111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Matthay MA, Geiser T, Matalon S, Ischiropoulos H. Oxidant-mediated lung injury in the acute respiratory distress syndrome. Crit Care Med. 1999;27(9):2028–2030. doi: 10.1097/00003246-199909000-00055. [DOI] [PubMed] [Google Scholar]
- 23.Liguori I, Russo G, Curcio F, Bulli G, Aran L, Della-Morte D, et al. Oxidative stress, aging, and diseases. Clin Interv Aging. 2018;13:757–772. doi: 10.2147/CIA.S158513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang J, Lei W, Chen X, Wang S, Qian W. Oxidative stress response induced by chemotherapy in leukemia treatment. Mol Clin Oncol. 2018;8(3):391–399. doi: 10.3892/mco.2018.1549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kudryavtseva AV, Krasnov GS, Dmitriev AA, Alekseev BY, Kardymon OL, Sadritdinova AF, et al. Mitochondrial dysfunction and oxidative stress in aging and cancer. Oncotarget. 2016;7(29):44879. doi: 10.18632/oncotarget.9821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ayala A, Muñoz MF, Argüelles S. Lipid peroxidation: production, metabolism, and signaling mechanisms of malondialdehyde and 4-Hydroxy-2-Nonenal. Oxid Med Cell Longev. 2014;2014:360438. doi: 10.1155/2014/360438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Esterbauer H, Eckl P, Ortner A. Possible mutagens derived from lipids and lipid precursors. Mutat Res. 1990;238(3):223–233. doi: 10.1016/0165-1110(90)90014-3. [DOI] [PubMed] [Google Scholar]
- 28.Singh RK, Tripathi AK, Tripathi P, Singh S, Singh R, Ahmad R. Studies on biomarkers for oxidative stress in patients with chronic myeloid leukemia. Hematol Oncol Stem Cell Ther. 2009;2(1):285–288. doi: 10.1016/S1658-3876(09)50039-8. [DOI] [PubMed] [Google Scholar]
- 29.Zarkovic N. 4-hydroxynonenal as a bioactive marker of pathophysiological processes. Mol Aspects Med. 2003;24(4–5):281–291. doi: 10.1016/S0098-2997(03)00023-2. [DOI] [PubMed] [Google Scholar]
- 30.Pizzimenti S, Ciamporcero E, Daga M, Pettazzoni P, Arcaro A, Cetrangolo G, et al. Interaction of aldehydes derived from lipid peroxidation and membrane proteins. Front Physiol. 2013;4:242. doi: 10.3389/fphys.2013.00242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dehennaut V, Loison I, Dubuissez M, Nassour J, Abbadie C, Leprince D. DNA double-strand breaks Lead to activation of Hypermethylated in cancer 1 (HIC1) by SUMOylation to regulate DNA repair. J Biol Chem. 2013;288(15):10254–10264. doi: 10.1074/jbc.M112.421610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhou BB, Elledge SJ. The DNA damage response: putting checkpoints in perspective. Nature. 2000;408(6811):433–439. doi: 10.1038/35044005. [DOI] [PubMed] [Google Scholar]
- 33.Caldecott KW. Single-strand break repair and genetic disease. Nat Rev Genet. 2008;9(8):619–631. doi: 10.1038/nrg2380. [DOI] [PubMed] [Google Scholar]
- 34.Richter C, Park JW, Ames BN. Normal oxidative damage to mitochondrial and nuclear DNA is extensive. Proc Natl Acad Sci U S A. 1988;85(17):6465–6467. doi: 10.1073/pnas.85.17.6465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shibutani S, Takeshita M, Grollman AP. Insertion of specific bases during DNA synthesis past the oxidation-damaged base 8-oxodG. Nature. 1991;349(6308):431–434. doi: 10.1038/349431a0. [DOI] [PubMed] [Google Scholar]
- 36.VALAVANIDIS A, VLACHOGIANNI T, FIOTAKIS C. 8-hydroxy-2′ -deoxyguanosine (8-OHdG): a critical biomarker of oxidative stress and carcinogenesis. J Environ Sci Health C. 2009;27(2):120–139. doi: 10.1080/10590500902885684. [DOI] [PubMed] [Google Scholar]
- 37.Tsamesidis I, Pantaleo A, Pekou A, Gusani A, Iliadis S, Makedou K, et al. Correlation of oxidative stress biomarkers and hematological parameters in blood cancer patients from Sardinia, Italy. Int J Hematol Oncol Stem Cell Res. 2019;13(2):49–57. [PMC free article] [PubMed] [Google Scholar]
- 38.Hlavackova A, Vydra J, Chrastinova L, Kotlin R, Stikarova J, Suttnar J, et al. Alteration of serum malondialdehyde level as biomarker of oxidative stress during acute myeloid Leukemia treatment. Blood. 2019;134(Supplement_1):5181. doi: 10.1182/blood-2019-122303. [DOI] [Google Scholar]
- 39.Battisti V, Maders LDK, Bagatini MD, Santos KF, Spanevello RM, Maldonado PA, et al. Measurement of oxidative stress and antioxidant status in acute lymphoblastic leukemia patients. Clin Biochem. 2008;41(7–8):511–518. doi: 10.1016/j.clinbiochem.2008.01.027. [DOI] [PubMed] [Google Scholar]
- 40.Hole PS, Darley RL, Tonks A. Do reactive oxygen species play a role in myeloid leukemias? Blood. 2011;117(22):5816–5826. doi: 10.1182/blood-2011-01-326025. [DOI] [PubMed] [Google Scholar]
- 41.Hole PS, Zabkiewicz J, Munje C, Newton Z, Pearn L, White P, et al. Overproduction of NOX-derived ROS in AML promotes proliferation and is associated with defective oxidative stress signaling. Blood. 2013;122(19):3322–3330. doi: 10.1182/blood-2013-04-491944. [DOI] [PubMed] [Google Scholar]
- 42.Wiseman H, Halliwell B. Damage to DNA by reactive oxygen and nitrogen species: role in inflammatory disease and progression to cancer. Biochem J. 1996;313(Pt 1):17–29. doi: 10.1042/bj3130017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Miki H, Funato Y. Regulation of intracellular signalling through cysteine oxidation by reactive oxygen species. J Biochem. 2012;151(3):255–261. doi: 10.1093/jb/mvs006. [DOI] [PubMed] [Google Scholar]
- 44.Jitschin R, Hofmann AD, Bruns H, Gießl A, Bricks J, Berger J, et al. Mitochondrial metabolism contributes to oxidative stress and reveals therapeutic targets in chronic lymphocytic leukemia. Blood. 2014;123(17):2663–2672. doi: 10.1182/blood-2013-10-532200. [DOI] [PubMed] [Google Scholar]
- 45.Sillar JR, Germon ZP, De Iuliis GN, Dun MD. The role of reactive oxygen species in acute myeloid leukaemia. Int J Mol Sci. 2019;20(23):6003. doi: 10.3390/ijms20236003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Forte D, Krause DS, Andreeff M, Bonnet D, Méndez-Ferrer S. Updates on the hematologic tumor microenvironment and its therapeutic targeting. Haematologica. 2019;104(10):1928–1934. doi: 10.3324/haematol.2018.195396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Snezhkina AV, Kudryavtseva AV, Kardymon OL, Savvateeva MV, Melnikova NV, Krasnov GS, et al. ROS generation and antioxidant defense Systems in Normal and Malignant Cells. Oxid Med Cell Longev. 2019;2019:1–17. doi: 10.1155/2019/6175804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Abooali M, Lall GS, Coughlan K, Lall HS, Gibbs BF, Sumbayev VV. Crucial involvement of xanthine oxidase in the intracellular signalling networks associated with human myeloid cell function. srep. 2014;4:6307. doi: 10.1038/srep06307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zhou F-L, Zhang W-G, Wei Y-C, Meng S, Bai G-G, Wang B-Y, et al. Involvement of oxidative stress in the relapse of acute myeloid leukemia. J Biol Chem. 2010;285(20):15010. doi: 10.1074/jbc.M110.103713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bernard MP, Bancos S, Sime PJ, Phipps RP. Targeting cyclooxygenase-2 in hematological malignancies: rationale and promise. Curr Pharm Des. 2008;14(21):2051–2060. doi: 10.2174/138161208785294654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chang Y-T, Hernandez D, Alonso S, Gao M, Su M, Ghiaur G, et al. Role of CYP3A4 in bone marrow microenvironment–mediated protection of FLT3/ITD AML from tyrosine kinase inhibitors. Blood Adv. 2019;3(6):908. doi: 10.1182/bloodadvances.2018022921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Su M. Role of cytochrome P450 enzymes in acute myeloid Leukemia bone marrow microenvironment. 2017. [Google Scholar]
- 53.Nowicki MO, Falinski R, Koptyra M, Slupianek A, Stoklosa T, Gloc E, et al. BCR/ABL oncogenic kinase promotes unfaithful repair of the reactive oxygen species-dependent DNA double-strand breaks. Blood. 2004;104(12):3746–3753. doi: 10.1182/blood-2004-05-1941. [DOI] [PubMed] [Google Scholar]
- 54.Koptyra M, Falinski R, Nowicki MO, Stoklosa T, Majsterek I, Nieborowska-Skorska M, et al. BCR/ABL kinase induces self-mutagenesis via reactive oxygen species to encode imatinib resistance. Blood. 2006;108(1):319–327. doi: 10.1182/blood-2005-07-2815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kindler T, Lipka DB, Fischer T. FLT3 as a therapeutic target in AML: still challenging after all these years. Blood. 2010;116(24):5089–5102. doi: 10.1182/blood-2010-04-261867. [DOI] [PubMed] [Google Scholar]
- 56.Sallmyr A, Fan J, Datta K, Kim K-T, Grosu D, Shapiro P, et al. Internal tandem duplication of FLT3 (FLT3/ITD) induces increased ROS production, DNA damage, and misrepair: implications for poor prognosis in AML. Blood. 2008;111(6):3173–3182. doi: 10.1182/blood-2007-05-092510. [DOI] [PubMed] [Google Scholar]
- 57.Hole PS, Pearn L, Tonks AJ, James PE, Burnett AK, Darley RL, et al. Ras-induced reactive oxygen species promote growth factor-independent proliferation in human CD34+ hematopoietic progenitor cells. Blood. 2010;115(6):1238–1246. doi: 10.1182/blood-2009-06-222869. [DOI] [PubMed] [Google Scholar]
- 58.Maraldi T, Prata C, Vieceli Dalla Sega F, Caliceti C, Zambonin L, Fiorentini D, et al. NAD(P) H oxidase isoform Nox2 plays a prosurvival role in human leukaemia cells. Free Radic Res. 2009;43(11):1111–1121. doi: 10.1080/10715760903186132. [DOI] [PubMed] [Google Scholar]
- 59.Lagadinou ED, Sach A, Callahan K, Rossi RM, Neering SJ, Minhajuddin M, et al. BCL-2 inhibition targets oxidative phosphorylation and selectively eradicates quiescent human leukemia stem cells. Cell Stem Cell. 2013;12(3):329–341. doi: 10.1016/j.stem.2012.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Um H-D. Bcl-2 family proteins as regulators of cancer cell invasion and metastasis: a review focusing on mitochondrial respiration and reactive oxygen species. Oncotarget. 2016;7(5):5193–5203. doi: 10.18632/oncotarget.6405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Patel KP, Ravandi F, Ma D, Paladugu A, Barkoh BA, Medeiros LJ, et al. Acute myeloid leukemia with IDH1 or IDH2 mutations: frequency and Clinicopathologic features. Am J Clin Pathol. 2011;135(1):35–45. doi: 10.1309/AJCPD7NR2RMNQDVF. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Reitman ZJ, Sinenko SA, Spana EP, Yan H. Genetic dissection of leukemia-associated IDH1 and IDH2 mutants and D-2-hydroxyglutarate in drosophila. Blood. 2015;125(2):336–345. doi: 10.1182/blood-2014-05-577940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Cairns RA, Mak TW. Oncogenic Isocitrate dehydrogenase mutations: mechanisms, models, and clinical opportunities. Cancer Discov. 2013;3(7):730–741. doi: 10.1158/2159-8290.CD-13-0083. [DOI] [PubMed] [Google Scholar]
- 64.Liu G, Claret FX, Zhou F, Pan Y. Jab1/COPS5 as a novel biomarker for diagnosis, prognosis, therapy prediction and therapeutic tools for human cancer. Front Pharmacol. 2018;9:135. doi: 10.3389/fphar.2018.00135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Shackleford TJ, Claret FX. JAB1/CSN5: a new player in cell cycle control and cancer. Cell Div. 2010;5:26. doi: 10.1186/1747-1028-5-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Bae M-K, Ahn M-Y, Jeong J-W, Bae M-H, Lee YM, Bae S-K, et al. Jab1 interacts directly with HIF-1alpha and regulates its stability. J Biol Chem. 2002;277(1):9–12. doi: 10.1074/jbc.C100442200. [DOI] [PubMed] [Google Scholar]
- 67.Guo Z, Wang Y, Zhao Y, Shu Y, Liu Z, Zhou H, et al. The pivotal oncogenic role of Jab1/CSN5 and its therapeutic implications in human cancer. Gene. 2019;687:219–227. doi: 10.1016/j.gene.2018.11.061. [DOI] [PubMed] [Google Scholar]
- 68.Zhou F, Pan Y, Wei Y, Zhang R, Bai G, Shen Q, et al. Jab1/Csn5-thioredoxin signaling in relapsed acute monocytic leukemia under oxidative stress. Clin Cancer Res. 2017;23(15):4450–4461. doi: 10.1158/1078-0432.CCR-16-2426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Sentürker S, Karahalil B, Inal M, Yilmaz H, Müslümanoglu H, Gedikoglu G, et al. Oxidative DNA base damage and antioxidant enzyme levels in childhood acute lymphoblastic leukemia. FEBS Lett. 1997;416(3):286–290. doi: 10.1016/S0014-5793(97)01226-X. [DOI] [PubMed] [Google Scholar]
- 70.Oltra AM, Carbonell F, Tormos C, Iradi A, Sáez GT. Antioxidant enzyme activities and the production of MDA and 8-oxo-dG in chronic lymphocytic leukemia. Free Radic Biol Med. 2001;30(11):1286–1292. doi: 10.1016/S0891-5849(01)00521-4. [DOI] [PubMed] [Google Scholar]
- 71.Mense SM, Zhang L. Heme: a versatile signaling molecule controlling the activities of diverse regulators ranging from transcription factors to MAP kinases. Cell Res. 2006;16(8):681–692. doi: 10.1038/sj.cr.7310086. [DOI] [PubMed] [Google Scholar]
- 72.Heasman S-A, Zaitseva L, Bowles KM, Rushworth SA, MacEwan DJ. Protection of acute myeloid leukaemia cells from apoptosis induced by front-line chemotherapeutics is mediated by haem oxygenase-1. Oncotarget. 2011;2(9):658–668. doi: 10.18632/oncotarget.321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Mayerhofer M, Florian S, Krauth M-T, Aichberger KJ, Bilban M, Marculescu R, et al. Identification of Heme Oxygenase-1 as a novel BCR/ABL-dependent survival factor in chronic myeloid leukemia. Cancer Res. 2004;64(9):3148–3154. doi: 10.1158/0008-5472.CAN-03-1200. [DOI] [PubMed] [Google Scholar]
- 74.Nishiura T, Suzuki K, Kawaguchi T, Nakao H, Kawamura N, Taniguchi M, et al. Elevated serum manganese superoxide dismutase in acute leukemias. Cancer Lett. 1992;62(3):211–215. doi: 10.1016/0304-3835(92)90098-G. [DOI] [PubMed] [Google Scholar]
- 75.Huang P, Feng L, Oldham EA, Keating MJ, Plunkett W. Superoxide dismutase as a target for the selective killing of cancer cells. Nature. 2000;407(6802):390–395. doi: 10.1038/35030140. [DOI] [PubMed] [Google Scholar]
- 76.Kos Z, Pavelić L, Pekić B, Pavelić K. Reversal of human myeloid leukemia cells into normal granulocytes and macrophages: activity and intracellular distribution of catalase. Oncology. 1987;44(4):245–247. doi: 10.1159/000226487. [DOI] [PubMed] [Google Scholar]
- 77.Coe E, Schimmer AD. Catalase activity and arsenic sensitivity in acute leukemia. Leuk Lymphoma. 2008;49(10):1976–1981. doi: 10.1080/10428190802353617. [DOI] [PubMed] [Google Scholar]
- 78.Maung ZT, Hogarth L, Reid MM, Proctor SJ, Hamilton PJ, Hall AG. Raised intracellular glutathione levels correlate with in vitro resistance to cytotoxic drugs in leukaemic cells from patients with acute lymphoblastic leukemia. Leukemia. 1994;8(9):1487–1491. [PubMed] [Google Scholar]
- 79.Xie W, Ma W, Liu P, Zhou F. Overview of thioredoxin system and targeted therapies for acute leukemia. Mitochondrion. 2019;47:38–46. doi: 10.1016/j.mito.2019.04.010. [DOI] [PubMed] [Google Scholar]
- 80.Collet J-F, Messens J. Structure, function, and mechanism of thioredoxin proteins. Antioxid Redox Signal. 2010;13(8):1205–1216. doi: 10.1089/ars.2010.3114. [DOI] [PubMed] [Google Scholar]
- 81.Robak T, Wierzbowska A. Current and emerging therapies for acute myeloid leukemia. Clin Ther. 2009;31(Pt 2):2349–2370. doi: 10.1016/j.clinthera.2009.11.017. [DOI] [PubMed] [Google Scholar]
- 82.Iacobini M, Menichelli A, Palumbo G, Multari G, Werner B, Del Principe D. Involvement of oxygen radicals in cytarabine-induced apoptosis in human polymorphonuclear cells. Biochem Pharmacol. 2001;61(8):1033–1040. doi: 10.1016/S0006-2952(01)00548-2. [DOI] [PubMed] [Google Scholar]
- 83.Groninger E, Meeuwsen-De Boer GJ, De Graaf SSN, Kamps WA, De Bont ESJM. Vincristine induced apoptosis in acute lymphoblastic leukaemia cells: a mitochondrial controlled pathway regulated by reactive oxygen species? Int J Oncol. 2002;21(6):1339–1345. doi: 10.3892/ijo.21.6.1339. [DOI] [PubMed] [Google Scholar]
- 84.Minotti G, Menna P, Salvatorelli E, Cairo G, Gianni L. Anthracyclines: molecular advances and pharmacologic developments in antitumor activity and cardiotoxicity. Pharmacol Rev. 2004;56(2):185–229. doi: 10.1124/pr.56.2.6. [DOI] [PubMed] [Google Scholar]
- 85.Wang J, Li L, Cang H, Shi G, Yi J. NADPH oxidase-derived reactive oxygen species are responsible for the high susceptibility to arsenic cytotoxicity in acute promyelocytic leukemia cells. Leuk Res. 2008;32(3):429–436. doi: 10.1016/j.leukres.2007.06.006. [DOI] [PubMed] [Google Scholar]
- 86.Noguera NI, Pelosi E, Angelini DF, Piredda ML, Guerrera G, Piras E, et al. High-dose ascorbate and arsenic trioxide selectively kill acute myeloid leukemia and acute promyelocytic leukemia blasts in vitro. Oncotarget. 2017;8(20):32550–32565. doi: 10.18632/oncotarget.15925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Petruccelli LA, Dupéré-Richer D, Pettersson F, Retrouvey H, Skoulikas S, Miller WH., Jr Vorinostat induces reactive oxygen species and DNA damage in acute myeloid leukemia cells. PLoS One. 2011;6(6):e20987. doi: 10.1371/journal.pone.0020987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Liesveld JL, Rosell KE, Bechelli J, Lu C, Messina P, Mulford D, et al. Proteasome inhibition in Myelodysplastic syndromes and acute Myelogenous leukemia cell lines. Cancer Invest. 2011;29(7):439–450. doi: 10.3109/07357907.2011.590567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Maiti AK. Gene network analysis of oxidative stress-mediated drug sensitivity in resistant ovarian carcinoma cells. Pharmacogenomics J. 2010;10(2):94–104. doi: 10.1038/tpj.2009.49. [DOI] [PubMed] [Google Scholar]
- 90.Trachootham D, Alexandre J, Huang P. Targeting cancer cells by ROS-mediated mechanisms: a radical therapeutic approach? Nat Rev Drug Discov. 2009;8(7):579–591. doi: 10.1038/nrd2803. [DOI] [PubMed] [Google Scholar]
- 91.D’Andrea GM. Use of antioxidants during chemotherapy and radiotherapy should be avoided. CA Cancer J Clin. 2005;55(5):319–321. doi: 10.3322/canjclin.55.5.319. [DOI] [PubMed] [Google Scholar]
- 92.Block KI, Koch AC, Mead MN, Tothy PK, Newman RA, Gyllenhaal C. Impact of antioxidant supplementation on chemotherapeutic toxicity: a systematic review of the evidence from randomized controlled trials. Int J Cancer. 2008;123(6):1227–1239. doi: 10.1002/ijc.23754. [DOI] [PubMed] [Google Scholar]
- 93.Simone CB, Simone NL, Simone V, Simone CB. Antioxidants and other nutrients do not interfere with chemotherapy or radiation therapy and can increase kill and increase survival, part 2. Altern Ther Health Med. 2007;13(2):40–47. [PubMed] [Google Scholar]
- 94.Singh K, Bhori M, Kasu YA, Bhat G, Marar T. Antioxidants as precision weapons in war against cancer chemotherapy induced toxicity – exploring the armoury of obscurity. Saudi Pharmaceutical J. 2018;26(2):177. doi: 10.1016/j.jsps.2017.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Mokhtari RB, Homayouni TS, Baluch N, Morgatskaya E, Kumar S, Das B, et al. Combination therapy in combating cancer. Oncotarget. 2017;8(23):38022–38043. doi: 10.18632/oncotarget.16723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Nakayama A, Alladin KP, Igbokwe O, White JD. Systematic review: generating evidence-based guidelines on the concurrent use of dietary antioxidants and chemotherapy or radiotherapy. Cancer Invest. 2011;29(10):655. doi: 10.3109/07357907.2011.626479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Gaman AM, Buga A-M, Gaman M-A, Popa-Wagner A. The role of oxidative stress and the effects of antioxidants on the incidence of infectious complications of chronic lymphocytic leukemia. Oxid Med Cell Longev. 2014;2014:158135. doi: 10.1155/2014/158135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Jin Y, Yang Q, Liang L, Ding L, Liang Y, Zhang D, et al. Compound kushen injection suppresses human acute myeloid leukaemia by regulating the Prdxs/ROS/Trx1 signalling pathway. J Exp Clin Cancer Res. 2018;37:277. doi: 10.1186/s13046-018-0948-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Garcia JS, Huang M, Medeiros BC, Mitchell BS. Selective toxicity of investigational Ixazomib for human leukemia cells expressing mutant cytoplasmic NPM1: role of reactive oxygen species. Clin Cancer Res. 2016;22(8):1978–1988. doi: 10.1158/1078-0432.CCR-15-1440. [DOI] [PubMed] [Google Scholar]
- 100.Shih W-L, Chang C-D, Chen H-T, Fan K-K. Antioxidant activity and leukemia initiation prevention in vitro and in vivo by N-acetyl-L-cysteine. Oncol Lett. 2018;16(2):2046–2052. doi: 10.3892/ol.2018.8864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Kennedy DD, Tucker KL, Ladas ED, Rheingold SR, Blumberg J, Kelly KM. Low antioxidant vitamin intakes are associated with increases in adverse effects of chemotherapy in children with acute lymphoblastic leukemia. Am J Clin Nutr. 2004;79(6):1029–1036. doi: 10.1093/ajcn/79.6.1029. [DOI] [PubMed] [Google Scholar]
- 102.Kelkel M, Jacob C, Dicato M, Diederich M. Potential of the dietary antioxidants resveratrol and Curcumin in prevention and treatment of hematologic malignancies. Molecules. 2010;15(10):7035–7074. doi: 10.3390/molecules15107035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Rafiq S, Raza MH, Younas M, Naeem F, Adeeb R, Iqbal J, et al. Molecular targets of Curcumin and future therapeutic role in leukemia. J Biosci Med. 2018;6(4):33–50. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.