Abstract
Purpose of Review
Anterior knee pain is a common musculoskeletal complaint among people of all ages and activity levels. Non-operative approaches with an emphasis on physical therapy management are the recommended initial course of care. The purpose of this review is to describe the current evidence for physical therapist management of anterior knee pain with consideration of biomechanical and psychosocial factors.
Recent Findings
The latest research suggests anterior knee pain is a combination of biomechanical, neuromuscular, behavioral, and psychological factors. Education strategies to improve the patient’s understanding of the condition and manage pain are supported by research. Strong evidence continues to support the primary role of exercise therapy and load progression to achieve long-term improvements in pain and function. Preliminary studies suggest blood flow restriction therapy and movement retraining may be useful adjunct techniques but require further well-designed studies.
Summary
Anterior knee pain includes multiple conditions with patellofemoral pain being the most common. An insidious onset is typical and often attributed to changes in activity and underlying neuromuscular impairments. A thorough clinical history and physical examination aim to identify the patient’s pain beliefs and behaviors, movement faults, and muscle performance that will guide treatment recommendations. Successful physical therapist management involves a combination of individualized patient education, pain management, and load control and progression, with an emphasis on exercise therapy.
Keywords: Patellofemoral, jumper’s knee, runner’s knee, Exercise therapy
Introduction
Anterior knee pain (AKP) is a common musculoskeletal complaint contributing to functional limitation in persons of all ages and activity levels. Symptoms associated with AKP can have a significant adverse impact on a person’s function, overall health, and quality of life [1, 2]. AKP encompasses multiple clinical conditions with patellofemoral pain being the most common. Various clinical findings are associated with AKP including patellar hyper- or hypo-mobility, impaired quadriceps or hip muscle performance, dynamic knee valgus, foot over-pronation, impaired mobility of anterior-lateral thigh soft tissues, chondral lesions, synovial, bursae or tendon reactivity, and fear-avoidance beliefs (e.g., catastrophization, kinesiophobia) [2–6, 7•]. Advanced imaging may reveal structural abnormalities (e.g., cartilage lesions, meniscus lesions, patellofemoral dysplasia, osteoarthritis) in persons with AKP. Despite these possible imaging findings, surgical interventions are not superior to non-operative treatment in persons 18–40 years old [3, 8], with evidence favoring non-operative management in older persons (48–63 years), as well [9]. Therefore, non-operative approaches with an emphasis on physical therapy treatment are the recommended initial course of care while surgery is reserved for non-responsive cases. The purpose of this review is to describe the current evidence for physical therapist management of AKP with consideration of biomechanical and psychosocial factors.
History and Physical Examination
Individuals with AKP complain of pain in the anterior knee or retropatellar regions that increase with running, squatting, ascending/descending stairs, and following periods of prolonged sitting. Rarely will an individual report a specific mechanism of injury, but rather an insidious onset of pain that is repeatedly aggravated by a continuation of the provoking activity. As such, the patient history should focus on corresponding changes in physical behaviors and characteristics. In the physically active patient, alterations in training load (intensity, duration, or frequency), environment, or mode are highly relevant and a frequent contributor to symptom development. Personal characteristic changes that contribute to AKP include weight gain or loss, shift in activity-related biomechanics (e.g., new running or squatting form), different footwear or foot orthoses, and modified daily behavior (e.g., time spent sitting, standing, walking, or stair use). Prior injury or surgery to the knee joint often leads to AKP, as inflammation, joint effusion, reduced joint mobility, and quadriceps neuromuscular dysfunction jeopardize efficient knee function. For example, following bone-patellar-tendon-bone anterior cruciate ligament reconstruction, up to 23% of patients experience AKP [10].
Baseline function and symptoms, along with progression of recovery, are typically assessed with patient-reported outcome measures including numeric or visual analog pain rating, patient-reported outcome measurement system (PROMIS), patellofemoral subscale of the knee injury and osteoarthritis outcome score (KOOS-PF), anterior knee pain scale (AKPS), and global rating of change scale [11–13]. Additional questionnaires such as the Tampa scale for kinesiophobia (TSK), fear-avoidance beliefs questionnaire (FABQ), and pain catastrophizing scale (PCS) can identify psychosocial factors in persons with AKP that informs patient education strategies and exercise progression [6, 13–17].
Physical examination of the patient with AKP aims to identify biomechanical, neuromuscular, and myofascial impairments that will guide treatment recommendations when integrated with the clinical history [4, 18–22]. Diagnostic tests generally have limited predictive value for AKP as conditions are typically diagnoses of exclusion. A test cluster is recommended in the diagnosis of patellofemoral pain and includes pain with (1) resisted knee extension; (2) palpation of the posteromedial or posterolateral patella; and (3) squatting [23]. If the patient has pain with two of the three tests, the +LR is 4.0 (−LR, 0.5). The step down test can help to rule in patellofemoral pain when the patient’s chief complaint is reproduced while slowly descending from a standard step (+LR, 2.34; −LR 0.7) [24]. Due to the variety of conditions involved with AKP, tenderness with palpation may also be present with the infrapatellar tendon and fat pad, tibial tubercle, and suprapatellar quadriceps tendon. Weakness of the posterolateral hip musculature, in particular the hip abductors, is often present and is associated with increased dynamic knee valgus during loading [25].
Interventions
Evolution of Care
The current patient education and load management approach to non-operative care of AKP has evolved from the best available evidence and expert consensus [26••]. Over the years, various clinical trends have emerged, only to fade as their inefficacy materializes. Biophysical agents (e.g., cryotherapy, ultrasound, transcutaneous electrical nerve stimulation), once considered a mainstay of AKP care, are now regarded as having no added benefit to therapeutic exercise intervention [27–29]. Patellar taping may have immediate pain management benefits when combined with exercise for some with AKP [30], but does not influence patellofemoral contact area, alignment, or muscle activation patterns [31–33]. Patellofemoral bracing (e.g., sleeve or strap) provides no additional benefit than exercise therapy alone [34]. Likewise, EMG-based biofeedback of the vastus medialis muscle during exercise therapy has no added benefit on pain or function than exercise alone [35]. Indeed, the goal of preferentially recruiting the vastus medialis (oblique) due to a delayed activation onset is ineffective save a potential subgroup of individuals [36, 37]. Transcutaneous electrical nerve stimulation can transiently increase quadriceps activation and decrease pain similar to other modalities such as ice, but no additional benefit to exercise has been demonstrated [28, 29, 38]. Despite the limited benefit from these adjunct treatments, exercise therapy remains the cornerstone of AKP care and is recommended to reduce pain in the short, medium, and long term, and to improve function in the medium and long term [26••].
Patient Education
Educational strategies are essential in management of AKP [39, 40] to improve the patient’s understanding of the condition, treatment options, and expectations, and to address treatment barriers related to pain beliefs and behaviors [2]. Patients with AKP want to know why they are hurting, and their adherence to the rehabilitation approach hinges on comprehension of the problem and confidence in the treatment plan [39, 41]. Most research on educational intervention for AKP is specific to persons with patellofemoral pain [2, 41, 42•], but these same concepts and those from research related to pain education [43, 44] can be applied to other AKP conditions. Patient education should target barriers to treatment, particularly management of exercise and activities that stem from patient concerns or confusion about pain mechanisms. These beliefs contribute to anxiety, fear-avoidance behaviors, and poor self-efficacy towards recovering function and managing pain. Successful patient education and pain management strategies provided as a part of AKP treatment improve pain, function, and psychological outcomes [14, 45, 46].
Pain Education
Patient education should acknowledge that various structures around the patella may be involved including muscles, nerves, ligaments, and tendons [46], but that pain mechanisms also include psychological and contextual factors [7•]. Patients with AKP commonly assume their pain is related to the accompanying joint noise (crepitus) [2, 47•] and is a result of structural damage, most commonly arthritis [2, 47•]. Although osteoarthritis and other knee structural pathologies can produce nociceptive stimuli and are relevant in plan of care decision-making [48, 49], pathology is often inconsistent with pain levels [50, 51]. In addition, patients without evidence of structural damage still associate their pain and crepitus to arthritis which contributes to anxiety and fear-avoidance behaviors [47•].
When crepitus is encountered during treatment, patients appreciate education on the nature of their joint noise and how to react to it [47•]. Common structural reasons the patient attributes to the crepitus (e.g., arthritis and pathomechanics) can be acknowledged [48] along with evidence that pathology is not always consistent with symptoms and function or likelihood of requiring a knee arthroplasty [52, 53]. Modifications to the loading program such as limiting range of motion, adjusting movement mechanics, or use of isometric versus isotonic muscle contractions may reduce crepitus while maintaining benefits of therapeutic intervention (Table 1).
Table 1.
Biomechanical modifications and considerations during prescription of squatting and lunging exercises that inform clinical decision-making to reduce symptoms or crepitus
| Biomechanical strategy | Considerations |
|---|---|
| Reduce weight-bearing (e.g., squat in a supine or semi-recumbent position) | Reduced weight-bearing reduces patellar contact area [54], patellofemoral, tibiofemoral, and patellar tendon load. There is less unilateral patellofemoral stress with a bilateral squat versus a unilateral squat, and in greater than 60° knee flexion, there is less stress during a forward or side lunge versus a single leg squat [55, 56]. |
| Limit range of knee flexion of motion |
Patellofemoral joint stress increases between 60 and 90° knee flexion in weight-bearing and 0–30° knee flexion in non-weight-bearing [57]. To reduce patellofemoral stress, perform weight-bearing exercises in 0–45° knee flexion and non-weight-bearing in 45–90° [57]. Patellar contact area increases to dissipate forces with increased knee flexion [54] and persons with patellofemoral pain have similar contact area at 40° knee flexion, but less contact area at 0° and 20° [58]. Because patellar contact area is the least at 0°, greater sensitivity may be exhibited at this angle with forces from quadriceps contraction. Tibiofemoral joint compressive forces increase from 0° to 55–75° knee flexion during a squat and leg press, and forces are greater during the squat versus the leg press due to greater quadriceps and hamstring activity [59]. Patellar tendon force is lower at lower knee flexion angles when performing a squat from a horizontal and decline surface [60]. |
| Reduce anterior knee translation by preventing knees to pass anterior to the toes |
Knee torque is reduced by 20% when preventing anterior knee translation during a barbell squat, but also increases hip and trunk torque 10-fold [61]. Patellofemoral stress is reduced at 90° knee flexion during a wall squat when the feet are further versus closer to the wall [56], and there is less patellofemoral joint stress when taking a larger step versus a shorter step when performing a forward lunge [62]. Patellar tendon peak stress and stress impulse is lower when performing a forward lunge with the knee behind, versus in front of the toes [63]. Many sport-related activities require tolerance of loading the knee anterior to the toes and require progression from reduced anterior knee translation modification to loading with more anterior knee translation. |
| Reduce knee dynamic valgus via reduced femur internal rotation and adduction | Medial femur rotation and adduction increases patella cartilage stress [64], and medial femur rotation is associated with smaller contact area in persons with patellofemoral pain [65]. Control of dynamic valgus is influenced by hip (e.g., femur abduction and external rotation) and foot and ankle strategies (e.g., rear foot inversion, subtalar supination) [66]. |
| Increase trunk and hip flexion |
In greater than 60° knee flexion, there is less patellofemoral stress when performing a single leg squat compared to a bilateral wall squat due to increased forward trunk flexion during the single leg squat [55, 56]. Increased forward trunk and hip flexion reduces ACL stress due to increased hamstring activity [67]. |
| Perform lunges in-place versus with a step | There is minimal difference in patellofemoral joint stress between lunge (forward and side) and squat (back at wall and single leg) variations in less than 60° knee flexion [55, 56, 62]. Patellofemoral joint stress is less when performing a forward or side lunge in-place versus stepping into the lunge [55]. |
| Perform isometric exercises | Isometric contractions can reduce patellar tendon pain for 45 min and increase maximum voluntary isometric contraction [68]. Static positions during isometric contractions can reduce frequency of crepitus which is associated with fear-avoidance behaviors [47•]. |
| Blood flow restriction training | Blood flow restriction and light-load resistance can improve quadriceps strength in individuals who cannot tolerate heavy-load resistance training [69, 70]. |
Patients can be empowered and engaged in active treatments by re-conceptualizing pain beliefs that are often reinforced by cultural perceptions not consistent with recent evidence [2, 41]. A common belief is the association of impact or knee loading activity (e.g., running and squatting) and development of osteoarthritis. This belief can create reluctance by the patient to participate in these loading activities, including exercises recommended for AKP treatment. Recreational levels of running do not increase knee symptoms or progression of structural pathology in persons with knee osteoarthritis [71], and are associated with reduced disability and mortality in people 50 years and older [72]. Concern regarding the role of physical activity in the development of osteoarthritis can be assuaged by providing education about cartilage development and conditioning. For example, physical activity in younger populations is necessary to maximize cartilage development that occurs until skeletal maturity [73, 74]. After maturity, articular cartilage is conditioned through moderate mechanical loading but will atrophy if loading is insufficient or excessive [75, 76].
Pain Management Strategies
Load management is fundamental to AKP treatment, but patients can be conflicted because loading activities (stairs, squatting, running, and jumping) are associated with their symptoms which results in pain-related fear and maladaptive coping behavior [2]. In addition to education on pain mechanisms, arming the patient with strategies to address pain can improve confidence and adherence throughout treatment.
Pain Monitoring
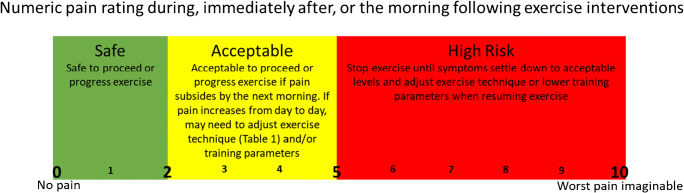
Teaching the patient how to use a pain monitoring system (Fig. 1) to guide load management decision-making is effective in persons with patellofemoral pain and patellar tendinopathy [46, 77, 78]. Pain level (0 = no pain, 10 = worst pain imaginable) is monitored during exercise and the subsequent 24 h. Pain between 0 and 2 is considered “safe,” 2–5 is “acceptable”, and pain greater than 5 should be avoided [45, 46, 78]. Using this system, patients can be considerate of pain related to activity but still engage in exercise or activities essential to their recovery. This system can be integrated into pain education, exercise, and load progression to reduce likelihood of symptom exacerbation. For example, improved pain and function was achieved in runners with patellofemoral pain by using pain monitoring to progress training volume and intensity; specifically, assuring pain during running and the following day was less than 2/10 [45].
Fig. 1.
Pain monitoring system used to guide clinical decision-making of modifications and progression of exercise-based intervention
Unloading
For some patients, a substantial or complete reduction in knee loading may be required as part of the initial symptom management plan. This will typically involve avoidance of sport-related activities (e.g., jumping, running downhill), but may need to extend to some daily activities such as ascending/descending stairs, squatting, and kneeling. This approach is recommended in those with evidence of joint or tissue swelling, highly reactive pain, or a history suggesting an increase in magnitude or frequency of knee tissue loading at a level that exceeds the tissue’s ability to recover. For those meeting this latter characteristic, there may not be any accompanying physical impairment to address through a progressive rehabilitation program. Instead, the unloading period may sufficiently resolve the condition; however, it is critical that this is followed by a period of progressive reloading to avoid symptom recurrence.
Complimentary Symptom Relief Strategies
Adjunct interventions that provide short-term pain relief can gain the patient’s trust and improve participation in exercise interventions [39]. A variety of such interventions include manual therapy, foot orthoses, knee taping/bracing, treatment of trigger points (e.g., dry needling), and cold or heat modalities [79, 80, 81•]. Manual techniques commonly used include patellofemoral joint mobilization, talocrural mobilization and manipulation (often to improve dorsiflexion), lumbopelvic manipulation, soft tissue mobilization (often localized to the lateral knee), and mobilization with movement of the patellofemoral and tibiofemoral joints [79, 80, 82]. Because of limited evidence for custom foot orthoses, prefabricated orthoses are recommended and may be more effective when used with patients based on foot posture and mobility, and when immediate symptom improvements are noted [81•]. Although patellar taping has not demonstrated patellofemoral biomechanical effects [31–33], taping strategies based on the intent to control lateral tilt, glide, and spin for are recommended to achieve pain reduction versus untailored medially directed taping [30]. Evidence suggests dry needling has a moderate short-term effect on improving pain and disability in persons with patellofemoral pain and when combined with exercise interventions [83•].
The determination and selection of complimentary interventions should consider existing evidence, the clinician’s experience, and patient characteristics, preferences, and expectations of interventions. An evidence-based rationale considerate of biopsychosocial mechanisms should be provided, as well as clear indication that these treatments are adjunctive to exercise interventions [84–86]. These interventions can then be modified or progressed based on short-term response while emphasizing the exercise component of the load management program.
Exercise
Therapeutic exercise for AKP represents the most evidence-supported management strategy. Combined hip and knee exercise reduces short term and chronic pain while contributing to improved functional capacity in the medium to long term [81•]. Resistance exercises to strengthen the hip extensors, abductors and external rotators [87], quadriceps [88], and core musculature [89] are supported by a large body of evidence [90, 91, 92•]. More high-quality research to determine the most effective exercise parameters to address AKP is required, as evidence to guide the specifics of exercise prescription and dosage is lacking [93•].
Hip- Versus Knee-Targeted Exercises
Over the past two decades, our understanding of the role that the hip musculature has on patellofemoral joint loading and associated risk for AKP has advanced. Consequently, there has been an increased emphasis on addressing hip muscle impairments in patients with AKP. In particular, hip abductors, external rotators and extensors are frequent targets with the intent of reducing dynamic knee valgus and the accompanying increase in patellofemoral joint stress. Clinical trials have demonstrated a small advantage of hip-targeted exercise therapy over knee-targeted exercise therapy in improving pain and function in the short and medium term [87, 94]. However, therapy that combines both hip- and knee-targeted exercises revealed superior long-term outcomes compared to only knee-targeted exercise therapy [95]. As such, the combination of hip and knee-targeted exercise is the current recommendation from the Academy of Orthopaedic Physical Therapy [26••] and the National Athletic Trainers’ Association [96•].
Weight Bearing (Closed Kinetic Chain) Versus Non-weight Bearing (Open Kinetic Chain)
Due to the location and direction of the applied force, patellofemoral loads can differ between weight-bearing and non-weight-bearing exercises. Specifically, patellofemoral stress is lowest during weight-bearing exercise between 0° and 45° of knee flexion and during non-weight-bearing exercise between 45° and 90° [57]. This difference has led to the recommendation to limit the exercise range of motion during early AKP rehabilitation to that corresponding to reduced patellofemoral stress. Thus, a combination of partial range of motion weight-bearing (0° to 45°) and non-weight-bearing (45° to 90°) exercises is traditionally considered the safest approach. Despite this biomechanical rationale, weight-bearing and non-weight-bearing exercises are equally effective in reducing pain and improving function in the short, medium, and long term in those with AKP [97–99].
Squat and lunge exercises are common to AKP rehabilitation programs. Because patients may associate squatting or lunging with their pain, patient education and individual-specific modifications are advised to facilitate performance of these exercises without further escalation of fear-avoidance behavior. Biomechanical investigations inform potential modifications to the squatting program (Table 1) to stay within the boundaries of pain monitoring (i.e., < 3–5/10 pain; Fig. 1) and with consideration of the diagnosis. For example, to reduce pain during a bilateral squat in a patient with patellofemoral pain, range-of-motion can be limited or anterior knee translation reduced to mitigate patellofemoral joint forces. In a patient with patellofemoral or tibiofemoral osteoarthritis with significant crepitus during squatting, isometric muscle contractions performed in pain- and crepitus-free ranges during bilateral or unilateral tasks are a recommended alternative. In addition, isometric exercise may be used for pain modulation in individuals with patellar or quadriceps tendinopathy, with eventual progression to eccentric or concentric exercises. Another consistent modification appropriate across AKP conditions is mitigation of dynamic knee valgus which may result from a combination of contralateral pelvic drop, femoral internal rotation, knee valgus, tibial internal rotation, and foot pronation during weight-bearing or jumping activities [66]. Elastic resistance bands can be placed around the knees, ankles, or forefoot to facilitate greater thigh abduction and external rotation torque production in addition to foot supination and tibial external rotation during squat and lunge exercises (Fig. 2). Foot orthoses can be added as another means to reduce transverse plane knee rotation [100]. A mirror can be added for biofeedback to correct contralateral pelvic drop or rotation and frontal plane knee alignment during unilateral tasks.
Fig. 2.

Squat variations performed with an elastic band to promote movement patterns and muscle activation that will reduce dynamic knee valgus. Bands can be placed above or below the knees, at the ankles or the forefoot during bilateral or unilateral activities. An isometric hold in a target range can be performed to accommodate pain or crepitus and progressed to a unilateral task with contralateral limb abduction or extension using no, or band resistance. Often a mirror is used to provide biofeedback to assure neutral frontal plane foot, ankle, knee, and pelvis position
Neuromuscular Electrical Stimulation
The use of NMES is recommended to improve quadriceps muscle neuromuscular function post-knee surgery [101] and may provide symptom relief via nociceptive effects. Evidence for the use of NMES in direct treatment of AKP remains inconclusive [102], but patients with AKP and quadriceps dysfunction indicative of voluntary activation failure have strong potential to benefit from NMES [103].
Blood Flow Restriction Training
The use of blood flow restriction training (BFRT) has generated a lot of recent interest in both the clinical and research communities as a potential tool for maintaining a high metabolic load to the target muscle (through restriction of vascular flow) while reducing potentially problematic joint forces. Recent investigations have reported this technique as effective in restoring quadriceps muscle performance post-knee injury and surgery, when increased musculoskeletal loads may be counterproductive and/or harmful [104, 105]. BFRT of the knee extensors has also been shown to immediately and transiently reduce AKP [106, 107], which may facilitate more effective therapeutic exercise intervention. Improved quadriceps strength following a program of BFRT can also contribute to functional improvements in people with AKP [108]. Although the optimal parameters and dosage of BFRT for improving lower extremity muscular function in the presence of AKP, or in directly addressing AKP are unknown, current available evidence suggests this is a promising treatment approach for mitigating AKP symptoms while improving neuromuscular function. This is particularly relevant for populations with load restrictions, such as post-surgical patients [69•].
Movement Retraining
When movement faults are present and consistent with symptom presentation, movement retraining designed to reduce tissue loading to the knee should be considered a component of the plan of care. This is especially true when movement faults are present in the absence of lower extremity muscle weakness. A variety of techniques have been successfully applied to repetitive tasks such as walking, running, and jump landing resulting in improved biomechanics and reduced tissue loading. For example, in individuals who display excessive hip adduction or knee medial displacement during walking or running, movement retraining involving targeted visual feedback led to improved kinematics that were maintained over time [109–111]. Other retraining approaches have focused on reducing load during early stance phase of running where the primary forces associated with AKP occur. Increasing running step rate has been a particularly effective strategy to reduce the cumulative load on the knee [112, 113].
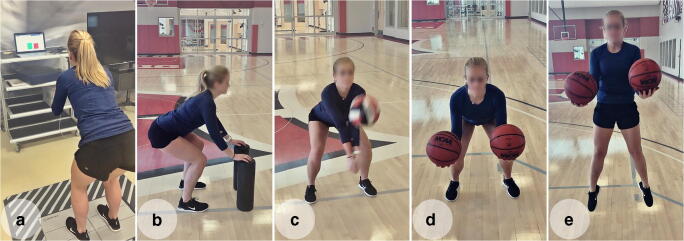
Safe and effective landing mechanics and lower extremity propulsive function are fundamental components in successful performance of sporting activities. Conversely, stiff landings with excessive frontal plane motion may contribute to AKP [114–116]. Retraining of lower extremity movement mechanics with an external focus of attention is recommended for improved retention and transfer of skills [117]. Neuromuscular training of loading and landing techniques with visual or video feedback and external focus is effective in improving lower extremity alignment and reducing landing stiffness [118–120], and may diminish patellofemoral joint forces [121]. Throughout training, a shift to reduced reliance on vision with increasing attentional demand is recommended to enhance retention and facilitate transfer to sport-specific tasks [122]. A progression of athletic movements, including jumping, bounding, and leaping actions with increasing task complexity, is recommended (Fig. 3). A sample progression would be (1) jumping and landing on two legs; (2) pushing off or landing on one leg; (3) reactionary movement with a visual component; and (4) reactionary movement with visual and sport-specific components (e.g., manipulating an object). These strategies serve to maximize effectiveness of biomechanical strategies to mitigate excessive tibiofemoral and patellofemoral joint forces that may contribute to AKP.
Fig. 3.
Retraining of movement strategies with feedback of performance, external focus of attention, and sport-specific training to enhance motor learning in performance of squatting and jumping. a Utilizing force plates for real-time feedback of performance to facilitate equal weight-bearing during a squatting motion. b Use of external focus of attention to facilitate appropriate squat depth and frontal plane knee alignment by instructing subject to align knees with cylinders and touch cylinders with hands. c Facilitating symmetric weight-bearing and appropriate squat depth with a volleyball pass. d, e Use of external focus of attention and dual-task conditions to facilitate appropriate stance width and frontal plane knee alignment during squatting and countermovement jumping
Conclusion
AKP is a common condition that is responsive to evidence-based physical therapy interventions focused on patient education, and restoring musculoskeletal load capacity through exercises supplemented by strategies to manage pain. Education is an important first step to ensure the patient understands the condition and the underlying rationale for the treatment plan. Exercise therapy is the foundation of AKP care and leads to long-term improvements in pain and function. Movement retraining should also be considered when faulty techniques are evident during activities that provoke pain.
Compliance with Ethical Standards
Conflict of Interest
Shane McClinton declares that he has no conflict of interest. Bryan Heiderscheit declares that he has no conflict of interest. Daniel Cobian declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Non-Operative Management of Anterior Knee Pain
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Shane M. McClinton, Email: shane.mcclinton@dmu.edu
Daniel G. Cobian, Email: cobian@ortho.wisc.edu
Bryan C. Heiderscheit, Email: heiderscheit@ortho.wisc.edu
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Coburn SL, Barton CJ, Filbay SR, Hart HF, Rathleff MS, Crossley KM. Quality of life in individuals with patellofemoral pain: a systematic review including meta-analysis. Phys Ther Sport. 2018;33:96–108. doi: 10.1016/j.ptsp.2018.06.006. [DOI] [PubMed] [Google Scholar]
- 2.Smith BE, Moffatt F, Hendrick P, Bateman M, Rathleff MS, Selfe J, Smith TO, Logan P. The experience of living with patellofemoral pain-loss, confusion and fear-avoidance: a UK qualitative study. BMJ Open. 2018;8(1):e018624. doi: 10.1136/bmjopen-2017-018624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kettunen JA, Harilainen A, Sandelin J, Schlenzka D, Hietaniemi K, Seitsalo S, Malmivaara A, Kujala UM. Knee arthroscopy and exercise versus exercise only for chronic patellofemoral pain syndrome: a randomized controlled trial. BMC Med. 2007;5:38. doi: 10.1186/1741-7015-5-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sisk D, Fredericson M. Update of risk factors, diagnosis, and management of patellofemoral pain. Curr Rev Musculoskelet Med. 2019;12(4):534–541. doi: 10.1007/s12178-019-09593-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Collins NJ, Bisset LM, Crossley KM, Vicenzino B. Efficacy of nonsurgical interventions for anterior knee pain: systematic review and meta-analysis of randomized trials. Sports Med. 2012;42(1):31–49. doi: 10.2165/11594460-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 6.Domenech J, Sanchis-Alfonso V, Lopez L, Espejo B. Influence of kinesiophobia and catastrophizing on pain and disability in anterior knee pain patients. Knee Surg Sports Traumatol Arthrosc. 2013;21(7):1562–1568. doi: 10.1007/s00167-012-2238-5. [DOI] [PubMed] [Google Scholar]
- 7.Maclachlan LR, Collins NJ, Matthews MLG, Hodges PW, Vicenzino B. The psychological features of patellofemoral pain: a systematic review. Br J Sports Med. 2017;51(9):732–742. doi: 10.1136/bjsports-2016-096705. [DOI] [PubMed] [Google Scholar]
- 8.Kettunen JA, Harilainen A, Sandelin J, Schlenzka D, Hietaniemi K, Seitsalo S, Malmivaara A, Kujala UM. Knee arthroscopy and exercise versus exercise only for chronic patellofemoral pain syndrome: 5-year follow-up. Br J Sports Med. 2012;46(4):243–246. doi: 10.1136/bjsm.2010.079020. [DOI] [PubMed] [Google Scholar]
- 9.Siemieniuk RAC, Harris IA, Agoritsas T, Poolman RW, Brignardello-Petersen R, Van de Velde S, et al. Arthroscopic surgery for degenerative knee arthritis and meniscal tears: a clinical practice guideline. BMJ. 2017;357:j1982. doi: 10.1136/bmj.j1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rousseau R, Labruyere C, Kajetanek C, Deschamps O, Makridis KG, Djian P. Complications after anterior cruciate ligament reconstruction and their relation to the type of graft: a prospective study of 958 cases. Am J Sports Med. 2019;47(11):2543–2549. doi: 10.1177/0363546519867913. [DOI] [PubMed] [Google Scholar]
- 11.Hajewski CJ, Baron JE, Glass NA, Duchman KR, Bollier M, Wolf BR, Westermann RW. Performance of the patient-reported outcome measurement information system in patients with patellofemoral instability. Orthop J Sports Med. 2020;8(4):2325967120915540. doi: 10.1177/2325967120915540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rathleff MS, Graven-Nielsen T, Hölmich P, Winiarski L, Krommes K, Holden S, Thorborg K. Activity modification and load management of adolescents with patellofemoral pain: a prospective intervention study including 151 adolescents. Am J Sports Med. 2019;47(7):1629–1637. doi: 10.1177/0363546519843915. [DOI] [PubMed] [Google Scholar]
- 13.Collins NJ, Tan JM, Menz HB, Russell TG, Smith AJ, Vicenzino B, Munteanu SE, Hinman RS, Haines TP, Hart HF, Patterson BE, Cleary G, Donnar JW, Maclachlan LR, Crossley KM. The FOOTPATH study: protocol for a multicentre, participant- and assessor-blind, parallel group randomised clinical trial of foot orthoses for patellofemoral osteoarthritis. BMJ Open. 2019;9(4):e025315. doi: 10.1136/bmjopen-2018-025315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Domenech J, Sanchis-Alfonso V, Espejo B. Changes in catastrophizing and kinesiophobia are predictive of changes in disability and pain after treatment in patients with anterior knee pain. Knee Surg Sports Traumatol Arthrosc. 2014;22(10):2295–2300. doi: 10.1007/s00167-014-2968-7. [DOI] [PubMed] [Google Scholar]
- 15.Mansfield CB, Selhorst M. The effects of fear-avoidance beliefs on anterior knee pain and physical therapy visit count for young individuals: a retrospective study. Phys Ther Sport. 2018;34:187–191. doi: 10.1016/j.ptsp.2018.10.008. [DOI] [PubMed] [Google Scholar]
- 16.Glaviano NR, Baellow A, Saliba S. Physical activity levels in individuals with and without patellofemoral pain. Phys Ther Sport. 2017;27:12–16. doi: 10.1016/j.ptsp.2017.07.002. [DOI] [PubMed] [Google Scholar]
- 17.Piva SR, Fitzgerald GK, Irrgang JJ, Fritz JM, Wisniewski S, McGinty GT, Childs JD, Domenech MA, Jones S, Delitto A. Associates of physical function and pain in patients with patellofemoral pain syndrome. Arch Phys Med Rehabil. 2009;90(2):285–295. doi: 10.1016/j.apmr.2008.08.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hiemstra LA, Kerslake S, Arendt EA. Clinical rehabilitation of anterior knee pain: current concepts. Am J Orthop (Belle Mead NJ) 2017;46(2):82–86. [PubMed] [Google Scholar]
- 19.Sanchis-Alfonso V, Dye SF. How to deal with anterior knee pain in the active young patient. Sports Health. 2017;9(4):346–351. doi: 10.1177/1941738116681269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Crossley KM, Stefanik JJ, Selfe J, Collins NJ, Davis IS, Powers CM, McConnell J, Vicenzino B, Bazett-Jones DM, Esculier JF, Morrissey D, Callaghan MJ. 2016 Patellofemoral pain consensus statement from the 4th International Patellofemoral Pain Research Retreat, Manchester. Part 1: Terminology, definitions, clinical examination, natural history, patellofemoral osteoarthritis and patient-reported outcome measures. Br J Sports Med. 2016;50(14):839–843. doi: 10.1136/bjsports-2016-096384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Powers CM, Witvrouw E, Davis IS, Crossley KM. Evidence-based framework for a pathomechanical model of patellofemoral pain: 2017 patellofemoral pain consensus statement from the 4th International Patellofemoral Pain Research Retreat, Manchester, UK: part 3. Br J Sports Med. 2017;51(24):1713–1723. doi: 10.1136/bjsports-2017-098717. [DOI] [PubMed] [Google Scholar]
- 22.Wheatley MGA, Rainbow MJ, Clouthier AL. Patellofemoral mechanics: a review of pathomechanics and research approaches. Curr Rev Musculoskelet Med. 2020;13:326–337. doi: 10.1007/s12178-020-09626-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cook C, Hegedus E, Hawkins R, Scovell F, Wyland D. Diagnostic accuracy and association to disability of clinical test findings associated with patellofemoral pain syndrome. Physiother Can. 2010;62(1):17–24. doi: 10.3138/physio.62.1.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cook CE, Hegedus EJ. Orthopedic physical examination tests: an evidence-based approach. Upper Saddle River, New Jersey: Pearson Prentice Hall; 2008. [Google Scholar]
- 25.Hollman JH, Ginos BE, Kozuchowski J, Vaughn AS, Krause DA, Youdas JW. Relationships between knee valgus, hip-muscle strength, and hip-muscle recruitment during a single-limb step-down. J Sport Rehabil. 2009;18(1):104–117. doi: 10.1123/jsr.18.1.104. [DOI] [PubMed] [Google Scholar]
- 26.Willy RW, Hoglund LT, Barton CJ, Bolgla LA, Scalzitti DA, Logerstedt DS, et al. Patellofemoral pain. J Orthop Sports Phys Ther. 2019;49(9):Cpg1–cpg95. doi: 10.2519/jospt.2019.0302. [DOI] [PubMed] [Google Scholar]
- 27.Lake DA, Wofford NH. Effect of therapeutic modalities on patients with patellofemoral pain syndrome: a systematic review. Sports Health. 2011;3(2):182–189. doi: 10.1177/1941738111398583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bily W, Trimmel L, Modlin M, Kaider A, Kern H. Training program and additional electric muscle stimulation for patellofemoral pain syndrome: a pilot study. Arch Phys Med Rehabil. 2008;89(7):1230–1236. doi: 10.1016/j.apmr.2007.10.048. [DOI] [PubMed] [Google Scholar]
- 29.Yu H, Randhawa K, Cote P, Optima C. The effectiveness of physical agents for lower-limb soft tissue injuries: a systematic review. J Orthop Sports Phys Ther. 2016;46(7):523–554. doi: 10.2519/jospt.2016.6521. [DOI] [PubMed] [Google Scholar]
- 30.Barton C, Balachandar V, Lack S, Morrissey D. Patellar taping for patellofemoral pain: a systematic review and meta-analysis to evaluate clinical outcomes and biomechanical mechanisms. Br J Sports Med. 2014;48(6):417–424. doi: 10.1136/bjsports-2013-092437. [DOI] [PubMed] [Google Scholar]
- 31.Leibbrandt DC, Louw QA. The use of McConnell taping to correct abnormal biomechanics and muscle activation patterns in subjects with anterior knee pain: a systematic review. J Phys Ther Sci. 2015;27(7):2395–2404. doi: 10.1589/jpts.27.2395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Logan CA, Bhashyam AR, Tisosky AJ, Haber DB, Jorgensen A, Roy A, Provencher MT. Systematic review of the effect of taping techniques on patellofemoral pain syndrome. Sports Health. 2017;9(5):456–461. doi: 10.1177/1941738117710938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ho KY, Epstein R, Garcia R, Riley N, Lee SP. Effects of patellofemoral taping on patellofemoral joint alignment and contact area during weight bearing. J Orthop Sports Phys Ther. 2017;47(2):115–123. doi: 10.2519/jospt.2017.6936. [DOI] [PubMed] [Google Scholar]
- 34.Smith TO, Drew BT, Meek TH, Clark AB. Knee orthoses for treating patellofemoral pain syndrome. Cochrane Database Syst Rev. 2015(12):Cd010513. 10.1002/14651858.CD010513.pub2. [DOI] [PMC free article] [PubMed]
- 35.Dursun N, Dursun E, Kiliç Z. Electromyographic biofeedback-controlled exercise versus conservative care for patellofemoral pain syndrome. Arch Phys Med Rehabil. 2001;82(12):1692–1695. doi: 10.1053/apmr.2001.26253. [DOI] [PubMed] [Google Scholar]
- 36.Chester R, Smith TO, Sweeting D, Dixon J, Wood S, Song F. The relative timing of VMO and VL in the aetiology of anterior knee pain: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2008;9:64. doi: 10.1186/1471-2474-9-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Briani RV, de Oliveira Silva D, Pazzinatto MF, Ferreira AS, Ferrari D, de Azevedo FM. Delayed onset of electromyographic activity of the vastus medialis relative to the vastus lateralis may be related to physical activity levels in females with patellofemoral pain. J Electromyogr Kinesiol. 2016;26:137–142. doi: 10.1016/j.jelekin.2015.10.012. [DOI] [PubMed] [Google Scholar]
- 38.Gabler CM, Lepley AS, Uhl TL, Mattacola CG. Comparison of transcutaneous electrical nerve stimulation and cryotherapy for increasing quadriceps activation in patients with knee pathologies. J Sport Rehabil. 2016;25(3):294–300. doi: 10.1123/jsr.2014-0292. [DOI] [PubMed] [Google Scholar]
- 39.Barton CJ, Lack S, Hemmings S, Tufail S, Morrissey D. The ‘best practice guide to conservative management of patellofemoral pain’: incorporating level 1 evidence with expert clinical reasoning. Br J Sports Med. 2015;49(14):923–934. doi: 10.1136/bjsports-2014-093637. [DOI] [PubMed] [Google Scholar]
- 40.Rathleff MS, Thomsen JL, Barton CJ. Patient education in patellofemoral pain: potentially potent and essential, but under-researched. Br J Sports Med. 2018;52(10):623–624. doi: 10.1136/bjsports-2017-098298. [DOI] [PubMed] [Google Scholar]
- 41.Smith BE, Moffatt F, Hendrick P, Bateman M, Selfe J, Rathleff MS, Smith TO, Logan P. Barriers and facilitators of loaded self-managed exercises and physical activity in people with patellofemoral pain: understanding the feasibility of delivering a multicentred randomised controlled trial, a UK qualitative study. BMJ Open. 2019;9(6):e023805. doi: 10.1136/bmjopen-2018-023805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.• de Oliveira Silva D, Pazzinatto MF, Rathleff MS, Holden S, Bell E, Azevedo F, et al. Patient education for patellofemoral pain: a systematic review. J Orthop Sports Phys Ther. 2020;1–36. 10.2519/jospt.2020.9400This systematic review identified 9 randomized controlled trials that investigated education intervention for patellofemoral pain. Trials were of low quality but suggested health professional–delivered education may produce similar improvements in pain and function outcomes as exercise therapy plus education. [DOI] [PubMed]
- 43.Louw A, Zimney K, Puentedura EJ, Diener I. The efficacy of pain neuroscience education on musculoskeletal pain: a systematic review of the literature. Physiother Theory Pract. 2016;32(5):332–355. doi: 10.1080/09593985.2016.1194646. [DOI] [PubMed] [Google Scholar]
- 44.Moseley GL, Baranoff J, Rio E, Stewart M, Derman W, Hainline B. Nonpharmacological management of persistent pain in elite athletes: rationale and recommendations. Clin J Sport Med. 2018;28(5):472–479. doi: 10.1097/JSM.0000000000000601. [DOI] [PubMed] [Google Scholar]
- 45.Esculier JF, Bouyer LJ, Dubois B, Fremont P, Moore L, McFadyen B, Roy JS. Is combining gait retraining or an exercise programme with education better than education alone in treating runners with patellofemoral pain? A randomised clinical trial. Br J Sports Med. 2018;52(10):659–666. doi: 10.1136/bjsports-2016-096988. [DOI] [PubMed] [Google Scholar]
- 46.Rathleff MS, Roos EM, Olesen JL, Rasmussen S. Exercise during school hours when added to patient education improves outcome for 2 years in adolescent patellofemoral pain: a cluster randomised trial. Br J Sports Med. 2015;49(6):406–412. doi: 10.1136/bjsports-2014-093929. [DOI] [PubMed] [Google Scholar]
- 47.Robertson CJ, Hurley M, Jones F. People’s beliefs about the meaning of crepitus in patellofemoral pain and the impact of these beliefs on their behaviour: A qualitative study. Musculoskelet Sci Pract. 2017;28:59–64. doi: 10.1016/j.msksp.2017.01.012. [DOI] [PubMed] [Google Scholar]
- 48.Schiphof D, van Middelkoop M, de Klerk BM, Oei EH, Hofman A, Koes BW, Weinans H, Bierma-Zeinstra SM. Crepitus is a first indication of patellofemoral osteoarthritis (and not of tibiofemoral osteoarthritis) Osteoarthr Cartil. 2014;22(5):631–638. doi: 10.1016/j.joca.2014.02.008. [DOI] [PubMed] [Google Scholar]
- 49.Dye SF. The pathophysiology of patellofemoral pain: a tissue homeostasis perspective. Clin Orthop Relat Res. 2005;436:100–110. doi: 10.1097/01.blo.0000172303.74414.7d. [DOI] [PubMed] [Google Scholar]
- 50.Stefanik JJ, Neogi T, Niu J, Roemer FW, Segal NA, Lewis CE, Nevitt M, Guermazi A, Felson DT. The diagnostic performance of anterior knee pain and activity-related pain in identifying knees with structural damage in the patellofemoral joint: the Multicenter Osteoarthritis Study. J Rheumatol. 2014;41(8):1695–1702. doi: 10.3899/jrheum.131555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rio E, Kidgell D, Moseley GL, Cook J. Elevated corticospinal excitability in patellar tendinopathy compared with other anterior knee pain or no pain. Scand J Med Sci Sports. 2016;26(9):1072–1079. doi: 10.1111/sms.12538. [DOI] [PubMed] [Google Scholar]
- 52.Pazzinatto MF, de Oliveira SD, Azevedo FM, Pappas E. Knee crepitus is not associated with the occurrence of total knee replacement in knee osteoarthritis - a longitudinal study with data from the Osteoarthritis Initiative. Braz J Phys Ther. 2019;23(4):329–336. doi: 10.1016/j.bjpt.2018.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.de Oliveira Silva D, Pazzinatto MF, Priore LBD, Ferreira AS, Briani RV, Ferrari D, et al. Knee crepitus is prevalent in women with patellofemoral pain, but is not related with function, physical activity and pain. Phys Ther Sport. 2018;33:7–11. doi: 10.1016/j.ptsp.2018.06.002. [DOI] [PubMed] [Google Scholar]
- 54.Besier TF, Draper CE, Gold GE, Beaupre GS, Delp SL. Patellofemoral joint contact area increases with knee flexion and weight-bearing. J Orthop Res. 2005;23(2):345–350. doi: 10.1016/j.orthres.2004.08.003. [DOI] [PubMed] [Google Scholar]
- 55.Escamilla RF, Zheng N, MacLeod TD, Edwards WB, Hreljac A, Fleisig GS, et al. Patellofemoral compressive force and stress during the forward and side lunges with and without a stride. Clin Biomech (Bristol, Avon) 2008;23(8):1026–1037. doi: 10.1016/j.clinbiomech.2008.05.002. [DOI] [PubMed] [Google Scholar]
- 56.Escamilla RF, Zheng N, Macleod TD, Brent Edwards W, Imamura R, Hreljac A, et al. Patellofemoral joint force and stress during the wall squat and one-leg squat. Med Sci Sports Exerc. 2009;41(4):879–888. doi: 10.1249/MSS.0b013e31818e7ead. [DOI] [PubMed] [Google Scholar]
- 57.Powers CM, Ho KY, Chen YJ, Souza RB, Farrokhi S. Patellofemoral joint stress during weight-bearing and non-weight-bearing quadriceps exercises. J Orthop Sports Phys Ther. 2014;44(5):320–327. doi: 10.2519/jospt.2014.4936. [DOI] [PubMed] [Google Scholar]
- 58.Salsich GB, Perman WH. Tibiofemoral and patellofemoral mechanics are altered at small knee flexion angles in people with patellofemoral pain. J Sci Med Sport. 2013;16(1):13–17. doi: 10.1016/j.jsams.2012.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Escamilla RF, Fleisig GS, Zheng N, Lander JE, Barrentine SW, Andrews JR, et al. Effects of technique variations on knee biomechanics during the squat and leg press. Med Sci Sports Exerc. 2001;33(9):1552–1566. doi: 10.1097/00005768-200109000-00020. [DOI] [PubMed] [Google Scholar]
- 60.Frohm A, Halvorsen K, Thorstensson A. Patellar tendon load in different types of eccentric squats. Clin Biomech (Bristol, Avon) 2007;22(6):704–711. doi: 10.1016/j.clinbiomech.2006.12.006. [DOI] [PubMed] [Google Scholar]
- 61.Fry AC, Smith JC, Schilling BK. Effect of knee position on hip and knee torques during the barbell squat. J Strength Cond Res. 2003;17(4):629–633. doi: 10.1519/1533-4287(2003)017<0629:eokpoh>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 62.Escamilla RF, Zheng N, Macleod TD, Edwards WB, Hreljac A, Fleisig GS, et al. Patellofemoral joint force and stress between a short- and long-step forward lunge. J Orthop Sports Phys Ther. 2008;38(11):681–690. doi: 10.2519/jospt.2008.2694. [DOI] [PubMed] [Google Scholar]
- 63.Zellmer M, Kernozek TW, Gheidi N, Hove J, Torry M. Patellar tendon stress between two variations of the forward step lunge. J Sport Health Sci. 2019;8(3):235–241. doi: 10.1016/j.jshs.2016.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Liao TC, Yin L, Powers CM. The influence of isolated femur and tibia rotations on patella cartilage stress: a sensitivity analysis. Clin Biomech (Bristol, Avon) 2018;54:125–131. doi: 10.1016/j.clinbiomech.2018.03.003. [DOI] [PubMed] [Google Scholar]
- 65.Salsich GB, Perman WH. Patellofemoral joint contact area is influenced by tibiofemoral rotation alignment in individuals who have patellofemoral pain. J Orthop Sports Phys Ther. 2007;37(9):521–528. doi: 10.2519/jospt.2007.37.9.521. [DOI] [PubMed] [Google Scholar]
- 66.Powers CM. The influence of altered lower-extremity kinematics on patellofemoral joint dysfunction: a theoretical perspective. J Orthop Sports Phys Ther. 2003;33(11):639–646. doi: 10.2519/jospt.2003.33.11.639. [DOI] [PubMed] [Google Scholar]
- 67.Escamilla RF. Knee biomechanics of the dynamic squat exercise. Med Sci Sports Exerc. 2001;33(1):127–141. doi: 10.1097/00005768-200101000-00020. [DOI] [PubMed] [Google Scholar]
- 68.Rio E, Kidgell D, Purdam C, Gaida J, Moseley GL, Pearce AJ, Cook J. Isometric exercise induces analgesia and reduces inhibition in patellar tendinopathy. Br J Sports Med. 2015;49(19):1277–1283. doi: 10.1136/bjsports-2014-094386. [DOI] [PubMed] [Google Scholar]
- 69.Barber-Westin S, Noyes FR. Blood flow-restricted training for lower extremity muscle weakness due to knee pathology: a systematic review. Sports Health. 2019;11(1):69–83. doi: 10.1177/1941738118811337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hughes L, Paton B, Rosenblatt B, Gissane C, Patterson SD. Blood flow restriction training in clinical musculoskeletal rehabilitation: a systematic review and meta-analysis. Br J Sports Med. 2017;51(13):1003–1011. doi: 10.1136/bjsports-2016-097071. [DOI] [PubMed] [Google Scholar]
- 71.Lo GH, Musa SM, Driban JB, Kriska AM, McAlindon TE, Souza RB, Petersen NJ, Storti KL, Eaton CB, Hochberg MC, Jackson RD, Kwoh CK, Nevitt MC, Suarez-Almazor ME. Running does not increase symptoms or structural progression in people with knee osteoarthritis: data from the osteoarthritis initiative. Clin Rheumatol. 2018;37(9):2497–2504. doi: 10.1007/s10067-018-4121-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Chakravarty EF, Hubert HB, Lingala VB, Fries JF. Reduced disability and mortality among aging runners: a 21-year longitudinal study. Arch Intern Med. 2008;168(15):1638–1646. doi: 10.1001/archinte.168.15.1638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Heinemeier KM, Schjerling P, Heinemeier J, Moller MB, Krogsgaard MR, Grum-Schwensen T, et al. Radiocarbon dating reveals minimal collagen turnover in both healthy and osteoarthritic human cartilage. Sci Transl Med. 2016;8(346):346ra90. doi: 10.1126/scitranslmed.aad8335. [DOI] [PubMed] [Google Scholar]
- 74.Jones G, Ding C, Glisson M, Hynes K, Ma D, Cicuttini F. Knee articular cartilage development in children: a longitudinal study of the effect of sex, growth, body composition, and physical activity. Pediatr Res. 2003;54(2):230–236. doi: 10.1203/01.PDR.0000072781.93856.E6. [DOI] [PubMed] [Google Scholar]
- 75.Jorgensen AEM, Kjaer M, Heinemeier KM. The effect of aging and mechanical loading on the metabolism of articular cartilage. J Rheumatol. 2017;44(4):410–417. doi: 10.3899/jrheum.160226. [DOI] [PubMed] [Google Scholar]
- 76.Miller RH. Joint loading in runners does not initiate knee osteoarthritis. Exerc Sport Sci Rev. 2017;45(2):87–95. doi: 10.1249/JES.0000000000000105. [DOI] [PubMed] [Google Scholar]
- 77.Malliaras P, Cook J, Purdam C, Rio E. Patellar tendinopathy: clinical diagnosis, load management, and advice for challenging case presentations. J Orthop Sports Phys Ther. 2015;45(11):887–898. doi: 10.2519/jospt.2015.5987. [DOI] [PubMed] [Google Scholar]
- 78.Thomee R. A comprehensive treatment approach for patellofemoral pain syndrome in young women. Phys Ther. 1997;77(12):1690–1703. doi: 10.1093/ptj/77.12.1690. [DOI] [PubMed] [Google Scholar]
- 79.Jayaseelan DJ, Scalzitti DA, Palmer G, Immerman A, Courtney CA. The effects of joint mobilization on individuals with patellofemoral pain: a systematic review. Clin Rehabil. 2018;32(6):722–733. doi: 10.1177/0269215517753971. [DOI] [PubMed] [Google Scholar]
- 80.Eckenrode BJ, Kietrys DM, Parrott JS. Effectiveness of manual therapy for pain and self-reported function in individuals with patellofemoral pain: systematic review and meta-analysis. J Orthop Sports Phys Ther. 2018;48(5):358–371. doi: 10.2519/jospt.2018.7243. [DOI] [PubMed] [Google Scholar]
- 81.Collins NJ, Barton CJ, van Middelkoop M, Callaghan MJ, Rathleff MS, Vicenzino BT, et al. 2018 Consensus statement on exercise therapy and physical interventions (orthoses, taping and manual therapy) to treat patellofemoral pain: recommendations from the 5th International Patellofemoral Pain Research Retreat, Gold Coast, Australia, 2017. Br J Sports Med. 2018;52(18):1170–1178. doi: 10.1136/bjsports-2018-099397. [DOI] [PubMed] [Google Scholar]
- 82.Brantingham JW, Bonnefin D, Perle SM, Cassa TK, Globe G, Pribicevic M, Hicks M, Korporaal C. Manipulative therapy for lower extremity conditions: update of a literature review. J Manip Physiol Ther. 2012;35(2):127–166. doi: 10.1016/j.jmpt.2012.01.001. [DOI] [PubMed] [Google Scholar]
- 83.• Rahou-El-Bachiri Y, Navarro-Santana MJ, Gomez-Chiguano GF, Cleland JA, Villanueva IL, Fernandez-de-Las-Penas C, et al. Effects of trigger point dry needling for the management of knee pain syndromes: a systematic review and meta-analysis. J Clin Med. 2020;9(7). 10.3390/jcm9072044This systematic review and meta-analysis identified 6 randomized controlled trials that investigated the effects of trigger point dry needling in persons with anterior knee pain. A moderate short-term improvement in pain and disability was found in persons with patellofemoral pain when trigger point dry needling was performed; and, in 5 out of 6 trials, dry needling was performed in conjunction with manual therapy or exercise interventions. [DOI] [PMC free article] [PubMed]
- 84.Bialosky JE, Bishop MD, Price DD, Robinson ME, George SZ. The mechanisms of manual therapy in the treatment of musculoskeletal pain: a comprehensive model. Man Ther. 2009;14(5):531–538. doi: 10.1016/j.math.2008.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Bialosky JE, Beneciuk JM, Bishop MD, Coronado RA, Penza CW, Simon CB, George SZ. Unraveling the mechanisms of manual therapy: modeling an approach. J Orthop Sports Phys Ther. 2018;48(1):8–18. doi: 10.2519/jospt.2018.7476. [DOI] [PubMed] [Google Scholar]
- 86.Testa M, Rossettini G. Enhance placebo, avoid nocebo: how contextual factors affect physiotherapy outcomes. Man Ther. 2016;24:65–74. doi: 10.1016/j.math.2016.04.006. [DOI] [PubMed] [Google Scholar]
- 87.Lack S, Barton C, Sohan O, Crossley K, Morrissey D. Proximal muscle rehabilitation is effective for patellofemoral pain: a systematic review with meta-analysis. Br J Sports Med. 2015;49(21):1365–1376. doi: 10.1136/bjsports-2015-094723. [DOI] [PubMed] [Google Scholar]
- 88.Kooiker L, Van De Port IG, Weir A, Moen MH. Effects of physical therapist-guided quadriceps-strengthening exercises for the treatment of patellofemoral pain syndrome: a systematic review. J Orthop Sports Phys Ther. 2014;44(6):391–402. doi: 10.2519/jospt.2014.4127. [DOI] [PubMed] [Google Scholar]
- 89.Ferber R, Bolgla L, Earl-Boehm JE, Emery C, Hamstra-Wright K. Strengthening of the hip and core versus knee muscles for the treatment of patellofemoral pain: a multicenter randomized controlled trial. J Athl Train. 2015;50(4):366–377. doi: 10.4085/1062-6050-49.3.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Alba-Martin P, Gallego-Izquierdo T, Plaza-Manzano G, Romero-Franco N, Nunez-Nagy S, Pecos-Martin D. Effectiveness of therapeutic physical exercise in the treatment of patellofemoral pain syndrome: a systematic review. J Phys Ther Sci. 2015;27(7):2387–2390. doi: 10.1589/jpts.27.2387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Clijsen R, Fuchs J, Taeymans J. Effectiveness of exercise therapy in treatment of patients with patellofemoral pain syndrome: systematic review and meta-analysis. Phys Ther. 2014;94(12):1697–1708. doi: 10.2522/ptj.20130310. [DOI] [PubMed] [Google Scholar]
- 92.Nascimento LR, Teixeira-Salmela LF, Souza RB, Resende RA. Hip and knee strengthening is more effective than knee strengthening alone for reducing pain and improving activity in individuals with patellofemoral pain: a systematic review with meta-analysis. J Orthop Sports Phys Ther. 2018;48(1):19–31. doi: 10.2519/jospt.2018.7365. [DOI] [PubMed] [Google Scholar]
- 93.Holden S, Rathleff MS, Jensen MB, Barton CJ. How can we implement exercise therapy for patellofemoral pain if we don't know what was prescribed? A systematic review. Br J Sports Med. 2018;52(6):385. doi: 10.1136/bjsports-2017-097547. [DOI] [PubMed] [Google Scholar]
- 94.van der Heijden RA, Lankhorst NE, van Linschoten R, Bierma-Zeinstra SM, van Middelkoop M. Exercise for treating patellofemoral pain syndrome. Cochrane Database Syst Rev. 2015;1:Cd010387. doi: 10.1002/14651858.CD010387.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Fukuda TY, Melo WP, Zaffalon BM, Rossetto FM, Magalhães E, Bryk FF, Martin RL. Hip posterolateral musculature strengthening in sedentary women with patellofemoral pain syndrome: a randomized controlled clinical trial with 1-year follow-up. J Orthop Sports Phys Ther. 2012;42(10):823–830. doi: 10.2519/jospt.2012.4184. [DOI] [PubMed] [Google Scholar]
- 96.Bolgla LA, Boling MC, Mace KL, DiStefano MJ, Fithian DC, Powers CM. National Athletic Trainers' Association Position Statement: management of individuals with patellofemoral pain. J Athl Train. 2018;53(9):820–836. doi: 10.4085/1062-6050-231-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Witvrouw E, Werner S, Mikkelsen C, Van Tiggelen D, Vanden Berghe L, Cerulli G. Clinical classification of patellofemoral pain syndrome: guidelines for non-operative treatment. Knee Surg Sports Traumatol Arthrosc. 2005;13(2):122–130. doi: 10.1007/s00167-004-0577-6. [DOI] [PubMed] [Google Scholar]
- 98.Bakhtiary AH, Fatemi E. Open versus closed kinetic chain exercises for patellar chondromalacia. Br J Sports Med. 2008;42(2):99–102. doi: 10.1136/bjsm.2007.038109. [DOI] [PubMed] [Google Scholar]
- 99.Herrington L, Al-Sherhi A. A controlled trial of weight-bearing versus non-weight-bearing exercises for patellofemoral pain. J Orthop Sports Phys Ther. 2007;37(4):155–160. doi: 10.2519/jospt.2007.2433. [DOI] [PubMed] [Google Scholar]
- 100.Barton CJ, Menz HB, Crossley KM. Effects of prefabricated foot orthoses on pain and function in individuals with patellofemoral pain syndrome: a cohort study. Phys Ther Sport. 2010;12(2):70–75. doi: 10.1016/j.ptsp.2010.09.002. [DOI] [PubMed] [Google Scholar]
- 101.Spector P, Laufer Y, Elboim Gabyzon M, Kittelson A, Stevens Lapsley J, Maffiuletti NA. Neuromuscular electrical stimulation therapy to restore quadriceps muscle function in patients after orthopaedic surgery: a novel structured approach. J Bone Joint Surg Am. 2016;98(23):2017–2024. doi: 10.2106/JBJS.16.00192. [DOI] [PubMed] [Google Scholar]
- 102.Martimbianco ALC, Torloni MR, Andriolo BN, Porfirio GJ, Riera R. Neuromuscular electrical stimulation (NMES) for patellofemoral pain syndrome. Cochrane Database Syst Rev. 2017;12:CD011289. doi: 10.1002/14651858.CD011289.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Maffiuletti NA, Gondin J, Place N, Stevens-Lapsley J, Vivodtzev I, Minetto MA. Clinical use of neuromuscular electrical stimulation for neuromuscular rehabilitation: what are we overlooking? Arch Phys Med Rehabil. 2018;99(4):806–812. doi: 10.1016/j.apmr.2017.10.028. [DOI] [PubMed] [Google Scholar]
- 104.Hughes L, Rosenblatt B, Haddad F, Gissane C, McCarthy D, Clarke T, Ferris G, Dawes J, Paton B, Patterson SD. Comparing the effectiveness of blood flow restriction and traditional heavy load resistance training in the post-surgery rehabilitation of anterior cruciate ligament reconstruction patients: a UK National Health Service Randomised Controlled Trial. Sports Med. 2019;49(11):1787–1805. doi: 10.1007/s40279-019-01137-2. [DOI] [PubMed] [Google Scholar]
- 105.Kilgas MA, Lytle LLM, Drum SN, Elmer SJ. Exercise with blood flow restriction to improve quadriceps function long after ACL reconstruction. Int J Sports Med. 2019;40(10):650–656. doi: 10.1055/a-0961-1434. [DOI] [PubMed] [Google Scholar]
- 106.Korakakis V, Whiteley R, Epameinontidis K. Blood flow restriction induces hypoalgesia in recreationally active adult male anterior knee pain patients allowing therapeutic exercise loading. Phys Ther Sport. 2018;32:235–243. doi: 10.1016/j.ptsp.2018.05.021. [DOI] [PubMed] [Google Scholar]
- 107.Korakakis V, Whiteley R, Giakas G. Low load resistance training with blood flow restriction decreases anterior knee pain more than resistance training alone. A pilot randomised controlled trial. Phys Ther Sport. 2018;34:121–128. doi: 10.1016/j.ptsp.2018.09.007. [DOI] [PubMed] [Google Scholar]
- 108.Giles L, Webster KE, McClelland J, Cook JL. Quadriceps strengthening with and without blood flow restriction in the treatment of patellofemoral pain: a double-blind randomised trial. Br J Sports Med. 2017;51(23):1688–1694. doi: 10.1136/bjsports-2016-096329. [DOI] [PubMed] [Google Scholar]
- 109.Noehren B, Scholz J, Davis I. The effect of real-time gait retraining on hip kinematics, pain and function in subjects with patellofemoral pain syndrome. Br J Sports Med. 2011;45(9):691–696. doi: 10.1136/bjsm.2009.069112. [DOI] [PubMed] [Google Scholar]
- 110.Willy RW, Scholz JP, Davis IS. Mirror gait retraining for the treatment of patellofemoral pain in female runners. Clin Biomech (Bristol, Avon) 2012;27(10):1045–1051. doi: 10.1016/j.clinbiomech.2012.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Barrios JA, Crossley KM, Davis IS. Gait retraining to reduce the knee adduction moment through real-time visual feedback of dynamic knee alignment. J Biomech. 2010;43(11):2208–2213. doi: 10.1016/j.jbiomech.2010.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Heiderscheit BC, Chumanov ES, Michalski MP, Wille CM, Ryan MB. Effects of step rate manipulation on joint mechanics during running. Med Sci Sports Exerc. 2011;43(2):296–302. doi: 10.1249/MSS.0b013e3181ebedf4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Willson JD, Ratcliff OM, Meardon SA, Willy RW. Influence of step length and landing pattern on patellofemoral joint kinetics during running. Scand J Med Sci Sports. 2015. 10.1111/sms.12383. [DOI] [PubMed]
- 114.Nunes GS, Barton CJ, Viadanna Serrao F. Females with patellofemoral pain have impaired impact absorption during a single-legged drop vertical jump. Gait Posture. 2019;68:346–351. doi: 10.1016/j.gaitpost.2018.12.013. [DOI] [PubMed] [Google Scholar]
- 115.De Bleecker C, Vermeulen S, De Blaiser C, Willems T, De Ridder R, Roosen P. Relationship between jump-landing kinematics and lower extremity overuse injuries in physically active populations: a systematic review and meta-analysis. Sports Med. 2020;50:1515–1532. doi: 10.1007/s40279-020-01296-7. [DOI] [PubMed] [Google Scholar]
- 116.Tamura A, Akasaka K, Otsudo T, Shiozawa J, Toda Y, Yamada K. Dynamic knee valgus alignment influences impact attenuation in the lower extremity during the deceleration phase of a single-leg landing. PLoS One. 2017;12(6):e0179810. doi: 10.1371/journal.pone.0179810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Benjaminse A, Gokeler A, Dowling AV, Faigenbaum A, Ford KR, Hewett TE, Onate JA, Otten B, Myer GD. Optimization of the anterior cruciate ligament injury prevention paradigm: novel feedback techniques to enhance motor learning and reduce injury risk. J Orthop Sports Phys Ther. 2015;45(3):170–182. doi: 10.2519/jospt.2015.4986. [DOI] [PubMed] [Google Scholar]
- 118.Benjaminse A, Welling W, Otten B, Gokeler A. Transfer of improved movement technique after receiving verbal external focus and video instruction. Knee Surg Sports Traumatol Arthrosc. 2018;26(3):955–962. doi: 10.1007/s00167-017-4671-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Hartigan E, Col Eman K, Brooks J, Frisbee A, Lawrence M, Hawke K, et al. Self-assessment during jump shot drills translates to decreased vertical ground reaction forces during single limb drop jump landing. Int J Sports Phys Ther. 2019;14(3):403–414. doi: 10.26603/ijspt20190403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Marshall AN, Hertel J, Hart JM, Russell S, Saliba SA. Visual biofeedback and changes in lower extremity kinematics in individuals with medial knee displacement. J Athl Train. 2020;55(3):255–264. doi: 10.4085/1062-6050-383-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Kernozek T, Schiller M, Rutherford D, Smith A, Durall C, Almonroeder TG. Real-time visual feedback reduces patellofemoral joint forces during squatting in individuals with patellofemoral pain. Clin Biomech (Bristol, Avon) 2020;77:105050. doi: 10.1016/j.clinbiomech.2020.105050. [DOI] [PubMed] [Google Scholar]
- 122.Grooms DR, Kiefer AW, Riley MA, Ellis JD, Thomas S, Kitchen K, DiCesare C, Bonnette S, Gadd B, Barber Foss KD, Yuan W, Silva P, Galloway R, Diekfuss JA, Leach J, Berz K, Myer GD. Brain-behavior mechanisms for the transfer of neuromuscular training adaptions to simulated sport: initial findings from the Train the Brain Project. J Sport Rehabil. 2018;27(5):1–5. doi: 10.1123/jsr.2017-0241. [DOI] [PMC free article] [PubMed] [Google Scholar]