Abstract
Abstract
Very low birth weight (VLBW; <1500 g birth weight) infants are substantially more likely to be born to black than to non-black mothers, predisposing them to potentially preventable morbidities that increase the risk for costly lifelong health problems. Mothers’ own milk (MOM) may be considered the ultimate “personalized medicine” since milk composition and bioactive components vary among mothers and multiple milk constituents provide specific protection based on shared exposures between mother and infant. MOM feedings reduce the risks and associated costs of prematurity-associated morbidities, with the greatest reduction afforded by MOM through to NICU discharge. Although black and non-black mothers have similar lactation goals and initiation rates, black VLBW infants are half as likely to receive MOM at NICU discharge in the United States. Black mothers are significantly more likely to be low-income, single heads of household and have more children in the home, increasing the burden of MOM provision. Although rarely considered, the out-of-pocket and opportunity costs associated with providing MOM for VLBW infants are especially onerous for black mothers. When MOM is not available, the NICU assumes the costs of inferior substitutes for MOM, contributing further to disparate outcomes. Novel strategies to mitigate these disparities are urgently needed.
Impact
Mother’s own milk exemplifies personalized medicine through its unique biologic activity.
Hospital factors and social determinants of health are associated with mother’s own milk feedings for very low-birth-weight infants in the neonatal intensive care unit. Notably, out-of-pocket and opportunity costs associated with providing mother’s own milk are borne by mothers. Conceptualizing mother’s own milk feedings as an integral part of NICU care requires consideration of who bears the costs of MOM provision—the mother or the NICU?
Introduction
Premature very low-birth-weight (VLBW; <1500 g birth weight) infants are almost three times more likely to be born to non-Hispanic black (black) than to non-black (non-Hispanic white (white), Hispanic, Asian, Native American) mothers in the United States.1 VLBW infants have exceptionally immature body organs and underdeveloped immunomodulatory and metabolic pathways, all of which are in critical stages of development at birth and during the neonatal intensive care unit (NICU) hospitalization.2–11 Ubiquitous NICU stressors of inflammation, oxidative stress and suboptimal nutrition represent ill-timed insults that program abnormal growth and development, affecting health and neurodevelopmental outcomes long after the actual insult.2–9,11–15 Serious but potentially preventable NICU morbidities are a consequence of these immature organs and pathways and are associated with increased rates of rehospitalizations and neurodevelopmental problems,16–22 as well as higher costs due to longer hospitalizations and additional resource utilization.23,24 The estimated healthcare cost in the first 6 months of life for VLBW infants is $332,225 (2019 USD) compared to $7247 (2019 USD) for term infants.24 After the NICU hospitalization, the economic burden continues with higher healthcare and educational costs that are borne by families of VLBW infants and society at large.25–27
Whereas the immaturity of these organs and pathways is not modifiable, mother’s own milk (MOM; excludes donor human milk (DHM)) feedings optimize their growth and development while simultaneously preventing or reducing the impact of noxious NICU stressors.2,12 A prospective cohort study of 430 diverse VLBW infants28 revealed a dose-dependent relationship between MOM feedings during the NICU hospitalization and reduction in the risk and associated costs of morbidities.17,18,21 A significant dose-dependent relationship was also noted between MOM intake and decreased number of rehospitalizations and higher cognitive scores after discharge from the NICU.16,22 These and other studies support a strong link between MOM feedings and protection from NICU morbidities and their associated costs, making strategies to procure MOM a global priority.
Access to MOM, however, is not equitable among VLBW infants in the United States, with black infants significantly less likely to receive any MOM feedings at NICU discharge.29–31 A cohort study of mothers revealed that goals for MOM feedings at NICU discharge did not differ for black and non-black mothers. However, black mothers were less likely to achieve their goals despite having similar rates of initial MOM feedings.32,33
The determinants of an enabling breastfeeding environment incorporate multiple factors at all societal levels (Fig. 1),34 not simply the individual maternal level. Social determinants of health (SDH)35 influence MOM provision for all infants, including hospitalized VLBW infants, and may mediate racial/ethnic disparities in MOM provision.29,36 This disparity in MOM feedings significantly increases the burden of prematurity that is already highest in the black population. Furthermore, lack of MOM predisposes infants to health and neurodevelopmental problems, exacerbating disparities throughout the lifespan between black and non-black populations.
Fig. 1. Determinants of an enabling breastfeeding environment.
Adapted with permission of Elsevier, from ref. 34 Permission conveyed through Copyright Clearance Center, Inc.
MOM as personalized medicine
MOM exemplifies personalized medicine in its truest form; even DHM differs significantly from MOM and does not yield the same beneficial outcomes for VLBW infants.37,38 There is remarkable synchrony between the longitudinal changes in MOM composition and the infant’s needs for nutrition and protection from morbidities. Colostrum is rich in developmental and protective (e.g., non-nutritive) proteins, consisting primarily of immunoglobulins, growth factors, cytokines, hormones, and enzymes.10 The concentrations of several of these proteins are higher in preterm MOM than in term MOM. With progression of lactation, developmental and protective MOM proteins decrease and nutritive protein and lipid production increase.39 During mature lactation, the mammary gland continues to provide personalized medicine for the infant via the enteromammary pathway by which the mother produces specific antibodies to pathogens in the dyadic environment and secretes them into MOM. Similarly, the MOM microbiome is highly specific to the breastfeeding dyad, and early secretion of bacteria in MOM serves as a programming function for the infant gut microbiota.40 Finally, recent studies describe synergistic anti-infective interactions between MOM and the infant’s stomach and saliva, indicating that the true protective impact of MOM may not be appreciated by studying its composition alone. Thus the nutrients and bioactive components in MOM function synergistically to stimulate tissue growth, maturation, and programming of immunologic and biologic processes. Although an exhaustive description of MOM composition is beyond the scope of this review, select components are highlighted (Fig. 2).
Fig. 2.
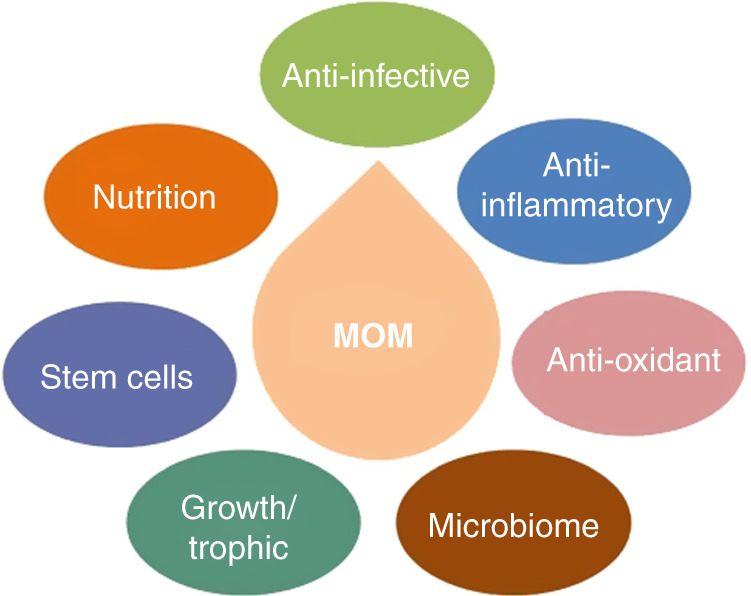
Mother’s own milk bioactive components.
Macronutrients and digestion
Factors including maternal diet, obesity, disease states, infections, genetics, and duration of gestation influence MOM composition.41,42 The protein content of MOM gradually decreases over the first several weeks of lactation, while carbohydrate and fat content increase. MOM fats provide substrate to support the rapidly growing brain, eyes and intestines,43 and play an important beneficial role in neurodevelopment.44,45 MOM contains enzymes, including lipases, proteases and amylases, to assist in digestion and absorption of nutrients, compensating for the immaturity of the neonatal digestive system.46
Bioactive components
Immunoglobulins
MOM immunoglobulins include secretory IgA, secretory IgM and IgG, which resist digestion. Secretory IgA is the predominant immunoglobulin, does not cross the placenta, and is available to the infant almost exclusively via MOM. Secretory IgA limits pathogen invasion of epithelial cells by binding and neutralizing bacteria and viruses,47 and is the highest during the first days after birth, especially in preterm MOM.48 MOM contains higher concentrations of immunoglobulins than does DHM.49
Leukocytes
Maternal immunity is also transferred to the infant through MOM leukocytes that originate from the mother’s gut and nasopharynx mucosa.50 Milk leukocyte concentration is highest in colostrum, except during infection in the mother and/or infant.51–54 MOM leukocytes survive immature neonatal digestive processes and have been found in distant sites. This microchimerism with maternally derived leukocytes may influence early and potentially later immune responses of the infant.
Growth factors
MOM contains at least 13 identified growth factors, many of which have specific roles in protection and maturation of the infant intestinal tract,55 immunomodulation,56 growth12 and neurodevelopment/neuroprotection.2,13,56 These growth factors are the highest in early lactation and both epidermal growth factor and transforming growth factor are higher in preterm than term MOM.55,57
Human milk oligosaccharides (HMOs)
HMOs are nondigestible carbohydrates and are the third most abundant component in MOM, despite having no known nutritional value. Over 200 different HMOs have been identified, varying in composition among mothers.58 HMOs have multiple actions that contribute to MOM’s anti-infective,59 anti-inflammatory,58 and gut colonizing effects.60
Stem cells
MOM contains pluripotent human breast milk stem cells (hBSCs).61 Concentrations of hBSCs are highest in colostrum, corresponding to the immature digestive tract that is conducive to transfer of cellular components. Preclinical studies demonstrate that hBSCs cross the neonatal gut, enter the circulation, and travel into various organs where they differentiate and become functional.62,63 Stem cells are destroyed by freezing or heating MOM, supporting the importance of feeding fresh MOM to infants.
Milk microbiome
MOM is not sterile, nor are all of the bacteria found in MOM simply due to contamination from the breast surface. In a breastfeeding dyad, bacteria from the infant’s oral cavity colonize the distal milk ducts during retrograde milk flow.64 Although controversial, maternal gut microflora, assisted by dendritic cells, are also thought to translocate across the maternal gut epithelial cells, transfer to the lactating mammary gland, and be secreted into MOM.65 Aseptically collected MOM was found to contain bacteria common to maternal feces, blood and milk, and also infant feces.66,67 Thus the milk microbiome may enable maternal microbes to colonize the infant’s gut, which has low microbial diversity early in life.40
Protective potential of MOM is not measured by milk composition alone
The interaction between MOM and infant may result in greater protection than is measured in the milk itself, with release of immunomodulatory and anti-infective peptides in the infant’s stomach that exceed the number in the pre-fed MOM,68 with higher peptide release in preterm MOM than term MOM.46 Similarly, the interaction between MOM enzymes and the infant’s saliva produce superoxide and hydrogen peroxide, which inhibit opportunistic pathogenic bacteria.69 In the NICU, the routine use of MOM as oropharyngeal care may reduce the risk of ventilator-associated pneumonia through multiple synergistic mechanisms, including this MOM−saliva interaction.70 Thus, MOM is the consummate personalized medicine for all infants, especially premature VLBW infants. However, the greatest benefit from MOM occurs when it is fed fresh (i.e., not frozen or pasteurized)10,71 to minimize reductions in multiple protective MOM components. A trial is underway to test whether feeding partial fresh milk each day improves clinical outcomes in premature infants in the NICU.72
Disparities in breastfeeding initiation and duration
Unlike mothers of healthy newborns, most mothers of VLBW infants are completely dependent on the breast pump to substitute for the infant during breastfeeding, which involves not only MOM removal but also regulating key lactation mechanisms that are essential for long-term MOM synthesis.71,73–75 Additionally, MOM synthesis and secretion may also be adversely affected by pregnancy and birth complications and the intense emotional distress associated with having a VLBW infant in the NICU.73,76–79
With recommendations from the American Academy of Pediatrics80 and quality initiatives focused on MOM,81–83 the initiation rates of MOM provision have increased in many institutions;81,82 however, disparities in sustaining MOM provision remain.29,84 Despite high initiation rates and a goal to continue MOM provision after NICU discharge, significantly fewer black VLBW infants continue to receive MOM at NICU discharge compared to non-black infants.29–32 This disparity is prevalent across the US, irrespective of the geographic region (Fig. 3).31
Fig. 3. US regional variation in any human milk at discharge by maternal race/ethnicity.
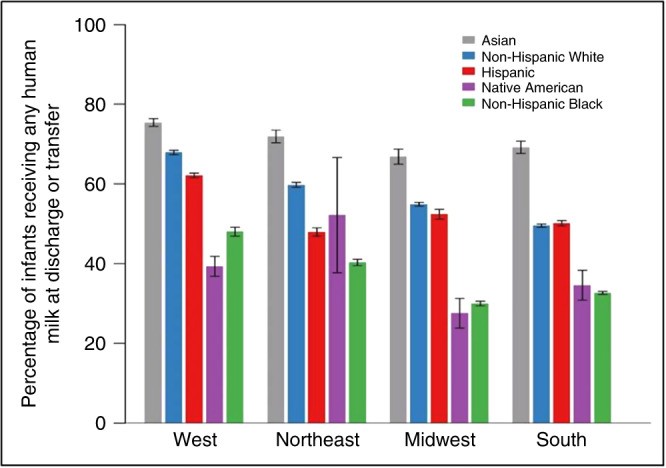
Reproduced with permission from ref. 31 Copyright© 2019 American Medical Association. All rights reserved. Permission conveyed through Copyright Clearance Center, Inc.
Hospital factors associated with MOM feedings and disparities
Hospital processes and structures have played a role in the existing disparities, but also have an important role in developing and implementing solutions. Recently, a large retrospective cohort study of very preterm neonates examined whether differences in neonatal morbidity and mortality rates among black, Hispanic, and white infants were explained by delivery hospital.85 Although infants’ health risks explained a significant proportion of differences in outcomes between black and white infants and between Hispanic and white infants, a significant proportion of disparity in outcomes was due to the quality of the hospital of delivery. In other words, differences in neonatal mortality and morbidity were attributed to the fact that white mothers received care at better performing hospitals than black or Hispanic mothers (Fig. 4).85
Fig. 4. Kolmogorov−Smirnov test of difference between racial-ethnic distribution of VPTB infants with increasing hospital neonatal morbidity-mortality rank.
Adapted with permission from ref. 85 Copyright© 2018 American Medical Association. All rights reserved. Permission conveyed through Copyright Clearance Center, Inc. Black and Hispanic VPTB infants are more likely to be born in New York City hospitals with higher risk-adjusted neonatal morbidity and mortality rates than are white VPTB infants. The dashed lines indicate the hospital rank cut-off at which 50% of infants are born for each race/ethnicity. The green line indicates that 50% white VPTB infants are born at hospitals that rank 1–20 in safety or have lower neonatal morbidity or mortality rates. The red line indicates that 50% Hispanic VPTB infants are born at hospitals that rank 1–21 in safety. The blue line indicates that 50% black VPTB infants are born at hospitals that rank 1–25 in safety. VPTB, very preterm birth.
Similarly, disparity in MOM feedings may also reflect hospital-level variation in quality. Boundy et al. found that NICU segregation (i.e., NICUs located in areas where the proportion of black residents was above or below the national average) was significantly associated with NICU nutritional practices.86 Provision of both MOM and DHM was lower in NICUs located in areas with higher percentages of black residents than those in areas with lower percentages of black residents. While many studies have found that MOM provision is associated with individual and hospital factors, DHM availability reflects hospital-level factors that are generally independent of maternal SDH or health factors.
Low provision of MOM is frequently reported as an outcome, but is a quality deficit that may reflect NICU and hospital processes; thus, it is potentially modifiable and represents opportunities for quality improvement.30 NICUs have made great efforts in recent years to encourage and provide resources to increase MOM feedings for all infants. However, unlike other racial/ethnic groups, the disparity between black and white infants of all gestations is widening and may reflect poor access or inequity of breastfeeding programs and supports provided to black mothers.87 Ultimately, hospital quality of care is one of the causal pathways by which segregation and inequality adversely affect outcomes of very preterm infants.88
Social determinants of health that contribute to disparities
Studies of hospitalized premature infants have revealed that maternal-level SDH influence MOM provision and contribute to racial/ethnic disparities. These SDH include race/ethnicity, economic factors, neighborhood factors and immigration status,36,89,90 and cultural factors. While race and ethnicity are established as contributing to disparities, the mediators that propagate these disparities have been minimally investigated.
In a study of the individual- and community-level factors35 that predict MOM feeding at NICU discharge and factors that mediate racial/ethnic disparity for VLBW infants. Patel et al. found that low daily pumping frequency during the first 14 days, low socioeconomic status (SES) and breastfeeding support from the mother’s mother were predictive of discontinuing MOM.29 The relation between white vs. black mothers and MOM at discharge was mediated by maternal age, low SES, and daily pumping frequency. Low SES may have also been reflected by access to a car, and black mothers were significantly less likely to have access to a car than white or Hispanic mothers.91 Furthermore, black mothers and families visited the NICU 20% less frequently than mothers and families of non-black VLBW infants,92 suggesting that black mothers and families were less likely to bring MOM from home to the NICU.
Despite having similar rates of low maternal SES, Hispanic infants were more likely to receive MOM at NICU discharge than black infants, mediated by maternal age and daily pumping frequency. This disparity persisted in the subgroup of WIC-eligible black and Hispanic mothers, similar to findings of an outpatient study in Philadelphia.93 Together, these data indicate that low SES affects MOM provision differently for Hispanic and black mothers, potentially due to differences in cultural support for breastfeeding and access to a car.36,90 However, two multicenter studies of VLBW infants demonstrated that Hispanic infants had lower rates of MOM at NICU discharge compared to white infants, suggesting there may be geographic variation in racial and ethnic differences.94,95
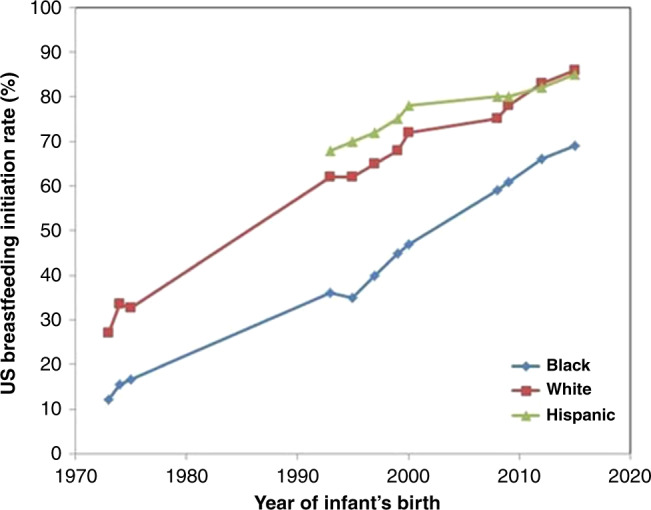
Another significant factor is the family’s previous history of breastfeeding,36 particularly the intergenerational transmission of breastfeeding beliefs and behaviors from the maternal grandmother to mother. In the US, black maternal grandmothers are the most frequent non-maternal caregivers during the first year of life96 and may transmit both supportive and maladaptive views regarding MOM.97–100 The historical context of slavery in which black women were forced to serve as wet-nurses may influence black women’s views of MOM, especially for maternal grandmothers.99,100 Furthermore, black mothers have few breastfeeding role models due to low breastfeeding rates in black US women (Fig. 5),101,102 especially in previous generations,103–105 and black mothers have reported a gap between the support desired and the support received from their own mothers.106
Fig. 5. US breastfeeding rates from 1970 to 2015 by maternal race/ethnicity.
Economic barriers associated with MOM feedings and disparities
Mothers of VLBW infants incur additional out-of-pocket costs to provide MOM that are not required by mothers of healthy term infants, including breast pump rental, transport of MOM to the NICU91 and the opportunity (time) cost of MOM provision that may exceed that of mothers of healthy term infants. The barriers to sustaining MOM provision through to NICU discharge are sizeable for all mothers but disproportionately impact black mothers who are more likely to be low income.107 The period of time while an infant is in the NICU is economically burdensome for low-income mothers due to the cost of transportation, parking, childcare and food outside the home due to frequent trips to the NICU. Additionally, because low-income mothers are less likely to have paid maternity leave, they experience additional earnings loss due to time away from work.
Common proxies for poverty include eligibility for the Special Supplemental Nutrition Program for Women, Infants and Children (WIC) and Medicaid, and both have been shown to have a negative association with MOM feedings.29,32 However, it is not clear whether the association between MOM provision and WIC and Medicaid eligibility is due to barriers to accessing high-quality equipment and services, such as NICU lactation experts, hospital-grade breast pumps, and other resources, such as a car to facilitate NICU visits,91 or due to breastfeeding promotion practices at WIC agencies.108
Access to high-quality, hospital-grade breast pump
The quality of breast pumps varies in terms of effectiveness, efficiency, comfort and convenience, with high-quality, hospital-grade electric breast pumps facilitating sustained MOM provision.73 Breast pumps provided by public nutrition and health programs do not consistently meet minimum criteria required for breast pump dependency and are intended instead to supplement MOM removal for breastfeeding mothers of term infants during brief separations.73 Despite evidence demonstrating that consistent, frequent breast pump use during the first 14 days postpartum significantly increases the likelihood of continued MOM feedings through NICU discharge,77 low-income mothers of VLBW infants often encounter several days of delay in acquiring a breast pump, which may be inferior in quality to a hospital-grade electric breast pump.71,73,109 While manual expression combined with breast pumping has been utilized,110 manual expression alone is inadequate for this population of mothers,111 thus highlighting the importance of ensuring access to hospital-grade electric breast pumps.
Opportunity cost of MOM provision
The opportunity cost of MOM provision, the value of the mother’s time spent pumping and storing breast milk, is greater for pump-dependent mothers than for mothers who directly breastfeed. Mothers of VLBW infants pump an average of 100 min daily to maintain established lactation112 and 20 min to label and store the pumped MOM and sanitize breast pump equipment, translating into foregone paid or unpaid work of approximately 120 min daily. Additionally, mothers of infants in the NICU have an additional opportunity cost of delivering pumped milk to the NICU.
Return to work
The opportunity cost of MOM provision is even more onerous for mothers once they return to work, and return-to-work is associated with reduced intensity and duration of breastfeeding.113,114 The opportunity cost is further exacerbated for mothers of infants in the NICU, particularly when mothers return to work prior to their infant’s discharge from the hospital. The United States and Australia were the only two countries in developed economies and the European Union that had unpaid maternity leave.115 Although US federal law requires employers to allow parents to take at least 12 weeks of leave with the birth of a child, the leave may be unpaid.116 There is a vast disparity in access to paid time off by income, with workers in the lowest quartile of wages receiving very limited time (47% paid sick time and 8% paid leave) compared to workers in the highest quartile of wages (90% paid sick time and 30% paid leave).117 This disparity in paid time off similarly disadvantages low-income women’s ability to provide MOM. Some low-wage jobs, such as manual and administrative positions, are associated with an even higher risk for discontinuing breastfeeding113 due to limited flexibility for breaks and lack of access to lactation rooms, further widening disparities. A recent study spanning more than 20 years, however, has demonstrated that state laws requiring or encouraging employers to provide breastfeeding facilities and breaks are associated with a significant increase in breastfeeding rates,118 suggesting that state-level policies can help address barriers to lactation in the workplace.
Perspectives regarding who incurs the cost of feedings in the NICU
These economic considerations give rise to further inequities because providing MOM is typically seen as a mother’s “job” or “special gift that only she can provide.”119–124 The out-of-pocket and opportunity costs are seldom recognized by NICU staff and hospital administrators, perpetuating the subtle disparity that black mothers who are unable to adhere to MOM provision are also less involved in infant care and lack of interest in breastfeeding. In contrast, research reveals that black mothers initiate MOM provision when encouraged by the NICU staff because they understand MOM’s beneficial effects on their infants’ health.120–124 However, current NICU strategies do not address the economic burden of MOM provision faced by mothers which is particularly relevant to low SES mothers, and may exacerbate inequities given that low SES mediates black−white disparities.29
In contrast, when MOM is not available for VLBW infants, the NICU acquires (i.e., assumes all the costs) DHM as the recommended alternative, although DHM feedings do not afford the same protections of MOM feedings.38 Similarly, NICUs assume the cost of formula when MOM or DHM are not available. Although health authorities80,125,126 prioritize MOM over DHM or formula, the NICU infrastructure is typically not funded to acquire MOM, thereby incentivizing the use of readily available but inferior substitutes.
Strategies for addressing social determinants of health
Racial and ethnic disparities in MOM feedings are due to factors that differ both within an individual NICU and between NICUs30,85,127; thus, strategies to address SDH need to target multiple areas. Standardized approaches to screening for SDH and access to social services have been recommended.128 The following strategies are based on expert opinions and quality improvement experiences due to the paucity of studies that provide evidence to guide initiatives. Guidelines proposed by Howell and Ahmed129 to address disparity in maternal health provide a framework for approaching disparity in MOM provision for VLBW infants.
Measurement
Measurement is a vital step in the quality improvement process to identify problems before potential strategies can be developed. Recent publications have clearly established the racial/ethnic disparities in MOM feeding in US NICUs;29,30,95 so, measuring these racial/ethnic variations in MOM feeding outcomes in individual NICUs is a key first step.
Standardize care
The significant disparities in quality of care within NICUs30 demonstrate opportunities for standardizing care, regardless of race or ethnicity. Of concern is that qualitative studies of black mothers report that they do not uniformly receive breastfeeding education or recommendations to provide MOM from healthcare providers.130,131 Education of NICU staff and providing breastfeeding education and support to mothers is a cornerstone of many successful NICU breastfeeding quality improvement initiatives.81,82,132,133 NICUs should ensure that all mothers of NICU infants receive the same education and support with careful review of reports of inequity or variation in practice.129
Develop new models of care
Black women are less likely to have seen other women provide MOM or receive education about MOM.100,134 Meier developed a novel model of providing evidence-based lactation support to mothers of infants in the NICU by employing NICU breastfeeding peer counselors, all of whom are parents of former NICU infants and reflect the racial and ethnic characteristics of NICU families.122–124,135,136 Research has shown that this model is effective in increasing MOM provision and is valued by mothers.136 Another potential model is the provision of breastfeeding education to fathers and other family members to increase support for the lactating mother, as some mothers report unsupportive behavior for pumping or providing MOM.121
Enhance communication
Healthcare providers exhibit implicit bias at similar levels as the general population. A systematic review demonstrated a significant positive relationship between level of implicit bias and lower quality of care and/or communication.137 Furthermore, black mothers report that they do not uniformly receive breastfeeding education or recommendations to provide MOM from healthcare providers, which may reflect implicit bias or racism.130,131 Incorporating cultural competency such as implicit bias training as part of training curricula has garnered support in recent years,138,139 although efficacy of this training in decreasing disparity in MOM provision is unknown at this time.
Strategies for mitigating economic barriers
One approach for addressing economic barriers to MOM provision for VLBW infants is shifting the costs of MOM provision from the mother to the NICU, mimicking the approach to acquiring DHM or formula. While some hospitals may provide free parking, childcare or meals at no cost, these measures do not directly address the costs associated with providing MOM. Strategies to address the economic barriers to MOM provision should consider the rental cost of a hospital-grade electric breast pump for in-home use, transportation of MOM from home to the NICU, and maternal opportunity cost. While provision of the breast pump and milk transportation have a straightforward market value, mechanisms for covering the maternal opportunity cost of MOM provision warrant further discussion.
A promising strategy for addressing the maternal opportunity cost is the use of conditional cash transfers (CCTs), specifically monetary transfers made to individuals for fulfilling a specific, pre-defined behavior or action that increases human capital.140 No previous research has studied the effectiveness of CCTs in increasing lactation rates for mothers of VLBW infants; however, several recent studies have examined whether CCTs and other financial incentives are effective strategies for increasing breastfeeding rates in term infants.141–145 One RCT from the United Kingdom enrolled mothers who resided in communities with lower than the country’s average SES and baseline breastfeeding rates. This study revealed higher rates of any but not of exclusive breastfeeding in the CCT group (receiving £200 total) at 6–8 weeks post-birth.141 The CCT had no effect on mothers’ decisions to initiate lactation, but mothers perceived CCT as showing “value” for breastfeeding, compensating for ongoing breastfeeding challenges and facilitating achievement of targeted breastfeeding milestones (e.g., 6 weeks, 3 months).145 Research on the use of financial incentives to increase breastfeeding in healthy but primarily disadvantaged populations reveal that mothers value cash or cash equivalents more than other financial incentives such as grocery vouchers or baby supplies,145,146 and healthcare providers are generally positive but cautioned about choosing the proper incentive.147–149 One small US study randomized 36 Puerto Rican mothers of healthy term infants to receive either WIC-only or WIC + CCT (≤$270 total over 6 months) and found that mothers in the WIC + CCT group had significantly higher rates of any but not of exclusive breastfeeding at 1 (89% vs 44%), 3 (89% vs 17%) and 6 (72% vs 0%) months post-birth.138 Both RCTs142,144 were limited in that financial incentives were not tied to actual opportunity costs of breastfeeding, and receipt of financial incentives was delayed (paid monthly or at longer intervals) despite the fact that breastfeeding incurs a daily opportunity cost and the effect of a CCT on behavior change diminishes with delay in its receipt.150
The existing research on CCTs has several implications for reducing disparities in MOM provision for VLBW infants. CCTs should (1) focus on sustaining not initiating MOM provision;142,144,145 (2) use cash rather than non-cash payments;145,146 (3) make payments frequently to strengthen the impact of the intervention;150 (4) compensate mothers fairly for MOM provision;140 and (5) focus on short-term behavior change, for which CCTs have been shown most effective vs long-term or lifelong behavior change.151 Ongoing RCTs of CCT in US term152 and VLBW infants153 will provide evidence regarding the efficacy of this strategy in reducing disparities in MOM feedings.
Conclusions
The composition and bioactive components in MOM evolve based on the maturation of the mammary gland and in response to the infant’s requirements to provide the ultimate personalized medicine to the infant, thereby supporting growth, development, and protection from infection and inflammation. Importantly, MOM feedings are associated with reductions in morbidities and their costs in VLBW infants. Despite the known benefits, disparities in MOM provision based on race, ethnicity and SES are prevalent in US NICUs. These disparities are mediated by hospital factors as well as other SDH, with black mothers of VLBW infants particularly impacted by variation in NICU quality and social and economic inequities. Conceptualizing MOM feedings as an integral part of NICU care requires consideration of who bears the costs of MOM provision—the mother or the NICU? Novel interventional studies to offset costs traditionally borne by mothers that include CCTs will provide data to inform NICU policies and practices.
Acknowledgements
A.L.P, T.J.J., and P.P.M. receive support from the National Institute on Minority Health and Health Disparities of the National Institutes of Health under Award Number R01MD013969. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author contributions
All authors approved the final manuscript as submitted. All authors contributed to the conception, design, and drafting of this article, revising it critically for intellectual content, and gave final approval of the version to be published.
Competing interests
A.L.P. declares no potential conflict of interest. T.J.J. has received consulting funds from Medela. P.P.M. has received research support and honoraria from Medela and serves on the Scientific Advisory Board for Family Larsson-Rosenquist Foundation.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.March of Dimes. Very low birthweight by race/ethnicity: United States, 2016−2018 Average. https://www.marchofdimes.org/Peristats/Peristats.aspx (2020).
- 2.Keunen K, van Elburg RM, van Bel F, Benders MJ. Impact of nutrition on brain development and its neuroprotective implications following preterm birth. Pediatr. Res. 2015;77:148–155. doi: 10.1038/pr.2014.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Collado MC, et al. Microbial ecology and host-microbiota interactions during early life stages. Gut Microbes. 2012;3:352–365. doi: 10.4161/gmic.21215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shah DK, et al. Adverse neurodevelopment in preterm infants with postnatal sepsis or necrotizing enterocolitis is mediated by white matter abnormalities on magnetic resonance imaging at term. J. Pediatr. 2008;153:170–175. doi: 10.1016/j.jpeds.2008.02.033. [DOI] [PubMed] [Google Scholar]
- 5.Chau V, et al. Postnatal infection is associated with widespread abnormalities of brain development in premature newborns. Pediatr. Res. 2012;71:274–279. doi: 10.1038/pr.2011.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Penido AB, et al. Malnutrition during central nervous system growth and development impairs permanently the subcortical auditory pathway. Nutr. Neurosci. 2012;15:31–36. doi: 10.1179/1476830511Y.0000000022. [DOI] [PubMed] [Google Scholar]
- 7.Volpe JJ. Systemic inflammation, oligodendroglial maturation, and the encephalopathy of prematurity. Ann. Neurol. 2011;70:525–529. doi: 10.1002/ana.22533. [DOI] [PubMed] [Google Scholar]
- 8.Strunk T, et al. Infection-induced inflammation and cerebral injury in preterm infants. Lancet Infect. Dis. 2014;14:751–762. doi: 10.1016/S1473-3099(14)70710-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thompson DK, et al. Longitudinal growth and morphology of the hippocampus through childhood: impact of prematurity and implications for memory and learning. Hum. Brain Mapp. 2014;35:4129–4139. doi: 10.1002/hbm.22464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sherman MP, Zaghouani H, Niklas V. Gut microbiota, the immune system, and diet influence the neonatal gut-brain axis. Pediatr. Res. 2015;77:127–135. doi: 10.1038/pr.2014.161. [DOI] [PubMed] [Google Scholar]
- 11.Lewis ED, Richard C, Larsen BM, Field CJ. The importance of human milk for immunity in preterm infants. Clin. Perinatol. 2017;44:23–47. doi: 10.1016/j.clp.2016.11.008. [DOI] [PubMed] [Google Scholar]
- 12.Hansen-Pupp I, et al. Influence of insulin-like growth factor I and nutrition during phases of postnatal growth in very preterm infants. Pediatr. Res. 2011;69(5 Pt 1):448–453. doi: 10.1203/PDR.0b013e3182115000. [DOI] [PubMed] [Google Scholar]
- 13.Hansen-Pupp I, et al. Circulatory insulin-like growth factor-I and brain volumes in relation to neurodevelopmental outcome in very preterm infants. Pediatr. Res. 2013;74:564–569. doi: 10.1038/pr.2013.135. [DOI] [PubMed] [Google Scholar]
- 14.Kuban KC, et al. The breadth and type of systemic inflammation and the risk of adverse neurological outcomes in extremely low gestation newborns. Pediatr. Neurol. 2015;52:42–48. doi: 10.1016/j.pediatrneurol.2014.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.O’Shea TM, et al. Inflammation-initiating illnesses, inflammation-related proteins, and cognitive impairment in extremely preterm infants. Brain Behav. Immun. 2013;29:104–112. doi: 10.1016/j.bbi.2012.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Patra K, et al. NICU Human milk dose and 20-month neurodevelopmental outcome in very low birth weight infants. Neonatology. 2017;112:330–336. doi: 10.1159/000475834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Patel AL, et al. Influence of own mother’s milk on bronchopulmonary dysplasia and costs. Arch. Dis. Child Fetal Neonatal Ed. 2017;102:F256–F261. doi: 10.1136/archdischild-2016-310898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Patel AL, et al. Impact of early human milk on sepsis and health care costs in very low birthweight infants. J. Perinatol. 2013;33:514–519. doi: 10.1038/jp.2013.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vohr BR, et al. Persistent beneficial effects of breast milk ingested in the neonatal intensive care unit on outcomes of extremely low birth weight infants at 30 months of age. Pediatrics. 2007;120:e953–e959. doi: 10.1542/peds.2006-3227. [DOI] [PubMed] [Google Scholar]
- 20.Lechner BE, Vohr BR. Neurodevelopmental outcomes of preterm infants fed human milk: a systematic review. Clin. Perinatol. 2017;44:69–83. doi: 10.1016/j.clp.2016.11.004. [DOI] [PubMed] [Google Scholar]
- 21.Johnson TJ, Patel AL, Bigger HR, Engstrom JL, Meier PP. Cost savings of human milk as a strategy to reduce the incidence of necrotizing enterocolitis in very low birth weight infants. Neonatology. 2015;107:271–276. doi: 10.1159/000370058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Johnson TJ, et al. NICU human milk dose and health care use after NICU discharge in very low birth weight infants. J. Perinatol. 2019;39:120–128. doi: 10.1038/s41372-018-0246-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Johnson TJ, Patel AL, Jegier BJ, Engstrom JL, Meier PP. Cost of morbidities in very low birth weight infants. J. Pediatr. 2013;162:243–249. doi: 10.1016/j.jpeds.2012.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Beam AL, et al. Estimates of healthcare spending for preterm and low-birthweight infants in a commercially insured population: 2008−2016. J. Perinatol. 2020;40:1091–1099. doi: 10.1038/s41372-020-0635-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hillman LS, Day LS, Hoffman HJ, Stockbauer JW. Poorer outcomes of all low birth weight groups at age 10: Missouri statewide case-control study. Early Hum. Dev. 2019;136:60–69. doi: 10.1016/j.earlhumdev.2019.05.006. [DOI] [PubMed] [Google Scholar]
- 26.Litt JS, et al. Academic achievement of adolescents born with extremely low birth weight. Acta Paediatr. 2012;101:1240–1245. doi: 10.1111/j.1651-2227.2012.02790.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Boulet SL, Schieve LA, Boyle CA. Birth weight and health and developmental outcomes in US children, 1997−2005. Matern. Child Health J. 2011;15:836–844. doi: 10.1007/s10995-009-0538-2. [DOI] [PubMed] [Google Scholar]
- 28.Meier PP. Human milk and clinical outcomes in preterm infants. Nestle Nutr. Inst. Workshop Ser. 2019;90:163–174. doi: 10.1159/000490304. [DOI] [PubMed] [Google Scholar]
- 29.Patel AL, et al. Mediators of racial and ethnic disparity in mother’s own milk feeding in very low birth weight infants. Pediatr. Res. 2019;85:662–670. doi: 10.1038/s41390-019-0290-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Profit J, et al. Racial/ethnic disparity in nicu quality of care delivery. Pediatrics. 2017;140:e20170918. doi: 10.1542/peds.2017-0918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Parker MG, et al. National trends in the provision of human milk at hospital discharge among very low-birth-weight infants. JAMA Pediatr. 2019;173:961–968. doi: 10.1001/jamapediatrics.2019.2645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pineda RG. Predictors of breastfeeding and breastmilk feeding among very low birth weight infants. Breastfeed. Med. 2011;6:15–19. doi: 10.1089/bfm.2010.0010. [DOI] [PubMed] [Google Scholar]
- 33.Hoban R, et al. Goals for human milk feeding in mothers of very low birth weight infants: how do goals change and are they achieved during the NICU hospitalization? Breastfeed. Med. 2015;10:305–311. doi: 10.1089/bfm.2015.0047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rollins NC, et al. Why invest, and what it will take to improve breastfeeding practices? Lancet. 2016;387:491–504. doi: 10.1016/S0140-6736(15)01044-2. [DOI] [PubMed] [Google Scholar]
- 35.Lorch SA, Enlow E. The role of social determinants in explaining racial/ethnic disparities in perinatal outcomes. Pediatr. Res. 2016;79:141–147. doi: 10.1038/pr.2015.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McKinney CO, et al. Racial and ethnic differences in breastfeeding. Pediatrics. 2016;138:e20152388. doi: 10.1542/peds.2015-2388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.O’Connor DL, et al. Effect of supplemental donor human milk compared with preterm formula on neurodevelopment of very low-birth-weight infants at 18 months: a randomized clinical trial. JAMA. 2016;316:1897–1905. doi: 10.1001/jama.2016.16144. [DOI] [PubMed] [Google Scholar]
- 38.Quigley M, Embleton ND, McGuire W. Formula versus donor breast milk for feeding preterm or low birth weight infants. Cochrane Database Syst. Rev. 2018;6:CD002971. doi: 10.1002/14651858.CD002971.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lemay DG, et al. RNA sequencing of the human milk fat layer transcriptome reveals distinct gene expression profiles at three stages of lactation. PLoS ONE. 2013;8:e67531. doi: 10.1371/journal.pone.0067531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pannaraj PS, et al. Association between breast milk bacterial communities and establishment and development of the infant gut microbiome. JAMA Pediatr. 2017;171:647–654. doi: 10.1001/jamapediatrics.2017.0378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Martin, C. R., Ling, P. R. & Blackburn, G. L. Review of infant feeding: key features of breast milk and infant formula. Nutrients10.3390/nu8050279 (2016). [DOI] [PMC free article] [PubMed]
- 42.Hinde K, et al. Daughter dearest: sex-biased calcium in mother’s milk among rhesus macaques. Am. J. Phys. Anthropol. 2013;151:144–150. doi: 10.1002/ajpa.22229. [DOI] [PubMed] [Google Scholar]
- 43.Ninkina N, et al. Stem cells in human breast milk. Hum. Cell. 2019;32:223–230. doi: 10.1007/s13577-019-00251-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Guxens M, et al. Breastfeeding, long-chain polyunsaturated fatty acids in colostrum, and infant mental development. Pediatrics. 2011;128:e880–e889. doi: 10.1542/peds.2010-1633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Blesa M, et al. Early breast milk exposure modifies brain connectivity in preterm infants. Neuroimage. 2018;184:431–439. doi: 10.1016/j.neuroimage.2018.09.045. [DOI] [PubMed] [Google Scholar]
- 46.Dallas DC, et al. Endogenous human milk peptide release is greater after preterm birth than term birth. J. Nutr. 2015;145:425–433. doi: 10.3945/jn.114.203646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Demers-Mathieu, V., Underwood, M. A., Beverly, R. L., Nielsen S. D. & Dallas, D. C. Comparison of human milk immunoglobulin survival during gastric digestion between preterm and term infants. Nutrients10.3390/nu10050631 (2018). [DOI] [PMC free article] [PubMed]
- 48.Ballabio C, et al. Immunoglobulin-A profile in breast milk from mothers delivering full term and preterm infants. Int. J. Immunopathol. Pharm. 2007;20:119–128. doi: 10.1177/039463200702000114. [DOI] [PubMed] [Google Scholar]
- 49.Demers-Mathieu, V. et al. Antenatal influenza A-Specific IgA, IgM, and IgG antibodies in mother’s own breast milk and donor breast milk, and gastric contents and stools from preterm infants. Nutrients10.3390/nu11071567 (2019). [DOI] [PMC free article] [PubMed]
- 50.Laouar A. Maternal leukocytes and infant immune programming during breastfeeding. Trends Immunol. 2020;41:225–239. doi: 10.1016/j.it.2020.01.005. [DOI] [PubMed] [Google Scholar]
- 51.Bode L, et al. It’s alive: microbes and cells in human milk and their potential benefits to mother and infant. Adv. Nutr. 2014;5:571–573. doi: 10.3945/an.114.006643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hassiotou F, et al. Maternal and infant infections stimulate a rapid leukocyte response in breastmilk. Clin. Transl. Immunol. 2013;2:e3. doi: 10.1038/cti.2013.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hassiotou F, Geddes DT. Immune cell-mediated protection of the mammary gland and the infant during breastfeeding. Adv. Nutr. 2015;6:267–275. doi: 10.3945/an.114.007377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Riskin A, et al. Changes in immunomodulatory constituents of human milk in response to active infection in the nursing infant. Pediatr. Res. 2012;71:220–225. doi: 10.1038/pr.2011.34. [DOI] [PubMed] [Google Scholar]
- 55.Kidwell, W. R. & Salomon, D. S. in Protein and Non-Protein Nitrogen in Human Milk (eds. Atkinson, S. A. & Lonnerdal, B.). 77−91 (CRC Press, Inc., Boca Raton, FL, 1989).
- 56.Collado MC, et al. Longitudinal study of cytokine expression, lipid profile and neuronal growth factors in human breast milk from term and preterm deliveries. Nutrients. 2015;7:8577–8591. doi: 10.3390/nu7105415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Dvorak B, Fituch CC, Williams CS, Hurst NM, Schanler RJ. Concentrations of epidermal growth factor and transforming growth factor-alpha in preterm milk. Adv. Exp. Med. Biol. 2004;554:407–409. doi: 10.1007/978-1-4757-4242-8_52. [DOI] [PubMed] [Google Scholar]
- 58.He Y, Lawlor NT, Newburg DS. Human milk components modulate toll-like receptor-mediated inflammation. Adv. Nutr. 2016;7:102–111. doi: 10.3945/an.115.010090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Morrow AL, Ruiz-Palacios GM, Jiang X, Newburg DS. Human-milk glycans that inhibit pathogen binding protect breast-feeding infants against infectious diarrhea. J. Nutr. 2005;135:1304–1307. doi: 10.1093/jn/135.5.1304. [DOI] [PubMed] [Google Scholar]
- 60.Yu ZT, et al. The principal fucosylated oligosaccharides of human milk exhibit prebiotic properties on cultured infant microbiota. Glycobiology. 2013;23:169–177. doi: 10.1093/glycob/cws138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hassiotou F, et al. Breastmilk is a novel source of stem cells with multilineage differentiation potential. Stem Cells. 2012;30:2164–2174. doi: 10.1002/stem.1188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hassiotou, F. et al. Breastmilk stem cell transfer from mother to neonatal organs. FASEB J.28, 10.1096/fasebj.28.1_supplement.216.4 (2014).
- 63.Aydin MS, Yigit EN, Vatandaslar E, Erdogan E, Ozturk G. Transfer and integration of breast milk stem cells to the brain of suckling pups. Sci. Rep. 2018;8:14289. doi: 10.1038/s41598-018-32715-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ramsay DT, Kent JC, Owens RA, Hartmann PE. Ultrasound imaging of milk ejection in the breast of lactating women. Pediatrics. 2004;113:361–367. doi: 10.1542/peds.113.2.361. [DOI] [PubMed] [Google Scholar]
- 65.Demmelmair H, Jimenez E, Collado MC, Salminen S, McGuire MK. Maternal and perinatal factors associated with the human milk microbiome. Curr. Dev. Nutr. 2020;4:nzaa027. doi: 10.1093/cdn/nzaa027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Perez PF, et al. Bacterial imprinting of the neonatal immune system: lessons from maternal cells? Pediatrics. 2007;119:e724–e732. doi: 10.1542/peds.2006-1649. [DOI] [PubMed] [Google Scholar]
- 67.Kordy K, et al. Contributions to human breast milk microbiome and enteromammary transfer of Bifidobacterium breve. PLoS ONE. 2020;15:e0219633. doi: 10.1371/journal.pone.0219633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Beverly RL, Underwood MA, Dallas DC. Peptidomics analysis of milk protein-derived peptides released over time in the preterm infant stomach. J. Proteome Res. 2019;18:912–922. doi: 10.1021/acs.jproteome.8b00604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Sweeney EL, et al. The effect of breastmilk and saliva combinations on the in vitro growth of oral pathogenic and commensal microorganisms. Sci. Rep. 2018;8:15112. doi: 10.1038/s41598-018-33519-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ma, A. et al. Oropharyngeal colostrum therapy reduces the incidence of ventilator-associated pneumonia in very low birth weight infants: a systematic review and meta-analysis. Pediatr. Res.10.1038/s41390-020-0854-1 (2020). [DOI] [PMC free article] [PubMed]
- 71.Meier PP, Johnson TJ, Patel AL, Rossman B. Evidence-based methods that promote human milk feeding of preterm infants: an expert review. Clin. Perinatol. 2017;44:1–22. doi: 10.1016/j.clp.2016.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Sun H, et al. A randomized controlled trial protocol comparing the feeds of fresh versus frozen mother’s own milk for preterm infants in the NICU. Trials. 2020;21:170. doi: 10.1186/s13063-019-3981-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Meier PP, Patel AL, Hoban R, Engstrom JL. Which breast pump for which mother: an evidence-based approach to individualizing breast pump technology. J. Perinatol. 2016;36:493–499. doi: 10.1038/jp.2016.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Battin DA, Marrs RP, Fleiss PM, Mishell DR., Jr. Effect of suckling on serum prolactin, luteinizing hormone, follicle-stimulating hormone, and estradiol during prolonged lactation. Obstet. Gynecol. 1985;65:785–788. [PubMed] [Google Scholar]
- 75.Pang WW, Hartmann PE. Initiation of human lactation: secretory differentiation and secretory activation. J. Mammary Gland Biol. Neoplasia. 2007;12:211–221. doi: 10.1007/s10911-007-9054-4. [DOI] [PubMed] [Google Scholar]
- 76.Greene MM, et al. Depression, anxiety, and perinatal-specific posttraumatic distress in mothers of very low birth weight infants in the neonatal intensive care unit. J. Dev. Behav. Pediatr. 2015;36:362–370. doi: 10.1097/DBP.0000000000000174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Hoban R, et al. Milk volume at 2 weeks predicts mother’s own milk feeding at neonatal intensive care unit discharge for very low birthweight infants. Breastfeed. Med. 2018;13:135–141. doi: 10.1089/bfm.2017.0159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Hoban R, et al. Human milk biomarkers of secretory activation in breast pump-dependent mothers of premature infants. Breastfeed. Med. 2018;13:352–360. doi: 10.1089/bfm.2017.0183. [DOI] [PubMed] [Google Scholar]
- 79.Dewey KG. Maternal and fetal stress are associated with impaired lactogenesis in humans. J. Nutr. 2001;131:3012S–3015S. doi: 10.1093/jn/131.11.3012S. [DOI] [PubMed] [Google Scholar]
- 80.American Academy of Pediatrics. Breastfeeding and the use of human milk. Pediatrics. 2012;129:e827–e841. doi: 10.1542/peds.2011-3552. [DOI] [PubMed] [Google Scholar]
- 81.Dereddy NR, Talati AJ, Smith A, Kudumula R, Dhanireddy R. A multipronged approach is associated with improved breast milk feeding rates in very low birth weight infants of an inner-city hospital. J. Hum. Lactation. 2015;31:43–46. doi: 10.1177/0890334414554619. [DOI] [PubMed] [Google Scholar]
- 82.Bixby C, Baker-Fox C, Deming C, Dhar V, Steele C. A multidisciplinary quality improvement approach increases breastmilk availability at discharge from the neonatal intensive care unit for the very-low-birth-weight infant. Breastfeed. Med. 2016;11:75–79. doi: 10.1089/bfm.2015.0141. [DOI] [PubMed] [Google Scholar]
- 83.Parker MG, Patel AL. Using quality improvement to increase human milk use for preterm infants. Semin. Perinatol. 2017;41:175–186. doi: 10.1053/j.semperi.2017.03.007. [DOI] [PubMed] [Google Scholar]
- 84.Sisk PM, Lovelady CA, Dillard RG, Gruber KJ, O’Shea TM. Maternal and infant characteristics associated with human milk feeding in very low birth weight infants. J. Hum. Lact. 2009;25:412–419. doi: 10.1177/0890334409340776. [DOI] [PubMed] [Google Scholar]
- 85.Howell EA, et al. Differences in morbidity and mortality rates in black, white, and Hispanic very preterm infants among New York City hospitals. JAMA Pediatr. 2018;172:269–277. doi: 10.1001/jamapediatrics.2017.4402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Boundy EO, Perrine CG, Nelson JM, Hamner HC, et al. Disparities in hospital-reported breast milk use in neonatal intensive care units ─ United States, 2015. MMWR. 2017;66:1313–1317. doi: 10.15585/mmwr.mm6648a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Li R, Perrine CG, Anstey EH. Anstey, E.H. Breastfeeding trends by race/ethnicity among US children born from 2009 to 2015. JAMA Pediatr. 2019;173:e193319. doi: 10.1001/jamapediatrics.2019.3319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Beck AF, et al. The color of health: how racism, segregation, and inequality affect the health and well-being of preterm infants and their families. Pediatr. Res. 2020;87:227–234. doi: 10.1038/s41390-019-0513-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.McGowan, E. C., Abdulla, L. S., Hawes, K. K., Tucker, R. & Vohr, B. R. Maternal immigrant status and readiness to transition to home from the NICU. Pediatrics10.1542/peds.2018-2657 (2019). [DOI] [PMC free article] [PubMed]
- 90.Singh GK, Kogan MD, Dee DL. Nativity/immigrant status, race/ethnicity, and socioeconomic determinants of breastfeeding initiation and duration in the United States, 2003. Pediatrics. 2007;119(Suppl 1):S38–S46. doi: 10.1542/peds.2006-2089G. [DOI] [PubMed] [Google Scholar]
- 91.Riley BS, et al. Barriers to human milk feeding at discharge of VLBW infants: Evaluation of neighborhood structural factors. Breastfeed. Med. 2016;11:335–342. doi: 10.1089/bfm.2015.0185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Greene MM, et al. Maternal psychological distress and visitation to the neonatal intensive care unit. Acta Paediatr. 2015;104:e306–e313. doi: 10.1111/apa.12975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Lee HJ, Ilo IT, McCollum KF, Culhane JF. Racial/ethnic differences in breastfeeding initiation and duration among low-income, inner-city mothers. Soc. Sci. Q. 2009;90:1251–1271. doi: 10.1111/j.1540-6237.2009.00656.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Lee HC, Gould JB. Factors influencing breast milk versus formula feeding at discharge for very low birth weight infants in California. J. Pediatr. 2009;155:657–662.e1−2. doi: 10.1016/j.jpeds.2009.04.064. [DOI] [PubMed] [Google Scholar]
- 95.Parker MG, et al. Addressing disparities in mother’s milk for VLBW infants through statewide quality improvement. Pediatrics. 2019;144:e20183. doi: 10.1542/peds.2018-3809. [DOI] [PubMed] [Google Scholar]
- 96.Wasser HM, et al. Who’s feeding baby? Non-maternal involvement in feeding and its association with dietary intakes among infants and toddlers. Appetite. 2013;71:7–15. doi: 10.1016/j.appet.2013.06.096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Grandmothers Tea Project. http://www.illinoisbreastfeeding.org/21401/21464.html. (2012).
- 98.DeVane-Johnson S, Woods-Giscombe C, Thoyre S, Fogel C, Williams R., 2nd Integrative literature review of factors related to breastfeeding in African American women: Evidence for a potential paradigm shift. J. Hum. Lact. 2017;33:435–447. doi: 10.1177/0890334417693209. [DOI] [PubMed] [Google Scholar]
- 99.Sublette, C. & Sublette, N. The American Slave Coast: A History of the Slave-Breeding Industry (Chicago Review Press, Chicago, IL, 2015).
- 100.Asiodu I, Flaskerud J. Got milk? A look at breastfeeding from an African American perspective. Issues Ment. Health Nurs. 2011;32:544–546. doi: 10.3109/01612840.2010.544842. [DOI] [PubMed] [Google Scholar]
- 101.Bentley ME, et al. Sources of influence on intention to breastfeed among African-American women at entry to WIC. J. Hum. Lact. 1999;15:27–34. doi: 10.1177/089033449901500109. [DOI] [PubMed] [Google Scholar]
- 102.Kim JH, Fiese BH, Donovan SM. Breastfeeding is natural but not the cultural norm: a mixed-methods study of first-time breastfeeding, African American mothers participating in WIC. J. Nutr. Educ. Behav. 2017;49:S151–S161. doi: 10.1016/j.jneb.2017.04.003. [DOI] [PubMed] [Google Scholar]
- 103.Hendershot, G. E. Trends in Breast Feeding Vol. 59 (US Department of Health, Education & Welfare, 1980).
- 104.McDowell, M. A., Wang, C.-Y. & Kennedy-Stephenson J. Breastfeeding in the United States: Findings from the National Health and Nutrition Examination Surveys 1999−2006. NCHS Data Briefs, No. 5 (National Center for Health Statistics, Hyattsville, MD, 2008). [PubMed]
- 105.Healthy People. https://www.healthypeople.gov/2020/data-search/Search-the-Data#objid=4859 (2020).
- 106.Grassley J, Eschiti V. Grandmother breastfeeding support: what do mothers need and want? Birth. 2008;35:329–335. doi: 10.1111/j.1523-536X.2008.00260.x. [DOI] [PubMed] [Google Scholar]
- 107.Semega, J. L., Fontenot, K. R. & Kollar, M. A. Income and poverty in the United States: 2016 current population reports. United States Census Bureau; U.S. Department of Commerce-Economics and Statistics Administration P60-259, 1–72 (2017).
- 108.Hedberg IC. Barriers to breastfeeding in the WIC population. MCN Am. J. Matern. Child Nurs. 2013;38:244–249. doi: 10.1097/NMC.0b013e3182836ca2. [DOI] [PubMed] [Google Scholar]
- 109.Parker, L. A., Sullivan, S., Kruger, C. & Mueller, M. Timing of milk expression following delivery in mothers delivering preterm very low birth weight infants: a randomized trial. J. Perinatol.10.1038/s41372-020-0688-z (2020). [DOI] [PubMed]
- 110.Morton J, et al. Combining hand techniques with electric pumping increases milk production in mothers of preterm infants. J. Perinatol. 2009;29:757–764. doi: 10.1038/jp.2009.87. [DOI] [PubMed] [Google Scholar]
- 111.Lussier MM, et al. Daily breastmilk volume in mothers of very low birth weight neonates: a repeated-measures randomized trial of hand expression versus electric breast pump expression. Breastfeed. Med. 2015;10:312–317. doi: 10.1089/bfm.2015.0014. [DOI] [PubMed] [Google Scholar]
- 112.Meier PP, et al. A comparison of the efficiency, efficacy, comfort, and convenience of two hospital-grade electric breast pumps for mothers of very low birthweight infants. Breastfeed. Med. 2008;3:141–150. doi: 10.1089/bfm.2007.0021. [DOI] [PubMed] [Google Scholar]
- 113.Kimbro RT. On-the-job moms: work and breastfeeding initiation and duration for a sample of low-income women. Matern. Child Health J. 2006;10:19–26. doi: 10.1007/s10995-005-0058-7. [DOI] [PubMed] [Google Scholar]
- 114.Ryan AS, Zhou W, Arensberg MB. The effect of employment status on breastfeeding in the United States. Women’s Health Issues. 2006;16:243–251. doi: 10.1016/j.whi.2006.08.001. [DOI] [PubMed] [Google Scholar]
- 115.International Labour Office. Maternity at Work: A Review of National Legislation. Findings from the ILO Database of Conditions of Work and Employment Laws (International Labour Organization, Geneva, Switzerland, 2010).
- 116.29 USC §2601 et seq.; 29 CFR Part 825.The Family and Medical Leave Act of 1993. U.S. Public Law 103-3 Enacted February 5, 1993.
- 117.Pizzella, P. & Beach, W. W. National Compensation Survey: Employee Benefits in the United States, Bulletin 2791 (U.S. Bureau of Labor Statistics, March 2019).
- 118.Hauck K, Miraldo M, Singh S. Integrating motherhood and employment: A 22-year analysis investigating impacts of US workplace breastfeeding policy. SSM Popul. Health. 2020;11:100580. doi: 10.1016/j.ssmph.2020.100580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Hurst N, Engebretson J, Mahoney JS. Providing mother’s own milk in the context of the NICU: a paradoxical experience. J. Hum. Lact. 2013;29:366–373. doi: 10.1177/0890334413485640. [DOI] [PubMed] [Google Scholar]
- 120.Miracle DJ, Meier PP, Bennett PA. Mothers’ decisions to change from formula to mothers’ milk for very-low-birth-weight infants. J. Obstet. Gynecol. Neonatal Nurs. 2004;33:692–703. doi: 10.1177/0884217504270665. [DOI] [PubMed] [Google Scholar]
- 121.Rossman B, Meier PP, Janes JE, Lawrence C, Patel AL. Human milk provision experiences, goals, and outcomes for teen mothers with low-birth-weight infants in the neonatal intensive care unit. Breastfeed. Med. 2017;12:351–358. doi: 10.1089/bfm.2017.0035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Rossman B, Greene MM, Meier PP. The role of peer support in the development of maternal identity for “NICU mom”. J. Obstet. Gynecol. Neonatal Nurs. 2015;44:3–16. doi: 10.1111/1552-6909.12527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Rossman B, Kratovil AL, Greene MM, Engstrom JL, Meier PP. “I have faith in my milk”: the meaning of milk for mothers of very low birth weight infants hospitalized in the neonatal intensive care unit. J. Hum. Lact. 2013;29:359–365. doi: 10.1177/0890334413484552. [DOI] [PubMed] [Google Scholar]
- 124.Rossman B, Engstrom JL, Meier PP. Healthcare providers’ perceptions of breastfeeding peer counselors in the neonatal intensive care unit. Res. Nurs. Health. 2012;35:460–474. doi: 10.1002/nur.21496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.American Academy of Pediatrics. Donor human milk for the high-risk infant: Preparation, safety, and usage options in the United States. Pediatrics10.1542/peds.2016-3440 (2017). [DOI] [PubMed]
- 126.World Health Organization: Media Centre: Statements. Exclusive breastfeeding for six months best for babies everywhere. http://www.who.int/mediacentre/news/statements/2011/breastfeeding_20110115/en/ (2011).
- 127.Horbar JD, et al. Racial segregation and inequality in the neonatal intensive care unit for very low-birth-weight and very preterm infants. JAMA Pediatr. 2019;173:455–461. doi: 10.1001/jamapediatrics.2019.0241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.American Academy of Pediatrics. Poverty and child health in the United States. Pediatrics. 2016;137:e20160339. doi: 10.1542/peds.2016-0339. [DOI] [PubMed] [Google Scholar]
- 129.Howell EA, Ahmed ZN. Eight steps for narrowing the maternal health disparity gap: step-by-step plan to reduce racial and ethnic disparities in care. Contemp. Ob. Gyn. 2019;64:30–36. [PMC free article] [PubMed] [Google Scholar]
- 130.Chapman DJ. Lessons learned from African American women who breastfeed. J. Hum. Lact. 2015;31:15–16. doi: 10.1177/0890334414560731. [DOI] [PubMed] [Google Scholar]
- 131.Spencer B, Wambach K, Domain EW. African American women’s breastfeeding experiences: cultural, personal, and political voices. Qual. Health Res. 2015;25:974–987. doi: 10.1177/1049732314554097. [DOI] [PubMed] [Google Scholar]
- 132.Lee HC, et al. A quality improvement project to increase breast milk use in very low birth weight infants. Pediatrics. 2012;130:e1679–e1687. doi: 10.1542/peds.2012-0547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Meier, P. P., Patel, A. L. & Janes, J. J. PROVIDE: a training compendium for providing mothers’ own milk in NICU settings. www.Lactahub.org/nicu-training (2020).
- 134.Asiodu IV, Waters CM, Dailey DE, Lyndon A. Infant feeding decision-making and the influences of social support persons among first-time African American mothers. Matern. Child Health J. 2017;21:863–872. doi: 10.1007/s10995-016-2167-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Meier PP, Engstrom JL, Rossman B. Breastfeeding peer counselors as direct lactation care providers in the neonatal intensive care unit. J. Hum. Lact. 2013;29:313–322. doi: 10.1177/0890334413482184. [DOI] [PubMed] [Google Scholar]
- 136.Rossman B, et al. “They’ve walked in my shoes”: mothers of very low birth weight infants and their experiences with breastfeeding peer counselors in the neonatal intensive care unit. J. Hum. Lact. 2011;27:14–24. doi: 10.1177/0890334410390046. [DOI] [PubMed] [Google Scholar]
- 137.FitzGerald C, Hurst S. Implicit bias in healthcare professionals: a systematic review. BMC Med. Ethics. 2017;18:19-017–0179-8. doi: 10.1186/s12910-017-0179-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Weech-Maldonado R, et al. Hospital cultural competency as a systematic organizational intervention: key findings from the national center for healthcare leadership diversity demonstration project. Health Care Manag. Rev. 2018;43:30–41. doi: 10.1097/HMR.0000000000000128. [DOI] [PubMed] [Google Scholar]
- 139.Pereda B, Montoya M. Addressing implicit bias to improve cross-cultural care. Clin. Obstet. Gynecol. 2018;61:2–9. doi: 10.1097/GRF.0000000000000341. [DOI] [PubMed] [Google Scholar]
- 140.Doetinchem, O., Xu, K. & Carrin G. Conditional Cash Transfers: What’s In It for Health? WHO Technical Briefs for Policy-Makers 1 (WHO, 2008).
- 141.Anokye N, et al. Cost-effectiveness of offering an area-level financial incentive on breast feeding: a within-cluster randomised controlled trial analysis. Arch. Dis. Child. 2020;105:155–159. doi: 10.1136/archdischild-2018-316741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Washio Y, et al. Incentive-based intervention to maintain breastfeeding among low-income Puerto Rican mothers. Pediatrics. 2017;139:e20163119. doi: 10.1542/peds.2016-3119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Relton C, et al. Effect of financial incentives on breastfeeding: a cluster randomized clinical trial. JAMA Pediatr. 2018;172:e174523. doi: 10.1001/jamapediatrics.2017.4523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Relton C, et al. Cluster randomised controlled trial of a financial incentive for mothers to improve breast feeding in areas with low breastfeeding rates: the NOSH study protocol. BMJ Open. 2016;6:e010158. doi: 10.1136/bmjopen-2015-010158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Johnson M, et al. Valuing breastfeeding: a qualitative study of women’s experiences of a financial incentive scheme for breastfeeding. BMC Pregnancy Childbirth. 2018;18:20. doi: 10.1186/s12884-017-1651-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Becker F, et al. Women’s preferences for alternative financial incentive schemes for breastfeeding: a discrete choice experiment. PLoS ONE. 2018;12:e0194231. doi: 10.1371/journal.pone.0194231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Whelan B, et al. Healthcare providers’ views on the acceptability of financial incentives for breastfeeding: a qualitative study. BMC Pregnancy Childbirth. 2014;14:355. doi: 10.1186/1471-2393-14-355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Moran VH, et al. Incentives to promote breastfeeding: a systematic review. Pediatrics. 2015;135:e687–e702. doi: 10.1542/peds.2014-2221. [DOI] [PubMed] [Google Scholar]
- 149.Thomson G, et al. Unintended consequences of incentive provision for behaviour change and maintenance around childbirth. PLoS ONE. 2014;9:e111322. doi: 10.1371/journal.pone.0111322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150. Levitt, S. D., List, J. A., Neckermann, S. & Sadoff, S. The Behavioralist Goes to School: Leveraging Behavioral Economics to Improve Educational Performance. NBER Working Paper No. 18165 (JEL NO. C9,C93,H75,I20) 1–43 (National Bureau of Economic Research 2012).
- 151.Kane RL, Johnson PE, Town RJ, Butler M. A structured review of the effect of economic incentives on consumers’ preventive behavior. Am. J. Prev. Med. 2004;27:327–352. doi: 10.1016/j.amepre.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 152.Washio Y, et al. Individual breastfeeding support with contingent incentives for low-income mothers in the USA: the ‘BOOST (Breastfeeding Onset & Onward with Support Tools)’ randomised controlled trial protocol. BMJ Open. 2020;10:e034510. doi: 10.1136/bmjopen-2019-034510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Patel, A. L. & Johnson, T. J. Reducing disparity in receipt of mother’s own milk in very low birth weight infants: an economic intervention to improve adherence to sustained maternal breast pump use (ReDiMOM). https://clinicaltrials.gov/ct2/show/NCT04540575 (2020). [DOI] [PMC free article] [PubMed]




