Abstract
Emergency management of the emerging infectious disease outbreak is critical for public health threats. Currently, control of the COVID-19 outbreak is an international concern and has become a crucial challenge in many countries. This article reviews significant information technologyIT) applications in emergency management of COVID-19 by considering the prevention/mitigation, preparedness, response, and recovery phases of the crisis. This review was conducted using MEDLINE PubMed), Embase, IEEE, and Google Scholar. Expert opinions were collected to show existence gaps, useful technologies for each phase of emergency management, and future direction. Results indicated that various IT-based systems such as surveillance systems, artificial intelligence, computational methods, Internet of things, remote sensing sensor, online service, and GIS geographic information system) could have different outbreak management applications, especially in response phases. Information technology was applied in several aspects, such as increasing the accuracy of diagnosis, early detection, ensuring healthcare providers’ safety, decreasing workload, saving time and cost, and drug discovery. We categorized these applications into four core topics, including diagnosis and prediction, treatment, protection, and management goals, which were confirmed by five experts. Without applying IT, the control and management of the crisis could be difficult on a large scale. For reducing and improving the hazard effect of disaster situations, the role of IT is inevitable. In addition to the response phase, communities should be considered to use IT capabilities in prevention, preparedness, and recovery phases. It is expected that IT will have an influential role in the recovery phase of COVID-19. Providing IT infrastructure and financial support by the governments should be more considered in facilitating IT capabilities.
Keywords: Outbreak, COVID-19, Emergency management, Information technology, Disaster, Epidemic
1. Introduction
Many disasters can be categorized into natural and human-made groups, and for dealing with them, collaboration, leadership, and management have a foundational role [1,2]. According to the literature, a crisis could be divided into four phases: prevention/mitigation, preparedness, response, and recovery, which refer to diminishing or eliminating the probability of disaster, preparing to handle, immediate reaction to safety, and return to normal situations. Therefore emergency management requires more consideration to control and manage the disaster [1,[3], [4], [5]]. Emergency management of health-related events can be achieved by considering the different aspects of knowledge, behavior, health care system, and public health system. Moreover, the operation and configuration of the emergency management systems should be considered [6].
When the community encounters infection outbreaks, it means the growth rate of illness becomes excess rather than of average expectancy [7]. In the 21st century emerging and re-emerging infectious disease outbreaks are rapidly increasing significantly in developing countries with devastating health, economic, and social consequences [8]. In recent years, viral outbreaks such as Pandemic Influenza A H1N1), Avian influenza A H7N9), Middle East respiratory syndrome MERS), and severe acute respiratory syndrome SARS), were epidemic [[9], [10], [11], [12]]. Emergency management of infectious disease outbreaks is essential because they can negatively impact public health, travel, and economics [13]. Hence, numerous factors, such as the number of cases, risk factors, intensity, outcomes, and transmission speed, are required to manage infectious disease epidemics [14].
Recently, COVID-19 as an emerging virus has become a major international public health disaster because, in a short period, the number of cases increased significantly at first in China and then in several countries around the world [15]. COVID-19 occurs at a severity level of slight to imminent. The COVID-19 can transmit indirectly by contamination of objects, asymptomatic cases, and aerosolization. However, it can also transmit directly through symptomatic patients [16,17]. Fever, cough, myalgia or fatigue, chest tightness, shortness of breath, expectoration, and dyspnea were reported as significant symptoms of COVID-19. There can be severe complications, including pneumonia, severe acute respiratory distress syndrome, and death [18,19]. There is a need to conduct a quickly targeted action and risk assessment, particularly at healthcare and social institutions with a high risk of transmission [20]. Using educational tools, health recommendations, infection control approaches, and infection prevention strategies could enhance healthcare providers’ safety protection [[21], [22], [23]]. Regarding the negative impact of COVID-19 on society, economy, and global value chains, the control of the virus in the early-stage has a critical role in preventing and managing the further outbreak [24,25].
The control of each phase of the crisis can be reached or facilitated using information technology IT). IT has become popular to use in public health surveillance. Evidence indicates that IT could be a useful approach in each phase of the disaster, particularly in the response phase [4,[26], [27], [28], [29]]. IT was used as a beneficial approach to increase the speed of diagnosis, improving epidemic management, save lives, and reduced the economic impact of outbreaks [30]. For example, surveillance cameras, drone-borne cameras, and portable digital recorders can monitor crowd gathering in public areas and are useful in monitoring diseases [31]. Many of these tools and techniques support emergency conditions and offer learning opportunities for providing healthcare in similar situations. For example, virtual reality-based training as a novel technology can be used to prepare and respond to different outbreaks [32]. Moreover, recent IT-based technologies e.g. digital communication technologies, data science, crisis informatics, bioinformatics, and computational modeling) provide new opportunities to reduce pandemics risk and response to international pandemics [[33], [34], [35]].
There are several reports and studies about the utilization of IT capabilities during the COVID-19 outbreak. The studies have used IT for different aims such as accurate diagnosis, statistical reporting, monitoring and controlling disease, forecasting, etc. [[36], [37], [38], [39]]. Besides, technology startups are working with government agencies, clinicians, and academics to prevent/control the outbreak [40]. Therefore, according to IT's various advantages in the COVID-19 pandemic, presenting an overview of IT applications can help software designers, healthcare providers, researchers, policymakers, and governments obtain information and ideas in the management and control of the COVID-19 outbreak. In this regard, in this study, applications of IT in the emergency management of the COVID-19 are reviewed. However, the current study's focus is on phases of emergency management. Moreover, a taxonomy of IT capabilities for response in COVID-19 was presented. Finally, expert opinions were collected to show the gaps, beneficial technologies, and future directions for each phase of the emergency management of COVID-19.
2. Methods
This review was conducted to identify IT applications in emergency management of the COVID-19 outbreak. The search was carried out in MEDLINE PubMed), Embase, IEEE, Google Scholar, and Google search engine up to July 2020. The searching keywords were selected by consulting with experts in the related fields, including medical informatics, health information technology, and librarian science experts. The recruited keywords in this study were as follows: information system, informatic*, decision support system, decision management system, dashboard, sensor, technology, information technology, Internet of things IoT), telehealth, telehealth, telemedicine, Electronic health, eHealth, e-health, surveillance system, artificial intelligence, AI, management system, mobile, mobile application, mobile health, portal, web, social network, health information technology, telemonitoring, geographic information system, GIS, virtual reality, Google trend, covid 19, 2019 ncov, coronavirus, novel coronavirus, coronavirus 2019, sars cov 2, coronavirus disease 2019, "Severe acute respiratory syndrome coronavirus 2".
All papers were included if they used each type of information technology for emergency management of the COVID-19 outbreak. Five authors carried out study selection and data extraction. Disagreed items were discussed and resolved in the online group. After information gathering, a taxonomy was presented for checking the contents of findings. The classification and results were sent to five experts with Ph.D. degrees and related experience to validate the taxonomy. Finally, an unstructured interview was conducted through eight experts, including health information technology N = 2), medical informatics N = 3), and IT experts N = 3), to determine useful tools for each phase of emergency management and future direction.
3. Results
3.1. Taxonomy of IT application in the response phase
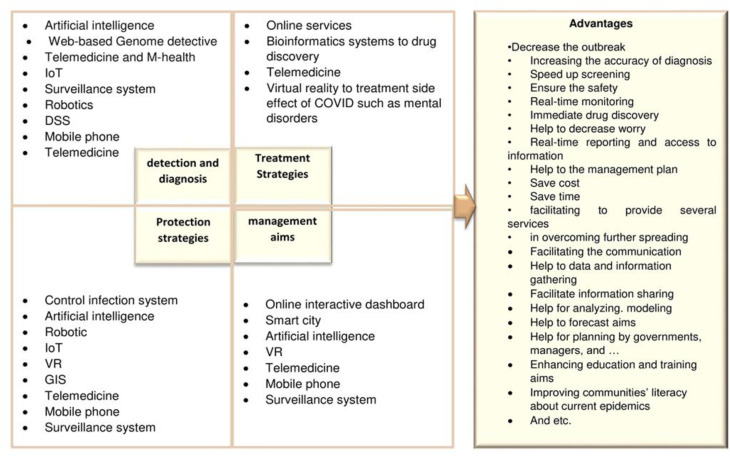
In this review, applications of IT for the response to the COVID-19 outbreak were classified and summarized to the following core topics: 1) detection and diagnosis, 2) treatment approach, 3) protection strategies and, 4) management aims. Fig. 1 . Shows these topics and involved technologies.
Fig. 1.
Overview of IT application for COVID-19 outbreak.
3.2. IT applications for COVID-19
Based on this review's findings, there were no efforts for the pre-crisis phases of emergency management, including mitigation/prevention and preparedness. In contrast, many advantages of IT were studied and reported in the response phase. However, after the COVID-19 outbreak, studies for the recovery phase should be completed. Table 1 shows the IT applications in the response phase of the COVID-19 epidemic.
Table 1.
Information technology based approaches employed in the response phase of the COVID-19 management.
| IT types | Applications according to literature | Example | References |
|---|---|---|---|
| Bioinformatics systems | ✓Help to Drug discovery by various methods such as: •To identify existence therapeutic agents •Rapid detection of COVID-19 •classifying and tracing the genomic sequence of COVID-19 •the discovery of COVID-19 antiviral and potential protein targets ✓Help to diagnosis |
*In Italy, virtual screening of FDA approved databases indicated some of the HIV protease inhibitors might be useful in COVID-19 treatment * chemical-informatics approach by integrating different ligand-based drug design strategies of some in-house chemicals was developed to help in the process of drug discovery in India * Modeller's version 9.11 was used to probe the molecular architecture of SARS-CoV-2 3CL and comparative homology modeling in China, as well, by using version 0.6 of MEGA software and the ProtParam tool, similar sequences and instability indices identified * In China, Isothermal LAMP-based method-iLACO adopted for rapid colorimetric detection of 2019-Novel Coronavirus RNA viruses) * web-based Genome Detective software used to help in immediate and accurate diagnosis of COVID-19. Moreover, the use of the mentioned system has the potential to characterize new mutations of viral |
[[40], [41], [42], [43], [44], [45], [46], [47], [48], [49], [50], [51], [52], [53], [54], [55], [56], [57]] |
| Artificial intelligence/deep learning and Machin learning | ✓Diagnosis ✓practical surveillance in quick detection and diagnosis of infection prediction ✓improving the CT diagnosis speed for each case even in some cases better than RT-PCR screening ✓early infection detection ✓to help physicians in quick diagnosis and judgment by the accurate screening of COVID-19 ✓AI tracking platform is interfaced hospitals for sharing information ✓Therapeutic monitoring ✓projection of infected individuals and mortality ✓drug discovery ✓traffic management ✓logistics supply chain ✓provides self-registration and crowd management modules for high-risk populations ✓to protect health care workers by giving information and alarming about COVID-19, critical medical recommendation ✓improved patient safety by increasing accuracy and speed of diagnosis and screening ✓Reducing healthcare providers' workloads ✓Help to prevention ✓Forecasting of disease ✓Lung Infection Quantification through CT images |
* a free online screening toolkit defined as “COVID-19 Quick Test” was designed to help that citizens quickly recognize their health status and infection risks in China, as well, it offers recommendations according to the screening results * AI with deep learning method was used as a useful technique for accurate, timely, and sensitive extraction of unique features of images and facilitate the diagnosis in China. * In China, AI has improved the CT diagnosis speed for COVID-19 cases in some cases, it was better than RT-PCR screening) *AI platform provides self-registration and crowd management modules for high-risk populations, as well, the AI tracking platform is interfaced with more than 400 hospitals for sharing information |
[39,[57], [58], [59], [60], [61], [62], [63], [64], [65], [66], [67], [68], [69]] |
| Telemedicine | ✓Telecommunication by online education ✓to reduce the impact on the cultural and educational consequences of this epidemic, especially for children who are vulnerable to environmental risks and their physical health, mental health, and productivity in adult life ✓overcome to limited access to specialists, particularly in rural hospitals ✓remotely sharing health care services by using of doctor- doctor approach to diagnosis and consulting aims ✓Alternative for face-to-face communication between people and health care providers ✓control and treatment of psychological problems such as depression, stress by developing online mental health services |
*In China, Emergency Telemedicine Consultation System ETCS) has developed telemedicine services across connected hospitals to share health care services by using a doctor-to-doctor approach to diagnosis, treatment, and consulting aims * NoviGuide as a guideline based software was used for point-of-care decision support in health systems for COVID-19 diagnosis *Consult Station Medical Booths was developed for telemonitoring and screening of Covid-19 cases |
[23,[69], [70], [71], [72]] |
| Mobile phone | ✓Collecting the basic travel history along with the more common indexes ✓to assist in the early screening and identification of possible COVID-19 infected individuals ✓Informing health-related news ✓Remote teleconsultation such as Mental health advise ✓telemedicine outpatient services ✓Group consulting ✓Education and training ✓monitor chronic orthopedic ✓Radiodiagnosis ✓Monitoring of COVID-19 individuals ✓Triage for avoiding face to face or unnecessary visits |
*mHero Health as a mobile phone-based system was used for health worker communications by using text messaging or SMS, *Community Health Toolkit was used for providing health communication between health workers and supervisors, *HealthBeats Remote was used for vitals monitoring at home, *CommCare Case Management software as open-source mobile case management was developed for COVID-19 diagnosis |
[60,[72], [73], [74], [75], [76]] |
| Decision support system | ✓Risk assessment for suspected individuals ✓to assist GPs ✓can use in healthcare supply chain ✓can help to demand management in the health care context ✓for characterizing severity of COVID-19 ✓Triage of COVD19 Patients |
*a mobile-based DSS was developed to assist GPs in gathering data, triaging, and risk assessment in China * a clinical DSS was developed for prediction of severity risk and triage of COVID-19 Patients at hospital admission at Wuhan China |
[[77], [78], [79], [80], [81]] |
| The infection Control system in hospital | ✓decrease of infection by real-time monitoring leading immediate protection and corrective response ✓protecting the safety of staff |
* the initial infection control system was used as an influential tool for decreasing infection by real-time monitoring, providing immediate protection and corrective response in China. | [38] |
| Robotics | ✓to perform most of the hazard actions instead of health providers on COVID-19 patients ✓protects the safety of health care providers ✓to assist in patrolling and monitoring the COVID-19 by public safety authorities, health authorities, and businesses ✓use robot-controlled noncontact ultraviolet UV) surface in prevention aims ✓to sterilize all high-touch surfaces ✓for autonomous or remote-controlled disinfection ✓mobile robots are useful for diagnosis and screening trough temperature ✓used to repetitively monitor temperatures of individuals in the hospitals with data sharing to hospital information systems ✓to use instead of experts in remote areas, especially in quarantine conditions ✓to assist surgery during the pandemic ✓protecting by using robotic potentials such as Receptionist Robots, Nurse Robots, Ambulance Robots, Telemedicine Robots, Serving Robots in Hospital, etc. |
* a robot designed to perform most of the hazard actions such as ultrasounds, take mouth swabs and listen to sounds made by a patient's organs instead of health providers on COVID-19 patients at a Chinese university. * In China, autonomic robots developed to assist public safety authorities, health authorities, and businesses in the COIVD-19 hit regions by following tasks: 1) Police use Robots for patrolling and monitoring 2) Driverless sweeping vehicles help to keep the city clean 3) Disinfectant Robots aid in bringing in a new level of epidemic resistance |
[80,[82], [83], [84], [85], [86]] |
| online interactive dashboard/GIS | ✓easy capture, identify, and statistical report the location and number of new cases, death, recovered cases ✓Help control the outbreak and improve the fight against the infectious disease epidemic ✓providing various information such as outbreak source, public events, site selection, supply chain, and resource locator ✓critical source for delivering and collecting information ✓to use in analyzing, modeling/spatial modeling of disease, and forecasting aims ✓To provide web-based mapping ✓to provide health geography ✓Risk assessment through GIS |
In the following, dashboards that used during COVID-19 pandemics was indicated: WHO, Johns Hopkins_CSSE, and Early Alert Inc dashboards |
[[87], [88], [89], [90], [91], [92], [93], [94], [95], [96], [97]] |
| Internet of things IoT) | ✓Screening and monitoring health data by using smart sensors at different places such as airports, terminal buses, health organizations in smart cities ✓Forecasting COVID-19 patients ✓Informing healthcare providers and providing quick response between healthcare providers and patients ✓To help remote consultation among patients and healthcare providers ✓To assist quickly identify COVID19 cases ✓To facilitate information sharing ✓Real-time monitoring and tracking ✓To support diagnosis e.g., Smart Helmet) ✓use in prevention and control of COVID-19 disease ✓Reduce the workload in health care organization |
* a smart helmet with a combination of Mounted Thermal Imaging System, thermal camera technology, and IoT technology was designed to diagnose the COVID-19 from the thermal image automatically. IoT helps to detect infected cases by providing real-time data and monitoring the screening process * In China, the COVID-19 intelligent diagnosis and treatment assistant program nCapp)” based on the IoT was developed to diagnose infected cases early. * Internet of Medical Things IoMT) was developed for providing treatment aided to orthopedic patients, especially in remote areas during the COVID-19 pandemic through data gathering, report monitoring, testing, and analyzing of images |
[[98], [99], [100], [101], [102], [103]] |
| Virtual reality VR) | ✓rehabilitation Physical therapy, Cognitive Rehabilitation) ✓using by patients in the hospital for controlling stress ✓Mental health and psychological Disorders ✓Pain management ✓training purpose ✓Palliative Care ✓Virtual traveling ✓Virtual communication and collaboration |
* a 360 -Degree VR Rendering of COVID-19 was used to visualize the better extent of COVID-19 inflicted damage to the lungs scan at Washington university hospital *During the COVID-19 outbreak, PwC has increased its use of VR training for managers especially while managers are working remotely) to soft skills related to leadership, diversity, equity and inclusion, and harassment prevention. * For the first time, NHS staff tackling Covid-19 on the front line are using virtual reality to support their mental health and wellbeing. |
[99,[104], [105], [106], [107], [108]] |
| surveillance systems | ✓surveillance systems are useful to identify quarantine individuals with COVID-19 symptoms ✓increase in response to COVID-19 cases ✓enhancing staff protection in a healthcare setting ✓improving health surveillance policies ✓to estimate COVID-19 growth rate through surveillance systems ✓early detection ✓timely updates of references and population's data ✓to help governments to create time for preparedness |
*the COVID-19 Laboratory-Based Surveillance System was used in Islamabad-Pakistan, which could provide the initial aims of the surveillance such as risk factor information of all suspected cases, providing timely and accurate reports * one health surveillance OHS) system was developed for early identification of COVID-19 to break the chain of transmission in India |
[98,[109], [110], [111], [112], [113], [114], [115]] |
| internet search queries | ✓Google Search Volume Index for: •Showing information flow of the COVID-19 pandemic •raising public awareness •an epidemiologic surveillance tool •online tracking system for COVID-19 pandemic ✓internet search data shows information-seeking responses to news of local COVID-19 cases and showing web-search behavior |
*Google trend was used to study correlation about loss‐of‐smell‒related searches during the COVID-19 outbreak. According to the results, there is a strong correlation between them *Internet search data indicate societies respond to early report of COVID-19 pandemic in their state by closely seeking information about COVID-19. It was measured by searches for coronavirus, coronavirus symptoms, and hand sanitizer. * in Italy, web search behavior during the COVID-19 outbreak was more related to “face masks,” “amuchina” disinfectant), “symptoms of the novel coronavirus,” “health bulletin,” and “vaccines for coronavirus.” |
[[116], [117], [118], [119]] |
3.2.1. Bioinformatics systems
Bioinformatics systems using various methods such as deep learning, machine learning [120], virtual screening, etc. have been applied to quick drug discovery [121]. In other words, the immediate discovery of COVID-19 antiviral plays a critical role in overcoming outbreaks [40,41,[43], [44], [45], [46], [47], [48], [49], [50], [51], [52], [53], [54]]. Virtual drug screening is a useful and affordable approach to rapidly identify effective antiviral agents and potential protein targets. Traditional drug investigation has high cost and needs time to develop [40,[46], [47], [48], [49], [50], [51],122]. Some of the protocols or methods used for computational drug discovery include ligand/target-based virtual screening, molecular docking, homology modeling, molecular dynamics simulations, small molecule docking, and machine intelligence-based GNC, homologous targets screening, and structure‐based ab initio drug design [54,123].
3.2.2. Artificial intelligence AI)
Concerning the rapid spread of COVID-19, the use of AI with various capabilities is a useful technology in the faster diagnosis of positive cases, managing the outbreak, and reducing the further outbreak of COVID-19 [39,[57], [58], [59], [60], [61], [62], [63], [64], [65], [66], [67], [68],95]. AI-based analysis and diagnosis help physicians diagnose, judge, and improve patient safety by increasing accuracy, speed of diagnosis, and screening. AI could protect health care workers by giving information and by providing critical medical recommendations [62,63]. AI uses deep learning algorithms for solving complex problems to improve the accuracy of results. For example, Covid-19 symptoms are nonspecific. Hence, AI uses deep learning methods as a useful technique for accurate, timely, and sensitive extraction of unique medical images’ features that facilitate the diagnosis [61]. Many studies have used deep learning for various aims such as lung infection quantification, improving diagnosis, detection, patient monitoring, quick screening, and drug discovery [65,[124], [125], [126]].
3.2.3. Telemedicine
Face-to-face communication between people and healthcare providers is a serious challenge during the fast prevalence of COVID-19 [23]. However, limited access to specialists, particularly in rural hospitals, is another problem. Telemedicine services were used to remotely share the healthcare services by using a doctor-to-doctor approach to diagnosis and consulting aims [71]. Telecommunication and online education can be an unprecedented solution to reduce the destructive impact on this epidemic's cultural and educational consequences, such as environmental risks, physical health, mental health, and social life [70]. Hence, the control and treatment of individuals' psychological problems were facilitated by developing online mental health services [72].
3.2.4. Mobile phone
Mobile technology has been widely used in this period due to its accessibility [60,72,[74], [75], [76],110]. For example, a phone-based online survey was used to assist in the early screening, diagnosis, and identification of COVID-19 infected individuals [60]. Moreover, mobile phones are the most popular tools for informing public health, performing telemedicine, educating, and training [60,72,[74], [75], [76],110].
3.2.5. Decision support system
For administrational and clinical aims, DSSs could be developed to help decision-makers managers or healthcare providers) make the appropriate decisions. For example, determining the severity score of COVID-19 patients and supply chain management are two applications of DSS that were established to respond to the COVID-19 outbreak [[78], [79], [80]].
3.2.6. Infection control system
Health providers in hospitals particularly negative pressure isolated units) have the most exposure during patient care. The infection control systems by real-time monitoring are used as an influential tool for decreasing the infection, leading to immediate protection and corrective response [38].
3.2.7. Robotics
The primary purpose of designing robots is to perform the most hazardous actions, instead of medical staff, on COVID-19 patients. Robots could protect health care staff during medical procedures. However, robots also facilitated other tasks that could reduce transmission of infections e.g., disinfection, real-time monitoring, and early screening and diagnosis) [80,[82], [83], [84], [85], [86]].
3.2.8. Online interactive dashboard/GIS
Various information types, including location, number of new cases, number of death, number of recovered cases, and controlling trends of the outbreak, are reported using the online Dashboards e.g., WHO, Johns Hopkins CSSE, and Early Alert Inc dashboard). As an essential data source, Dashboards are supervised by regional and local health departments [[87], [88], [89], [90]]. Moreover, GISs are useful tools by providing various information could result in better management of the outbreak. Identifying the spreading sources, location-based data for analysis/modeling, informing public events, site selection, supply chain management, and resource locator are advantages of using GISs [[91], [92], [93]].
3.2.9. Internet of things IoT)
For screening and monitoring COVID-19 patients, health-related data such as body temperature are captured using smart sensors at different places such as airports, bus terminals, and health organizations in smart cities. Additionally, IoT applications such as collecting data and information, monitoring or tracking COVID-19 patients, monitoring infected regions, and information sharing could be beneficial in preventing further spreading [[98], [99], [100], [101], [102]].
3.2.10. Virtual reality VR)
Virtual reality technology is defined as a computerized simulation of the real world using various software and hardware [127]. According to human demands, VR has multiple applications by providing a virtual world for relaxation, traveling, video calls, improving mental disorders by reducing stress, and training healthcare providers [99,104,105].
3.2.11. Surveillance system
The safe city can be determined by adopting a terminal tracking system. Surveillance systems are useful to identify individuals with COVID-19 symptoms and quarantine them. In other words, by applying this technology, COVID-19 cases are screened and diagnosed quickly. Surveillance systems are capable tools for the safety protection of public health [98,[109], [110], [111], [112], [113]].
3.2.12. Internet search queries
Internet search queries e.g., the Google search volume index) were used to capture the penetration of information related to the COVID-19 pandemic. For example, Sousa-Pinto et al. showed that COVID-19–related Google trend data are more related to media coverage than to epidemic trends. Furthermore, people's web search behavior during the pandemic could be identified by analyzing internet search queries [[116], [117], [118], [119]].
3.3. Experts opinion for IT applications in emergency management of COVID-19 outbreak
Table 2 shows existing gaps, future directions, and experts’ opinions regarding what technologies were suitable for each phase of emergency management in the COVID-19 outbreak.
Table 2.
IT roles in each phase of emergency management according to experts opinions.
| Emergency management phase | Identified gaps | what tools are more powerful/useful | Future direction |
|---|---|---|---|
| Prevention/mitigation | *inadequate education for societies against infection outbreak before occurrence it *inadequate monitoring and controlling system in many countries * Lack of accurate predictive and forecasting models before the infection pandemic *inadequate management of resources equipment, human, etc.) |
*virtual reality for training aims *mobile health capabilities for education aims *Internet of Things IoT) and surveillance system for health monitoring aims *Robotics for monitoring purposes and using them as an alternative for human resources * developing infection control system in hospital for alerting general symptoms of patients *AI and deep learning methods for developing forecasting models |
*Communities should learn how to respond to infection outbreaks in stressful conditions so the use of a designed VR environment can immerse users in simulated situations to experience the adverse condition and learn how they should answer to infection epidemics before the occurrence of them *countries should be equipped with IoT and surveillance systems to screen and monitor the people and environmental factors to provide safe and healthy communities. *development of robots can play an essential alternative for limited human resources and hazard tasks. *Hospitals should be equipped with control systems to control the environment and patient condition automatically *forecasting and predictive model should be used for predicting emergency conditions for conducting prevention efforts. *improvement of IT literacy in communities |
| Preparedness | *inadequate management of resources such as healthcare centers, human resource *Inadequate education and informing about adverse effects of an infectious outbreak and efforts against the pandemic * inefficient smart technologies to help early screening and diagnosis before the pandemic occurs *inadequate information system for help manages, governments, and healthcare providers in decision making |
*mobile technologies for education aims *information systems for management and control of resources *VR for preparing people to respond against infection disease *develop robots for doing hazardous tasks and alternative for human resources * development of smart cities by using intelligent technologies for screening people across cities *development of decision support system for clinical and administrative aims *improvement of IT infrastructure in countries |
*mobile technologies can improve people skills for preparing people to respond to infection outbreaks when a pandemic occurs *VR should be used for preparing people before pandemics to education response, prevention, and preparedness requirements *cities should equip with smart technologies for early screening and diagnosis of patients e.g., IoT could be used for measuring body temperature, or surveillance system for monitoring detecting disease symptoms.) *improvement of IT infrastructure *improvement of electronic-governments in each industry such as healthcare, business, education, and so on *clinical and administrative DSS could help to achieve an optimal decision, especially in stressful conditions. |
| Response | *Lack in immediate response to pandemic *Inadequate in the use of all IT capabilities in some countries |
In the response phase, all types of technologies must be used to achieve an effective response see Table 1) | *Effective response to a pandemic is related to good planning in the prevention and preparedness phases, which should be considered in communities. * developing IT-based services delivery in healthcare and business are essential issues in immediate response o pandemics |
| Recovery | Need to planning at present for post-crisis | *Mobile technologies, telehealth, social media, and VR can be used for mental health recovery. *Use or continue the use of technology-based business and health services for saving time and cost e.g., telehealth, telemonitoring, online services, and so on) *management of resources by using information systems *Administrative DSS for helping managers to achieve optimal recovery *providing educational contents for transmitting experiences in the future |
*mental disorders such as depression, stress, and phobia are common after infection outbreaks, and IT-based technologies such as telemedicine, mobile health, and VR can play a critical role in the recovery phase *Negative effects of outbreaks in economy and business could be improved by using IT-based solutions such as online services delivery and decision support systems for administrative and clinical aims. *Using databases and big data for providing strategic planning in the future *Using decision systems can help managers make decisions by considering different dimensions such as time, place, cost, resources, etc. *Improvement of IT infrastructure and literacy |
According to experts’ opinions, all IT utilization in each phase of emergency management of pandemics depends on aims, IT infrastructure, IT literacy, economy, IT acceptance, and government support in each country.
4. Discussion
This review has presented IT applications in four-phases of emergency management, including mitigation/prevention, preparedness, response, and recovery for the COVID-19 epidemic. It seems that before the COVID-19 outbreak, there were not performed pre-crisis efforts mitigation/prevention, preparedness phases) for facilitating a pandemic, while IT advantages were already proven for other viral outbreaks such as SARS, MERS, and H1N1 [119,[128], [129], [130], [131], [132], [133], [134], [135], [136]]. In the mitigation/prevention phase of emergency management, IT was used for different aims. Optimal evaluation and selecting the best influenza mitigation strategies by Bayesian algorithm, providing the framework for modeling epidemic spreading and mitigation, comprehensive interactive model for predicting geographically epidemic progression, the control system for early detection of disease, the mathematical decision support tool for modeling mitigating infectious disease pandemics, deep learning short-term memory LSTM) methods for influenza epidemic prediction, flood risk management information system to support natural disaster mitigation measures are some IT-based strategies for the mitigation/prevention phase [[137], [138], [139], [140], [141], [142], [143], [144], [145], [146], [147], [148], [149], [150]].
In the preparedness phase of previous infectious disease pandemics, the AI prediction platform AiRBO) and Canadian automatic infectious disease surveillance BlueDot) were used for correctly predicting the location and the outbreak occurrence [60,128]. The mobile phone was used to report and reach local healthcare agencies. The global epidemic and mobility model GLEaM) is a computational epidemic model used to simulate the worldwide spread of influenza-like illnesses [151,152]. Web-based systems as an immediate surveillance tool are useful in predicting epidemics and creating preparedness plans against outbreaks [153]. Accordingly, investigation of the previous experiences of epidemics is an essential issue; in other words, lack of appropriate planning to answer serious concerns such as COVID-19 has led to such disagreeable conditions in many countries.
Concerning the COVID-19 outbreak, most of the efforts were conducted after the crisis occurred. Currently, IT has a critical role in the response phase of emergency management because there is a need for immediate reaction to disaster to reduce the hazard effect of the COVID-19 epidemic. Our review indicated that IT has a beneficial role in responding to emergency management by providing safety, immediate response, and easing the actions. Real-time control, monitoring and exchange information, response coordination, optimal use of time and cost, optimal screening, optimal diagnosis, and treatment are some benefits of IT during COVID-19 outbreak [38,40,[45], [46], [47], [48], [49], [50], [51], [52],[61], [62], [63],71,72,74,82,83,[87], [88], [89], [90], [91], [92], [93],98,105,109,110,131,132,140,154]. Furthermore, AI, computer-aided drug discovery, online service, robots, image processing, mobile health, and virtual reality are some other technologies that are used during the COVD-19 epidemic [[44], [45], [46], [47],60,61,83]. Portable analytical devices for point of care and easily screen of coronavirus infection [155], facilitating the detection of the adult respiratory virus by fully automated multiplex Polymerase chain reaction PCR) system [156], support vector machines SVM) for prediction of the severe acute respiratory syndrome [129], applying various computer-aided methods to drug discovery of epidemic infection [130,133,[157], [158], [159]], using IoT for Smart monitoring and management of MERS or SARS [131,136], cloud computing and social networks analysis with good accuracy as a useful tool for analyzing and monitoring H1N1outbreak [134] are other experiences of IT in infectious disease management. Many smartphone apps for several aims, such as education, alerting, facilitating the data exchange, communication, and coordinated reaction to respond in an emergency disaster, were developed [160], [161]. Therefore, many forms of IT applications could be used in disaster situations to achieve safety and reduce the viral outbreak's hazard effect.
Finally, for the recovery phase of COVID-19, we have to wait for the disaster's ends. However, IT's role in the recovery phase of the previous disasters using social networks, mobile health, etc. in recovering mental health, economy, and organizations function is proven [[162], [163], [164], [165], [166], [167], [168], [169]]. Indeed, mental disorders and economic problems will arise as important implications of COVID-19. Social networks for meditation, sport, healing, and sharing experiences with psychologists and social workers could play a useful role in the recovery of negative psychological effects of pandemics such as depression, anxiety, and phobia. Besides, mobile health tools such as cell phones, tablets, computers, personal digital assistants PDAs), and monitoring devices could be used to enhance health by providing self-care, self-management, and health-monitoring apps for managing stress, physical activity, and healthy eating behaviors. Economic problems due to decreased incomes is expected in this period. Therefore, information technologies could provide exciting tools for economic recovery during and after the COVID-19 pandemics. In other words, public organizations and agencies could consider social networks and online web-based solutions in their marketing program. Communities should use the experiences of the current condition for prevention aims in the future. Also, organizations could use databases with the content of COVID-19 data to change and improve their management strategies. Besides, Social network analysis of disaster conditions has a significant role in enhancing knowledge management, especially in the sharing, capturing, and using of knowledge. Data mining techniques can be used to predict and develop appropriate disaster management strategies from the collected information about epidemic diseases.
IT has proven its various capabilities for all phases of emergency management in previous infectious disease outbreaks. We should consider that facilitating and overcoming the crisis will be difficult without the use of IT. Unfortunately, more efforts to overcome infectious disease outbreaks such as COVID-19 usually are conducted after a crisis occurs. In other words, most IT applications were highlighted in the response phase, while the use of IT capabilities before the crisis has a critical role in reducing the destructive effect of infectious disease. For example, predicting, modeling, educating, training, informing, and automated alarming can be conducted before the crisis using various IT-based approaches. Many of the problems with COVID-19 are related to emergency management before it occurs. In addition to IT advantages in emergency management, some barriers i.e., lack of financial resources, poor organizational coordination, and collaboration of government, security problems, and privacy in e-government) should be addressed as much as possible.
There are different examples for each IT application during the COVID-19 outbreak. However, neglected tools for emergency management of COVID-19 should be extracted for each country according to their IT infrastructure, income level, etc. For example, smart city features could help in early screening and diagnosis of infected cases. However, it has not been provided in many cities. In this study, we tried to present an overview of the IT application and the existing gaps in the emergency management of the COVID-19 outbreak.
5. Conclusion
Applications of Information technology are an inevitable issue in any disaster situation, such as the COVID-19 outbreak. The crucial role of IT in the response phase of emergency management was highlighted during this period. Using IT could help manage the risk and hazardous effects of the outbreak and minimize the crisis damages. Successful experiences of various IT applications in countries during epidemics could enlighten the societies about infectious disease and outbreak management. There was no proper planning for emergency management of COVID-19 before the virus appeared, which could be a reason for the further spreading of this epidemic around the world. Improving technologies for predicting infectious disease outbreaks should be considered because they have an essential role in enhancing the country's and government's capabilities to cope with epidemics before they are involved in hazardous epidemics. Appropriate strategic planning will improve public health response to outbreaks, mitigate economic losses, and save lives. To sum up, the communities should utilize the maximum advantage of IT to support emergency management.
Sources of funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Consent
Studies on patients or volunteers require ethics committee approval and fully informed written consent which should be documented in the paper.
CRediT authorship contribution statement
Afsoon Asadzadeh: Conceptualization, Verification, Investigation, Data collection, Resources, Writing - original draft, Writing - review & editing, Review & Editing, Visualization. Saba Pakkhoo: Investigation, Data collection, Resources. Mahsa Mirzaei Saeidabad: Investigation, Data collection, Resources. Hero Khezri: Investigation, Data collection, Resources. Reza Ferdousi: Conceptualization, Verification, Writing - review & editing, Visualization, Supervision, Project administration.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
Not applicable.
References
- 1.Khorram-Manesh A. 2017. Handbook of disaster and emergency management. [Google Scholar]
- 2.Waugh W.L., Jr., Streib G. Collaboration and leadership for effective emergency management. Publ Adm Rev. 2006;66:131–140. [Google Scholar]
- 3.Duo E., Trembanis A.C., Dohner S., Grottoli E., Ciavola P. Local-scale post-event assessments with GPS and UAV-based quick-response surveys: a pilot case from the Emilia-Romagna Italy) coast. Nat Hazards Earth Syst. 2018;18(11):2969–2989. [Google Scholar]
- 4.Sakurai M., Murayama Y. Information technologies and disaster management–Benefits and issues. Progress in Disaster Science. 2019;2:100012. [Google Scholar]
- 5.Poser K., Dransch D. Volunteered geographic information for disaster management with application to rapid flood damage estimation. Geomatica. 2010;64(1):89–98. [Google Scholar]
- 6.Lee A.C., Phillips W., Challen K., Goodacre S. Emergency management in health: key issues and challenges in the UK. BMC Publ Health. 2012;12(1):884. doi: 10.1186/1471-2458-12-884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bellou M., Kokkinos P., Vantarakis A. Shellfish-borne viral outbreaks: a systematic review. Food Environ Virol. 2013;5(1):13–23. doi: 10.1007/s12560-012-9097-6. [DOI] [PubMed] [Google Scholar]
- 8.Aylward B., Barboza P., Bertherat E., Bilivogui P., Blake I., Brennan R. Ebola virus disease in west africa - the first 9 Months of the epidemic and forward projections. N Engl J Med. 2014;371:1481–1495. doi: 10.1056/NEJMoa1411100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Girard M.P., Tam J.S., Assossou O.M., Kieny M.P. The 2009 A H1N1) influenza virus pandemic: a review. Vaccine. 2010;28(31):4895–4902. doi: 10.1016/j.vaccine.2010.05.031. [DOI] [PubMed] [Google Scholar]
- 10.Tanner W., Toth D., Gundlapalli A. The pandemic potential of avian influenza A H7N9) virus: a review. Epidemiol Infect. 2015;143(16):3359–3374. doi: 10.1017/S0950268815001570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zumla A., Hui D.S., Perlman S. Middle East respiratory syndrome. Lancet. 2015;386(9997):995–1007. doi: 10.1016/S0140-6736(15)60454-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Peiris J.S., Yuen K.Y., Osterhaus A.D., Stöhr K. The severe acute respiratory syndrome. N Engl J Med. 2003;349(25):2431–2441. doi: 10.1056/NEJMra032498. [DOI] [PubMed] [Google Scholar]
- 13.Lam W., Zhong N., Tan W. Overview on SARS in asia and the world. Respirology. 2003;8(Suppl 1):S2–S5. doi: 10.1046/j.1440-1843.2003.00516.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lipsitch M., Swerdlow D.L., Finelli L. Defining the epidemiology of Covid-19—studies needed. N Engl J Med. 2020;382:1194–1196. doi: 10.1056/NEJMp2002125. [DOI] [PubMed] [Google Scholar]
- 15.Malik Y.S., Sircar S., Bhat S., Sharun K., Dhama K., Dadar M. Emerging novel Coronavirus 2019-nCoV)-Current scenario, evolutionary perspective based on genome analysis and recent developments. Vet Q. 2020;40(1):68–76. doi: 10.1080/01652176.2020.1727993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liu W., Zhang Q., Chen J., Xiang R., Song H., Shu S. N Engl J Med; 2020. Detection of covid-19 in children in early january 2020 in wuhan, China. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cai J., Sun W., Huang J., Gamber M., Wu J., He G. Indirect virus transmission in cluster of COVID-19 cases, wenzhou, China. Emerg Infect Dis. 2020;26(6) doi: 10.3201/eid2606.200412. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lippi G., Plebani M. Diagnosis; Berlin, Germany): 2020. The novel coronavirus 2019-nCoV) outbreak: think the unthinkable and be prepared to face the challenge. [DOI] [PubMed] [Google Scholar]
- 19.Chen Q., Quan B., Li X., Gao G., Zheng W., Zhang J. A report of clinical diagnosis and treatment of 9 cases of coronavirus disease 2019. J Med Virol. 2020;92(6):683–687. doi: 10.1002/jmv.25755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li L.H., Zhang G., Dang X.W., Li L. [Treatment strategies of Budd-Chiari syndrome during the epidemic period of 2019 coronavirus disease] Zhonghua wai ke za zhi [Chinese journal of surgery] 2020;580:E007. doi: 10.3760/cma.j.cn112139-20200221-00109. [DOI] [PubMed] [Google Scholar]
- 21.Adams J.G., Walls R.M. Supporting the health care workforce during the COVID-19 global epidemic. Jama. 2020 doi: 10.1001/jama.2020.3972. [DOI] [PubMed] [Google Scholar]
- 22.Meng L., Hua F., Bian Z. Coronavirus disease 2019 COVID-19): emerging and future challenges for dental and oral medicine. Journal of dental research. 2020 doi: 10.1177/0022034520914246. 22034520914246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wong J., Goh Q.Y., Tan Z., Lie S.A., Tay Y.C., Ng S.Y. Preparing for a COVID-19 pandemic: a review of operating room outbreak response measures in a large tertiary hospital in Singapore. Canadian journal of anaesthesia = Journal canadien d'anesthesie. 2020 doi: 10.1007/s12630-020-01620-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang Y., Su X., Chen W., Fei C.N., Guo L.R., Wu X.L. [Epidemiological investigation on a cluster epidemic of COVID-19 in a collective workplace in Tianjin] Zhonghua liu xing bing xue za zhi = Zhonghua liuxingbingxue zazhi. 2020;41(5):649–653. doi: 10.3760/cma.j.cn112338-20200219-00121. [DOI] [PubMed] [Google Scholar]
- 25.Unctad Global trade impact of the coronavirus COVID-19) epidemic. https://unctad.org/en/PublicationsLibrary/ditcinf2020d1.pdf Available from:
- 26.Reddick C. Information technology and emergency management: preparedness and planning in US states. Disasters. 2011;35(1):45–61. doi: 10.1111/j.1467-7717.2010.01192.x. [DOI] [PubMed] [Google Scholar]
- 27.Louis M.S. Global health surveillance. MMWR (Morb Mortal Wkly Rep) 2012;61(3):15–19. [Google Scholar]
- 28.Tom-Aba D., Olaleye A., Olayinka A.T., Nguku P., Waziri N., Adewuyi P. Innovative technological approach to Ebola virus disease outbreak response in Nigeria using the open data kit and form hub technology. PloS One. 2015;10(6) doi: 10.1371/journal.pone.0131000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.WHO Report of the WHO-China joint mission on coronavirus disease 2019 COVID-19) 2020. https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf Available from:
- 30.George D.B., Taylor W., Shaman J., Rivers C., Paul B., O'Toole T. Technology to advance infectious disease forecasting for outbreak management. Nat Commun. 2019;10(1):3932. doi: 10.1038/s41467-019-11901-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Murphy R.J. BMJ military health; 2020. Communicable diseases in humanitarian operations and disasters. [DOI] [PubMed] [Google Scholar]
- 32.Hsu E.B., Li Y., Bayram J.D., Levinson D., Yang S., Monahan C. State of virtual reality based disaster preparedness and response training. PLoS Curr. 2013;5 doi: 10.1371/currents.dis.1ea2b2e71237d5337fa53982a38b2aff. ecurrents.dis.1ea2be71237d5337fa53982a38b2aff. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wilson C., Jumbert M.G. The new informatics of pandemic response: humanitarian technology, efficiency, and the subtle retreat of national agency. J Int Humanit Action. 2018;3(1):8. doi: 10.1186/s41018-018-0036-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fonseca V., Xavier J., de Oliveira T., de Filippis A.M.B., Alcantara L.C.J., Giovanetti M. Mosquito-borne viral diseases: control and prevention in the genomics era. Current topics in the epidemiology of vector-borne diseases. Intech. 2019:1–14. [Google Scholar]
- 35.Kim H. Bioinformatics technology in clinical and public health microbiology applying computational methods. J Med Biomed Appl Sci. 2018;6(9):136–140. [Google Scholar]
- 36.Wang S., Kang B., Ma J., Zeng X., Xiao M., Guo J. Preprint); medRxiv: 2020. A deep learning algorithm using CT images to screen for Corona Virus Disease COVID-19) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Boulos M.N.K., Geraghty E.M. Geographical tracking and mapping of coronavirus disease COVID-19/severe acute respiratory syndrome coronavirus 2 SARS-CoV-2) epidemic and associated events around the world: how 21st century GIS technologies are supporting the global fight against outbreaks and epidemics. Int J Health Geogr. 2020;19(1):8. doi: 10.1186/s12942-020-00202-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chen X., Tian J., Li G., Li G. Initiation of a new infection control system for the COVID-19 outbreak. Lancet Infect Dis. 2020;20(4) doi: 10.1016/S1473-3099(20)30110-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hu Z., Ge Q., Jin L., Xiong M. 2020. Artificial intelligence forecasting of covid-19 in China. arXiv preprint arXiv:200207112. [Google Scholar]
- 40.Zhavoronkov A., Aladinskiy V., Zhebrak A., Zagribelnyy B., Terentiev V., Bezrukov D.S. Potential COVID-2019 3C-like protease inhibitors designed using generative deep learning approaches. Chem Rxivpreprint) 2020 [Google Scholar]
- 41.Elfiky A.A. Anti-HCV, nucleotide inhibitors, repurposing against COVID-19. Life Sci. 2020;248:117477. doi: 10.1016/j.lfs.2020.117477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yu L., Wu S., Hao X., Li X., Liu X., Ye S. 2020. Rapid colorimetric detection of COVID-19 coronavirus using a reverse tran-scriptional loop-mediated isothermal amplification RT-LAMP) diagnostic plat-form: iLACO. medRxivPreprint) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.ul Qamar M.T., Alqahtani S.M., Alamri M.A., Chen L.-L. Structural basis of SARS-CoV-2 3CLpro and anti-COVID-19 drug discovery from medicinal plants. J Pharm Anal. 2020 doi: 10.1016/j.jpha.2020.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Randhawa G.S., Soltysiak M.P., El Roz H., de Souza C.P., Hill K.A., Kari L. Machine learning using intrinsic genomic signatures for rapid classification of novel pathogens: COVID-19 case study. PloS One. 2020;15(4) doi: 10.1371/journal.pone.0232391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cleemput S., Dumon W., Fonseca V., Karim W.A., Giovanetti M., Alcantara L.C. Bioinformatics; Oxford, England): 2020. Genome Detective Coronavirus Typing Tool for rapid identification and characterization of novel coronavirus genomes. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jin Z., Du X., Xu Y., Deng Y., Liu M., Zhao Y. Structure-based drug design, virtual screening and high-throughput screening rapidly identify antiviral leads targeting COVID-19. Nature. 2020;582(7811):289–293. [Google Scholar]
- 47.Ahmed S.F., Quadeer A.A., McKay M.R. Preliminary identification of potential vaccine targets for the COVID-19 coronavirus SARS-CoV-2) based on SARS-CoV immunological studies. Viruses. 2020;12(3) doi: 10.3390/v12030254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Shanmugaraj B., Malla A., Phoolcharoen W. Emergence of novel coronavirus 2019-nCoV: need for rapid vaccine and biologics development. Pathogens Basel, Switzerland) 2020;9(2) doi: 10.3390/pathogens9020148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wang J. Fast identification of possible drug treatment of coronavirus disease-19 COVID-19) through computational drug repurposing study. J Chem Inf Model. 2020;60(6):3277–3286. doi: 10.1021/acs.jcim.0c00179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Talluri S. Preprint; 2020. Virtual high throughput screening based prediction of potential drugs for COVID-19. [DOI] [PubMed] [Google Scholar]
- 51.Kong R., Yang G., Xue R., Liu M., Wang F., Hu J. 2020. COVID-19 Docking Server: an interactive server for docking small molecules, peptides and antibodies against potential targets of COVID-19. arXiv preprint arXiv:200300163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Contini A. Virtual screening of an FDA approved drugs database on two COVID-19 coronavirus proteins. Preprint. 2020 [Google Scholar]
- 53.Kim J., Cha Y., Kolitz S., Funt J., Escalante Chong R., Barrett S. Advanced bioinformatics rapidly identifies existing therapeutics for patients with coronavirus disease-2019 COVID-19) J Transl Med. 2020;18:257. doi: 10.1186/s12967-020-02430-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mohamed K., Yazdanpanah N., Saghazadeh A., Rezaei N. 2020. Computational drug discovery and repurposing for the treatment of Covid-19: a systematic review. Available at SSRN 3583748preprint) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Contini A. 2020. Virtual screening of an FDA approved drugs database on two COVID-19 coronavirus proteins. [Google Scholar]
- 56.Amin S.A., Ghosh K., Gayen S., Jha T. Chemical-informatics approach to COVID-19 drug discovery: Monte Carlo based QSAR, virtual screening and molecular docking study of some in-house molecules as papain-like protease PLpro) inhibitors. J Biomol Struct Dynam. 2020:1–10. doi: 10.1080/07391102.2020.1780946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Yu L., Wu S., Hao X., Dong X., Mao L., Pelechano V. Rapid detection of COVID-19 coronavirus using a reverse transcriptional loop-mediated isothermal amplification RT-LAMP) diagnostic platform. Clin Chem. 2020;66(7):975–977. doi: 10.1093/clinchem/hvaa102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Xu C., Luo X., Yu C., Cao S.-J. The 2019-nCoV epidemic control strategies and future challenges of building healthy smart cities. Indoor Built Environ. 2020;29:639–644. [Google Scholar]
- 59.Xie X., Zhong Z., Zhao W., Zheng C., Wang F., Liu J. Chest CT for typical 2019-nCoV pneumonia: relationship to negative RT-PCR testing. Radiology. 2020 doi: 10.1148/radiol.2020200343. 200343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Rao A., Vazquez J.A. Identification of COVID-19 can be quicker through artificial intelligence framework using a mobile phone-based survey in the populations when cities/towns are under quarantine. Infect Contr Hosp Epidemiol. 2020:1–18. doi: 10.1017/ice.2020.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Xu B, Meng X. A deep learning algorithm using CT images to screen for Corona Virus Disease COVID-19). Preprint. [DOI] [PMC free article] [PubMed]
- 62.Peng M., Yang J., Shi Q., Ying L., Zhu H., Zhu G. Artificial intelligence application in COVID-19 diagnosis and prediction. Preprint. 2020 [Google Scholar]
- 63.McCall B. COVID-19 and artificial intelligence: protecting health-care workers and curbing the spread. Lancet Digit Health. 2020;2(4):e166–e167. doi: 10.1016/S2589-7500(20)30054-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Vaishya R., Javaid M., Khan I.H., Haleem A. Artificial Intelligence AI) applications for COVID-19 pandemic. Diabetes Metab Syndr. 2020;14(4):337–339. doi: 10.1016/j.dsx.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Shan F., Gao Y., Wang J., Shi W., Shi N., Han M. 2020. Lung infection quantification of covid-19 in ct images with deep learning. arXiv preprint arXiv:200304655. [Google Scholar]
- 66.Ghoshal B., Tucker A. 2020. Estimating uncertainty and interpretability in deep learning for coronavirus COVID-19) detection. arXiv preprint arXiv:200310769. [Google Scholar]
- 67.Zhang J., Xie Y., Li Y., Shen C., Xia Y. 2020. Covid-19 screening on chest x-ray images using deep learning based anomaly detection. arXiv preprint arXiv:200312338. [Google Scholar]
- 68.Huang L., Han R., Ai T., Yu P., Kang H., Tao Q. Serial quantitative chest ct assessment of covid-19: deep-learning approach. Radiol Cardiothorac Imaging. 2020;2(2) doi: 10.1148/ryct.2020200075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.行业|新冠疫情会是发展互联网+医疗健康的催化剂吗? 2020. Available from: https://www.cn-healthcare.com/articlewm/20200224/wap-content-1090153.html.
- 70.Wang G, Zhang Y, Zhao J, Zhang J, Jiang F. Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet.. [DOI] [PMC free article] [PubMed]
- 71.Zhai Y., Wang Y., Zhang M., Gittell J.H., Jiang S., Chen B. Preprint); 2020. From isolation to coordination: how can telemedicine help combat the COVID-19 outbreak? medRxiv. [Google Scholar]
- 72.Liu S., Yang L., Zhang C., Xiang Y.-T., Liu Z., Hu S. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7(4):e17–e18. doi: 10.1016/S2215-0366(20)30077-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.NoviGuide https://www.noviguide.com/ . Available from:
- 74.mHero. mHero health worker communications. https://www.mhero.org/ Available from:
- 75.CommCare case management. https://www.commcarehq.org/accounts/login/ Available from:
- 76.Iyengar K., Upadhyaya G.K., Vaishya R., Jain V. COVID-19 and applications of smartphone technology in the current pandemic. Diabetes Metab Syndr. 2020;14(5):733–737. doi: 10.1016/j.dsx.2020.05.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Liu Y., Wang Z., Ren J., Tian Y., Zhou M., Zhou T. A COVID-19 risk assessment decision support system for general practitioners: design and development study. J Med Internet Res. 2020;22(6) doi: 10.2196/19786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Govindan K., Mina H., Alavi B. A decision support system for demand management in healthcare supply chains considering the epidemic outbreaks: a case study of coronavirus disease 2019 COVID-19) Transp Res E Logist Transp Rev. 2020;138:101967. doi: 10.1016/j.tre.2020.101967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.McRae M.P., Simmons G.W., Christodoulides N.J., Lu Z., Kang S.K., Fenyo D. Clinical decision support tool and rapid point-of-care platform for determining disease severity in patients with COVID-19. Lab Chip. 2020;20(12):2075–2085. doi: 10.1039/d0lc00373e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Wu G., Yang P., Xie Y., Woodruff H.C., Rao X., Guiot J. Development of a clinical decision support system for severity risk prediction and triage of COVID-19 patients at hospital admission: an international multicenter study. Eur Respir J. 2020;2:2001104. doi: 10.1183/13993003.01104-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Wu G., Yang P., Xie Y., Woodruff H.C., Rao X., Guiot J. Development of a clinical decision support system for severity risk prediction and triage of COVID-19 patients at hospital admission: an international multicentre study. Eur Respir J. 2020;56(2):2001104. doi: 10.1183/13993003.01104-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.staff ETe. Robotic arm could save lives on medical frontline amid coronavirus outbreak. 2020. https://eandt.theiet.org/content/articles/2020/03/robotic-arm-could-save-lives-on-medical-frontline-amid-coronavirus-outbreak/ Available from:
- 83.Vardhan H. Autonomous Robots aid in patrolling and disinfecting COVID-19 hit China. 2020. Available from: https://www.geospatialworld.net/blogs/autonomous-robots-aid-in-patrolling-and-disinfecting-covid-19-hit-china/
- 84.Kimmig R., Verheijen R.H., Rudnicki M. Robot assisted surgery during the COVID-19 pandemic, especially for gynecological cancer: a statement of the Society of European Robotic Gynaecological Surgery SERGS) J Gynecol Oncol. 2020;31(3) doi: 10.3802/jgo.2020.31.e59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Zeng Z., Chen P.-J., Lew A.A. From high-touch to high-tech: COVID-19 drives robotics adoption. Tourism Geogr. 2020;22(3):724–734. [Google Scholar]
- 86.Khan Z.H., Siddique A., Lee C.W. Robotics utilization for healthcare digitization in global COVID-19 management. Int J Environ Res Publ Health. 2020;17(11):3819. doi: 10.3390/ijerph17113819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.WHO Novel coronavirus COVID-19) situation public dashboard) http://healthcybermap.org/WHO_COVID19/ Available from:
- 89.JohnsHopkins _CSSE. Coronavirus COVID-19 global cases dashboard) https://gisanddata.maps.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6 Available from:
- 90.EarlyAlertInc. Coronavirus 2020 dashboard) https://earlyalert.maps.arcgis.com/apps/opsdashboard/index.html#/20bfbf89c8e74c0494c90b1ae0fa7b78 Available from:
- 91.Boulos MNK, Geraghty EM. Geographical tracking and mapping of coronavirus disease COVID-19/severe acute respiratory syndrome coronavirus 2 SARS-CoV-2) epidemic and associated events around the world: how 21st century GIS technologies are supporting the global fight against outbreaks and epidemics. Int J Health Geogr.191). [DOI] [PMC free article] [PubMed]
- 92.Anastassopoulou C., Russo L., Tsakris A., Siettos C. Data-based analysis, modelling and forecasting of the novel coronavirus 2019-nCoV) outbreak. medRxiv. 2020 doi: 10.1371/journal.pone.0230405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Li D, Liu Z, Liu Q, Gao Z, Zhu J, Yang J, et al. Estimating the efficacy of quarantine and traffic blockage for the epidemic caused by 2019-nCoV COVID-19): a simulation analysis. medRxiv preprint..
- 94.Mollalo A., Vahedi B., Rivera K.M. GIS-based spatial modeling of COVID-19 incidence rate in the continental United States. Sci Total Environ. 2020;728:138884. doi: 10.1016/j.scitotenv.2020.138884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Bherwani H., Anjum S., Kumar S., Gautam S., Gupta A., Kumbhare H. Understanding COVID-19 transmission through Bayesian probabilistic modeling and GIS-based Voronoi approach: a policy perspective. Environ Dev Sustain. 2020:1–19. doi: 10.1007/s10668-020-00849-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Franch-Pardo I., Napoletano B.M., Rosete-Verges F., Billa L. Spatial analysis and GIS in the study of COVID-19. A review. Sci Total Environ. 2020;739:140033. doi: 10.1016/j.scitotenv.2020.140033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Kanga S., Meraj G., Farooq M., Nathawat M., Singh S.K. Risk assessment to curb COVID-19 contagion: a preliminary study using remote sensing and GIS. Resaerch squarepreprint) 2020 [Google Scholar]
- 98.Allam Z., Jones D.S. On the coronavirus COVID-19) outbreak and the smart city network: universal data sharing standards coupled with artificial intelligence AI) to benefit urban health monitoring and management. Healthcare. 2020;8(1):46. doi: 10.3390/healthcare8010046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Singh R.P., Javaid M., Haleem A., Suman R. Internet of things IoT) applications to fight against COVID-19 pandemic. Diabetes Metab Syndr. 2020;14(4):521–524. doi: 10.1016/j.dsx.2020.04.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Swayamsiddha S., Mohanty C. Application of cognitive internet of medical things for COVID-19 pandemic. Diabetes Metab Syndr. 2020;15(5):911–915. doi: 10.1016/j.dsx.2020.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Mohammed M., Syamsudin H., Al-Zubaidi S., AKS R.R., Yusuf E. Novel COVID-19 detection and diagnosis system using IOT based smart helmet. Int J Psychosoc Rehabil. 2020;24(7) [Google Scholar]
- 102.Bai L., Yang D., Wang X., Tong L., Zhu X., Zhong N. Chinese experts' consensus on the Internet of Things-aided diagnosis and treatment of coronavirus disease 2019 COVID-19) CEH. 2020;3:7–15. [Google Scholar]
- 103.Pratap Singh R., Javaid M., Haleem A., Vaishya R., Ali S. Internet of medical things IoMT) for orthopaedic in COVID-19 pandemic: roles, challenges, and applications. J Clin Orthop Trauma. 2020;11(4):713–717. doi: 10.1016/j.jcot.2020.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Wang S.S., Teo W.Z., Teo W.Z., Chai Y.W. Virtual reality as a bridge in palliative care during COVID-19. J Palliat Med. 2020;23(6):756. doi: 10.1089/jpm.2020.0212. [DOI] [PubMed] [Google Scholar]
- 105.Javaid M., Haleem A., Vaishya R., Bahl S., Suman R., Vaish A. Industry 4.0 technologies and their applications in fighting COVID-19 pandemic. Diabetes Metab Syndr. 2020;14(4):419–422. doi: 10.1016/j.dsx.2020.04.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Keith M. 360-Degree virtual reality rendering of COVID-19 infected lungs. 2020. https://www.ctsnet.org/article/360-degree-virtual-reality-rendering-covid-19-infected-lungs Available from:
- 107.Roepe L.R. Virtual reality training for managers in a post-COVID-19 workplace. 2020. Available from: https://www.shrm.org/resourcesandtools/hr-topics/technology/pages/virtual-reality-training-managers-covid-19-workplace.aspx.
- 108.University C. 2020. NHS staff tackling Covid-19 try out virtual reality to help reduce stress and anxiety. [Google Scholar]
- 109.Htun H.L., Lim D.W., Kyaw W.M., Loh W.-N.J., Lee L.T., Ang B. Responding to the COVID-19 outbreak in Singapore: staff protection and staff temperature and sickness surveillance systems. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Yue M., Clapham H.E., Cook A.R. Estimating the size of a COVID-19 epidemic from surveillance systems. Epidemiology. 2020;31(4):567–569. doi: 10.1097/EDE.0000000000001202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Chu H.Y., Englund J.A., Starita L.M., Famulare M., Brandstetter E., Nickerson D.A. Early detection of covid-19 through a citywide pandemic surveillance platform. N Engl J Med. 2020 doi: 10.1056/NEJMc2008646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Michelozzi P., de'Donato F., Scortichini M., De Sario M., Noccioli F., Rossi P. Mortality impacts of the coronavirus disease COVID-19) outbreak by sex and age: rapid mortality surveillance system, Italy, 1 February to 18 April 2020. Euro Surveill : bulletin Europeen sur les maladies transmissibles = European communicable disease bulletin. 2020;25(19) doi: 10.2807/1560-7917.ES.2020.25.19.2000620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Peixoto V.R., Nunes C., Abrantes A. Epidemic surveillance of covid-19: considering uncertainty and under-ascertainment. Port J Public Health. 2020;38:23–29. [Google Scholar]
- 114.Mushtaq A., Ikram A., Chaudhry A., Sandhu M., Khalid F., Hussain S. Evaluation of the COVID-19 laboratory-based surveillance system in islamabad-Pakistan 2020. Global Biosecurity. 2020;1(4) [Google Scholar]
- 115.Yasobant S., Patel K., Saxena D., Falkenberg T. COVID-19 in India: making a case for the one health surveillance system. Indian J Publ Health. 2020;64(6):135. doi: 10.4103/ijph.IJPH_488_20. [DOI] [PubMed] [Google Scholar]
- 116.Chundakkadan R., Ravindran R. Information flow and COVID-19 recovery. World Dev. 2020;136:105112. doi: 10.1016/j.worlddev.2020.105112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.The use of google trends to investigate the loss of smell related searches during COVID‐19 outbreak. Walker A., Hopkins C., Surda P., editors. International Forum of Allergy & Rhinology. 2020 doi: 10.1002/alr.22580. Wiley Online Library. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Sousa-Pinto B., Anto A., Czarlewski W., Anto J.M., Fonseca J.A., Bousquet J. Assessment of the impact of media coverage on COVID-19-related google trends data: infodemiology study. J Med Internet Res. 2020;22(8) doi: 10.2196/19611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Rovetta A., Bhagavathula A.S. COVID-19-Related web search behaviors and infodemic attitudes in Italy: infodemiological study. JMIR public health and surveillance. 2020;6(2) doi: 10.2196/19374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Raef B., Ferdousi R. A review of machine learning approaches in assisted reproductive technologies. Acta Inf Med. 2019;27(3):205–211. doi: 10.5455/aim.2019.27.205-211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Ferdousi R., Jamali A.A., Safdari R. Identification and ranking of important bio-elements in drug-drug interaction by Market Basket Analysis. Bioimpacts. 2020;10(2):97–104. doi: 10.34172/bi.2020.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Emami N., Pakchin P.S., Ferdousi R. Computational predictive approaches for interaction and structure of aptamers. J Theor Biol. 2020;497:110268. doi: 10.1016/j.jtbi.2020.110268. [DOI] [PubMed] [Google Scholar]
- 123.Raef B., Maleki M., Ferdousi R. Computational prediction of implantation outcome after embryo transfer. Health Inf J. 2020;26(3):1810–1826. doi: 10.1177/1460458219892138. [DOI] [PubMed] [Google Scholar]
- 124.Gozes O., Frid-Adar M., Greenspan H., Browning P.D., Zhang H., Ji W. 2020. Rapid ai development cycle for the coronavirus covid-19) pandemic: initial results for automated detection & patient monitoring using deep learning ct image analysis. arXiv preprint arXiv:200305037. [Google Scholar]
- 125.Wang S., Zha Y., Li W., Wu Q., Li X., Niu M. A fully automatic deep learning system for COVID-19 diagnostic and prognostic analysis. Eur Respir J. 2020 doi: 10.1183/13993003.00775-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Patankar S. Preprint; 2020. Deep learning-based computational drug discovery to inhibit the RNA Dependent RNA Polymerase: application to SARS-CoV and COVID-19. [Google Scholar]
- 127.Asadzadeh A., Samad-Soltani T., Rezaei-Hachesu P., Salahzadeh Z., editors. Low-cost interactive device for virtual reality. 2020 6th international conference on web research ICWR) IEEE; 2020. [Google Scholar]
- 128.Bogoch, Brady O.J., Kraemer M.U.G., German M., Creatore M.I., Kulkarni M.A. Anticipating the international spread of Zika virus from Brazil. Lancet. 2016;387(10016):335–336. doi: 10.1016/S0140-6736(16)00080-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Cai C.Z., Han L.Y., Chen X., Cao Z.W., Chen Y.Z. Prediction of functional class of the SARS coronavirus proteins by a statistical learning method. J Proteome Res. 2005;4(5):1855–1862. doi: 10.1021/pr050110a. [DOI] [PubMed] [Google Scholar]
- 130.De Groot A.S., Einck L., Moise L., Chambers M., Ballantyne J., Malone R.W. Making vaccines "on demand": a potential solution for emerging pathogens and biodefense? Hum Vaccines Immunother. 2013;9(9):1877–1884. doi: 10.4161/hv.25611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Fatima SA, Hussain N, Balouch A, Rustam I, Saleem M, Asif M. IoT enabled smart monitoring of coronavirus empowered with fuzzy inference system. Int J Agric Res Innovat Technol.61)..
- 132.Francis F., Ishengoma D.S., Mmbando B.P., Rutta A.S.M., Malecela M.N., Mayala B. Deployment and use of mobile phone technology for real-time reporting of fever cases and malaria treatment failure in areas of declining malaria transmission in Muheza district north-eastern Tanzania. Malar J. 2017;16(1):308. doi: 10.1186/s12936-017-1956-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Lan J., Lu S., Deng Y., Wen B., Chen H., Wang W. [Bioinformatics-based design of peptide vaccine candidates targeting spike protein of MERS-CoV and immunity analysis in mice] Bing du xue bao = Chinese journal of virology. 2016;32(1):77–81. [PubMed] [Google Scholar]
- 134.Sandhu R., Gill H.K., Sood S.K. Smart monitoring and controlling of pandemic influenza A H1N1) using social network analysis and cloud computing. J Comput Sci. 2016;12:11–22. doi: 10.1016/j.jocs.2015.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Song Y., Jiang J., Yang D., Bai C. Prospect and application of Internet of Things technology for prevention of SARIs. Clinical eHealth. 2020;3:1–4. [Google Scholar]
- 136.Xuanyang X., Yuchang G., Shouhong W., Xi L., editors. Computer aided detection of SARS based on radiographs data mining. 2005 IEEE Engineering in Medicine and Biology 27th Annual Conference. IEEE; 2006. [DOI] [PubMed] [Google Scholar]
- 137.Lonkar Y.S., Bhagat A.S., Manjur S.A.S., editors. Smart disaster management and prevention using reinforcement learning in IoT environment. 2019 3rd international conference on trends in electronics and informatics ICOEI) IEEE; 2019. [Google Scholar]
- 138.Kim H. Bioinformatics tools in clinical microbiology and infectious disease prevention algorithms. J Med Biomed Appl Sci. 2018;6(9):159–165. [Google Scholar]
- 139.Libin P.J., Verstraeten T., Roijers D.M., Grujic J., Theys K., Lemey P., editors. Bayesian best-arm identification for selecting influenza mitigation strategies. Joint European conference on machine learning and knowledge discovery in databases. Springer; Cham: 2018. [Google Scholar]
- 140.Chen Y., Zhou Y., Murch R., Nakano T. Molecular communications at the macroscale: a novel framework for modeling epidemic spreading and mitigation. 2018. https://arxiv.org/abs/1801.04627 Available from.
- 141.Mourant J.R., Fenimore P.W., Manore C.A., McMahon B.H. Decision Support for mitigation of livestock disease: rinderpest as a case study. Front Vet Sci. 2018;5:182. doi: 10.3389/fvets.2018.00182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Maharjan L., Ditsworth M., Niraula M., Narvaez C.C., Fahimi B. Machine learning based energy management system for grid disaster mitigation. IET Smart Grid. 2019;2(2):172–182. [Google Scholar]
- 143.Ahmed K., Bukhari M.A.S., Altaf M.D., Lugala P.C., Popal G.R., Abouzeid A. Development and implementation of electronic disease early warning systems for optimal disease surveillance and response during humanitarian crisis and ebola outbreak in Yemen, Somalia, Liberia and Pakistan. Online J Public Health Inform. 2019;11(2) doi: 10.5210/ojphi.v11i2.10157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Musa A., Watanabe O., Matsuoka H., Hokari H., Inoue T., Murashima Y. Real-time tsunami inundation forecast system for tsunami disaster prevention and mitigation. J Supercomput. 2018;74(7):3093–3113. [Google Scholar]
- 145.Grabowski M.K., Herbeck J.T., Poon A.F. Genetic cluster analysis for HIV prevention. Curr HIV AIDS Rep. 2018;15(2):182–189. doi: 10.1007/s11904-018-0384-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Zlojutro A., Rey D., Gardner L. A decision-support framework to optimize border control for global outbreak mitigation. Sci Rep. 2019;9:2216. doi: 10.1038/s41598-019-38665-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Sood S.K., Mahajan I. Fog-cloud based cyber-physical system for distinguishing, detecting and preventing mosquito borne diseases. Future Generat Comput Syst. 2018;88:764–775. [Google Scholar]
- 148.Zhu X., Fu B., Yang Y., Ma Y., Hao J., Chen S. Attention-based recurrent neural network for influenza epidemic prediction. BMC Bioinf. 2019;20:575. doi: 10.1186/s12859-019-3131-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Alessa A., Faezipour M. Preliminary flu outbreak prediction using twitter posts classification and linear regression with historical centers for disease control and prevention reports: prediction framework study. JMIR public health and surveillance. 2019;5(2) doi: 10.2196/12383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Kim Y.-J., Yura E., Kim T.-W., Yoon J.-S. Development of disaster prevention system based on deep neural network using deep learning with dropout. J Coast Res. 2019;91(sp1):186–190. [Google Scholar]
- 151.Yang C., Yang J., Luo X., Gong P. Use of mobile phones in an emergency reporting system for infectious disease surveillance after the Sichuan earthquake in China. Bull World Health Organ. 2009;87(8):619–623. doi: 10.2471/BLT.08.060905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Balcan D., Gonçalves B., Hu H., Ramasco J.J., Colizza V., Vespignani A. Modeling the spatial spread of infectious diseases: the GLobal Epidemic and Mobility computational model. J Comput Sci. 2010;1(3):132–145. doi: 10.1016/j.jocs.2010.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Christaki E. New technologies in predicting, preventing and controlling emerging infectious diseases. Virulence. 2015;6(6):558–565. doi: 10.1080/21505594.2015.1040975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Pang J., Wang M.X., Ang I.Y.H., Tan S.H.X., Lewis R.F., Chen J.I. Potential rapid diagnostics, vaccine and therapeutics for 2019 novel coronavirus 2019-nCoV): a systematic review. J Clin Med. 2020;9(3) doi: 10.3390/jcm9030623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Romao V.C., Martins S.A.M., Germano J., Cardoso F.A., Cardoso S., Freitas P.P. Lab-on-Chip devices: gaining ground losing size. ACS Nano. 2017;11(11):10659–10664. doi: 10.1021/acsnano.7b06703. [DOI] [PubMed] [Google Scholar]
- 156.Branche A.R., Walsh E.E., Formica M.A., Falsey A.R. Detection of respiratory viruses in sputum from adults by use of automated multiplex PCR. J Clin Microbiol. 2014;52(10):3590–3596. doi: 10.1128/JCM.01523-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Chou K.C., Wei D.Q., Du Q.S., Sirois S., Zhong W.Z. Progress in computational approach to drug development against SARS. Curr Med Chem. 2006;13(27):3263–3270. doi: 10.2174/092986706778773077. [DOI] [PubMed] [Google Scholar]
- 158.Law G.L., Tisoncik-Go J., Korth M.J., Katze M.G. Drug repurposing: a better approach for infectious disease drug discovery? Curr Opin Immunol. 2013;25(5):588–592. doi: 10.1016/j.coi.2013.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Nur S.M., Hasan M.A., Amin M.A., Hossain M., Sharmin T. Design of potential RNAi miRNA and siRNA) molecules for Middle East respiratory syndrome coronavirus MERS-CoV) gene silencing by computational method. Interdisciplinary sciences. computational life sciences. 2015;7(3):257–265. doi: 10.1007/s12539-015-0266-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Bachmann D.J., Jamison N.K., Martin A., Delgado J., Kman N.E. Emergency preparedness and disaster response: there's an app for that. Prehospital Disaster Med. 2015;30(5):486–490. doi: 10.1017/S1049023X15005099. [DOI] [PubMed] [Google Scholar]
- 161.Tambo E., Kazienga A., Talla M., Chengho C., Fotsing C. Digital technology and mobile applications impact on Zika and Ebola epidemics data sharing and emergency response. J Health Med Informat. 2017;8(2):254. [Google Scholar]
- 162.Akhgar B., Fortune D., Hayes R.E., Guerra B., Manso M., editors. Social media in crisis events: open networks and collaboration supporting disaster response and recovery. 2013 IEEE International conference on technologies for Homeland Security HST) IEEE; 2013. [Google Scholar]
- 163.Bonchi F., Castillo C., Gionis A., Jaimes A. Social network analysis and mining for business applications. ACM TIST. 2011;2(3):1–37. [Google Scholar]
- 164.Cassa C.A., Chunara R., Mandl K., Brownstein J.S. Twitter as a sentinel in emergency situations: lessons from the Boston marathon explosions. PLoS currents. 2013;5 doi: 10.1371/currents.dis.ad70cd1c8bc585e9470046cde334ee4b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Free C., Phillips G., Watson L., Galli L., Felix L., Edwards P. The effectiveness of mobile-health technologies to improve health care service delivery processes: a systematic review and meta-analysis. PLoS Med. 2013;10(1) doi: 10.1371/journal.pmed.1001363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Goswami S., Chakraborty S., Ghosh S., Chakrabarti A., Chakraborty B. A review on application of data mining techniques to combat natural disasters. ASEJ. 2018;9(3):365–378. [Google Scholar]
- 167.Jukic T., Merlak M. The use of social networking sites in public administration: the case of Slovenia. EJEG. 2017;15(1):2. [Google Scholar]
- 168.Shirota Y. 2014. Temporal awareness of needs after east Japan great earthquake using latent semantic analysis. 200. [Google Scholar]
- 169.Xu Z., Lu X., Cheng Q., Guan H., Deng L., Zhang Z. A smart phone-based system for post-earthquake investigations of building damage. INT J DISAST RISK RE. 2018;27:214–222. [Google Scholar]