Abstract
Objectives. To quantify changes in US health care spending required to reach parity with high-resource nations by 2030 or 2040 and identify historical precedents for these changes.
Methods. We analyzed multiple sources of historical and projected spending from 1970 through 2040. Parity was defined as the Organisation for Economic Co-operation and Development (OECD) median or 90th percentile for per capita health care spending.
Results. Sustained annual declines of 7.0% and 3.3% would be required to reach the median of other high-resource nations by 2030 and 2040, respectively (3.2% and 1.3% to reach the 90th percentile). Such declines do not have historical precedent among US states or OECD nations.
Conclusions. Traditional approaches to reducing health care spending will not enable the United States to achieve parity with high-resource nations; strategies to eliminate waste and reduce the demand for health care are essential.
Public Health Implications. Excess spending reduces the ability of the United States to meet critical public health needs and affects the country’s economic competitiveness. Rising health care spending has been identified as a threat to the nation’s health. Public health can add voices, leadership, and expertise for reversing this course.
In its 2012 report For the Public’s Health: Investing in a Healthier Future, the Institute of Medicine (IOM; now the National Academy of Medicine and the Health and Medicine Division of the National Academies of Sciences, Engineering, and Medicine) recommended that the secretary of the US Department of Health and Human Services adopt an explicit life expectancy target and establish a specific per capita health expenditure target to be achieved by 2030. The report specifically noted that efforts to reach these targets “should engage all health system stakeholders in actions intended to achieve parity with averages among comparable nations on healthy life expectancy and per capita health expenditures.”1(p4)
In a recent analysis, Kindig et al. explored the plausibility of meeting the life expectancy target by 2030.2 They found that to achieve parity with the United Nations’ projected 2030 mortality estimates for Western Europe, US life expectancy would have to increase by 0.32% per year between 2016 and 2030.2 Although this rate is high, it does have at least some historical precedent among Organisation for Economic Co-operation and Development (OECD) nations and US states.
Similar analyses have not been undertaken to determine the plausibility of achieving the IOM’s health care spending parity target. This is an especially important evidence gap given that the United States has spent more per person on health care than every other wealthy nation since 1976.3 In 2018, total health care spending in the United States rose to $3.6 trillion, or $11 172 per person.4 The second and third highest spending nations—Switzerland and Norway—spent US$7317 and US$6187 per capita on health care, respectively. Other high-income countries spent much less; the median expenditure among the 34 OECD member countries in 2018 was US$4342, about 39% of US spending.
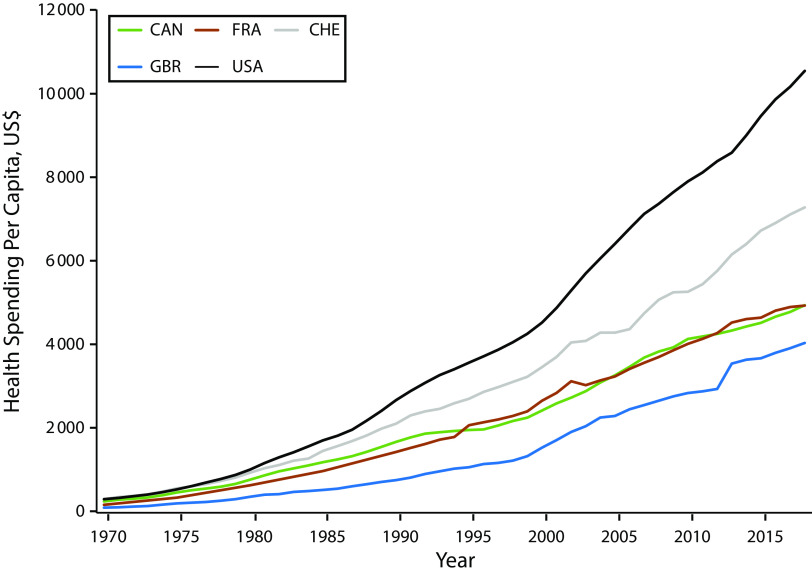
The growing divergence in spending between the United States and the other OECD nations has been attributed to a range of potential factors,5 including higher prices in the United States for labor, goods, services, and administration of health care6,7; greater intensity of services provided8; differences in social spending9; and the practice of “defensive medicine.”10 Figure 1 illustrates the historical trend of spending in the United States relative to 3 other high-income countries. Full historical comparisons between all OECD member countries are available in the Appendix (see Figure A, available as a supplement to the online version of this article at http://www.ajph.org). Unfortunately, this divergence in health care spending is not producing commensurate value (Figure B, available as a supplement to the online version of this article at http://www.ajph.org). US health outcomes lag behind those of other OECD nations,11 and gaps in life expectancy between the United States and other OECD nations continue to grow.2
FIGURE 1—
Total Health Spending per Capita in Selected OECD Nations, 1970–2018
Note. OECD = Organisation for Economic Co-operation and Development. The countries included are Canada (CAN), France (FRA), Switzerland (CHE), Great Britain (GBR), and the United States. All US spending totals are adjusted for inflation to 2018 US dollars. All international spending totals are purchasing power parity adjusted to 2018 US dollars. An alternative measure of health care spending is the percentage of a nation’s gross domestic product devoted to health care (see Figure C, available as a supplement to the online version of this article at http://www.ajph.org). When viewed graphically these 2 measures, although conceptually distinct, represent similar views of US health care spending in comparison with OECD nations over the time period assessed.
Health care spending constitutes an increasingly large share of the US economy, so reaching spending parity could have important effects on the country’s international competitiveness. We therefore assess the feasibility of achieving the IOM’s spending parity target. Because nearly a decade has passed since the original target was recommended, we extend the window for meeting this target to 2040, focusing on a pair of questions. First, what level of decline (in terms of both total dollars and percentage decrease) in US health care spending would be required to reach parity with high-resource nations (i.e., the 50th percentile [median] or 90th percentile of OECD spending) by 2030 or 2040? Second, is this decline in health care spending plausible on the basis of historical precedent, either at the state level or among other high-resource nations?
METHODS
We analyzed both historical and projected health care expenditures within the United States and among other high-resource nations. We chose the 34 OECD countries to provide relevant comparisons with the United States and also to maintain consistency with the Kindig et al. analysis of the life expectancy target.2 We compiled secondary data from 3 sources to measure health care spending: OECD,12 the Institute for Health Metrics and Evaluation,13 and the Centers for Medicare and Medicaid Services.4,14 All international spending totals are purchasing power parity adjusted to 2018 US dollars. Expenditure projections for 2030 were obtained from OECD,12 and 2040 projections were obtained from the Institute for Health Metrics and Evaluation.13 Additional details on the approaches and methods used by OECD and the Institute for Health Metrics and Evaluation to generate these projections are available in the Appendix and from the organizations directly.12,13 We use Centers for Medicare and Medicaid Services National Health Expenditure data when reporting US spending in 2018 or 2019.4,14
We used available OECD spending projections to assess changes needed to reach spending parity with OECD nations by 2030.12 OECD projections are produced across a range of policy situations. These situations include a “base” scenario—estimates of health care spending growth in the absence of major policy changes—and a number of alternative scenarios that model the impact on health care spending of policies that increase productivity or contribute to better lifestyles or, conversely, ineffective policies that contribute to additional cost pressures on health systems. For the purposes of our analyses, we used the base scenario projections. The Appendix contains results obtained with alternative OECD scenario projections as a means of exploring the sensitivity of our findings to such projections.
To assess changes needed to reach spending parity with OECD nations by 2040, we obtained 2017 to 2050 health spending data for all 34 OECD countries from the Institute for Health Metrics and Evaluation’s Financing Global Health 2017 database.13 These spending totals are inclusive of government health spending from domestic sources, prepaid private health spending, out-of-pocket health spending, and the financial and in-kind resources transferred from development agencies to low-income and middle-income nations.13
We calculated spending changes necessary to reach parity with OECD member nations under several scenarios. We considered parity to be matching either the median (50th percentile) or 90th percentile spending thresholds among the 34 OECD member countries. Defining parity as the 90th percentile would be the more feasible goal, with the 50th percentile more in line with the IOM’s original recommendation. Our main analyses centered around the annual declines that the United States would have to realize to reach parity with other OECD nations, assuming that those nations continue to experience growth as currently projected by the OECD. We present annual percentage changes and per capita spending changes needed to reach the median and 90th percentiles of the OECD nations by both 2030 (90th percentile country: Ireland) and 2040 (90th percentile country: Norway).
A secondary analysis examined a separate scenario. Using assumptions, data inputs, and calculation strategies similar to those outlined thus far, we calculated how long the United States would need to sustain zero health care spending growth (meaning a $0 change in spending each year) for the OECD nations to reach parity with current US spending levels. In our analysis, we assumed that those nations continue to experience spending growth as currently projected by the OECD. Additional information on future spending projections can be found in the Appendix.
Health care spending as a percentage of gross domestic product (GDP) could also be used to assess parity; however, this strategy requires projections of GDP as well as health care spending, and such projections are not available. Historical projections among OECD nations are shown in Figure C (available as a supplement to the online version of this article at http://www.ajph.org). In 2018 the United States spent 17% of its GDP on health care, as compared with 9% in the median OECD nation (Finland) and 11% in the 90th percentile OECD nation (Germany). Thus, whether measured as a percentage of GDP or in dollars, the United States had a large spending gap relative to other OECD nations as of 2018.
RESULTS
In 2018, the United States spent $11 172 per person on health care. Finland (the median OECD nation) spent $4338, and Switzerland (the 90th percentile OECD nation) spent $7702. For the United States to achieve parity with median OECD health care spending by 2030, health care expenditures in the country would need to decline by 7.0% each year until 2030 (Table 1 ). Put another way, reaching this goal would require an average annual decline of $575 per person each year until 2030. For the United States to reach the 90th percentile of OECD nations, an annualized spending decline of 3.2% (or an average of $317 per person per year) by the same year would be necessary. Calculation details can be found in the Appendix (Table F, available as a supplement to the online version of this article at http://www.ajph.org).
TABLE 1—
Per Capita Health Care Spending Decreases Needed to Achieve Parity With OECD Nations by 2030 or 2040
| Parity Target Among OECD Member Countries | Target per Capita Spending Amount, US$ | Annual Decline Necessary to Achieve Spending Parity, % | Annual Average Decline Necessary to Achieve Spending Parity, US$ |
| 2030a | |||
| Median | 5230 | −7.0 | −575 |
| 90th percentile | 8068 | −3.2 | −317 |
| 2040b | |||
| Median | 5775 | −3.3 | −275 |
| 90th percentile | 8816 | −1.3 | −131 |
Note. OECD = Organisation for Economic Co-operation and Development.
Calculations performed with OECD health spending data and projections.
Calculations performed with Institute for Health Metrics and Evaluation global expected health spending data and projections.
If the target date for OECD parity is pushed back to 2040, US health care spending would need to decline by 3.3% ($275 per person) each year to achieve parity with the OECD median or 1.3% ($131 per person) each year to match the 90th percentile among OECD member countries.
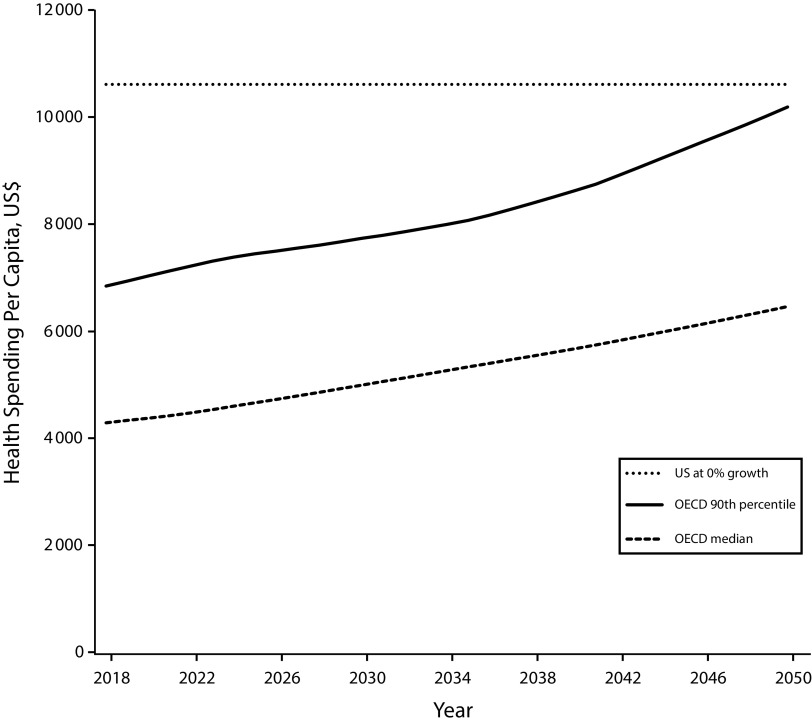
An alternative path to the United States achieving spending parity with other OECD nations involves the country ceasing all growth in spending (as of 2018) while other nations continue to experience increases. Figure 2 contrasts no growth in US spending (shown in the figure as a dashed line) with 2 different thresholds of OECD member countries’ per capita health care spending projections: 90th percentile growth (dark gray line) and median growth (light gray line). Spending projections were available only through 2050, and at that point the United States still would not have reached the 90th percentile of OECD nations’ per capita health care spending even if all spending growth stopped as of 2018. Using 2019 US health care spending estimates as the baseline also delays parity until 2050 or later.
FIGURE 2—
Hypothetical Health Care Spending Comparison From 2018 to 2050 Assuming That All US Spending Growth Stopped as of 2018 and Spending Trends Among Various Percentiles of Organisation for Economic Co-operation and Development (OECD) Nations Continued
To explore the plausibility of achieving spending reductions of the magnitude calculated here, we examined 1224 periods of health care spending for the 50 states and the District of Columbia from 1991 to 2014. Of these 1224 periods, only 7 saw year-over-year personal health spending declines of any magnitude (the full list of periods with spending declines is provided in Table G, available as a supplement to the online version of this article at http://www.ajph.org). No states experienced declines in health care spending over consecutive years, even during the 2008 to 2010 recession. Even if sustained, none of the individual spending declines during these periods would be sufficient to achieve parity with OECD nations by 2030 or 2040. Figure D (available as a supplement to the online version of this article at http://www.ajph.org) shows monotonic increases in US census region spending. Although substantial regional differences exist, annual health care spending is far in excess of OECD median and 90th percentile spending even in the lowest-spending region.
Internationally, 25 of 34 OECD nations recorded at least 1 year-over-year decline in per capita spending from 1970 to 2018. Over the 1434 periods examined, 71 countries (5%) exhibited a decline of any magnitude. Iceland (2008–2010), Luxembourg (2009–2011), Portugal (2010–2012), and Turkey (1993–1995) had 3-year sustained declines in per capita health spending of 1.3% or greater. Greece had the longest sustained decline in spending (7 years; 2008–2014), followed by Finland (4 years; 1991–1994).
DISCUSSION
Although spending far more per person on health care, the United States consistently lags behind other high-resource nations in terms of life expectancy. In 2012, the IOM recommended that the secretary of the US Department of Health and Human Services set a goal of reaching parity in both life expectancy and health care spending with other high-resource nations by 2030. Previous work suggests that achieving the level of gains in life expectancy necessary to achieve the IOM’s goal would be challenging but achievable.2 We assessed the feasibility of attaining the IOM’s health spending goal.
Our findings reaffirm that the United States far exceeds other wealthy nations in health care spending. Reaching the ambitious OECD median in health care spending by 2030 would require the country to decrease spending by 7.0% annually. This is an unprecedented rate that has not been achieved at the state or national level over any period during the past several decades other than by countries experiencing severe economic challenges. Internationally, there are no prolonged spending declines that can be primarily attributed to health reform efforts. The early 1990s were a period of significant economic turmoil in Turkey as a result of the Kurdish–Turkish conflicts. Spending declines in Iceland, Luxembourg, and Portugal all occurred during economic recessions, although Luxembourg undertook some system reforms.15 Elsewhere, the sovereign debt crisis in Greece and the serious economic crisis in Finland are the likely drivers of their respective declines rather than concerted efforts to curb spending on health care.16,17
A more modest parity target—reaching the 90th percentile of OECD nations by 2040—would still require sustained annual spending declines of 1.3% annually through 2040. In short, achieving spending parity with other OECD member countries by 2030 will require more than stagnant US health expenditures. Even if spending growth were to stop, several decades of growth among other OECD nations would be required before the United States reached parity.
The current COVID-19 pandemic may ultimately affect health care spending or the overall economy more or less than these historical crises.18 The pandemic may prod the United States to make meaningful changes in health care. It is too soon to know how health care spending in the United States may change relative to that in other OECD nations, an important consideration for how readily the country can achieve parity with other nations.
Although achieving per capita spending parity is ambitious, there are major opportunities for reducing spending that could contribute to progress toward that goal. Rationing of health care is unlikely to be a popular or plausible solution. However, to the degree that prices rather than volume contribute to US spending levels, price reductions should encounter less resistance to rationing concerns than volume restrictions often encounter. Waste in health care spending in the United States is extraordinary, with an estimated $600 billion to $1.9 trillion ($1800 to $5700 per capita) per year not contributing to improved health outcomes.19–21 For comparison, the difference between the lowest spending US region (the Rocky Mountain region; $6814 in 2014) and the 90th percentile OECD nation (New Zealand; $4955 in 2014) is $1869 per capita. Reducing wasteful spending may offer a path toward the goal of achieving ambitious spending parity targets.
Waste has been shown to arise from a number of sources, including pricing failures, administrative complexities, overtreatment or low-value care, and fraud and abuse.19–21 Eliminating this waste would be a major step toward achieving parity with other wealthy nations and, by definition, would have no deleterious effects on the public’s health. Others have examined sources of waste and their opportunity costs in greater detail.22,23 We recognize that whereas waste is rightfully considered a major problem at the system level, this spending represents income to many system stakeholders; one person’s expenditure is another’s revenue. Although painful for stakeholders who benefit from this waste, if we explored other industries’ approach to “just transitions,” an appropriate reduction of waste would represent progress toward the IOM’s formidable spending parity goal.
Regional differences in the United States are also substantial and suggest that organization, delivery, and pricing of care in low-cost areas could serve as models for other parts of the nation. Achieving these reductions requires responsible protections for populations that underuse value-added services, especially disadvantaged populations.
In addition, it is important to maintain a distinction between intensive (i.e., level of service use) and extensive (i.e., proportion of the population with coverage) margins of health care provision across the diverse US landscape. Prices and the proportion of the population with insurance coverage vary by state. The goal of determining and working toward a plausible spending target is not to deprive individuals of health care but to ensure the long-term viability of a system that can afford equitable and universal access to health. Our analyses considered spending per capita (total spending divided by total population), which assumes that everyone is served. People who are not covered still incur health care costs, but it is important to make clear that removing access to necessary care is not a preferred path toward reduced health care spending. Furthermore, given that most other OECD nations already offer nearly universal coverage, it is perhaps worth considering whether a more viable path would be to look for ways to increase access.
As argued by Zimmerman, health care spending in the United States has reached the point at which more spending may actually be reducing life expectancy.23 Moreover, wasteful spending is an enormous tax on the US people. The nation’s international competitiveness suffers from the waste of hundreds of billions of dollars,21 resources that could be deployed more productively by the private and not-for-profit sectors.22 There is an enormous opportunity cost in terms of unimplemented interventions that could actually improve health, such as those focused on improving the environment and adverse social conditions. Others have calculated that reallocation of wasteful health care spending to social programs could prevent thousands of premature deaths annually.24 Some may be concerned that lowering health spending will deprive people of needed care through either underuse or lack of coverage. By decreasing waste appropriately, however, health care dollars can be unleashed to address policy priorities that affect the public’s health, including underuse of certain health care services, inequities in health outcomes, expansion of health care access, and other priorities.
Conclusions
We examined historical health care spending growth among OECD nations and within US states to assess the feasibility of achieving the IOM’s 2012 spending parity target and the changes needed to reach that target. Reaching parity will require unprecedented health care spending declines, declines that have not been achieved at the state or national level over any period during the past several decades except among countries experiencing severe economic challenges. Traditional approaches to reducing health care expenditures will not enable the United States to achieve parity with high-resource nations; strategies to eliminate waste and reduce the demand for health care are essential.
Public Health Implications
Significant declines in US health care expenditures are required to reach parity (i.e., median or 90th percentile) with high-resource nations by 2030 or 2040. Sustained spending declines of such magnitude are unprecedented, both at the US state level and nationally among other OECD member countries. Nonetheless, significant movement toward these goals is achievable if, as a nation, we are willing to confront heretofore intractable vested interests to eliminate waste and improve awareness among the population about the toll this waste places on each individual. Reallocating these resources to policies and programs that improve health equity can build more resilient communities and lower long-term health care costs.
We need to mobilize public opinion. Setting a target for achieving parity, as the IOM recommends, would be an important first step in mobilizing the public and policymakers and facilitating the creation of a national strategy to eliminate waste. Not all spending is the same, so identifying and protecting expenditures in which dollars should not be cut (e.g., prevention, immunizations, ensuring equity) is an important part of that roadmap, along with efforts to continue to create universal coverage.
The first recommendation of For the Public’s Health is setting targets for life expectancy and per capita costs.1 The wisdom of the report authors in linking these 2 targets is clear. Rising per capita health care costs erode federal, state, and family budgets. Less money is available for investments in other determinants of health, such as education, job development, housing, and environmental issues, as well as necessary infrastructure such as public health; all of these factors contribute to better life expectancy in a population. Of great concern, we will not have additional dollars for investments to improve equity, especially in the first years of life.
For the Public’s Health identifies unsustainable, rising health care costs as a threat to the nation’s health. It does not serve us well to continue to ignore this risk, and public health can add voices, leadership, and expertise for reversing this course.
ACKNOWLEDGMENTS
This work grew out of discussions at the National Academies of Sciences, Engineering, and Medicine (NASEM) Health Care Expenditure Collaborative, an activity associated with the NASEM Roundtable on Population Health Improvement.
We thank Elinore Faustino for editorial assistance.
Note. The conclusions presented are those of the authors and do not necessarily reflect the official position of the NASEM Roundtable on Population Health Improvement Health Care Expenditure Collaborative or its individual members.
CONFLICTS OF INTEREST
None of the authors declare any potential conflicts of interest.
HUMAN PARTICIPANT PROTECTION
No protocol approval was needed for this study because no human participants were involved.
Footnotes
REFERENCES
- 1.Institute of Medicine. For the Public’s Health: Investing in a Healthier Future. Washington, DC: National Academies Press; 2012. [PubMed] [Google Scholar]
- 2.Kindig D, Nobles J, Zidan M. Meeting the Institute of Medicine’s 2030 US life expectancy target. Am J Public Health. 2018;108(1):87–92. doi: 10.2105/AJPH.2017.304099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Organisation for Economic Co-operation and Development. Health expenditure indicators. Available at: https://www.oecd-ilibrary.org/content/data/data-00349-en. Accessed January 20, 2020.
- 4.Sisko AM, Keehan SP, Poisal JA et al. National health expenditure projections, 2018–27: economic and demographic trends drive spending and enrollment growth. Health Aff (Millwood) 2019;38(3):491–501. doi: 10.1377/hlthaff.2018.05499. [DOI] [PubMed] [Google Scholar]
- 5.Bentley TG, Effros RM, Palar K, Keeler EB. Waste in the US health care system: a conceptual framework. Milbank Q. 2008;86(4):629–659. doi: 10.1111/j.1468-0009.2008.00537.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Papanicolas I, Woskie LR, Jha AK. Health care spending in the United States and other high-income countries. JAMA. 2018;319(10):1024–1039. doi: 10.1001/jama.2018.1150. [DOI] [PubMed] [Google Scholar]
- 7.Anderson GF, Hussey P, Petrosyan V. It’s still the prices, stupid: why the US spends so much on health care, and a tribute to Uwe Reinhardt. Health Aff (Millwood) 2019;38(1):87–95. doi: 10.1377/hlthaff.2018.05144. [DOI] [PubMed] [Google Scholar]
- 8.Dieleman JL, Squires E, Bui AL et al. Factors associated with increases in US health care spending. JAMA. 1996–2013;2017;318(17):1668–1678. doi: 10.1001/jama.2017.15927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bradley E, Sipsma H, Taylor L. American health care paradox—high spending on health care and poor health. QJM. 2017;110(2):61–65. doi: 10.1093/gimed/hcw187. [DOI] [PubMed] [Google Scholar]
- 10.Reschovsky JD, Saiontz‐Martinez CB. Malpractice claim fears and the costs of treating Medicare patients: a new approach to estimating the costs of defensive medicine. Health Serv Res. 2018;53(3):1498–1516. doi: 10.1111/1475-6773.12660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schneider EC, Sarnak DO, Squires D, Shah A. Mirror, mirror 2017: international comparison reflects flaws and opportunities for better US health care. Available at: https://www.commonwealthfund.org/publications/fund-reports/2017/jul/mirror-mirror-2017-international-comparison-reflects-flaws-and. Accessed August 31, 2020.
- 12.Lorenzoni L, Marino A, Morgan D, James C. Health spending projections to 2030: new results based on a revised OECD methodology. Available at: https://www.oecd.org/officialdocuments/publicdisplaydocumentpdf/?cote=DELSA/HEA/WD/HWP(2019)3&docLanguage=En. Accessed August 31, 2020.
- 13.Chang AY, Cowling K, Micah AE et al. Past, present, and future of global health financing: a review of development assistance, government, out-of-pocket, and other private spending on health for 195 countries, 1995–2050. Lancet. 2019;393(10187):2233–2260. doi: 10.1016/S0140-6736(19)30841-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hartman M, Martin AB, Benson J, Catlin A. National health care spending in 2018: growth driven by accelerations in Medicare and private insurance spending. Health Aff (Millwood) 2020;39(1):8–17. doi: 10.1377/hlthaff.2019.01451. [DOI] [PubMed] [Google Scholar]
- 15.Docteur E, Oxley H. Health-care systems: lessons from the reform experience. Available at: https://www.oecd.org/els/health-systems/22364122.pdf. Accessed September 10, 2020.
- 16.Keskimäki I. How did Finland’s economic recession in the early 1990s affect socio-economic equity in the use of hospital care? Soc Sci Med. 2003;56(7):1517–1530. doi: 10.1016/S0277-9536(02)00153-3. [DOI] [PubMed] [Google Scholar]
- 17.Ifanti AA, Argyriou AA, Kalofonou FH, Kalofonos HP. Financial crisis and austerity measures in Greece: their impact on health promotion policies and public health care. Health Policy. 2013;113(1–2):8–12. doi: 10.1016/j.healthpol.2013.05.017. [DOI] [PubMed] [Google Scholar]
- 18.Glied S, Levy H. The potential effects of coronavirus on national health expenditures. JAMA. 2020;323(20):2001–2002. doi: 10.1001/jama.2020.6644. https://doi: 10.1001/jama.2020.6644. [DOI] [PubMed] [Google Scholar]
- 19.Speer M, McCullough JM, Teutsch SM, Fielding JE. Excess medical care spending: the categories, magnitude, and opportunity costs of wasteful spending in the United States. Am J Public Health. 2020;110(12):1743–1748. doi: 10.2105/AJPH.2020.305865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Berwick DM, Hackbarth AD. Eliminating waste in US health care. JAMA. 2012;307(14):1513–1516. doi: 10.1001/jama.2012.362. [DOI] [PubMed] [Google Scholar]
- 21.Shrank WH, Rogstad TL, Parekh N. Waste in the US health care system: estimated costs and potential for savings. JAMA. 2019;322(15):1501–1509. doi: 10.1001/jama.2019.13978. [DOI] [PubMed] [Google Scholar]
- 22.McCullough JC, Zimmerman FJ, Fielding JE, Teutsch SM. A health dividend for America: the opportunity cost of excess medical expenditures. Am J Prev Med. 2012;43(6):650–654. doi: 10.1016/j.amepre.2012.08.013. [DOI] [PubMed] [Google Scholar]
- 23.Zimmerman FJ. Less health care, more health: the inverse U of medical spending and health in the United States. Am J Public Health. 2020;110(12):1755–1757. doi: 10.2105/AJPH.2020.305981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tran LD, Zimmerman FJ, Fielding JE. Public health and the economy could be served by reallocating medical expenditures to social programs. SSM Popul Health. 2017;3:185–191. doi: 10.1016/j.ssmph.2017.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]