Abstract
Landmark reports from reputable sources have concluded that the United States wastes hundreds of billions of dollars every year on medical care that does not improve health outcomes. While there is widespread agreement over how wasteful medical care spending is defined, there is no consensus on its magnitude or categories. A shared understanding of the magnitude and components of the issue may aid in systematically reducing wasteful spending and creating opportunities for these funds to improve public health.
To this end, we performed a review and crosswalk analysis of the literature to retrieve comprehensive estimates of wasteful medical care spending. We abstracted each source’s definitions, categories of waste, and associated dollar amounts. We synthesized and reclassified waste into 6 categories: clinical inefficiencies, missed prevention opportunities, overuse, administrative waste, excessive prices, and fraud and abuse.
Aggregate estimates of waste varied from $600 billion to more than $1.9 trillion per year, or roughly $1800 to $5700 per person per year. Wider recognition by public health stakeholders of the human and economic costs of medical waste has the potential to catalyze health system transformation.
In 2018, national health expenditures in the United States grew to $3.6 trillion, nearly 18% of the gross domestic product.1 The United States spends nearly twice as much per capita as other high-income countries,2 but mounting evidence demonstrates that a significant amount of US medical care spending does little or nothing to improve population health outcomes and is therefore wasteful.
In 2009, the Institute of Medicine (since renamed and now part of the National Academies of Sciences, Engineering, and Medicine [NASEM]) Roundtable on Value and Science-Driven Health Care convened a 4-part workshop series to examine the major causes of excess medical care spending, waste, and inefficiency in the United States.3 According to findings from these workshops, the lower-bound totals of estimates of excess expenditures amounted to $765 billion in 2009 ($879 billion in 2019 dollars; note that all subsequent amounts are in 2019 dollars unless otherwise noted) or 30% of national health expenditures. A separate analysis by Berwick and Hackbarth in 2012 estimated that the range of annual medical care waste was between 21% and 47% of national health expenditures.4 Extrapolating Berwick and Hackbarth’s estimates using the most recent data available yields a range of $803 billion to $1.8 trillion in wasted spending.
While there has been more attention paid to waste over the past few decades,5 this has not translated into a shared understanding among the larger public health community about the categories and magnitude of waste nor its opportunity costs. To put these estimates in perspective, the lower-bound opportunity cost of reducing waste could fund the entire 2020 budget request for the Department of Defense; the upper-bound estimate would be sufficient to completely erase outstanding student loans in the United States in a single year. Indeed, an underexplored aspect of waste is what other high-priority national needs are not adequately funded because the money funds medical care waste instead. These funds could even be allocated to reduce the unprecedented governmental debt from our response to the COVID-19 pandemic. In any other sector, waste of the same relative magnitude would be considered a crisis.6
The purpose of this essay is to advance a shared understanding of medical care waste and its constituent components through a review and synthesis of comprehensive estimates in the recent literature.
LITERATURE REVIEW
We performed a literature review to retrieve system-wide estimates of the magnitude of wasteful spending for medical care in the United States. We examined the opportunity cost of wasteful spending by identifying topical alternative public health priorities that are roughly equivalent in cost to wasteful medical care spending.
Inclusion criteria for our literature review were sources (peer-reviewed studies or reports from the gray literature) that developed and published an aggregate estimate of total wasteful medical care spending in the United States. We excluded sources that rereported previously published waste estimates. We also excluded sources that examined only single categories of wasteful spending (e.g., a study that only quantified the total waste attributable to medical care fraud). We eliminated these studies because we sought to get total estimates of waste and needed studies that were comprehensive and minimized double counting. Aggregating waste estimates from studies that originally examined only specific categories of waste risked both overcounting (i.e., including more costs than might be expected in a category) and undercounting (i.e., being too narrowly focused). We performed searches of PubMed, Google Scholar, and Google databases. After we removed ineligible, irrelevant, or duplicate sources, there were 34 remaining potential studies, reports, and gray literature records, which we then screened for eligibility and relevance. The final sample comprised 6 sources (see sample composition flowchart in Appendix Figure A, available as a supplement to the online version of this article at http://www.ajph.org).
Two authors (M. S. and J. M. M.) reviewed each included source. We reviewed each article’s definition of wasteful spending, its estimate of the overall magnitude of waste, and the categories it used to describe the components of waste. Not all studies included an exhaustive set of categories (see Appendix Table A). Because some of the categories differed substantially across all studies, we harmonized and recategorized them (see Appendix Table A). We then reclassified the categories in each study into our classification system and synthesized and crosswalked findings across sources to obtain overall estimates and waste categories. All authors independently coded and reviewed categories to determine a final set of crosswalked waste categories for all 6 sources. We adjusted all estimates of medical care waste by using the Consumer Price Index medical index growth rate and reported them in 2019 dollars unless otherwise specified. A complete description of our methodology, including search terms, screening criteria, and eligibility criteria, can be found in the Appendix Table A.
ESTIMATES OF WASTEFUL MEDICAL CARE SPENDING
The 6 system-wide estimates of wasteful spending we identified were conducted by diverse stakeholders and employed different approaches to generating estimates. Importantly, only 2 of the sources were published after 2012, and many predate the Affordable Care Act (ACA). Despite the variation in their methodologies, all sources suggest that a minimum of hundreds of billions of dollars per year are wasted on non–value-added medical expenses.
DEFINITIONS AND ESTIMATES OF MEDICAL CARE WASTE
The sources included in this analysis offer nearly identical definitions of medical care waste as a whole. Formal definitions are provided in the Appendix Table A, but there was widespread agreement that wasteful medical care spending is spending that can be reduced or eliminated without adversely affecting the quality of care or health outcomes.
Despite consensus regarding the overall definition of medical care waste and general agreement that this waste amounts to hundreds of billions of dollars annually, there is not widespread agreement on the total cost of wasteful spending, how to categorize its components, or the amount of each component.
As shown in Table 1, there was a nearly 3-fold difference between the highest and lowest aggregate estimates of waste in US medical care. However, the sources did tend to cluster in their overall estimates; the low end of the range was from approximately $600 billion to $900 billion per year, with 3 sources estimating waste between $876 billion and $891 billion per year. The high-end estimates of wasteful spending ranged from approximately $900 billion to more than $1.9 trillion per year.
TABLE 1—
Overview of Published Estimates of Comprehensive Wasteful US Medical Care Spending, in 2019 US$ Billions and Per Capita
| Source | Aggregate Magnitude of Waste (Shown in 2019 US$ Billions) | Aggregate Magnitude of Waste (Shown in 2019 US$ Per Capita) |
| “The Price of Excess—Identifying Waste in Healthcare Spending”7 | 891–1345 | 2685–4053 |
| “Where Can $700 Billion in Waste Be Cut Annually From the US Healthcare System?”8 | 876–1226 | 2639–3694 |
| “The Healthcare Imperative: Lowering Costs and Improving Outcomes: Workshop Series Summary”3 | 879 | 2649 |
| “Eliminating Waste in US Health Care”4 | 639–1449 | 1925–4366 |
| “How Much of US Health Care Spending Provides Direct Care or Benefit to Patients?”9 | 601–1905 | 1811–5740 |
| “Waste in the Health Care System: Estimated Costs and Potential for Savings”10 | 760–935 | 2290–2817 |
Even at the lowest end of the range, wasteful medical care spending is still at least a $600-billion-per-year issue in the United States—more than $1800 per person per year. A problem of this magnitude deserves substantial attention from consumers and policymakers. It is somewhat disconcerting, then, that there has been minimal, if any, progress in reducing wasteful spending.11 While it is not necessary to achieve consensus on the magnitude of wasteful spending to make progress toward reducing it, a better understanding by the public of how much is wasted, the specific areas to address, and the opportunity costs could help catalyze needed changes.
CATEGORIES OF WASTEFUL SPENDING
Each of the 6 study sources categorized the components of wasteful spending differently. Many sources included all 6 forms of waste shown in Figure 1, but other sources included only a subset. For example, fraud and missed prevention opportunities were not explicitly incorporated into all of the estimates, and excessive prices were only included by 4 of the 6 sources. Moreover, even when multiple sources included a nominally similar category, operationalization varied. For example, within missed prevention opportunities, some authors notably distinguished between clinical and nonclinical forms of prevention, suggesting that the authors considered the latter to be outside the purview of medical care stakeholders. By so narrowly focusing on the clinical aspects of the medical care system, however, they failed to recognize major preventive opportunities to improve health outcomes and address waste, not to mention upstream resources such as public education and urban planning that can also improve health outcomes, but are outside the scope of all of these studies, including the present one.12
FIGURE 1—
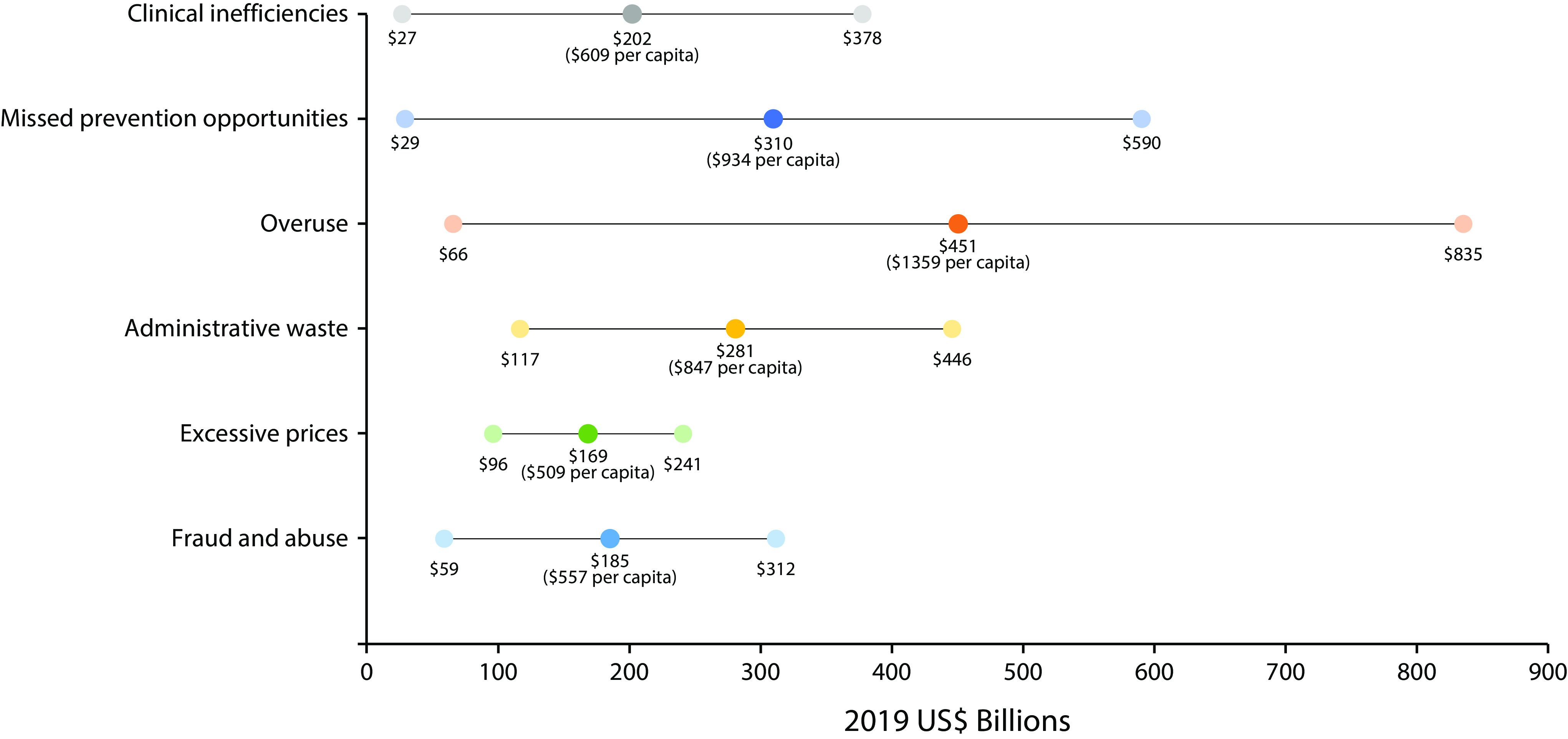
Estimates of Wasteful US Medical Care Spending Identified in the Published Literature, Shown as Median Estimate and Range in 2019 US$ Billions and Per Capita
THE OPPORTUNITY COST OF WASTE
Even the low end of aggregate waste estimates—approximately $600 billion per year in 2019 dollars—suggests that wasteful medical care spending is a major drain on the nation’s resources. As shown in Table 2, the median values of waste in each category are comparable in magnitude with major unmet investment priorities in other sectors affecting safety, social goods, and the environment. For example, the median estimate of fraud and abuse in medical care ($185 billion) is equivalent to the total annual estimated costs to provide free tuition at public colleges and universities ($79 billion), universal child care ($42 billion), universal pre-K ($26 billion), and partial wage replacement for up to 12 weeks of family leave ($28 billion). Fraud and abuse are highly visible examples of medical care spending that do not contribute to improved health. The idea that seemingly contentious policy priorities such as the 4 mentioned here could be financially addressed through redirecting resources from just 1 category of waste is powerful. From a financial or opportunity cost perspective, other less visible types of wasteful spending are no less costly, and the benefits of addressing them, even if challenging, are no less impactful.
TABLE 2—
Range Estimates of Wasteful US Medical Care Spending by Category of Waste and Corresponding Analogous Expenditures, 2019
| Category of Waste | 2019 Range of Estimates (US$ Billions) | Median Estimate (US$ Billions) | Median Estimate (US$ Per Capita) | Examples of Opportunity Cost of Wastea |
| Clinical inefficiencies | 27–378 | 202 | 609 | Triple the annual National Institutes of Health Research Budget ($117.6 billion) and annual US biopharmaceutical sector research and development ($71.4 billion)1 |
| Missed prevention opportunities | 29–590 | 310 | 934 | Total annual direct and indirect costs of diagnosed diabetes in the United States ($245 billion)13 and annual estimated costs of the American Housing and Economic Mobility Act ($50 billion) |
| Overuse | 66–835 | 451 | 1359 | Annual estimated costs associated with switching to 100% renewable energy in the United States ($423.9 billion)14 |
| Administrative waste | 117–461 | 281 | 847 | Repeal of the estate tax ($64 billion) and a 10% tax reduction to households earning less than $200 000 ($174 billion) |
| Excessive prices | 96–241 | 169 | 509 | Universal child care ($42 billion), paid family leave ($28 billion), and double the budget of the Supplemental Nutrition Assistance Program ($68 billion) |
| Fraud and abuse | 59–312 | 185 | 557 | Free annual tuition across all public US colleges and universities ($79 billion) and free annual universal pre-K ($26 billion) |
Note. All amounts shown in table are in constant 2019 dollars, adjusted for inflation using the Consumer Price Index medical price index growth rate.
What median estimate amount could cover if addressed and reinvested.
As public health officials contend with concerns over a US life expectancy that has decreased each year since 2014,15 additional tools and resources to have a positive impact on the life course may be needed. Despite clear and persistent warnings that we would be unprepared for the threat of an emerging pandemic, the United States failed to adequately invest in its public health infrastructure in advance of the COVID-19 pandemic. Evidence suggests that investing in policies and interventions that improve the social determinants of health is important, yet financial resources and political will are always limited. Climate change, for example, is an existential threat in which US commitment to renewable energy would show leadership in reducing the pace and effects of climate change. While the mechanisms for transferring wasteful medical care spending into such initiatives remain a policy challenge, public and policymaker understanding is critical to enable the nation to tackle deeply entrenched vested interests and capitalize on the enormous opportunity to repurpose wasted dollars.6,12
LIMITATIONS
Our findings should be viewed with some limitations in mind. First, because of the range of publication types and venues included, this study was not structured as a formal systematic review, and there may be other relevant sources not retrieved through our searches. To identify as many relevant sources as possible, we used a multifaceted search strategy across multiple databases. We sought to describe our methods in sufficient detail to enable transparency and replication to reduce risk of bias from this multifaceted search.
Second, data from the 6 sources reflect different years, may reflect factors that have since changed, or may have been measured differently based on specific definitions of variables. Perhaps most notably, most of the studies included were conducted before the ACA was fully implemented. Although the ACA did not focus extensively on reducing waste, there have been important changes in the medical care system that may have affected waste. Not every source provides enough methodological detail to recreate its estimates with post-ACA data.
Third, this analysis was able to present only descriptive findings as reported by each study. Further causal inferences related to the categorization or magnitude of medical care waste would require additional data. Lastly, we did not examine sources that addressed only a single category or more limited categories of waste (e.g., only clinical waste) as many did not contain sufficient methodological detail to ensure that aggregation of estimates from multiple sources would not result in under- or overcounting of waste. We focused only on studies whose goal was to estimate system-level waste estimates.
WHERE DO WE GO FROM HERE?
By more clearly defining and categorizing the problem of wasteful spending in medical care and suggesting important missed opportunities to reduce disparities and improve health outcomes, this essay is intended to help public health practitioners more fully understand the problem and drive action. The ongoing COVID-19 pandemic demonstrates the horrendous health inequities resulting from a failure of the nation to fully address upstream determinants of health. Public health now has a generational opportunity to articulate the problem of waste, its consequences, and the opportunities for change.
The potential for waste reduction in medical care is substantial, in terms of its impact on both US population health and the US economy. Eliminating medical care waste could allow us to recapture hundreds of billions of dollars every year that provide no health value. Many of those savings would accrue to the private sector—savings that could be used to increase wages, reduce unemployment, and enhance international competitiveness. Substantial amounts would also accrue to federal and state governments and could be used for public health programs as well as social and environmental initiatives. Previous analyses have shown that reallocating wasted medical care dollars toward other priorities can yield meaningful dividends to our health status and outcomes.6 Yet concrete strategies for doing so remain elusive.
Existing literature identifies many potential sources of waste and provides a broad range of estimates of the magnitude of excess spending. Yet, among the 6 sources included here, only 2 outlined definitive steps for stakeholders to address wasteful spending. In their Workshop Series Summary, Yong et al. and the NASEM offered 10 strategies to lower costs and improve outcomes.3 Cumulatively, these opportunities represent total potential savings of $428 billion to $552 billion annually, or $1289 to $1662 per person. Berwick alternatively proposed a “wedges” model for reducing medical care spending, based on the previous work of Pacala and Socolow.16 Addressing each of the 6 wedges, or categories, of wasteful spending would require identifying specific services within each wedge that do not improve health outcomes and using all available policy, training, and managerial levers to reduce their use.
Despite the identification of approaches to reducing waste, widespread adoption of those strategies has been slow. Given that the ACA and other recent reforms aimed to “bend the cost curve,” it is disappointing that nearly all comprehensive estimates of medical care waste predate the ACA. The ACA authorized a broad agenda of reform projects, including accountable care organizations, bundled payments, value-based purchasing, primary care initiatives, and other payment and service delivery models, all of which have the potential to modestly reduce wasteful spending. Yet most care is still not delivered under value-based payment models. The percentage of medical care payments tied to value-based care reached 34% in 2017, short of the 50%-by-2018 target sought by the US Department of Health and Human Services.17 The ACA’s overall impact on health spending remains somewhat open to debate, but data suggest that it has been successful at moderating spending growth.18,19 Still, no studies to date have concluded that the ACA has resulted in changes that would avert hundreds of billions of dollars’ worth of wasteful medical care spending each year. More research is needed to determine the degree to which the ACA has actually bent versus merely dented the cost curve.18
Comprehensive demand-side and supply-side innovations could be pursued in parallel to reduce wasteful spending. Demand-side reforms would involve introducing regulations that promote price and quality transparency and payer innovations that substitute value for volume, such as reference-based pricing.20 However, this approach may have drawbacks as evidence suggests that some portion of the reduction in costs would result from patients forgoing necessary care because of increased out-of-pocket costs.21 Innovation and redesign of insurance models, such as the Medicare Advantage Value-Based Insurance Design Model, could mitigate those concerns by reducing cost sharing for effective clinical services. Supply-side reforms would involve facilitating the migration from fee-for-service payment systems to more cost-effective alternatives, such as bundled payments, and evidence suggests that adoption of such strategies does not adversely affect the quality of care.22 Both demand-side and supply-side innovations to meaningfully reduce waste should focus on large-scale systems change, rather than modifying or appending existing processes.
As expected, there are complex barriers impeding major change. The political will to accomplish this and the entrenched interests for whom waste represents income are frequently misaligned and cannot be underestimated. Leaders must reconcile constituent values, effective policy, and political saliency.5 The United States could adopt large-scale reforms capable of addressing some areas of waste, such as administrative complexity, that the strategies discussed here are not equipped to eliminate. Notably, a shift to a single-payer system (e.g., Medicare for All) could curb administrative costs and potentially reduce unnecessary care.23
Yet there is little to suggest that expanded or universal access would reduce overall wasteful spending in the United States. It is important to consider then the potential that even if universal access is achieved, some categories of wasteful spending may remain unaddressed or underaddressed. Viewed differently, addressing existing wasteful spending and reinvesting the $1800 to $5700 or more per person per year could fund meaningful amounts of value-added medical care for those who currently lack or have inadequate coverage. So, despite slower increases in medical care expenditure growth since the introduction of the ACA, substantial work remains. A standardized, well-described, and universally accepted set of categories would be most useful to organize policy and practice initiatives, develop valid tracking mechanisms, and monitor progress over time. There is a critical need for timely and regular data sources to accurately track indicators of wasteful spending, perhaps integrated into the Centers for Medicare and Medicaid Services (CMS) annual national health expenditure monitoring processes. Both NASEM and CMS could play a vital role in defining benchmark targets and providing data to assess progress toward reduction of waste.
While these needs and challenges can sound imposing, it is important to reiterate the scale of the problem. The ongoing COVID-19 pandemic has exposed the consequences of pervasive systemic inequities and has already begun to reshape medical care. The tragedy can provide the impetus for significant policy change. Eliminating or even substantially reducing wasteful medical care spending could be an opportunity to fundamentally reshape our nation’s medical care system, economy, and allocation of societal resources. Making progress on a single subset of the categories of waste described here would also yield cost savings that could facilitate enactment of an expansive set of new initiatives to improve the health of the US population. To make such fundamental change at the system level requires a change in will from policymakers and the population at large. Were elected officials—prodded by employers, nonprofits, and policy organizations—to fully recognize and muster the strength to take on the magnitude of waste borne by everyone, to understand that eliminating waste does not mean eliminating valuable clinical services, and to discern all the benefits they could receive were these resources redirected to priorities that add value and meaning to their lives, we could begin the journey to real change.
ACKNOWLEDGMENTS
We thank members of the National Academies of Sciences, Engineering, and Medicine Roundtable on Population Health Improvement’s Health Care Expenditures Collaborative for productive discussions on the article.
CONFLICTS OF INTEREST
None of the authors declare any potential conflicts of interest.
HUMAN PARTICIPANT PROTECTION
This study did not involve human participants.
Footnotes
REFERENCES
- 1.Sisko AM, Keehan SP, Poisal JA et al. National health expenditure projections, 2018-27: economic and demographic trends drive spending and enrollment growth. Health Aff (Millwood) 2019;38(3):491–501. doi: 10.1377/hlthaff.2018.05499. [DOI] [PubMed] [Google Scholar]
- 2.Papanicolas I, Woskie LR, Jha AK. Health care spending in the United States and other high-income countries [erratum in JAMA. 2018;319(17):1824] JAMA. 2018;319(10):1024–1039. doi: 10.1001/jama.2018.1150. [DOI] [PubMed] [Google Scholar]
- 3.Yong PL, Saunders RS, Olsen LA, editors. The Healthcare Imperative: Lowering Costs and Improving Outcomes: Workshop Series Summary. Washington, DC: National Academies Press; 2010. [PubMed] [Google Scholar]
- 4.Berwick DM, Hackbarth AD. Eliminating waste in US health care. JAMA. 2012;307(14):1513–1516. doi: 10.1001/jama.2012.362. [DOI] [PubMed] [Google Scholar]
- 5.Mashaw JL, Marmor TR. Conceptualizing, estimating, and reforming fraud, waste, and abuse in healthcare spending. Yale J Regul. 1994;11:455–494. [Google Scholar]
- 6.McCullough JC, Zimmerman FJ, Fielding JE, Teutsch SM. A health dividend for America: the opportunity cost of excess medical expenditures. Am J Prev Med. 2012;43(6):650–654. doi: 10.1016/j.amepre.2012.08.013. [DOI] [PubMed] [Google Scholar]
- 7.The price of excess: identifying waste in healthcare spending. PricewaterhouseCoopers’ Health Research Institute; 2008. [Google Scholar]
- 8.Kelley R. Where can $700 billion in waste be cut annually from the US healthcare system? Ann Arbor, MI: Thomson Reuters; 2009. p. 24. [Google Scholar]
- 9.Fredell MN, Kantarjian HM, Shih YT, Ho V, Mukherjee B. How much of US health care spending provides direct care or benefit to patients? Cancer. 2019;125(9):1404–1409. doi: 10.1002/cncr.31865. [DOI] [PubMed] [Google Scholar]
- 10.Shrank WH, Rogstad TL, Parekh N. Waste in the US health care system: estimated costs and potential for savings. JAMA. 2019;322(15):1501. doi: 10.1001/jama.2019.13978. [DOI] [PubMed] [Google Scholar]
- 11.Figueroa JF, Wadhera RK, Jha AK. Eliminating wasteful health care spending—is the United States simply spinning its wheels? JAMA Cardiol. 2019 doi: 10.1001/jamacardio.2019.4339. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 12.McCullough JM, Speer M, Teutsch SM, Fielding JE. Non-clinical prevention opportunities and waste in the US healthcare system. Am J Prev Med. 2019;56(6):904–907. doi: 10.1016/j.amepre.2018.11.023. [DOI] [PubMed] [Google Scholar]
- 13.American Diabetes Association. Economic costs of diabetes in the US in 2017. Diabetes Care. 2018;41(5):917–928. doi: 10.2337/dci18-0007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Barbier EB. How to make the next Green New Deal work. Nature. 2019;565(7737):6. doi: 10.1038/d41586-018-07845-5. [DOI] [PubMed] [Google Scholar]
- 15.Woolf SH, Schoomaker H. Life expectancy and mortality rates in the United States, 1959–2017. JAMA. 2019;322(20):1996–2016. doi: 10.1001/jama.2019.16932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pacala S, Socolow R. Stabilization wedges: solving the climate problem for the next 50 years with current technologies. Science. 2004;305(5686):968–972. doi: 10.1126/science.1100103. [DOI] [PubMed] [Google Scholar]
- 17.Burwell SM. Setting value-based payment goals—HHS efforts to improve US health care. N Engl J Med. 2015;372(10):897–899. doi: 10.1056/NEJMp1500445. [DOI] [PubMed] [Google Scholar]
- 18.Buntin MB, Graves JA. How the ACA dented the cost curve. Health Aff (Millwood). 2020;39(3):403–412. doi: 10.1377/hlthaff.2019.01478. [DOI] [PubMed] [Google Scholar]
- 19.Chernew ME, Conway PH, Frakt AB. Transforming Medicare’s payment systems: progress shaped by the ACA. Health Aff (Millwood) 2020;39(3):413–420. doi: 10.1377/hlthaff.2019.01410. [DOI] [PubMed] [Google Scholar]
- 20.Robinson JC, Brown TT, Whaley C. Reference pricing changes the “choice architecture” of health care for consumers. Health Aff (Millwood) 2017;36(3):524–530. doi: 10.1377/hlthaff.2016.1256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brook RH, Keeler EB, Lohr KN . The health insurance experiment: a classic RAND study speaks to the current health care reform debate. Santa Monica, CA: RAND Corporation; 2006. [Google Scholar]
- 22.Song Z, Rose S, Safran DG, Landon BE, Day MP, Chernew ME. Changes in health care spending and quality 4 years into global payment. N Engl J Med. 2014;371(18):1704–1714. doi: 10.1056/NEJMsa1404026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Woolhandler S, Himmelstein DU. Single-payer reform—“Medicare for All. JAMA. 2019;321(24):2399–2400. doi: 10.1001/jama.2019.7031. [DOI] [PubMed] [Google Scholar]


