INTRODUCTION
Burnout is a serious concern in medical education and practice with negative impacts on professionalism and patient care. Accurate measurement of burnout is necessary for medical education scholarship and intervention evaluation. The Maslach Burnout Inventory (MBI) is a validated 22-item tool with three domains of emotional exhaustion (EE), depersonalization (DP), and personal accomplishment (PA) 1. EE refers to the feeling of being overextended and depleted, while DP refers to a detached or callous attitude towards patients and PA refers to a sense of professional achievement.
A 1-item measure used in the Physician Work Life Study (PWLS) correlates well with the full MBI among practicing physicians 2. This measure shows stronger correlation with EE than with DP for physicians and other practitioners, suggesting that these domains of burnout may not be captured equally 3. The 1-item PWLS measure is thought to be faster and easier to administer than the full MBI and is available at no cost. However, the correlation between this 1-item measure and the domains of the full MBI has not been established for physicians-in-training. Medical students, residents, and practicing physicians all have higher levels of burnout than the general population, but the patterns of stressors they experience may differ. During medical school, students experience the stress of new clinical responsibilities and emotional burdens, in addition to the pressure of succeeding at their academic work, with implications for their future career paths. Different dimensions of distress may affect different stages of training and career more than others 4. Therefore, we sought to investigate whether measures previously correlated among practicing physicians would demonstrate similar performance in medical students. We aimed to compare measurement of burnout by the PWLS measure as compared with the full MBI domains among medical students.
METHODS
All medical students at the University of Virginia School of Medicine receive an online survey annually for observational study of their burnout and well-being. Since 2014, this survey has included the full MBI to measure burnout. In the 2017–2018 academic year, we added the 1-item PWLS burnout measure. This item asks respondents to rate their level of burnout with responses from 1 (no burnout) to 5 (severe burnout). Previously established cut-offs for high scores were used for both measures 2,4. Scores on the 1-item PWLS burnout measure and the full MBI domains of EE, DP, and PA were compared using Spearman’s correlation and chi-squared tests. Sensitivity, specificity, and area under the receiver operating characteristic (ROC) curve were calculated using the ROC curve procedure. Students from all four years of training were pooled for cross-sectional analysis. The study was approved by the IRB. Analyses were performed with SPSS Statistics version 26 (IBM, Armonk, NY, USA).
RESULTS
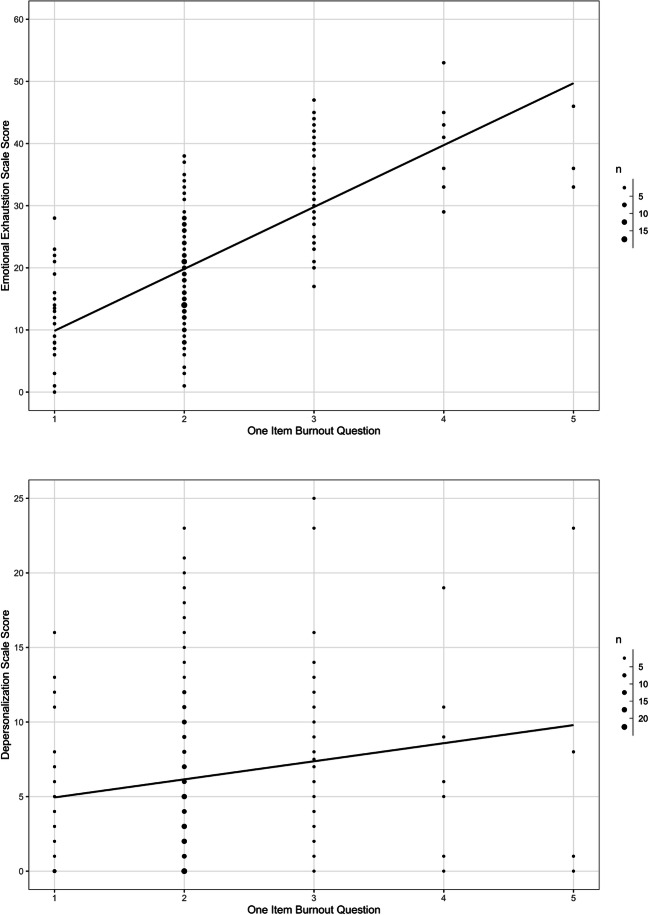
Of the 631 surveys sent, 287 students completed the 1-item PWLS burnout question and the full MBI (46% response rate). Survey respondents were 54% female, 63% single in relationship status, comparable to the medical school population. The median score for EE was 20 (range 0 to 53), for DP was 5 (range 0 to 25), and for PA was 38 (range 3 to 48). The median score on the 1-item PWLS measure was 2 (range 1 to 5). For each of these measures, higher scores indicate higher burnout except for PA where lower scores indicate higher burnout. Scores on EE and DP domains were moderately correlated with each other (r = 0.425, p < 0.001). The correlation of PA with EE was 0.284 (p < 0.001) and with DP was 0.071 (p = 0.013). Scores on the 1-item PWLS measure showed stronger correlation with EE scores (r = 0.642, p < 0.001) than with DP scores (r = 0.172, p = 0.007), as shown in Figure 1, and PA scores (r = 0.321, p < 0.001). High burnout was reported by 34% of students for EE (scores above 27), 25% for DP (above 10), and 17% for PA (below 32). On the 1-item PWLS measure, 21% of students reported high burnout (3 and above). Students with high scores on the 1-item PWLS measure were more likely to have high EE than those who had low scores (86% vs. 19%, p < 0.001) and low vs. high PA (33% vs. 13%, p = 0.001) but no significant difference for high vs. low DP (31% vs. 24%, p = 0.248). The sensitivity of the 1-item PWLS measure for a high score on the EE scale was 0.552 with a specificity of 0.953 (area under the ROC curve 0.782); for a high score on the DP scale, the sensitivity was 0.260 with a specificity of 0.814 (area under the ROC curve 0.552); and for a low score on the PA scale, the sensitivity was 0.408 with a specificity of 0.826 (area under the ROC curve 0.639).
Figure 1.
Correlation of burnout levels as measured by the Maslach Burnout Inventory domains of emotional exhaustion and depersonalization with burnout levels on the single-item Physician Work Life Study measure (“1-Item Burnout”). Higher numbers on each axis indicate higher levels of burnout.
DISCUSSION
The 1-item PWLS measure correlated better with EE than with DP or PA domains of burnout. This is consistent with studies comparing the PWLS measure with the full MBI in physicians and other practitioners 2,3. For all three components of burnout, the specificity of the one-question test is higher than the sensitivity. A high PWLS score was significantly more likely to be associated with a high EE or low PA score than was a low score, while there was no significant difference for DP. Even for EE which has the highest ROC, at a cut-off of 3, the PWLS measure only identified 55% of students who had high EE scores. Most students with high PWLS scores had high EE, but it failed to identify almost half who did.
When asked by the 1-item measure to rate their own level of burnout, respondents may primarily express how drained or fatigued they feel, which corresponds better to EE. However, DP appears to measure a different concept which captures the ability to treat patients with empathy. DP is a particularly worrisome aspect of burnout because it may undermine the formation of therapeutic relationships with patients and how well future physicians deliver patient-centered care. DP may not be well evaluated by the 1-item PWLS burnout measure, as compared to the full MBI, and should be used and interpreted with caution by medical educators and researchers. Also, a small proportion of students reported high levels of burnout on the PWLS measure, which suggests that its discriminatory ability may not be confidently assessed in individuals at highest risk for burnout, but it may be more useful as a tool to rule out high burnout.
Single-item measures have been developed from the MBI, one to capture the EE domain (MBI:EE) and one for the DP domain (MBI:DP), and have demonstrated concurrent validity with the full MBI 5. The PWLS measure correlates well with the MBI:EE among primary care providers and staff 6. Using these measures would be another option to overcome the survey burden of the full MBI, though not the issue of proprietary use. The PWLS measure could also be used in situations where emotional exhaustion is the main variable or outcome of interest and the full MBI when other domains of burnout are needed.
Limitations to this study include risk of limited generalizability from a single-institution study and possible selection bias, if students responding to the survey are inherently different from their peers. Next steps include longitudinal study of burnout predictors and further investigation of how best to prevent and mitigate burnout among our physicians-in-training.
Compliance with Ethical Standards
This study was approved by the University of Virginia Institutional Review Board for the Social and Behavioral Sciences.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Maslach C, Jackson SE. The measurement of experienced burnout. Journal of Organizational Behavior. 1981;2:99–113. doi: 10.1002/job.4030020205. [DOI] [Google Scholar]
- 2.Rohland B, Kruse GR, Rohrer JE. Validation of a single-item measure of burnout against the Maslach Burnout Inventory among physicians. Stress and Health. 2004;20:75–9. doi: 10.1002/smi.1002. [DOI] [Google Scholar]
- 3.Waddimba AC, Scribani M, Nieves MA, Krupa N, May JJ, Jenkins P. Validation of Single-Item Screening Measures for Provider Burnout in a Rural Health Care Network. Eval Health Prof. 2016;39:215–25. [DOI] [PubMed]
- 4.Dyrbye LN, West CP, Satele D, et al. Burnout among U.S. medical students, residents, and early career physicians relative to the general U.S. population. Acad Med. 2014;89:443–51. doi: 10.1097/ACM.0000000000000134. [DOI] [PubMed] [Google Scholar]
- 5.West CP, Dyrbye LN, Satele DV, Sloan JA, Shanafelt TD. Concurrent validity of single-item measures of emotional exhaustion and depersonalization in burnout assessment. J Gen Intern Med 2012;27:1445–52. [DOI] [PMC free article] [PubMed]
- 6.Dolan ED, Mohr D, Lempa M, et al. Using a single item to measure burnout in primary care staff: a psychometric evaluation. J Gen Intern Med 2015;30:582–7. [DOI] [PMC free article] [PubMed]