Abstract
Cancer-associated fibroblasts (CAFs) are the key component of tumor stromal. High heterogeneity of CAFs reflects in their origin, phenotype and function. Biological function which can be suggested by biomarkers of distinct CAF subgroups may be different, even opposite, just like water and fire. Identifying CAF subpopulations expressing different biomarkers and reconciling the relationship of the “water and fire” among distinct CAF subsets may be a breakthrough in tumor therapy. Herein, we briefly summarize the biomarkers commonly used or newly identified for distinct CAFs in terms of their features and potential clinical benefits.
Keywords: Biomarker, Cancer-associated fibroblasts, Heterogeneity
As the most abundant and main component in the tumor microenvironment (TME), cancer-associated fibroblasts (CAFs) are generally considered as all the fibroblasts found within and surrounding tumor tissues, which are activated from normal resident tissue fibroblasts or transdifferentiated from non-fibroblastic lineage such as epithelial cells and adipocytes due to the stimulation of TME [1, 2]. CAFs were thought to be tumor-promoting by building up and remodeling extracellular matrix (ECM). However, latest study revealed the extensive inter- and intra-organ heterogeneity of fibroblasts in the physiological context [3], and several preclinical studies attempted to target CAFs directly in mouse models also failed [4, 5]. These evidences suggest an obvious heterogeneity of CAFs which may harbor both tumor-promoting and anti-tumor properties.
Traditional CAF biomarkers such as α-smooth muscle actin (α-SMA), fibroblast activation protein (FAP), S100A4, platelet-derived growth factor receptors (PDGFRα/β) or vimentin have been well-studied despite none of them are specific to CAFs (Table 1) [6]. Moreover, increasing CAF subsets with distinct biomarkers expression and different cellular functions have been identified recently. We here briefly outline the biomarkers for identifying CAF heterogeneity and potential therapeutic targets.
Table 1.
List of commonly used biomarkers for CAFs
| Marker | Cell origin | Biological effects | Effects on tumors | Clinical application |
|---|---|---|---|---|
| Neutral biomarkers with dual functions | ||||
| α-SMA | Normal fibroblasts, quiescent stellate cells, smooth muscle cells | Cell contractility, structure and integrity, desmoplasia | Tumor proliferation, immunosuppressive; protection mechanism, impeding drug delivery | Preclinical trials by targeting α-SMA directly failed; prognostic indicator |
| S100A4 | Normal fibroblasts, epithelial cells, endothelial cells | Cell motility, tissue fibrosis | Promoting metastasis, immune evasion; immune surveillance and response | Unknown |
| Accomplices: pro-tumorigenesis biomarkers | ||||
| FAP | Normal fibroblasts, quiescent stellate cells, CD45+ immune cells | ECM remodeling, fibrogenesis, serine protease activity | Tumor progression and metastasis, shaping the immunosuppressive TME | Preclinical trials (antibody, inhibitor, DNA vaccination, oncolytic adenovirus, CAR-T); phase II clinical trials (PT-100, sibrotuzumab) failed; prognostic indicator |
| PDGFRα/β | Normal fibroblasts, vascular smooth muscle cells, pericytes | Receptor tyrosine kinase activity | Immunomodulation, M2 polarization, angiogenesis | Dasatinib normalizes CAFs; targeting Saa3 in PDGFRα+ CAFs; prognostic indicator |
| PDPN | Endothelial cells | Cell motility and adhesion | Immunosuppressive | Unknown |
| CD70 | T and B lymphocytes, mature dendritic cells | T cell function regulation | Immunosuppressive, tumor cell migration, T cell exhaustion | Prognostic indicator |
| Vimentin | Epithelial cells, endothelial cells | Cell motility, structure and integrity | Tumor invasion | Unknown |
| GPR77 | Polymorphonuclear neutrophils | Complement activation, pro-inflammatory signaling | Sustaining cancer stemness, cancer formation, chemoresistance | Neutralizing anti-GPR77 antibody abolishes tumor formation in a PDX model |
| CD10 | BMSCs, pre-B lymphocytes | Metalloendoprotease | Sustaining cancer stemness, cancer formation, chemoresistance | Unknown |
| CD74 | Normal fibroblasts, monocytes/macrophages, epithelial cells | MHC II chaperone, protein trafficking | Immunomodulation | Unknown |
| Defenders: tumor-suppressive biomarkers | ||||
| CD146 | Endothelial cells | Cell adhesion | Maintaining ER expression, sensitive to tamoxifen | Prognostic indicator; Considered as a drug? |
| CAV1 | Normal fibroblasts, endothelial cells, adipocytes | Structure component, cell signaling and transport | CAV1low associated with poor prognosis | Prognostic indicator |
| Saa3− | Smooth muscle cells, adipocytes | Collagenase production | PDGFRα+Saa3− CAF impairing tumor proliferation | Targeting Saa3 in PDGFRα+ CAF; prognostic indicator |
CAFs isolation and characterization
CAFs can be easily digested and cultured on plastic flasks, whereas other types of cells not, which is the basis of CAFs isolation [7]. Briefly, obtained tumor tissues are minced into small pieces about 1 mm and then digested at 37 °C with shaking. Usage of gentle tissue dissociators may improve separation efficiency. For digestion, diverse collagenases, trypsin, hyaluronidase and dispase can be used alone or combined. The cells acquired are filtered through cell strainers and then planted in culture plates. Breast tumor tissues are usually incubated at room temperature for 5 min without shocking after digestion. Red blood cell lysis buffer is optional.
The primary CAFs should be negative for epithelial (EpCAM), endothelial (CD31) and leukocyte (CD45) with an elongated spindle-like morphology [1]. In practice, traditional CAF biomarkers are typically combined with lineage exclusion to identify CAFs. Notably, the passage number of cultured CAFs between 1 to 6 is suitable for experiments.
Neutral biomarkers with dual functions
α-SMA: a snapshot of CAF heterogeneity
As the marker of activated fibroblasts, α-SMA, a cytoskeletal protein associated with TGF-β production and highly contractile phenotype, is the first identified and most frequent CAF biomarker [8, 9]. Studies have verified that α-SMA+ CAFs could promote tumor progression, confer therapeutic resistance and mediate immunosuppressive TME in multiple ways, such as paracrine and ECM remodeling [2, 10, 11].
However, depleting α-SMA+ CAFs directly has been failed to treat pancreatic ductal adenocarcinoma (PDAC) in murine models, probably due to the immune surveillance suppression [4]. Patients with high desmoplasia defined by expression of collagen I and CAF markers including α-SMA have better prognosis in PDAC, breast and lung cancer patients [12, 13]. These results show that the fibrotic response of α-SMA+ CAFs may be a host protection mechanism against tumor progression, which needs further investigation.
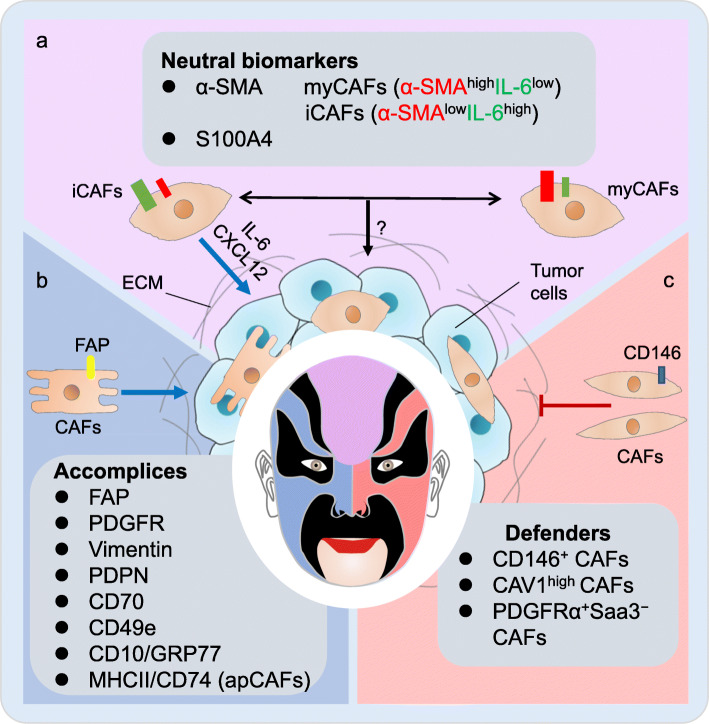
The contradictory conclusions above indicate the α-SMA+ CAF heterogeneity which has been confirmed in a recent study classifying different subtypes of α-SMA+ CAFs. Typically, inflammatory CAFs (iCAFs) being α-SMAlowIL-6high are identified in PDAC and located more distantly from neoplastic cells than α-SMAhighIL-6low myofibroblastic CAFs (myCAFs) (Fig. 1a). ICAFs appear to be more tumor-promoting than myCAFs by producing chemokines and cytokines [14] and indicate a higher malignancy in pancreatic tumorigenesis [15]. On the other hand, myCAFs may deposit ECM extensively to impede drug delivery despite less cancer-stimulating [16]. Considering the biological effects of myCAFs and iCAFs, the composition of myCAFs and iCAFs in the TME may have different implications for treatment. High iCAF content may indicate a higher degree of malignancy, while high myCAF content may indicate a poor response to treatment.
Fig. 1.
The “double face” of cancer-associated fibroblasts (CAFs). CAF subsets identified by different biomarkers play distinct roles in tumor microenvironment. a, several studies have shown that CAFs expressing α-SMA or S100A4, which are considered tumorigenic previously, are also potentially anti-tumor. Identification of myCAFs and iCAFs among α-SMA+ CAFs may represent an aspect of CAF heterogeneity, which is believed that two subsets can convert into each other. b, most biomarkers represent tumor-promoting CAFs including traditional CAF biomarkers (FAP, PDGFR, Vimentin, PDPN and CD70) as well as some newly identified markers (CD49e, CD10/GRP77 and MHCII/CD74). c, CD146+ CAFs, CAV1high CAFs and PDGFRα+Saa3− have been identified as tumor-suppressive CAF subsets
Accordingly, combination of reducing the upstream formation of iCAFs with inhibiting the downstream desmoplasia derived from myCAFs may design the treatment strategy. Furthermore, IL-1/JAK/STAT signaling cascades and TGF-β have been found involved in the formation and mutual transformation of these two CAF subtypes. JAK inhibitors can suppress tumor growth as well as shift iCAFs to myCAFs while TGFBR inhibition could partially attenuate the function of myCAFs without influencing tumor growth [16]. Patients might benefit from combination therapy of these two drugs. Altogether, classification of α-SMA+ CAFs deepens our understanding of CAF heterogeneity as well as provides new ideas for CAF targeted therapy which remains further study.
Bidirectional roles of S100A4
S100A4, also called fibroblast-specific protein-1, is usually expressed on CAFs transited from epithelial or endothelial cells [17, 18]. However, the biological effects of S100A4+ CAFs are controversial (Fig. 1a). S100A4+ CAFs promote tumor metastasis through secretion of VEGF- A and Tenascin-C [19]. Chemokine ligand 2 (CCL2) derived from S100A4+ CAFs contributes to immune evasion by maintaining macrophage infiltration [20]. On the other hand, fibroblasts expressing S100A4 can product collagen and encapsulate carcinogens to enhance immune surveillance ability [21]. α-SMA+S100A4+ CAFs can activate tumor immune response by promoting CD8+ T cell activation through fusion with dendritic cells [20]. These findings confirmed the CAF heterogeneity, and S100A4+ CAFs remain further characterization.
Accomplices: pro-tumorigenesis biomarkers
FAP: a promising therapeutic target
FAP is another wide-spread biomarker for CAFs, as well as a serine protease participating in ECM remodeling and fibrogenesis, thereby accelerating tumor progression [22]. FAP+ CAFs can shape the immunosuppressive TME by secreting distinct chemokines and cytokines [2]. A recent study in ovarian cancer found that FAPhigh CAFs are correlated with poor patient outcomes [23].
So far, FAP might be one of the most promising therapeutic targets of CAFs. In distinct murine tumor models, multiple strategies targeting FAP exhibited therapeutic effects, including genetic deletion [24], pharmacological inhibition (PT630, PT-100) [25, 26], a novel monoclonal antibody (mAb) FAP5-DM1 [27], conditional ablation of FAP+ CAFs using diphtheria toxin [28] or αFAP-PE38 [29], and even novel FAP-targeting immunotherapies such as DNA vaccination [30], chimeric antigen receptor (CAR) T cells [31, 32] or oncolytic adenovirus [33, 34].
However, sibrotuzumab, a FAP-specific antibody, which has been found clinically safe and effective in a phase I trial of advanced cancers, showed no beneficial effect in a phase II trial of metastatic colorectal cancer [35–37]. Another phase II trial utilizing PT-100 in metastatic colorectal cancer also failed [38]. It is noted that the patients involved in both of these phase II trials were heavily pre-treated and represented a refractory patient population, which may account for the failure. FAP may probably contribute more in the earlier-stage tumors rather than late-stage metastasis [39]. Nevertheless, FAP is still the most promising CAF therapeutic target and more exploration is needed.
Other traditional biomarkers: PDGFR, Vimentin, PDPN and CD70
PDGFRα/β are both upregulated in multiple tumors [40], and PDGFRβ is correlated with poor survival in breast cancer [41]. PDGFRα/β+ CAFs participate in immunomodulation by inducing macrophage migration and M2 polarization [2]. Blocking PDGFR signaling can suppress angiogenesis and tumor growth in human cervical cancer [42]. Furthermore, a PDGFR inhibitor, Dasatinib can partially reverse the pro-tumorigenic CAFs of lung adenocarcinoma (LUAD) to a quiescent state [43], which might be a potential treatment strategy for LUAD.
Vimentin is a biomarker for epithelial-to-mesenchymal transition (EMT) maintaining structure and motility during cell migration [44], involved in CAF motility to lead cell invasion in LUAD [45]. Podoplanin (PDPN)+ CAFs in LUAD have been reported as the inducer of immunosuppressive microenvironment [46]. Moreover, CAFs expressing CD70 enrich regulatory T cells to invasive colorectal cancer and CD70 expression is negatively correlated with survival of patients with colorectal cancer (Fig. 1b) [47]. PDPN seems to be a potential therapeutic target while CD70 and vimentin might be more suitable for prognostic indicators and more evidences are warranted.
Defenders: tumor-suppressive biomarkers
The potential anti-tumor function of CAFs exhibits when we attempt to inhibit hedgehog pathway which has been proved to activate fibroblasts [48–50], indicating the existence of tumor-suppressive CAF subsets. Studies on CAF heterogeneity has identified several potential anti-tumor CAF subpopulations and biomarkers (Fig. 1c).
CD146 expression is found to distinguish at least two CAF subpopulations in ER+ breast cancer, among which CD146+ CAFs could promote tamoxifen sensitivity by continuously expressing ER, whereas CD146− CAFs opposite [51]. Another stroma-derived gene expression signature of breast tumor shows that CAV1low CAFs are correlated with poor prognosis [52]. Serum amyloid A3 (Saa3) is also identified as new biomarker of mouse PDGFRα+ CAFs in PDAC, as PDGFRα+Saa3+ CAFs could facilitate tumor growth while PDGFRα+Saa3− CAFs impairing tumor proliferation [53]. In summary, increasing proportion of CD146+ CAFs in ER+ breast cancer and targeting Saa3 specifically in PDAC might be promising strategies to revert the TME to an anti-tumor environment. So far it might be too immaturely to use the defensive CAFs as a cellular therapeutic strategy, however at least these biomarkers might be benefit for prognostic diagnosis.
Newly identified CAF subpopulations and biomarkers
Recent advances using single-cell RNA sequencing (scRNA-seq) provide us technical advantages to better understand CAF heterogeneity and identify novel biomarkers. For example, CD49e has been identified as a new cell surface pan-CAF biomarker in ovarian cancer recently, just like α-SMA [23]. Herein, we list the CAF subpopulations and biomarkers newly identified in distinct tumor tissues (Table 2).
Table 2.
List of CAF subpopulations and biomarkers newly identified
| CAF subsets | Biomarkers | Tumor tissues | Signatures/functions | Refs |
|---|---|---|---|---|
| pan-CAF | CD49e | Ovarian cancer | [23] | |
| myCAF | α-SMAhighIL-6low; RGS5 | PDAC; TNBC; bladder cancer | Myofibroblast-like; matrix deposition; | [14, 56, 58] |
| iCAF | α-SMAlowIL-6high; PDGFR; CXCL12; Ly6c1high; FBLN1 | PDAC; TNBC; bladder cancer; ICC | Inflammatory infiltration; chemokines and cytokines secretion; tumor-promoting | [14, 56–59] |
| apCAF | MHC-II gene; CD74 | PDAC; TNBC; ICC | Antigen presenting; immunomodulation | [57–59] |
| vCAF | MCAM; IL-6 | ICC | Response to hypoxia; mesenchymal cell proliferation | [59] |
| mCAF | POSTN; COL5A1 | ECM; collagen fibril organization | ||
| EMT-like CAF | KRT19 | Epithelium-like | ||
| vCAF | Nidogen-2 | Breast cancer | Vascular development; angiogenesis | [60] |
| mCAF | Fibulin-1; PDGFRα | ECM and EMT | ||
| developmental CAF | SCRG1 | Differentiation of cells; development and morphogenesis of tissues | ||
| CAF-A | MMP2; DCN; COL1A2 | Colorectal cancer | ECM remodeling | [61] |
| CAF-B | α-SMA; TAGCN; PDGFA | Myofibroblast-like | ||
| CAF-cluster2 | CDK1 | TNBC | Cell cycling | [58] |
| CAF-cluster3 | CD53 | Structural integrity and function of muscle | ||
| CAF-cluster4 | CRABP1 | Basement membrane protease associated | ||
| Immunomodulatory CAF | IL-6; IL-10; C1QA/B/C; CFB; CXCL1/2/10/12 | HGSOC | Immunomodulation | [62] |
| CAF-S1/S4 | CD29; FAP; α-SMA; FSP1; PDGFRβ; CAV1 | Breast cancer; ovarian cancer | Immunomodulation; myCAFs and iCAFs | [63–66] |
| CAF-S2/S3 | Not activated | |||
| CD10+GPR77+ CAFs | CD10; GPR77 | Breast and lung cancer | Promoting cancer formation and chemoresistance | [54] |
GPR77 and CD10 are potential targeted biomarkers as the infiltration of CD10+GPR77+ CAFs indicates chemotherapy resistance and poor survival, especially in the ER−HER2− subtype and high-grade breast tumors. Blocking GPR77 substantially can suppress tumorigenesis along with enhancing chemosensitivity in a patient-derived xenograft model [54].
The existence of iCAFs and myCAFs has been verified in triple-negative breast cancer (TNBC) and bladder urothelial carcinoma by scRNA-seq, despite the biomarkers identified are different. For specific, CX-chemokine ligand 12 (CXCL12) is the biomarker of TNBC iCAFs [55]. RGS5 and PDGFR are the biomarkers for myCAFs and iCAFs in bladder tumor, respectively [56].
Major histocompatibility complex (MHC) class II family genes and CD74 have been identified as biomarkers of another PDAC CAF subpopulation termed as antigen presenting CAFs (apCAFs) besides myCAFs and iCAFs. ApCAFs process an immunomodulatory role by interacting with CD4+ T cells [57]. All of these three CAF subpopulations with another three are verified in TNBC. It is noted that apCAFs are also found in normal tissues, indicating that the phenotype is not TME-induced. Furthermore, PDGFRα is found highly expressed in iCAFs while PDGFRβ is found highly expressed in myCAFs [58].
A recent scRNA-seq study conducted in human intrahepatic cholangiocarcinoma (ICC) found five CAF subpopulations: vascular CAFs (vCAFs) defined by MCAM expressing high level of IL-6, matrix CAFs (mCAFs) defined by POSTN, iCAFs defined by FBLN1, apCAFs defined by CD74 and EMT-like CAFs defined by KRT19 [59]. Another study identified three CAF subpopulations with distinct biomarkers in breast cancer: vCAFs with marker Nidogen-2, mCAFs with marker PDGFRα and developmental CAFs with marker SCRG-1 [60]. Moreover, two CAF subpopulations are detected in colorectal tumors: CAF-A expressing ECM remodeling genes such as MMP2, DCN, COL1A2 and CAF-B expressing markers of myofibroblasts such as α-SMA, TAGLN, PDGFA [61]. PDPN, DCN and THY1 are another group of biomarkers classifying four CAF subpopulations in high-grade serous ovarian cancer (HGSOC). Immunomodulatory CAFs expressing highly IL-6/CXCL12 identified could activate JAK/STAT signaling in tumor cells [62], just like iCAFs.
Mechta-Grigoriou et al. characterized four CAF subsets in breast, ovarian cancers and metastatic lymph node of breast cancer with distinct properties by analyzing six fibroblast biomarkers (FAP, α-SMA, β1/CD29, S100A4, PDGFRβ, and CAV1). The identified CAF-S1 subset can promote an immunosuppressive environment and stimulate migration of cancer cells [63–65]. Further investigation classified the CAF-S1 subset into 8 different clusters by scRNA-seq, among which three clusters belong to the iCAFs while another 5 clusters belong to the myCAFs [66].
As we summarized above, increasing CAF subsets with distinct biomarkers have been identified to coexist in tumor tissues and play different biological functions. However, due to the tissue heterogeneity, distinct classification criteria, biomarkers and nomenclature selected by different laboratories, the identification of CAF subsets is somewhat messy and intersecting at present. Among the CAF subsets identified, myCAFs and iCAFs both seem prevalent across-organ despite the biomarkers identified are different, probably due to the tissue heterogeneity. Furthermore, iCAFs have been widely proved to promote tumor progression by secreting chemokines and cytokines such as IL-6 and CXCL12. On the other hand, several CAF subgroups identified from different tissues have been named the same by different studies, such as vCAFs and mCAFs. However, given their different biological functions and biomarkers, whether they are the same subgroup is worth further discussion. We believe that with the further research on the CAF heterogeneity, there will be a unified standard for the selection of CAF biomarkers and nomenclature of CAF subpopulations.
With the further development of the technology, we believe that our understanding of the CAF subsets and biomarkers will be more profound. CAF biomarkers can be utilized as both prognostic indicators and therapeutic targets for clinical benefits. Hopefully, we can reverse the accomplice CAFs to defender ones by targeting appropriate molecules.
Acknowledgements
Not applicable.
Abbreviations
- CAF
Cancer-associated fibroblast
- TME
Tumor microenvironment
- ECM
Extracellular matrix
- α-SMA
Αlpha-smooth muscle actin
- FAP
Fibroblast activation protein
- PDGFR
Platelet-derived growth factor receptor
- TGF-β
Transforming growth factor-beta
- PDAC
Pancreatic ductal adenocarcinoma
- iCAFs
Inflammatory CAFs
- myCAFs
Myofibroblastic CAFs
- IL-1/6
Interleukin-1/6
- JAK
Janus kinase
- STAT
Signal transducer and activator of transcription
- TGFBR
Transforming growth factor receptor
- FSP-1
Fibroblast-specific protein-1
- VEGF
Vascular endothelial growth factor
- CCL2
Chemokine ligand 2
- mAb
Monoclonal antibody
- CAR
Chimeric antigen receptor
- LUAD
Lung adenocarcinoma
- EMT
Epithelial-to-mesenchymal transition
- PDPN
Podoplanin
- CAV1
Caveolin1
- ER
Estrogen receptor
- Saa3
Serum amyloid A3
- scRNA-seq
Single-cell RNA sequencing
- GPR77
G protein- coupled receptor 77
- TNBC
Triple-negative breast cancer
- CXCL12
CX-chemokine ligand 12
- RGS5
Regulator of G-protein signaling 5
- MHC
Major histocompatibility complex
- apCAFs
Antigen presenting CAFs
- ICC
Intrahepatic cholangiocarcinoma
- vCAFs
Vascular CAFs
- mCAFs
Matrix CAFs
- MCAM
Melanoma cell adhesion molecule
- POSTN
Periostin
- FBLN1
Fibulin 1
- KRT19
Keratin 19
- SCRG-1
Stimulator of chondrogenesis 1
- MMP2
Matrix metallopeptidase 2
- DCN
Decorin
- COL1A2
Collagen type I alpha 2 chain
- TAGLN
Transgelin
- THY1
Thy-1 cell surface antigen
- HGSOC
High-grade serous ovarian cancer
Authors’ contributions
YR conceived the design of the review. HCC and LTY wrote the manuscript. All authors read and approved the final manuscript.
Funding
This work was supported by National Science Foundation of China (81872378, 81672295, 81802277), China Postdoctoral Science Foundation (2018 M642198), and the Project of Jiangsu Provincial Medical Talent (ZDRCA2016033).
Availability of data and materials
Not applicable.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The author declares that he has no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Chencheng Han and Tongyan Liu contributed equally to this work.
References
- 1.Sahai E, Astsaturov I, Cukierman E, DeNardo DG, Egeblad M, Evans RM, Fearon D, Greten FR, Hingorani SR, Hunter T, et al. A framework for advancing our understanding of cancer-associated fibroblasts. Nat Rev Cancer. 2020;20:174–186. doi: 10.1038/s41568-019-0238-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liu T, Han C, Wang S, Fang P, Ma Z, Xu L, Yin R. Cancer-associated fibroblasts: an emerging target of anti-cancer immunotherapy. J Hematol Oncol. 2019;12:86. doi: 10.1186/s13045-019-0770-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Muhl L, Genove G, Leptidis S, Liu J, He L, Mocci G, Sun Y, Gustafsson S, Buyandelger B, Chivukula IV, et al. Single-cell analysis uncovers fibroblast heterogeneity and criteria for fibroblast and mural cell identification and discrimination. Nat Commun. 2020;11:3953. doi: 10.1038/s41467-020-17740-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ozdemir BC, Pentcheva-Hoang T, Carstens JL, Zheng X, Wu CC, Simpson TR, Laklai H, Sugimoto H, Kahlert C, Novitskiy SV, et al. Depletion of carcinoma-associated fibroblasts and fibrosis induces immunosuppression and accelerates pancreas cancer with reduced survival. Cancer Cell. 2014;25:719–734. doi: 10.1016/j.ccr.2014.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rhim AD, Oberstein PE, Thomas DH, Mirek ET, Palermo CF, Sastra SA, Dekleva EN, Saunders T, Becerra CP, Tattersall IW, et al. Stromal elements act to restrain, rather than support, pancreatic ductal adenocarcinoma. Cancer Cell. 2014;25:735–747. doi: 10.1016/j.ccr.2014.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen X, Song E. Turning foes to friends: targeting cancer-associated fibroblasts. Nat Rev Drug Discov. 2019;18:99–115. doi: 10.1038/s41573-018-0004-1. [DOI] [PubMed] [Google Scholar]
- 7.Kalluri R. The biology and function of fibroblasts in cancer. Nat Rev Cancer. 2016;16:582–598. doi: 10.1038/nrc.2016.73. [DOI] [PubMed] [Google Scholar]
- 8.Lazard D, Sastre X, Frid MG, Glukhova MA, Thiery JP, Koteliansky VE. Expression of smooth muscle-specific proteins in myoepithelium and stromal myofibroblasts of normal and malignant human breast tissue. Proc Natl Acad Sci U S A. 1993;90:999–1003. doi: 10.1073/pnas.90.3.999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rockey DC, Weymouth N, Shi Z. Smooth muscle alpha actin (Acta2) and myofibroblast function during hepatic wound healing. PLoS One. 2013;8:e77166. doi: 10.1371/journal.pone.0077166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huang M, Li Y, Zhang H, Nan F. Breast cancer stromal fibroblasts promote the generation of CD44+CD24- cells through SDF-1/CXCR4 interaction. J Exp Clin Cancer Res. 2010;29:80. doi: 10.1186/1756-9966-29-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lau EY, Lo J, Cheng BY, Ma MK, Lee JM, Ng JK, Chai S, Lin CH, Tsang SY, Ma S, et al. Cancer-associated fibroblasts regulate tumor-initiating cell plasticity in hepatocellular carcinoma through c-met/FRA1/HEY1 signaling. Cell Rep. 2016;15:1175–1189. doi: 10.1016/j.celrep.2016.04.019. [DOI] [PubMed] [Google Scholar]
- 12.Paulsson J, Micke P. Prognostic relevance of cancer-associated fibroblasts in human cancer. Semin Cancer Biol. 2014;25:61–68. doi: 10.1016/j.semcancer.2014.02.006. [DOI] [PubMed] [Google Scholar]
- 13.Wang WQ, Liu L, Xu HX, Luo GP, Chen T, Wu CT, Xu YF, Xu J, Liu C, Zhang B, et al. Intratumoral alpha-SMA enhances the prognostic potency of CD34 associated with maintenance of microvessel integrity in hepatocellular carcinoma and pancreatic cancer. PLoS One. 2013;8:e71189. doi: 10.1371/journal.pone.0071189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ohlund D, Handly-Santana A, Biffi G, Elyada E, Almeida AS, Ponz-Sarvise M, Corbo V, Oni TE, Hearn SA, Lee EJ, et al. Distinct populations of inflammatory fibroblasts and myofibroblasts in pancreatic cancer. J Exp Med. 2017;214:579–596. doi: 10.1084/jem.20162024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bernard V, Semaan A, Huang J, San Lucas FA, Mulu FC, Stephens BM, Guerrero PA, Huang Y, Zhao J, Kamyabi N, et al. Single-cell Transcriptomics of pancreatic Cancer precursors demonstrates epithelial and microenvironmental heterogeneity as an early event in neoplastic progression. Clin Cancer Res. 2019;25:2194–2205. doi: 10.1158/1078-0432.CCR-18-1955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Biffi G, Oni TE, Spielman B, Hao Y, Elyada E, Park Y, Preall J, Tuveson DA. IL1-induced JAK/STAT signaling is antagonized by TGFbeta to shape CAF heterogeneity in pancreatic ductal adenocarcinoma. Cancer Discov. 2019;9:282–301. doi: 10.1158/2159-8290.CD-18-0710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Iwano M, Plieth D, Danoff TM, Xue C, Okada H, Neilson EG. Evidence that fibroblasts derive from epithelium during tissue fibrosis. J Clin Investig. 2002;110:341–350. doi: 10.1172/JCI0215518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zeisberg EM, Potenta S, Xie L, Zeisberg M, Kalluri R. Discovery of endothelial to mesenchymal transition as a source for carcinoma-associated fibroblasts. Cancer Res. 2007;67:10123–10128. doi: 10.1158/0008-5472.CAN-07-3127. [DOI] [PubMed] [Google Scholar]
- 19.O'Connell JT, Sugimoto H, Cooke VG, MacDonald BA, Mehta AI, LeBleu VS, Dewar R, Rocha RM, Brentani RR, Resnick MB, et al. VEGF-A and Tenascin-C produced by S100A4+ stromal cells are important for metastatic colonization. Proc Natl Acad Sci U S A. 2011;108:16002–16007. doi: 10.1073/pnas.1109493108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Qian L, Tang Z, Yin S, Mo F, Yang X, Hou X, Liu A, Lu X. Fusion of dendritic cells and Cancer-associated fibroblasts for activation of anti-tumor cytotoxic T lymphocytes. J Biomed Nanotechnol. 2018;14:1826–1835. doi: 10.1166/jbn.2018.2616. [DOI] [PubMed] [Google Scholar]
- 21.Zhang J, Chen L, Liu X, Kammertoens T, Blankenstein T, Qin Z. Fibroblast-specific protein 1/S100A4-positive cells prevent carcinoma through collagen production and encapsulation of carcinogens. Cancer Res. 2013;73:2770–2781. doi: 10.1158/0008-5472.CAN-12-3022. [DOI] [PubMed] [Google Scholar]
- 22.Huber MA, Kraut N, Park JE, Schubert RD, Rettig WJ, Peter RU, Garin-Chesa P. Fibroblast activation protein: differential expression and serine protease activity in reactive stromal fibroblasts of melanocytic skin tumors. J Invest Dermatol. 2003;120:182–188. doi: 10.1046/j.1523-1747.2003.12035.x. [DOI] [PubMed] [Google Scholar]
- 23.Hussain A, Voisin V, Poon S, Karamboulas C, Bui NHB, Meens J, Dmytryshyn J, Ho VW, Tang KH, Paterson J, et al. Distinct fibroblast functional states drive clinical outcomes in ovarian cancer and are regulated by TCF21. J Exp Med. 2020;217. [DOI] [PMC free article] [PubMed]
- 24.Kraman M, Bambrough PJ, Arnold JN, Roberts EW, Magiera L, Jones JO, Gopinathan A, Tuveson DA, Fearon DT. Suppression of antitumor immunity by stromal cells expressing fibroblast activation protein-alpha. Science. 2010;330:827–830. doi: 10.1126/science.1195300. [DOI] [PubMed] [Google Scholar]
- 25.Adams S, Miller GT, Jesson MI, Watanabe T, Jones B, Wallner BP. PT-100, a small molecule dipeptidyl peptidase inhibitor, has potent antitumor effects and augments antibody-mediated cytotoxicity via a novel immune mechanism. Cancer Res. 2004;64:5471–5480. doi: 10.1158/0008-5472.CAN-04-0447. [DOI] [PubMed] [Google Scholar]
- 26.Santos AM, Jung J, Aziz N, Kissil JL, Pure E. Targeting fibroblast activation protein inhibits tumor stromagenesis and growth in mice. J Clin Invest. 2009;119:3613–3625. doi: 10.1172/JCI38988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ostermann E, Garin-Chesa P, Heider KH, Kalat M, Lamche H, Puri C, Kerjaschki D, Rettig WJ, Adolf GR. Effective immunoconjugate therapy in cancer models targeting a serine protease of tumor fibroblasts. Clin Cancer Res. 2008;14:4584–4592. doi: 10.1158/1078-0432.CCR-07-5211. [DOI] [PubMed] [Google Scholar]
- 28.Feig C, Jones JO, Kraman M, Wells RJ, Deonarine A, Chan DS, Connell CM, Roberts EW, Zhao Q, Caballero OL, et al. Targeting CXCL12 from FAP-expressing carcinoma-associated fibroblasts synergizes with anti-PD-L1 immunotherapy in pancreatic cancer. Proc Natl Acad Sci U S A. 2013;110:20212–20217. doi: 10.1073/pnas.1320318110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fang J, Xiao L, Joo KI, Liu Y, Zhang C, Liu S, Conti PS, Li Z, Wang P. A potent immunotoxin targeting fibroblast activation protein for treatment of breast cancer in mice. Int J Cancer. 2016;138:1013–1023. doi: 10.1002/ijc.29831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Loeffler M, Kruger JA, Niethammer AG, Reisfeld RA. Targeting tumor-associated fibroblasts improves cancer chemotherapy by increasing intratumoral drug uptake. J Clin Invest. 2006;116:1955–1962. doi: 10.1172/JCI26532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kakarla S, Chow KK, Mata M, Shaffer DR, Song XT, Wu MF, Liu H, Wang LL, Rowley DR, Pfizenmaier K, Gottschalk S. Antitumor effects of chimeric receptor engineered human T cells directed to tumor stroma. Mol Ther. 2013;21:1611–1620. doi: 10.1038/mt.2013.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wang LC, Lo A, Scholler J, Sun J, Majumdar RS, Kapoor V, Antzis M, Cotner CE, Johnson LA, Durham AC, et al. Targeting fibroblast activation protein in tumor stroma with chimeric antigen receptor T cells can inhibit tumor growth and augment host immunity without severe toxicity. Cancer Immunol Res. 2014;2:154–166. doi: 10.1158/2326-6066.CIR-13-0027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Freedman JD, Duffy MR, Lei-Rossmann J, Muntzer A, Scott EM, Hagel J, Campo L, Bryant RJ, Verrill C, Lambert A, et al. An Oncolytic virus expressing a T-cell engager simultaneously targets Cancer and immunosuppressive stromal cells. Cancer Res. 2018;78:6852–6865. doi: 10.1158/0008-5472.CAN-18-1750. [DOI] [PubMed] [Google Scholar]
- 34.de Sostoa J, Fajardo CA, Moreno R, Ramos MD, Farrera-Sal M, Alemany R. Targeting the tumor stroma with an oncolytic adenovirus secreting a fibroblast activation protein-targeted bispecific T-cell engager. J Immunother Cancer. 2019;7:19. doi: 10.1186/s40425-019-0505-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Welt S, Divgi CR, Scott AM, Garin-Chesa P, Finn RD, Graham M, Carswell EA, Cohen A, Larson SM, Old LJ, et al. Antibody targeting in metastatic colon cancer: a phase I study of monoclonal antibody F19 against a cell-surface protein of reactive tumor stromal fibroblasts. J Clin Oncol. 1994;12:1193–1203. doi: 10.1200/JCO.1994.12.6.1193. [DOI] [PubMed] [Google Scholar]
- 36.Scott AM, Wiseman G, Welt S, Adjei A, Lee FT, Hopkins W, Divgi CR, Hanson LH, Mitchell P, Gansen DN, et al. A phase I dose-escalation study of sibrotuzumab in patients with advanced or metastatic fibroblast activation protein-positive cancer. Clin Cancer Res. 2003;9:1639–1647. [PubMed] [Google Scholar]
- 37.Hofheinz RD, al-Batran SE, Hartmann F, Hartung G, Jager D, Renner C, Tanswell P, Kunz U, Amelsberg A, Kuthan H, Stehle G. Stromal antigen targeting by a humanised monoclonal antibody: an early phase II trial of sibrotuzumab in patients with metastatic colorectal cancer. Onkologie. 2003;26:44–48. doi: 10.1159/000069863. [DOI] [PubMed] [Google Scholar]
- 38.Narra K, Mullins SR, Lee HO, Strzemkowski-Brun B, Magalong K, Christiansen VJ, McKee PA, Egleston B, Cohen SJ, Weiner LM, et al. Phase II trial of single agent Val-boroPro (Talabostat) inhibiting fibroblast activation protein in patients with metastatic colorectal cancer. Cancer Biol Ther. 2007;6:1691–1699. doi: 10.4161/cbt.6.11.4874. [DOI] [PubMed] [Google Scholar]
- 39.Gieniec KA, Butler LM, Worthley DL, Woods SL. Cancer-associated fibroblasts-heroes or villains? Br J Cancer. 2019;121:293–302. doi: 10.1038/s41416-019-0509-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Paulsson J, Ehnman M, Ostman A. PDGF receptors in tumor biology: prognostic and predictive potential. Future Oncol. 2014;10:1695–1708. doi: 10.2217/fon.14.83. [DOI] [PubMed] [Google Scholar]
- 41.Frings O, Augsten M, Tobin NP, Carlson J, Paulsson J, Pena C, Olsson E, Veerla S, Bergh J, Ostman A, Sonnhammer EL. Prognostic significance in breast cancer of a gene signature capturing stromal PDGF signaling. Am J Pathol. 2013;182:2037–2047. doi: 10.1016/j.ajpath.2013.02.018. [DOI] [PubMed] [Google Scholar]
- 42.Pietras K, Pahler J, Bergers G, Hanahan D. Functions of paracrine PDGF signaling in the proangiogenic tumor stroma revealed by pharmacological targeting. PLoS Med. 2008;5:e19. doi: 10.1371/journal.pmed.0050019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Haubeiss S, Schmid JO, Murdter TE, Sonnenberg M, Friedel G, van der Kuip H, Aulitzky WE. Dasatinib reverses cancer-associated fibroblasts (CAFs) from primary lung carcinomas to a phenotype comparable to that of normal fibroblasts. Mol Cancer. 2010;9:168. doi: 10.1186/1476-4598-9-168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Vuoriluoto K, Haugen H, Kiviluoto S, Mpindi JP, Nevo J, Gjerdrum C, Tiron C, Lorens JB, Ivaska J. Vimentin regulates EMT induction by slug and oncogenic H-Ras and migration by governing Axl expression in breast cancer. Oncogene. 2011;30:1436–1448. doi: 10.1038/onc.2010.509. [DOI] [PubMed] [Google Scholar]
- 45.Richardson AM, Havel LS, Koyen AE, Konen JM, Shupe J, Wiles WG, Martin WD, Grossniklaus HE, Sica G, Gilbert-Ross M, Marcus AI. Vimentin is required for lung adenocarcinoma metastasis via heterotypic tumor cell-Cancer-associated fibroblast interactions during collective invasion. Clin Cancer Res. 2018;24:420–432. doi: 10.1158/1078-0432.CCR-17-1776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sakai T, Aokage K, Neri S, Nakamura H, Nomura S, Tane K, Miyoshi T, Sugano M, Kojima M, Fujii S, et al. Link between tumor-promoting fibrous microenvironment and an immunosuppressive microenvironment in stage I lung adenocarcinoma. Lung Cancer. 2018;126:64–71. doi: 10.1016/j.lungcan.2018.10.021. [DOI] [PubMed] [Google Scholar]
- 47.Jacobs J, Deschoolmeester V, Zwaenepoel K, Flieswasser T, Deben C, Van den Bossche J, Hermans C, Rolfo C, Peeters M, De Wever O, et al. Unveiling a CD70-positive subset of cancer-associated fibroblasts marked by pro-migratory activity and thriving regulatory T cell accumulation. Oncoimmunology. 2018;7:e1440167. doi: 10.1080/2162402X.2018.1440167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Catenacci DV, Junttila MR, Karrison T, Bahary N, Horiba MN, Nattam SR, Marsh R, Wallace J, Kozloff M, Rajdev L, et al. Randomized phase Ib/II study of gemcitabine plus placebo or Vismodegib, a hedgehog pathway inhibitor, in patients with metastatic pancreatic Cancer. J Clin Oncol. 2015;33:4284–4292. doi: 10.1200/JCO.2015.62.8719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kim EJ, Sahai V, Abel EV, Griffith KA, Greenson JK, Takebe N, Khan GN, Blau JL, Craig R, Balis UG, et al. Pilot clinical trial of hedgehog pathway inhibitor GDC-0449 (vismodegib) in combination with gemcitabine in patients with metastatic pancreatic adenocarcinoma. Clin Cancer Res. 2014;20:5937–5945. doi: 10.1158/1078-0432.CCR-14-1269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ko AH, LoConte N, Tempero MA, Walker EJ, Kate Kelley R, Lewis S, Chang WC, Kantoff E, Vannier MW, Catenacci DV, et al. A phase I study of FOLFIRINOX plus IPI-926, a hedgehog pathway inhibitor, for advanced pancreatic adenocarcinoma. Pancreas. 2016;45:370–375. doi: 10.1097/MPA.0000000000000458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Brechbuhl HM, Finlay-Schultz J, Yamamoto TM, Gillen AE, Cittelly DM, Tan AC, Sams SB, Pillai MM, Elias AD, Robinson WA, et al. Fibroblast subtypes regulate responsiveness of luminal breast Cancer to estrogen. Clin Cancer Res. 2017;23:1710–1721. doi: 10.1158/1078-0432.CCR-15-2851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Simpkins SA, Hanby AM, Holliday DL, Speirs V. Clinical and functional significance of loss of caveolin-1 expression in breast cancer-associated fibroblasts. J Pathol. 2012;227:490–498. doi: 10.1002/path.4034. [DOI] [PubMed] [Google Scholar]
- 53.Djurec M, Grana O, Lee A, Troule K, Espinet E, Cabras L, Navas C, Blasco MT, Martin-Diaz L, Burdiel M, et al. Saa3 is a key mediator of the protumorigenic properties of cancer-associated fibroblasts in pancreatic tumors. Proc Natl Acad Sci U S A. 2018;115:E1147–E1156. doi: 10.1073/pnas.1717802115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Su S, Chen J, Yao H, Liu J, Yu S, Lao L, Wang M, Luo M, Xing Y, Chen F, et al. CD10(+)GPR77(+) Cancer-associated fibroblasts promote Cancer formation and Chemoresistance by sustaining Cancer Stemness. Cell. 2018;172:841–856. doi: 10.1016/j.cell.2018.01.009. [DOI] [PubMed] [Google Scholar]
- 55.Wu SZ, Roden DL, Wang C, Holliday H, Harvey K, Cazet AS, Murphy KJ, Pereira B, Al-Eryani G, Bartonicek N, et al. Stromal cell diversity associated with immune evasion in human triple-negative breast cancer. EMBO J. 2020:e104063. [DOI] [PMC free article] [PubMed]
- 56.Chen Z, Zhou L, Liu L, Hou Y, Xiong M, Yang Y, Hu J, Chen K. Single-cell RNA sequencing highlights the role of inflammatory cancer-associated fibroblasts in bladder urothelial carcinoma. Nat Commun. 2020;11:5077. doi: 10.1038/s41467-020-18916-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Elyada E, Bolisetty M, Laise P, Flynn WF, Courtois ET, Burkhart RA, Teinor JA, Belleau P, Biffi G, Lucito MS, et al. Cross-species single-cell analysis of pancreatic ductal adenocarcinoma reveals antigen-presenting Cancer-associated fibroblasts. Cancer Discov. 2019;9:1102–1123. doi: 10.1158/2159-8290.CD-19-0094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sebastian A, Hum NR, Martin KA, Gilmore SF, Peran I, Byers SW, Wheeler EK, Coleman MA, Loots GG. Single-cell Transcriptomic analysis of tumor-derived fibroblasts and Normal tissue-resident fibroblasts reveals fibroblast heterogeneity in breast Cancer. Cancers (Basel). 2020;12. [DOI] [PMC free article] [PubMed]
- 59.Zhang M, Yang H, Wan L, Wang Z, Wang H, Ge C, Liu Y, Hao Y, Zhang D, Shi G, et al. Single-cell transcriptomic architecture and intercellular crosstalk of human intrahepatic cholangiocarcinoma. J Hepatol. 2020. [DOI] [PubMed]
- 60.Bartoschek M, Oskolkov N, Bocci M, Lövrot J, Larsson C, Sommarin M, Madsen CD, Lindgren D, Pekar G, Karlsson G, et al. Spatially and functionally distinct subclasses of breast cancer-associated fibroblasts revealed by single cell RNA sequencing. Nat Commun. 2018;9. [DOI] [PMC free article] [PubMed]
- 61.Li H, Courtois ET, Sengupta D, Tan Y, Chen KH, Goh JJL, Kong SL, Chua C, Hon LK, Tan WS, et al. Reference component analysis of single-cell transcriptomes elucidates cellular heterogeneity in human colorectal tumors. Nat Genet. 2017;49:708–718. doi: 10.1038/ng.3818. [DOI] [PubMed] [Google Scholar]
- 62.Izar B, Tirosh I, Stover EH, Wakiro I, Cuoco MS, Alter I, Rodman C, Leeson R, Su MJ, Shah P, et al. A single-cell landscape of high-grade serous ovarian cancer. Nat Med. 2020;26:1271–1279. doi: 10.1038/s41591-020-0926-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Givel AM, Kieffer Y, Scholer-Dahirel A, Sirven P, Cardon M, Pelon F, Magagna I, Gentric G, Costa A, Bonneau C, et al. miR200-regulated CXCL12beta promotes fibroblast heterogeneity and immunosuppression in ovarian cancers. Nat Commun. 2018;9:1056. doi: 10.1038/s41467-018-03348-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Costa A, Kieffer Y, Scholer-Dahirel A, Pelon F, Bourachot B, Cardon M, Sirven P, Magagna I, Fuhrmann L, Bernard C, et al. Fibroblast heterogeneity and immunosuppressive environment in human breast Cancer. Cancer Cell. 2018;33:463–479. doi: 10.1016/j.ccell.2018.01.011. [DOI] [PubMed] [Google Scholar]
- 65.Pelon F, Bourachot B, Kieffer Y, Magagna I, Mermet-Meillon F, Bonnet I, Costa A, Givel AM, Attieh Y, Barbazan J, et al. Cancer-associated fibroblast heterogeneity in axillary lymph nodes drives metastases in breast cancer through complementary mechanisms. Nat Commun. 2020;11:404. doi: 10.1038/s41467-019-14134-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kieffer Y, Hocine HR, Gentric G, Pelon F, Bernard C, Bourachot B, Lameiras S, Albergante L, Bonneau C, Guyard A, et al. Single-cell analysis reveals fibroblast clusters linked to immunotherapy resistance in Cancer. Cancer Discov. 2020;10:1330–1351. doi: 10.1158/2159-8290.CD-19-1384. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.