Abstract
Epidemiological studies have documented a high incidence of diabetes in hypertensive patients.Insulin resistance is defined as a less than expected biologic response to a given concentration of the hormone and plays a pivotal role in the pathogenesis of diabetes. However, over the last decades, it became evident that insulin resistance is not merely a metabolic abnormality, but is a complex and multifaceted syndrome that can also affect blood pressure homeostasis. The dysregulation of neuro-humoral and neuro-immune systems is involved in the pathophysiology of both insulin resistance and hypertension. These mechanisms induce a chronic low grade of inflammation that interferes with insulin signalling transduction. Molecular abnormalities associated with insulin resistance include the defects of insulin receptor structure, number, binding affinity, and/or signalling capacity. For instance, hyperglycaemia impairs insulin signalling through the generation of reactive oxygen species, which abrogate insulin-induced tyrosine autophosphorylation of the insulin receptor. Additional mechanisms have been described as responsible for the inhibition of insulin signalling, including proteasome-mediated degradation of insulin receptor substrate 1/2, phosphatase-mediated dephosphorylation and kinase-mediated serine/threonine phosphorylation of both insulin receptor and insulin receptor substrates. Insulin resistance plays a key role also in the pathogenesis and progression of hypertension-induced target organ damage, like left ventricular hypertrophy, atherosclerosis and chronic kidney disease. Altogether these abnormalities significantly contribute to the increase the risk of developing type 2 diabetes.
Keywords: Cardiovascular risk, Left ventricular hypertrophy, Atherosclerosis, Microalbuminuria, Vascular inflammation
Essential Hypertension and Type 2 Diabetes the Link
Essential hypertension is characterised by both hemodynamic and metabolic abnormalities. Epidemiological studies have documented a high incidence of diabetes in hypertensive patients. The Women’s Health Study [1] showed that in healthy, middle-aged women, blood pressure (BP), and BP progression are strong and independent predictors of incident type 2 diabetes (T2D). Similarly, the Monitoring Trends and Determinants on Cardiovascular Diseases/Cooperative Health Research in the Region of Augsburg Cohort Study [2] showed that high normal BP, as well as, established hypertension were strongly and independently related to the development of an incident T2Din men. However, in women only established hypertension significantly increased the risk of T2D. Although these studies clearly demonstrated the link between hypertension and T2D, they lacked of rigorous criteria to diagnosis T2D, since in many cases the diagnosis was based on self-reported incident diabetes. However, Kramer et al. [3] demonstrated, in the cohort of subjects of The Rancho Bernardo Study, that hypertension and pre-hypertension increase the risk of T2D. In this study, the new onset of T2Dwas assessed with oral glucose tolerance test (OGTT). In particular, OGTT was performed at baseline and after a mean follow-up period of 8.3 years. This methodological approach gave a more precise information about the incidence of T2D in hypertensive patients during the follow-up. Therefore, the results of this study rather than being merely confirmatory, reinforced the concept that hypertension enhances the risk of developing T2D. The risk increases by 13% and 15% for increments of 10 mmHg and 5 mmHg for systolic and diastolic BP, respectively. These data were confirmed by two population-based studies: the Gothemburg Primary Prevention Study [4] and Tehran Lipid and Glucose Study [5]. We extended these epidemiological data demonstrating that in a cohort of hypertensives, those with an uncontrolled hypertension had a higher risk of developing T2D. In particular, in nondiabetic hypertensive subjects, uncontrolled BP was associated with twofold increased risk of incident T2D independently of age, body mass index (BMI), baseline BP, or fasting glucose [6]. The strong association between hypertension and diabetes has been further documented by the evidence that patients with essential hypertension and concomitant hypertension-related target organ damage (TOD), such as left ventricular hypertrophy (LVH)end/or carotid atherosclerosis (CA), are at higher risk of incident T2D, compared to those without TOD. In fact, in 4176 treated hypertensive patients, LVH and CA were significant predictors of new onset T2D,independently of initial metabolic profile, anti-hypertensive therapy, and other significant covariates[7]. Of note, the association between TOD and incidence of T2D has also been documented in unselected populations; in particular, the Strong Heart Study showed that the cardio-renal TOD increases the risk of incident T2D at 4 years [8].
Altogether these data strongly support the notion that essential hypertension and T2Dshare a common pathophysiological mechanism.
Insulin Resistance and Hypertension
Insulin resistance is defined as a less than expected biologic response to a given concentration of the hormone and plays a pivotal role in the pathogenesis of T2D [9]. For many years, the term insulin resistance has been associated exclusively with an inadequate effect of insulin on glucose metabolism and did not address other aspects of insulin action. However, insulin is a pleiotropic hormone and exerts a multitude of effects on lipid and protein metabolism, ion and amino acid transport, cell cycle, proliferation and differentiation, and nitric oxide (NO) synthesis (Fig. 1).
Fig. 1.
The pleiotropic action of insulin. Insulin regulates different physiological process including the glucose, protein and lipid metabolism, the cell cycle, growth and survival, the vascular tone and inflammation, the ions and amino-acid exchange/transport, and neuro-hormonal activity. Na+, sodium; Ca++, calcium; RAAS, Renin–angiotensin–aldosterone system; TNF-α, tumor necrosis factor-α; IL-6, interleukin-6; IL-1, interleukin-1; PAI-1, plasminogen activator inhibitor-1
In the context of the vascular system, insulin stimulation induces vasodilation through NO production [10], and the state of insulin resistance impairs NO synthesis and vasodilation. Insulin resistance contributes to increase BP through several mechanisms, among which are the enhanced tissue angiotensin II (AngII) and aldosterone activities [11, 12], the increased sympathetic nervous system activity [13], and oxidative stress [14]. However, emerging evidence indicate that endothelial dysfunction may represent the upstream event preceding peripheral reduction of insulin sensitivity, due to impairment of peripheral tissue blood flow. This phenomenon is known as “endothelial insulin resistance” and is mediated by increased oxidative stress, through a protein kinase C beta-dependent pathway. In fact, the suppression of reactive oxygen species-dependent pathways in the endothelium has been shown to restore insulin delivery to peripheral organs by preserving NO availability [15, 16]. According to this view, endothelial loss of insulin signalling may represent an important mechanism linking hypertension to endothelial dysfunction. Molecular and pathophysiological mechanisms underlying the reciprocal relationship between insulin resistance and hypertension result in a vicious cycle which reinforces the link between metabolic and hemodynamic disorders. In fact, insulin resistance affects negatively myocardial energetic efficiency in hypertensive patients [17] and in unselected population [18].
The association between hypertension, insulin resistance, and resultant hyperinsulinemia is well documented [19]. In untreated patients with essential hypertension, fasting and postprandial insulin levels are higher than in normotensive controls, with a direct correlation between plasma insulin concentrations and BP. Interestingly, the association of insulin resistance and essential hypertension does not occur in secondary hypertension [20]. Of note, insulin resistance and hyperinsulinemia also exist in rats with genetic hypertension such as Dahl hypertensive and spontaneously hypertensive rat (SHR) strains. Altogether these data suggest the existence of a common genetic pathway for essential hypertension and insulin resistance, a concept that is also supported by the finding of altered glucose metabolism in normotensive offspring of hypertensive patients [21]. The common genetic background of insulin resistance and hypertension is further supported by the discovery of specific genetic abnormalities in people with combinations of insulin resistance, obesity, dyslipidaemia, and hypertension. These defects include a mutation of the β3-adrenergic receptors (ARs), which regulates lipolysis in visceral fat, and the presence of two mutated genes on chromosome 7q, one that controls insulin levels and BP and the other, leptin, a peptide that regulates food intake [22]. Deficiency in CD36, a known fatty acid transporter, is also believed to be involved in the predisposition to insulin resistance and hypertension in Asians [23].The relationship between insulin resistance and hypertension is a complex and multifactorial phenomenon which involves both genetic basis and environmental factors. In the western countries, sedentary life style and hypercaloric food intake are endemic behaviours which play a key role in the development of insulin resistance, mainly through epigenetic modifications. In particular, DNA methylation, histone modifications and noncoding RNA activity (miRNA) are the principal mechanisms that alter the protein transcription and expression, which, in turn, modify the cellular phenotype. The translocation of GLUT 4 to the cell membrane is the principal step of insulin-induced glucose uptake. Insulin resistance state is characterized by lower expression levels and impaired translocation of GLUT 4. Experimental data indicate that the metilation of DNA, induced by over-nutrition during fetal life, decreases the gene expression of proteins involved in insulin signal transduction, like GLUT 4. The expression of GLUT 4 is also affected by mi RNA. In particular, in myocytes the miRNA 106b impairs insulin signalling by decreasing insulin-stimulated translocation of GLUT 4. Mitochondrial dysfunction, which also plays a key role in the genesis of insulin resistance, is affected by epigenetic modifications. In particular, methylation of the gene encoding for peroxisome proliferator-activated receptor alpha (PPARα) has been reported in obese subjects. These data reinforce the hypothesis that epigenetic modifications are at lease partially responsible for the link between behaviour habits and insulin resistance [24].
Insulin Resistance Directly Affects Blood Pressure Control
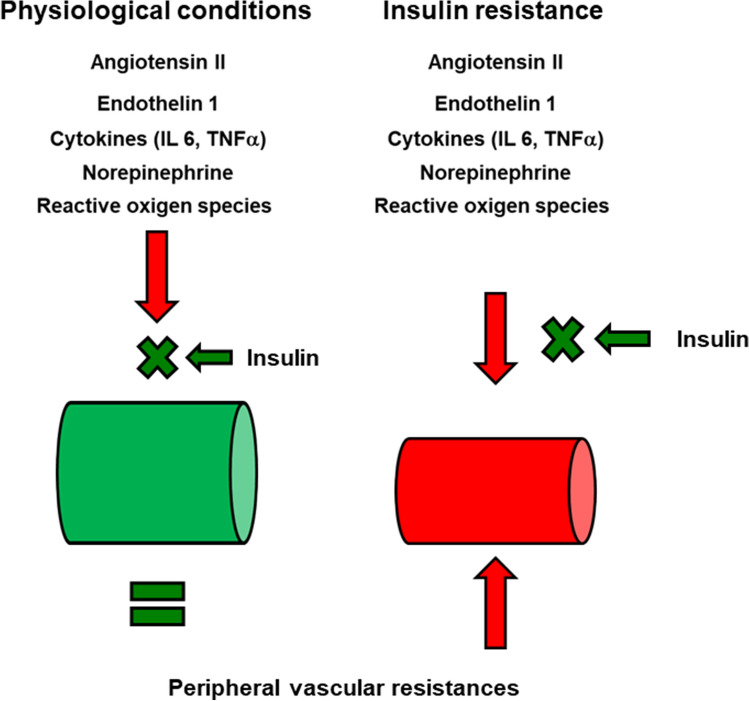
In healthy subjects, insulin evokes a net reflex in sympathetic outflow and at the same time it blunts the vasoconstrictive effect resulting from this sympathetic activation. On the contrary, in hypertensive patients insulin evokes a sympathetic activation that is three times greater than in normal subjects, and moreover its vaso-relaxant action is impaired [13]. This mechanism is involved in dysregulation of peripheral vascular resistance, which contributes to increase BP levels (Fig. 2). The key role of insulin resistance in the pathogenesis of hypertension has been further supported by the evidence that in aortic rings of SHR the resistance to the vascular action of insulin is already present at the age of 5 weeks, before the onset of arterial hypertension [25], suggesting that in SHR vascular resistance to insulin action is specific and not related to the compensatory hyperinsulinemia or hyperglycemia. On the other hand, we have demonstrated, in rats fed for 6 months with hypercaloric diet that the increase of BP and the development of LVH are associated with both hyperinsulinemia or hyperglycemia [26]. In addition, insulin resistance and the resultant hyperinsulinemia are involved in the development of hypertension-related TOD, through the abnormalities of the counter-regulatory effects of insulin. In particular, impairment of cell membrane ion exchange, enhanced sympathetic nervous and renin-angiotensin systems, suppressed atrial natriuretic peptide activities, sodium retention, and plasma volume expansion contribute to the development of chronic kidney disease, LVH, CA.
Fig. 2.
Regulation of peripheral vascular resistances by insulin and effects of insulin resistance. In physiological conditions, insulin antagonizes (green arrows) the effects of vasoconstrictor mediators (red arrows), contributing to maintain the normal vascular tone. Insulin resistance (red arrows), impairs the capability of insulin to counterbalance the action of vasoconstrictor mediators, resulting in the increase of vascular peripheral resistances. TNF-α, tumor necrosis factor-α; IL-6, interleukin-6
Molecular Mechanisms of Insulin Resistance
Abnormalities of insulin signalling account for insulin resistance. Insulin mediates its action on target organs through phosphorylation of a transmembrane-spanning tyrosine kinase receptor, the insulin receptor (IR). The binding of insulin to the α subunit of its receptor activates the tyrosine kinase of the β subunit of the receptor, leading to autophosphorylation, as well as tyrosine phosphorylation of several IR substrates (IRS), including IRS-1 and IRS-2 [27]. These, in turn, interact with phosphatidylinositol 3-kinase (PI3K). Activation of PI3K stimulates the main downstream effector Akt, a serine/theronine kinase, which stimulates the glucose uptake through the translocation of the major glucose transporter GLUT-4 to the plasma membrane [28]. Abnormalities of the IR function that may contribute to insulin resistance include the defects of receptor structure, number, binding affinity, and/or its signalling capacity. It is noteworthy that hyperglycaemia, accounts for the development of insulin resistance through the generation of reactive oxygen species (ROS), which abrogate insulin-induced tyrosine autophosphorylation of IR [29]. In addition, several mechanisms have been described as responsible for the inhibition of insulin-stimulated tyrosine phosphorylation of IR and the IRS proteins, including proteasome-mediated degradation [30], phosphatase-mediated dephosphorylation [31], and kinase-mediated serine/threonine phosphorylation [32]. In particular, phosphorylation of IRS-1 on serine Ser612 causes dissociation of the p85 subunit of PI3-K, inhibiting further signalling. In addition, phosphorylation of IRS-1 on Ser307 results in its dissociation from the IR and triggers proteasome-dependent degradation, also impairing insulin signalling.
The mechanistic role of abnormalities of IR or IRS-1 signalling in the pathogenesis of insulin resistance and hypertension is supported by several pioneering studies performed in genetically engineered mice. In particular, transgenic mice with targeted disruption of the IRS-1 gene, exhibited higher BP and plasma triglyceride levels compared to wild-type mice. They also showed impairment of endothelium-dependent vascular relaxation [33]. On the other hand, mice heterozygous for knockout of the IR showed fasting blood glucose, insulin, free fatty acid, and triglyceride levels similar to those of wild-type mice. Interestingly, these mice had increased systolic BP and blunted insulin-stimulated aortic endothelial nitric oxide synthase (NOS) phosphorylation [34]. The results of these studies demonstrate that the abnormalities of IR or IRS signalling play a mechanistic role in the development of hypertension, independently form glucose homeostasis and plasma insulin levels, and indicate that insulin resistance by itself is involved the pathogenesis of hypertension.
It is noteworthy that IR defects are tissue-specific and depends upon the type of stress; therefore, the insulin resistance phenomenon can be localized in specific tissues and does not necessarily associated with metabolic abnormalities.
Insulin Resistance and Neuro-Hormonal Activities in Hypertension
Several pathophysiological mechanisms contribute to impair insulin signal in hypertension, such as renin angiotensin and sympathetic nervous systems, and oxidative stress. On the other hand, mechanisms playing a protective role against insulin resistance, (i.e. natriuretic peptides) are impaired in hypertension.
Renin-angiotensin system
In vivo and in vitro studies have shown that Ang II stimulation induces insulin resistance [35, 36]. Interventional studies have documented that angiotensin converting enzyme (ACE) inhibitors [37] and angiotensin type 1 receptor blockers [38] reduce the incidence of T2D in hypertensive patients. Therefore, the dysregulation of the renin-angiotensin system observed in hypertension is likely to impair insulin signalling and contribute to insulin resistance. Furthermore, it has been reported that an ACE-inhibitor-based long term treatment does not reduce the occurrence of diabetes mellitus in subjects with impaired glucose tolerance [39]. This observation suggests that the pathophysiological mechanisms underlying the development of insulin resistance in hypertensive patients are partially different from those responsible for impaired insulin sensitivity in diabetics.
Ang II acting through angiotensin type 1 (AT1) receptor inhibits the actions of insulin via generation of reactive oxygen species (ROS) by NADPH oxidase [40]. ROS are important intracellular second messengers. The generation of ROS is implicated in Ang II-induced insulin resistance. At this regard, it has been Epidemiological studies have documented a high incidence of diabetes in hypertensive patients.Insulin resistance is defined as a less than expected biologic response to a given concentration of the hormone and plays a pivotal role in the pathogenesis of diabetes. However, over the last decades, it became evident that insulin resistance is not merely a metabolic abnormality, but is a complex and multifaceted syndrome that can also affect blood pressure homeostasis. The disregulation of neuro-humoral and neuro-immune systems is involved in the pathophysiology of both insulin resistance and hypertension.
These mechanisms induce a chronic low grade of inflammation that interferes with insulin signalling transduction. Molecular abnormalities associated with insulin resistance include the defects of insulin receptor structure, number, binding affinity, and/or signalling capacity. For instance, hyperglycaemia impairs insulin signalling through the generation of reactive oxygen species, which abrogate insulin-induced tyrosine autophosphorylation of the insulin receptor. Additional mechanisms have been described as responsible for the inhibition of insulin signalling, including proteasome-mediated degradation of insulin receptor substrate 1/2, phosphatase-mediated dephosphorylation and kinase-mediated serine/threonine phosphorylation of both insulin receptor and insulin receptor substrates. Insulin resistance plays a key role also in the pathogenesis and progression of hypertension-induced target organ damage, like left ventricular hypertrophy, atherosclerosis and chronic kidney disease. Altogether these abnormalities significantly contribute to the increase the risk of developing type 2 diabetes. That in vascular smooth muscle cells (VSMC) isolated from rat thoracic aorta, Ang II profoundly decreases IRS-1 protein levels via ROS-mediated phosphorylation of IRS-1 on Ser307 and subsequent proteasome-dependent degradation [41] (Fig. 3). The key role of ROS in the pathogenesis of Ang II-induced insulin resistance has been also confirmed by in vivo studies. In particular, in rats chronic infusion of Ang II induced hypertension and reduced insulin-evoked glucose uptake during hyperinsulinemic-euglycemic clamp, and increased plasma cholesterylester hydroperoxide levels, indicating an increased oxidative stress. Treatment with tempol, a superoxide dismutase mimetic, normalized plasma cholesterylester hydroperoxide levels in Ang II-infused rats. In the same setting, tempol normalized insulin resistance in Ang II-infused rats, and enhanced insulin-induced PI3K activation, suggesting that Ang II-induced insulin resistance can be restored by removing the oxidative stress [42]. On the other hand, in the endothelial cells, Ang II induces insulin resistance through the phosphorylation of IRS-1 at Ser312 and Ser616 via JNK- and ERK1/2-dependent mechanisms, respectively. This impairs the interaction of IRS-1 with the p85 regulatory subunit of PI3K and compromises the insulin vasodilatory signalling pathway involving PI3K/Akt/eNOS [43]. A further mechanism that account for role of insulin resistance in the aetiology of hypertension is the upregulation of AT1 receptors induced by hyperinsulinemia. This potentiates the detrimental effects of Ang II on cardiovascular (CV) system. Altogether, these observations provide clear insights of the pathogenic mechanisms of Ang II–induced insulin resistance in the development of hypertension.
Fig. 3.
Molecular mechanisms that account for angiotensin II-induced insulin resistance. The binding of insulin to its own receptor evokes the tyrosine autophosphorylation of the β subunit, which, in turn activates, in sequence, the insulin receptor substrate-1 and phosphatidylinositol 3-kinase (green arrows). This cascade, accounts for the biological effects of insulin. Angiotensin II stimulation, through the activation of NADPH oxidase, stimulates the generation of reactive oxygen species, which, in turn promote the threonine phosphorylation of insulin receptor substrate-1 (red arrows). This induces the proteasome-dependent degradation of insulin receptor substrate-1, interrupting the insulin signalling cascade. Ser, serine; P, phospho; Tyr, tyrosine; ROS, reactive oxygen species; PI3K, phosphatidylinositol 3-kinase; IRS-1, insulin receptor substrate-1
Sympathetic Nervous System
Dysregulation of sympathetic nervous system is a feature of hypertension [44]. It has been documented that increased sympathetic tone resulting in an abnormal stimulation of β-ARs, is able to induce insulin resistance through the activation of different serine/threonine kinases that blunt insulin signal by phosphorylating IR or IRS-1. It has been demonstrated that the molecular mechanisms accounting for β-ARs-induced insulin resistance are tissue-specific and depend upon the receptor subtype expressed by the organ/tissue. For instance, adipocytes and cardiac myocytes are both target organs of insulin, and mainly express β3 and β1-ARs, respectively. β-ARs stimulation results in an impairment of insulin signalling and insulin-induced glucose uptake, which profoundly differs between the two cell types regarding the kinetic and molecular mechanisms involved. In particular, β-ARs stimulation in adipocytes impairs insulin signalling within few minutes, whereas, in cardiac myocytes stimulation of β-ARs has a biphasic effect on insulin-stimulated glucose uptake, with an initial additive followed by an inhibitory action. β3-ARs stimulation impairs insulin signalling through protein kinase A (PKA)- and protein kinase C (PKC)-dependent mechanisms; interestingly β3-ARs stimulation does not phosphorylate/activate Akt [45]. On the contrary, in cardiac myocytes Akt plays a key role in the cross-talk between β1-ARs and IR. Actually, upon the phosphorylation site, Akt can have a favourable or detrimental effect on insulin signalling and insulin-induced glucose uptake. In particular, short-term β-ARs stimulation induces Akt phosphorylation in threonine that results in an increase in glucose uptake, whereas long-term stimulation induces Akt phosphorylation in serine and impairs insulin evoked-glucose uptake and insulin-induced tyrosine autophosporylation of IR [46]. In addition, it has been demonstrated in cardiac myocytes, that chronic Akt activation is sufficient to impair insulin signal by inducing IRS-1 phosphorylation and proteasome-dependent degradation [47].
Insulin Resistance and Hypertension Related Target Organ Damage
LVH, CA, and renal dysfunction are expression of hypertension-evoked TOD, and are independent risk factors for both fatal and nonfatal cardio- and cerebro-vascular events [48–52].Several studies have shown that insulin resistance promotes the development of left ventricular hypertrophy, carotid atherosclerosis and chronic kidney disease (CKD).
Left Ventricular Hypertrophy
Development of LVH is a complex and multifactorial process which involves genetic, hemodynamic and anthropometric components, neuro-hormonal stimulation, growth factors and inflammatory mediators [53–55]. The hemodynamic and metabolic disorders associated with insulin resistance increase the risk LVH. Insulin and insulin-like growth factor (IGF) -1 are powerful independent determinants of LV mass and geometry in untreated subjects with essential hypertension and normal glucose tolerance [56]. The presence of both insulin resistance and hypertension in the same patient results in a mixed pattern of cardiac hypertrophy, caused by an elevation in both cardiac preload and afterload [57]. Experimental data suggest that insulin might be involved in the pathogenesis of both the concentric and eccentric patterns of LVH. Stimulation of myocardial cell growth and activation of the sympathetic nervous system might preferentially lead to concentric LV hypertrophy through a direct trophic effect and pressure overload, whereas sodium and water retention could lead to eccentric LV hypertrophy through volume overload [58]. The direct effect of insulin on myocardial cell growth could be mediated, at least in part, by the IGF-1 receptors [59]. In addition, the myocardium in the insulin-resistant individual shows the presence of mononuclear cell infiltration all along the conduction system making the myocardium in the insulin-resistant hypertensive patient an ideal substrate for cardiac arrhythmia and sudden death.
Atherosclerosis
Several epidemiological studies have underlined the role of insulin resistance, hyperinsulinemia in the development of atherosclerosis, and in the pathogenesis of its clinical consequences. Several mechanisms have been proposed as responsible for these phenomena. These include both direct effects on the arterial wall and indirect actions on lipid and glucose metabolism. Considerable evidence exists that demonstrate that endothelium as a physiological target of insulin and, consequently, a potential link between insulin resistance and atherosclerosis. In the endothelium, the stimulation of IRs activates insulin signaling via the PI3-K pathway, leading to NO production. The production of NO by endothelial cells, stimulated by insulin or insulin-like growth factor, leads to a host of anti-inflammatory and antithrombotic effects, which are antiatherogenic. The anti-inflammatory effects of NO include the decreases of expression of vascular cell adhesion molecule-1, intracellular adhesion molecule-1, and E-selectin and reduced secretion of the proinflammatory cytokines monocyte chemoattractant protein–1 and tumor necrosis factor-α (TNF-α). Interestingly, the insulin-induced antithrombotic effects depends on gene expression regulation, which decreases the platelet adhesion by increasing prostacyclin production [60]. Of note, the gene encoding for coagulation factor II thrombin receptor, which is involved in the enhanced risk of coronary artery diseases in patients with hypertension [61], and it has been recently proposed as a marker of clinical conditions characterized by insulin resistance like metabolic syndromes, obesity, T2D, hepatic steatosis, and atherosclerosis [62].
Atherosclerotic process is regulated by inflammatory mechanisms [63–65]. Notably, insulin resistance has been recognized as a chronic, low-level, inflammatory state [66]. Although several mechanisms may contribute to the pathogenesis of hypertension, the NO system appears to play a major role. NO is an important messenger molecule that plays a critical role in a wide variety of physiological functions, including immune modulation, vascular relaxation, neuronal transmission, and cytotoxicity. Interestingly, the polymorphism of the promoter of the inducible nitric oxide synthase (iNOS) gene, NOS2A, revealed a positive association with essential hypertension [67]. This aspect is linked to insulin resistance because insulin stimulation of glucose uptake in skeletal muscle and adipose tissue is a NO-dependent phenomenon. Moreover, iNOS has been shown to be crucial for the development of insulin resistance [68]. The role that inflammation plays in atherosclerosis is amplified by the renin-angiotensin system via its effects on adhesion molecules, growth factors, and chemoattractant molecules, which modulate the migration of inflammatory cells into the subendothelial space. Clinical and experimental data have increased our knowledge on the effects of the Ang II. In particular, it has been documented that Ang II stimulates the production of ROS through its AT1 receptor [69], resulting in a proinflammatory modulator.
The low grade of inflammation is a common feature of atherosclerosis and insulin resistance. The two major determinants of this state are the pro-inflammatory cytokines, TNF-α and interleukin-6 (IL-6). The available experimental data indicate that TNF-α is involved in the pathophysiology of hypertension. In particular, in vitro, TNF-α stimulates the production of endothelin-1 and angiotensinogen. Moreover, in SHR, TNF-α synthesis and secretion and fat angiotensinogen mRNA are increased in response to lipopolysaccharide (LPS) stimulation in comparison with non-hypertensive control rats [70]. At molecular level, TNF-α blocks the action of insulin in cultured cells [71], though the serine phosphorylation of IRS-1, decreasing the tyrosine kinase activity of the insulin receptor [72]. The key role of TNF-α in the pathogenesis of hypertension has been also documented in humans. In particular, the TNF-α gene locus seems to be involved in insulin resistance-associated hypertension [73]. A positive correlation has been found between serum TNF-α concentration and both SBP and insulin resistance [74]. Up-regulation of TNF-α secretion has also been observed in peripheral blood monocytes from hypertensive patients [75]. TNF-α also determines endothelial dysfunction linked to insulin resistance [76]. Neutralization of TNF-α in obese fa/fa rats by administration of a sTNFR-IgG chimeric protein substantially improved insulin sensitivity and restored the tyrosine kinase activity in fat and muscle [77]. In contrast, treatment of T2D or obese human subjects with an antibody specific for TNF had no effect on insulin sensitivity [78].
IL-6 is a multifunctional cytokine produced by many different cell types, including immune cells, endothelial cells, fibroblasts, myocytes, and adipose tissue, which mediates inflammatory as well as stress-induced responses. It has been documented that BP was a significant and independent predictor of circulating IL-6 concentrations in women but not in men [79]. A polymorphism in the promoter of the IL-6 gene has also shown divergent associations with BP [80]. IL-6 stimulates the central nervous system and the sympathetic nervous system, which may result in hypertension [81]. However, other mechanisms cannot be excluded. IL-6 might increase in parallel to the modification of the redox state of the vascular wall in chronic hypertension, as occurs in some animal models of hypertension [82]. IL-6 is a well-characterized acute inducer of fibrinogen, which is a determinant of blood viscosity. Finally, IL-6 might increase BP enhancing the expression of angiotensinogen, leading to higher concentration of Ang II. Interestingly, leptin, a cytokine-like molecule increasingly recognized to regulate several inflammatory pathways acting on a receptor of the IL-6 family seems also to be associated with hypertension. The leptin signal, via central leptin receptors, is believed to interact with the central sympathetic nervous system [83]. Infusion of leptin leads to increases in BP [84]. Transgenic mice overexpressing leptin had elevated BP, which is normalized by adrenergic and ganglionic blockade [85].
Renal Disease
Diabetes, hypertension and insulin resistance/hyperinsulinemia, which frequently coexist, are the leading cause CKD which often evolves in end-stage renal disease (ESRD). Hypertension is believed to contribute to CKD by increasing glomerular capillary pressure, proteinuria, endothelial dysfunction, and sclerosis, leading to nephron damage [86]. Insulin resistance is associated with activation of both renin-angiotensin system and sympathetic nervous system activities, contributing to increased renal sodium reabsorption, associated fluid retention and hypertension [87]. Moreover, this state is accompanied by the increased endothelial cells proliferation and intrarenal lipid and hyaluronate deposition in the matrix and inner medulla [88]. These depositions increase intrarenal pressure and volume in the tightly encapsulated kidney, leading to parenchymal prolapse and urine outflow obstruction, which result in slow tubular flow and subsequently increased sodium reabsorption, especially in the loop of Henle. This leads to inappropriately small natriuretic response to saline load at mean and glomerular pressure, often referred to as “impaired pressure natriuresis”. These functional and structural changes provoke compensatory lowered renal vascular resistance, elevated kidney plasma flow, glomerular hyperfiltration, and stimulation of renin angiotensin system, despite volume expansion. In addition, these changes in combination with the raise in BP levels associated with the insulin-resistant state increase the tubular reabsorption and maintain sodium balance. The persistence of these compensatory responses, increasing glomerular wall stress, precipitate gradual nephron loss, glomerulosclerosis and eventually end-stage renal disease. Glomerulosclerosis in the insulin-resistant kidney is peculiar and characterized by lower rate of nephrotic syndrome, fewer lesions of segmental sclerosis and a greater glomerular size compared with the idiopathic variety. In summary, persistence of insulin resistance and suboptimal control of associated hemodynamic and metabolic abnormalities cause renal injury with functional as well as structural nephron loss contributing to elevated BP, which in turn leads to further renal injury, thereby setting off a vicious circle of events leading to further elevated BP and renal injury.
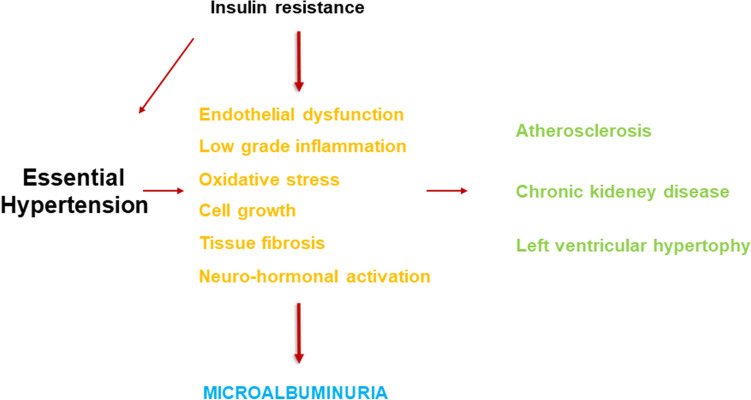
Microalbuminuria is now established as a modifiable predictor of CV morbidity and mortality [52, 89] and is considered a manifestation hypertension-induced TOD. Despite its strong association with CV risk, the exact pathogenic mechanisms that link microalbuminuria to CV diseases remains unknown. Evidence has been garnered that microalbuminuria is a marker of generalized endothelial dysfunction and consequently a risk factor for CV diseases. In particular, this abnormality has been characterized by the presence of transmembrane leakiness [90]. In addition, microalbuminuria has also been associated with alterations in hemodynamic and vascular responses. In general, microalbuminuria can be considered as an early marker of generalized hypertension-evoked TOD (Fig. 4) in the continuum of CV disease.
Fig. 4.
Relationship between microalbuminuria and insulin resistance in the continuum of cardiovascular disease. Microalbuminuria, is clinical marker of activation of the insulin resistance-dependent pathogenic mechanisms involved in the genesis and progression of hypertension and hypertension-induced target organ damage
Conclusions
Epidemiological data show that hypertension is a risk factor for the development of T2D.The combination of hypertension and T2D increases CV risk and requires a strict control of both BP and glycaemia [91]. Insulin resistanceis involved in the pathogenesis and progression of hypertension as well as T2D.The low-grade of inflammation induced by insulin resistance is the principal mechanism that accounts for development of endothelial dysfunction, hypertension-induced TOD, and metabolic abnormalities [92] (Fig. 5). Altogether these data encourage the adoption of a holistic strategy to prevent the development of insulin resistance. In particular, it is well known that hypocaloric diet, and regular exercise training improve insulin sensitivity [93]. Both are recommended for primary and secondary CV prevention. It is noteworthy that consistent body of evidence supports the notion that exercise training is able to modify the epigenetics changes that are involved in the development of insulin resistance [24].
Fig. 5.
Insulin resistance is a time-dependent organ and tissue specific phenomenon. Insulin resistance contributes to the dysregulation of peripheral vascular resistance, resulting in an increase of blood pressure. In arterial hypertension, insulin resistance participates to the development of target organ damage. The persistence of insulin resistance induces the metabolic abnormalities that account for development of type 2 diabetes. The increased caloric intake and the sedentary habit are the principal environmental factors that account for the development and progression of insulin resistance
The dysregulation of renin-angiotensin system plays a pivotal role in the development of insulin resistance; thus, the prevention of incident T2D in patients with hypertension requires the inhibition of RAS with AT1 antagonist or ACE inhibitors [94]. Finally, in the last decades the beneficial effects on the CV system of different classes of glucose-lowering agents have been reported. In particular, Glucagon-like peptide-1 receptor agonists (GLP-1RAs) stimulate insulin release and supress glucagon synthesis. There is growing body of evidence that the GLP-1RAs improve CV outcomes in type 2 diabetes. In fact, they are recommended as first- and second-choice agents in diabetic patients at high CV risk or with overt atherosclerosis, independently from achievement of glycemic control [95, 96].
In conclusion, the prevention of the insulin resistance-induced continuum of CV disease requires an integrated approach which involves non pharmacologic and pharmacologic therapies.
Declarations
Funding
Open access funding provided by Università degli Studi di Napoli Federico II within the CRUI-CARE Agreement. Giuseppe Di Gioia received a grant from the Cardiopath PhD program.
Conflicts of interest/Competing interests
None.
Availability of data and material
Findings were gathered from the published articles in the literature.
Authors contribution
CM and CM had the idea for this article, RI, MAL, and GDG, performed the literature search, CM and CM drafted, and EB critically revised the work.
References
- 1.Conen D, Ridker PM, Mora S, Buring JE, Glynn RJ. Blood pressure and risk of developing type 2 diabetes mellitus: the Women’s Health Study. Eur Heart J. 2007;28:2937–2943. doi: 10.1093/eurheartj/ehm400. [DOI] [PubMed] [Google Scholar]
- 2.Meisinger C, Döring A, Heier M. Blood pressure and risk of type 2 diabetes mellitus in men and women from the general population: the Monitoring Trends and Determinants on Cardiovascular Diseases/Cooperative Health Research in the Region of Augsburg Cohort Study. J Hypertens. 2008;26:1809–1815. doi: 10.1097/HJH.0b013e328307c3e9. [DOI] [PubMed] [Google Scholar]
- 3.Kramer CK, von Mühlen D, Barrett-Connor E. Mid-life blood pressure levels and the 8-year incidence of type 2 diabetes mellitus: the Rancho Bernardo study. J Hum Hypertens. 2010;24:519–524. doi: 10.1038/jhh.2009.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stahl CH, Novak M, Lappas G, Wilhelmsen L, Björck L, Hansson P-O, Rosengren A. High-normal blood pressure and long-term risk of type 2 diabetes: 35-year prospective population based cohort study of men. BMC Cardiovasc Disord. 2012;15(12):89. doi: 10.1186/1471-2261-12-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Derakhshan A, Bagherzadeh-Khiabani F, Arshi B, Ramezankhani A, Azizi F, Hadaegh F. Different combinations of glucose tolerance and blood pressure status and incident diabetes, hypertension, and chronic kidney disease. J Am Heart Assoc. 2016;5:e003917. doi: 10.1161/JAHA.116.003917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Izzo R, de Simone G, Chinali M, Iaccarino G, Trimarco V, Rozza F, et al. Insufficient control of blood pressure and incident diabetes. Diabetes Care. 2009;32:845–850. doi: 10.2337/dc08-1881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Izzo R, de Simone G, Trimarco V, Gerdts E, Giudice R, Vaccaro O, De Luca N, Trimarco B. Hypertensive target organdamagepredictsincidentdiabetesmellitus. Eur Heart J. 2013;34:3419–3426. doi: 10.1093/eurheartj/eht281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.de Simone G, Wang W, Best LG, Yeh F, Izzo R, Mancusi C, Roman MJ, Lee ET, Howard BV, Devereux RB. Target organ damage and incident type 2 diabetes mellitus: the Strong Heart Study. Cardiovasc Diabetol. 2017;16:64. doi: 10.1186/s12933-017-0542-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Olefsky J, Farquhar JW, Reaven G. Relationship between fasting plasma insulin level and resistance to insulin-mediated glucose uptake in normal and diabetic subjects. Diabetes. 1973;22:507–513. doi: 10.2337/diab.22.7.507. [DOI] [PubMed] [Google Scholar]
- 10.Scherrer U, Randin D, Vollenweider P, Vollenweider L, Nicod P. Nitric oxide release accounts for insulin’s vascular effects in humans. J Clin Invest. 1994;94:2511–2515. doi: 10.1172/JCI117621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Steinberg HO, Chaker H, Leaming R, Johnson A, Brechtel G, Baron AD. Obesity/insulin resistance is associated with endothelial dysfunction. Implications for the syndrome of insulin resistance. J Clin Invest. 1996;97:2601–2610. doi: 10.1172/JCI118709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fukuda N, Satoh C, Hu WY, Nakayama M, Kishioka H, Kanmatsuse K. Endogenous angiotensin ii suppresses insulin signaling in vascular smooth muscle cells from spontaneously hypertensive rats. J Hypertens. 2001;19:1651–1658. doi: 10.1097/00004872-200109000-00018. [DOI] [PubMed] [Google Scholar]
- 13.Lembo G, Napoli R, Capaldo B, Rendina V, Iaccarino G, Volpe M, Trimarco B, Sacca L. Abnormal sympathetic overactivity evoked by insulin in the skeletal muscle of patients with essential hypertension. J Clin Invest. 1992;90:24–29. doi: 10.1172/JCI115842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sowers JR. Hypertension, angiotensin ii, and oxidative stress. N Engl J Med. 2002;346:1999–2001. doi: 10.1056/NEJMe020054. [DOI] [PubMed] [Google Scholar]
- 15.Tabit CE, Chung WB, Hamburg NM, Vita JA. Endothelial dysfunction in diabetes mellitus: molecular mechanisms and clinical implications. Rev Endocr Metab Disord. 2010;11:61–74. [DOI] [PMC free article] [PubMed]
- 16.Tabit CE, Shenouda SM, Holbrook M, Fetterman JL, Kiani S, Frame AA, Kluge MA, Held A, Dohadwala MM, Gokce N, Farb MG, Rosenzweig J, Ruderman N, Vita JA, Hamburg NM. Protein kinase C-β contributes to impaired endothelial insulin signaling in humans with diabetes mellitus. Circulation. 2013;127(1):86–95. doi: 10.1161/CIRCULATIONAHA.112.127514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mancusi C, Losi MA, Izzo R, Canciello G, Manzi MV, Sforza A, De Luca N, Trimarco B, de Simone G. Effect of diabetes and metabolic syndrome on myocardial mechano-energetic efficiency in hypertensive patients. The Campania Salute Network. J Hum Hypertens. 2017;31:395–399. [DOI] [PubMed]
- 18.Mancusi C, de Simone G, Best LG, Wang W, Zhang Y, Roman MJ, Lee ET, Howard BV, Devereux RB. Myocardial mechano-energetic efficiency and insulin resistance in non-diabetic members of the Strong Heart Study cohort. Cardiovasc Diabetol. 2019;18:56. [DOI] [PMC free article] [PubMed]
- 19.Ferrannini E, Buzzigoli G, Bonadonna R, Giorico MA, Oleggini M, Graziadei L, Pedrinelli R, Brandi L, Bevilacqua S. Insulinresistance in essentialhypertension. N Engl J Med. 1987;317:350–357. doi: 10.1056/NEJM198708063170605. [DOI] [PubMed] [Google Scholar]
- 20.Reaven GM, Lithell H, Landsberg L. Hypertension and associated metabolic abnormalities–the role of insulin resistance and the sympathoadrenal system. N Engl J Med. 1996;334:374–381. doi: 10.1056/NEJM199602083340607. [DOI] [PubMed] [Google Scholar]
- 21.Grunfeld B, Balzareti M, Romo M, Gimenez M, Gutman R. Hyperinsulinemia in normotensive offspring of hypertensive parents. Hypertension. 1994;23:12–15. doi: 10.1161/01.hyp.23.1_suppl.i12. [DOI] [PubMed] [Google Scholar]
- 22.Cheng LS, Davis RC, Raffel LJ, Xiang AH, Wang N, Quinones M, Wen PZ, Toscano E, Diaz J, Pressman S, Henderson PC, Azen SP, Hsueh WA, Buchanan TA, Rotter JI. Coincident linkage of fasting plasma insulin and blood pressure to chromosome 7q in hypertensive hispanic families. Circulation. 2001;104:1255–1260. doi: 10.1161/hc3601.096729. [DOI] [PubMed] [Google Scholar]
- 23.Miyaoka K, Kuwasako T, Hirano K, Nozaki S, Yamashita S, Matsuzawa Y. Cd36 deficiency associated with insulin resistance. Lancet. 2001;357:686–687. doi: 10.1016/s0140-6736(00)04138-6. [DOI] [PubMed] [Google Scholar]
- 24.Dos Santos JM, Moreli ML, Tewari S, Benite-Ribeiro SA. The effect of exercise on skeletal muscle glucose uptake in type 2 diabetes: an epigenetic perspective. Metabolism. 2015;64:1619–1628. doi: 10.1016/j.metabol.2015.09.013. [DOI] [PubMed] [Google Scholar]
- 25.Lembo G, Iaccarino G, Vecchione C, Rendina V, Trimarco B. Insulin modulation of vascular reactivity is already impaired in prehypertensive spontaneously hypertensive rats. Hypertension. 1995;26:290–293. doi: 10.1161/01.hyp.26.2.290. [DOI] [PubMed] [Google Scholar]
- 26.Mazzone G, Morisco C, Lembo V, D’Argenio G, D’Armiento M, Rossi A, Del Giudice C, Trimarco B, Caporaso N, Morisco F. Dietary Supplementation of Vitamin D Prevents the Development of Western Diet-Induced Metabolic, Hepatic and Cardiovascular Abnormalities in Rats. United European Gastroenterol J. 2018;6:1056–1064. doi: 10.1177/2050640618774140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lee J, Pilch PF. The insulin receptor: structure, function, and signaling. Am J Physiol. 1994;266:C319–C334. doi: 10.1152/ajpcell.1994.266.2.C319. [DOI] [PubMed] [Google Scholar]
- 28.Cong LN, Chen H, Li Y, Zhou L, McGibbon MA, Taylor SI, Quon MJ. Physiological role of akt in insulin-stimulated translocation of glut4 in transfected rat adipose cells. Mol Endocrinol. 1997;11:1881–1890. doi: 10.1210/mend.11.13.0027. [DOI] [PubMed] [Google Scholar]
- 29.Hansen L, Ikeda Y, Olsen GS, Busch AK, Mosthaf L. Insulin signaling is inhibited by micromolar concentrations of H(2)O(2). Evidence for a role of H(2)O(2) in tumor necrosis factor alpha-mediated insulin resistance. J Biol Chem. 1999;274:25078–25084. [DOI] [PubMed]
- 30.Egawa K, Nakashima N, Sharma PM, Maegawa H, Nagai Y, Kashiwagi A, Kikkawa R, Olefsky JM. Persistent activation of phosphatidylinositol 3-kinase causes insulin resistance due to accelerated insulin-induced insulin receptor substrate-1 degradation in 3t3-l1 adipocytes. Endocrinology. 2000;141:1930–1935. doi: 10.1210/endo.141.6.7516. [DOI] [PubMed] [Google Scholar]
- 31.Goldstein BJ, Ahmad F, Ding W, Li PM, Zhang WR. Regulation of the insulin signalling pathway by cellular protein-tyrosine phosphatases. Mol Cell Biochem. 1998;182:91–99. [PubMed] [Google Scholar]
- 32.Hotamisligil GS. Mechanisms of TNF-alpha-induced insulin resistance. Exp Clin Endocrinol Diabetes. 1999;107:119–125. doi: 10.1055/s-0029-1212086. [DOI] [PubMed] [Google Scholar]
- 33.Abe H, Yamada N, Kamata K, Kuwaki T, Shimada M, Osuga J, Shionoiri F, Yahagi N, Kadowaki T, Tamemoto H, Ishibashi S, Yazaki Y, Makuuchi M. Hypertension, hypertriglyceridemia, and impaired endothelium-dependent vascular relaxation in mice lacking insulin receptor substrate-1. J Clin Invest. 1998;101:1784–1788. doi: 10.1172/JCI1594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wheatcroft SB, Shah AM, Li JM, Duncan E, Noronha BT, Crossey PA, Kearney MT. Preserved glucoregulation but attenuation of the vascular actions of insulin in mice heterozygous for knockout of the insulin receptor. Diabetes. 2004;53:2645–2652. doi: 10.2337/diabetes.53.10.2645. [DOI] [PubMed] [Google Scholar]
- 35.Zhang S, Wei M, Yue M, Wang P, Yin X, Wang L, Yang X, Liu H. Hyperinsulinemia precedes insulin resistance in offspring rats exposed to angiotensin II type 1 autoantibody in utero. Endocrine. 2018;62:588–601. doi: 10.1007/s12020-018-1700-7. [DOI] [PubMed] [Google Scholar]
- 36.Mori J, Alrob OA, Wagg CS, Harris RA, Lopaschuk GD, Oudit GY. ANG II causes insulin resistanceand induces cardiac metabolic switch and inefficiency: a critical role of PDK4. Am J Physiol Heart Circ Physiol. 2013;304:H1103–1113. [DOI] [PubMed]
- 37.Yusuf S, Gerstein H, Hoogwerf B, Pogue J, Bosch J, Wolffenbuttel BH, Zinman B. Ramipril and the development of diabetes. JAMA. 2001;286:1882–1885. doi: 10.1001/jama.286.15.1882. [DOI] [PubMed] [Google Scholar]
- 38.Julius S, Kjeldsen SE, Weber M, Brunner HR, Ekman S, Hansson L, Hua T, Laragh J, McInnes GT, Mitchell L, Plat F, Schork A, Smith B, Zanchetti A. Outcomes in hypertensive patients at high cardiovascular risk treated with regimens based on valsartan or amlodipine: the value randomised trial. Lancet. 2004;363:2022–2031. doi: 10.1016/S0140-6736(04)16451-9. [DOI] [PubMed] [Google Scholar]
- 39.Scheen AJ. dream study: prevention of type 2 diabetes with ramipril and/or rosiglitazone in persons with dysglycaemia but no cardiovascular desease. RevMed Liege. 2006;61:728–732. [PubMed] [Google Scholar]
- 40.Sowers JR. Insulin resistance and hypertension. Am J Physiol Heart Circ Physiol. 2004;286:H1597–H1602. doi: 10.1152/ajpheart.00026.2004. [DOI] [PubMed] [Google Scholar]
- 41.Taniyama Y, Hitomi H, Shah A, Alexander RW, Griendling KK. Mechanisms of reactive oxygen species-dependent downregulation of insulin receptor substrate-1 by angiotensin II. ArteriosclerThrombVasc Biol. 2005;25:1142–1147. doi: 10.1161/01.ATV.0000164313.17167.df. [DOI] [PubMed] [Google Scholar]
- 42.Ogihara T, Asano T, Ando K, Chiba Y, Sakoda H, Anai M, Shojima N, Ono H, Onishi Y, Fujishiro M, Katagiri H, Fukushima Y, Kikuchi M, Noguchi N, Aburatani H, Komuro I, Fujita T. Angiotensin II-induced insulin resistance is associated with enhanced insulin signaling. Hypertension. 2002;40:872–879. doi: 10.1161/01.hyp.0000040262.48405.a8. [DOI] [PubMed] [Google Scholar]
- 43.Andreozzi F, Laratta E, Sciacqua A, Perticone F, Sesti G. Angiotensin ii impairs the insulin signaling pathway promoting production of nitric oxide by inducing phosphorylation of insulin receptor substrate-1 on ser312 and ser616 in human umbilical vein endothelial cells. Circ Res. 2004;94:1211–1218. doi: 10.1161/01.RES.0000126501.34994.96. [DOI] [PubMed] [Google Scholar]
- 44.Mancia G, Grassi G, Giannattasio C, Seravalle G. Sympathetic activation in the pathogenesis of hypertension and progression of organ damage. Hypertension. 1999;34:724–728. doi: 10.1161/01.hyp.34.4.724. [DOI] [PubMed] [Google Scholar]
- 45.Klein J, Fasshauer M, Ito M, Lowell BB, Benito M, Kahn CR. Beta(3)-adrenergic stimulation differentially inhibits insulin signaling and decreases insulin-induced glucose uptake in brown adipocytes. J Biol Chem. 1999;274:34795–34802. doi: 10.1074/jbc.274.49.34795. [DOI] [PubMed] [Google Scholar]
- 46.Morisco C, Condorelli G, Trimarco V, Bellis A, Marrone C, Sadoshima J, Trimarco B. Akt mediates the cross-talk between beta-adrenergic and insulin receptors in neonatal cardiomyocytes. Circ Res. 2005;96:180–188. doi: 10.1161/01.RES.0000152968.71868.c3. [DOI] [PubMed] [Google Scholar]
- 47.Nagoshi T, Matsui T, Aoyama T, Leri A, Anversa P, Li L, Ogawa W, del Monte F, Gwathmey JK, Grazette L, Hemmings BA, Kass DA, Champion HC, Rosenzweig A. PI3K rescues the detrimental effects of chronic akt activation in the heart during ischemia/reperfusion injury. J Clin Invest. 2005;115:2128–2138. doi: 10.1172/JCI23073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Levy D, Garrison RJ, Savage DD, Kannel WB, Castelli WP. Prognostic implications of echocardiographically determined left ventricular mass in the Framingham heart study. N Engl J Med. 1990;322:1561–1566. doi: 10.1056/NEJM199005313222203. [DOI] [PubMed] [Google Scholar]
- 49.Bots ML, Hoes AW, Koudstaal PJ, Hofman A, Grobbee DE. Common carotid intima-media thickness and risk of stroke and myocardial infarction: the Rotterdam study. Circulation. 1997;96:1432–1437. doi: 10.1161/01.cir.96.5.1432. [DOI] [PubMed] [Google Scholar]
- 50.Schiffrin EL, Lipman ML, Mann JF. Chronic kidney disease: effects on the cardiovascular system. Circulation. 2007;116:85–97. doi: 10.1161/CIRCULATIONAHA.106.678342. [DOI] [PubMed] [Google Scholar]
- 51.Carpinella G, Pagano G, Buono F, Petitto M, Guarino G, Orefice G, Rengo G, Trimarco B, Morisco C. Prognostic value of combined target-organ damage in patients with essential hypertension. Am J Hypertens. 2015;28:127–134. doi: 10.1093/ajh/hpu098. [DOI] [PubMed] [Google Scholar]
- 52.Meccariello A, Buono F, Verrengia E, Orefice G, Grieco F, Romeo F, Trimarco B, Morisco C. Microalbuminuria predicts the recurrence of cardiovascular events in patients with essential hypertension. J Hypertens. 2016;34:646–653. doi: 10.1097/HJH.0000000000000846. [DOI] [PubMed] [Google Scholar]
- 53.Morisco C, Sadoshima J, Trimarco B, Arora R, Vatner DE, Vatner SF. Is treating cardiac hypertrophy salutary or detrimental: the two faces of Janus. Am J Physiol Heart Circ Physiol. 2003;284:H1043–H1047. doi: 10.1152/ajpheart.00990.2002. [DOI] [PubMed] [Google Scholar]
- 54.Buono F, Crispo S, Pagano G, Rengo G, Petitto M, Grieco F, Trimarco B, Morisco C. Determinants of left ventricular hypertrophy in patients with recent diagnosis of essential hypertension. J Hypertens. 2014;32:166–173. doi: 10.1097/HJH.0b013e328365c87d. [DOI] [PubMed] [Google Scholar]
- 55.Izzo R, Losi MA, Stabile E, Lönnebakken MT, Canciello G, Esposito G, Barbato E, De Luca N, Trimarco B, de Simone G. Development of left ventricular hypertrophy in treated hypertensive outpatients: the campania salute network. Hypertension. 2017;69:136–142. doi: 10.1161/HYPERTENSIONAHA.116.08158. [DOI] [PubMed] [Google Scholar]
- 56.Verdecchia P, Reboldi G, Schillaci G, Borgioni C, Ciucci A, Telera MP, Santeusanio F, Porcellati C, Brunetti P. Circulating insulin and insulin growth factor-1 are independent determinants of left ventricular mass and geometry in essential hypertension. Circulation. 1999;100:1802–1807. doi: 10.1161/01.cir.100.17.1802. [DOI] [PubMed] [Google Scholar]
- 57.Hall JE, Crook ED, Jones DW, Wofford MR, Dubbert PM. Mechanisms of obesity-associated cardiovascular and renal disease. Am J Med Sci. 2002;324:127–137. doi: 10.1097/00000441-200209000-00003. [DOI] [PubMed] [Google Scholar]
- 58.de Simone G, Mancusi C, Izzo R, Losi MA, Ferrara A. Obesity and hypertensive heart disease: focus on body composition and sex differences. Diabetol Metab Syndr. 2016;8:79. [DOI] [PMC free article] [PubMed]
- 59.Halldin M, Brismar K, Fahlstadius P, Vikström M, de Faire U, Hellénius ML. The metabolic syndrome and ECG detected left ventricular hypertrophy–influences from IGF-1 and IGF-binding protein-1. PLoS One. 2014;9:e108872. doi: 10.1371/journal.pone.0108872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kuboki K, Jiang ZY, Takahara N, Ha SW, Igarashi M, Yamauchi T, Feener EP, Herbert TP, Rhodes CJ, King GL. Regulation of endothelial constitutive nitric oxide synthase gene expression in endothelial cells and in vivo: a specific vascular action of insulin. Circulation. 2000;101:676–681. doi: 10.1161/01.cir.101.6.676. [DOI] [PubMed] [Google Scholar]
- 61.Gigante B, Bellis A, Visconti R, Marino M, Morisco C, Trimarco V, Galasso G, Piscione F, De Luca N, Prince JA, de Faire U, Trimarco B. Retrospective analysis of coagulation factor ii receptor (F2R) sequence variation and coronary heart disease in hypertensive patients. Arterioscler Thromb Vasc Biol. 2007;27:1213–9. [DOI] [PubMed]
- 62.Yi X, Wu P, Liu J, Gong Y, Xu X, Li W. Identification of the potential key genes for adipogenesis from human mesenchymal stem cells by RNA-seq. J Cell Physiol. 2019;234:20217–20227. doi: 10.1002/jcp.28621. [DOI] [PubMed] [Google Scholar]
- 63.Ross R. Atherosclerosis—an inflammatory disease. N Engl J Med. 1999;340:115–126. doi: 10.1056/NEJM199901143400207. [DOI] [PubMed] [Google Scholar]
- 64.Danesh J, Whincup P, Walker M, Lennon L, Thomson A, Appleby P, Gallimore JR, Pepys MB. Low grade inflammation and coronary heart disease: prospective study and updated meta-analyses. BMJ. 2000;321:199–204. doi: 10.1136/bmj.321.7255.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Fiordelisi A, Iaccarino G, Morisco C, Coscioni E, Sorriento D. NFkappaB is a key player in the crosstalk between inflammation and cardiovascular diseases. Int J Mol Sci. 2019;20:1599. doi: 10.3390/ijms20071599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Festa A, D’Agostino R, Jr, Howard G, Mykkanen L, Tracy RP, Haffner SM. Chronic subclinical inflammation as part of the insulin resistance syndrome: the insulin resistance atherosclerosis study (iras) Circulation. 2000;102:42–47. doi: 10.1161/01.cir.102.1.42. [DOI] [PubMed] [Google Scholar]
- 67.Rutherford S, Johnson MP, Curtain RP, Griffiths LR. Chromosome 17 and the inducible nitric oxide synthase gene in human essential hypertension. Hum Genet. 2001;109:408–415. doi: 10.1007/s004390100565. [DOI] [PubMed] [Google Scholar]
- 68.Perreault M, Marette A. Targeted disruption of inducible nitric oxide synthase protects against obesity-linked insulin resistance in muscle. Nat Med. 2001;7:1138–1143. doi: 10.1038/nm1001-1138. [DOI] [PubMed] [Google Scholar]
- 69.Luft FC. Angiotensin, inflammation, hypertension, and cardiovascular disease. Curr Hypertens Rep. 2001;3:61–67. doi: 10.1007/s11906-001-0082-y. [DOI] [PubMed] [Google Scholar]
- 70.Nyui N, Tamura K, Yamaguchi S, Nakamaru M, Ishigami T, Yabana M, Kihara M, Ochiai H, Miyazaki N, Umemura S, Ishii M. Tissue angiotensinogen gene expression induced by lipopolysaccharide in hypertensive rats. Hypertension. 1997;30:859–867. doi: 10.1161/01.hyp.30.4.859. [DOI] [PubMed] [Google Scholar]
- 71.Hotamisligil GS, Peraldi P, Budavari A, Ellis R, White MF, Spiegelman BM. Irs-1-mediated inhibition of insulin receptor tyrosine kinase activity in tnf-alpha- and obesity-induced insulin resistance. Science. 1996;271:665–668. doi: 10.1126/science.271.5249.665. [DOI] [PubMed] [Google Scholar]
- 72.Morisco C, Lembo G, Trimarco B. Insulin resistance and cardiovascular risk: new insights from molecular and cellular biology. Trends Cardiovasc Med. 2006;16:183–188. doi: 10.1016/j.tcm.2006.03.008. [DOI] [PubMed] [Google Scholar]
- 73.Pausova Z, Deslauriers B, Gaudet D, Tremblay J, Kotchen TA, Larochelle P, Cowley AW, Hamet P. Role of tumor necrosis factor-alpha gene locus in obesity and obesity-associated hypertension in frenchcanadians. Hypertension. 2000;36:14–19. doi: 10.1161/01.hyp.36.1.14. [DOI] [PubMed] [Google Scholar]
- 74.Zinman B, Hanley AJ, Harris SB, Kwan J, Fantus IG. Circulating tumor necrosis factor-alpha concentrations in a native canadian population with high rates of type 2 diabetes mellitus. J Clin Endocrinol Metab. 1999;84:272–278. doi: 10.1210/jcem.84.1.5405. [DOI] [PubMed] [Google Scholar]
- 75.Dorffel Y, Latsch C, Stuhlmuller B, Schreiber S, Scholze S, Burmester GR, Scholze J. Preactivated peripheral blood monocytes in patients with essential hypertension. Hypertension. 1999;34:113–117. doi: 10.1161/01.hyp.34.1.113. [DOI] [PubMed] [Google Scholar]
- 76.Winkler G, Lakatos P, Salamon F, Nagy Z, Speer G, Kovacs M, Harmos G, Dworak O, Cseh K. Elevated serum tnf-alpha level as a link between endothelial dysfunction and insulin resistance in normotensive obese patients. Diabet Med. 1999;16:207–211. doi: 10.1046/j.1464-5491.1999.00052.x. [DOI] [PubMed] [Google Scholar]
- 77.Hotamisligil GS, Shargill NS, Spiegelman BM. Adipose expression of tumor necrosis factor-alpha: direct role in obesity-linked insulin resistance. Science. 1993;259:87–91. doi: 10.1126/science.7678183. [DOI] [PubMed] [Google Scholar]
- 78.Ofei F, Hurel S, Newkirk J, Sopwith M, Taylor R. Effects of an engineered human anti-tnf-alpha antibody (cdp571) on insulin sensitivity and glycemic control in patients with niddm. Diabetes. 1996;45:881–885. doi: 10.2337/diab.45.7.881. [DOI] [PubMed] [Google Scholar]
- 79.Fernandez-Real JM, Vayreda M, Richart C, Gutierrez C, Broch M, Vendrell J, Ricart W. Circulating interleukin 6 levels, blood pressure, and insulin sensitivity in apparently healthy men and women. J Clin Endocrinol Metab. 2001;86:1154–1159. doi: 10.1210/jcem.86.3.7305. [DOI] [PubMed] [Google Scholar]
- 80.Humphries SE, Luong LA, Ogg MS, Hawe E, Miller GJ. The interleukin-6 -174 g/c promoter polymorphism is associated with risk of coronary heart disease and systolic blood pressure in healthy men. Eur Heart J. 2001;22:2243–2252. doi: 10.1053/euhj.2001.2678. [DOI] [PubMed] [Google Scholar]
- 81.Perrotta M, Lembo G, Carnevale D. The interactions of the immune system and the brain in hypertension. CurrHypertens Rep. 2018;20:7. doi: 10.1007/s11906-018-0808-8. [DOI] [PubMed] [Google Scholar]
- 82.Gonzalez W, Fontaine V, Pueyo ME, Laquay N, Messika-Zeitoun D, Philippe M, Arnal JF, Jacob MP, Michel JB. Molecular plasticity of vascular wall during n(g)-nitro-l-arginine methyl ester-induced hypertension: modulation of proinflammatory signals. Hypertension. 2000;36:103–109. doi: 10.1161/01.hyp.36.1.103. [DOI] [PubMed] [Google Scholar]
- 83.Haynes WG, Morgan DA, Walsh SA, Mark AL, Sivitz WI. Receptor-mediated regional sympathetic nerve activation by leptin. J Clin Invest. 1997;100:270–278. doi: 10.1172/JCI119532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Shek EW, Brands MW, Hall JE. Chronic leptin infusion increases arterial pressure. Hypertension. 1998;31:409–414. doi: 10.1161/01.hyp.31.1.409. [DOI] [PubMed] [Google Scholar]
- 85.Aizawa-Abe M, Ogawa Y, Masuzaki H, Ebihara K, Satoh N, Iwai H, Matsuoka N, Hayashi T, Hosoda K, Inoue G, Yoshimasa Y, Nakao K. Pathophysiological role of leptin in obesity-related hypertension. J Clin Invest. 2000;105:1243–1252. doi: 10.1172/JCI8341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Sowers JR, Epstein M, Frohlich ED. Diabetes, hypertension, and cardiovascular disease: an update. Hypertension. 2001;37:1053–1059. doi: 10.1161/01.hyp.37.4.1053. [DOI] [PubMed] [Google Scholar]
- 87.Zhang R, Reisin E. Obesity-hypertension: the effects on cardiovascular and renal systems. Am J Hypertens. 2000;13:1308–1314. doi: 10.1016/s0895-7061(00)01254-1. [DOI] [PubMed] [Google Scholar]
- 88.Henegar JR, Bigler SA, Henegar LK, Tyagi SC, Hall JE. Functional and structural changes in the kidney in the early stages of obesity. J Am SocNephrol. 2001;12:1211–1217. doi: 10.1681/ASN.V1261211. [DOI] [PubMed] [Google Scholar]
- 89.Palaniappan L, Carnethon M, Fortmann SP. Association between microalbuminuria and the metabolic syndrome: NHANES III. Am J Hypertens. 2003;16:952–958. doi: 10.1016/s0895-7061(03)01009-4. [DOI] [PubMed] [Google Scholar]
- 90.Castro JP, El-Atat FA, McFarlane SI, Aneja A, Sowers JR. Cardiometabolic syndrome: pathophysiology and treatment. Curr Hypertens Rep. 2003;5:393–401. doi: 10.1007/s11906-003-0085-y. [DOI] [PubMed] [Google Scholar]
- 91.Volpe M, Battistoni A, Gallo G, et al. Executive summary of the 2018 joint consensus document on cardiovascular disease prevention in Italy. High Blood Press Cardiovasc Prev. 2018;25:327–341. doi: 10.1007/s40292-018-0278-8. [DOI] [PubMed] [Google Scholar]
- 92.Carrizzo A, Izzo C, Oliveti M, et al. The main determinants of diabetes mellitus vascular complications: endothelial dysfunction and platelet hyperaggregation. Int J Mol Sci. 2018;19:2968. doi: 10.3390/ijms19102968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Iaccarino G, Franco D, Sorriento D, Strisciuglio T, Barbato E, Morisco C. Modulation of insulin sensitivity by exercise training: implications for cardiovascular prevention [published online ahead of print, 2020 Jul 31]. J Cardiovasc Transl Res. 2020; 10.1007/s12265-020-10057-w. [DOI] [PMC free article] [PubMed]
- 94.Borghi C, SIIA Task Force, Rossi F, SIF Task Force. Role of the renin-angiotensin-aldosterone system and its pharmacological inhibitors in cardiovascular diseases: complex and critical issues. High Blood Press Cardiovasc Prev. 2015;22:429–444. [DOI] [PubMed]
- 95.Brown JM, Everett BM. Cardioprotective diabetes drugs: what cardiologists need to know. Cardiovasc Endocrinol Metab. 2019;8:96–105. doi: 10.1097/XCE.0000000000000181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Patel KV, Sarraju A, Needland IJ, McGuire DK. Cardiovascular Effects of Dipeptidyl Peptidase-4 Inhibitors and Glucagon-Like Peptide-1 Receptor Agonists : a Review for the General Cardiologist. Curr Cardiol Rep. 2020;22:105. doi: 10.1007/s11886-020-01355-5. [DOI] [PubMed] [Google Scholar]