Abstract
Introduction
Despite hypertension guidelines suggest that the most effective treatment strategy to improve blood pressure (BP) target achievement is to implement the use of combination treatment, monotherapy is still widely used in the clinical practice of hypertension.
Aim
To investigate BP control under monotherapy in the setting of real-life.
Methods
We extracted data from a medical database of adult outpatients who were referred to the Hypertension Unit, Sant’Andrea Hospital, Rome (IT), including anthropometric data, CV risk factors and comorbidities, presence or absence of antihypertensive therapy and concomitant medications. Among treated hypertensive patients, we identified only those under single antihypertensive agent (monotherapy). Office BP treatment targets were defined according to 2018 ESC/ESH guidelines as: (a) < 130/80 mmHg in individuals aged 18–65 years; (b) < 140/80 mmHg in those aged > 65 years.
Results
From an overall sample of 7797 records we selected 1578 (20.2%) hypertensive outpatients (47.3% female, age 59.5 ± 13.6 years, BMI 26.6 ± 4.4 kg/m2) treated with monotherapies, among whom 30.5% received ACE inhibitors, 37.7% ARBs, 15.8% beta-blockers, 10.6% CCBs, 3.0% diuretics, and 2.0% alpha-blockers. 36.6% of these patients reached the conventional clinic BP goal of < 140/90 mmHg, whilst the 2018 European guidelines BP treatment targets were fulfilled only in 14.0%. In particular, 10.2% patients aged 18–65 years and 20.4% of those aged > 65 years achieved the recommended BP goals. All these proportions results significantly lower than those achieved with dual (18.2%) or triple (22.2%) combination therapy, though higher than those obtained with life-style changes (10.8%). Proportions of patients on monotherapies with normal home and 24-h BP levels were 22.0% and 30.2%, respectively, though only 5.2% and 7.3% of these patients achieved sustained BP control, respectively. Ageing and dyslipidaemia showed significant and independent positive predictive value for the achievement of the recommended BP treatment targets, whereas European SCORE resulted a negative and independent predictor in outpatients treated with monotherapies.
Conclusions
Our data showed a persistent use of monotherapy in the clinical practice, though with unsatisfactory BP control, especially in light of the BP treatment targets suggested by the last hypertension guidelines.
Electronic supplementary material
The online version of this article (10.1007/s40292-020-00420-y) contains supplementary material, which is available to authorized users.
Keywords: Blood pressure control, Hypertension, Antihypertensive therapy, Monotherapy, Cardiovascular risk
Introduction
Antihypertensive drug therapy can be based on different classes of blood pressure (BP) lowering agents, whose efficacy and safety have been widely investigated and demonstrated in randomized controlled clinical trials [1–5]. Despite the large armamentarium of antihypertensive drug classes, now available both in monotherapies and in fixed or free combination therapies, the number of patients achieving the recommended BP goals is still unacceptably low [6–9].
Several reasons have been proposed to explain the gap between expected and attained BP control rates, among which the persistently use of monotherapy has been one of the most frequently reported [10]. Indeed, more than 70% of treated hypertensive patients require at least two antihypertensive drugs, either as initial combination therapy or as add-on therapy [10]. Also the most recent hypertension guidelines [11] support the use of monotherapy for very limited subgroup of individuals, being the use of combination therapies clearly recommended for the vast majority of hypertensive outpatients at different cardiovascular (CV) risk profile.
Monotherapy is frequently used to treat patients with hypertension at different CV risk profile [12], despite the recommendations from hypertension guidelines [11], which strongly support the use of combination therapies in many clinical settings. In this regard, it should be taken into account the latency between issue of new guidelines and their implementation in the clinical practice, in which the roots of the long-term habit to prescribe monotherapy are very prolonged. In addition, it should be considered that the vast majority of hypertensive patients showed concomitant risk factors and comorbidities [13–15], which render per se more difficult to achieve the recommended BP goals. Despite these indications, however, single-agent treatment strategy is widely adopted not only in relatively young and apparently low risk subjects with high-normal BP elevations, but also in normotensive individuals with high and very high risk and comorbidities, including those coronary artery disease (CAD), myocardial infarction (MI), stroke, and diabetes with hypertension-mediated organ damage (HMOD).
Another reason for the relatively high use of monotherapy is the so-called “clinical inertia”, which is characterized by the absence of therapy upgrade despite the lack of blood pressure control [16, 17]. Mancia et al. showed that starting antihypertensive treatment with a single drug lead not only to lower BP control rate compared to combination therapies, but also to the maintenance of the same therapeutic regimen (“clinical inertia”) lasting for years after treatment initiation [16], Furthermore, it has been also reported that the rate of treatment discontinuations was lower in those patients starting their treatment with a combination therapy than in those starting with single-class antihypertensive regimen [16].
Whatever the case, a not marginal proportion of hypertensive patients are currently treated with various monotherapies (and lifestyle changes) in a setting of clinical practice. On the basis of these considerations, the primary aim of this study was to investigate the real-world BP control rate in a relatively large cohort of adult hypertensive patients treated with monotherapy with different classes of antihypertensive drugs, who were referred to a high volume specialized center for hypertension, recognised by the European Society of Hypertension (ESH).
Methods
Methodology of the Study
The methodology of the study has been previously described [18, 19]. This is a single-center, cross-sectional, observational study designed to evaluate the rate of BP control in hypertensive adult outpatients treated with single antihypertensive agent (monotherapy), who were consecutively evaluated at the Hypertension Unit of Sant’Andrea Hospital, University of Rome Sapienza, in Rome, Italy, from February 2004 to April 2020. The center has been recognised by European Society of Hypertension (ESH) and Italian Society of Hypertension (SIIA) to fulfil the criteria for an excellence center.
To be included in the study, patients had to fulfil the following inclusion criteria: (1) adult individuals aged more than 18 years; (2) valid clinic systolic and diastolic BP measurements; (3) signature of informed consent for study participation; (4) adoption of single-agent antihypertensive strategy (monotherapy). In addition, the following exclusion criteria were considered: (1) secondary hypertension or true resistant hypertension; (2) recent (less than 6 months) history of acute CV diseases, including at least one of the following: CAD, transient ischemic attack (TIA), stroke, congestive heart failure, severe valve disease, or peripheral artery disease; (3) any neurological or psychiatric disease which may at least, in part, affect the BP assessment or the signature of the informed consent.
Once included in the study population, adult outpatients were stratified into two age groups, according to the indications of ESH/ESC guidelines [11]: (1) patients aged 18–65 years; (2) patients aged more than 65 years.
Collected information included anthropometric data, blood test parameters, class of antihypertensive agents, CV risk factors and comorbidities. Clinical systolic and diastolic BP, home BP levels and 24-h ambulatory BP levels, when available, were also extracted.
The study conformed to the Declaration of Helsinki and its subsequent modifications, and was authorized by the reference Ethical Committee. As applied in previous studies, the confidentiality of the data was carefully and strictly protected.
Blood Pressure Measurements
Office attended BP measurements were performed according to recommendations by ESH/ESC guidelines [11]. Sequential clinic BP measurements (1–2 min apart), using an adequate bladder cuff, were performed in all patients in a quiet room, after 10 min of rest, on the left arm and with the participant in supine position, by using an automated oscillometric device (Omron 705 IT). The average of three consecutive BP measurements was considered as office (clinic) BP values; all clinic BP measurements were attended.
Ambulatory BP monitoring (ABPM) was performed according to clinician indications, by an oscillometric device (Spacelabs 90207, Spacelabs Inc., Redmond, Washington, USA). Automatic BP readings were obtained every 15 min during the day-time and every 30 min during the night over 24 h. Each patient was instructed not to alter her/his usual schedule during the monitoring period, asked to avoid unusual physical exercise, to maintain the arm still during BP measurements and to record daily activities and sleep time on a diary. A minimum of 70% valid BP measurements were required for considering valid the monitoring. Average values for the 24-h, day-time and night-time systolic and diastolic BP levels and heart rate were collected.
Clinical BP treatment targets were initially set as < 140/90 mmHg in the overall population sample [20]. According to the recent 2018 European hypertension guidelines [11], the following office BP treatment targets were defined: (a) systolic BP ≤ 130 mmHg and diastolic BP < 80 mmHg in individuals aged 18–65 years; (b) systolic/diastolic BP < 140/80 mmHg in those aged > 65 years. In addition, home and 24-h BP thresholds considered as goal for optimal treatment target were < 135/85 mmHg and < 130/80 mmHg, respectively.
For the purposes of the present analysis and the assessment of BP control rates in different age strata and drug therapies, the last available clinic (or home and 24-h) BP levels were used from those available in our medical database during the predefined observational period. Thus, the vast majority of the BP assessments have been collected over the past two years.
Definition of Cardiovascular Risk Factors and Comorbidities
Based on anthropometric data, calculation of body mass index (BMI) was made and it was expressed as body weight in kg divided by the square of height in m (kg/m2).
Diagnosis of hypertension was defined in the presence of systolic BP levels ≥ 140 mmHg and/or diastolic BP levels ≥ 90 mmHg in untreated subjects or in the presence of stable (≥ 6 months) antihypertensive drug treatment [11]. Diagnosis of hypercholesterolemia was made in the presence of total cholesterol levels ≥ 190 mg/dl or low-density lipoprotein (LDL) cholesterol levels ≥ 130 mg/dl, while hypertriglyceridemia for triglyceride levels ≥ 150 mg/dl or stable lipid-lowering drug treatment in both conditions [21]. Diabetes was defined in the presence of plasma glucose levels ≥ 126 mg/dl or in the presence of glucose-lowering therapy [22].
CAD, including non-fatal MI, was defined according to the presence of the two of the following three items: symptoms (e.g. chest pain) lasting longer than 15 min, transient increase in serum concentrations of enzymes indicating cardiac damage (more than twice the upper limit of normal) and electrocardiographic changes typical of myocardial ischemia (new persistent ST-segment elevation or pathological Q waves in two contiguous leads [23]. The diagnosis of CAD may also include other coronary events, for example acute coronary syndrome, recurrent angina and coronary revascularization [23].
Non-fatal stroke was defined as a neurological deficit with sudden onset and persistence of symptoms for more than 24 h or leading to death with no apparent causes other than vascular ones [24]. TIA was defined as a neurological event with the signs and symptoms of stroke, but which resolve within a short period of time (typically less than 24 h) [25].
Statistical Analysis
Patients’ characteristics are presented as number and percentage for dichotomous variables and mean ± standard deviation (SD) of the mean for continuous variables. Normal distribution of data was assessed using histograms and Kolmogorov–Smirnov test. Continuous variables were tested with either t Student or ANOVA tests, whereas dichotomous variables were tested by Chi square test. Correlations between continuous variables were assessed by Pearson analysis. All tests were two-sided, and a P value of less than 0.05 was considered statistically significant. To evaluate the significance of predictors of the achievement of the recommended BP treatment targets, odds ratios (OR) and 95% confidence intervals (CI) were derived from logistic regression analysis. This analysis was applied only to those patients treated with monotherapies. All calculations were generated using SPSS, version 20.0 for MacOs (SPSS Inc., Chicago, Illinois).
Results
Study Population
From an overall sample of 9010 individuals, we initially identified 7797 adult individuals, among whom we selected 1578 (18.7%) patients (47.3% female, age 59.5 ± 13.6 years, BMI 26.6 ± 4.4 kg/m2) treated with single antihypertensive agent (monotherapy) and valid BP data. In this population, 62.7% patients were aged between 18 and 65 years, and 37.3% were aged more than 65 years. Flow-chart for the selection of the study population is illustrated in Electronic Fig. 1 (online available), while general characteristics of the study population are reported on Table 1.
Table 1.
General characteristics of the study population of hypertensive outpatients treated with monotherapies
| Parameters | Overall sample | Age 18–65 years (%) | Age > 65 years (%) | P value |
|---|---|---|---|---|
| Outpatients (%) | 1575 (100.0) | 988 (62.7) | 587 (37.3) | – |
| Age (years) | 59.5 ± 13.6 | 51.2 ± 9.3 | 73.5 ± 6.0 | < 0.001 |
| BMI (kg/m2) | 26.6 ± 4.4 | 26.9 ± 4.7 | 26.0 ± 3.8 | 0.004 |
| Smoke (%) | 157 (17.5) | 120 (20.9) | 37 (11.4) | < 0.001 |
| Obesity (%) | 935 (59.4) | 612 (61.9) | 323 (55.0) | 0.007 |
| Dyslipidaemia (%) | 489 (31.0) | 246 (24.9) | 243 (41.4) | < 0.001 |
| Diabetes (%) | 142 (9.0) | 72 (7.3) | 70 (11.9) | 0.002 |
| CAD (%) | 27 (1.7) | 6 (0.6) | 21 (3.6) | < 0.001 |
| TIA/stroke (%) | 69 (4.4) | 28 (2.8) | 41 (7.0) | < 0.001 |
| Glucose (mg/dl) | 96.7 ± 23.0 | 96.7 ± 25.1 | 96.9 ± 16.7 | 0.936 |
| TOT-C (mg/dl) | 200.1 ± 37.4 | 202.2 ± 37.6 | 194.7 ± 36.7 | 0.080 |
| HDL-C (mg/dl) | 52.7 ± 13.9 | 52.4 ± 13.8 | 53.5 ± 14.3 | 0.524 |
| LDL-C (mg/dl) | 124.4 ± 35.7 | 127.2 ± 36.2 | 116.4 ± 33.3 | 0.013 |
| TG (mg/dl) | 117.0 ± 61.2 | 117.7 ± 65.1 | 115.3 ± 49.8 | 0.739 |
| Creatinine (mg/dl) | 0.96 ± 0.6 | 0.96 ± 0.7 | 0.95 ± 0.3 | 0.931 |
| Uric acid (mg/dl) | 5.6 ± 1.7 | 5.5 ± 1.6 | 6.1 ± 1.8 | 0.321 |
BMI body mass index, CAD coronary artery disease, TIA transient ischaemic attack, TOT-C total cholesterol, HDL-C high density lipoprotein cholesterol, LDL-C low density lipoprotein cholesterol, TG triglycerides, BUN blood urea nitrogen
*Risk scores were calculated only in those patients aged between 40 and 65 years
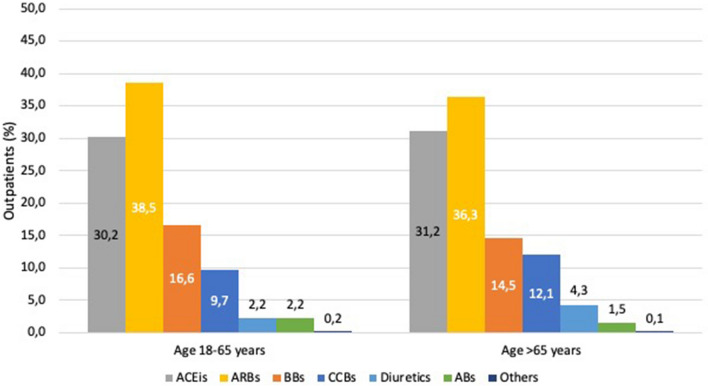
Angiotensin receptor blockers (ARBs) were the most commonly used antihypertensive drugs, accounting for 37.7% of the entire study population, followed by angiotensin converting enzyme (ACE) inhibitors (30.5%), beta-blockers (15.8%), calcium channel blockers (CCBs) (10.6%), diuretics (3.0%), while alpha blockers accounted for a paltry 2.0%. Age distribution of different classes of antihypertensive agents, used in monotherapies, is illustrated in Fig. 1.
Fig. 1.
Age distribution of different classes of antihypertensive agents used in monotherapies. ACEIs Angiotensin converting enzyme inhibitors, ARBs angiotensin receptor blockers, BBs beta-blockers, CCBs calcium channel blockers, Abs alpha-blockers.
Patients aged 18–65 years showed significantly higher BMI (26.9 ± 4.7 vs. 26.0 ± 3.8; P = 0.004) and higher prevalence of smoking habits (20.9% vs. 11.4%; P < 0.001) and obesity (61.9% vs. 55.0%; P = 0.007) than those aged more than 65 years, whereas dyslipidaemia (41.4% vs. 24.9%: P < 0.001), diabetes (11.9% vs. 7.3%; P = 0.002), CAD (3.6% vs. 0.6%; P < 0.001) and previous stroke or TIA (7.0% vs. 2.8%; P < 0.001) were significantly more prevalent in elderly patients than in adult ones
No significant differences were found between two age groups with regard to metabolic and renal parameters, with the only exception of LDL-C (127.2 ± 36.2 vs. 116.4 ± 33.3 mg/dl; P = 0.013), which resulted significantly higher in patients aged 18–65 years than in those aged more than 65 years.
In the subgroup of patients aged between 40 and 65 years, both Italian Cuore Score (15.3 ± 11.2 vs. 6.5 ± 6.4%; P < 0.001) and European SCORE (5.6 ± 10.2 vs. 2.9 ± 5.9%; P < 0.001) resulted significantly higher in men than in women.
Office, Home and 24-h Blood Pressure Levels and Control
BP levels in the study population are reported in Table 2. In the overall population of patients treated with single antihypertensive agents mean office BP levels were 141.6 ± 17.9/87.7 ± 11.4 mmHg.
Table 2.
Office, home and 24-h blood pressure levels in hypertensive outpatients treated with monotherapies
| Parameters | Overall sample (%) | Age 18–65 years (%) | Age > 65 years (%) | P value |
|---|---|---|---|---|
| Clinic systolic BP (mmHg) | 141.6 ± 17.9 | 140.1 ± 16.7 | 144.2 ± 19.4 | < 0.001 |
| Clinic diastolic BP (mmHg) | 87.7 ± 11.4 | 90.0 ± 11.2 | 84.0 ± 10.8 | < 0.001 |
| Home systolic BP (mmHg) | 134.3 ± 16.6 | 133.1 ± 15.1 | 136.7 ± 19.0 | 0.004 |
| Home diastolic BP (mmHg) | 81.9 ± 10.8 | 83.2 ± 10.3 | 79.2 ± 11.3 | < 0.001 |
| 24-h Systolic BP (mmHg) | 128.4 ± 12.4 | 127.7 ± 11.9 | 129.4 ± 13.2 | 0.021 |
| 24-h Diastolic BP (mmHg) | 78.1 ± 8.9 | 80.8 ± 8.6 | 74.0 ± 7.8 | < 0.001 |
| Day-time systolic BP (mmHg) | 131.5 ± 12.9 | 131.2 ± 12.2 | 132.1 ± 13.8 | 0.253 |
| Day-time diastolic BP (mmHg) | 81.0 ± 9.3 | 84.0 ± 8.9 | 76.5 ± 8.1 | < 0.001 |
| Night-time systolic BP (mmHg) | 119.4 ± 32.1 | 117.2 ± 13.3 | 120.5 ± 14.1 | < 0.001 |
| Night-time diastolic BP (mmHg) | 69.2 ± 9.4 | 71.1 ± 9.4 | 66.3 ± 8.7 | < 0.001 |
BP blood pressure
Elderly patients aged more than 65 years showed significantly higher systolic BP levels than those recorded in patients aged between 18 and 65 years at both clinic (144.2 ± 19.4 vs. 140.1 ± 16.7 mmHg; P < 0.001), home (136.7 ± 19.0 vs. 133.1 ± 15.1 mmHg; P = 0.004), 24-h (129.4 ± 13.2 vs. 127.7 ± 11.9 mmHg; P = 0.021), and night-time (120.5 ± 14.1 vs. 117.2 ± 13.3 mmHg; P < 0.001) BP assessments, whilst no significant difference was observed for day-time BP levels between the two age groups. On the other hand, diastolic BP levels resulted significantly higher in those patients aged 18–65 years compared to those aged more than 65 years (P < 0.001 for all comparisons).
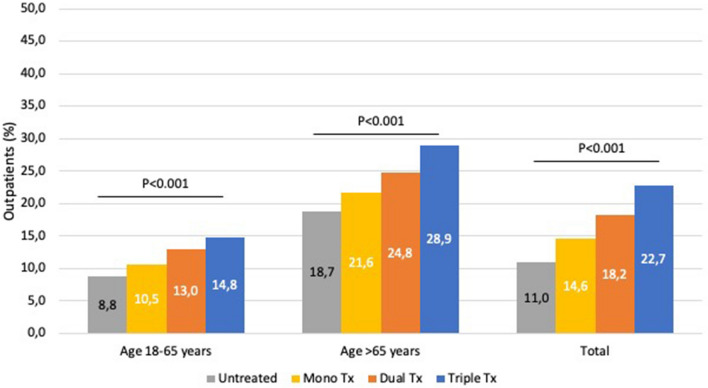
Proportion of hypertensive patients treated with monotherapies and achieving the conventional BP goal of less than 140/90 mmHg was 36.6%. Proportions of patients achieving the office BP goals recommended by the current European guidelines [11] and according to different age strata are illustrated in Fig. 2. Only 14.0% of those patients under single antihypertensive agent reached the BP treatment targets. In particular, 10.2% patients aged 18–65 years and 20.4% of those aged > 65 years achieved the recommended BP goals, respectively. When compared these data with other antihypertensive strategies applied in hypertensive outpatients extracted from the same database during the same observational period, both these proportions results significantly lower than those achieved with dual (18.2%) or triple (22.2%) combination therapy, though higher than those obtained with life-style changes (10.8%).
Fig. 2.
Proportions of hypertensive outpatients treated with monotherapies and achieving the recommended BP targets according to 2018 ESC/ESH hypertension guidelines and age strata.
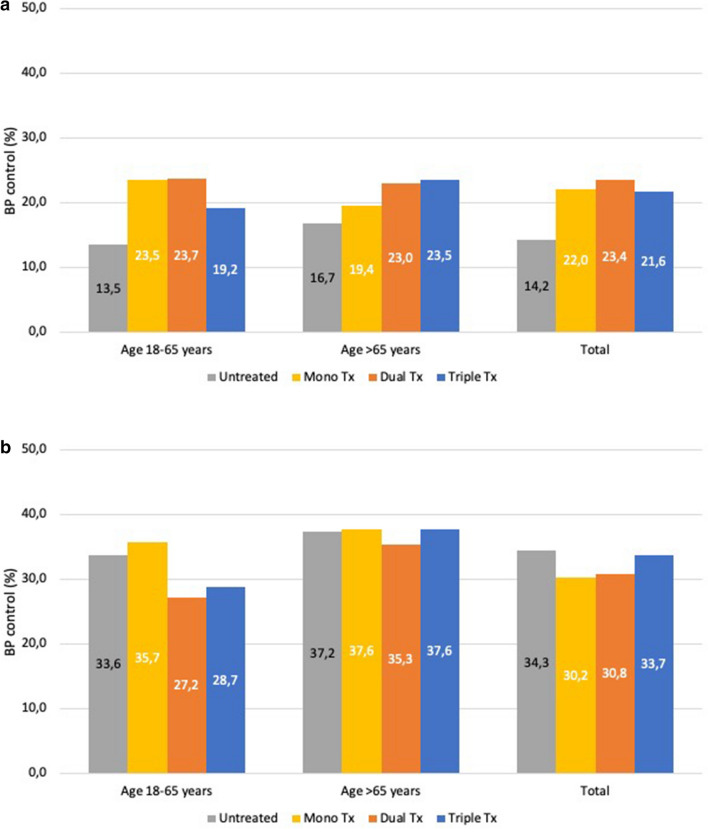
Proportions of patients with home and 24-hour BP levels within the normal values are illustrated in Fig. 3. In the overall population, 22.0% of patients had home BP values < 135/85 mmHg and 30.2% of patients had 24-h BP values < 130/80 mmHg under monotherapies. Of note, only 5.2% and 7.3% of these patients achieved sustained BP control according to clinic and either home or 24-h BP, respectively.
Fig. 3.
Proportions of hypertensive outpatients treated with monotherapies and achieving the recommended home (a) and 24-h (b) BP targets and age strata.
Among patients treated with different classes of antihypertensive agents used in monotherapies, 15.5% of those treated with ARBs achieved the BP treatment targets recommended by guidelines, whilst these BP goals were achieved in 12.7% patients with ACE inhibitors, 14.9% with beta blockers, 12.0% with CCBs, and 8.5% with diuretics. Of note, about half of patients treated with ARB-based monotherapies also showed out-of-office BP levels within the normal BP thresholds; in particular, 51.1% had home BP levels less than 135/85 mmHg, and 42.4% 24-h BP levels less than 130/80 mmHg, thus resulting in sustained BP control.
Univariate and Multivariate Analysis for the Achievement of BP Treatment Targets
This analysis for predicting the achievement of predefined BP treatment targets is reported in Table 3. Ageing and presence of dyslipidaemia resulted significant and independent predictive factors for the predefined BP treatment targets, whilst European SCORE showed negative predictive value at multivariate analysis.
Table 3.
Univariate and multivariate analysis for factors predisposing the achievement of systolic/diastolic blood pressure treatment targets in hypertensive outpatients treated with monotherapies
| Parameters | Univariate analysis | Multivariate analysis | ||
|---|---|---|---|---|
| HR (95% CI) | P value | HR (95% CI) | P value | |
| Age (years) | 1.032 (1.020–1.043) | < 0.001 | 1.050 (1.035–1.065) | < 0.001 |
| BMI (kg/m2) | 0.992 (0.960–1.025) | 0.621 | – | – |
| Smoke (%) | 0.719 (0.433–1.194) | 0.203 | – | – |
| Obesity (%) | 0.953 (0.734–1.272) | 0.746 | – | – |
| Dyslipidaemia (%) | 1.878 (1.404–2.512) | < 0.001 | 1.742 (1.287–2.359) | < 0.001 |
| Diabetes (%) | 1.423 (0.906–2.235) | 0.126 | – | – |
| CAD (%) | 2.182 (0.912–5.222) | 0.080 | – | – |
| TIA/stroke (%) | 1.449 (0.779–2.695) | 0.242 | – | – |
| TOT-C (mg/dl) | 1.001 (0.993–1.009) | 0.803 | – | – |
| HDL-C (mg/dl) | 1.006 (0.986–1.027) | 0.566 | – | – |
| LDL-C (mg/dl) | 0.997 (0.989–1.005) | 0.458 | – | – |
| TG (mg/dl) | 0.999 (0.994–1.004) | 0.759 | – | – |
| BUN (mg/dl) | 1.012 (0.987–1.037) | 0.363 | – | – |
| Creatinine (mg/dl) | 0.881 (0.437–1.775) | 0.723 | – | – |
| eGFR (mg/ml) | 0.999 (0.995–1.004) | 0.819 | – | – |
| Uric acid (mg/dl) | 1.311 (0.747–2.302) | 0.345 | – | – |
| Esc score (%)* | 0.984 (0.969–0.999) | 0.038 | 0.941 (0.918–0.965) | < 0.001 |
| Italian Cuore Score (%)* | 0.988 (0.968–1.009) | 0.258 | – | – |
Discussion
It has been repeatedly reported that in most countries only about 40% of patients affected by hypertension are treated and among these only 35% achieved the recommended BP treatment targets of less than 140/90 mmHg [6–9]. Several reasons might be proposed for trying to explain such relatively low rate of BP control, despite the availability of numerous, safe and effective antihypertensive agents [26–28] and an acceptable level of individuals’ awareness [29]. Among these reasons, the “single-pill approach” of low risk or newly diagnosed hypertensive patients is probably the most relevant issue.
Over the last decades, the most frequently adopted antihypertensive strategy was based on the initial use of different monotherapies, increasing their dose, or substituting for another single agent in case of unsatisfactory BP control during patients’ follow up. This approach was recommended by international scientific societies until the issue of the 2013 European hypertension guidelines [20], whilst the guidelines released in 2018 [11] gave more emphasis on first-line combination treatment and on add-on strategy, with the aim of reducing the number of patients without effective and sustained BP control. This was a landmark revolution for the clinical management of hypertension, since it changed the therapeutic approach used so far.
This novel approach was based on the consideration that the initial use of different monotherapies, by antagonizing only one pathophysiological pathway involved in the multifactorial BP control, have demonstrated to provide limited BP outcomes. On the other hand, the use of combinations of different drug classes, by acting on several pathophysiological mechanisms involved in the BP regulation (i.e. blocking RAS as well as induce diuresis and/or vasodilating) may lead to greater antihypertensive effect compared to that obtained with monotherapy [1–4, 30, 31]. A potential limitation of the “fixed-dose combination pill approach” is the lack of possibility in titrating single dose agent, however it offers greater benefit in term of organ damage protection and therapeutic adherence when compared to increasing the dose of monotherapy [32].
Our study started on the recognition that nowadays monotherapies are still widely used in low-risk or naïve hypertensive patients. However, limited data are available regarding how is the proportion of patients under monotherapies and how many achieve the recommended 2018 ESC/ESH BP treatment targets. In our population sample, we were able to demonstrate that monotherapies are used in about 18% of treated hypertensive patients and that only about 37% of these patients reached the conventional clinic BP goal of < 140/90 mmHg. However, when considering the most recent 2018 European guidelines BP treatment targets [11], only 14% of patients treated with monotherapies achieved these BP goals, thus confirming a relatively low antihypertensive effect provided by this therapeutic approach compared to dual or triple combination therapies.
Our analysis was also able to confirm that different classes of antihypertensive agents used in onotherapies resulted in relatively poor rate of control of out-of-office BP levels, including home and 24-h ambulatory BP measurements. This is of key clinical relevance, since it has been clearly demonstrated a positive and significant relationship between high out-of-office BP levels and increased risk of developing HMOD [33–36], metabolic abnormalities [37–41] and CV outcomes [19, 42–44].
Although antihypertensive treatment should be individualized depending on characteristics of single patient [45, 46], and short follow-up of patients treated with monotherapy may contribute to implement the attained BP control rate, our findings highlight the need to readdress clinicians’ approach to antihypertensive therapy in favour of a more extended use of combination therapies with respect to monotherapies.
Study Limitations
The present study has some potential limitations that should be acknowledged. First of all, patients included in the present analysis were consecutively enrolled more than 15 years ago. During this time, several sets of guidelines and recommendations from national and international societies have been produced [11, 20], furthermore single-pill combination therapy has been proposed and widely prescribed in the last few years, so this may influence the current rate of BP control. Second, we have no data on therapeutic adherence since we have not routinely applied questionnaire or executed serum levels of drugs analyses which could may help to understand the reason of low rate of BP target achievement. Finally, data have been extracted from a large and long database of hypertensive outpatients who were referred to an excellence hypertension center, thus potential selection bias with regard to difficult-to-treat hypertension phenotypes should be considered. This might also explain the relatively low rates of BP control reported in our population sample, independently by how BP were measured or how many drugs were used [18, 47].
Conclusions
Our study confirms that BP control with monotherapy regimen is relatively low compared to that obtained with dual or triple combination therapies. According to our findings, and in line with the recommendations of current European guidelines [11], it is necessary to implement both pharmacologic and non-pharmacologic antihypertensive strategies, in order to reach the recommended BP targets, achieve an effective and sustained BP control and reduce the burden of hypertension-related CV diseases and CV death. In this view, combination therapy seem to provide greater antihypertensive effect than monotherapy, even when the latter are used at high doses. Therefore, physicians should consider combination therapy with more attention for reach BP levels goal especially in the light of new ambitious BP target proposed by recent guidelines [11], and the deserve the use of monotherapies in some selected clinical conditions, depending on physicians’ judgment and individual global CV risk profile.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary file1 Flow-chart for the selection of the study population of hypertensive patients under monotherapies (JPEG 64 kb)
Declarations
Funding
Open access funding provided by Università degli Studi di Roma La Sapienza within the CRUI-CARE Agreement.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Code availability statements
Not applicable.
References
- 1.Dahlöf B, et al. Prevention of cardiovascular events with an antihypertensive regimen of amlodipine adding perindopril as required versus atenolol adding bendroflumethiazide as required, in the Anglo-Scandinavian Cardiac Outcomes Trial-Blood Pressure Lowering Arm (ASCOT-BPLA): a multicentre randomised controlled trial. Lancet. 2005;366(9489):895–906. doi: 10.1016/S0140-6736(05)67185-1. [DOI] [PubMed] [Google Scholar]
- 2.Julius S, et al. Outcomes in hypertensive patients at high cardiovascular risk treated with regimens based on valsartan or amlodipine: the VALUE randomised trial. Lancet. 2004;363(9426):2022–2031. doi: 10.1016/S0140-6736(04)16451-9. [DOI] [PubMed] [Google Scholar]
- 3.ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) JAMA. 2002;288(23):2981–2997. doi: 10.1001/jama.288.23.2981. [DOI] [PubMed] [Google Scholar]
- 4.Jamerson K, et al. Benazepril plus amlodipine or hydrochlorothiazide for hypertension in high-risk patients. N Engl J Med. 2008;359(23):2417–2428. doi: 10.1056/NEJMoa0806182. [DOI] [PubMed] [Google Scholar]
- 5.Dahlöf B, et al. Cardiovascular morbidity and mortality in the Losartan intervention for endpoint reduction in hypertension study (LIFE): a randomised trial against atenolol. Lancet. 2002;359(9311):995–1003. doi: 10.1016/S0140-6736(02)08089-3. [DOI] [PubMed] [Google Scholar]
- 6.Chow CK, et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA. 2013;310(9):959–968. doi: 10.1001/jama.2013.184182. [DOI] [PubMed] [Google Scholar]
- 7.Borghi C, et al. Lack of control of hypertension in primary cardiovascular disease prevention in Europe: results from the EURIKA study. Int J Cardiol. 2016;218:83–88. doi: 10.1016/j.ijcard.2016.05.044. [DOI] [PubMed] [Google Scholar]
- 8.Tocci G, et al. Prevalence and control of hypertension in the general practice in Italy: updated analysis of a large database. J Hum Hypertens. 2017;31(4):258–262. doi: 10.1038/jhh.2016.71. [DOI] [PubMed] [Google Scholar]
- 9.Geldsetzer P, et al. The state of hypertension care in 44 low-income and middle-income countries: a cross-sectional study of nationally representative individual-level data from 1·1 million adults. Lancet. 2019;394(10199):652–662. doi: 10.1016/S0140-6736(19)30955-9. [DOI] [PubMed] [Google Scholar]
- 10.Volpe M, et al. 2012 consensus document of the Italian Society of Hypertension (SIIA): strategies to improve blood pressure control in Italy: from global cardiovascular risk stratification to combination therapy. High Blood Press Cardiovasc Prev. 2013;20(1):45–52. doi: 10.1007/s40292-013-0007-2. [DOI] [PubMed] [Google Scholar]
- 11.Williams B, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018;39(33):3021–3104. doi: 10.1093/eurheartj/ehy339. [DOI] [PubMed] [Google Scholar]
- 12.Volpe M, Gallo G, Tocci G. Novel blood pressure targets in patients with high-normal levels and grade 1 hypertension: room for monotherapy? Int J Cardiol. 2019;291:105–111. doi: 10.1016/j.ijcard.2019.04.074. [DOI] [PubMed] [Google Scholar]
- 13.Del Pinto R, et al. Prevalence of hypertension and associated cardiovascular risk factors among pharmacies customers: an Italian nationwide epidemiological survey. Eur J Prev Cardiol. 2020;27(11):1228–1230. doi: 10.1177/2047487319851301. [DOI] [PubMed] [Google Scholar]
- 14.Torlasco C, et al. Nation-wide hypertension screening in Italy: data from May measurements month 2017—Europe. Eur Heart J Suppl. 2019;21(Suppl D):D66–D70. doi: 10.1093/eurheartj/suz058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.De Giusti M, et al. A survey on blood pressure levels and hypertension control in a sample of the Italian general population. High Blood Press Cardiovasc Prev. 2012;19(3):129–135. doi: 10.2165/11632190-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 16.Rea F, et al. Initial antihypertensive treatment strategies and therapeutic inertia. Hypertension. 2018;72(4):846–853. doi: 10.1161/HYPERTENSIONAHA.118.11308. [DOI] [PubMed] [Google Scholar]
- 17.Egan BM, et al. Initial monotherapy and combination therapy and hypertension control the first year. Hypertension. 2012;59(6):1124–1131. doi: 10.1161/HYPERTENSIONAHA.112.194167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tocci G, et al. Reclassification of hypertensive outpatients according to new US guidelines on high blood pressure. Am J Hypertens. 2019;32(1):77–87. doi: 10.1093/ajh/hpy139. [DOI] [PubMed] [Google Scholar]
- 19.Tocci G, et al. Prevalence and clinical outcomes of white-coat and masked hypertension: analysis of a large ambulatory blood pressure database. J Clin Hypertens (Greenwich) 2018;20(2):297–305. doi: 10.1111/jch.13181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mancia G, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) Eur Heart J. 2013;34(28):2159–2219. doi: 10.1093/eurheartj/eht151. [DOI] [PubMed] [Google Scholar]
- 21.Expert Panel on Detection, and Treatment of High Blood Cholesterol in Adults The Third Report of The National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III) JAMA. 2001;285(19):2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 22.Rydén L, et al. ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD: the Task Force on diabetes, pre-diabetes, and cardiovascular diseases of the European Society of Cardiology (ESC) and developed in collaboration with the European Association for the Study of Diabetes (EASD) Eur Heart J. 2013;34(39):3035–3087. doi: 10.1093/eurheartj/eht108. [DOI] [PubMed] [Google Scholar]
- 23.Thygesen K, et al. Universal definition of myocardial infarction. Eur Heart J. 2007;28(20):2525–2538. doi: 10.1093/eurheartj/ehm355. [DOI] [PubMed] [Google Scholar]
- 24.Goldstein LB, et al. Primary prevention of ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council: cosponsored by the Atherosclerotic Peripheral Vascular Disease Interdisciplinary Working Group; Cardiovascular Nursing Council; Clinical Cardiology Council; Nutrition, Physical Activity, and Metabolism Council; and the Quality of Care and Outcomes Research Interdisciplinary Working Group. Circulation. 2006;113(24):e873–923. doi: 10.1161/01.STR.0000223048.70103.F1. [DOI] [PubMed] [Google Scholar]
- 25.Easton JD, et al. Definition and evaluation of transient ischemic attack: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association Stroke Council; Council on Cardiovascular Surgery and Anesthesia; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Nursing; and the Interdisciplinary Council on Peripheral Vascular Disease. The American Academy of Neurology affirms the value of this statement as an educational tool for neurologists. Stroke. 2009;40(6):2276–2293. doi: 10.1161/STROKEAHA.108.192218. [DOI] [PubMed] [Google Scholar]
- 26.Cicero AFG, et al. Nutrients and nutraceuticals for the management of high normal blood pressure: an evidence-based consensus document. High Blood Press Cardiovasc Prev. 2019;26(1):9–25. doi: 10.1007/s40292-018-0296-6. [DOI] [PubMed] [Google Scholar]
- 27.Borghi C, et al. Role of the renin-angiotensin-aldosterone system and its pharmacological inhibitors in cardiovascular diseases: complex and critical issues. High Blood Press Cardiovasc Prev. 2015;22(4):429–444. doi: 10.1007/s40292-015-0120-5. [DOI] [PubMed] [Google Scholar]
- 28.Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure-lowering treatment on cardiovascular outcomes and mortality: 14—effects of different classes of antihypertensive drugs in older and younger patients: overview and meta-analysis. J Hypertens. 2018;36(8):1637–1647. doi: 10.1097/HJH.0000000000001777. [DOI] [PubMed] [Google Scholar]
- 29.Volpe M, et al. New opportunities for monitoring blood pressure control and awareness in the population: insights from 12-year editions of the World Hypertension Day. High Blood Press Cardiovasc Prev. 2016;23(4):333–335. doi: 10.1007/s40292-016-0172-1. [DOI] [PubMed] [Google Scholar]
- 30.Wald DS, et al. Combination therapy versus monotherapy in reducing blood pressure: meta-analysis on 11,000 participants from 42 trials. Am J Med. 2009;122(3):290–300. doi: 10.1016/j.amjmed.2008.09.038. [DOI] [PubMed] [Google Scholar]
- 31.SPRINT Research Group A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2017;377(25):2506. doi: 10.1056/NEJMx170008. [DOI] [PubMed] [Google Scholar]
- 32.Tocci G, Volpe M. Modern clinical management of arterial hypertension: fixed or free combination therapies? High Blood Press Cardiovasc Prev. 2011;18(Suppl 1):3–11. doi: 10.2165/1159615-s0-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 33.Cuspidi C, et al. Incident left ventricular hypertrophy in masked hypertension. Hypertension. 2019;74(1):56–62. doi: 10.1161/HYPERTENSIONAHA.119.12887. [DOI] [PubMed] [Google Scholar]
- 34.Tadic M, Cuspidi C. Left ventricular remodeling and masked hypertension: don't forget nighttime diastolic blood pressure. Am J Hypertens. 2019;32(6):535–537. doi: 10.1093/ajh/hpz047. [DOI] [PubMed] [Google Scholar]
- 35.Cuspidi C, et al. Untreated masked hypertension and carotid atherosclerosis: a meta-analysis. Blood Press. 2015;24(2):65–71. doi: 10.3109/00365521.2014.992185. [DOI] [PubMed] [Google Scholar]
- 36.Tientcheu D, et al. Target organ complications and cardiovascular events associated with masked hypertension and white-coat hypertension: analysis from the Dallas heart study. J Am Coll Cardiol. 2015;66(20):2159–2169. doi: 10.1016/j.jacc.2015.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cuspidi C, et al. Risk of new-onset metabolic syndrome associated with white-coat and masked hypertension: data from a general population. J Hypertens. 2018;36(9):1833–1839. doi: 10.1097/HJH.0000000000001767. [DOI] [PubMed] [Google Scholar]
- 38.Mengden T, et al. Blood pressure control and cardiovascular risk in hypertensive patients with type 2 diabetes: The German T2Target registry. J Clin Hypertens (Greenwich) 2017;19(8):757–763. doi: 10.1111/jch.13001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hänninen MR, et al. Metabolic risk factors and masked hypertension in the general population: the Finn-Home study. J Hum Hypertens. 2014;28(7):421–426. doi: 10.1038/jhh.2013.129. [DOI] [PubMed] [Google Scholar]
- 40.Franklin SS, et al. Masked hypertension in diabetes mellitus: treatment implications for clinical practice. Hypertension. 2013;61(5):964–971. doi: 10.1161/HYPERTENSIONAHA.111.00289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mancia G, et al. Increased long-term risk of new-onset diabetes mellitus in white-coat and masked hypertension. J Hypertens. 2009;27(8):1672–1678. doi: 10.1097/HJH.0b013e32832be5f9. [DOI] [PubMed] [Google Scholar]
- 42.Presta V, et al. Nocturnal blood pressure patterns and cardiovascular outcomes in patients with masked hypertension. J Clin Hypertens (Greenwich) 2018;20(9):1238–1246. doi: 10.1111/jch.13361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Satoh M, et al. Long-term stroke risk due to partial white-coat or masked hypertension based on home and ambulatory blood pressure measurements: the Ohasama study. Hypertension. 2016;67(1):48–55. doi: 10.1161/HYPERTENSIONAHA.115.06461. [DOI] [PubMed] [Google Scholar]
- 44.Mancia G, et al. Long-term risk of sustained hypertension in white-coat or masked hypertension. Hypertension. 2009;54(2):226–232. doi: 10.1161/HYPERTENSIONAHA.109.129882. [DOI] [PubMed] [Google Scholar]
- 45.Volpe M, et al. Personalised single-pill combination therapy in hypertensive patients: an update of a practical treatment platform. High Blood Press Cardiovasc Prev. 2017;24(4):463–472. doi: 10.1007/s40292-017-0239-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Volpe M, et al. ARB-based single-pill platform to guide a practical therapeutic approach to hypertensive patients. High Blood Press Cardiovasc Prev. 2014;21(2):137–147. doi: 10.1007/s40292-014-0043-6. [DOI] [PubMed] [Google Scholar]
- 47.Tocci G, et al. Blood pressure targets achievement according to 2018 ESC/ESH guidelines in three European excellence centers for hypertension. High Blood Press Cardiovasc Prev. 2020;27(1):51–59. doi: 10.1007/s40292-020-00359-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary file1 Flow-chart for the selection of the study population of hypertensive patients under monotherapies (JPEG 64 kb)