Abstract
Background
We examined the association between improved mobility and distal health outcomes in older adults using secondary analysis of data from a cluster-randomized controlled group exercise trial.
Methods
Participants were 303 men and women aged ≥65 and older in 32 independent living facilities, senior apartments, and community centers who participated in 12-week group exercise interventions. Included were those who completed ≥1 follow-up phone call regarding outcomes assessment in the following year. Gait speed and 6-minute walk distance (6MWD) were assessed at baseline and immediately after 12-week interventions to determine mobility performance change status. Falls, emergency department (ED) visits, and hospitalizations were assessed monthly for 12 months following the end of interventions via interactive voice response phone calls. Incident rate ratios (IRRs) were calculated to quantify incidence of adverse outcomes with respect to mobility performance change.
Results
Each 0.05 m/s increase in gait speed resulted in an 11% reduction in falls (IRR = 0.89; 95% confidence interval [CI], 0.84–0.94; p < .0001); a similar decrease was seen for each 20 m increase in 6MWD (IRR = 0.89; 95% CI, 0.83–0.93; p = .0003). Those who improved gait speed had 61 falls per 1,000 person-months versus 135 in those who had no change/a decline. Those who improved 6MWD had 67 falls per 1,000 person-months versus 110 per 1,000 person-months in those who had no change/a decline. Differences in ED visits and hospitalizations were not statistically significant.
Conclusion
Improvements in mobility performance are associated with lower incidence of future falls. Given the exploratory nature of the findings, further investigation is warranted.
Keywords: Gait, Falls, Outcomes, Physical activity
Mobility is a useful clinical indicator of the overall health of older adults. It can act as a marker of the functioning of multiple physiologic systems and how well these systems interact with one another (1). As of 2013, over a quarter of those 65 years and older in the United States reported experiencing mobility disability, defined as self-reported general difficulty walking or climbing a flight of stairs (2). Mobility disability can lead to numerous negative health outcomes and high healthcare costs (3). As assessed in longitudinal studies of the natural history of mobility ability using a single performance measure at one point in time, limitations in mobility performance predict nursing home admission, hospitalization, falls, all-cause disability, and all-cause mortality (4–10).
Gait speed and 6-minute walk distance (6MWD) are commonly used measures of mobility performance and are modifiable through rehabilitative interventions (11–17). Whether improvements in mobility performance are associated with lower future falls, emergency department (ED) visits, or hospitalization is largely unknown. A decline in measured gait speed over 1 year was associated with worse survival rates in 5 years (18). Conversely, improved self-reported mobility over 1 year was associated with improved survival rates in the following 8 years (19). In these studies, the focus was natural change in mobility considered over a year and not change in mobility related to behavioral modification, such as participation in group exercise or rehabilitation.
We sought to determine whether changes in mobility performance after participation in a 3-month group exercise program had an impact on the 1-year incidence of the distal adverse health outcomes of falls, ED visits, and hospitalization. We hypothesized that improvements in mobility performance would be associated with a lower incidence of each of these outcomes.
Methods
Design
We used data from a cluster-randomized controlled trial of two group exercise interventions to improve mobility in community-dwelling older adults. The parent study has been described previously (12,20). Briefly, community-dwelling older adults (≥65 years) participated in an hour of group exercise twice a week for 12 weeks. Randomization occurred at the facility level (ie, senior centers, independent living facilities, and senior subsidized apartment buildings) to limit intervention contamination with the group nature of the program. The facilities were randomized to either a usual care seated strengthening and endurance program or a motor control program with walking and stepping patterns designed to improve their mobility through timing and coordination activities related to walking. After completion of the program, participants were followed for 12 months via automated phone calls. The overall attrition in the parent study was approximately 4%. All facilities were in the greater Pittsburgh, Pennslyvania area. The parent study was registered on clinicaltrials.gov (NCT01986647). The study was approved by the University of Pittsburgh Institutional Review Board. Signed informed consent was obtained from all participants.
Our goal was to examine the association of outcomes with mobility performance improvement after exercise, regardless of type of exercise. As such, we collapsed both intervention arms to form a single cohort of individuals who were part of group exercise interventions for 12 weeks. We assessed the incidence of distal health outcomes during the following year via automated interactive voice response (IVR) phone calls.
Participants
The participants included in the parent study were community-dwelling older adults who were capable of walking household distances independently (with or without a straight cane) with a gait speed of at least 0.60 m/s. Individuals who were unable to complete the informed consent process, planning to leave the area during the trial period, diagnosed with a progressive neuromuscular disorder or an unstable medical condition were excluded. The testing was completed on-site by study personnel blinded to intervention arm. For our analysis, individuals were included if they completed at least one follow-up phone call in the 12 months following the end of the intervention.
Measures
Participant characteristics
At baseline, participants self-reported age, sex, race, height and weight (body mass index [BMI] then calculated as weight in kilograms divided by the height in meters squared), and prior year fall history. The Duke Comorbidity Index was used to measure comorbidity burden by number of body systems affected, such as neurological, cardiovascular, and musculoskeletal (21). Scores range 0–8, with lower scores indicating fewer systems affected.
Gait speed
Performance-based mobility measures were assessed at baseline and immediately upon completing the 12-week interventions. Gait speed assessments were completed using a 4.27-m (14 ft) instrumented walkway (Zeno Walkway, Prokinetics, Havertown, PA). Participants completed six passes at their usual gait speed with initial and final segments for acceleration and deceleration, respectively; the speeds were averaged over all passes for the usual gait speed recorded. Gait speed assessment is a reliable measure of mobility performance (22) with a small but meaningful change defined as 0.05 m/s (16).
Six-minute walk distance
We followed the American Thoracic Society protocol for completion of the Six-Minute Walk Test (23). At baseline and at the 12-week follow-up, participants completed the test over a 15.24 m (50 ft) course; participants could take standing rests as needed and use their typical walking for longer-than-household distances. The 6MWD has excellent reliability (24) and validity for community-dwelling older adults (25). A small but meaningful change in 6MWD is 20 m (16).
Distal health outcomes
Upon completing the intervention, participants were called by an automated IVR system monthly for 12 months (26). The system called individuals every month, twice a day for 9 days until they responded. In the phone call, participants were asked if in the past 30 days they had a fall, a visit to the ED for any reason, or a hospitalization for one or more nights. They responded “yes” or “no” by pushing buttons on their phone. The use of this IVR system has been demonstrated to be reliable relative to in-person calls to capture information from older adults (27). The present analysis included those responding to at least one phone call.
Statistical Analysis
We used appropriate descriptive statistics to summarize participant characteristics for those in the parent study who were included in and excluded from the present secondary analysis. To compare continuous measures, we used linear mixed models with subsample inclusion status (yes or no) as a fixed effect and a facility random effect to account for clustering due to facility. To compare dichotomous measures, we used generalized estimating equations (GEE) models with a binomial distribution, a logit link function, and subsample inclusion status (yes or no) as the independent variable and an exchangeable working correlation structure to account for clustering due to facility.
For the main analysis of distal health count outcomes, we computed incident rate ratios (IRRs) to express frequency of outcomes relative to the number of months participants responded to IVR calls. We operationalized mobility change in one set of models as a continuous variable and in a second set of models as dichotomous variables (participants categorized as either having achieved at least a small meaningful change in the measure or having experienced no change or a decline). We then fit a series of GEE models with counts of events as the dependent variable, a negative binomial distribution, a log link function, mobility performance change (both continuous and dichotomous operational definitions in different models) as the main independent variable of interest, and an exchangeable working correlation structure to account for clustering due to facility. IRRs for continuous operational definitions of mobility performance change were rescaled so that they are presented per 0.05 m/s in gait speed change and 20 m in 6MWD change. We successively added baseline value of mobility performance, age, race, gender, BMI, comorbidity index, and prior history of falls to examine the relation of the change in mobility performance to future adverse health outcomes. As participants from two different interventions in the parent trial had been condensed to form a single cohort, we completed a sensitivity analysis by repeating the main analysis with additional adjustment for intervention arm. SAS version 9.3 (SAS Institute, Inc., Cary, NC) was used for all statistical analyses.
Results
Of the 424 participants in the parent trial, 303 completed at least one follow-up phone call (Table 1). Those excluded were not significantly different from those included in the final sample except that those excluded had a shorter baseline 6MWD. Participants completed a median of 10 phone calls of the possible 12. Of the 303 participants, the vast majority were older, white, and female. Participants had a mean BMI of 28.96 kg/m2 and a mean of comorbidities in about three body systems. Eighty-seven (28.7%) of the participants had fallen in the prior year. At baseline, participants demonstrated mild to moderately slow gait speed with mean gait speed of 0.92 m/s, and moderately reduced mobility endurance with 6MWD of 286.7 m. There were 117 (38.6%) individuals who experienced at least a small meaningful change in gait speed and 120 (42.4%) in 6MWD.
Table 1.
Baseline Descriptive Sample Characteristics: Mean ± SD or N (%)
| Characteristics | Included (n = 303) | Excluded (n = 121) | p Value |
|---|---|---|---|
| Age in years | 80.9 ± 7.7 | 80.4 ± 8.1 | .5336 |
| Female, n (%) | 252 (83.2) | 97 (80.2) | .4659 |
| White, n (%) | 260 (85.8) | 92 (76.03) | .9018 |
| Body mass index (kg/m2) | 29.0 ± 14.6 | 28.8 ± 9.8 | .8704 |
| Comorbidity index (0–8) | 2.9 ± 1.4 | 2.7 ± 1.4 | .2603 |
| Fall in the prior year, n (%) | 87 (28.7) | 41 (33.9) | .2869 |
| Gait speed (m/s) | 0.92 ± 0.20 | 0.88 ± 0.21 | .2233 |
| Six-minute walk distance (m) | 286.7 ± 85.4 | 251.83 ± 95.04 | .0027 |
Note: Continuous measures compared using linear mixed models with subsample inclusion status (yes/no) as a fixed effect and a facility random effect to account for clustering due to facility. Dichotomous measures were compared using generalized estimating equations models with a binomial distribution, a logit link function, subsample inclusion status (yes/no) as the independent variable, and an exchangeable working correlation structure to account for clustering due to facility.
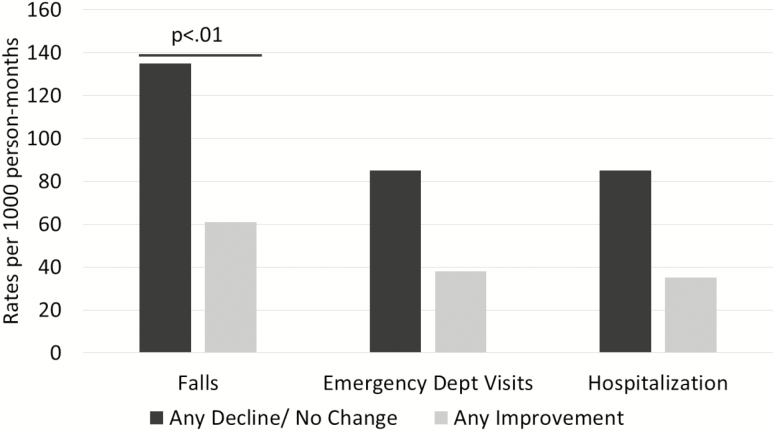
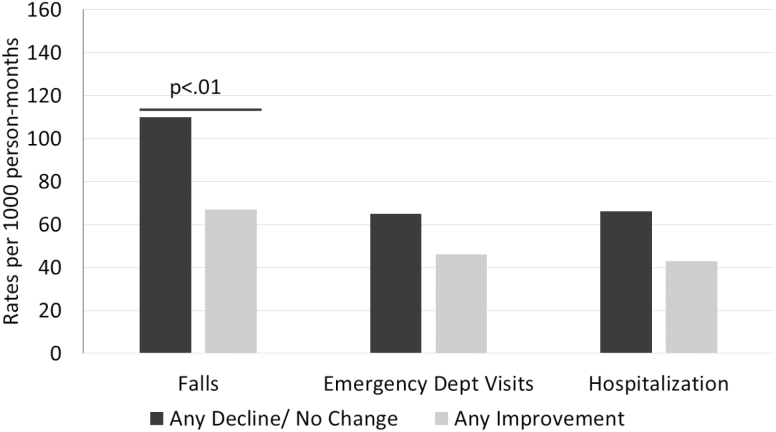
There was a reduction in incidence of negative health outcomes for clinically relevant improvements in mobility performance (Figures 1 and 2). Those who improved gait speed had 61 falls per 1,000 person-months compared to 135 in those who had no change/a decline. Those who improved 6MWD had 67 falls per 1,000 person-months compared to 110 per 1,000 person-months in those who had no change/a decline. We found no significant differences in ED visits and hospitalizations associated with improved mobility performance.
Figure 1.
Rate of outcomes by gait speed change category.
Figure 2.
Rate of outcomes by 6-minute walk distance (6MWD) change category.
When gait speed change was treated as a continuous independent variable, for every 0.05 m/s increase in gait speed from baseline to follow up, there was an 11% (p < .0001) reduction in falls in the following year, adjusting for baseline gait speed, demographics, comorbidities, and fall history (Table 2). There was a 41% (p = .0035) adjusted reduction in falls in the following year in those who improved gait speed by at least 0.05 m/s compared to those whose gait speed did not change or declined. Findings were not statistically significant for incidence of ED visits or hospitalization.
Table 2.
Association Between Mobility Performance Change and Incidence Rates of Distal Health Outcomes
| Distal Health Outcome | ||||||
|---|---|---|---|---|---|---|
| Falls | Hospitalization | ED Visit | ||||
| Mobility Performance Measure Change | IRR (95% CI) | p Value | IRR (95% CI) | p Value | IRR (95% CI) | p Value |
| Gait speed change (continuous—for each 0.05 m/s) | ||||||
| Unadjusted analysis | 0.95 (0.88–1.02) | .1425 | 0.96 (0.90–1.02) | .1474 | 0.97 (0.90–1.04) | .3745 |
| Fully-adjusted model | 0.89 (0.84–0.94) | <.0001 | 0.95 (0.90–1.01) | .0874 | 0.96 (0.90–1.03) | .2524 |
| Gait speed change (dichotomous—improvement vs no change/decline) | ||||||
| Unadjusted analysis | 0.69 (0.48–1.00) | .0510 | 0.65 (0.41–1.02) | .0631 | 1.22 (0.76–1.96) | .4065 |
| Fully-adjusted model | 0.59 (0.41–0.84) | .0035 | 0.64 (0.40–1.04) | .0702 | 0.74 (0.44–1.23) | .2460 |
| 6MWD change (continuous—for each 20 m) | ||||||
| Unadjusted analysis | 0.97 (0.90–1.05) | .4551 | 0.95 (0.88–1.02) | .1723 | 0.97 (0.89–1.06) | .4903 |
| Fully-adjusted model | 0.89 (0.83–0.95) | .0003 | 0.93 (0.86–1.00) | .0577 | 0.94 (0.86–1.03) | .2025 |
| 6MWD change (dichotomous—improvement vs no change/ decline) | ||||||
| Unadjusted analysis | 0.79 (0.54–1.14) | .1999 | 0.84 (0.54–1.31) | .4393 | 0.92 (0.51–1.67) | .7881 |
| Fully-adjusted model | 0.49 (0.34–0.70) | <.0001 | 0.74 (0.46–1.18) | .2059 | 0.77 (0.42–1.42) | .4065 |
Note: Fully-adjusted model: baseline mobility performance, age, race, gender, body mass index, comorbidity index, and fall history. CI = Confidence interval; ED = Emergency department; IRR = Incidence rate ratio; 6MWD = Six-minute walk distance.
When 6MWD change was treated as a continuous independent variable, for every 20 m increase in distance walked, there was an 11% (p = .0003) reduction in falls in the following year, adjusting for baseline distance walked, demographics, comorbidities, and fall history (Table 2). There was a 51% (p < .0001) adjusted reduction in falls in those who increased 6MWD by at least 20 m compared to those whose 6MWD did not change or declined. Findings were not statistically significant for the incidence of ED visits.
In a partially adjusted model only accounting for baseline performance, age, race, gender, and BMI, mobility improvements were associated with a decrease in hospitalizations. The findings, however, did not maintain significance when fully adjusted, including comorbidity burden and fall history (results not shown).
The sensitivity analysis results additionally adjusting for intervention arm in the parent trial demonstrated no significant differences compared to the main analysis results (Supplementary Table 2).
Discussion
Improvements in mobility performance are significantly associated with a reduction in falls. In combination with baseline mobility performance, participant characteristics, and health status, change in mobility performance is a contributing variable in regard to future incidence of falls. In a comprehensive review on mobility and physical function, Ferruci and colleagues (1) underscored the importance of walking speed and endurance as key indicators of overall health. Our results for incidence of adverse health outcomes after change in mobility performance add to this thought, indicating that experiencing a change in mobility status can have a positive impact on health outcomes.
Furthermore, the connection between mobility and falls is more direct than the connection between mobility and ED visits or hospitalizations. There may be additional factors unrelated to mobility that can lead to ED visits or hospitalizations. For example, the amount, capability and availability of assistance or caregivers, the environment, and economic factors may influence the latter. While the association between mobility improvements and reduced hospitalizations became significant in a partially adjusted model, accounting for health status factors such as comorbidity burden and fall history rendered the association nonsignificant; comorbidities greatly influence the likelihood that someone will be hospitalized (28).
While there is limited evidence regarding the implications of changes in mobility performance in community-dwelling older adults, our findings are supported by the available literature. Hardy and colleagues (19) found that natural improvements in usual gait speed over 1 year were predictive of improved survival rates over 8 years in older adults. Improvements in walking speed over 1 year in acutely ill older male veterans was associated with fewer disabilities at 1 year posthospitalization (29); and in patients with stroke, positive changes in walking speed over 3 months were associated with improved self-reported function and quality of life over the same time frame (30). In our study, the changes in mobility performance occurred over a short time frame (12 weeks) in which participants were engaged in group exercise interventions. This improvement in mobility more closely links participation in exercise, improvement in mobility performance, and their impact on reduced incidence of future falls.
This study had several strengths. Our data demonstrate that the change in mobility occurred prior to the outcomes. Our results illustrate a pattern of mobility change and initial health and performance characteristics of the person relates to a future reduced incidence of falls. The sample was inclusive of community-dwelling older adults with varying abilities; the mean gait speed of 0.92 m/s is below the 1.0 m/s indicative of an independent community ambulator, suggesting some of the participants did not have an optimal walking capacity while others were closer to it (8). Likewise, our sample had a 6MWD that fell below the age-specific (for mean age of 80.8 years) average of 422 m (31). Thus, mobility performance change was an important factor when combined with other covariates among participants with diversity in performance and health. Additionally, the IVR system provided an efficient method for capturing information about a participant’s monthly experiences in the year following the original study.
This study is not without limitation. As our analyses were not the primary aim of the parent study, we did not expect to have the appropriate statistical power to detect all possible relationships nor subgroup-specific findings. We did have more women than men in our sample. However, the greater population to which we hope to generalize our findings also have more women than men. Any stratified analyses would have smaller sample sizes resulting in low statistical power. Health care utilization in the form of ED visits and hospitalization occurred infrequently in this sample relative to falls overall, limiting assessment of possible relationships. As this is an observational study, we cannot definitively establish a causal pathway from mobility performance improvement to reduced incidence of future negative outcomes. However, we believe our evidence provides a necessary first step within the confines of an exploratory secondary data analysis, and the risk of falling without intervention is already well-documented for this population (32).
This study is the combination of participants from different intervention arms in a clinical trial; on average, those who participated in the group that completed timing and coordination exercises had greater gains in gait speed and 6MWD than those who completed the standard program (12). We addressed this concern by completing a sensitivity analysis, which demonstrated that nothing materially changed in the results when accounting for intervention arm in the main trial. In this sample, change in mobility performance status was associated with the reduction of incidence of falls regardless of specific intervention.
Additionally, there are limitations with the use of the IVR system: participants may have disproportionately recalled falls only if they were injured; or they may have had difficulty understanding the prompts. In-person fall monitoring over the course of a year, however, can be burdensome for participants and researchers; the IVR system allows for efficient capture of distal health outcomes (26). Thus, we feel the use of IVR is justified for an initial investigation such as ours. Finally, we excluded 121 people due to not having completed a single call, which may have influenced the findings. Those excluded from the analyses, however, were similar on all measures except in that they had a shorter 6MWD. Although the shorter 6MWD in those excluded is a limitation, it is not unique to our study and quite common to observe those with lower level of performance or poorer health effectively being excluded from longitudinal studies in older populations, leading to the phenomenon of informative censoring.
Impaired mobility is related to negative distal health outcomes (4,6,7,18,33). Based on our secondary data analysis, improved mobility is related to a decreased incidence of falls. This finding warrants further investigation with more rigorous methodology for outcome measurement and appropriate statistical power. Studies should consider using a more objective modality of monitoring distal outcomes to account for potential variations in recall and participant reports on the measures. Alternative means of monitoring, such as via electronic health record information may be useful, and monitoring over a longer time frame may lead to better capture because some of these distal outcomes are relatively infrequent.
Over 3 million older adults were treated for fall-related injuries in the ED in 2017 (34); markers such as improvements in mobility performance that demonstrate a reduction in fall incidence have practical significance and can be used to demonstrate the effectiveness of interventions. Importantly, poor mobility is a modifiable risk factor (11–13,15). The reduction of incidence of negative distal health outcomes like falls has the potential to decrease the burdens associated with them.
The results of the current study help justify the use of interventions to improve mobility so that individuals are less likely to experience negative distal health outcomes. It is important for patients, clinicians, policymakers, and payers to understand the urgency of older adults maintaining and improving mobility. Our research adds to the growing body of literature connecting mobility and health outcomes.
Supplementary Material
Acknowledgments
Author Contributions: Study concept and design: V.S., P.C.C., S.P., J.V.S., S.M.A., and J.S.B. Acquisition of data: J.V.S. and J.S.B. Analysis and interpretation of data: V.S., P.C.C., S.P., J.V.S., S.M.A., and J.S.B. Drafting of manuscript: V.S. and P.C.C. Critical revision of manuscript for important intellectual content: V.S., P.C.C., S.P., J.V.S., S.M.A., and J.S.B.
The main contents of this paper were presented by the first author during Rehabilitation Institute Research Day 2019 (May 2019, Pittsburgh, PA, USA) and the American Physical Therapy Combined Sections Meeting 2020 (February 2020, Denver, CO, USA).
Impact Statement: We certify that this work is novel. Improving mobility in older adults is associated with a lower incidence of future falls.
Funding
This work was supported by Patient-Centered Outcomes Research Institute (grant number CE-1304–6301), Pittsburgh Claude D. Pepper Older Americans Independence Center (grant number NIA P30 AG024827), and National Institute on Aging (grant number NIA K24 AG057728). The funding agencies had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
A portion of this work was presented at the 2020 American Physical Therapy Association Combined Sections Meeting in Denver, Colorado.
Conflict of Interest
None reported.
References
- 1. Ferrucci L, Cooper R, Shardell M, Simonsick EM, Schrack JA, Kuh D. Age-related change in mobility: perspectives from life course epidemiology and geroscience. J Gerontol A Biol Sci Med Sci. 2016;71:1184–1194. doi: 10.1093/gerona/glw043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Courtney-Long EA, Carroll DD, Zhang QC, et al. Prevalence of disability and disability type among adults--United States, 2013. MMWR Morb Mortal Wkly Rep. 2015;64(29):777–783. doi: 10.15585/mmwr.MM6429a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hoffman JM, Ciol MA, Huynh M, Chan L. Estimating transition probabilities in mobility and total costs for Medicare beneficiaries. Arch Phys Med Rehabil. 2010;91:1849–1855. doi: 10.1016/j.apmr.2010.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Studenski S, Perera S, Patel K, et al. Gait speed and survival in older adults. JAMA. 2011;305:50–58. doi: 10.1001/jama.2010.1923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Guralnik JM, Ferrucci L, Pieper CF, et al. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci. 2000;55:M221–M231. doi: 10.1093/gerona/55.4.m221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Perera S, Patel KV, Rosano C, et al. Gait speed predicts incident disability: a pooled analysis. J Gerontol A Biol Sci Med Sci. 2016;71:63–71. doi: 10.1093/gerona/glv126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Newman AB, Simonsick EM, Naydeck BL, et al. Association of long-distance corridor walk performance with mortality, cardiovascular disease, mobility limitation, and disability. JAMA. 2006;295:2018–2026. doi: 10.1001/jama.295.17.2018 [DOI] [PubMed] [Google Scholar]
- 8. Studenski S, Perera S, Wallace D, et al. Physical performance measures in the clinical setting. J Am Geriatr Soc. 2003;51:314–322. doi: 10.1046/j.1532-5415.2003.51104.x [DOI] [PubMed] [Google Scholar]
- 9. Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–M94. doi: 10.1093/geronj/49.2.m85 [DOI] [PubMed] [Google Scholar]
- 10. Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988;319:1701–1707. doi: 10.1056/NEJM198812293192604 [DOI] [PubMed] [Google Scholar]
- 11. Van Abbema R, De Greef M, Crajé C, Krijnen W, Hobbelen H, Van Der Schans C. What type, or combination of exercise can improve preferred gait speed in older adults? A meta-analysis. BMC Geriatr. 2015;15:72. doi: 10.1186/s12877-015-0061-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Brach JS, Perera S, Gilmore S, et al. Effectiveness of a timing and coordination group exercise program to improve mobility in community-dwelling older adults: a randomized clinical trial. JAMA Intern Med. 2017;177:1437–1444. doi: 10.1001/jamainternmed.2017.3609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Brach JS, Van Swearingen JM, Perera S, Wert DM, Studenski S. Motor learning versus standard walking exercise in older adults with subclinical gait dysfunction: a randomized clinical trial. J Am Geriatr Soc. 2013;61:1879–1886. doi: 10.1111/jgs.12506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. VanSwearingen JM, Perera S, Brach JS, Cham R, Rosano C, Studenski SA. A randomized trial of two forms of therapeutic activity to improve walking: effect on the energy cost of walking. J Gerontol A Biol Sci Med Sci. 2009;64:1190–1198. doi: 10.1093/gerona/glp098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. VanSwearingen JM, Perera S, Brach JS, Wert D, Studenski SA. Impact of exercise to improve gait efficiency on activity and participation in older adults with mobility limitations: a randomized controlled trial. Phys Ther. 2011;91:1740–1751. doi: 10.2522/ptj.20100391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Perera S, Mody SH, Woodman RC, Studenski SA. Meaningful change and responsiveness in common physical performance measures in older adults. J Am Geriatr Soc. 2006;54:743–749. doi: 10.1111/j.1532-5415.2006.00701.x [DOI] [PubMed] [Google Scholar]
- 17. Narotzki B, Reznick AZ, Levy Y. Moderate exercise for improvement in 6-minute walk test performance in stable coronary heart disease. JAMA Intern Med. 2013;173:168–169. doi: 10.1001/2013.jamainternmed.1077 [DOI] [PubMed] [Google Scholar]
- 18. Perera S, Studenski S, Chandler JM, Guralnik JM. Magnitude and patterns of decline in health and function in 1 year affect subsequent 5-year survival. J Gerontol A Biol Sci Med Sci. 2005;60:894–900. doi: 10.1093/gerona/60.7.894 [DOI] [PubMed] [Google Scholar]
- 19. Hardy SE, Perera S, Roumani YF, Chandler JM, Studenski SA. Improvement in usual gait speed predicts better survival in older adults. J Am Geriatr Soc. 2007;55:1727–1734. doi: 10.1111/j.1532-5415.2007.01413.x [DOI] [PubMed] [Google Scholar]
- 20. Brach JS, Perera S, Gilmore S, et al. Stakeholder involvement in the design of a patient-centered comparative effectiveness trial of the “On the Move” group exercise program in community-dwelling older adults. Contemp Clin Trials. 2016;50:135–142. doi: 10.1016/j.cct.2016.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Rigler SK, Studenski S, Wallace D, Reker DM, Duncan PW. Co-morbidity adjustment for functional outcomes in community-dwelling older adults. Clin Rehabil. 2002;16:420–428. doi: 10.1191/0269215502cr515oa [DOI] [PubMed] [Google Scholar]
- 22. Brach JS, Perera S, Studenski S, Katz M, Hall C, Verghese J. Meaningful change in measures of gait variability in older adults. Gait Posture. 2010;31:175–179. doi: 10.1016/j.gaitpost.2009.10.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166(1):111–117. doi: 10.1164/ajrccm.166.1.at1102 [DOI] [PubMed] [Google Scholar]
- 24. Harada ND, Chiu V, Stewart AL. Mobility-related function in older adults: assessment with a 6-minute walk test. Arch Phys Med Rehabil. 1999;80:837–841. doi: 10.1016/s0003-9993(99)90236-8 [DOI] [PubMed] [Google Scholar]
- 25. Enright PL, McBurnie MA, Bittner V, et al. ; Cardiovascular Health Study The 6-min walk test: a quick measure of functional status in elderly adults. Chest. 2003;123:387–398. doi: 10.1378/chest.123.2.387 [DOI] [PubMed] [Google Scholar]
- 26. Albert SM, King J, Keene RM. Assessment of an interactive voice response system for identifying falls in a statewide sample of older adults. Prev Med. 2015;71:31–36. doi: 10.1016/j.ypmed.2014.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Albert SM, Edelstein O, King J, et al. Assessing the quality of a non-randomized pragmatic trial for primary prevention of falls among older adults. Prev Sci. 2015;16:31–40. doi: 10.1007/s11121-014-0466-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Inouye SK, Zhang Y, Jones RN, et al. Risk factors for hospitalization among community-dwelling primary care older patients: development and validation of a predictive model. Med Care. 2008;46:726–731. doi: 10.1097/MLR.0b013e3181649426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Purser JL, Weinberger M, Cohen HJ, et al. Walking speed predicts health status and hospital costs for frail elderly male veterans. J Rehabil Res Dev. 2005;42:535–546. doi: 10.1682/jrrd.2004.07.0087 [DOI] [PubMed] [Google Scholar]
- 30. Schmid A, Duncan PW, Studenski S, et al. Improvements in speed-based gait classifications are meaningful. Stroke. 2007;38:2096–2100. doi: 10.1161/STROKEAHA.106.475921 [DOI] [PubMed] [Google Scholar]
- 31. Rikli RE, Jones CJ. The reliability and validity of a 6-minute walk test as a measure of physical endurance in older adults. J Aging Phys Act. 1998;6(4):363–375. doi: 10.1123/japa.6.4.363 [DOI] [Google Scholar]
- 32. Soriano TA, DeCherrie LV, Thomas DC. Falls in the community-dwelling older adult: a review for primary-care providers. Clin Interv Aging. 2007;2:545–554. doi: 10.2147/cia.s1080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Hardy SE, Kang Y, Studenski SA, Degenholtz HB. Ability to walk ¼ mile predicts subsequent disability, mortality, and health care costs. J Gen Intern Med. 2011;26:130–135. doi: 10.1007/s11606-010-1543-2m [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Control CfD. Important facts about falls | home and recreational safety | CDC injury center https://www.cdc.gov/homeandrecreationalsafety/falls/adultfalls.html. Updated February 10, 2017. Accessed May 1, 2019.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.