Abstract
The COVID-19 pandemic has affected patient care deliver throughout the world, resulting in a greater emphasis on efficiently and safety. In this article, we discuss the experiences of several North American centers in utilizing cardiac CT during the pandemic. We also provide a case-based overview which highlights the advantages of cardiac CT in evaluating the following scenarios: (1) patients with possible myocardial injury versus myocardial infarction; (2) patients with acute chest pain; (3) patients with stable chest pain; (4) patients with possible intracardiac thrombus; (5) patients with valvular heart disease. For each scenario, we also provide an overview of various societies recommendations which have highlighted the use of cardiac CT during different phases of the COVID-19 pandemic. We hope that the advantages of cardiac CT that have been realized during the pandemic can help promote wider adoption of this technique and improved coverage and payment by payors.
Keywords: Coronary CTA, Cardiac CT, COVID-19
Abbreviations
- 18F-FDG PET/CT =
2-deoxy-2-[fluorine-18] fluoro- d-glucose PET integrated with CT
- ACS =
Acute coronary syndrome
- BMI =
Body mass index
- BWH =
Brigham and Women’s Hospital
- CABG =
Coronary artery bypass graft
- CAD =
Coronary artery disease
- CMP =
Cardiomyopathy
- CMR =
Cardiovascular magnetic resonance
- COVID-19 =
Coronavirus disease 2019
- CT =
Computed tomography
- CTA =
Computed tomography angiography
- CV =
Cardiovascular
- ECG =
Electrocardiogram
- ED =
Emergency department
- EF =
Ejection fraction
- ESC =
European Society of Cardiology
- FFRct =
Fractional flow reserve computed tomography
- GFR =
Glomerular filtration rate
- ICA =
Invasive coronary angiography
- LAD =
Left anterior descending
- LBBB =
Left bundle branch block
- LCx =
Left circumflex
- LIMA =
Left internal mammary artery
- LV =
Left ventricle
- MAC =
Mitral annular calcification
- NSTEACS =
Non-ST elevation acute coronary syndrome
- PET =
Positron emission tomography
- PPE =
Personal protective equipment
- RCA =
Right coronary artery
- SARS-CoV-2 =
Severe acute respiratory syndrome coronavirus-2
- SCCT =
Society of Cardiovascular Computed Tomography
- STEMI =
ST segment elevation myocardial infarction
- TAVR =
Transcatheter aortic valve replacement
- TEE =
Transesophageal echocardiogram
- TMVR =
Transcatheter mitral valve replacement
- TnT-hs =
Troponin T-high sensitivity
- TTE =
Transthoracic echocardiogram
1. Introduction
The United States currently possesses the highest number of documented Coronavirus Disease 2019 (COVID-19) cases caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Similar to other parts of the world, the pandemic has affected patient care delivery in North America in unprecedented ways, and cardiovascular (CV) imaging has been no exception, as concerns about safety and efficiency in the COVID-19 era has introduced new challenges and opportunities. The ability of cardiac computed tomography (CT) to rapidly evaluate multiple cardiovascular conditions ranging from coronary artery disease to valvular heart disease, has allowed CT to emerge as an important attribute during the COVID-19 pandemic. This article summarizes the experience of several North American programs in delivering cardiac CT services during the COVID-19 pandemic, and provides a case-based overview of key societal recommendations.
2. North American institutional experience during the COVID-19 pandemic
2.1. Brigham and Women’s Hospital, Boston, Massachusetts
In keeping with the objective of balancing safety with effective healthcare delivery, the cardiovascular (CV) imaging program at Brigham and Women’s Hospital (BWH) deferred all elective imaging studies in stable patients in mid-March 2020, until June 2020 when the peak of the initial surge of COVID-19 cases had passed. During this time non-elective cases such as coronary CT angiography (CTA) in patients with unstable chest pain or coronary CTA in selected patients with non ST-elevation myocardial infarction continued. In addition, cardiac CT was performed without delay for patients who required planning prior to urgent cardiac procedures, including transcatheter aortic valve replacement (TAVR) and transcatheter mitral valve replacement (TMVR) cases, as well as cardioversion, or atrial and ventricular ablation procedures.
During the pandemic, coronary CTA emerged as a useful test for COVID-19 patients who had elevated cardiac troponin levels in whom the etiology was unclear, and coronary CTA was used in selected cases to avoid invasive coronary angiography (ICA) (See Fig. 1 for example). Due to the increased off-hours demand for evaluating such urgent cases, our coronary CTA service was temporarily made available 7 days a week. The coronary CTA protocol that was used for such urgent cases included a multiphase acquisition to evaluate for left and right ventricular systolic function and regional wall motion abnormalities. In addition, a full chest CT was also performed at the same time, in cases where this information was felt to be useful by the clinical team. Because our COVID-19 coronary CTA cases were performed off-hours, we instituted the use of nitroglycerin patches (instead of sublingual tablets). The advantages of using patches was that they could be placed by the emergency room or inpatient team prior to the patient arriving in the CT room (where physicians were not present off hours).
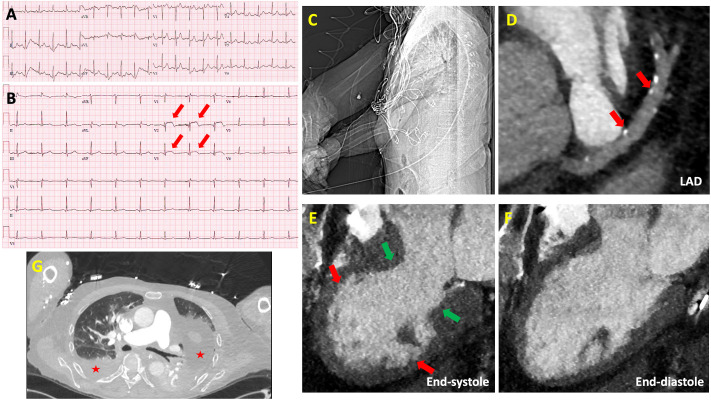
Fig. 1.
Role of Coronary CTA in Acute Chest Pain Associated with ST changes.
A) Electrocardiogram (ECG) on admission showing sinus tachycardia. B) Subsequent ECG during inpatient admission showing new ST-segment elevations in the anteroseptal leads (red arrows). C) Scout image from cardiac CT showing arms down position during image acquisition. D) Small amount of calcified plaque in the proximal and mid left anterior descending (LAD) artery resulting in minimal (1–24%) stenosis (red arrows). E) 3-chamber end-systolic image of cine-cardiac CT showing akinesis and ballooning of the apical segments, hypokinesis of the mid segments (red arrows) and normal contractility of the basal segments (green arrows) consistent with stress induced cardiomyopathy. F) 3-chamber end-diastolic image of cine-cardiac CT, left ventricular ejection fraction was quantified at 25%. G) Ground-glass opacities and pleural effusions (loculated on the left side) are visualized in bilateral lungs (red stars) consistent with known COVID-19 pneumonia.
Another important change to our cardiac CT program related to education of trainees. To promote social distancing, we minimized the number of individuals in our reading room, and reading sessions and cardiac CT conferences were all performed virtually using Microsoft Teams, in keeping with all other educational activities in the hospital. Our “virtual reading room” was also made available to all referring clinicians in order to allow them to join if they were interested in reviewing any studies, or to ask any questions related to cardiac CT. In addition, our BWH faculty and fellows participated in international teaching sessions and webinars organized by the Society of Cardiovascular Computed Tomography (SCCT).
2.2. University of Virginia, Charlottesville, Virginia
Shortly following the onset of the COVID-19 pandemic in March 2020 the University of Virginia cardiac CT program deferred most elective studies until after the peak of the pandemic. Outpatients that were previously scheduled to be scanned were referred to the imaging team for review of the clinical information and study indications. Patients deemed to not to have an urgent need for study performance were the majority and the referring provider was contacted to let them know that the patient was going to be rescheduled to a later date. Referring providers were provided the opportunity to discuss patients that they felt should not be delayed and these patients were scheduled on a case-by-case basis, with most elective procedures ultimately being rescheduled.
In patients with acute presentations, such as non-ST elevation acute coronary syndrome (ACS) or newly decreased left ventricular systolic function, the utilization of coronary CTA increased. While coronary CTA was routinely performed for these indications, the interest and enthusiasm to order coronary CTAs by Emergency Department providers and among our interventional and non-imaging colleagues increased substantially. Furthermore, during this time, exercise testing had virtually ceased and the performance of pharmacologic stress imaging studies that required longer patient-staff exposure time, such as stress cardiovascular magnetic resonance (CMR) or nuclear modalities, were generally not available. Even in patients with low-risk non-ST segment elevation MI presentations, a population not typically referred for coronary CTA, we shifted to selective utilization of coronary CTA in lieu of ICA, many times at the request of our interventional cardiology colleagues. Finally, in patients with an urgent need for surgical valve intervention, coronary CTA quickly became the default study to evaluate for coronary artery disease. While coronary CTA had been previously performed in many such low risk patients, providers quickly realized the value and high diagnostic accuracy in higher risk patients without known coronary artery disease.
The COVID-19 pandemic also significantly and permanently changed our utilization of transesophageal echocardiography (TEE) to evaluate for left atrial appendage thrombus prior to cardioversion procedures in patients with atrial fibrillation or atrial flutter. In March 2020, the performance of TEE for this indication virtually ceased except for patients with advanced kidney disease or those who needed TEE for valvular interrogation. Interestingly, this shift has persisted with cardiac CT now serving as the default test for this indication at our institution.
2.3. St Paul’s Hospital, Vancouver, British Columbia
As the COVID-19 pandemic descended upon us in March our lab in Vancouver was faced with similar but also some unique challenges. Cardiac CT has grown rapidly over the last decade in Vancouver, and it is the primary modality for the evaluation of symptomatic patients with suspected but not yet confirmed coronary disease. This is in addition to the central role cardiac CT has been playing for years for acute chest pain as well as for structural heart disease planning. The demand for cardiac CT has outstripped our supply which is a reality that would be hard to imagine in other health care systems but is not uncommon in our capitated healthcare system. Given that with COVID-19 we could not afford to stop outpatient cardiac CT testing given the pre-existing waitlist and attempted to re-triage the requisitions focusing on those with compelling symptoms and positive or equivocal ECG treadmills. Our daily case volume was reduced from 25 to 15 through patient selection and also owing to requirements for spacing and enhanced cleaning protocols. Through the pandemic we continued to use non-invasive physiology with FFRct to guide medical and revascularization management in patients with anatomical CAD. This approach proved to be particularly effective and safe during COVID-19 as it provides physiology without having to bring the patient back to the hospital for additional testing.
Beyond stable chest pain, for patients with acute chest pain we have been using coronary CTA to evaluate patients with indeterminate high sensitivity troponin levels. Early on in the pandemic, in particular when there was significant concerns regarding PPE supply, the use of coronary CTA extended to include many patients who would have historically proceeded for ICA. The clinical utility of this approach was meaningful, perhaps not surprisingly so, as the push to reserve an invasive approach for those requiring revascularization gained further momentum in this pandemic. As well, our efforts to explore coronary CTA in order to help avoid pre-TAVR ICA has seen increased interest with the declining anatomical disease burden with decreasing surgical risk making coronary CTA a viable option for more patients. With COVID-19 we have seen growing demand for expanding the role of coronary CTA in this population to help expedite the work up of these patients and get them to their definitive therapy as quickly and safely as possible. To that end, we have begun optimizing acquisition protocols for coronary CTA in selected patients where safe and feasible to enable more robust coronary evaluation beyond proximal coronary segments again exploring non-invasive physiology (FFRct). These changes to practice have continued as we have returned to our routine clinical volumes and while predictions are difficult it would seem that COVID-19 has served as a crucible for change and its impact on coronary CTA usage will likely remain well after the pandemic subsides.
2.4. The George Washington University, Washington, District of Columbia
The George Washington University Medical Center is an academic campus situated six blocks from the White House in Washington, DC. As the pandemic took hold in early 2020, our hospital entered into a state of full disaster preparedness with safety at the forefront of all care provisions. Since the first reported case of COVID-19 on March 7, 2020 in Washington, DC, cardiac CT has been a vital means to our care approach.
Pre-pandemic, our institution had already shifted to a heart team model that incorporated the use of coronary CTA in selected patients with myocardial injury and stable non-ST segment elevation MI in conjunction with the clinical care and interventional cardiology team. This practice continued through the pandemic as a means to identify appropriate patients for invasive angiography and revascularization planning while excluding patients without obstructive coronary artery disease to reduce potential virus exposure. Evaluation for structural interventions including TAVR and TMVR continued without delay or cessation for those patients with urgent symptoms. Our institution advanced the practice of foregoing ICA in appropriately selected TAVR/TMVR patients in which coronary CTA could exclude high risk coronary artery anatomy.
The pandemic resulted in the dramatic reduction in use of TEE with a definitive evolution in the use of cardiac CT in structural heart evaluation to reduce potential aerosolization exposure to the virus. Cardiac CT use shifted to become the preferred pathway in acute atrial arrhythmias for left atrial appendage evaluation prior to cardioversion and continued for outpatients undergoing atrial fibrillation ablation and left atrial appendage closure evaluation. Endocarditis evaluation changed to incorporate multiphase Cardiac CT for patients with low risk echocardiography findings, persistent bacteremia and ongoing clinical suspicion in lieu of TEE. For patients with definitive endocarditis requiring surgical intervention, both pre-operative TEE and cardiac catheterization was routinely deferred when possible in favor of cardiac CT to allow for evaluation of peri-valvular complications and coronary anatomy in patients without known coronary disease with less resource use.
In the midst of the pandemic peak, outpatient stable chest pain evaluation was triaged on a case by case basis and largely deferred. As COVID-19 cases have abated in our region, outpatient utilization of coronary CTA has increased as exercise stress testing has halted. Coronary CTA has often been preferred to pharmacologic stress testing approaches that require longer acquisition times and increased staff exposure; this approach is specifically reflected in our electronic medical record order set decision tree. The pandemic has created renewed interest from end-users of cardiac CT that include general internal medicine physicians who sought to better understand and utilize a safe, efficient approach to chest pain through coronary CTA that optimizes diagnosis, enhances cardiovascular prevention and aims to improve long-term outcomes.
3. Cardiac CT in the COVID-19 era
Throughout North America and around the world, the pandemic resulted in an estimated 50–90% decreased utilization of cardiovascular imaging tests, especially for imaging modalities that cause aerosolization of respiratory droplets such as transesophageal echocardiography (TEE) and exercise stress testing.1 In addition, there was a significant decrease in the number of elective invasive coronary angiograms. In many centers, cardiac CT was used in place of such tests to provide a safer alternative and to conserve personal protective equipment (PPE).2, 3, 4, 5, 6, 7, 8 Coronary CTA was also used to avoid inpatient admissions and expedite emergency room care among patients with acute chest pain.
Table 1 summarizes various expert consensus statements and societal recommendations related to the use of cardiac CT during the COVID-19 pandemic.
Table 1.
Key COVID-19 Guidance Documents that Provide Recommendations on use of Cardiac CT.
| Publication | Year | Objective/Scope | Summary/Selected recommendations related to CCT |
|---|---|---|---|
| Use of Cardiac Computed Tomography Amidst the COVID-19 Pandemic – SCCT Guidance Document Endorsed by ACC8 | Choi et al. JCCT 2020 Living document: https://scct.org/page/COVID-19 |
Guidance document for cardiac CT practitioners. |
|
| Safe Reintroduction of Cardiovascular Services During the COVID-19 Pandemic: From the North American Society Leadership2 | Wood et al. JACC 2020 | Guidance on the safe reintroduction of invasive CV procedures and diagnostic tests after the initial peak of the COVID-19 pandemic. |
|
| Multimodality Cardiovascular Imaging in the Midst of the COVID-19 Pandemic Ramping Up Safely to a New Normal1 |
Zoghbi et al., JACC CV Imaging 2020 | Expert opinion from the editors of JACC: Cardiovascular Imaging and developed in collaboration with the Cardiovascular Imaging Council of the American College of Cardiology. |
|
| Multimodality Imaging in Evaluation of Cardiovascular Complications in Patients With COVID-1940 | Rudski et al. JACC 2020 | Expert Panel from the ACC Cardiovascular Imaging Leadership Council. |
|
| Management of Acute Myocardial Infarction During the COVID-19 Pandemic13 | Mahmud et al., JACC 2020 | Consensus statement from SCAI, ACC, and ACEP for care of patients with acute MI. |
|
| ESC Guidance for the Diagnosis and Management of CV Disease during the COVID-19 Pandemic25 | Online at: https://www.escardio.org/Education/COVID-19-and-Cardiology/ESCCOVID-19-Guidance (Last update: June 10, 2020) | A guidance document relevant for all aspects of CV care during the COVID-19 pandemic. |
|
Society for Cardiovascular Angiography and Interventions (SCAI), American College of Cardiology (ACC), and the American College of Emergency Physicians (ACEP).
The following section will provide patient examples and a discussion of some of the key roles of cardiac CT during the pandemic.
3.1. Role of coronary CTA in acute chest pain and elevated troponin levels: myocardial injury versus myocardial infarction
An 87 year old male with long standing hypertension was admitted with severe COVID-19 pneumonia septic shock. While intubated in the medical intensive care unit, he developed acute ST elevations in the anteroseptal leads on electrocardiogram (ECG) (Fig. 1A and B). A bedside transthoracic echocardiogram (TTE) revealed new akinesis of the apical segments. High sensitivity Troponin T- (hsTn) increased from 65 to 994 ng/L (normal reference range = 0–9 ng/L). It was unclear if these acute changes were due to acute myocardial injury in the setting of severe COVID-19 pneumonia versus acute plaque rupture ST segment elevation myocardial infarction (STEMI). Review of prior chest CT images for this elderly male showed no significant calcifications. Such prior imaging, if available, should be reviewed as it may provide important guidance for test selection. Considering all factors, the primary team decided to obtain an urgent coronary CTA to evaluate for high-risk CAD. At the time of the cardiac CT, the patient was on three vasopressor medications. The coronary CTA study was further limited by the fact that the patient was on a ventilator and was unable to place his arms above the head (Fig. 1C). No beta-blockers or nitroglycerin was administered prior to the scan due to shock. The coronary CTA showed a small amount of calcified plaque in the proximal and mid left anterior descending (LAD) resulting in minimal (1–24%) stenosis (Fig. 1D). Cine images of the entire cardiac cycle demonstrated severe left ventricular (LV) systolic dysfunction, and the ejection fraction (EF) was quantified at 25%. There was akinesis of the apical segments, hypokinesis of the mid segments and normal contractility of the basal segments, most likely representing stress induced cardiomyopathy (CMP) related to acute COVID-19 infection. There was no evidence of a LV apical thrombus (Fig. 1E and F). Ground-glass opacities and pleural effusions (loculated on the left side) were visualized in bilateral lungs, consistent with known COVID pneumonia (Fig. 1G). He was eventually extubated, and the EF recovered to normal.
The SCCT COVID-19 guidance document indicates that coronary CTA may be valuable in cautiously selected patients who have symptoms of possible acute coronary syndrome (ACS), inconclusive ECG findings, and elevated cardiac biomarkers, for ruling out significant obstructive CAD. However, such utilization of coronary CTA should only be contemplated at centers with high-level of expertise and when diagnostic quality images can be attained.8 An early case series9 of 18 patients with confirmed COVID-19 and ST-segment elevation on ECG from 6 New York City hospitals identified a high prevalence of non-CAD related myocardial injury (n = 10 of 18). Similar experiences were also described throughout the United States.10 The mechanism of COVID-19 induced myocardial injury is postulated to be multifactorial, with possible contributors which include plaque rupture, coronary artery spasm, coronary microthrombi, hypoxic injury, via a cytokine storm, or from direct endothelial injury.11
While not routinely performed in all centers, another method to evaluate for myocarditis is by the use of CT delayed enhancement imaging. This technique often requires the administration of a larger dose of intravenous contrast, and acquiring an additional post contrast scan.12 In the appropriate clinical setting, areas of subepicardial delayed enhancement can be useful for diagnosing myocarditis.12
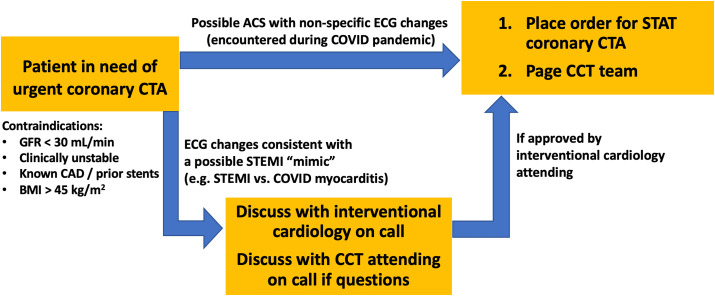
Cardiac CT is not recommended to evaluate patients with definitive ST elevation myocardial infarction. These patients should proceed directly for definitive therapy as per local institutional protocol.13 In patients with equivocal symptoms and atypical ECG, joint decision making between the Emergency Department (ED) provider, imaging team and interventional cardiology team regarding coronary CTA or invasive angiography is recommended.2 , 8 , 13 Fig. 2 shows the BWH algorithm that was used during the COVID-19 pandemic.
Fig. 2.
An institutional experience: Expanded BWH coronary CTA service during COVID-19 pandemic, off-hours (5pm–11pm) coronary CTA workflow.
The recently published VERDICT (Very Early Versus Deferred Invasive Evaluation Using Computerized Tomography in Patients With Acute Coronary Syndromes) trial15 was an observational sub-study using blinded coronary CTA in 1023 patients with non-ST elevation ACS (NSTEACS) with the objective to test if coronary CTA can exclude ≥ 50% stenosis among these patients. The trial demonstrated that coronary CTA had a high diagnostic accuracy (NPV 91%, PPV 88%) to rule out clinically significant CAD in patients with NSTEACS. Specifically, 30% of patients had no obstructive CAD, and were accurately identified by coronary CTA. The CARMENTA (The Supplementary Role of Non-invasive Imaging to Routine Clinical Practice in Suspected Non-ST-elevation Myocardial Infarction) randomized controlled trial16 evaluated whether coronary CTA or CMR can serve as a gatekeeper to invasive angiography among 207 patients with NSTEMI. A coronary CTA-first strategy was able to safely defer invasive coronary angiography in about one-third of patients. In addition, there was a trend of decreased complications and major adverse cardiac events among patients randomized to the imaging-first groups. While these trials were performed in the pre-COVID era, the results were useful in influencing recommendations during the COVID-19 pandemic. More recently, the 2020 European Society of Cardiology guidelines for NSTEMI also supported the role of coronary CTA with a Class I indication to allow for selective invasive angiography to exclude ACS when there is a low-to-intermediate likelihood of CAD and when cardiac troponin and/or ECG are normal or inconclusive.17
3.2. Role of coronary CTA in acute chest pain in the ED or observation unit: to facilitate rapid discharge
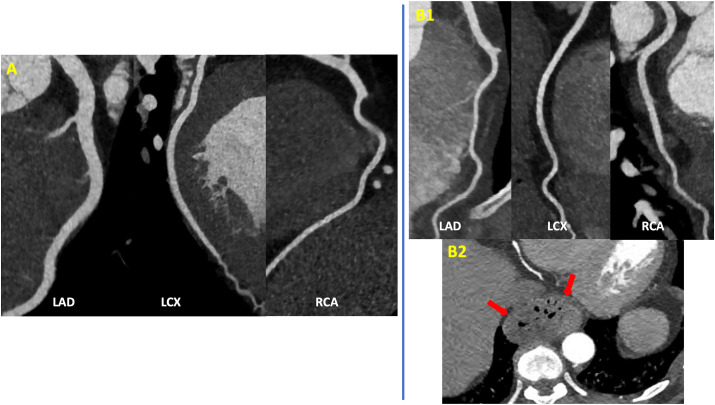
A 45 year old male healthcare worker with long standing uncontrolled hypertension (non-compliance to medications) presented with intermittent central chest pressure, nausea, myalgias, and subjective fever. Physical exam was notable for a high resting blood pressure of 180/90 mmHg. ECG in the Emergency Department (ED) was unremarkable and two serial TnT-hs were negative. His first COVID-19 test was negative, and a second one was pending. The patient was referred for an expedited coronary CTA from the ED to elucidate the cause of his acute chest pain. Coronary CTA demonstrated no plaque or stenosis (Fig. 3 A). He was started on anti-hypertensive medications with improvement of symptoms, and discharged home after the second COVID test came back negative.
Fig. 3.
Role of Coronary CTA in Acute Chest Pain in the ED or Observation Unit.
A) Normal coronary CTA showing no plaque or stenosis. B1) Coronary CTA showing no plaque or stenosis, B2) Moderate size hiatal hernia (red arrows).
A 59 year old female, current smoker, with prediabetes, obesity, and a family history of CAD presented with episodic epigastric pain for the past two weeks. Her physical exam and ECG were unremarkable in the ED. Two serial TnT-hs levels were within normal limits. An urgent coronary CTA ordered from the ED showed no coronary plaque or stenosis but revealed a moderate size hiatal hernia which was probably the cause for this patient’s symptoms (Fig. 3B).
Coronary CTA is useful for evaluating patients with suspected acute coronary syndrome who do not have a prior history of CAD. To date, there have been multiple randomized trials of coronary CTA in the ED, all demonstrating the safety and efficiency of this technique.18, 19, 20, 21, 22 Use of coronary CTA in the EDD and observation unit setting has been shown to reduce the time to diagnosis, as well as length of stay.23 Coronary CTA is also useful in identifying other etiologies of chest pain (e.g. aortic or pulmonary pathology and hiatal hernia). Patients with no plaque or stenosis on a coronary CTA have excellent prognosis, with a very low future risk of cardiac death or MI.23 Conversely, patients who are diagnosed with CAD on coronary CTA are most likely to benefit from lifestyle and preventive pharmacologic treatment. In addition, coronary CTA has the ability to detect atherosclerosis and therefore impact patient management on a larger scale, although implementation of preventive therapies following CTA in the ED remain suboptimal.24 The European Society of Cardiology (ESC) guidance for the diagnosis and management of CV disease during the pandemic advocates coronary CTA as the preferred non-invasive imaging modality in patients with acute chest pain and suspected significant CAD, due to its accuracy, short scan time and minimal exposure risk of patients and healthcare team.25
3.3. Role of coronary CTA in stable chest pain: to evaluate for high-risk coronary anatomy
A 58 year old male with distal esophageal cancer (Fig. 4A1 ) on chemoradiation was suffering from worsening dysphagia, and was planned for an expedited surgical esophagectomy. He had diabetes mellitus, hyperlipidemia and was also complaining of intermittent central chest pain that was sometimes relieved with sublingual nitroglycerin. A cardiac CT was ordered during the COVID-19 pandemic to evaluate for high risk coronary anatomy prior to emergent surgery, which showed only minimal stenosis (1–24%) of the mid LAD and the left circumflex (LCX) (Fig. 4A2). The patient underwent a successful surgical esophagectomy within the next few days.
Fig. 4.
Role of Coronary CTA in Stable Chest Pain - To Evaluate for High-risk Coronary Anatomy.
A1) 18F-FDG PET/CT scan showing distal esophageal cancer as an FDG avid lesion (blue arrow), A2) Coronary CTA showing a small amount of calcified plaque in the mid LAD causing minimal (1–24%) stenosis (red arrows), and a small amount of calcified and non-calcified plaque in the proximal and mid LCX causing minimal (1–24%) stenosis (green arrows). B1) 4-chamber end-systolic and end-diastolic image of cine-cardiac CT showing hypokinesis of all LV segments, B2) Coronary CTA showing a small amount of calcified plaque in proximal LAD causing minimal (1–24%) stenosis (red arrows), and a small amount of non-calcified plaque in the mid LAD causing mild (25–49%) stenosis (blue arrows).
A 72 year old female with newly diagnosed breast cancer was planned to be started on chemotherapy. A screening TTE prior to initiation of the chemotherapeutic regimen revealed moderately reduced LVEF, with no prior TTEs for comparison. Cardiac CT was ordered for assessment of significant CAD, that showed a small amount of calcified and non-calcified plaque resulting in minimal stenosis (1–24%) of the proximal LAD and mild stenosis (25–49%) of the mid LAD (Fig. 4B2). There was moderate biatrial enlargement, moderate LV cavity dilatation along with moderately reduced LV systolic function (Fig. 4B1,Fig. 4). Overall, the cardiac CT findings were consistent with a non-ischemic cardiomyopathy. The patient was started on optimal medical therapy for LV dysfunction and non-cardiotoxic chemotherapy was initiated.
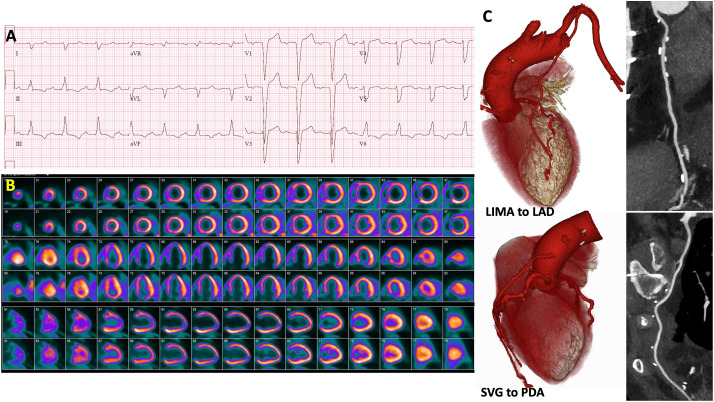
A 66 year old female with known CAD and recent coronary artery bypass graft (CABG) surgery presented with new onset dyspnea on exertion and heart failure. She was referred for a regadenoson myocardial perfusion positron emission tomography (PET) study that showed a dilated left ventricle with severe systolic dysfunction. There was a large reversible perfusion defect of moderate intensity involving the entire septum, associated with an abnormal interventricular septal motion (Fig. 5 B). Her ECG demonstrated a baseline left bundle branch block (LBBB) (Fig. 5A). One plausible explanation for the stress induced septal perfusion defect would be related to LBBB. On the other hand, with a recent CABG including a left internal mammary artery (LIMA) bypass graft to LAD raised concern for LIMA graft occlusion. Coronary CTA demonstrated a patent LIMA to LAD and a patent saphenous venous graft to posterior descending artery along with known multivessel native CAD (Fig. 5C). The patient was treated conservatively with medical therapy with good symptom control.
Fig. 5.
Role of Coronary CTA in Stable Chest Pain – Inconclusive Functional Test.
A) Baseline ECG demonstrating left bundle branch block. B) Regadenoson PET myocardial perfusion images showing a dilated left ventricle with a large reversible perfusion defect of moderate intensity involving the entire septum (stress: top row, rest: bottom row). C) Coronary CTA dedicated for bypass graft evaluation showing a patent left internal mammary artery graft to left anterior descending artery, and a patent saphenous venous graft to posterior descending artery.
The potential role of coronary CTA in selecting patients for treatment with aggressive medical therapy was demonstrated by the recent International Study of Comparative Health Effectiveness with Medical and Invasive Approaches (ISCHEMIA) trial. Over a median follow-up period of 3.3 years, coronary revascularization did not reduce the risk of cardiovascular events in stable patients with symptomatic CAD and moderate to severe ischemia, when compared with optimal medical therapy.26 This trial provided support that an initial treatment strategy using aggressive medical therapy was safe. In this study coronary CTA was used to rule out left main disease (∼5% of patients) and patients who did not have obstructive CAD (∼14% of patients) despite an abnormal functional study. However, in patients with angina, coronary revascularization led to a reduction in anginal symptoms and improved quality of life. In patients with significant symptoms and severe stenosis on coronary CTA, or in those with high risk coronary anatomy on coronary CTA (left main disease or multivessel CAD), coronary revascularization may be preferred. Therefore, in patients who demonstrate ischemia on functional testing, coronary CTA can be used to exclude high risk coronary anatomy, especially if a strategy of medical therapy alone is being pursued.27 , 28
3.4. Role of Cardiac CT in Evaluation of Intracardiac Thrombus thus avoiding transesophageal echocardiography, an aerosol generating procedure
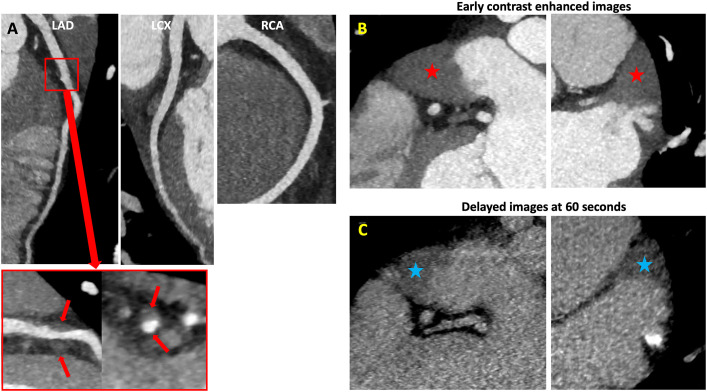
A 60 year old male with hypertension presented with episodes of chest pain, palpitations and nausea for several days. He was found to be in atrial fibrillation with rapid ventricular response. He was experiencing significant palpitations and intermittent episodes of chest pain. Labs showed mildly elevated hsTn levels of 45 and 50 ng/L. The first COVID-19 test was negative in the ED, and results from the second sample were pending. The patient was scheduled for an expedited cardioversion after ruling out a left atrial appendage thrombus. Considering all factors, a cardiac CT was ordered from the ED to evaluate for both significant CAD as a cause of his chest pain, and an intracardiac thrombus prior to cardioversion. Cardiac CT showed a small amount of non-calcified plaque resulting in mild stenosis (25–49%) of the mid LAD (Fig. 6 A), and also revealed a left atrial appendage thrombus, seen as a filling defect on both early (Fig. 6B) and delayed contrast enhanced images (Fig. 6C). The patient was started on high intensity statin therapy, rate control medications and anticoagulation. His symptoms improved with heart rate control and he was discharged from the ED after the second COVID-19 test was negative.
Fig. 6.
Role of Cardiac CT in Evaluation of Intracardiac Thrombus.
A) Coronary CTA showing a small amount of non-calcified plaque in the mid LAD causing mild (25–49%) stenosis (red arrows). B) Early contrast enhanced images showing a filling defect in the left atrial appendage which could represent mixing of contrast due to a low flow state or a thrombus (red stars). C) Delayed images acquired after 60 s showing a persistent filling defect thereby confirming the presence of a left atrial appendage thrombus (blue stars).
Cardiac CT has a high accuracy to exclude left atrial appendage thrombus with a sensitivity and NPV of nearly 100%,29 when a delayed phase is also acquired. A filling defect in the left atrial appendage on early contrast enhanced images can represent stasis, and thus post-contrast delayed imaging may be necessary in such cases to confirm or exclude the presence of a clot.30 TEE is an aerosol generating procedure considered by expert opinion and available evidence to be at high risk for potential spread of the virus through direct contact with patient secretions. The procedure also involves multiple team members including a physician, technologist, circulating nurse and anesthesiologist.1 , 31 In contrast, in the current scenario, cardiac CT enables reduced PPE use, decreased resource utilization, and enhanced safety to patients and health care workers. For this reason, in all of our institutions, cardiac CT was used in preference to TEE for excluding left atrial appendage thrombus.
3.5. Role of Cardiac CT in Evaluation of Valvular Heart Disease: endocarditis and complications, prosthetic heart valve dysfunction and prior to urgent structural interventions
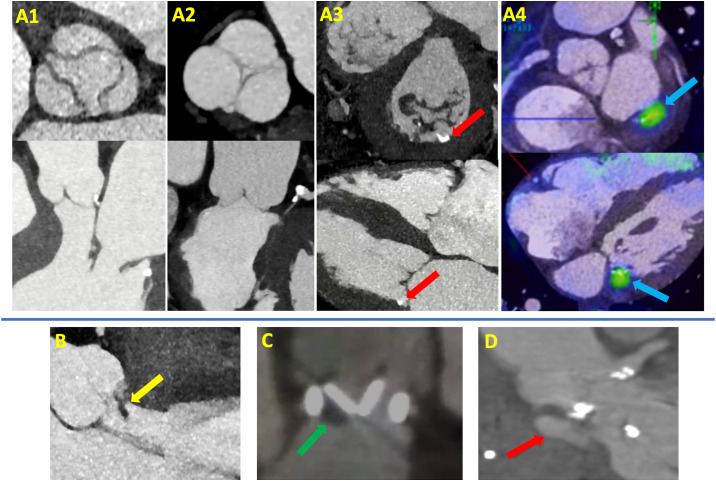
A 52 year old female with end stage renal disease on hemodialysis presented with fever and body aches for the past week. Her blood culture was positive for methicillin resistant staphylococcus aureus bacteremia. A TTE showed extensive posterior mitral annular calcification (MAC), but no definitive large valvular vegetations. Her COVID-19 test was positive. A joint decision was made between the primary team and the CV imaging team to pursue a cardiac CT and 2-deoxy-2-[fluorine-18] fluoro- d-glucose PET integrated with CT (18F-FDG PET/CT) as a non-aerosol generating test to evaluate for valvular vegetations, and infective endocarditis complications such as perivalvular abscess and aortic root pseudoaneurysms. Cardiac CT showed no valvular vegetations (Fig. 7A1-3 ), however posterior MAC was visualized. When cardiac CT images were fused with 18F-FDG PET/CT images, focal FDG uptake was demonstrated at the mitral annulus at the site of MAC concerning for a nidus of focal infection (Fig. 7A4). While not commonly observed, it has been shown that MAC is an inflammatory process that may serve as a nidus for infective endocarditis especially with staphylococcus aureus species due to mechanism of attachment, as demonstrated in this case with intense focal FDG uptake at the MAC location in a patient with sepsis of otherwise unknown source.32 The patient was treated with a prolonged course of antibiotics and did well.
Fig. 7.
Role of Cardiac CT in Evaluation of Valvular Heart Disease.
A) Cardiac CT showed no valvular vegetations: A1) Aortic valve in short and long axis views, A2) Pulmonic valve in short and long axis views, A3) Mitral and tricuspid valves in short and long axis views, posterior mitral annular calcification (MAC) is seen (red arrows). A4) Fused Cardiac CT images with 18F-FDG PET/CT images demonstrate focal FDG uptake at the mitral annulus at the site of MAC concerning for a nidus of focal infection (blue arrows). B) A large hypodensity (yellow arrow) is seen attached to the aortic valve, most likely representing a vegetation in a patient with gram positive bacteremia. C) A large hypodensity (green arrow) is seen attached to a bileaflet mechanical aortic valve, representing a thrombus in a patient with elevated transvalvular gradient and non-compliance to anticoagulation. D) Aortic root pseudoaneurysm (red arrow) in a patient with recent infective endocarditis.
Cardiac CT is an excellent alternative for evaluating patients with known or suspected infective endocarditis (Fig. 7B), especially when an initial TTE is inconclusive, or when TEE is not feasible. A distinctive advantage of cardiac CT over echo is the ability to evaluate prosthetic valves (Fig. 7C),33 and is suitable for detecting perivalvular involvement, including pseudoaneurysm (Fig. 7D) or fistulas. Accordingly, the current ESC guidelines recommend the modified Duke Criteria where identification of paravalvular involvement by cardiac CT is a major criteria for the diagnosis of infective endocarditis.34 A survey published in 2020 by the European Association of Cardiovascular Imaging reported that 60% of surveyed sites pre-pandemic were using cardiac CT for diagnostic purposes in infective endocarditis, most often in those patients with complex prosthetic valve endocarditis and in cases when TEE was inconclusive.35
In addition to evaluation of endocarditis, cardiac CT continued to have an important role in evaluating patients prior to urgent transcatheter aortic valve replacement (TAVR)33 or transcatheter mitral valve replacement (TMVR)36 procedures. In addition, coronary CTA has become more widely used as part of these scans in order to evaluate for significant CAD and thus avoid additional diagnostic angiography procedures.33
4. Conclusions
In summary, cardiac CT has been used in many roles during the COVID-19 pandemic (Fig. 8 ).37, 38, 39
Fig. 8.
Cardiac CT: One test, many uses.
While the selective utilization of cardiac CT has proven to be vital to many North American centers such as ours during the acute phase of COVID-19, access to this test remains limited in many parts of the country. As we look ahead, we anticipate that cardiac CT, along with other cardiovascular imaging modalities, will play an important role in evaluating patients with cardiac symptoms who present during the convalescent and chronic phases of COVID-19.40
Finally, we anticipate that many lessons learned during this pandemic may remain well past the COVID-19 era, including placing increased value on efficiency and safety of care (e.g. avoiding hospitalizations, avoiding invasive procedures). We also hope that some of the unique advantages of cardiac CT can be realized by payors, as payment and coverage for this test in the U.S. remains inadequate, and has been recognized as a significant barrier to wider adoption of this technique.41 In conclusion, the ability of cardiac CT to safely guide key management decisions, improve patient outcomes, decrease inpatient admissions, shorten ED DDDD length of stay, and reduce the need for invasive testing has made it a central diagnostic modality in the COVID-19 era and beyond.
Declaration of competing interest
None of the authors of this manuscript have a conflict of interest relevant to this topic.
References
- 1.Zoghbi W.A., DiCarli M.F., Blankstein R. Multimodality cardiovascular imaging in the midst of the COVID-19 pandemic: ramping up safely to a new normal. JACC Cardiovasc Imag. 2020;13:1615–1626. doi: 10.1016/j.jcmg.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wood D.A., Mahmud E., Thourani V.H. Safe reintroduction of cardiovascular services during the COVID-19 pandemic: guidance from North American society leadership. J Am Coll Cardiol. 2020;36(7):971–976. doi: 10.1016/j.cjca.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zoghbi William A., DiCarli Marcelo F., Blankstein Ron, Choi Andrew D., Flachskampf Frank A., Geske Jeffrey B., Grayburn Paul A., Jaffer Farouc A., Kwong Raymond Y., Jonathan A. 2020. Multimodality Cardiovascular Imaging in the Midst of the COVID-19 Pandemic: Ramping up Safely to a New Normal. JACC: Cardiovascular Imaging. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Skulstad H., Cosyns B., Popescu B.A. COVID-19 pandemic and cardiac imaging: EACVI recommendations on precautions, indications, prioritization, and protection for patients and healthcare personnel. Eur Heart J Cardiovasc Imag. 2020;21:592–598. doi: 10.1093/ehjci/jeaa072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Skali H., Murthy V.L., Al-Mallah M.H. Guidance and best practices for nuclear cardiology laboratories during the coronavirus disease 2019 (COVID-19) pandemic: an Information Statement from ASNC and SNMMI. J Nucl Med. 2020;27(3):1022–1029. doi: 10.1007/s12350-020-02123-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kirkpatrick J.N., Mitchell C., Taub C., Kort S., Hung J., Swaminathan M. ASE statement on protection of patients and echocardiography service providers during the 2019 novel coronavirus outbreak: endorsed by the American College of cardiology. J Am Coll Cardiol. 2020;75:3078–3084. doi: 10.1016/j.jacc.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Han Y., Chen T., Bryant J. Society for Cardiovascular Magnetic Resonance (SCMR) guidance for the practice of cardiovascular magnetic resonance during the COVID-19 pandemic. J Cardiovasc Magn Reson. 2020;22:26. doi: 10.1186/s12968-020-00628-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Choi A.D., Abbara S., Branch K.R. Society of cardiovascular computed tomography guidance for use of cardiac computed tomography amidst the COVID-19 pandemic endorsed by the American College of cardiology. J Cardiovasc Comput Tomogr. 2020;14:101–104. doi: 10.1016/j.jcct.2020.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bangalore S., Sharma A., Slotwiner A. ST-segment elevation in patients with covid-19 - a case series. N Engl J Med. 2020;382:2478–2480. doi: 10.1056/NEJMc2009020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Garcia S., Albaghdadi M.S., Meraj P.M. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75:2871–2872. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tavazzi G., Pellegrini C., Maurelli M. Myocardial localization of coronavirus in COVID-19 cardiogenic shock. Eur J Heart Fail. 2020;22:911–915. doi: 10.1002/ejhf.1828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pontone G., Baggiano A., Conte E. Quadruple rule-out" with computed tomography in a COVID-19 patient with equivocal acute coronary syndrome presentation. JACC Cardiovasc Imag. 2020;13:1854–1856. doi: 10.1016/j.jcmg.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mahmud E., Dauerman H.L., Fgp Welt. Management of acute myocardial infarction during the COVID-19 pandemic: a position statement from the society for cardiovascular angiography and interventions (SCAI), the American College of cardiology (ACC), and the American College of emergency physicians (ACEP) J Am Coll Cardiol. 2020;76:1375–1384. doi: 10.1016/j.jacc.2020.04.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Linde J.J., Kelbaek H., Hansen T.F. Coronary CT angiography in patients with non-ST-segment elevation acute coronary syndrome. J Am Coll Cardiol. 2020;75:453–463. doi: 10.1016/j.jacc.2019.12.012. [DOI] [PubMed] [Google Scholar]
- 16.Smulders M.W., Kietselaer B., Wildberger J.E. Initial imaging-guided strategy versus routine care in patients with non-ST-segment elevation myocardial infarction. J Am Coll Cardiol. 2019;74:2466–2477. doi: 10.1016/j.jacc.2019.09.027. [DOI] [PubMed] [Google Scholar]
- 17.Collet J.P., Thiele H., Barbato E. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J. 2020;2020 doi: 10.1093/eurheartj/ehaa624. [DOI] [PubMed] [Google Scholar]
- 18.Meijboom W.B., Meijs M.F., Schuijf J.D. Diagnostic accuracy of 64-slice computed tomography coronary angiography: a prospective, multicenter, multivendor study. J Am Coll Cardiol. 2008;52:2135–2144. doi: 10.1016/j.jacc.2008.08.058. [DOI] [PubMed] [Google Scholar]
- 19.Litt H.I., Gatsonis C., Snyder B. CT angiography for safe discharge of patients with possible acute coronary syndromes. N Engl J Med. 2012;366:1393–1403. doi: 10.1056/NEJMoa1201163. [DOI] [PubMed] [Google Scholar]
- 20.Hoffmann U., Truong Q.A., Schoenfeld D.A. Coronary CT angiography versus standard evaluation in acute chest pain. N Engl J Med. 2012;367:299–308. doi: 10.1056/NEJMoa1201161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gueret P., Deux J.F., Bonello L. Diagnostic performance of computed tomography coronary angiography (from the prospective national multicenter multivendor EVASCAN study) Am J Cardiol. 2013;111:471–478. doi: 10.1016/j.amjcard.2012.10.029. [DOI] [PubMed] [Google Scholar]
- 22.Budoff M.J., Dowe D., Jollis J.G. Diagnostic performance of 64-multidetector row coronary computed tomographic angiography for evaluation of coronary artery stenosis in individuals without known coronary artery disease: results from the prospective multicenter ACCURACY (Assessment by Coronary Computed Tomographic Angiography of Individuals Undergoing Invasive Coronary Angiography) trial. J Am Coll Cardiol. 2008;52:1724–1732. doi: 10.1016/j.jacc.2008.07.031. [DOI] [PubMed] [Google Scholar]
- 23.Hulten E., Pickett C., Bittencourt M.S. Meta-analysis of coronary CT angiography in the emergency department. Eur Heart J Cardiovasc Imag. 2013;14:607. doi: 10.1093/ehjci/jet027. [DOI] [PubMed] [Google Scholar]
- 24.Honigberg M.C., Lander B.S., Baliyan V. Preventive management of nonobstructive CAD after coronary CT angiography in the emergency department. JACC Cardiovasc Imag. 2020;13:437–448. doi: 10.1016/j.jcmg.2019.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.The European Society for Cardiology ESC guidance for the diagnosis and management of CV disease during the COVID-19 pandemic. https://www.escardio.org/Education/COVID-19-and-Cardiology/ESC-COVID-19-Guidance Last update: 10 June 2020.
- 26.Maron D.J., Hochman J.S., Reynolds H.R. Initial invasive or conservative strategy for stable coronary disease. N Engl J Med. 2020;382:1395–1407. doi: 10.1056/NEJMoa1915922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shaw L., Kwong R.Y., Nagel E. Cardiac imaging in the post-ISCHEMIA trial era: a Multisociety viewpoint. JACC Cardiovasc Imag. 2020;13:1815–1833. doi: 10.1016/j.jcmg.2020.05.001. [DOI] [PubMed] [Google Scholar]
- 28.Blankstein R., Shaw L.J. Ischemia trial: implications for coronary CT angiography. J Cardiovasc Comput Tomogr. 2020;14:1–2. doi: 10.1016/j.jcct.2019.12.030. [DOI] [PubMed] [Google Scholar]
- 29.Pathan F., Hecht H., Narula J., Marwick T.H. Roles of transesophageal echocardiography and cardiac computed tomography for evaluation of left atrial thrombus and associated pathology: a review and critical analysis. JACC Cardiovasc Imag. 2018;11:616–627. doi: 10.1016/j.jcmg.2017.12.019. [DOI] [PubMed] [Google Scholar]
- 30.Romero J., Husain S.A., Kelesidis I., Sanz J., Medina H.M., Garcia M.J. Detection of left atrial appendage thrombus by cardiac computed tomography in patients with atrial fibrillation: a meta-analysis. Circ Cardiovasc Imag. 2013;6:185–194. doi: 10.1161/CIRCIMAGING.112.000153. [DOI] [PubMed] [Google Scholar]
- 31.Nicoara A., Maldonado Y., Kort S., Swaminathan M., Mackensen G.B. Specific considerations for the protection of patients and echocardiography service providers when performing perioperative or periprocedural transesophageal echocardiography during the 2019 novel coronavirus outbreak: council on perioperative echocardiography supplement to the statement of the American society of echocardiography endorsed by the society of cardiovascular anesthesiologists. J Am Soc Echocardiogr. 2020;33:666–669. doi: 10.1016/j.echo.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pressman G.S., Rodriguez-Ziccardi M., Gartman C.H. Mitral annular calcification as a possible nidus for endocarditis: a descriptive series with bacteriological differences noted. J Am Soc Echocardiogr. 2017;30:572–578. doi: 10.1016/j.echo.2017.01.016. [DOI] [PubMed] [Google Scholar]
- 33.Blanke P., Weir-McCall J.R., Achenbach S. Computed tomography imaging in the context of transcatheter aortic valve implantation (TAVI)/transcatheter aortic valve replacement (TAVR): an expert consensus document of the Society of Cardiovascular Computed Tomography. J Cardiovasc Comput Tomogr. 2019;13:1–20. doi: 10.1016/j.jcct.2018.11.008. [DOI] [PubMed] [Google Scholar]
- 34.Habib G., Lancellotti P., Antunes M.J. [2015 ESC Guidelines for the management of infective endocarditis] Kardiol Pol. 2015;73:963–1027. doi: 10.5603/KP.2015.0227. [DOI] [PubMed] [Google Scholar]
- 35.Holte E., Dweck M.R., Marsan N.A. EACVI survey on the evaluation of infective endocarditis. Eur Heart J Cardiovasc Imag. 2020;21:828–832. doi: 10.1093/ehjci/jeaa066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Murphy D.J., Ge Y., Don C.W. Use of cardiac computerized tomography to predict neo-left ventricular outflow tract obstruction before transcatheter mitral valve replacement. J Am Heart Assoc. 2017;6 doi: 10.1161/JAHA.117.007353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Feuchtner GM, Barbieri F, Luger A. Myocardial injury in COVID-19: The role of coronary computed tomography angiography (CTA) J Cardiovasc Comput Tomogr. 2020 doi: 10.1016/j.jcct.2020.07.002. [published online ahead of print, 2020 Jul 17] S1934-5925(20)30391-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Farooqi K.M., Ghoshhajra B.B., Shah A.M. Recommendations for risk stratified use of cardiac computed tomography for congenital heart disease during the COVID-19 pandemic. J Cardiovasc Comput Tomogr. 2020;14:291–293. doi: 10.1016/j.jcct.2020.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pontone G, Scafuri S, Mancini ME. Role of computed tomography in COVID-19. J Cardiovasc Comput Tomogr. 2020 doi: 10.1016/j.jcct.2020.08.013. [published online ahead of print, 2020 Sep 4] S1934-5925(20)30436-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rudski L., Januzzi J.L., Rigolin V.H. Multimodality imaging in evaluation of cardiovascular complications in patients with COVID-19: JACC scientific expert panel. J Am Coll Cardiol. 2020;76:1345–1357. doi: 10.1016/j.jacc.2020.06.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Poon M., Lesser J.R., Biga C. Current evidence and recommendations for coronary CTA first in evaluation of stable coronary artery disease. J Am Coll Cardiol. 2020;76:1358–1362. doi: 10.1016/j.jacc.2020.06.078. [DOI] [PubMed] [Google Scholar]