Abstract
Objective
We started an information technology (IT) system that encodes the medical treatment status of hepatitis B virrus (HBV) with a 9-digit number, automatically checks for inappropriate situations occurring due to immunosuppression and chemotherapy that do not comply with the flowchart of the hepatitis B countermeasure guideline, and promotes correct HBV medical treatment in our hospital. We conducted a prospective study of HBV reactivation using this system.
Methods
Among 21,607 cases that were managed using this system, 1,206 patients who were HBs antigen-negative, HBc antibody- and/or HBs antibody-positive and in whom HBV DNA quantification was performed two times or more were examined for the occurrence of HBV reactivation. The study population included: malignant lymphoma patients using rituximab (n=40), patients with malignant tumors using anticancer agents (n=546), patients treated with steroids (n=274), rheumatoid arthritis (RA) patients (n=144), patients using immunosuppressants/biologics (n=26), and patients undergoing hepatitis C direct acting antiviral (DAA) treatment (n=176).
Results
HBV reactivation was observed in 27 cases undergoing treatment with the following agents: rituximab (n=6), anticancer agents (n=8), steroids (n=10), anti-RA agents (n=1), and hepatitis C DAA (n=2). Among the 40 patients who were using rituximab, 6 (18.2%) showed a high rate of reactivation. In 10 in which HBV reactivation occurred at a median of 10 (range, 4-32) months after steroid administration, 6 occurred after the 7th month, and 1 patient showed HBs antigen positivity and severe hepatitis.
Conclusion
Continuing of the operation of an automatic check system using coded medical information to check for the reactivation enabled this prospective study of HBV reactivation. Careful attention should be paid to patients using steroids, as well as malignant lymphoma patients who are treated with rituximab. The results of the present study suggest that the present IT encoding system would be useful for preventing HBV reactivation.
Keywords: HBV reactivation, immunosuppression/chemotherapy, medical information coding, rituximab, steroids
Introduction
Various drugs are associated with hepatitis B virus (HBV) reactivation, including steroids, immunosuppressants (1, 2), anticancer agents (3, 4) molecular biologic agents (5, 6) anti-rheumatic agents (7), hepatitis C direct acting antivirals (DAAs) (8), and their target diseases are diverse. Hepatitis that develops due to HBV reactivation and progresses to fulminant hepatitis shows extremely high lethality. In Japan, measures are taken according to guidelines for measures against hepatitis B that develops due to immunosuppression/chemotherapy (9); however, the rate of compliance to the guidelines is low, especially among non-hepatic specialists who have very low awareness of HBV reactivation. We have been operating a system that automatically checks for HBV reactivation by encoding HBV-related medical information (10). Both non-hepatologists and hepatologists can automatically prevent HBV reactivation by using this system. This system also facilitates a prospective study on HBV reactivation in patients undergoing immunosuppressive chemotherapy. We examined the HBV reactivation status in our hospital over a 6-year period.
Materials and Methods
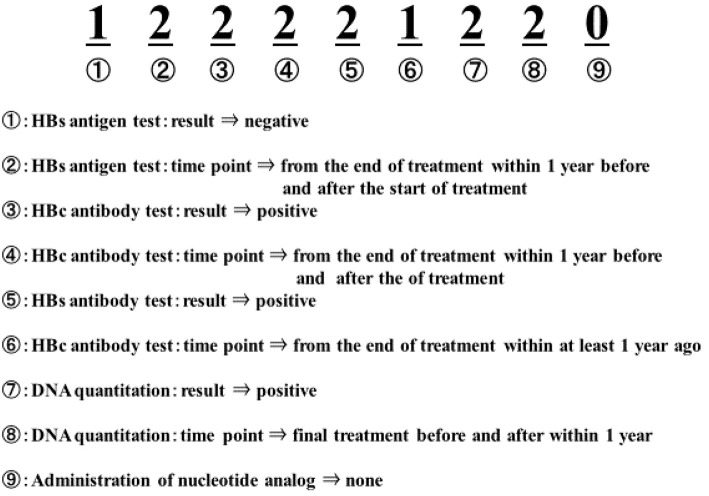
In our hospital, we encode the HBV treatment status of patients undergoing immunosuppressive chemotherapy with a 9-digit numerical value, and use a computer to automatically check for inappropriate situations that do not comply with the flowchart of hepatitis B countermeasure guidelines (Table 1, Fig. 1). The contents of the system have been described in a previous report (10). In target patients who received immunosuppressive therapy/chemotherapy within the past 1 year (including patients who completed treatment), the following 9 digit clinical information codes were assigned based on the HBs antigen, HBc/HBs antibody, and HBV-DNA quantitative test data from 1 year before and after the last day of administration of the therapeutic drug, test results, and the last day of administration of nucleoside analog preparations.
Table 1.
The Encoding of Patient Medical Records.
| HBs Ag test | HBc Ab test | HBs Ab test | Quantitative HBV DNA test | Nucleotide analog treatment | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| result | timing | result | timing | result | timing | result | timing | timing | |||||||||||||||||
| None | 0 | None | 0 | None | 0 | None | 0 | None | 0 | None | 0 | None | 0 | None | 0 | None | 0 | ||||||||
| Negative | 1 | More than 1 year before completion of the treatment | 1 | Negative | 1 | More than 1 year before completion of the treatment | 1 | Negative | 1 | More than 1 year before completion of the treatment | 1 | Negative | 1 | More than 1 year before completion of the treatment | 1 | Administered after an HBsAg or an HBV DNA test | 1 | ||||||||
| Positive | 2 | More than 1 year before and after completion of the treatment | 2 | Positive | 2 | Within 1 year before and after completion of the treatment | 2 | Positive | 2 | Within 1 year before and after completion of the treatment | 2 | Positive | 2 | Within 1 year before and after completion of the treatment | 2 | Not Admistered after an HBsAg or an HBV DNA test | 2 | ||||||||
| More than 1 month after the previous test | 3 | Within 1 year after completion of the treatment | 3 | ||||||||||||||||||||||
Figure 1.
Examples of medical record encoding. A 9-digit number is determined by encoding each of the following statuses with 0, 1, 2 and 3: test results and their measure timings for HBsAg, HBcAb, HBsAb, HBV-DNA, respectively, administration history of nucleotide analogue.
1st digit: HBs antigen test result 0=none, 1=present/negative, 2=present/positive
2nd digit: HBs antigen test report 0=no, 1=present, ≥1 year before the final day of treatment, 2=present within 1 year
3rd digit: HBc antibody test result 0=absent, 1=present/negative, 2=present/positive
4th digit: HBc antibody test report 0=no, 1=present, ≥1 year before the last day of treatment, 2=present within 1 year
5th digit: HBs antibody test result 0=none, 1=present/negative, 2=present/positive
Digits 6: HBs antibody test report 0=no, 1=present, ≥1 year before the final day of treatment, 2=present within 1 year
7th digit: HBVDNA test result 0=none, 1=present/negative, 2=present/positive
8th digit: HBVDNA test report 0=no, 1=present at least 1 year before the final day of treatment, 2=present at least 1 year, 3=present for more than 1 month since the last examination
9th digit: Administration of nucleic acid analog 0=no administration, 1=Administration after positivity for HBs antigen or HBV-DNA was detected, 2=no drug administration after positivity was detected, 3=within 1 year after the end of drug administration.
By encoding the status at each stage of the Hepatitis B Management Guideline in the same way and contrasting it with the patient's medical information code (9) (Fig. 2) we could determine whether the current status was not consistent with the proper medical care described in the flow chart of the Hepatitis B Management Guideline.
Figure 2.
Example of record encoding (speech balloon). Each of the statuses of the flow chart in the practical guidelines for hepatitis B is encoded in a 1 to 9 digit number with 0, 1, and 2.
In addition, we identified the status of improper medical practice based on each medical information code (Table 2).
Table 2.
Example of Suggested Instructions and Decisions Derived from the Patent Code Analyses.
| HBs antigen | HBs antibody | HBc antibody | HBV-DNA | Nucleotide analog | Current situation Improper medical practice | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Result | Timing | Result | Timing | Result | Timing | Result | Timing | Timing | |||||
| 1 | 2 | × | × | × | × | × | × | 2 | No nucleotide analog was adminstrated Consult hepatologist | ||||
| × | × | × | × | × | × | 2 | 2 | 2 | No nucleotide analog was adminstrated Consult hepatologist | ||||
| 1 | 2 | 2 | 2 | 1 | 2 | 0 | 0 | 0 | HBc antibody positive HBV-DNA was not measured | ||||
| 1 | 2 | 0 | 0 | 2 | 2 | 2 | 3 | 1 | >1 month after the start of nucleic acid analog HBV-DNA was not measured | ||||
| 2 | 1 | 1 | 2 | 1 | 2 | 1 | 3 | 0 | >1 month after HBV-DNA measurement HBV-DNA was not measured | ||||
| 1 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | HBs antigen negative HBc/HBs Ab was not measured | ||||
| 1 | 2 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | The timing of HBc/HBs antibody measurement is old. HBc/HBs Ab was not measured | ||||
| 1 | 2 | 0 | 0 | 1 | 2 | 0 | 0 | 0 | HBc antibody was not measured | ||||
| 1 | 2 | 1 | 2 | 0 | 0 | 0 | 0 | 0 | HBs antibody was not measured | ||||
| 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | HBs antigen was not measured | ||||
| 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | HBs antigen measurement is old HBs antigen was not measured | ||||
The obtained list of measures against hepatitis B was converted into instruction texts to promote the correction of improper situations that were not in compliance with the Guidelines for Measures against Hepatitis B, was prepared as a list of measures against hepatitis B, and the list was distributed to each physician. The physicians will be informed of any corrections that are listed.
The list was distributed once a month, and if necessary tests were not performed, the list was re-listed in the following month. The list of patients requiring nucleic acid analog treatment was also distributed to the liver pharmacist so that if the patient did not receive nucleic acid analog treatment, the liver pharmacist would call the attending physician directly to facilitate administration. The check interval was set to 1 month (3 months for anticancer drugs) according to the guideline. A system that encourages doctors to optimize HBV medical care has been in operation since October 1, 2012 (10) With this system, the required physician input has been almost 100%. A total of 2,531 checks were performed with this system in the six years until September 30, 2018, and a total 21,607 HBV DNA measurement tests were performed. Among these patients, the occurrence of HBV reactivation was checked by this system in 1,206 patients who were HBs antigen-negative, HBc antibody- and/or HBs antibody-positive and who underwent HBV DNA quantification two times or more. HBV reactivation was defined by a change in the HBV DNA titer from an undetectable level to ≥1.3 log IU/mL more (or ≥2.1 log copies/mL) during the observation period. This study was reviewed and approved by our ethics committee (Fukui Saiseikai Hospital).
Results
The characteristics of the 1,206 patients in the study population were as follows: male, n=649; female, n=557, median age is 72 years (range 22-99 years), HBc antibody-negative (CLEIA method), n=179; HBc antibody-positive, n=1,024 (<10.0, n=88; ≥10.0, n=143 cases); HBs antibody-negative, n=341; and HBs antibody-positive, n=864. The conditions and treatments of the patients were as follows: malignant lymphoma, n=85 (anticancer drugs with rituximab, n=40), malignant disease treated with antitumor drugs, n=546; steroid therapy, n=274 (administered for ≥2 weeks), rheumatoid arthritis (RA) treated with antirheumatic drugs, n=144, diseases treated with immunosuppressive agents or biologics, n=26; and hepatitis C treated with DAA, n=176 (Table 3). In the median observation period of 15.0 (range, 1 to 81 months), HBV reactivation was observed in 27 cases (malignant lymphoma treated with rituximab, n=6; malignant disease treated with antitumor agents, n=8; steroid therapy, n=10; RA treated with anti-RA drug, n=1; hepatitis C treated with DAA, n=2) (Table 4) Reactivation was observed at 1 to 49 months (median duration is 11 months) after administration (Table 4). The overall cumulative HBV reactivation rate was 1.3% at 1 year, 2.7% at 2 years, and 4.4% at 3 years (Fig. 3). HBV reactivation was observed in 6 of 40 with malignant lymphoma who were using rituximab, and all patients started to use nucleic acid analog preparations immediately (Table 4). A comparison of the cumulative survival rates between the 40 patients treated with rituximab and 1,166 patients treated without rituximab showed that the survival rate of patients using rituximab was significantly higher (Fig. 4). In the analysis of factors contributing to HBV reactivation the overall study population (n=1,206), HBV reactivation rates were higher in elderly patients, male patients, patients treated with rituximab, and patients with previous HBV infection who were positive for HBc antibody alone (Table 5). Among 274 patients treated with steroids, 10 experienced reactivation, which occurred 1 to 49 months after the start of steroid administration, and 6 out of 10 cases occurred more than 6 months after the start of steroid administration (Table 4). In 10 experiencsd reactivation cases treated steroids, 5 cases were followed without the use of nucleic acid analog preparations, but no HBV DNA elevation or hepatitis occurred. One patient was HBs antigen-positive and developed hepatitis. The patient was a 67-year-old man who started to receive prednisolone a dose of 55 mg, which was continuously tapered, for vasculitis. Prior to the administration, the patient was HBs antigen-negative, HBs antibody-negative, and HBc antibody-positive. The our information technology encoding system was updated with the results of HBV DNA sampling and checks performed every month. However, blood sampling and checks were not performed at 10 months due to a change of the attending physician.
Table 3.
Patient Demographics.
| Sex Male/Female | 649/557 |
| Age Mean (Min-Max) | 72 (22-99) |
| HBc Ab (CLEIA) -/+(<10.0) /+(≥10.0) | 179/881/143 |
| HBs Ab (CLEIA) -(<10.0) /+(≥10.0) | 341/864 |
| Drug | |
| Rituximab combined with anticancer agents | 40 |
| Antitumor agents. (including 45 patients above) | 546 |
| Steroid | 274 |
| Anti-RA | 144 |
| Immunosuppressant/Biological | 26 |
| DAA | 176 |
| Observation (Month) Mean (Min-Max) | 15.0 (1-81) |
*Ab: antibody, RA: rheumatoid arthritis, DAA: direct acting antivirals
Table 4.
Cases of HBV Reactivation (n=27).
| Age | Sex | Diagnosis | Medicine | Department | Medicine 2 | HBc antibody | HBs antibody | HBc antibody | HBs Antibody | Reactivation M |
|---|---|---|---|---|---|---|---|---|---|---|
| 74 | F | ML | R-CVP | Internal | Rituximab | + | + | 8.2 | 76.14 | 40 |
| 73 | M | ML | DA-EPOCH-R | Internal | Rituximab | + | - | 8,32 | 2 | |
| 78 | M | ML | R-CHOP | Oncology | Rituximab | + | - | 8.78 | 6 | |
| 64 | M | ML | R-CHOP | Oncology | Rituximab | + | - | 9.08 | 11 | |
| 71 | M | ML | R-CHOP | Oncology | Rituximab | + | - | 14.28 | 31 | |
| 83 | M | ML | R-CHOP | Oncology | Rituximab | + | - | 6.21 | 9 | |
| 72 | F | ML | Mogamulizumab | Oncology | Chemotherapy | + | + | 6.31 | 118.99 | 19 |
| 91 | F | ET | hydroxycarbamide | Internal | Chemotherapy | + | + | 9.61 | 499.62 | 30 |
| 83 | M | Lung cancer | CDBCA+PEM | Internal | Chemotherapy | + | - | 8.27 | 24 | |
| 55 | M | Plasmacytoma | CHOP | Oncology | Chemotherapy | + | + | 8.88 | 116.38 | 40 |
| 75 | F | Lung cancer | UFT | Internal | Chemotherapy | + | - | 10.17 | 4 | |
| 72 | M | Lung cancer | CDDP+PEM | Internal | Chemotherapy | + | + | 11.95 | 61.75 | 22 |
| 74 | M | ML | CHOP | Internal | Chemotherapy | + | - | 7.93 | 27 | |
| 88 | M | MM | VRd | Internal | Chemotherapy | + | + | 9.15 | 21.37 | 3 |
| 77 | F | Aortitis syndrome | Steroid | Internal | Steroid | + | + | 12.61 | 38.78 | 13 |
| 85 | M | Pemphigus | Steroid | Dermatology | Steroid | + | - | 6.68 | 6 | |
| 74 | M | Eosinophilic pneumonia | Steroid | Internal | Steroid | + | + | 8.44 | 42.21 | 4 |
| 67 | M | Vasculitis | Steroid | Internal | Steroid | + | - | 10.11 | 20 | |
| 58 | F | SLE | Steroid | Internal | Steroid | - | + | 4.19 | 30 | |
| 71 | M | Polymyositis | Steroid | Neurology | Steroid | + | + | 1.77 | 27.2 | 9 |
| 75 | M | IP | Steroid | Internal | Steroid | + | - | 7.98 | 1 | |
| 79 | M | Eosinophilic pneumonia | Steroid | Internal | Steroid | + | + | 5.94 | 15.52 | 10 |
| 70 | M | ITP | Steroid | Internal | Steroid | + | - | 3.46 | 10 | |
| 84 | M | Erythroderma | Steroid | Internal | Steroid | + | - | 9.63 | 49 | |
| 83 | M | RA | MTX+Steroid | Internal | Anti-RA | + | + | 9.4 | 31 | |
| 75 | M | LCC | DAA | Internal | DAA | + | + | 7.96 | 581.12 | 12 |
| 84 | F | CHC | DAA | Internal | DAA | + | - | 10.43 | 1 |
Reactivation M, period from the initiation of drug administration to reactivation (months).
ML: malignant lymphoma, ET: essential thrombocythemia, MM: multiple myeloma, SLE: systemic lupus erythematosus, IP: interstitial pneumonia, ITP: idiopathic thrombocytopenic purpura, LCC: luxatio coxae congenita, CHC: chronic hepatitis C, R-CVP: rituximab, cyclophosphamide, vincristine (Oncovin), and prednisone, DA-EPOCH-R: dose-adjusted etoposide, prednisone, vincristine, cyclophosphamide, doxorubicin, and rituximab, R-CHOP: rituximab, cyclophosphamide, doxorubicin, hydrochloride (hydroxydaunorubicin), vincristine (oncovin), and prednisone, CDBCA+PEM: carboplatin plus pemetrexed, UFT: Uracil/Tegafur, CDDP+PEM: cisplatin plus pemetrexed, VRd: bortezomib, lenalidomide, and dexamethasone, MTX: methotrexate, DAA: direct acting antivirals
Figure 3.

Overall cumulative HBV reactivation rate. n=1,206: Kaplan-Meier method.
Figure 4.

Comparison of the cumulative HBV reactivation rate in patients treated with/without rituximab. Kaplan Meier method; Log rank test p<0.001. The comparison of the cumulative HBV reactivation rates by rituximab clearly and significantly resulted in the HBV reactivation rate being higher in patients prescribing rituximab than those not.
Table 5.
Factors Contributing to HBV Reactivation in All 1206 Cases.
| Log rank test P |
p value | Hazard ratio |
95% confidence interval | |||
|---|---|---|---|---|---|---|
| Lower limit | Upper Limit | |||||
| Age | ≥72/<72 | 0.007 | 0.020 | 2.797 | 1.175 | 6.659 |
| Gender | Male/Female | 0.021 | 0.004 | 2.444 | 1.024 | 5.812 |
| Rituximab | +/- | <0.001 | <0.001 | 7.756 | 3.097 | 19.423 |
| HBV infection HBcAb(+)/ HBsAb(+) and HBcAb(+), HBsAb(+) |
<0.001 | 0.001 | 3.492 | 1.616 | 7.546 | |
The factors contributing to HBV reactivation in all cases were high age, male, rituximab use cases and HBc antibody alone positive cases.
Ab: antibody
The patient's ALT value increased to 548 (IU/L). Meanwhile, his PT% was 97.7, his PT-INR was 1.01, and his T.Bil was 0.5 (mg/dL), which were all within the normal ranges. His ALT level quickly normalized after the administration of nucleoside analog, and the patient was thereby successfully treated without experiencing any severe hepatitis.
When the cumulative HBV reactivation rate in 1,166 cases - excluding 40 cases in which rituximab was used - was examined according to the presence or absence of steroid use, the results showed a significantly higher HBV reactivation rate among steroid users (Fig. 5). In the study of factors contributing to HBV reactivation in these 1,166 cases, in addition to steroid users, the HBV reactivation rates were higher in elderly patients, and patients who were positive for HBc antibodies alone in their past HBV infection (Table 6).
Figure 5.

Comparison of cumulative HBV reactivation rate in patients treated with/without steroids. n=1,166 (patients treated with rituximab were excluded). Kaplan Meier method; Log-rank test p=0.038. 1,166 cases other than rituximab, the cumulative HBV reactivation rates focused on steroid, it turned out that HBV reactivation rate was significantly higher in the steroid administration.
Table 6.
Factors Contributing to HBV Reactivation in Patients Treated with Agents Other than Rituximab N=1,166.
| Log rank test P |
p value | Hazard ratio |
95% confidence interval | |||
|---|---|---|---|---|---|---|
| Lower limit | Upper Limit | |||||
| Age | ≥72/<72 | 0.010 | 0.035 | 2.959 | 1.078 | 8.125 |
| Gender | Male/Female | 0.068 | 0.206 | 3.935 | 0.472 | 32.803 |
| Steroid | +/- | 0.038 | 0.016 | 2.933 | 1.221 | 7.042 |
| HBV infection HBcAb(+)/ HBsAb(+), HBcAb(+) and HBsAb(+) |
0.007 | 0.014 | 3.010 | 1.251 | 7.243 | |
Factors contributing to HBV reactivation in cases other than rituximab were high age, steroids use cases and HBc antibody alone positive cases.
Ab: antibody
Discussion
Death due to reactivation of hepatitis B has long been a major issue. In 2009, the guidelines for measures against hepatitis B caused by immunosuppression/chemotherapy were created (9); however, cases of hepatitis due to HBV activation continue. This is thought to be because the guidelines are not recognized or followed, especially by non-hepatic specialists, there are still many physicians who are not knowledgeable about HBV reactivation. The number of lawsuits related to fulminant hepatitis B caused by HBV reactivation has increased, and countermeasures must be taken sooner before lawsuits related to fulminant hepatitis B due to HBV reactivation. Thus, we built a countermeasure system using IT, which has been in use since 2012. This system guides appropriate HBV-related examinations and treatments by extracting drug use information and information on the medical treatment of HBV from electronic medical records and feeds information back to the attending physician. The effect was confirmed immediately after the system became operational (10) and the input rate (by physicians) has remained almost 100%. In other words, all patients treated with immunosuppressive agents or chemotherapy in our hospital have been treated according to the hepatitis B countermeasure guidelines. This system has also enabled a prospective survey of cases of hepatitis B reactivation since 2012. Thus, we conducted a prospective study of HBV reactivation in the 6 years from October 2012, when the system was introduced, to October 2018.
During the 6-year study period, 27 cases of HBV reactivation were observed among 1,206 patients who had been previously been diagnosed with HBV infection. Among these patients, reactivation was observed in 6 of 40 patients who were treated with rituximab, and the cumulative HBV reactivation rate was clearly higher in comparison to patients treated without rituximab, as has been previously reported (11-14). It was reaffirmed that the risk of reactivation was extremely high in these patients. Rituximab is a monoclonal antibody preparation against the B cell surface antigen CD20, but is mediated by complement-dependent cytotoxicity (CDC) and antibody-dependent cell-mediated cytotoxicity (ADCC). It is reported to cause B cell lymphocyte injury and to suppress the production of antibodies against HBV over a long period of time. In fact, there are some reports of cases in which HBV reactivation occurred long after the end of rituximab treatment, and moreover, even after long-term treatment with nucleic acid analog and long-term HBV-DNA negative, HBV reactivation may occur after completion nucleic acid analog preparation. In our hospital, we carefully monitor patients treated with rituximab, prevent omissions in testing, and continue to administer nucleic acid analog preparations.
In addition to patients treated with rituximab, we observed that HBV reactivation was significantly more common in steroid users than in steroid non-users. Steroids are not only immunosuppressive but also act on glucocorticoid responsive elements in the HBV genome, and are involved in the direct increase of the HBV-DNA. Thus, attention is required to detect HBV reactivation in steroid users (15). However, although case reports show examples of HBV reactivation during steroid treatment, no studies have statistically analyzed the risk of HBV reactivation in group of steroid population. In the analysis of the present study population, after the exclusion of rituximab-treated patients, steroid use was found to be a significant risk factor for HBV reactivation. In the present study, steroid use was defined as the administration of steroids for ≥2 weeks; however, steroids are very widely used. Thus, further studies are necessary to investigate the impact of the administration period, dosage, administration schedule, and other drugs on the risk of HBV reactivation in patients treated with steroids. In addition, 1 patient experienced reactivation while receiving anti-RA treatment and 2 patients experienced reactivation during DAA treatment for chronic hepatitis C (both showed transient HBV reactivation, that is, HBV DNA titer was only transiently elevated and then naturally decreased). Although the data suggested that these drugs caused HBV reactivation, the risk of severe HBV reactivation in patients treated with these drugs is expected to be low. In some cases, HBV reactivation due to steroid treatment was relieved in the natural course; however, on patient became HBs antigen-positive and developed hepatitis. There have been reports of death after de novo hepatitis B during steroid treatment, and it is considered necessary to investigate the risk of HBV reactivation and the severity of HBV reactivation in a larger number of steroid users.
Recently, new molecular targeted drugs and antibody preparations have been developed (16-21). The mechanisms of many of these drugs raise concerns about HBV reactivation and further attention will be needed in the near future. The possibility of high-sensitivity HBs antigen measurement as a substitute for HBV DNA monitoring is also being investigated (22). However, at present, the only way to prevent severe HBV reactivation is to continuously monitor HBV DNA titers in patients with risk factors for HBV reactivation and diagnose HBV reactivation at an early stage, as we do in our hospital.
A recent prospective multicenter study on the evaluation of HBV reactivation during treatment with antirheumatic drugs and other immunotherapeutic drugs has been reported (23, 24). This is truly the first prospective evaluation of HBV reactivation in all patients receiving immunosuppressive chemotherapy at a single institution. In the future, we plan to conduct further prospective studies and to clarify the risk factors for HBV reactivation in detail.
The authors state that they have no Conflict of Interest (COI).
References
- 1.Lubel JS, Angus PW. Hepatitis B reactivation in patients receiving cytotoxic chemotherapy:diagnosis and management. J Gastroenterol Hepatol 25: 864-871, 2010. [DOI] [PubMed] [Google Scholar]
- 2.Wursthorn K, Wedemeyer H, Manns MP. Managing HBV in patients with impaired immunity. Gut 59: 1430-1445, 2010. [DOI] [PubMed] [Google Scholar]
- 3.Lok AS, Liang RH, Chiu EK, et al. Reactivation of hepatitis B virus replication in patients receiving cytotoxic therapy. Report of a prospective study. Gastroenterology 100: 182-188, 1991. [DOI] [PubMed] [Google Scholar]
- 4.Yeo W, Chan PK, Zhong S, et al. Frequency of hepatitis B virus reactivation un cancer patients undergoing cytotoxic chemotherapy: a prospective study of 626 patients with identification of risk factors. J Med Virol 62: 299-307, 2000. [DOI] [PubMed] [Google Scholar]
- 5.Lubel JS, Testro AG, Angus PW. Hepatitis B virus reactivation following immunosuppressive therapy: guidelines for prevention and management. Intern Med J 16: 13-18, 1992. [DOI] [PubMed] [Google Scholar]
- 6.Carrol MB, Forgione MA. Use of tumor necrosis factor alfa inhibitors in hepatitis B surface antigen-positive patients: a literature review and potential mechanisms of action. Clin Rheumatol 29: 1021-1029, 2010. [DOI] [PubMed] [Google Scholar]
- 7.Urata Y, Uesato R, Tanaka D, et al. Prevalance of reactivation of hepatitis B virus replication in rheumatoid arthritis patients. Mod Rheumatol 21: 16-23, 2011. [DOI] [PubMed] [Google Scholar]
- 8.Aqqeletopoulou I, Konstantakis C, Manolakopoulos S, et al. Risk of hepatitis B reactivation in patients treated with direct-acting antivirals for hepatitis C. World J Gastroenterol 23: 4317-4323, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.JSH Guidelines for the Management of Hepatitis B. Committee for Hepatitis Management Guidelines and the Japan Society. 2019. [Google Scholar]
- 10.Notsumata K, Kumai T, Ueda T, et al. Automated risk management of HBV reactivation by encoding patients'medical records. Kanzo 55: 91-99, 2014. (in Japanese, Abstract in English). [Google Scholar]
- 11.Kusumoto S, Tanaka Y, Mizokami M, et al. Reactivation of hepatitis B virus following systemic chemotherapy for malignant lymphoma. Int J Hematol 90: 13-23, 2009. [DOI] [PubMed] [Google Scholar]
- 12.Kusumoto S, Tanaka Y, Ueda R, et al. Reactivation of hepatitis B virus following rituximab-plus-steroid combination chemotherapy. J Gastroenterol 46: 9-16, 2011. [DOI] [PubMed] [Google Scholar]
- 13.Hsu C, Tsaou HH, Lin SJ, et al. Chemotherapy-induced hepatitis B reactivation in lymphoma patients with resolved HBV infection: a prospective study. Hepatology 59: 2092-2100, 2014. [DOI] [PubMed] [Google Scholar]
- 14.Kusumoto S, Tanaka Y, Suzuki R, et al. Monitoring of hepatitis B virus (HBV) DNA and risk of HBV reactivation in B-cell lymphoma: a prospective observational study. Clin Infect Dis 61: 719-725, 2015. [DOI] [PubMed] [Google Scholar]
- 15.Chou CK, Wang LH, Lin HM, et al. Glucocortiroid stimulates hepatitis B viral gene expression in cultured human hepatoma cell. Hepatology 16: 13-18, 1992. [DOI] [PubMed] [Google Scholar]
- 16.Mitka M. FDA: increased HBV reactivation risk with ofatumumab or rituximab. JAMA 310: 1664, 2013. [DOI] [PubMed] [Google Scholar]
- 17.Kusumoto S, Arcaini I, Hong X, et al. Risk of HBV reactivation in patients with B-cell lymphomas receiving obinutuzumab or rituximab immunochemotherapy. Blood 133: 137-146, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nakano N, Kusumoto S, Tanaka Y, et al. Reactivation of hepatitis B virus in a patient with adult T-cell leukemia-lymphoma receiving the ant-CC chemokine receptor 4 antibody mogamulizumab. Hepatol Res 44: 354-357, 2014. [DOI] [PubMed] [Google Scholar]
- 19.Iannitto E, Minardi V, Calvaruso G, et al. Hepatitis B virus reactivation and alemtuzumab therapy. Eur J Haematol 74: 254-258, 2005. [DOI] [PubMed] [Google Scholar]
- 20.Law MF, Ho R, Cheung CK, et al. Prevention and management of hepatitis B virus reactivation in patients with hematological malignancies treated with anticancer therapy. World J Gastroenterol 22: 6484-6500, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Noguchi Y, Tsurushima M, Tamura Y, et al. A case of hepatitis B virus reac ivation with prior resolved hepatitis B infection during bevacizumab plus FORFIRI treatment. Gan To Kagaku Ryoho 40: 1561-1563, 2013. (in Japanese, Abstract in English). [PubMed] [Google Scholar]
- 22.Shinkai N, Kusumoto S, Murakami S, et al. Novel monitoring of hepatitis B reactivation based on ultra-high sensitive hepatitis B surface antigen assay. Liver Int. [DOI] [PubMed] [Google Scholar]
- 23.Fukuda W, Hanyu T, Katayama M, et al. Risk stratification and clinical course of hepatitis B virus reactivation in rheumatoid arthritis patients with resolved infection: final report of a multicenter prospective observational study at Japanese Red Cross Hospital. Arthritis Res Ther 21: 255, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mochida S, Nakao M, Nakayama N, et al. Nationwide prospective and retrospective surveys for hepatitis B virus reactivation during immunosuppressive therapies. J Gastroenterol 51: 999-1010, 2016. [DOI] [PubMed] [Google Scholar]