Abstract
Background
In 2009, the South Korean government expanded universal health insurance to include oral health services. In the present study, we sought to examine whether improved access resulted in a reduction in income-based self-reported oral health inequalities.
Methods
We analyzed repeated cross-sectional data from the Korea National Health and Nutrition Examination Survey (KNHANES) waves IV through VI (2007–2015). We analyzed self-reported oral health status among 68,431 subjects. Changes in oral health inequalities across four income levels (low, middle-low, middle-high, and high) were assessed with the Slope Index of Inequality (SII) and the Relative Index of Inequality (RII).
Results
The average oral health status of children and adolescents improved the most over the observation period. The absolute magnitude of oral health inequalities (measured by the SII) improved for most groups, with the notable exception of young male adults. By contrast, the ratio of poor oral health between high- and low-income groups (measured by the RII) changed little over time, indicating that relative inequalities remained resistant to change.
Conclusions
The expansion of dental health insurance may not be sufficient to move the needle on self-reported oral health inequalities among adults.
Key words: health insurance, income, inequality, KNHANES, self-reported oral health
INTRODUCTION
The Republic of Korea achieved universal coverage of health insurance for the population in 1989. However, many challenges remain regarding the performance of the system, including high out-of-pocket (OOP) payments.1 Oral health is a critical component of overall health, yet the initial stages of Korea’s health insurance system failed to finance access to oral health care as part of the package. Therefore, the Korean government initiated an expansion of health insurance coverage for dental services in 2009. The expansion sought to improve access to dental care and reduce oral health inequalities. The services covered under the expansion included dental sealants (for caries prevention), dental scaling (for periodontal disease prevention), and fitting of prosthetics (for edentulous rehabilitation).
The main condition for improving oral health inequalities involves providing equitable access to dental care at the national level.2–4 Further work is required to verify whether dental health insurance affects inequalities in oral health beyond access to dental care. Studies conducted in the aftermath of the insurance expansion confirmed that access to dental service was improved5–7; however, disparities in access to services remained.6,8,9 Currently, few studies have evaluated whether the dental health insurance expansion improved oral health inequalities (not just service access).
There are significant reasons to be cautious in assuming that an expansion in health insurance will achieve a reduction in health inequalities. For example, when the National Health Service was established after the Second World War in Britain, politicians at the time expected it to herald the end of health inequalities. More than 70 years later, however, health inequalities in Britain have not shrunk; instead, they have persisted and in some cases even widened.10 Despite universal coverage and dental care reform, oral health inequalities have persisted or even widened in Thailand, Sweden, and Finland.3,4,11,12
The continuing inequalities exist because access to health insurance (by itself) is not the primary reason for socioeconomic disparities in health status. According to the “social determinants of health” framework, health is determined by multiple “upstream” social circumstances, including the conditions in which people are born, grow, learn, work, and age.13 Expanding health insurance can only do so much to redress these social circumstances. Indeed, in some instances, the expansion of access to certain health technologies could even widen health inequalities because those who need the services the least (ie, the most advantaged) are better able to take advantage of the expanded services.14 The so-called Inverse Care Law—originally formulated by Julian Tudor Hart15—maintains that people receive care “in inverse proportion to their level of need”.
Given these debates, we sought to evaluate whether the expansion of health insurance to cover dental services led to a reduction in self-reported oral health inequalities in Korea.
METHODS
This study design utilized repeated cross-sectional nationally representative data. Our study sample comprised all respondents to the Self-Reported Oral Health (SROH) module (N = 68,431; 30,817 men and 37,614 women) of the Korea National Health and Nutrition Examination Survey (KNHANES). Our data were obtained from three waves of the survey (waves IV–VI, corresponding to 2007–09, 2010–12, and 2013–15, respectively). The KNHANES waves are redesigned once every 3 years to every year to provide timely health statistics for monitoring changes in health risk factors and diseases.16
We included all age groups (children/adolescents: 0–19 years, young adults: 20–44 years, middle-aged adults: 45–64 years, and older adults: ≥65 years). Sample weights were used to represent the general population.
Ethical considerations
The KNHANES has been reviewed and approved annually since 2007 by the KCDC Research Ethics. In accordance with ethical guidelines, advance review and approval were obtained from the Institutional Review Board for Human Research, Yonsei University Wonju Severance Christian Hospital (CR318339).
Variables of interest
Our outcome of interest was self-reported poor oral health, which was assessed via responses to the single item: “How do you rate your oral health, including your teeth and gums?”. The participants chose one of the following responses: “very good”, “good”, “average”, “bad”, or “very bad”. We combined the “bad” and “very bad” responses to represent “poor oral health”.
Household income (equivalized for household size) was our indicator of socioeconomic status (SES). We grouped income into four categories by quartiles: low, middle-low, middle-high, and high income. Parents answered instead of children under 12 years of age.
Calculation of indices of inequality
We calculated two indices of health inequality: the Slope Index of Inequality (SII) and the Relative Index of Inequality (RII). We initially estimated the prevalence of poor oral health (using survey weights) in each wave. The adjusted prevalence and 95% confidence intervals (CIs) for poor oral health according to income rank were calculated. These indices are regression-based measures that consider the whole income distribution, rather than only comparing the two most extreme groups. A ridit score is assigned to each income category based on the midpoint of the range in the cumulative distribution of the population of participants in the given category. Individuals were cumulatively ranked from 0 to 1 according to ascending income position, with “0” representing the lowest income level and “1” representing the highest income. The relative income position variable was then entered as an independent variable in the regression model. SII is the difference in the prevalence of oral health (absolute inequality), and RII is the prevalence rate ratio (relative inequality) between those with the top rank (highest income level) and those with a rank of zero (lowest income level). If there is no inequality, the SII takes a value of zero. Negative SII values indicate a higher prevalence of poor oral health in the low-income group. In general, RII takes positive values; however, RII values can also take on negative values, indicating a gradient in favor of lower-income groups.17 The model was adjusted for age and income and stratified by gender. Differences in income inequalities among study years were tested using interaction terms. We pooled the three waves of data from the assessed study years and included an interaction term between SII, RII, and study year for each age group and gender.18 All analyses were controlled for age group- and wave-specific fixed effects. We used Stata statistical software (version 15.1) (Stata Corp LP, College Station, TX, USA) for all statistical analyses. R (version 3.5.1, SNU General Public License, Korea; R Foundation for Statistical Computing, Vienna, Austria) was used to visualize the results.
RESULTS
Trends in the prevalence of self-reported poor oral health according to age group, gender, and household income
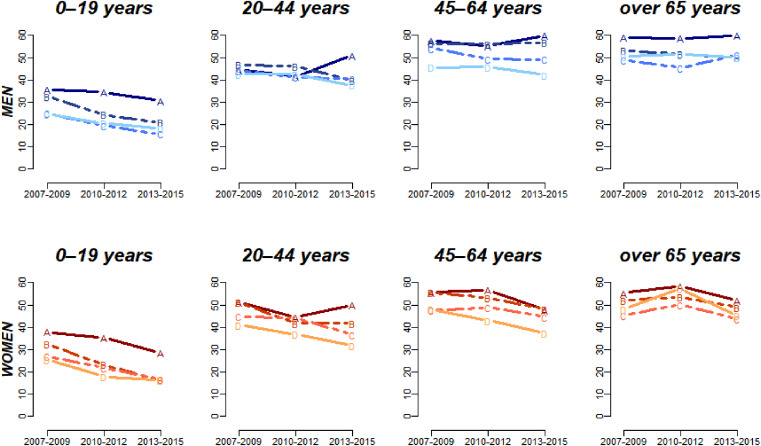
The age-adjusted prevalence rates of self-reported poor oral health are summarized in Figure 1. Two patterns are evident within each wave: first, oral health deteriorates with increasing age; second, there is an income gradient in poor oral health (individuals from lower-income households report worse oral health).
Figure 1. Trends in the prevalence of self-reported poor oral health according to age, gender, and household income. Unit (%) A: Low income, B: Middle-low, C: Middle-high, D: High income.
Across waves, it is also evident that SROH improved over time for every group (age group, sex, income level). However, there are some exceptions to this overall trend. For example, an improving trend was not observed among men aged 20–44, 45–64, and over 65 years across survey years.
Trends in oral health inequalities over time
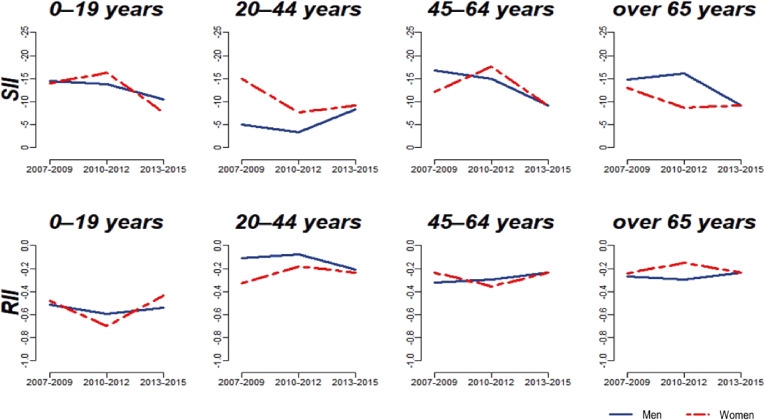
Figure 2 shows the inequality indices of SII and RII. Among children and adolescents, oral health inequalities declined in absolute terms (SII) over the period of observation. This was indicated by the change in SII from −14.4 (2007) to −10.4 (2013) in boys and from −14.0 (2007) to −7.6 (2013) in girls. Conversely, for both boys and girls, oral health inequalities on the relative scale (RII) remained essentially unchanged during the period of observation (RII changed from −0.51 (2007) to −0.54 (2013) in boys and from −0.48 (2007) to −0.43 (2013) in girls). This indicates that, although the absolute size of the gap in poor oral health declined over the 8-year period, the relative inequality (between high- and low-income groups) remained resistant to change (Figure 2).
Figure 2. Trends in income-based absolute (SII) and relative (RII) self-reported oral health inequalities over time across age, gender, and study waves.
Similar overall trends were found for all age and sex groups in adults, as demonstrated by a decline in oral health inequalities on the absolute scale, but relatively unchanged inequalities on the relative scale. The one notable exception to these trends was observed among young adult men (Figure 2), among whom inequalities increased on both the absolute and relative scales. The reason for this was that the oral health of high-income males improved, whereas the prevalence of oral health in low-income males deteriorated during the third wave (Figure 1).
DISCUSSION
The goal of our study was to explore whether the expansion of health insurance (to cover dental services) achieved a reduction in self-reported oral health inequalities by income. Our findings suggest that, although health insurance expansion improved access to dental care and may have contributed to an absolute improvement in self-reported oral health for most groups, the relative income gradient in oral health remained resistant to change.
The reasons for the persistence (or even widening) of inequality after dental care reform have focused on dental care systems that feature a fee-for-service structure, and/or rely on the provision of services from the private sector.3,11,12,19 Although the national health insurance in Korea covers the entire population, the proportion of OOP payment in dental services expenditure is high. Several dental services have only just recently been included as benefits of the insurance expansion.
Nevertheless, we observed that oral health inequalities can be reduced over time on the absolute scale, yet they remain unchanged (or even worsen) on the relative scale. The stable or narrowing inequality trends may be related to health changes caused by different factors that affect groups according to their income.20 It seems that the decrease in absolute inequality is due to the improvement of oral health among all income groups. The unchanged relative inequality might be due to the fact that self-reported oral health improved more among the better-off than among the poor, potentially due to economic and social changes during this period. This finding has previously been highlighted in other contexts. For example, racial disparities in infant mortality in the United States have improved over time on the absolute scale, with both black and white infants experiencing an absolute decline in mortality.21 This has also resulted in a lower SII over time. However, the relative gap between blacks and whites has remained very persistent (and even increased).22,23
In the field of oral health, an age-period-cohort analysis in the United Kingdom (spanning the period from 1988 to 2009) showed that in the entire adult population, although absolute inequalities in tooth loss narrowed over time, relative inequalities increased steadily.24 It is a matter of debate as to whether the persistence of relative inequalities represents a problem for public health. On the one hand, the “widening” of relative inequalities can be the product of a mathematical artifact: it is easier to generate large ratio measures with falling rates of bad health. On the other hand, the presence of between-group inequalities can be viewed as an indicator of persistent injustice.
In the United States, Medicaid coverage of dental services has increased access to dental care (by reducing OOP costs paid by beneficiaries under the Affordable Care Act)25 and may have contributed to an improvement in oral health status. However, improved access to dental care may not be sufficient to close the gap in oral health status because oral health is determined by many other factors outside of health services (eg, water fluoridation and the use of fluoridated toothpaste).
An encouraging finding from our analysis is that income-based absolute inequalities in self-reported oral health improved for most groups. Children/adolescents recorded the best improvements in oral health status in addition to reduced inequalities (Figure 1 and Figure 2). The treatment of dental fissures was included for the first time in the health insurance coverage in 2009. The insurance covered just the first molars of 6- to 14-year-olds. Even so, a sharp decline in dental caries was recorded among 8- to 12-year-olds in Korea between 2006 and 2012.26 In 2013, the insurance was expanded again to cover the second molars and all age groups under 18 years old.
Despite these achievements, we also noted some remaining areas of concern. Young males bucked the overall trend in terms of widening inequalities; self-reported oral health in women improved more than that in men (even though the insurance expansion covered everyone), and that in the worst off groups did not improve the most. The inequalities appeared to be related to the time since the last dental care visit and income itself in this age group.12 Young males tend to have greater and more severe dental caries and periodontal disease compared to women, but they are less likely to have received dental care.27 The reasons seem related to their low level of oral health perception or concern.28,29 Men did not appear to use dental services more often after the health insurance expansion.6
Annual dental scaling has been covered by insurance since 2013 for everyone aged ≥20 years. Although dental scaling visits remain more common among high socioeconomic groups,6 all outpatient dental visits have been reported to increase among middle-aged Koreans after the insurance expansion.5 We verified that dental service utilization increased as a result of reduced OOP expenses.7,25,30 Whether these results are linked to oral health inequalities requires confirmation over a longer period of time.
Since 2012, denture treatment has been offered for people aged ≥75 years every 7 years. The coverage was expanded to everyone ≥70 years in 2015 and again for everyone ≥65 years in 2016. The patient cost amounts to 10–30% of the total fee depending on the income level of the patient and treatment materials. Many edentulous older adults may nonetheless believe (erroneously) that once all their teeth have been extracted, they no longer need to be concerned about oral health.31 This may be one of the reasons why the high prevalence of poor oral health among older adult men has not changed. Our results of inequality among older adults might be due to cohort-related historic inequality-shaping forces and the high costs associated with dental care.4
In previous studies, SROH has shown a high reliability with clinical oral health outcomes.32 Thus, SROH is regarded as a practical and easily interpreted measure to assess inequalities in the oral health of a population.11,12,33,34 We confirmed the same patterns of the outcome variable through a sensitivity analysis and robustness check. The supplemental table (eTable 1) shows the results separating “poor” versus “very poor”. However, we found that the proportion of “very poor” self-reported oral health status increased among children/adolescents in the low income group during the survey years from 2013–2015. This indicates a sub-group of special concern, given the two-fold increase, and the likely persistence of poor oral health status as the children advance toward adulthood.
One strength of our research is that we examined all age ranges from children to older adults. We used KNHANES data, so our results can be generalized to the entire population in South Korea. In addition, we could identify population-level trends from the long-term repeated cross-sectional data. Nevertheless, we also note several limitations. First, we cannot draw inferences about the impact of dental insurance expansion on self-reported oral health inequalities because the trends in self-reported oral health that we found appear to have already started before the health insurance expansion. Because the Korean health insurance expansion was national in scope (as opposed to varying by state, as in the Affordable Care Act in the United States),35 we lack a “control” group to be able to identify any causal effects of the policy change (eg, through difference-in-difference estimations).
Second, we have considered only income-based health inequalities. Current household income may not adequately represent the standard of living for different generations nor the cumulative socioeconomic position of households across the life course.36 Although the main outcome was self-reported poor oral health, it may be subject to bias due to under- or over-reporting by different groups.
In conclusion, the expansion of dental health may have contributed to an absolute improvement in self-reported oral health for most groups, but the relative income gradient remained resistant to change. Thus, the expansion of dental health insurance may not be sufficient to move the needle on self-reported oral health inequalities among adults so far. Future trends in self-reported oral health inequalities must be monitored with long-term data.
ACKNOWLEDGEMENTS
All authors take responsibility for the entire content of the manuscript. Each of the listed authors meets both of the two authorship requirements as stated in the Uniform Requirements for Manuscripts. All authors conceptualized and designed the revised study design and provided expert interpretation of the new analyses and results. NHK drafted the original manuscript, and IK provided supervision throughout, critically revised the manuscript, and provided additional supervision. NHK acquired and analyzed the data, critically reviewed the manuscript, and conducted all statistical analyses. IK interpreted the study results and policy implications.
Conflicts of interest: None declared.
APPENDIX A. SUPPLEMENTARY DATA
The following is the supplementary data related to this article:
eTable 1. Stratified prevalence of self-reported poor and very poor oral health according to income by age, gender, and survey years
REFERENCES
- 1.Regional Office for the Western Pacific, World Health Organization. Republic of Korea Health System Review. Manila, Philippines: WHO Regional Office for the Western Pacific; 2015. [Google Scholar]
- 2.Wamala S, Merlo J, Boström G. Inequity in access to dental care services explains current socioeconomic disparities in oral health: the Swedish National Surveys of Public Health 2004–2005. J Epidemiol Community Health. 2006;60:1027–1033. 10.1136/jech.2006.046896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Molarius A, Engström S, Flink H, Simonsson B, Tegelberg A. Socioeconomic differences in self-rated oral health and dental care utilisation after the dental care reform in 2008 in Sweden. BMC Oral Health. 2014;14:134. 10.1186/1472-6831-14-134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vikum E, Krokstad S, Holst D, Westin S. Socioeconomic inequalities in dental services utilisation in a Norwegian county: the third Nord-Trøndelag Health Survey. Scand J Public Health. 2012;40:648–655. 10.1177/1403494812458989 [DOI] [PubMed] [Google Scholar]
- 5.Park HJ, Lee JH, Park S, Kim TI. Trends in the utilization of dental outpatient services affected by the expansion of health care benefits in South Korea to include scaling: a 6-year interrupted time-series study. J Periodontal Implant Sci. 2018;48:3–11. 10.5051/jpis.2018.48.1.3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jang YE, Kim CB, Kim NH. Utilization of preventive dental services before and after health insurance covered dental scaling in Korea: 2009 to 2014 Community Health Survey. Asia Pac J Public Health. 2017;29:70–80. 10.1177/1010539516684944 [DOI] [PubMed] [Google Scholar]
- 7.Jang YE, Kim CB, Kim NH. Influence of dental insurance coverage on access to preventive periodontal care in middle-aged and elderly populations: analysis of representative Korean Community Health Survey Data (2011–2015). Int Dent J. 2019;69(6):445–453. 10.1111/idj.12488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Choi JS, Park DY. The impact of national health insurance coverage on pit and fissure sealing experience. Rural Remote Health. 2018;18:4804. 10.22605/RRH4804 [DOI] [PubMed] [Google Scholar]
- 9.Jang YE, Lee MY, Park SK, et al. A 7-year study of the regional distribution of differences in scaling experience rate among Koreans. J Korean Acad Oral Health. 2015;39:201–206. 10.11149/jkaoh.2015.39.3.201 [DOI] [Google Scholar]
- 10.Shaw M, Dorling D, Gordon D, Smith D, Raphael D. The widening gap: health inequalities and policy in Britain. Bristol: The Policy Press; 1999. [Google Scholar]
- 11.Somkotra T. Socioeconomic inequality in self-reported oral health status: the experience of Thailand after implementation of the universal coverage policy. Community Dent Health. 2011;28:136–142. [PubMed] [Google Scholar]
- 12.Raittio E, Aromaa A, Kiiskinen U, Helminen S, Suominen AL. Income-related inequality in perceived oral health among adult Finns before and after a major dental subsidization reform. Acta Odontol Scand. 2016;74:348–354. 10.3109/00016357.2016.1142113 [DOI] [PubMed] [Google Scholar]
- 13.WHO Commission on Social Determinants of Health. Closing the gap in a generation: Health equity through action on the social determinants of health. Commission on Social Determinants of Health Final Report. Geneva, Switzerland: World Health Organization, Commission on Social Determinants of Health; 2008. [Google Scholar]
- 14.Dehmoobadsharifabadi A, Singhal S, Quiñonez C. Investigating the “inverse care law” in dental care: a comparative analysis of Canadian jurisdictions. Can J Public Health. 2017;107(6):e538–e544. 10.17269/CJPH.107.5454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hart JT. The inverse care law. Lancet. 1971;1:405–412. 10.1016/S0140-6736(71)92410-X [DOI] [PubMed] [Google Scholar]
- 16.Kweon S, Kim Y, Jang MJ, et al. Data resource profile: the Korea National Health and Nutrition Examination Survey (KNHANES). Int J Epidemiol. 2014;43:69–77. 10.1093/ije/dyt228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Erreygers G, Van Ourti T. Measuring socioeconomic inequality in health, health care and health financing by means of rank-dependent indices: a recipe for good practice. J Health Econ. 2011;30:685–694. 10.1016/j.jhealeco.2011.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chiou ST, Wu CY, Hurng BS, Lu TH. Changes in the magnitude of social inequality in the uptake of cervical cancer screening in Taiwan, a country implementing a population-based organized screening program. Int J Equity Health. 2014;13:4. 10.1186/1475-9276-13-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Donaldson AN, Everitt B, Newton T, Steele J, Sherriff M, Bower E. The effects of social class and dental attendance on oral health. J Dent Res. 2008;87:60–64. 10.1177/154405910808700110 [DOI] [PubMed] [Google Scholar]
- 20.Hiyoshi A, Fukuda Y, Shipley MJ, Brunner EJ. Inequalities in self-rated health in Japan 1986–2007 according to household income and a novel occupational classification: national sampling survey series. J Epidemiol Community Health. 2013;67:960–965. 10.1136/jech-2013-202608 [DOI] [PubMed] [Google Scholar]
- 21.Callaghan WM, MacDorman MF, Shapiro-Mendoza CK, Barfield WD. Explaining the recent decrease in US infant mortality rate, 2007–2013. Am J Obstet Gynecol. 2017;216(1):73.e1–73.e8. 10.1016/j.ajog.2016.09.097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.King NB, Kaufman JS, Harper S. Relative measures alone tell only part of the story. Am J Public Health. 2010;100:2014–2015. 10.2105/AJPH.2010.203232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Riddell CA, Harper S, Kaufman JS. Trends in differences in US mortality rates between black and white infants. JAMA Pediatr. 2017;171:911–913. 10.1001/jamapediatrics.2017.1365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bernabé E, Sheiham A. Tooth loss in the United Kingdom—trends in social inequalities: an age-period-and-cohort analysis. PLoS One. 2014;9(8):e104808. 10.1371/journal.pone.0104808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Decker SL, Lipton BJ. Do Medicaid benefit expansions have teeth? The effect of Medicaid adult dental coverage on the use of dental services and oral health. J Health Econ. 2015;44:212–225. 10.1016/j.jhealeco.2015.08.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kim HN, Han DH, Jun EJ, Kim SY, Jeong SH, Kim JB. The decline in dental caries among Korean children aged 8 and 12 years from 2000 to 2012 focusing SiC Index and DMFT. BMC Oral Health. 2016;16:38. 10.1186/s12903-016-0188-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brennan D, Spencer J, Roberts-Thomson K. Dental knowledge and oral health among middle-aged adults. Aust N Z J Public Health. 2010;34:472–475. 10.1111/j.1753-6405.2010.00592.x [DOI] [PubMed] [Google Scholar]
- 28.Diop M, Kanouté A, Diouf M, et al. The role of health insurance in the coverage of oral health care in Senegal. J Public Health Africa. 2018;9:772. 10.4081/jphia.2018.772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Maida CA, Marcus M, Spolsky VW, Wang Y, Liu H. Socio-behavioral predictors of self-reported oral health-related quality of life. Qual Life Res. 2013;22:559–566. 10.1007/s11136-012-0173-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Choi MK. The impact of Medicaid insurance coverage on dental service use. J Health Econ. 2011;30:1020–1031. 10.1016/j.jhealeco.2011.08.002 [DOI] [PubMed] [Google Scholar]
- 31.Razak PA, Richard KMJ, Thankachan RP, Hafiz KAA, Kumar KN, Sameer KM. Geriatric oral health: a review article. J Int Oral Health. 2014;6:110–116. [PMC free article] [PubMed] [Google Scholar]
- 32.Kim SY, Kim JE, Kim HN, et al. Association of self-perceived oral health and function with clinically determined oral health status among adults aged 35–54 years: a cross-sectional study. Int J Environ Res Public Health. 2018;15:E1681. 10.3390/ijerph15081681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yörük BK. Health insurance coverage and self-reported health: new estimates from the NLSY97. Int J Health Econ Manag. 2016;16(3):285–295. 10.1007/s10754-016-9189-1 [DOI] [PubMed] [Google Scholar]
- 34.Widener MJ, Metcalf SS, Northridge ME, Chakraborty B, Marshall SM, Lamster IB. Exploring the role of peer density in the self-reported oral health outcomes of older adults: a kernel density based approach. Health Place. 2012;18:782–788. 10.1016/j.healthplace.2012.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kino S, Kawachi I. The impact of ACA Medicaid expansion on socioeconomic inequality in health care services utilization. PLoS One. 2018;13:e0209935. 10.1371/journal.pone.0209935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kim JH, Park EC. Impact of socioeconomic status and subjective social class on overall and health-related quality of life. BMC Public Health. 2015;15:783. 10.1186/s12889-015-2014-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.