Abstract
Objectives
The pandemic spread of the coronavirus SARS‐CoV‐2 is due, in part, to the immunological properties of the host–virus interaction. The clinical presentation varies from individual to individual, with asymptomatic carriers, mild‐to‐moderate‐presenting patients and severely affected patients. Variation in immune response to SARS‐CoV‐2 may underlie this clinical variation.
Methods
Using a high‐dimensional systems immunology platform, we have analysed the peripheral blood compartment of 6 healthy individuals, 23 mild‐to‐moderate and 20 severe COVID‐19 patients.
Results
We identify distinct immunological signatures in the peripheral blood of the mild‐to‐moderate and severe COVID‐19 patients, including T‐cell lymphopenia, more consistent with peripheral hypo‐ than hyper‐immune activation. Unique to the severe COVID‐19 cases was a large increase in the proportion of IL‐10‐secreting regulatory T cells, a lineage known to possess anti‐inflammatory properties in the lung.
Conclusion
As IL‐10‐secreting regulatory T cells are known to possess anti‐inflammatory properties in the lung, their proportional increase could contribute to a more severe COVID‐19 phenotype. We openly provide annotated data (https://flowrepository.org/experiments/2713) with clinical correlates as a systems immunology resource for the COVID‐19 research community.
Keywords: COVID‐19, IL‐10, open resource, SARS‐CoV‐2, systems immunology, T regulatory cells
Clinical presentation of patients infected with the new coronavirus SARS‐CoV‐2 is very variable and possibly due to differences in the immune response. To address this hypothesis, we investigated the peripheral blood compartment of healthy individuals, mild‐to‐moderate and severe COVID‐19 patients in a systems immunology platform. We identified a large proportion of IL‐10‐secreting regulatory T cells in severe cases only and provide annotated data as a resource for the COVID‐19 research community.

Introduction
The novel severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) has infected millions of people worldwide and impacted the society and the global economy in an unprecedented manner. Variation in immune response to SARS‐CoV‐2 may underlie the clinical variation observed. Unravelling the immunological features associated with progression into severe and life‐threatening disease is highly needed in order to guide therapeutic decision‐making and biomarker discovery.
Innate immune responses are an essential first‐line defence against viruses, including type I and III interferon (IFN). Recent studies have suggested that SARS‐CoV‐2 inhibits type I IFN production and signalling, 1 potentially explaining the long pre‐symptomatic period and persistent viral load in many patients. Defects in NK cell function may also be present, with reports of higher expression of activation and exhaustion markers on NK cells, and impaired NK cytotoxicity and cytokine production, 1 , 2 and additional problems with innate immunity are likely to be identified. Other studies suggest a defect in the adaptive immune system. Lymphopenia is widely reported in COVID‐19, and the severity of lymphopenia has been correlated with disease severity. 2 , 3 Functional defects within T cells have been reported, with an increased number of non‐functional CD4+ T cells and impaired T‐cell cytokine production. 2 , 3 , 4 This was confirmed in an independent study, but without significant changes between moderate and severe patients, 5 while another study reported no change. 1 Parallel findings were reported in bronchoalveolar lavage fluid of COVID‐19 patients, with enrichment of naïve CD4+ T cells in severely affected patients. 6 Overall, it remains to be determined whether defects in innate or adaptive immunity or a synergistic effect of both underlie the unusually long infectious period of SARS‐CoV‐2.
Immune analysis is also contributing to an understanding of COVID‐19 pathology. Parallels with other respiratory infections, such as influenza, 7 have led to the hypothesis that pathology is immune‐mediated rather than due to direct viral induction, and the potential success of immune‐modulating therapeutics in small‐scale clinical trials provides preliminary support for this model. 8 , 9 , 10 , 11 Neutrophils seem to be consistently elevated in severe patients and are associated with poor outcomes. 2 , 3 , 5 , 12 Several studies have identified COVID‐19 as a hyper‐inflammatory status, with a ‘cytokine storm’ of pro‐inflammatory cytokines. 1 , 3 , 6 , 13 , 14 , 15 , 16 Interleukin (IL)‐6, in particular, was consistently higher in severely affected patients compared to moderate and milder cases, suggesting it might be associated with disease severity. 3 , 6 , 13 , 15 , 16 Inconsistent findings have been reported regarding the changes in myeloid subsets 1 , 12 , 17 , 18 ; however, severe COVID‐19 patients seem to have an increased number of inflammatory monocytes, producing higher levels of IL‐6 and GM‐CSF. 12 , 18 Bronchoalveolar lavage fluid of severe COVID‐19 cases also revealed high levels of monocytes and neutrophils as well as a pro‐inflammatory environment. 6 , 19 Excessive T‐cell activation has also been suggested as a possible driver of disease, with increased expression of activation markers (such as HLA‐DR, CD38, CD69, CD25, CD44, Ki‐67, OX40 and CD137) by CD4+ and CD8+ T cells in severe patients. 1 , 3 , 4 , 12 , 16 , 20 As with the cause of poor viral clearance, the cause of excessive immune pathology remains unclear.
The ambiguity of the COVID‐19 immune profile is based, in part, on the recent origin of the pandemic, but also on the design of COVID‐19 clinical trials, many of which have substandard design, lacking suitable controls or data transparency. 21 A potential solution is to provide open‐access high‐dimensional data, allowing independent analysis with alternative strategies, while still preserving the rapid publication process required to deal with an evolving pandemic. As part of the CONTAGIOUS consortium, multi‐omic approaches are being performed in a systematic and coordinated manner against a longitudinal COVID‐19 cohort. Here, we provide the first high‐dimensional flow cytometry analysis for the CONTAGIOUS cohort. The peripheral blood of 6 healthy individuals, 23 mild‐to‐moderate COVID‐19 patients and 20 severe COVID‐19 patients was assessed for changes to the T‐cell compartment and identified a signature of IL‐10‐producing regulatory T cells in those patients with severe COVID‐19. Annotated data are openly available (https://flowrepository.org/experiments/2713), allowing transparent and evolving data analysis.
Results
As part of the CONTAGIOUS study into the immunome of COVID‐19, patients were recruited through the University Hospital in Leuven, Belgium, beginning 27th March 2020. The data set was generated on 6 healthy individuals, 23 mild‐to‐moderate COVID‐19 patients (WHO score 3–4) and 20 severe COVID‐19 patients (WHO score 5–7). Demographic data for the patients are summarised in Table 1, with individual data on demographic and clinical values in Supplementary table 1.
Table 1.
Clinical features of the COVID‐19 cohort
| Parameter | Healthy | Mild‐to‐moderate COVID‐19 | Severe COVID‐19 |
|---|---|---|---|
| Number of patients | 6 | 23 | 20 |
| Age (years) | 56 (40–62) | 58 (53–69) | 64.5 (53–69) |
| Male:female ratio | 3:3 | 10:13 | 14:6 |
| WHO score | n/a | Score 3: 11/Score 4: 12 | Score 5: 12/Score 6: 8 |
| BMI | n/a | 25.1 (22.7–31.7) | 29.1 (24.4–32.5) |
| CRP (mg L−1) | n/a | 72.35 (27.6–138.9) | 141.2 (74.75–239.2) |
| WBC (103 μL−1) | n/a | 6.32 (4.07–9.4) | 8.42 (6.72–10.06) |
| Neutrophil count (×103 μL−1) | n/a | 4.5 (2.9–7.1) | 6.05 (5.23–8.2) |
| Lymphocyte count (×103 μL−1) | n/a | 1.0 (0.8–1.7) | 0.9 (0.625–1.225) |
| Degradation of clinical status (from mild‐moderate to severe) | n/a | 2 | n/a |
| Number of patients receiving treatment before sampling | |||
| Hydroxychloroquine | n/a | 18 | 20 |
| Itraconazole | n/a | 6 | 3 |
| Corticosteroids | n/a | 1 | 2 |
Median (25–75 percentiles) for key demographic and clinical parameters of patients entered into the study. BMI, body mass index; CRP, C‐reactive protein; n/a, not available; WBC, white blood cell count; WHO, World Health Organization.
In order to determine the T‐cell phenotypes associated with clinical heterogeneity in COVID‐19, we stimulated T cells ex vivo and used high parameter flow cytometry covering a comprehensive set of subset markers, activation markers and cytokines. Appropriate compensation matrices were calculated using AutoSpill, 22 allowing optimal distinction of subsets. First, we assessed the number of major leukocyte subsets in PBMCs, using key lineage markers (CD3, CD4, CD8, FOXP3, CD14, CD19). Cluster‐based flow cytometry analysis, pooling all samples, separated leukocytes into populations that corresponded to CD4+ T cells, CD8+ T cells, CD19+ B cells, CD14+ monocytes and CD4−CD8− T cells (Figure 1a and b, Supplementary figure 1). Traditional gating was used to quantify these populations, and FOXP3+ regulatory T cells, in each sample. Despite the marked lymphopenia in COVID‐19 patients (Figure 1c), the relative proportion of these leukocyte populations remained unchanged with COVID‐19 patients (Figure 1d), other than a trend towards lower CD8 T‐cell numbers, indicating a non‐specific mechanism of leukopenia. Subtle, but significant, differences were observed in the expression of lineage markers, with comparison of pooled mild‐to‐moderate and severe COVID‐19 patient samples showing a more similar expression pattern than pooled healthy controls (Figure 1e). At the individual level, healthy individuals were largely clustered together, while mild‐to‐moderate and severe COVID‐19 patients exhibited similar cellular phenotypes (Figure 1f and g). Together, these data indicate only subtle shifts in the balance of blood leukocyte populations with COVID‐19, without any discrimination between mild‐to‐moderate and severe cases.
Figure 1.
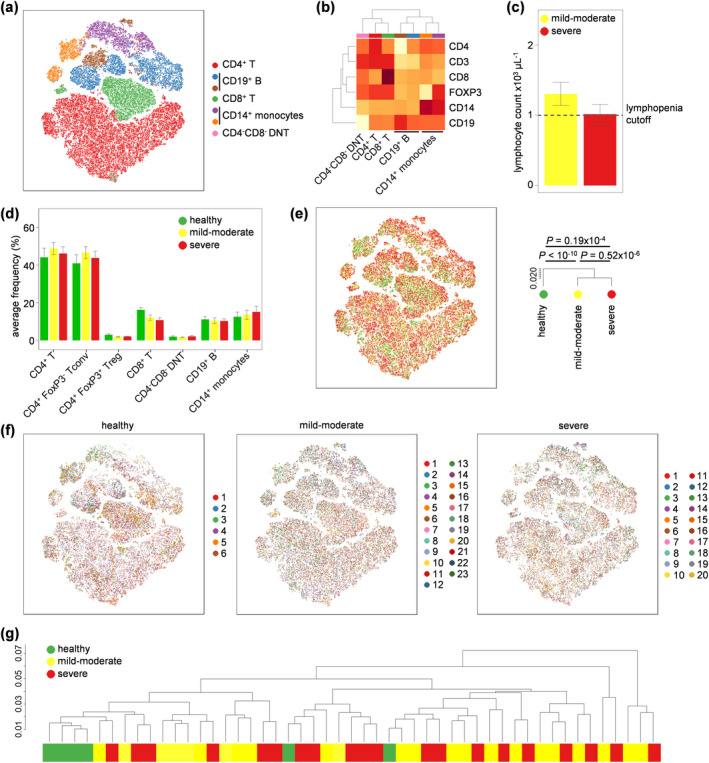
Peripheral blood leukocyte changes in mild‐to‐moderate and severe COVID‐19 patients. PBMCs were isolated from healthy controls (n = 6), mild‐to‐moderate COVID‐19 patients (n = 23) and severe COVID‐19 patients (n = 20), stimulated and assessed through flow cytometry. (a) tSNE representation of PBMC populations based on the expression of lineage markers: CD3, CD4, CD8, FOXP3, CD19 and CD14. FlowSOM clusters were annotated based on (b) expression of lineage markers across each cluster (see also Supplementary figure 1). (c) Clinical lymphocyte counts for mild‐to‐moderate and severe COVID‐19 patients. (d) Quantification of leukocyte subsets in healthy controls, mild‐to‐moderate COVID‐19 and severe COVID‐19 patients based on manual gating. (e) tSNE representation of PBMC populations based on aforementioned lineage markers for each condition, namely healthy controls, mild‐to‐moderate COVID‐19 and severe COVID‐19 patients. The dendrogram shows the comparative similarity based on the Kolmogorov–Smirnov statistic calculated using the cross‐entropy distributions derived from tSNE. (f) tSNE representation of PBMC populations based on aforementioned lineage markers for each condition, namely healthy controls, mild‐to‐moderate COVID‐19 and severe COVID‐19 patients, with each individual represented in a different colour. (g) Dendrogram showing the comparative similarity between individuals based on the Kolmogorov–Smirnov statistic calculated using the cross‐entropy distributions derived from tSNE. Mean ± SEM.
We next investigated the activation and polarisation of conventional CD4+ T cells in COVID‐19 patients. Using the expression of CD45RA, CCR7, 4‐1BB, CD25, CTLA‐4, HLA‐DR, IFNγ, IL‐2, IL‐4, IL‐6, IL‐10, IL‐17a, PD‐1, RORγt, T‐BET and TNFα, we clustered the conventional CD4+ T‐cell population into 15 biologically distinct subsets: naïve CTLA‐4− cells, naïve CTLA‐4+ cells, T central memory (TCM), TCM CTLA‐4+, TCM IL‐2+, T effector memory (TEM), TEM Th1 CTLA4+, TEM Th1 CTLA‐4−, TEM IL‐2+, TEM TNFα+, TEM TNFα+ CTLA‐4+, TEM PD‐1high, T effector memory re‐expressing CD45RA (TEMRA), TEMRA Th1 and TEMRA Th17 (Figure 2a and b, Supplementary figure 2). Quantification of these subsets across healthy volunteers and COVID‐19 patients demonstrated no significant changes, with only a trend towards increased TCM and decreased TEM being present in severe COVID‐19 patients, with mild‐to‐moderate patients intermediate in number between healthy and severe COVID‐19 patients (Figure 2c). Global phenotypic analysis, by contrast, found the cellular phenotype of conventional CD4+ T cells to be more similar between healthy individuals and severe COVID‐19 patients (Figure 2d). At an individual level, the cellular phenotypes of healthy, mild‐to‐moderate COVID‐19 and severe COVID‐19 samples were intermingled (Figure 2e and f). These data do not support a peripheral CD4 T‐cell hyper‐activation model of COVID‐19.
Figure 2.
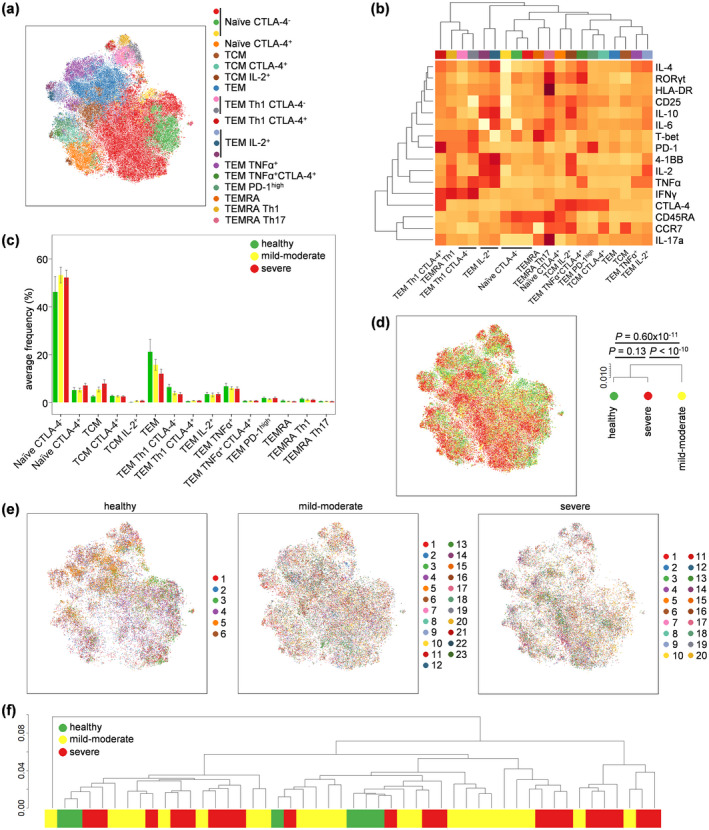
Altered conventional CD4+ T‐cell phenotypes in COVID‐19. PBMCs were isolated from healthy controls (n = 6), mild‐to‐moderate COVID‐19 patients (n = 23) and severe COVID‐19 patients (n = 20), stimulated and assessed through flow cytometry. CD3+CD14−CD4+CD8−FOXP3− conventional T cells were manually gated in FlowJo. (a) tSNE representation of conventional CD4 T‐cell cluster populations based on the expression of phenotypic markers: CD45RA, CCR7, 4‐1BB, CD25, CTLA‐4, HLA‐DR, IFNγ, IL‐2, IL‐4, IL‐6, IL‐10, IL‐17a, PD‐1, RORγt, T‐BET and TNFα. FlowSOM clusters were annotated based on (b) expression of phenotypic markers across each cluster (see also Supplementary figure 2). (c) Quantification of conventional T‐cell subsets in healthy controls, mild‐to‐moderate COVID‐19 and severe COVID‐19 patients. (d) tSNE representation of PBMC populations based on aforementioned phenotypic markers for each condition, namely healthy controls, mild‐to‐moderate COVID‐19 and severe COVID‐19 patients. The dendrogram shows the comparative similarity based on the Kolmogorov–Smirnov statistic calculated using the cross‐entropy distributions derived from tSNE. (e) tSNE representation of PBMC populations based on aforementioned phenotypic markers for each condition, namely healthy controls, mild‐to‐moderate COVID‐19 and severe COVID‐19 patients, with each individual represented in a different colour. (f) Dendrogram showing the comparative similarity between individuals based on the Kolmogorov–Smirnov statistic calculated using the cross‐entropy distributions derived from tSNE. Mean ± SEM.
Using the same approach, we investigated the phenotype of FOXP3+ regulatory T cells. Clustering based on expression markers identified 13 regulatory T‐cell subsets with biologically distinct characteristics: naïve CTLA‐4−, naïve CTLA‐4+, TEM, TEM CTLA‐4+, TCM, TCM CTLA‐4+, IL‐2 producing CTLA‐4+, IL‐10‐producing, TNFα‐producing CTLA‐4+, TNFα‐producing CTLA‐4−, IFNγ‐producing CTLA‐4−, IFNγ‐producing CTLA‐4+ and HLA‐DR+ cells (Figure 3a and b, Supplementary figure 3a and b). Quantification of these subsets across healthy volunteers and COVID‐19 patients demonstrated an increase in TCM CTLA‐4+ regulatory T cells and IL‐10‐producing regulatory T cells in severe COVID‐19 patients, with mild‐to‐moderate patients being intermediate (Figure 3c). Manual gating of IL‐10‐producing regulatory T cells confirmed a 5‐fold increase in severe COVID‐19 patients only, a significant rise over both healthy individuals and mild‐to‐moderate COVID‐19 patients (Figure 3d, Supplementary figure 3c). Cellular phenotypes were largely similar across healthy individuals and COVID‐19 patients at both the pool (Figure 3e) and individual (Figure 3f and g) level. While preliminary, the increase in IL‐10‐producing regulatory T cells in severe COVID‐19 patients is of particular interest, given the role of the murine equivalent in controlling lung inflammation. 23 In addition, we demonstrated that IL‐10‐producing regulatory T cells expressed higher levels of both CD25 and FOXP3 compared to the total regulatory T‐cell population (Supplementary figure 3d). As Miyara et al. 24 showed, this confers a higher suppressive capacity to this specific subpopulation of regulatory T cells.
Figure 3.
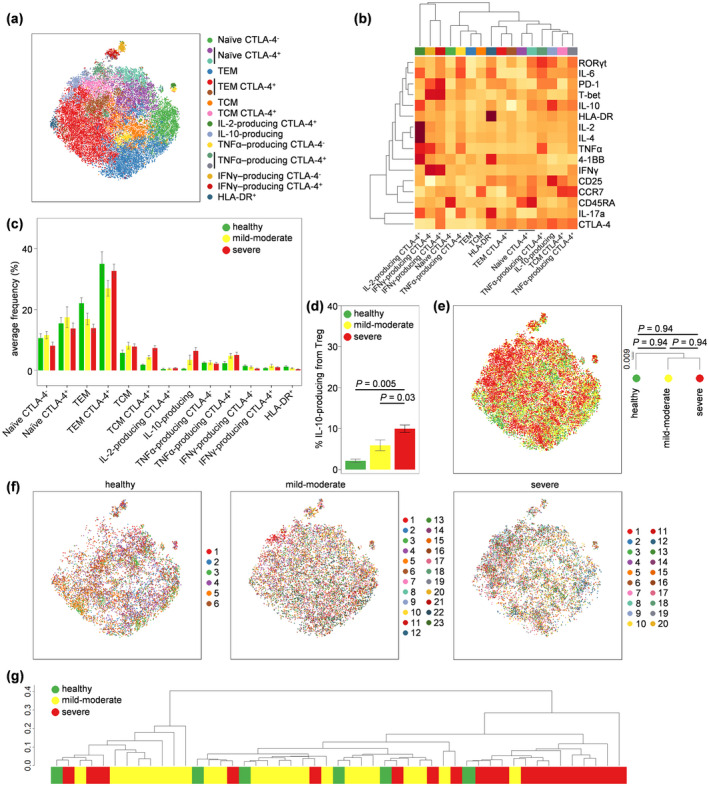
Altered regulatory T‐cell phenotypes in severe and moderate COVID‐19. PBMCs were isolated from healthy controls (n = 6), mild‐to‐moderate COVID‐19 patients (n = 23) and severe COVID‐19 patients (n = 20), stimulated and assessed through flow cytometry. CD3+CD14−CD4+CD8−FOXP3+ regulatory T cells were manually gated in FlowJo. (a) tSNE representation of regulatory T cells based on the expression of phenotypic markers: CD45RA, CCR7, 4‐1BB, CD25, CTLA‐4, HLA‐DR, IFNγ, IL‐2, IL‐4, IL‐6, IL‐10, IL‐17a, PD‐1, RORγt, T‐BET and TNFα. FlowSOM clusters were annotated based on (b) expression of phenotypic markers across each cluster (see also Supplementary figure 3). (c) Quantification of regulatory T‐cell subsets in healthy, mild‐to‐moderate COVID‐19 and severe COVID‐19 patients. (d) Manually gated IL‐10+ regulatory T cells in healthy, mild‐to‐moderate COVID‐19 and severe COVID‐19 patients. (e) tSNE representation of PBMC populations based on aforementioned phenotypic markers for each condition, namely healthy controls, mild‐to‐moderate COVID‐19 and severe COVID‐19 patients. The dendrogram shows the comparative similarity based on the Kolmogorov–Smirnov statistic calculated using the cross‐entropy distributions derived from tSNE. (f) tSNE representation of PBMC populations based on aforementioned phenotypic markers for each condition, namely healthy controls, mild‐to‐moderate COVID‐19 and severe COVID‐19 patients, with each individual represented in a different colour. (g) Dendrogram showing the comparative similarity between individuals based on the Kolmogorov–Smirnov statistic calculated using the cross‐entropy distributions derived from tSNE. Mean ± SEM.
Finally, we investigated changes in the CD8+ T‐cell compartment. Twelve subsets of CD8+ T cells were identified that correlate to biologically distinct functions: naïve CTLA‐4−, naïve CTLA‐4+, TEM, TEM Th1, TEM Tc1 IL‐2+, TEM Tc1/17, TEM Tc17, TEM IL‐2+, TEM TNFα+, TCM CTLA‐4+, TEMRA and TEMRA Tc1 (Figure 4a and b, Supplementary figure 4). Quantification of individual subsets did not identify any significant changes (Figure 4c); however, the highly inflammatory TEM Tc1/Tc17 population (expressing both IFNγ and IL‐17) was 13‐fold more numerous in COVID‐19 patients than in healthy controls, with 27/43 (63%) COVID‐19 patients exhibiting numbers > 2 standard deviations above the average of healthy individuals (Figure 4d, Supplementary table 1). This population did not discriminate between mild‐to‐moderate and severe COVID‐19 patients. At a global level, the cellular phenotype of CD8+ T cells was largely unchanged by COVID‐19‐status, using both pooled (Figure 4e) and individual (Figure 4f and g) analysis. Together, these data suggest an ongoing CD8 T‐cell response in COVID‐19 patients, with expansion of the potent Tc1/Tc17 TEM subset; however, the comparative weakness of the response and its failure to predict disease severity argue against systemic CD8 T‐cell responses being a pathogenic driver.
Figure 4.
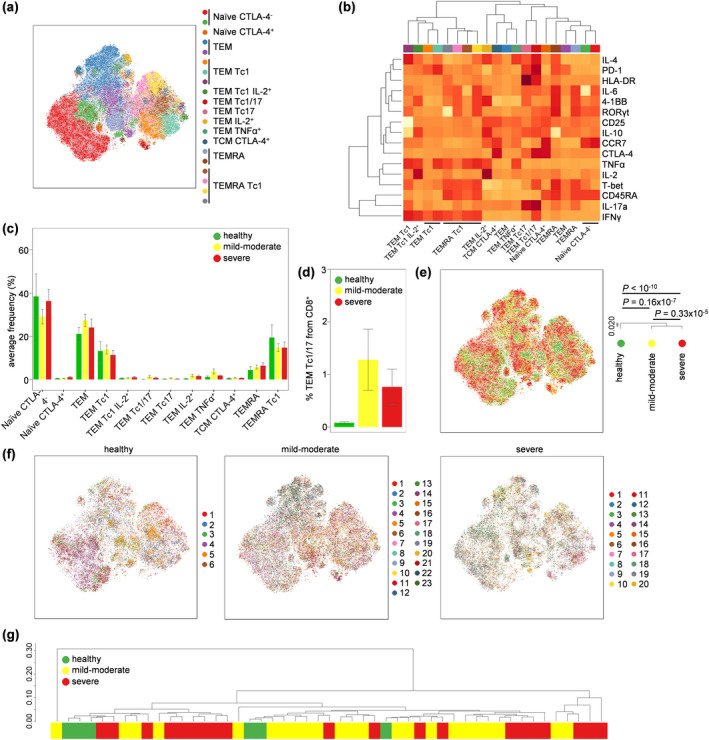
Profound activation of CD8+ T cells in both severe and moderate COVID‐19. PBMCs were isolated from healthy controls (n = 6), mild‐to‐moderate COVID‐19 patients (n = 23) and severe COVID‐19 patients (n = 20), stimulated and assessed through flow cytometry. CD3+CD14−CD4−CD8+ T cells were manually gated in FlowJo. (a) tSNE representation of CD8 T‐cell cluster populations based on the expression of phenotypic markers: CD45RA, CCR7, 4‐1BB, CD25, CTLA‐4, HLA‐DR, IFNγ, IL‐2, IL‐4, IL‐6, IL‐10, IL‐17a, PD‐1, RORγt, T‐BET and TNFα. FlowSOM clusters were annotated based on (b) expression of phenotypic markers across each cluster (see also Supplementary figure 4). (c) Quantification of CD8 T‐cell subsets in healthy, moderate COVID‐19 patients and severe COVID‐19 patients. (d) Detailed depiction of TEM Tc1/17 from CD8+ cells in healthy, mild‐to‐moderate COVID‐19 and severe COVID‐19 patients. (e) tSNE representation of PBMC populations based on aforementioned phenotypic markers for each condition, namely healthy controls, mild‐to‐moderate COVID‐19 and severe COVID‐19 patients. The dendrogram shows the comparative similarity based on the Kolmogorov–Smirnov statistic calculated using the cross‐entropy distributions derived from tSNE. (f) tSNE representation of PBMC populations based on aforementioned phenotypic markers for each condition, namely healthy controls, mild‐to‐moderate COVID‐19 and severe COVID‐19 patients, with each individual represented in a different colour. (g) Dendrogram showing the comparative similarity between individuals based on the Kolmogorov–Smirnov statistic calculated using the cross‐entropy distributions derived from tSNE. Mean ± SEM.
As a resource to the COVID‐19 research community, we provide in Supplementary table 1 the quantification of leukocyte subsets at an individual level, paired with demographic and clinical correlates. We further advocate for independent analysis of this resource, with the raw data available from https://flowrepository.org/experiments/2713.
Discussion
In this study, we present an in‐depth investigation of the T‐cell compartment of mild‐to‐severe COVID‐19 patients, using a platform with the capacity to investigate both intracellular transcription factor expression and, in parallel, functional cytokine production on a single cell level. Strikingly, COVID‐19 patients that required hospitalisation due to their condition harboured a peripheral T‐cell landscape that did not differ substantially from the healthy control one regarding the viral response. This is in stark contrast to the normal phenotype arising with viral infections, which specifically trigger Th1/Tc1‐driven responses, with increased secretion of IFNγ and cytotoxic capacity. This condition has been particularly well studied in the case of influenza which could be considered to date one of the most prevalent respiratory viral infections. 25 , 26 , 27 However, patients infected with SARS‐CoV‐2 do not display this distinct Th1/Tc1 polarisation. While the mechanism for this polarisation failure remains unknown, a potential explanation lies in the presence of a strong IL‐6 environment. 1 , 28 , 29 IL‐6 is known to affect the Th1/Tc1 response by direct inhibition of IFNγ gene expression. 30 , 31 Accordingly, this observation would support ongoing clinical trials testing the efficacy of tocilizumab in COVID‐19 patients.
Our results are in line with recent studies regarding the absence of pro‐inflammatory cytokines in the T‐cell compartment 32 or even a decrease of CD4+ secreting IFNγ. 3 These contrast with data identifying a Th1 signature in COVID‐19 patients; the latter, however, being based on convalescent and non‐hospitalised patients. 33 Intriguingly, IFNγ levels in COVID‐19 patient serum have been reported to be slightly elevated compared to healthy controls. 1 If this is not due to differences in the patient cohort, the lack of a Tc1/Th1 phenotype would suggest a myeloid origin as the IFNγ source.
Our study was not able to unravel one of the most prominent features of COVID‐19, the prevalent lymphopenia observed in most of the severely affected patients. In our study, both T and B lymphocyte compartments were affected equally, with a possible predominance for CD8+ T cells. Importantly, naïve T cells remained present in normal, or elevated, numbers, suggesting that T‐cell production/renewal was intact. Interestingly, this lymphocytopenia seems to be systemic, as previous studies in SARS‐CoV‐1 34 and recently in COVID‐19 patient autopsy revealed a pan‐depletion in all secondary lymphoid organs, including satellite mediastinal lymph nodes with a disrupted architecture 35 (CONTAGIOUS consortium, unpublished data). As massive lymphocyte infiltrates are not reported in lung anatomopathological investigations, lymphodepletion is unlikely to be explained by active recruitment of T cells to the lung tissues. An alternative cause of this lymphodepletion would be an increased T‐cell death, either through direct viral cytolysis or increased apoptosis through activation induced cell death (AICD). While lymphopenia may remain an epiphenomenon, the paucity of T cells may equally be contributing to disease. This is tentatively supported by results showing HIV‐positive patients with a slight trend towards poorer COVID‐19 outcome. 36 , 37 , 38 In addition, patients who received haematopoietic stem cell transplantation (HSCT), which leads to profound T‐cell lymphopenia, 39 seem to have a worse outcome after SARS‐CoV‐2 infection, since preliminary data suggest 30% mortality according to an ongoing European Society for Blood and Marrow Transplantation survey. 40 The loss of B cells is less likely to contribute to disease, with patients who are genetically depleted of B cells showing normal outcomes. 41 , 42
While the overall T‐cell compartment did not display major differences in comparison with healthy controls, there were two particular enriched T‐cell subsets in more severely affected patients that could reflect the inflammatory condition present in COVID‐19 patients. The inflammatory subset Tc1/Tc17 represents highly activated T cells with high expression of PD‐1 and HLA‐DR in addition to its ability to secrete both IFNγ and IL‐17 cytokines. The presence of this population may reflect a deviation from the normal Tc1 anti‐viral response caused by the pro‐inflammatory IL‐6‐enriched environment. 43 The contribution of this population to the inflammatory setting is, however, debatable, as the increase in relative number is mitigated by the lymphopenia, and no differences were observed between the mild‐to‐moderate and severe COVID‐19 patients.
The only peripheral biomarker that did delineate disease severity was the increase in IL‐10‐producing regulatory T cells. Elevated IL‐10 has been observed in the serum of COVID‐19 patients before 3 ; however, the cellular source was not elucidated. Production of IL‐10 is a hallmark of activated regulatory T cells that reside in tissues such as the lung. This population, normally rare in healthy individuals, rose up to ~ 10% of the regulatory T‐cell pool in severe COVID‐19 patients. The murine analogue to this population has a potent ability to limit inflammation and tissue damage triggered by microbial and environmental interactions at mucosal surfaces. 23 , 44 In the case of viral infections of the lung, IL‐10 restrains the development of IL‐17‐producing cells that damage the tissue, 45 , 46 inhibits the innate inflammatory response to viral particles, and is likely beneficial in reducing the production of cytokines such as IL‐6 that have been implicated in COVID‐19 morbidity. 47 , 48 Increase of this suppressive regulatory T‐cell subset could be a direct response to the progressing lung inflammation in COVID‐19 patients, comprising a feedback inhibition circuit to prevent runaway inflammation and death. 49 Potentially, elevated IL‐10 could provide a blood‐based biomarker for cases progressing to more severe lung damage. A more intriguing possibility is that individuals with higher IL‐10‐producing regulatory T cells exhibit defective adaptive immunity. IL‐10+ regulatory T cells are symptomatic of many unresolved viral infections and are associated with long‐term persistence. In respiratory infections, IL‐10 potently suppresses anti‐viral responses 44 , 50 and weakens the immune reaction to superinfection with bacteria. 51 , 52 Since secondary infection leading to pneumonia is a major cause of death in influenza, and perhaps for some COVID‐19 patients as well, 53 , 54 , 55 excessive IL‐10 production by regulatory T cells may be a key factor in COVID‐19 outcomes. In principle, this truncated adaptive immune response could allow persistent infection and cause an over‐reliance on innate responses, driving the pathological state. Under this latter model, early intervention (such as with IL‐10 neutralisation) could potentially restore appropriate adaptive immunity and quieten the excessively exuberant innate response in the tissue. However, key replication, longitudinal and mechanistic studies would be first required, and IL‐10 has proven stubbornly refractory to immune modulation in the past. 56
Key limitations in our study are the study size and the cross‐sectional nature. The data presented here rely on a small number of patients without longitudinal follow‐up, and lacking asymptomatic patients to screen the full spectrum of the COVID‐19 immune signature. Study expansion and follow‐up are ongoing to correct these deficits and identify key components of the immune system responsible for a better protection against SARS‐CoV‐2. The other major limitation of the current work is the focus on T cells. With the limited phenotype changes observed here, a more comprehensive study of systemic myeloid cell changes in COVID‐19 would be justified. Altogether, our study highlights the absence of a strong anti‐viral response against SARS‐CoV‐2 across mild‐to‐severe COVID‐19 patients and the elevated presence of anti‐inflammatory IL‐10‐producing regulatory T cells in the severely affected patients. These data suggest that a route to normalisation of anti‐SARS‐CoV‐2 immunity is critical in the attempt to cure these patients. Finally, with the intent to share and exchange knowledge to accelerate research on this pandemic, our data are available on the following open access repository for further investigation: https://flowrepository.org/experiments/2713.
Methods
Patient material
Healthy controls and symptomatic SARS‐CoV‐2‐infected patients (qPCR confirmed) were collected as part of the CONTAGIOUS consortium (CONTAGIOUS consortium, unpublished data). Briefly, between 27th March and 17th April 2020, healthy volunteers and adult COVID‐19 patients were recruited at COVID‐19 hospitalisation ward at UZ Leuven (Leuven, Belgium) after informed consent. COVID‐19 diagnosis was made based on a positive qRT‐PCR on respiratory sample and/or CT imaging compatible with SARS‐CoV‐2 disease. Patients were classified as mild‐to‐moderate (WHO clinical score 3–4) or severe (WHO clinical score 5–7) at point of sampling. All procedures were approved by the UZ Leuven Ethical Committee (protocol study number S63881). Blood samples from healthy controls and patients were stored at 15°C for 3–6 h prior to peripheral blood mononuclear cells (PBMCs) isolation using lymphocyte separation medium (LSM; MP Biomedicals, Santa Ana, CA, USA) and freezing in liquid nitrogen. Whole blood count and differential values from the clinical laboratory were obtained concomitantly or within the 24 h of the blood sample for the flow cytometry analysis.
Flow cytometry
Frozen PBMCs were thawed, plated and incubated for 4 h with complete RPMI containing phorbol myristate acetate (PMA 50 ng mL−1), ionomycin (500 ng mL−1) and Brefeldin A (8 µg mL−1; all Tocris Bioscience, Bristol, UK) at 37°C with 5% CO2. Cells were then washed twice with PBS (Fisher Scientific, Hampton, NH, USA) and stained with live/dead marker (fixable viability dye eFluor780; eBioscience, San Diego, CA, USA) and fluorochrome‐conjugated antibodies against surface markers: anti‐CD14 (TuK4), anti‐CCR7 (G043H7) (eBioscience); anti‐CD3 (REA613) (Miltenyi Biotec, Bergisch Gladbach, Germany); anti‐CD4 (SK3), anti‐CD8 (SK1), anti‐PD1 (EH12.1), anti‐CD45RA (HI100) (all from BD Biosciences, San Jose, CA, USA); and anti‐CD25 (BC96), anti‐HLA‐DR (L243), anti‐CD40L (24–31), anti‐4‐1BB (4B4‐1), anti‐CD19 (HIB19) (all from BioLegend, San Diego, CA, USA). Cells were fixed with 2% Formaldehyde (VWR chemicals, Radnor, Pennsylvania, PA, USA) and then permeabilised with eBioscience permeabilisation buffer according to manufacturer’s instructions. Cells were stained overnight at 4°C with anti‐IFNγ (4S.B3), anti‐IL‐6 (MQ2‐13A5), anti‐IL17a (N49‐653), anti‐RORγt (Q21‐559), anti‐IL‐2 (MQ1‐17H12), anti‐IL‐10 (JES3‐9D7), anti‐T‐bet (4B10), anti‐CTLA‐4 (BNI3), anti‐GATA3 (L50‐823) (all from BD Biosciences); anti‐IL‐4 (MP4‐25D2), anti‐TNFα (Mab11), anti‐FOXP3 (206D) (all from BioLegend). Data were collected on BD Symphony (BD Biosciences). A maximum of 5 × 105 events were acquired for each sample. tSNE, FlowSOM and heatmap analysis were performed in R (version 3.6.2). Raw.fcs data were compensated using AutoSpill, 22 and dead cells and debris were gated out prior to file export. The complete set of FCS files used for the COVID‐19 cytokine immune phenotyping has been deposited on FlowRepository and annotated in accordance with the MIFlowCyt standard. These files may be downloaded for further analysis from https://flowrepository.org/experiments/2713.
Flow cytometry analysis
The concatenated data set was analysed through successive FlowSOM clustering and tSNE representation after exporting similar event numbers for each sample per condition group and then subsampling equal event numbers per condition. First, lineage markers (CD3, CD4, CD8, FOXP3, CD19, CD14) were used to separate leukocyte subsets. Second, activation markers (4‐1BB, CCR7, CD25, CD45RA, CTLA‐4, HLA‐DR, IFNγ, IL‐2, IL‐4, IL‐6, IL‐10, IL‐17a, PD‐1, RORγt, T‐bet, TNFα) were used to distinguish phenotypic clusters of each leukocyte subset, again using FlowSOM and tSNE. The characteristics of each identified cluster were assessed by means of histograms and heatmaps. Comparisons between groups (healthy, moderate COVID‐19 and severe COVID‐19) were performed with tests on the cross‐entropy distributions of the tSNE representations of each group. In brief, for the original and t‐SNE space of each tSNE plot, a probability per data point was calculated following the same approach as in the tSNE algorithm. From these point probabilities, the distribution of cross‐entropy in the tSNE space relative to the original space was obtained for each group represented in the plot. All pairwise comparisons between groups were evaluated with Kolmogorov–Smirnov tests on the difference between the cross‐entropy distributions. Resulting P‐values were corrected with the Holm method. Dendrograms were obtained from hierarchical clustering, using as distance the Kolmogorov–Smirnov statistic, that is, the L‐infinity distance between the cross‐entropy distributions CONTAGIOUS consortium, unpublished data).
Conflict of interest
The authors declare no conflict of interest.
Author contributions
Julika Neumann: Formal analysis; Investigation; Visualization; Writing‐original draft. Teresa Prezzemolo: Investigation; Methodology. Lore Vanderbeke: Investigation; Resources. Carlos P. Roca: Software; Visualization. Margaux Gerbaux: Writing‐original draft. Silke Janssens: Investigation. Mathijs Willemsen: Investigation. Oliver Burton: Methodology. Pierre Van Mol: Resources. Yannick Van Herck: Resources. Joost Wauters: Conceptualization; Resources; Supervision. Els Wauters: Conceptualization; Resources; Supervision. Adrian Liston: Conceptualization; Project administration; Supervision; Visualization; Writing‐original draft; Writing‐review & editing. Stephanie Humblet‐Baron: Conceptualization; Formal analysis; Project administration; Supervision; Visualization; Writing‐original draft; Writing‐review & editing.
Supporting information
Acknowledgments
This work was supported by the VIB Grand Challenges Program, the KUL C1 program, the FWO Hercules program, the European Union’s Horizon 2020 research and innovation programme under grant agreement No. 779295 (to AL), and the Biotechnology and Biological Sciences Research Council through Institute Strategic Program Grant funding BBS/E/B/000C0427 and BBS/E/B/000C0428, and the Biotechnology and Biological Sciences Research Council Core Capability Grant to the Babraham Institute. MG is supported by a fellowship from the Belgian Kid’s Fund. The authors acknowledge the important contributions of the COVID‐19 clinical team and Pier‐Andrée Penttila and the KUL FACS Core. We are grateful to Per Lungman who kindly provided us with data on COVID‐19 disease after HSCT. The manuscript is dedicated to the memory of Michael Wakelam (Babraham Institute).
CONTAGIOUS co‐authors
Francesca Bosisio, Frederik De Smet, Christophe Dooms, Abhishek Garg, Jan Gunst, Greet Hermans, Diether Lambrechts, Natalie Lorent, Kim Martinod, Patrick Matthys, Philippe Meersseman, Johan Neyts, Paul Proost, Jeroen Raes, Sabine Tejpar, Dries Testelmans, Karin Thevissen, Robin Vos, Birgit Weynand, Alexander Wilmer, Carine Wouters, Jonas Yserbyt
Contributor Information
Adrian Liston, Email: adrian.liston@babraham.ac.uk.
Stephanie Humblet‐Baron, Email: stephanie.humbletbaron@kuleuven.be.
CONTAGIOUS co‐authors:
Francesca Bosisio, Frederik De Smet, Christophe Dooms, Abhishek Garg, Jan Gunst, Greet Hermans, Diether Lambrechts, Natalie Lorent, Kim Martinod, Patrick Matthys, Philippe Meersseman, Johan Neyts, Paul Proost, Jeroen Raes, Sabine Tejpar, Dries Testelmans, Karin Thevissen, Robin Vos, Birgit Weynand, Alexander Wilmer, Carine Wouters, and Jonas Yserbyt
References
- 1. Hadjadj J, Yatim N, Barnabei L et al Impaired type I interferon activity and exacerbated inflammatory responses in severe Covid‐19 patients. Science 2020; 369: 718–724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Zheng M, Gao Y, Wang G et al Functional exhaustion of antiviral lymphocytes in COVID‐19 patients. Cell Mol Immunol 2020; 17: 533–535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Chen G, Wu D, Guo W et al Clinical and immunological features of severe and moderate coronavirus disease 2019. J Clin Invest 2020; 130: 2620–2629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Zheng H‐Y, Zhang M, Yang C‐X et al Elevated exhaustion levels and reduced functional diversity of T cells in peripheral blood may predict severe progression in COVID‐19 patients. Cell Mol Immunol 2020; 17: 541–543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Qin C, Zhou L, Hu Z et al Dysregulation of immune response in patients with coronavirus 2019 (COVID‐19) in Wuhan, China. Clin Infect Dis 2020; 71: 762–768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bost P, Giladi A, Liu Y et al Host‐viral infection maps reveal signatures of severe COVID‐19 patients. Cell 2020; 181: 1475–1488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Herold S, Becker C, Ridge KM, Budinger GRS. Influenza virus‐induced lung injury: pathogenesis and implications for treatment. Eur Respir J 2015; 45: 1463–1478. [DOI] [PubMed] [Google Scholar]
- 8. Cavalli G, De Luca G, Campochiaro C et al Interleukin‐1 blockade with high‐dose anakinra in patients with COVID‐19, acute respiratory distress syndrome, and hyperinflammation: a retrospective cohort study. Lancet Rheumatol 2020; 2: e325–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Toniati P, Piva S, Cattalini M et al Tocilizumab for the treatment of severe COVID‐19 pneumonia with hyperinflammatory syndrome and acute respiratory failure: A single center study of 100 patients in Brescia, Italy. Autoimmun Rev 2020; 19: 102568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Xu X, Han M, Li T et al Effective treatment of severe COVID‐19 patients with tocilizumab. Proc Natl Acad Sci USA 2020; 117: 10970–10975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Merad M, Martin JC. Pathological inflammation in patients with COVID‐19: a key role for monocytes and macrophages. Nat Rev Immunol 2020; 20: 355–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Zhou Y, Fu B, Zheng X et al Pathogenic T‐cells and inflammatory monocytes incite inflammatory storm in severe COVID‐19 patients. Natl Sci Rev 2020; 7: 998–1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Diao B, Wang C, Tan Y et al Reduction and functional exhaustion of T cells in patients with coronavirus disease 2019 (COVID‐19). Front Immunol 2020; 11: 827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Yang Y, Shen C, Li J et al Plasma IP‐10 and MCP‐3 levels are highly associated with disease severity and predict the progression of COVID‐19. J Allergy Clin Immunol 2020; 146: e119–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Liu T, Zhang J, Yang Y et al The potential role of IL‐6 in monitoring coronavirus disease 2019. SSRN Electron J 2020. [Google Scholar]
- 16. De Biasi S, Emilia R, Campi V, Meschiari M, Gibellini L. Marked T cell activation, senescence, exhaustion and skewing towards TH17 in patients with COVID‐19 pneumonia. Nat Commun 2020; 11: 3434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Zheng Y, Huang Z, Yin G et al Study of the lymphocyte change between COVID‐19 and non‐COVID‐19 pneumonia cases suggesting other factors besides uncontrolled inflammation contributed to multi‐organ injury. medRxiv 2020. 10.1101/2020.02.19.20024885 [DOI] [Google Scholar]
- 18. Zhang D, Guo R, Lei L et al COVID‐19 infection induces readily detectable morphological and inflammation‐related phenotypic changes in peripheral blood monocytes. J Leukoc Biol 2020;1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Liao M, Liu Y, Yuan J et al Single‐cell landscape of bronchoalveolar immune cells in patients with COVID‐19. Nat Med 2020; 26: 842–844. [DOI] [PubMed] [Google Scholar]
- 20. Yang X, Dai T, Zhou X et al Analysis of adaptive immune cell populations and phenotypes in the patients infected by SARS‐CoV‐2. medRxiv 2020. 10.1101/2020.03.23.20040675 [DOI] [Google Scholar]
- 21. Glasziou PP, Sanders S, Hoffmann T. Waste in covid‐19 research. BMJ 2020; 369: m1847. [DOI] [PubMed] [Google Scholar]
- 22. Roca CP, Burton OT, Prezzemolo T et al AutoSpill: a method for calculating spillover coefficients in high‐parameter flow cytometry. bioRxiv 2020. 10.1101/2020.06.29.177196 [DOI] [Google Scholar]
- 23. Rubtsov YP, Rasmussen JP, Chi EY et al Regulatory T cell‐derived interleukin‐10 limits inflammation at environmental interfaces. Immunity 2008; 28: 546–558. [DOI] [PubMed] [Google Scholar]
- 24. Miyara M, Yoshioka Y, Kitoh A et al Functional delineation and differentiation dynamics of human CD4+ T cells expressing the FoxP3 transcription factor. Immunity 2009; 30: 899–911. [DOI] [PubMed] [Google Scholar]
- 25. Chen K, Kolls JK. T cell‐mediated host immune defenses in the lung. Annu Rev Immunol 2013; 31: 605–633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Zielinski CE, Corti D, Mele F, Pinto D, Lanzavecchia A, Sallusto F. Dissecting the human immunologic memory for pathogens. Immunol Rev 2011; 240: 40–51. [DOI] [PubMed] [Google Scholar]
- 27. Wong S‐S, Oshansky CM, Guo X‐ZJ et al Severe influenza is characterized by prolonged immune activation: results from the SHIVERS cohort study. J Infect Dis 2018; 217: 245–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Blanco‐Melo D, Nilsson‐Payant BE, Liu W‐C et al Imbalanced host response to SARS‐CoV‐2 drives development of COVID‐19. Cell 2020; 181: 1036–1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Chen R, Sang L, Jiang M et al Longitudinal hematologic and immunologic variations associated with the progression of COVID‐19 patients in China. J Allergy Clin Immunol 2020; 146: 89–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Diehl S, Anguita J, Hoffmeyer A et al Inhibition of Th1 differentiation by IL‐6 is mediated by SOCS1. Immunity 2000; 13: 805–815. [DOI] [PubMed] [Google Scholar]
- 31. Yang R, Masters AR, Fortner KA et al IL‐6 promotes the differentiation of a subset of naive CD8+ T cells into IL‐21–producing B helper CD8+ T cells. J Exp Med 2016; 213: 2281–2291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Wilk AJ, Rustagi A, Zhao NQ et al A single‐cell atlas of the peripheral immune response to severe COVID‐19. Nat Med 2020; 26: 1070–1076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Grifoni A, Weiskopf D, Ramirez SI et al Targets of T cell responses to SARS‐CoV‐2 coronavirus in humans with COVID‐19 disease and unexposed individuals. Cell 2020; 181: 1489–1501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Gu J, Korteweg C. Pathology and pathogenesis of severe acute respiratory syndrome. Am J Pathol 2007; 170: 1136–1147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Chen Y, Feng Z, Diao B et al The novel severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) directly decimates human spleens and lymph nodes. medRxiv 2020. 10.1101/2020.03.27.20045427 [DOI] [Google Scholar]
- 36. Blanco JL, Ambrosioni J, Garcia F et al COVID‐19 in patients with HIV: clinical case series. Lancet HIV 2020; 7: e314–e316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Kamen‐Tuohy S, Carlucci PM, Zacharioudakis IM et al Outcomes among HIV‐positive patients hospitalized with COVID‐10. J Acquir Immune Defic Syndr 2020; 85: 6–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Härter G, Spinner CD, Roider J et al COVID‐19 in people living with human immunodeficiency virus: a case series of 33 patients. Infection 2020; 48: 681–686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hannon M, Beguin Y, Ehx G et al Immune recovery after allogeneic hematopoietic stem cell transplantation following flu‐TBI versus TLI‐ATG conditioning. Clin Cancer Res 2015; 21: 3131–3139. [DOI] [PubMed] [Google Scholar]
- 40. Ljungman P, Styczynski J, Mikulska M, De la Camara R.Coronavirus Disease Covid‐19: Ebmt Recommendations Version 8 – May 18, 2020.
- 41. Quinti I, Lougaris V, Milito C et al A possible role for B cells in COVID‐19? Lesson from patients with agammaglobulinemia. J Allergy Clin Immunol 2020; 146: 211–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Soresina A, Moratto D, Chiarini M et al Two X‐linked agammaglobulinemia patients develop pneumonia as COVID‐19 manifestation but recover. Pediatr Allergy Immunol 2020; 31: 565–569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Gartlan KH, Markey KA, Varelias A et al Tc17 cells are a proinflammatory, plastic lineage of pathogenic CD8+ T cells that induce GVHD without antileukemic effects. Blood 2015; 126: 1609–1620. [DOI] [PubMed] [Google Scholar]
- 44. Bedoya F, Cheng G‐S, Leibow A et al Viral antigen induces differentiation of Foxp3+ natural regulatory T cells in influenza virus‐infected mice. J Immunol 2013; 190: 6115–6125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Chaudhry A, Samstein RM, Treuting P et al Interleukin‐10 signaling in regulatory T cells is required for suppression of Th17 cell‐mediated inflammation. Immunity 2011; 34: 566–578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. McKinstry KK, Strutt TM, Buck A et al IL‐10 deficiency unleashes an influenza‐specific Th17 response and enhances survival against high‐dose challenge. J Immunol 2009; 182: 7353–7363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Chang J, Kunkel SL, Chang C‐H. Negative regulation of MyD88‐dependent signaling by IL‐10 in dendritic cells. Proc Natl Acad Sci USA 2009; 106: 18327–18332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Coomes EA, Haghbayan H. Interleukin‐6 in Covid‐19: a systematic review and meta‐analysis. Rev Med Virol 2020; e2141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Rojas JM, Avia M, Martín V, Sevilla N. IL‐10: a multifunctional cytokine in viral infections. J Immunol Res 2017; e6104054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Sun K, Torres L, Metzger DW. A detrimental effect of interleukin‐10 on protective pulmonary humoral immunity during primary influenza A virus infection. J Virol 2010; 84: 5007–5014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Barthelemy A, Ivanov S, Fontaine J et al Influenza A virus‐induced release of interleukin‐10 inhibits the anti‐microbial activities of invariant natural killer T cells during invasive pneumococcal superinfection. Mucosal Immunol 2017; 10: 460–469. [DOI] [PubMed] [Google Scholar]
- 52. van der Sluijs KF, van Elden LJR, Nijhuis M et al IL‐10 is an important mediator of the enhanced susceptibility to pneumococcal pneumonia after influenza infection. J Immunol 2004; 172: 7603–7609. [DOI] [PubMed] [Google Scholar]
- 53. Cox MJ, Loman N, Bogaert D, O’Grady J. Co‐infections: potentially lethal and unexplored in COVID‐19. Lancet Microbe 2020; 1: e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Morens DM, Taubenberger JK, Fauci AS. Predominant role of bacterial pneumonia as a cause of death in pandemic influenza: implications for pandemic influenza preparedness. J Infect Dis 2008; 198: 962–970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Zhou F, Yu T, Du R et al Clinical course and risk factors for mortality of adult inpatients with COVID‐19 in Wuhan, China: a retrospective cohort study. Lancet 2020; 395: 1054–1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Saxena A, Khosraviani S, Noel S, Mohan D, Donner T, Hamad ARA. Interleukin‐10 paradox: a potent immunoregulatory cytokine that has been difficult to harness for immunotherapy. Cytokine 2015; 74: 27–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


