The coronavirus disease 2019 (COVID-19) pandemic has spanned over 213 countries and territories with more than 28 million confirmed cases and more than 912 000 deaths as of September 10, 2020.1 In Africa, the number of confirmed cases of COVID-19 as of the same date is more than 1 328 282 with 31 964 deaths.1 Although there are widespread fears that the COVID-19 pandemic may cause a staggering number of deaths in Africa,2 the total figures reported from the continent indicate otherwise. Plausible explanations are the relatively young age of the population and the inadequate testing capacity in many African countries.
In this context, Uganda has handled COVID-19 admirably. Uganda is an East African country with an estimated population of 43.3 million (July 2020) and a gross domestic product of US $26.6 billion.3 The Ugandan government demonstrated its preparedness to respond to COVID-19 before the country recorded its first case. The initial measures included restricting travel to and from high-risk countries; dispersing concentration points of people such as schools and colleges and religious, political, or social gatherings; and enforcing mandatory institutional quarantine of all incoming travelers.4
Uganda recorded its first COVID-19 case on March 22, 2020, 11 days after the World Health Organization declared COVID-19 a global pandemic.5 The first case triggered the Ugandan government to respond more aggressively by restricting public gatherings and imposing a curfew and a total travel ban into and out of the country, allowing only essential goods.4 As of September 10, 2020, Uganda has only 2179 active cases, 4101 confirmed cases, 1876 recoveries, and 46 COVID-19–related deaths.4 It has the seventh lowest number of cases (89) per million population in Africa (after Burkina Faso, Chad, Niger, Burundi, Western Sahara, and Tanzania) and the fourth lowest number of COVID-19–related deaths (1.0) per million population, with some of the countries with lower numbers (Tanzania and Burundi) having questionable data.1
SUCCESSFUL UGANDAN COVID-19 RESPONSE FACTORS
The government of Uganda had an effective national response strategy including risk communication, testing, contact tracing at district and community levels, and implementing physical and social distancing measures. Before recording their first COVID-19 case, the Ugandan government through the Ministry of Health used the “window of opportunity” (being one of the last countries to record a COVID-19 case) to act early by establishing preventive measures. This entailed screening all incoming travelers at ports of entries, training and preparing health workers, and repurposing hospitals to manage COVID-19 cases.4
Risk Communication
The COVID-19 risk communication was transparent, consistent, and inclusive. The government adopted mainstream, social, and print media for their public health messaging. The president held periodic press briefings to manage public perception and deliver situation reports about the pandemic. The COVID-19 Response Committee, led by the prime minister, coordinated the testing, contact tracing, and response in collaboration with districts and local councils (the smallest administrative unit in the country), the Uganda Virus Research Institute, and other relevant stakeholders (Figure 1).
FIGURE 1—
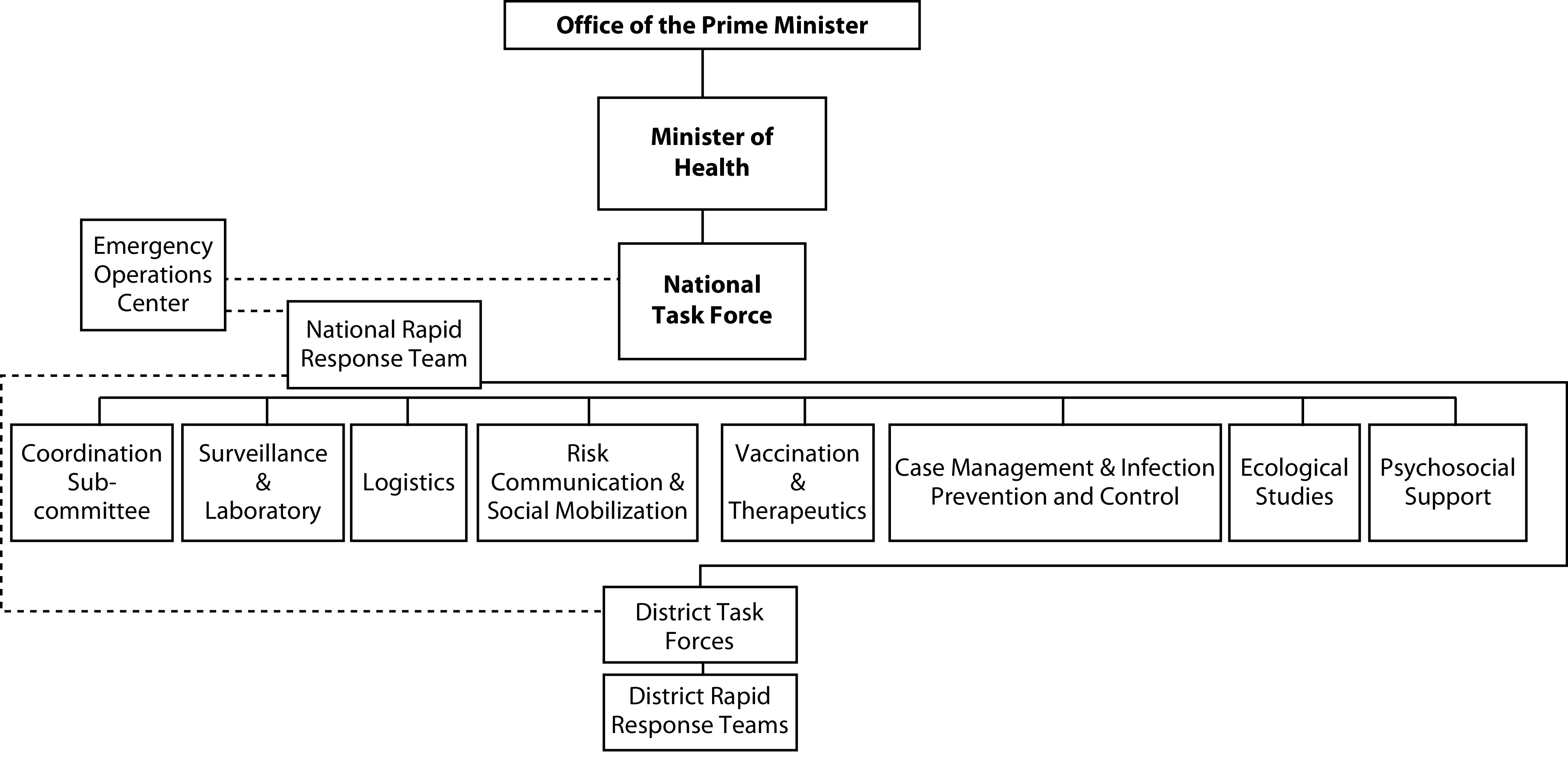
Organizational Structure for Managing Disease Outbreaks in Uganda
Testing
Uganda has the eighth highest number of people tested in Africa.1 The positivity rate of daily tests conducted in Uganda was consistently less than 5%; the cumulative positivity rate of tests done (417 897) versus the confirmed cases (4101) as of September 10, 2020, was 0.98%.4 Furthermore, Uganda has carried out 9084 tests per million population1 compared with an average 8932 tests per million population in Africa. However, the tests per million population in Africa is affected by tests in countries with very small populations such as Mauritius, Cape Verde, Djibouti, and Mayotte or countries with very high COVID-19 cases such as South Africa and Morocco.
District Task Forces
The government of Uganda set up district task forces in all 134 districts of Uganda. In many districts, the district task forces have taken several initiatives to drive their COVID-19 response strategies, including updating risk communication strategies, increasing awareness through mainstream and social media, conducting social mobilization activities, distributing information and educational and communication materials in local languages, and facilitating community dialogue and engagement activities.6
Community-Based Disease Surveillance
The Ugandan government established a community-based disease surveillance (CBDS) and contact tracing model that comprised a diverse group of health professionals. The CBDS is lauded as a game changer in the COVID-19 response.6 For example, the CBDS has been most effective in detecting COVID-19 cases at the border districts. Specifically, in Rakai District, the first four community cases were detected through the vigilance of village health teams and local councils by using CBDS guidelines. Evidence shows that positive cases and contacts have been detected through CBDS in several districts including border communities.6 The CBDS was largely successful because of the strong administrative structures in Uganda at the village and grassroots levels.
Gradual Lifting of Restrictions
The government of Uganda has been lifting restrictions gradually since May 4, 2020, with a phased transition to reopen the economy. Most important, as of September 10, 2020, restrictions are in place regarding public, religious, and social gatherings.4 This contrasts with other countries like Nigeria—currently lifting restrictions despite increasing numbers of cases and deaths. Furthermore, the government made wearing of masks in public settings mandatory and is currently distributing face masks to all households across the 134 districts in Uganda.4
Lessons Learned
Although some Asian countries such as South Korea, Vietnam, and Taiwan are considered as exemplary around the world in their public health response to COVID-19,7 we believe that the Ugandan response, in both African and global contexts, is equally commendable, and it teaches us that the economic standing (high or low income) of a country does not necessarily determine preparedness for pandemics. This is true not only for countries in Africa such as Nigeria, South Africa, and Egypt (the top three economies and the three countries with the most COVID-19 cases) but also for high-income countries such as the United States and the United Kingdom.
We emphasize that dealing with a pandemic in the twenty-first century requires a coordinated national strategy with multistakeholder and multifaceted approaches revolving around effective leadership; evidence-based risk communication; and strategic public health interventions such as mass testing, contact tracing, isolation and quarantining of affected individuals, hand hygiene, and social distancing measures.
The Uganda Virus Research Institute has been actively responding to disease outbreaks in other parts of Africa. The institute’s experience, coupled with the existence of a strong pool of local experts who are very knowledgeable in handling highly infectious organisms and a clear structure for public health emergency response within the Ministry of Health, played a major role in making Uganda’s response to COVID-19 successful.
Almost 80% of COVID-19 cases in Uganda are caused by truck drivers from neighboring countries.4 In case of a second wave of COVID-19, the Ugandan government will need a clear strategy to address this risk. We also stress that people with other diseases and pregnant women need more attention to avoid a spike in mortalities and morbidities from pregnancy and other diseases.
CONCLUSIONS
Overall, Uganda is rated highly in handling the COVID-19 pandemic in Africa compared with countries such as Nigeria, South Africa, and Egypt. Because of the large, informal urban settlements and rural areas of Africa, a successful pandemic response is dependent on success being recorded in these communities. This includes robust testing, contact tracing, clear risk communication strategies, gradual easing of restrictions, hand hygiene, and personal protective equipment.
Other African countries can learn from the Ugandan model of pandemic containment, especially in the event of a second wave of COVID-19 or another pandemic. We also underscore the critical role of building local capacity for effective pandemic response.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to disclose.
Footnotes
REFERENCES
- 1.Worldometer. COVID-19 coronavirus pandemic. August 2020. Available at: https://www.worldometers.info/coronavirus. Accessed September 10, 2020.
- 2.Baker A. Few doctors, fewer ventilators: African countries fear they are defenseless against inevitable spread of coronavirus. Time. April 7, 2020. Available at: https://time.com/5816299/coronavirus-africa-ventilators-doctors. Accessed July 6, 2020.
- 3.Central Intelligence Agency. The World Factbook: Uganda. July 2020. Available at: https://www.cia.gov/library/publications/the-world-factbook/geos/ug.html. Accessed July 28, 2020.
- 4.Ministry of Heath Uganda. COVID-19 status. August 2020. Available at: https://www.health.go.ug/covid/#Published. Accessed September 10, 2020.
- 5. Africanews. Uganda confirms first COVID-19 case. March 2020. Available at: https://www.africanews.com/2020/03/22/uganda-confirms-first-covid-19-case. Accessed June 15, 2020.
- 6.World Health Organization Africa. Uganda to win or lose COVID-19 war in communities. June 17, 2020. Available at: https://www.afro.who.int/news/uganda-win-or-lose-covid-19-war-communities. Accessed July 8, 2020.
- 7.Shokoohi M, Osooli M, Stranges S. COVID-19 pandemic: what can the West learn from the East? Int J Health Policy Manag. 2020 doi: 10.34172/ijhpm.2020.85. E-pub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]


