Abstract
Background
Real-life community mobility (CM) measures for older adults, especially those with Parkinson’s disease (PD), are important tools when helping individuals maintain optimal function and quality of life. This is one of the first studies to compare an objective global positioning system (GPS) sensor and subjective self-report CM measures in an older clinical population.
Methods
Over 14 days, 54 people in Ontario, Canada with early to mid-stage PD (mean age = 67.5 ± 6.3 years; 47 men; 46 retired) wore a wireless inertial measurement unit with GPS (WIMU-GPS), and completed the Life Space Assessment and mobility diaries. We assessed the convergent validity, reliability and agreement on mobility outcomes using Spearman’s correlation, intraclass correlation coefficient, and Bland-Altman analyses, respectively.
Results
Convergent validity was attained by the WIMU-GPS for trip frequency (rs = .69, 95% confidence interval [CI] = 0.52–0.81) and duration outside (rs = .43, 95% CI = 0.18–0.62), but not for life space size (rs = .39, 95% CI = 0.14–0.60). The Life Space Assessment exhibited floor and ceiling effects. Moderate agreements were observed between WIMU-GPS and diary for trip frequency and duration (intraclass correlation coefficients = 0.71, 95% CI = 0.51–0.82; 0.67, 95% CI = 0.42–0.82, respectively). Disagreement was more common among nonretired individuals.
Conclusions
WIMU-GPS could replace diaries for trip frequency and duration assessments in older adults with PD. Both assessments are best used for retired persons. However, the Life Space Assessment may not reflect actual mobility.
Keywords: Parkinson’s disease, Geriatric assessment, Mobility assessment, Functional performance, Measurement comparison
Mobility limitations have serious consequences for older adults, including increased falls, institutionalization and mortality (1,2). Such limitations are usually the result of musculoskeletal aging, and are accelerated by neurodegenerative conditions, such as Parkinson’s disease (PD). In the context of PD, mobility limitations are an important predictor of reduced health-related quality of life (3), and current therapeutic interventions for PD mainly target improvements of motor function. Therefore, valid and reliable assessment tools are essential to capture the functional impact of mobility limitations and its impact on daily lives of individuals. Appropriate tools are also vital for evaluating the effectiveness of interventions aiming at maintaining optimal mobility levels.
Measuring mobility is complicated by its multidimensional nature: real-life mobility includes both capacity and actual performance of mobility within one’s home and community (4,5). The latter comprehensive view of mobility, termed community mobility (CM), is considered a key instrumental activity of daily living (6,7). Various aspects of CM are measurable, including trip frequency (8), duration, and area (9–12).
The effects of PD on CM are highly variable among patients, which complicates accurate assessment. The most frequently used assessments are self-reports. These include cross-sectional questionnaires that commonly define CM as concentric circles (“life spaces”) that expand as an individual move outward from the home to the wider community (9, 10), as well as daily diaries. The referent time window for cross-sectional questionnaires typically ranges from the past week to the time since last clinical visit. Such retrospective measures are subject to random (eg, memory) error, as well as recall bias due to social desirability and floor effects (13). Alternatively, daily diary entries may reduce memory error but fail to account for changes in mobility across time (14). Since no “gold standard” measure of CM currently exists, self-reporting remains the most common approach to CM assessment (15,16).
Global positioning system (GPS) receivers are promising tools to prospectively assess the CM of people with PD (PwP) over long time periods (13,17,18). One example is the WIMU-GPS (wireless inertial motion unit with GPS (19)), a wearable sensor platform which could be worn at the hip or trunk of participants (Supplementary Figure 1 in the Supplementary Material). The WIMU-GPS incorporates 3D inertial measures of motion (accelerometers, gyroscope, and magnetometers) and GPS receivers, which allows the extraction of specific metrics commonly captured by self-report measures, such as frequency and duration of trips, destinations, and CM lifespace sizes through geospatial renderings (19). As physical devices, sensors should be free of measurement biases common to self-report measures, such as perceived social desirability, memory, or other cognitive challenges.
Despite these advances, few studies have thoroughly compared new versus older mobility assessment methods in older adults, especially among older clinical populations at higher risk of mobility declines (17,20,21). Comparisons of validity, reliability, and agreement should be conducted between alternative assessment methods before new measures replace established ones. The lack of such studies of CM measures may be partly due to the absence of a consensus gold standard assessment of CM. Conventional measurement evaluation uses a gold standard to determine empirical types of validity (eg, criterion validity). However, criterion validity is not required for initial evaluations of new approaches; much can be learned by examining the level of agreement between existing measures without meeting the assumptions that underlie the test-criterion framework (17,22).
The objectives of this study were to systematically compare data from a wearable sensor GPS platform to self-report measures to assess its validity, reliability and agreement in an older clinical population. Our secondary objective is to identify individual characteristics of older adults that affect the agreement between objective and self-report measures of mobility.
Methods
Reporting of this study follows the Guidelines for Reporting Reliability and Agreement Studies (23) and the COnsensus-based Standards for the selection of health Measurement INstruments (COSMIN (24,25)).
Participants
We recruited a convenience sample of 70 ambulatory community dwelling PwP (Hoehn & Yahr Stages I–III) from the Movement Disorders Clinic of London Health Sciences Center, Canada in person or over the phone. Inclusion and exclusion criteria are outlined in Supplementary Table S1 in the Supplementary Materials. We obtained written informed consent from all participants and ethical approval from Western University’s Human Subjects Research Ethics Board (HSREB #102337).
Assessments and Common Outcomes
Over 14 days, all participants wore the WIMU-GPS during hours awake as they navigated their home and communities. We instructed all participants to remove the device from their bodies just prior to sleeping each evening and charge the device in their “ON” mode throughout the night. We also instructed participants to put the WIMU-GPS back on once they wake up in the morning, so it starts recording. They also recorded daily diary entries (14) about the start and end time of each trip taken outside. On Days 1 and 14, participants completed the Life Space Assessment (LSA (10)). This cross-sectional scale quantifies the size of one’s life space in the past 4 weeks as a score of 0–120 (0 = confined to bedroom, 120 = daily travel to places outside of one’s city/town).
We assessed the convergent validity, reliability, and agreement between the WIMU-GPS and diary recordings for recordings of “hourly frequency” (ie, number of trips taken outside of the home per hour sampled) and “daily duration” (ie, percentage of total time sampled per day individuals were outside of home). We established construct validity of the WIMU-GPS against self-report diaries by capturing these same two mobility outcomes. Similar to a previous study that used the WIMU-GPS (26), all WIMU-GPS devices were calibrated to begin recording distance relative to a central location within the participants’ homes (ie, usually the kitchen or living room where the rest of the assessments took place). Our analysis considered participants’ home to be a geographic cluster that covered 50 m in radius from this central location, and any travel extending beyond this threshold was considered “outside” of the home. This distance was selected to account for variation in home sizes. Trips were defined as when the participant leaves this home cluster.
Whereas participants recorded any travels in their diaries over the entire 24 hours each day, they could remove the WIMU-GPS for reasons such as sleeping, charging, bathing, etc. The longest length of WIMU-GPS recording in a day obtained was just under 19 hours, and that was used as the daily sampling period for the diary to standardize time during which sensors may have been off-body and not recording (eg, sleeping, bathing). Diary entries were checked to ensure the timeframe included all documented trips outside, and the time of its first and last recordings overlapped with WIMU-GPS’ start and end recording times each day. The WIMU-GPS recorded displacement and life-space mobility data during the time sampled using a geospatial statistical approach based on the computation of a minimum span ellipse that fitted all the recorded data points for a given individual (19). The surface area of the minimum span ellipse (geometric 2D area in km2) was used as a direct quantifier of life space size. In comparison, the LSA uses single scores to represent relative life space sizes. In this study, the average Day 1 and 14 LSA scores were not statistically different (p = .14), and the LSA has shown good test–retest reliability (intraclass correlation [ICC] = 0.72 (27)). Therefore, we compared Day 14 LSA scores against WIMU-GPS recorded “life space size.” To ensure sampled data averaged variability in mobility across hours of the day and days of the week, we included only participants whose WIMU-GPS recorded a minimum of 6 days with at least 600 minutes (10 hours) of data for analysis. Among participants who met this criterion, we also excluded any remaining recorded days with less than 600 minutes of data. Although previous GPS mobility tracking studies defined a “valid GPS day” as having shorter recording lengths (28,29), these studies did not focus on average travel time and distance, nor did they account for the sampling period of self-reported measures (typically 24 hours). Then, we removed sampled days without both WIMU-GPS and diary data from the analysis. In total, 54 participants were included in the analysis, providing a total of 592 days of frequency and life space size data, and 573 days of duration data.
Additional Covariates
Discrepancies between GPS and self-report mobility measures were previously observed to be associated with sociodemographic characteristics such as age, gender, employment or volunteering status, education, income, mode of travel, day of travel (17,30), and travel behavior (31). We assessed these demographics information, along with individuals’ cognitive status using the MOntreal Cognitive Assessment (MoCA (32)), and the impact of PD using the Parkinson’s Disease Questionnaire (PDQ-39 (33)).
Analysis
Concurrent validity between the WIMU-GPS and self-report measures was established by comparing simultaneously collected data (34). Convergent validity was assessed using the Spearman correlation. Reliability in assessment comparison studies refers to how well one assessment can duplicate another’s ability to detect variability in outcomes (35). We assessed reliability between the WIMU-GPS and diary using the intraclass correlation (ICC). We did not examine reliability between the WIMU-GPS and LSA scores as there was no analogous measure produced by the WIMU-GPS. We visually compared agreement between “hourly frequency” and “daily duration” captured by WIMU-GPS and diaries using parallel line plots (36), and quantified agreement using Bland-Altman (B-A) plots (22,37,38) for frequency and duration data after log-transformation (22,39). We calculated 95% limits of agreement (LoA) using adjusted standard deviation for multiple sampling (22). Since no meaningful cutoff values for trip frequency and duration are available in existing literature, we evaluated bias by examining the distribution of disagreement scores within the LoA. We compared variability among the measurements after adjusting for means expressed in different measurement units using the coefficient of variation (CV), which was defined as standard deviation divided by mean.
We examined subgroups validity using partial correlations, and estimated incidence rate ratios (eβ) using Poisson regression models to determine covariate effects on agreement. We applied offset corrections to account for the unequal number of matched days included for analysis for each participant. Unless indicated, we observed statistical significance when two-side p-value was < .05. Our analyses were conducted using SAS (v9.3, SAS Institute Inc., 2011) and SPSS (v20, IBM Corp, 2011).
Results
Participant demographic characteristics and PD symptoms are presented in Table 1.
Table 1.
Participant Demographics and Impact of Parkinson’s Disease (n = 54)
| Demographics Covariates | n (range or %) |
|---|---|
| Age (years) | 67.5 ± 6.3 (55–79) |
| Gender | |
| Men | 38 (70.4%) |
| Women | 16 (29.6%) |
| Marital status | |
| Married/common law | 45 (83.3%) |
| Income | |
| 0–$19, 999 | 11 (20.4%) |
| $20,000–$39,999 | 12 (22.2%) |
| $40,000–$59,999 | 14 (25.9%) |
| $60,000–$89,999 | 11 (20.4%) |
| >$90,000 | 6 (11.1%) |
| Employment status | Fully retired = 46 (85.2%) |
| Education | |
| < High school | 11 (20.4%) |
| High school graduate | 11 (20.4%) |
| Some college | 3 (5.6%) |
| College diploma | 9 (16.7%) |
| Undergraduate degree | 8 (14.8%) |
| Postgraduate program | 1 (1.9%) |
| Graduate degree | 11 (20.4%) |
| Residential setting | |
| Urban | 15 (27.8%) |
| Suburban | 11 (20.4%) |
| Rural, in town | 18 (33.3%) |
| Rural, outside of town | 10 (18.5%) |
| Living situation | Cohabiting (with family/friends) = 45 (83.3%) |
| Driving status Drives | 52 (96.3%) |
| Cognitive score (MoCA) | 25.6 ± 2.7 (22–30) |
| Time since PD diagnosis (years) | 6.2 ± 5.7 (0–30) |
| Impact of PD on dimensions of daily living (PDQ-39 scores): | (0 = no impact, 100 = total impairment) |
| 1. Mobility | 17.9 ± 20.9 (0–70.0) |
| 2. Activities of daily living | 23.2 ± 18.4 (0–70.8) |
| 3. Emotional well being | 19.1 ±16.6 (0–66.7) |
| 4. Perceived stigma | 13.3 ± 16.0 (0–68.8) |
| 5. Social Support | 8.3 ± 12.3 (0–50.0) |
| 6. Cognition | 24.1 ± 19.3 (0–68.8) |
| 7. Communication | 20.7 ± 19.0 (0–75.0) |
| 8. Bodily discomfort (eg, pain) | 26.6 ±23.4 (0–100.0) |
| 9. Overall quality of life | 19.1 ± 13.7 (1.8–64.7) |
Note: Montreal COgnitive Assessment (MoCA) scores suggest some participants may have undetected mild cognitive impairment, even though it did not appear to affect their activities of daily living performance or performance on the orientation section of the MoCA. PD = Parkinson’s disease.
Community Mobility Outcomes
Mobility outcomes are presented in Table 2. WIMU-GPS recorded significantly higher “daily duration” than diaries (an average of 5.0% vs 20.3% of the day outside, respectively; p < .05), whereas there was no evidence to suggest a significant difference between “hourly frequency” captured by WIMU-GPS and diary.
Table 2.
Mean Mobility Outcomes Measured by Self-report Measures and WIMU-GPS
| Community Mobility Outcome | Mean ± SD (range) | Shapiro–Wilk Normality Test (S-W; normal distribution: p ≥ .05) | Coefficient of Variation (CV) | Mean Difference in Comparable Outcomes (WIMU-GPS – Diary) ± SD (range) | Wilcoxon Signed Rank Test of Difference |
|---|---|---|---|---|---|
| WIMU-GPS “hourly frequency” | 0.12 ± 0.06 (0.03–0.28) | p = .0002 log-transformed: p = 0.6071 | 0.50 | 0.01 ± 0.05 (−0.15–0.16) Shapiro–Wilk test: p = .1056 | W<W α = 0.05,53 =149.5, p < .2 |
| Diary “hourly frequency” | 0.11 ± 0.06 (0.03–0.34) | p = .0005 log-transformed: p = 0.9327 | 0.55 | ||
| WIMU-GPS “daily duration” | 25.0 ± 11.6% (6.2%–60.8%) | p = .04 log-transformed: p = 0.1618 | 0.46 | 4.8% ± 11.4% (−41.6%–25.1%) Shapiro–Wilk test: p < .0001 | W<W α = 0.05,53 =500.5, p < .0001† |
| Diary “daily duration” | 20.3 ±12.2% (0.2%–57.4%) | p = .01 log-transformed: p < .0001 | 0.60 | ||
| LSA “life space size”†† | 84.8 ± 16.3 (48–120) | p = .36 | 0.19 | ||
| WIMU-GPS “life space size” (km 2) | 4 048.8 ± 6 432.3 (8.2–29 448.6) | p < .0001 | 1.59 |
Note: “Hourly frequency” refers to the number of trips taken outside of the home per hour sampled, and “daily duration” refers to the percentage of total time sampled per day that participants were outside of home.
†Statistically significant differences in comparison pairs, shown using the Wilcoxon Signed Ranks test (p ≤ .05). Non-normal distribution of differences remained after log and logit transformations (both S-W tests yielded. p < .0001).
††LSA Maximum = 120.
Shapiro–Wilk tests showed that LSA scores and mean “hourly frequency” differences were the only normally distributed outcomes; hence, subsequent Bland-Altman analyses of agreement were performed on log-transformed difference scores. The estimated CVs suggested similar dispersion for “hourly frequency” measured by WIMU-GPS and diary. Diary recordings of “daily duration” (showing percentage of the day outside ranged from 6.2% to 60.8%) and WIMU-GPS recordings of “life space sizes” (showing geographic area travelled over 2 weeks ranged from 8.2 to 29,448.6 km2) were notably more variable than WIMU-GPS recordings of “daily duration” and LSA measured “life space sizes”, respectively.
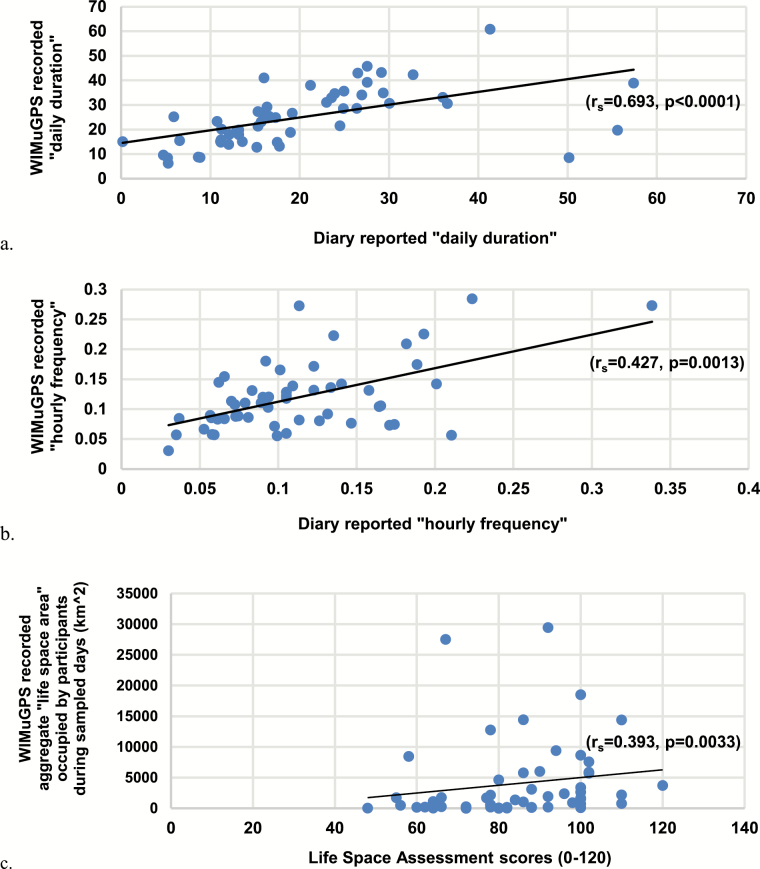
Convergent Validity
Good convergent validity (r ≥ .4) was detected only between WIMU-GPS and diary on “daily duration” (rs = .693, p < .001, 95% confidence interval [CI] = 0.52–0.81; Figure 1a) and “hourly frequency” (rs = .427, p = .001, 95% CI = 0.18–0.62; Figure 1b). Adequate convergent validity was not observed between the WIMU-GPS and LSA on “life space sizes” (rs = .393, p = .003, 95% CI = 0.14–0.60; Figure 1c). Validity was not affected by demographic covariates as partial correlation coefficients did not change more than 5% from the crude correlation.
Figure 1.
Relationship between “daily duration” (a), “hourly frequency” (b), “life space size” (c) measured using WIMU-GPS and diary. Good convergent validity (r ≥ .4) was shown using Spearman correlation analysis for “daily duration” (a), “hourly frequency” (b), but not for “life space size” (c).
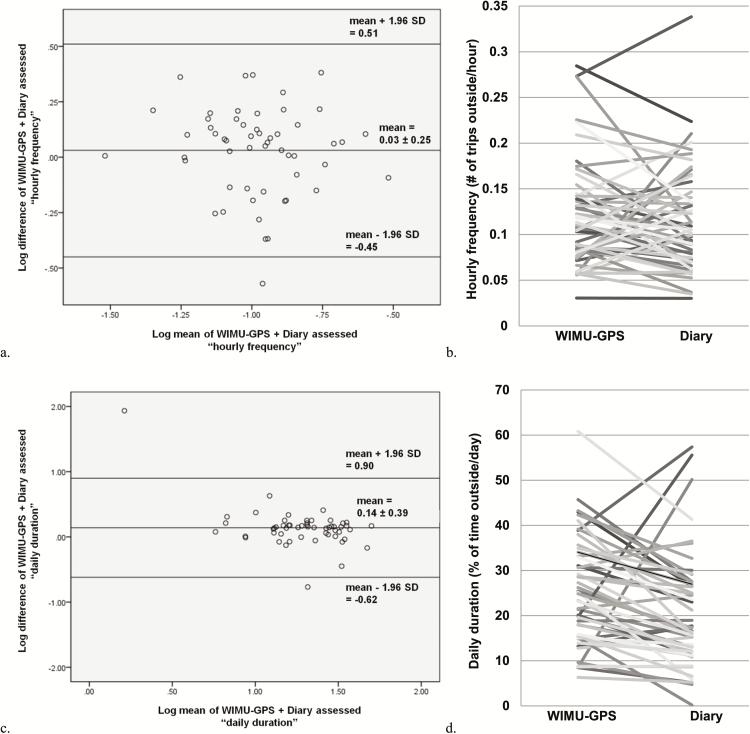
Reliability and Agreement
Good reliability was demonstrated for both “daily duration” (ICC = 0.674, p < .001, 95% CI = 0.42–0.82) and “hourly frequency” (ICC = 0.714, p < .001, 95% CI = 0.51–0.82). B-A plots were constructed to evaluate the imperfect agreements (ie, ICC ≠ 1) between the WIMU-GPS and diary records.
Agreement between WIMU-GPS and diaries are shown in B-A plots of log base 10-transformed data (Figure 2a and c). The mean difference and 95% LOA for log “hourly frequency” is 0.03, and 0.51 to −0.45, respectively (Figure 2a). Hence, 95% of the time, WIMU-GPS “hourly frequency” averaged 1.07 times higher than the diary reports and was between 0.35 and 3.2 times higher than diary reports. ICC values for both outcomes did not change more than 10% after the removal of outliers.
Figure 2.
Bland-Altman plots of agreement between log mean and log difference of WIMU-GPS and Diary measured “hourly frequency” (a) and “daily duration” (c). Majority of participants recorded higher WIMU-GPS “hourly frequency” (b) and “daily duration” (d) than the Diary (66.7% and 79.6%, respectively). All n = 54.
The mean difference and 95% LOA, for “daily duration” is 0.14 and −0.62 to 0.90, respectively (Figure 2c). Antilog of difference between two log values yields a ratio. Therefore, mean WIMU-GPS “daily duration” is 1.38 times higher than the diary, and 95% of the WIMU-GPS recorded “daily duration” were between 0.24 and 7.9 times of diary-reported values.
Higher mean WIMU-GPS recordings of both outcomes were observed in most participants (Figure 2b and d). For “hourly frequency,” 66.7% (n = 36) of PwP recorded higher WIMU-GPS outcomes compared to 33.3% (n = 18) with higher diary reports. For “daily duration,” 79.6% (n = 43) participants had higher WIMU-GPS recordings compared to 22.2% (n = 12) with higher diary reports. As well, daily agreement between WIMU-GPS and diary seldom occurred. Agreement occurred more often for “hourly frequency” than for “dailyduration” (10.1% of days vs 0.07% of days, respectively). The WIMU-GPS recorded greater “hourly frequency” and “daily duration” than the diary across most days (67.0% and 75.6% of days for frequency and duration, respectively).
A summary of the statistically significant demographic and disease-related covariates affecting the agreement types are presented in Table 3. No significant predictors of higher WIMU-GPS recordings of “hourly frequency” were found (Table 3, a). Agreement was not assessed for “daily duration” due to too few days of occurrence (Table 3, b). Employment status was the only common predictor of most disagreement for both outcomes. Higher diary reports (ie, over self-reporting) of “hourly frequency” and “daily duration” than WIMU-GPS recordings were 1.66 and 1.93 times more likely to occur among working PwP than retired PwP.
Table 3.
Statistically Significant Predictors of “Hourly Frequency” (a) and “Daily Duration” (b) Captured by the WIMU-GPS and Diary
| a. “Hourly frequency” captured by the WIMU-GPS and Diary | ||||
|---|---|---|---|---|
| Participant characteristics | Higher Diary | Agreement | ||
| Incidence rate ratio (eβ) | p | Incidence rate ratio (eβ) | p | |
| Age α | 0.97 | .0336 † | 1.06 | .0065 † |
| Gender (ref: women) | 0.69 | .0406 † | 1.135 | .6635 |
| Employment status α (ref: retired) | 1.66 | .0152 † | 0.398 | .0754 †† |
| Education (ref: graduate degree) | ||||
| < High school | 0.76 | .3919 | 1.331 | .4714 |
| High school graduate | 2.41 | .1487 | 0.880 | .7703 |
| Some college | 0.59 | .3891 | 3.286 | .0105 † |
| College diploma | 1.44 | .2057 | 0.924 | .8654 |
| Undergraduate degree | 1.31 | .3703 | 1.044 | .9264 |
| Postgraduate program | 2.41 | .0745 †† | 5.17 × 10−11 | .9999 |
| Income α (ref: >$90,000) | ||||
| 0–$19,999 | 0.55 | .1005 †† | 1.727 | .2799 |
| $20,000–$39,999 | 0.6903 | .2926 | 1.221 | .7079 |
| $40,000–$59,999 | 0.781 | .4391 | 1.061 | .9085 |
| $60,000–$89,999 | 1.78 | .0570 †† | 0.915 | .8743 |
| Years since diagnosis | 0.95 | .0077 † | 1.027 | .1671 |
| Impact of PD on dimensions of daily living (PDQ-39 scores): | ||||
| 1. Mobility α | 0.992 | .0727 †† | 1.006 | .2698 |
| 2. Activity of daily living α | 0.99 | .0470 † | 1.010 | .1203 |
| 3. Emotional well being | 0.9966 | .5293 | 0.992 | .3294 |
| 4. Perceived stigma | 0.988 | .0557 †† | 1.016 | .0210 † |
| 5. Social Support | 1.009 | .1571 | 0.987 | .2804 |
| 6. Cognition | 0.991 | .0717 †† | 1.004 | .5415 |
| 7. Communication | 0.997 | .5785 | 1.002 | .7497 |
| 8. Bodily discomfort α | 0.992 | .0555 †† | 0.998 | .7395 |
| 9. Overall quality of life α | 0.989 | .0919 †† | 1.0055 | .5367 |
| b. “Daily duration” captured by the WIMU-GPS and Diary | ||||
| Higher WIMU-GPS | Higher Diary | |||
| Participant characteristics | Incidence rate ratio (e β) | p | Incidence rate ratio (e β) | p |
| Age α | 1.0078 | .3121 | 0.974 | .0552 †† |
| Employment status α (ref: retired) | 0.748 | .0482 † | 1.932 | .0007 † |
| Income α (ref: >$90,000) | ||||
| 0–$19,999 | 0.972 | .8722 | 1.165 | .7147 |
| $20,000–$39, 999 | 0.833 | .3208 | 1.920 | .1000 †† |
| $40,000–$59, 999 | 0.866 | .3983 | 1.709 | .1641 |
| $60,000–$89,999α | 0.817 | .2707 | 2.015 | .0746 †† |
| Residential setting (ref: rural, outside of town) | ||||
| Urban | 0.944 | .7004 | 1.157 | .5336 |
| Suburban | 1.099 | .5463 | 0.740 | .2835 |
| Rural, in town | 1.134 | .3561 | 0.662 | .0929 †† |
| Impact of PD on dimensions of daily living (PDQ-39 scores): | ||||
| 1. Mobility α | 1.003 | .1553 | 0.987 | .0100 † |
| 2. Activity of daily living α | 1.004 | .1141 | 0.986 | .0060 † |
| 3. Emotional well being | 1.000 | .9982 | 0.9995 | .9264 |
| 4. Perceived stigma | 1.002 | .4522 | 0.993 | .2068 |
| 5. Social Support | 0.998 | .6674 | 1.005 | .4726 |
| 6. Cognition | 1.001 | .5691 | 0.995 | .2992 |
| 7. Communication | 1.002 | .5079 | 0.995 | .3131 |
| 8. Bodily discomfort α | 1.002 | .3119 | 0.993 | .0782 †† |
| 9. Overall quality of life α | 1.004 | .3084 | 0.988 | .0735 †† |
Note: Significant predictors of higher WIMU-GPS recordings were not found for “hourly frequency.” Significant predictors of agreement between the measurements were not assessed for “daily duration.” PD = Parkinson’s disease.
†Significant at p = .05, p = .01. ††Significant at p = .1. αCovariate was significant for both community mobility outcomes.
Discussion
To the best of our knowledge, this is the first study to systematically compare wearable GPS technology and self-reported measures in recording mobility outcomes in a clinical population. In the absence of a gold standard, assessment validations are done against existing measures of a common outcome (22,23). WIMU-GPS was a valid measure for capturing hourly frequency and daily duration outside the home when compared with travel diaries. Both WIMU-GPS and diary also showed similar ability to distinguish participants’ frequency and duration outside (ICC = 0.714 and 0.674, respectively).
Discrepancies Between Assessments
Methods seldom agree exactly (22). Disagreement between the measures was detected across most sampled days for both outcomes. Higher degree of agreement was found for frequency than duration. This may be due to the increased complexity of duration recall. As well, WIMU-GPS recorded longer “daily duration” than diary report. The discrepancy between our results and a previous report showing longer duration in self-reported diaries than GPS recordings (40) may be because duration data was previously compared for each trip instead of over an entire day.
In terms of “hourly frequency,” mean WIMU-GPS measurements were also higher than diary reports, but this difference was not statistically significant. Previous studies often compared assessments in terms of frequency and duration per day (16), which do not account for the different time length sampled due to variations in actual sensor wear time, sensor time without data interference or loss, and diary completion. When hours sampled was not considered, a significant difference on daily frequency was found. In general, the differences in “hourly frequency” and “daily duration” of time outside recorded by the WIMU-GPS and self-reported in the diaries did not appear to be clinically significant.
The importance of using matched common time is highlighted by this study. The results differed when sampled time between the assessments was standardized. A population study comparing matched trips showed only 64% of trips recorded by GPS and diaries matched in the time of departure from origin and/or arrival at destination (40). Although this study did not employ trip level matching (16), it accounted for the different lengths of actual sampled time by the assessments.
Finally, it is possible that by being aware of the simultaneous GPS recordings, participants may become more diligent with completing their diary recordings. Thus, independent diary recordings may be less reliable as a solo assessment method.
Limitations of Cross-sectional Measures
Our results suggest the LSA should be reserved for characterizing longitudinal change in self-perceived mobility within individuals. Good convergent validity was not found when comparing WIMU-GPS and LSA assessed “life space size,” indicating an inherent issue with the LSA’s discriminatory power. We observed the actual sizes of life space area recorded by the WIMU-GPS often differ widely among different individuals with the same LSA score (Figure 1c; Supplementary Figure 2 of Supplementary Materials). For example, the area of mobility of individuals with a LSA score of 100 spanned a wide range, from 104.12 to 18,509.57 km2. This issue may extend to other cross-sectional measures as a study recently showed a different cross-sectional self-report measure underestimated the life space sizes of a general older population when compared to a GPS (20). Such differences in life space sizes obtained are clinically relevant given the LSA scores have been associated with various health outcomes and mortality (1). Therefore, researchers and clinicians should avoid using single administrations of the LSA (ie, baseline LSA scores) to compare different populations, and careful considerations are needed when interpreting the associations between single baseline LSA scores and health outcomes. Possible reasons for the LSA’s ceiling effect and imprecision may include: poor discrimination ability with large life spaces, and/or difficulties remembering distance travelled especially when “trip chaining” (visiting multiple locations during one commute) or when travel activities increased during warmer weather.
Further, although the LSA instructions contain examples of neighborhood boundaries, subjective interpretation of questions may influence self-reporting. Participants of this study occupied diverse settings. When participants in a larger municipality reported no travel outside of town, they may report low LSA scores but still record a larger area travelled using the WIMU-GPS due to their community’s larger geographic boundaries. A study conducted in a general older adult population also only found weak correlations between life space areas measured by the WIMU-GPS and LSA (26). Floor effects are common in cross-sectional retrospective recall measures (13), and Figure 1c further illustrates that the LSA are sensitive to floor effects too.
Subgroup Variations
Working PwP were more likely to over self-report their mobility outcomes than their retired peers. As well, agreement between the WIMU-GPS and diary on frequency was more likely among retired PwP than those who worked. Hence, the assessments can likely be interchangeably used among retirees. People who worked may be less able to comply with the recording protocol during work hours. A difference in agreement between GPS and self-report has been shown to be dependent on the type of work performed in the general population (30). Compared to those who volunteered, people with paid work were more likely to self-report more trips than GPS recordings. Therefore, those without formal paid work may be travelling more, often in a trip-chaining pattern, which can complicate record keeping.
Incidence of diary over-reporting was also more sensitive to education, income, place of residence. These characteristics may have influenced participants’ understanding of study requirements and technology use. Women were more likely to over self-report frequency than men. In the general population, age was a significant predictor of disagreement between GPS and self-report (30) and led to higher probability of more GPS-derived trips (17). Age distribution of this sample was homogenous relative to general population samples in existing studies; this may be why age was not shown to be a strong predictor of inter-assessment agreement and disagreement. Time since diagnosis and PD status were significant predictors, but they did not notably change the incidence of agreement or disagreement between WIMU-GPS and Diary. Hence, disease status alone likely does not affect agreement between assessments.
WIMU-GPS Data Quality
The present analysis included 60.4% (592/980) of sampled days. Sampled days excluded from the analysis were due to insufficient recorded time by the GPS. However, this was to be expected and it was within the range of data quantity excluded in existing GPS studies (42,43).
Reasons for insufficient recordings using the WIMU-GPS were consistent with other studies (42), and included the following: participants forgot to charge the battery during data collection period, WIMU-GPS was not continuously worn, and equipment errors (eg, spurious data loss occurred during 7 days from 6 PwP). The impact of including incomplete data collection days will be examined in a subsequent study.
Diary Data Quality
There were 7.7% (75/980 days) of diary entries were that were missing or incorrect. This is likely an underestimation, as the accuracy of diary entries was not always apparent to the transcriber. An inconsistent quality of diary completion was observed, with high variability in how much detail and precision was given (eg, digit preference as seen in rounding to nearest 15 minutes, and incomplete origin locations given for trips). Almost all participants also expressed uncertainty or displeasure with the task of diary completion.
Common reasons for diary under-reporting are known to be survey length, recall issues, compliance, judging trips to be unimportant, unwillingness for full disclosure, and reporting error (31,40,44). Short trips, especially when occurring in sequence (trip chaining), and trips by nonmotorized modes were often omitted or forgotten in the general population (30,31). Recall based assessments are also prone to recall bias due to social desirability, floor effects and subjective interpretations (45).
Strengths of Study
Some existing comparison studies of the general public limited GPS sampling to 1 week or less (43,44) due to storage and battery limitations, to minimize participant burden and inevitable data loss (the latter of which increases with sampled time). As mobility is unstable over time, the best approximation of real-life mobility requires longer duration recordings. This study optimized the trade-off between capturing representative data and data loss by using a data collection protocol of 2 weeks, and then applying a minimum sampled criterion for the analysis.
Time-standardized outcomes are not always done in comparison studies of the general public as many available GPS models provide users with ready-processed aggregate data. We used the WIMU-GPS as it allowed access to raw data to identify and filter out common GPS signal noise, as well as accounting for unmatched start and end times. By standardizing sampling time, validity, reliability, and agreement between frequency and duration data reported by this study may be more accurate than previously reported.
We also minimized selection and recall bias in this study by breaking down the data collection to three home visits and providing follow-up phone calls with reminder slips. All participants’ data were collected by the same trained researcher (L.Z.) in order to minimize inter-rater bias.
Study Limitations
The generalizability of this study’s findings may be limited as participants were high functioning, community dwelling older adults with PD who did not use any mobility aids. Subsequent studies are needed to determine whether similar validity, reliability and agreement outcomes are repeatable in other clinical populations. Also, this study’s interpretation of acceptable error was greatly limited by the lack of a predetermined clinically relevant cutoff limit.
Clinical and Research Recommendations
Wearable sensors may be able to improve the ability to track mobility changes by traditional clinical and laboratory assessments (46). The absence of clinically significant cutoff scores and a gold standard measure of CM (47) limited clinical relevance interpretation of values contained within the 95% LOAs (22). However, the difference between trip frequency was small (ie, mean difference and LOA ranges were all <1 trip per day). Hence, the WIMU-GPS could be used to replace the diary to measure trip frequency when burden and recall biases of diaries are issues.
Previous findings of diaries’ over-reporting of trip duration, relative to GPS recordings, were not duplicated (16). Mean difference between diary and WIMU-GPS detected was low (4.77% of sampled time). Although this difference between WIMU-GPS and diary may not be clinically significant overall, it may be clinically relevant for individuals confined to the home who wish to increase time outside.
Furthermore, diary use to capture trip duration presents a high amount of participant burden as respondents must record every time of arrival and departure. In this study, many older participants mentioned they found writing down trip timing to be the most cumbersome task. Since participant burden may hamper the quality of the self-report data, the WIMU-GPS should also be considered as a reasonable alternative measure to capture trip duration.
Despite the wide use of the LSA’s life-space mobility score in research (11) and clinical settings (1,48), nonstandard environmental and neighborhood characteristics hinder the LSA’s ability to capture different mobility space sizes. As such, the discriminatory power of the LSA is sensitive to floor and ceiling effects, and single LSA scores may not reflect true mobility performance. Therefore, the current LSA is more useful as an assessment of longitudinal changes within individuals, than as a cross-sectional assessment of mobility differences between individuals or groups.
Research and clinical assessment of real-life mobility typically rely on even fewer questions than the LSA. Therefore, it is reasonable to assume that most ways of approximating mobility through simple patient recall are not representative of the true situation due to floor and ceiling effects. Accuracy in life space size measurement may be improved through more contextual questions or longer duration assessments; both are possible when using GPS sensors. Nevertheless, researchers and clinicians need to carefully consider how much passively recorded GPS information is minimally required to make research or clinical judgment, to avoid risking participant and patient privacy and anonymity by over-collecting data.
Conclusions
The WIMU-GPS shows good construct and convergent validity with long duration self-report measures, and could reasonably replace self-report diaries to capture trip frequency and duration in PwP. When considering life space sizes, researchers and clinicians should avoid relying on a single cross-sectional LSA score, as it cannot accurately gauge individuals’ span of mobility below and above a certain distance threshold. Overall, GPS technology is a promising research and clinical measure of real-life mobility in older adults with PD.
Supplementary Material
Supplementary data is available at The Journals of Gerontology, Series A: Biological Sciences and Medical Sciences online.
Supplementary Figure 1a. Wireless inertial unit with GPS (WIMU-GPS) (26). b. WIMU-GPS worn across the front of participants’ chests, either under or over clothing, depending on individual preference.
Supplementary Figure 2. Different life space sizes were often recorded by the WIMU-GPS for participants with the same Life Space Assessment (LSA) score. Shown here are examples of WIMU-GPS recorded trips belonging to two participants with the same LSA score of 100. a. Over the 2 weeks, participant A largely travelled within their home city with occasional trips to adjacent regions. WIMU-GPS recorded their life spaces to span 10.97km2. (The two straight diagonal lines shown reflected spurious signal bounces, which were filtered out in the analysis.) b. During the same 2 weeks, participant B commuted between two nearby regions, with their life space spanning 202.06km2.
Supplementary Table S1. Study inclusion and exclusion criteria.
Acknowledgments
We acknowledge assistance from Dr. Roderick Edwards when designing the analysis. We also thank Matthew Dibsdale, Catherine Lavigne-Pelletier, Margaux Blamoutier, and the clinic staff and patients of the NPF Center of Excellence Movement Disorders Clinic at London Health Sciences Center for assistance with recruitment and data collection.
Funding
This work was supported by a Mobility in Aging team grant from the Canadian Institutes of Health Research (grant number: 200907AMG-208147-AML-CFEB-56596). L.Z. was funded by the Ontario Graduate Scholarship by the Government of Ontario and the Joseph Scott Studentship in Mobility and Aging from Parkwood Hospital.
Conflict of Interest
No conflict of interest was reported by any of the study authors. The opinions, results, and conclusions reported in this paper are those of the authors and are independent from the funding sources.
References
- 1. Kennedy RE, Sawyer P, Williams CP, et al. Life-space mobility change predicts 6-month mortality. J Am Geriatr Soc. 2017;65:833–838. doi: 10.1111/jgs.14738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Montero-Odasso M, Bherer L, Studenski S, et al. Mobility and cognition in seniors. Report from the 2008 Institute of Aging (CIHR) Mobility and Cognition Workshop. Can Geriatr J. 2015;18:159–167. doi: 10.5770/cgj.18.188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Forsaa EB, Larsen JP, Wentzel-Larsen T, Herlofson K, Alves G. Predictors and course of health-related quality of life in Parkinson’s disease. Mov Disord. 2008;23:1420–1427. doi: 10.1002/mds.22121 [DOI] [PubMed] [Google Scholar]
- 4. Webber SC, Porter MM, Menec VH. Mobility in older adults: a comprehensive framework. Gerontologist. 2010;50:443–450. doi: 10.1093/geront/gnq013 [DOI] [PubMed] [Google Scholar]
- 5. Frank JS, Patla AE. Balance and mobility challenges in older adults: implications for preserving community mobility. Am J Prev Med. 2003;25 (3 Suppl 2):157–163. doi: 10.1016/s0749-3797(03)00179-x [DOI] [PubMed] [Google Scholar]
- 6. Gardner P. The role of social engagement and identity in community mobility among older adults aging in place. Disabil Rehabil. 2014;36:1249–1257. doi: 10.3109/09638288.2013.837970 [DOI] [PubMed] [Google Scholar]
- 7. Patla AE, Shumway-Cook A. Dimensions of mobility: defining the complexity and difficulty associated with community mobility. J Aging Phys Act. 1999;7:7–19. doi: 10.1123/japa.7.1.7 [DOI] [Google Scholar]
- 8. Davis MG, Fox KR, Hillsdon M, et al. Getting out and about in older adults: the nature of daily trips and their association with objectively assessed physical activity. Int J Behav Nutr Phys Act. 2011;8:116. doi: 10.1186/1479-5868-8-116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Stalvey BT, Owsley C, Sloane ME, Ball K. The life space questionnaire: a measure of the extent of mobility of older adults. J Appl Gerontol. 1999;18:460–478. doi: 10.1177/073346489901800404 [DOI] [Google Scholar]
- 10. Baker PS, Bodner EV, Allman RM. Measuring life-space mobility in community-dwelling older adults. J Am Geriatr Soc. 2003;51:1610–1614. doi: 10.1046/j.1532-5415.2003.51512.x [DOI] [PubMed] [Google Scholar]
- 11. Rantakokko M, Iwarsson S, Slaug B, Nilsson MH. Life-space mobility in Parkinson’s disease: associations with motor and non-motor symptoms. J Gerontol A Biol Sci Med Sci. 2019;74:507–512. doi: 10.1093/gerona/gly074 [DOI] [PubMed] [Google Scholar]
- 12. Oswald F, Hans-Werner W, Voss E, et al. The use of tracking technologies for the analysis of outdoor mobility in the face of dementia: first steps into a project and some illustrative findings from Germany. J Hous Elderly. 2010;24:55–73. doi: 10.1080/02763890903327481 [DOI] [Google Scholar]
- 13. Maetzler W, Domingos J, Srulijes K, Ferreira JJ, Bloem BR. Quantitative wearable sensors for objective assessment of Parkinson’s disease. Mov Disord. 2013;28:1628–1637. doi: 10.1002/mds.25628 [DOI] [PubMed] [Google Scholar]
- 14. Wirtz M, Streit T, Chlond B, Vortisch P. On new measures for detection of data quality risks in mobility panel surveys. Transport Res Rec. 2013;2354:19–28. doi: 10.3141/2354-03 [DOI] [Google Scholar]
- 15. Phillips JL, Lam L, Luckett T, Agar M, Currow D. Is the Life Space Assessment applicable to a palliative care population? Its relationship to measures of performance and quality of life. J Pain Symptom Manage. 2014;47:1121–1127. doi: 10.1016/j.jpainsymman.2013.06.017 [DOI] [PubMed] [Google Scholar]
- 16. Kelly P, Krenn P, Titze S, Stopher P, Foster C. Quantifying the difference between self-reported and global positioning systems-measured journey durations: a systematic review. Transp Rev. 2013;33:443–459. doi: 10.1080/01441647.2013.815288 [DOI] [Google Scholar]
- 17. Houston D, Luong TT, Boarnet MG. Tracking daily travel; assessing discrepancies between GPS-derived and self-reported travel patterns. Transp Res Part C Emerg Technol. 2014;48:97–108. doi: 10.1016/j.trc.2014.08.013 [DOI] [Google Scholar]
- 18. Liddle J, Ireland D, McBride SJ, et al. Measuring the lifespace of people with Parkinson’s disease using smartphones: proof of principle. JMIR Mhealth Uhealth. 2014;2:e13. doi: 10.2196/mhealth.2799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Boissy P, Brière S, Hamel M, et al. Wireless inertial measurement unit with GPS (WIMU-GPS)-wearable monitoring platform for ecological assessment of lifespace and mobility in aging and disease. Conf Proc IEEE Eng Med Biol Soc. 2011;5815–5819. doi: 10.1109/IEMBS.2011.6091439 [DOI] [PubMed] [Google Scholar]
- 20. Fillekes MP, Röcke C, Katana M, Weibel R. Self-reported versus GPS-derived indicators of daily mobility in a sample of healthy older adults. Soc Sci Med. 2019;220:193–202. doi: 10.1016/j.socscimed.2018.11.010 [DOI] [PubMed] [Google Scholar]
- 21. Tung JY, Rose RV, Gammada E, et al. Measuring life space in older adults with mild-to-moderate Alzheimer’s disease using mobile phone GPS. Gerontology. 2014;60:154–162. doi: 10.1159/000355669 [DOI] [PubMed] [Google Scholar]
- 22. Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1(8476):307–310. doi: 10.1016/S0140-6736(86)90837-8 [DOI] [PubMed] [Google Scholar]
- 23. Kottner J, Audigé L, Brorson S, et al. Guidelines for reporting reliability and agreement studies (GRRAS) were proposed. J Clin Epidemiol. 2011;64:96–106. doi: 10.1016/j.jclinepi.2010.03.002 [DOI] [PubMed] [Google Scholar]
- 24. Mokkink LB, Terwee CB, Gibbons E, et al. Inter-rater reliability of the COSMIN (COnsensus-based standards for the selection of health Measurement INstruments) Checklist. BMC Med Res Methodol. 2010;10:82. doi: 10.1186/1471-2288-10-82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Mokkink LB, Terwee CB, Patrick DL, et al. The COSMIN checklist for assessing the methodological quality of studies on measurement properties of health status measurement instruments: an international Delphi study. Qual Life Res. 2010;19:539–549. doi: 10.1007/s11136-010-9606-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Boissy P, Blamoutier M, Brière S, Duval C. Quantification of free-living community mobility in healthy older adults using wearable sensors. Front Public Health. 2018;6:216. doi: 10.3389/fpubh.2018.00216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Portegijs E, Iwarsson S, Rantakokko M, Viljanen A, Rantanen T. Life-space mobility assessment in older people in Finland; measurement properties in winter and spring. BMC Res Notes. 2014;7:323. doi: 10.1186/1756-0500-7-323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Wu J, Jiang C, Liu Z, Houston D, Jaimes G, McConnell R. Performances of different global positioning system devices for time-location tracking in air pollution epidemiological studies. Environ Health Insights. 2010;4:93–108. doi: 10.4137/EHI.S6246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Almanza E, Jerrett M, Dunton G, Seto E, Pentz MA. A study of community design, greenness, and physical activity in children using satellite, GPS and accelerometer data. Health Place. 2012;18:46–54. doi: 10.1016/j.healthplace.2011.09.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Bricka SG, Sen S, Paleti R, Bhat CR. An analysis of the factors influencing differences in survey-reported and GPS-recorded trips. Transp Res Part C Emerg Technol. 2012;21:67–88. doi: 10.1016/j.trc.2011.09.005 [DOI] [Google Scholar]
- 31. Wolf J, Oliveira M, Thompson M. Impact of underreporting on mileage and travel time estimates: results from global positioning system-enhanced household travel survey. Transp Res Rec J Transp Res Board. 2003;1854:189–198. doi: 10.3141/1854-21 [DOI] [Google Scholar]
- 32. Gill DJ, Freshman A, Blender JA, Ravina B. The Montreal Cognitive Assessment as a screening tool for cognitive impairment in Parkinson’s disease. Mov Disord. 2008;23:1043–1046. doi: 10.1093/ageing/26.5.353 [DOI] [PubMed] [Google Scholar]
- 33. Jenkinson C, Fitzpatrick R, Peto V, Greenhall R, Hyman N. The Parkinson’s Disease Questionnaire (PDQ-39): development and validation of a Parkinson’s disease summary index score. Age Ageing. 1997;26:353–357. doi: 10.1093/ageing/26.5.353 [DOI] [PubMed] [Google Scholar]
- 34. Shumway-Cook A, Patla A, Stewart AL, Ferrucci L, Ciol MA, Guralnik JM. Assessing environmentally determined mobility disability: self-report versus observed community mobility. J Am Geriatr Soc. 2005;53:700–704. doi: 10.1111/j.1532-5415.2005.53222.x [DOI] [PubMed] [Google Scholar]
- 35. de Vet HC, Terwee CB, Knol DL, Bouter LM. When to use agreement versus reliability measures. J Clin Epidemiol. 2006;59:1033–1039. doi: 10.1016/j.jclinepi.2005.10.015 [DOI] [PubMed] [Google Scholar]
- 36. McNeil D. On graphing paired data. Am. Stat. 1992;46(4):307–311. doi: 10.1080/00031305.1992.10475915 [DOI] [Google Scholar]
- 37. Bland JM, Altman DG. Measuring agreement in method comparison studies. Stat Methods Med Res. 1999;8:135–160. doi: 10.1177/096228029900800204 [DOI] [PubMed] [Google Scholar]
- 38. Chhapola V, Kanwal SK, Brar R. Reporting standards for Bland-Altman agreement analysis in laboratory research: a cross-sectional survey of current practice. Ann Clin Biochem. 2015;52(Pt 3):382–386. doi: 10.1177/0004563214553438 [DOI] [PubMed] [Google Scholar]
- 39. Euser AM, Dekker FW, le Cessie S. A practical approach to Bland-Altman plots and variation coefficients for log transformed variables. J Clin Epidemiol. 2008;61:978–982. doi: 10.1016/j.jclinepi.2007.11.003 [DOI] [PubMed] [Google Scholar]
- 40. Stopher P, Shen L. In-depth comparison of global positioning system and diary records. Transp Res Rec J Transp Res Board. 2011;2246:32–37. doi: 10.3141/2246-05 [DOI] [Google Scholar]
- 41. Krenn PJ, Titze S, Oja P, Jones A, Ogilvie D. Use of global positioning systems to study physical activity and the environment: a systematic review. Am J Prev Med. 2011;41:508–515. doi: 10.1016/j.amepre.2011.06.046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Hirsch JA, Winters M, Ashe MC, Clarke P, McKay H. Destinations that older adults experience within their GPS activity spaces relation to objectively measured physical activity. Environ Behav. 2016;48:55–77. doi: 10.1177/0013916515607312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Wolf J, Loechl M, Thompson M, Arce C. Trip rate analysis in GPS-enhanced personal travel surveys. In: Jones P, Stopher P, ed. Transport Survey Quality and Innovation. Oxford, UK: Elsevier; 2003b:483–498. doi: 10.1108/9781786359551-028 [DOI] [Google Scholar]
- 44. Chlond B, Wirtz M, Zumkeller D. Data quality and completeness issues in multiday or panel surveys. In: Zmud J, Lee-Gosselin M, Munizaga M, Carrasco AJ. eds. Transport Survey Methods. Bingley UK: Emerald Publishing; 2013:373–392. doi: 10.1108/9781781902882-020 [DOI] [Google Scholar]
- 45. Bernad-Elazari H, Herman T, Mirelman A, Gazit E, Giladi N, Hausdorff JM. Objective characterization of daily living transitions in patients with Parkinson’s disease using a single body-fixed sensor. J Neurol. 2016;263:1544–1551. doi: 10.1007/s00415-016-8164-6 [DOI] [PubMed] [Google Scholar]
- 46. Hanneman SK. Design, analysis, and interpretation of method-comparison studies. AACN Adv Crit Care. 2008;19:223–234. doi: 10.1097/01.AACN.0000318125.41512.a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Shen L, Stopher PR. Review of GPS travel survey and GPS data-processing methods. Transp Rev. 2014;34:316–334. doi: 10.1080/01441647.2014.903530 [DOI] [Google Scholar]
- 48. Hirsch JA, Winters M, Clarke P, McKay H. Generating GPS activity spaces that shed light upon the mobility habits of older adults: a descriptive analysis. Int J Health Geogr. 2014;13:51. doi: 10.1186/1476-072X-13-51 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.