Abstract
(1) Background: Few antifungal drugs are currently available, and drug-resistant strains have rapidly emerged. Thus, the aim of this study is to evaluate the effectiveness of the antifungal activity from a combinational treatment of chitosan with a clinical antifungal drug on Candida albicans and Candida tropicalis. (2) Methods: Minimum inhibitory concentration (MIC) tests, checkerboard assays, and disc assays were employed to determine the inhibitory effect of chitosan with or without other antifungal drugs on C. albicans and C. tropicalis. (3) Results: Treatment with chitosan in combination with fluconazole showed a great synergistic fungicidal effect against C. albicans and C. tropicalis, but an indifferent effect on antifungal activity when challenged with chitosan-amphotericin B or chitosan-caspofungin simultaneously. Furthermore, the combination of chitosan and fluconazole was effective against drug-resistant strains. (4) Conclusions: These findings provide strong evidence that chitosan in combination with fluconazole is a promising therapy against two Candida species and its drug-resistant strains.
Keywords: Candida albicans, Candida tropicalis, chitosan, fluconazole, synergistic effect
1. Introduction
The incidence of fungal infections has increased significantly in recent decades. Current epidemiological surveys have reported that Candida species are the leading causes of nosocomial bloodstream infections, which can lead to high mortality rates in at-risk populations [1,2]. However, the issues of currently available antifungal drugs include undesirable side effects and therapeutic failure of the antifungal treatment against drug-resistant strains.
Chitosan, poly-(β-1→4)-2-amino-2-deoxy-D-glucopyranose, is a linear polysaccharide produced by the partial deacetylation of chitin [3,4,5,6,7,8]. Because of its biocompatible, biodegradable, and nontoxic properties, chitosan has been used in many biomedical and therapeutic applications [3,4,5,6,7,8]. For example, halloysite nanotubes coated by chitosan and chitosan nanoparticles have been intensively investigated, and the findings demonstrated that chitosan is a suitable drug delivery system for in vitro and in vivo treatment, thus indicating that chitosan could have promising medicinal applications [9,10,11,12,13]. Additionally, chitosan shows considerable antimicrobial activity against a variety of bacteria and fungi [5,6,7,14,15,16,17,18,19,20,21,22,23,24,25]. However, the mechanisms underlying its antimicrobial activity remain largely unclear. Chitosan has been suggested to exhibit polycationic polymers when the environmental pH is below 6.5 [17,21,23], which leads to interactions with the negatively charged bacterial or fungal cell surface, thereby causing an inhibitory effect [6,7,8,22,23,24].
Combination therapy is generally effective against pathogenic microbes that show drug resistance [26,27,28,29]. The use of chitosan as a fluconazole delivery system or a polymer film containing clinical drugs has been developed to treat infectious candidiasis [30,31]. These studies showed that the advantages of chitosan-based scaffold materials include the control of drug release and the maintenance of a high local concentration of the antibacterial or antifungal drug over a long period of time [30,31]. However, the antifungal efficacy of chitosan in combination with clinical antifungal drugs has been quantified, and the results presented contradictory conclusions [14,32]. Low-molecular-weight chitosan (LMWC; 70 kDa; > 75% deacetylation) exhibited promising anti-Candida effects at pH 4.0, whereas the combination of LMWC and fluconazole did not have a synergistic effect at neutral pH [14]. Interestingly, C32, a 15 kDa chitooligosaccharide (CHOS) with 0.15 FA (fraction of acetylation), showed great synergistic effects against Candida albicans, Candida guilliermondii, and Candida lusitaniae, but had an indifferent effect against Candida tropicalis when in combination with different antifungals [32]. These data suggest that the molecular weight (MW) and degree of deacetylation of chitosan might result in different outcomes. Nevertheless, previous studies have mainly focused on one chitosan with a low MW or oligo form. Chitosan with different MWs and degrees of deacetylation against C. albicans and C. tropicalis as well as drug-resistant strains have never been studied.
In this study, six commercial chitosans with distinct MWs and degrees of deacetylation were analyzed to evaluate their antifungal activity and synergistic effects with antifungal drugs against C. albicans SC5314 [33], C. tropicalis MYA3404 [33], and drug-resistant strains because C. albicans and C. tropicalis are the most isolated fungal pathogens in tropical and subtropical regions, including Taiwan [34,35,36]. In this study, we first determined the minimum inhibitory concentration (MIC) of chitosan, fluconazole, amphotericin B, and caspofungin. The fractional inhibitory concentration (FICindex) determined by checkerboard assays further showed great synergistic antifungal activity against two Candida species and the drug-resistant strains in liquid medium after treatment with chitosan-fluconazole, but not chitosan-amphotericin B or chitosan-caspofungin. Together, our findings will reveal new potential and promising therapeutic methods or medical applications to control Candida infections.
2. Results
2.1. Susceptibility of C. albicans SC5314 to Antifungal Drugs and Chitosan with Different MWs
Many review articles have implied that the major mechanism of chitosan against microorganisms is the targeting of the cell wall and cell membrane [4,5,6,7,17,19,22,23,24,31]. Therefore, three classes of antifungal drugs, namely, fluconazole, amphotericin B, and caspofungin, were selected for this study. The in vitro antifungal activities of fluconazole, amphotericin B, caspofungin, and chitosan with different properties were analyzed against C. albicans SC5314. As shown in Table 1, the commercial chitosans alone did not exhibit great antifungal activity because the MICs ranged from >2000 μg/mL (3 kDa chitosan oligomer and 20–35 kDa chitosan) to 1000 μg/mL (15 kDa and MMW chitosans), thus corroborating a previous report [32]. Notably, the MIC of HMW chitosan could not be determined because it can only dissolve at higher concentrations of acetic acid (giving a pH < 4.5), and the low pH profoundly inhibited the growth of C. albicans (Table 1). Thus, HMW chitosan was not analyzed in the following experiments. Similar to previous reports [37], C. albicans SC5314 was highly susceptible to fluconazole (MIC: 0.125 μg/mL), amphotericin B (MIC: 1.0 μg/mL), and caspofungin (0.25 μg/mL).
Table 1.
Minimum inhibitory concentrations (MICs) of chitosans with different MWs and deacetylation degrees in combination with antifungal drugs against C. albicans SC5314.
| Chitosan or Drug | Strain | MIC (μg/mL) |
|---|---|---|
| 3 kDa chitosan | C. albicans | >2000 |
| ~15 kDa chitosan | C. albicans | 1000 |
| 20–30 kDa chitosan | C. albicans | >2000 |
| LMW chitosan | C. albicans | 2000 |
| MMW chitosan | C. albicans | 1000 |
| HMW chitosan: | C. albicans | n.d. |
| Fluconazole | C. albicans | 0.125 |
| Amphotericin B | C. albicans | 1 |
| Caspofungin | C. albicans | 0.25 |
2.2. Chitosan Can Enhance the Antifungal Activity of Fluconazole
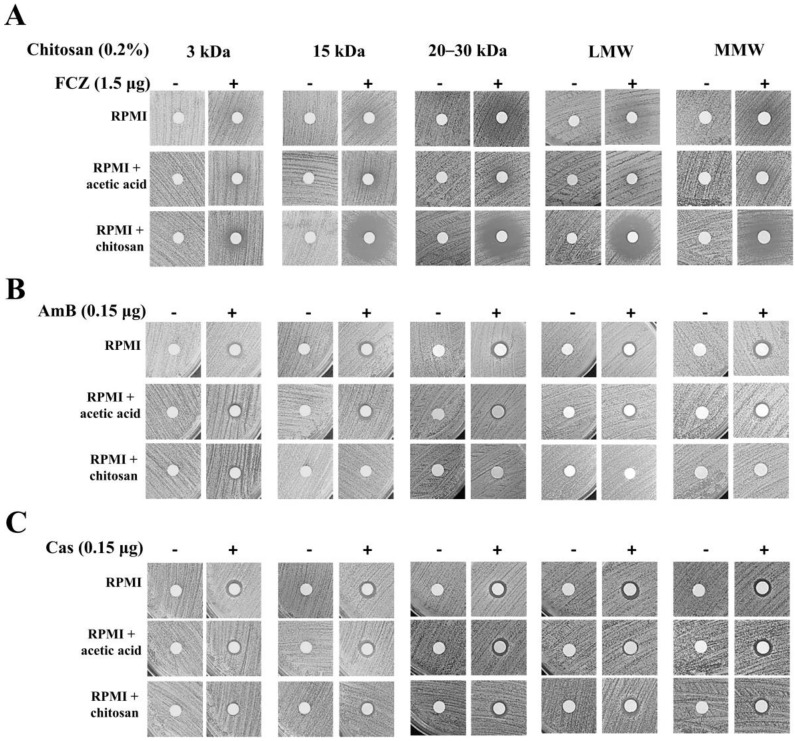
The susceptibility range of C. albicans was evaluated using three antifungal drugs (fluconazole, amphotericin B, and caspofungin) with chitosans presenting different properties (except HMW chitosan). The combination of the abovementioned antifungal drugs and chitosan showed synergistic action with fluconazole and exhibited a remarkable inhibitory effect on C. albicans SC5314. The FICindex of each sample in the chitosan-fluconazole checkerboard assay was <0.5 (Table 2). However, chitosan in combination with amphotericin B or caspofungin showed an indifferent effect, with each FICindex between 0.5 and 4.0 (Table 2). To obtain better visualization results, disk diffusion assays were utilized. We further demonstrated that the combined treatment of a particular chitosan with fluconazole exhibited great antifungal activity (Figure 1A); however, obvious inhibitory effects were not observed for the combinations of chitosan-amphotericin B (Figure 1B) and chitosan-caspofungin (Figure 1C). Notably, the 3 kDa and MMW chitosans with fluconazole had no obvious synergistic antifungal effects on C. albicans SC5314 in the disk diffusion assays (Figure 1A). Turbid haloes were observed after treatment with fluconazole alone because fluconazole is a fungistatic antifungal drug rather than a fungicidal agent [38]. These data suggest that the synergistic effects against C. albicans SC5314 are profoundly affected by the assay that was performed (MIC tests in liquid medium versus disk diffusion assays on agar medium).
Table 2.
Checkerboard assays of each chitosan in combination with an antifungal drug against C. albicans SC5314. FIC, fractional inhibitory concentration.
| Antifungal Drug | Chitosan | FICindex |
|---|---|---|
| Fluconazole | 3 kDa chitosan | 0.5 ± 0.125 |
| ~15 kDa chitosan | 0.125 ± 0.035 | |
| 20–30 kDa chitosan | 0.113 ± 0.038 | |
| LMW chitosan | 0.118 ± 0.043 | |
| MMW chitosan | 0.041 ± 0.021 | |
| Amphotericin B | 3 kDa chitosan | 1.75 ± 0.25 |
| ~15 kDa chitosan | 1.625 ± 0.625 | |
| 20–30 kDa chitosan | 1.505 ± 0.495 | |
| LMW chitosan | 1.05 ± 0.02 | |
| MMW chitosan | 1.505 ± 0.495 | |
| Caspofungin | 3 kDa chitosan | 2.515 ± 1.485 |
| ~15 kDa chitosan | 1.078 ± 0.048 | |
| 20–30 kDa chitosan | 2.505 ± 1.495 | |
| LMW chitosan | 1.03125 ±0.12 | |
| MMW chitosan | 1.578 ± 0.453 |
Figure 1.
Disk diffusion assay of each chitosan with or without an antifungal drug against C. albicans 5314. (A) Synergistic effects were observed for chitosan in combination with fluconazole (FCZ) against C. albicans SC5314, whereas indifferent effects were observed when chitosan was combined with (B) amphotericin B (AmB) and (C) caspofungin (Cas).
2.3. C. tropicalis MYA3404 Is Highly Susceptible to Chitosan and Chitosan-Fluconazole Treatment Exhibits Synergistic Effects Against C. tropicalis MYA3404
C. tropicalis was selected for this analysis because it is the second most isolated fungal pathogen in Taiwan. The MIC of fluconazole against C. tropicalis MYA3404 was 0.5 (Table 3). Interestingly, except for the 3 kDa chitosan oligomer, each chitosan exhibited a remarkable reduction in MIC (ranging from 1.56–7.81 μg/mL) (Table 3) compared with C. albicans SC5314 (Table 1). Checkerboard assays of each chitosan with fluconazole (but not with amphotericin B or caspofungin) were performed because of the indifferent effects of chitosan-amphotericin B and chitosan-caspofungin against C. albicans, as previously observed (Table 2). Similar to the results obtained for C. albicans SC5314, chitosan in combination with fluconazole had a synergistic effect against C. tropicalis MYA3404 (FICindex < 0.5) (Table 4). Additionally, the disk diffusion assays also indicated that treatment with chitosan-fluconazole exhibited a larger clear zone than treatment with chitosan or fluconazole alone, although 3 kDa and MMW chitosan did not exhibit a clear inhibition zone in the combination treatment (Figure 2).
Table 3.
MICs of chitosans of different MWs and degrees of deacetylation in combination with fluconazole against C. tropicalis MYA3404.
| Chitosan or Drug | Strain | MIC (μg/mL) |
|---|---|---|
| 3 kDa chitosan | C. tropicalis | 1000 |
| ~15 kDa chitosan | C. tropicalis | 7.81 |
| 20–30 kDa chitosan | C. tropicalis | 1.56 |
| LMW chitosan | C. tropicalis | 7.81 |
| MMW chitosan | C. tropicalis | 7.81 |
| Fluconazole | C. tropicalis | 0.5 |
Table 4.
Checkerboard assays of each chitosan in combination with fluconazole against C. tropicalis MYA3404.
| Antifungal Drug | Chitosan | FICindex |
|---|---|---|
| Fluconazole | 3 kDa chitosan | 0.375 ± 0.125 |
| ~15 kDa chitosan | 0.435 ± 0.165 | |
| 20–30 kDa chitosan | 0.21 ± 0.07 | |
| LMW chitosan | 0.39 ± 0.11 | |
| MMW chitosan | 0.42 ± 0.14 |
Figure 2.
Disk diffusion assay of each chitosan with or without fluconazole against C. tropicalis MYA3404. Different MWs of chitosan (except 3 kDa chitosan) with fluconazole exhibited great cytocidal effects on C. tropicalis MYA3404.
2.4. Combination of Chitosan and Fluconazole Showed Great Fungicidal Activity Against Drug-Resistant C. albicans and C. tropicalis Isolates
To further explore whether the chitosan-fluconazole combination treatment is able to inhibit fluconazole-resistant C. albicans and C. tropicalis isolates, checkerboard assays were performed. First, the MIC values after treatment with fluconazole (8 μg/mL for C. albicans and 512 μg/mL for C. tropicalis isolates) confirmed that these clinical isolates were fluconazole-resistant strains. Nevertheless, combination treatment exhibited a synergistic antifungal effect in both drug-resistant C. albicans (FICindex < 0.5) and drug-resistant C. tropicalis (FICindex < 0.5) and showed an excellent inhibition zone after treatment with chitosan with MWs of 15 kDa and 20–35 kDa and LMW (Table 5 and Figure 3).
Table 5.
Checkerboard assays of each chitosan in combination with fluconazole against fluconazole-resistant clinical strains.
| Drug-Resistant Strain | Chitosan | FICindex |
|---|---|---|
| C. albicans | 3 kDa chitosan | 0.375 ± 0.125 |
| ~15 kDa chitosan | 0.188 ± 0.063 | |
| 20–30 kDa chitosan | 0.208 ± 0.168 | |
| LMW chitosan | 0.16 ± 0.09 | |
| MMW chitosan | 0.085 ± 0.015 | |
| C. tropicalis | 3 kDa chitosan | 0.19 ± 0.07 |
| ~15 kDa chitosan | 0.26 ± 0.24 | |
| 20–30 kDa chitosan | 0.265 ± 0.235 | |
| LMW chitosan | 0.26 ± 0.24 | |
| MMW chitosan | 0.31 ± 0.19 |
Figure 3.
Disk diffusion assay of each chitosan with or without fluconazole against drug-resistant Candida strains. Fluconazole-resistant strains of C. albicans and C. tropicalis were significantly inhibited after treatment the combination of chitosan and fluconazole, particularly 15 kDa, 20–35 kDa, and LMW chitosan.
3. Discussion
The influence of the MW and degree of acetylation of chitosan on antimicrobial activity is diverse and has shown different outcomes [39,40,41]. In particular, lower deacetylation degrees and MWs of chitosan (between 42.5 and 135 kDa) exhibited stronger antimicrobial activity against gram-negative bacteria [41]. However, higher MW (300–400 kDa) chitosan and chitosan with a lower degree of deacetylation (but not chitooligosaccharides) had stronger activity against gram-positive bacteria [42]. A similar study indicated that HMW chitosan exhibited better antibacterial activity than chitosan oligomers [39]. These data suggested that the inhibitory effects were also dependent on the pathogen type and chitosan properties as well as the preparation method and chitin source. Indeed, our results showed that the chitosan used in this study exhibited different antifungal effects against C. albicans and C. tropicalis. The 3 kDa chitosan oligomers and HMW chitosan exhibited lower antifungal effects against Candida species. Furthermore, 15 kDa, 20 kDa, and LMW chitosan (but not 3 kDa and MMW chitosan) in combination with fluconazole in the checkerboard and disk diffusion assays showed remarkable antifungal effects.
We observed a hundred- to thousand-fold increase in chitosan susceptibility to C. tropicalis compared with C. albicans, thus implying that the cell surface properties of the two Candida species are different. Previous reports have shown that the contents of unsaturated fatty acids positively influence the membrane fluidity [43]. Moreover, the membrane fluidity of filamentous fungi has been reported to contribute to chitosan susceptibility [44]. Higher membrane fluidity tends to result in a more negative charge on the cell membrane [43,45], thus facilitating cationic chitosan binding to the cell membrane. Previous studies have shown that the cell membrane of C. tropicalis contains more polyunsaturated fatty acids than that of C. albicans, suggesting that the C. tropicalis cell membrane has a greater negative charge than the C. albicans cell membrane, although the differences are highly dependent on the analytical methods and culture conditions [46,47,48,49]. Furthermore, glucan, chitin, and mannan carbohydrates and a few proteins constitute the outer layer of the cell walls of Candida species [50,51]. Mannoproteins (protein-linked mannan) harboring phosphate groups (phosphorylated mannosyl side chains) also confer a negative charge to the fungal cell wall [50,51,52]. Previous studies have demonstrated that mannan components and the phosphomannan content on the C. tropicalis cell wall are significantly higher than those on the C. albicans cell wall [53,54], which might explain why C. tropicalis exhibited remarkably greater chitosan sensitivity than C. albicans.
The mode of action of chitosan against microbes has been investigated and reported in several review articles [3,4,6,7,8,22,24,40]. (1) Chitosan (>50 kDa or higher MW) binds on the microbial cell wall to prevent nutrients from entering the cell, alters the cell permeability, and could act as a metal chelator that inhibits microbial growth [5,6,17,22,55]. Thus, the LMW, MMW, and HMW chitosans used in this study might only target the fungal cell wall. Although the LMW, MMW, or HMW chitosan likely cannot pass through cell wall, because chitosan is a linear polysaccharide, it might be able to penetrate the cell wall and bind to the cell membrane. (2) Chitosan (<50 kDa or lower molecular weight) might also have intracellular activity, thereby affecting the molecular aspects of DNA, RNA, or protein synthesis. Indeed, reports have demonstrated that chitosan (≤50 kDa) and nano-sized particles can penetrate the bacteria cell wall and inhibit DNA transcription [4,56]. Therefore, 3 kDa, 15 kDa, or 20–30 kDa chitosan may not only present antimicrobial activity when interacting with the cell wall and cell membrane, but also present intracellular antifungal effects. Obviously, the molecular size of chitosan determines its antifungal activity intracellularly or extracellularly. The structure rather than the MW of chitosan also plays crucial roles in the location of antifungal activity.
In this study, three chitosans with specific MWs were applied in combination with fluconazole and caused great synergistic antifungal activity against C. albicans and C. tropicalis as well as drug-resistant strains with liquid and agar media. However, the combinations of chitosan-amphotericin B and chitosan-caspofungin against C. albicans showed indifferent effects. Phospholipids and ergosterol (a targeting site of amphotericin B) are important components of the Candida cell membrane [57]. The NH3+ groups of chitosan are believed to be able to bind to negatively charged plasma membranes, thus leading to changes in membrane permeabilization and inhibiting microorganisms [5,6,7,23,38,58]. Amphotericin B consists of mycosamine and macrolactone moieties that can alter the membrane ion permeability and potential on fungal cell membranes [59]. In particular, the mycosamine NH3+ of amphotericin B is a critical appendage for the binding to ergosterol [59,60,61]. Therefore, competitive inhibition likely occurs between chitosan and amphotericin B on the fungal membrane. However, the mechanisms underlying the indifferent effects of the combination of chitosan with caspofungin remain unclear.
C. albicans (~50%) and C. tropicalis (~20%) are the most frequently isolated Candida species that affect humans in Taiwan [35,62,63]. Moreover, C. tropicalis develops fluconazole resistance much more rapidly than C. albicans [64]. Indeed, more fluconazole-resistant isolates are observed for C. tropicalis (15%) than C. albicans (4%) [65]. However, currently available antifungal drugs are limited and ineffective against new and drug-resistant strains [66,67]. Our findings provide strong evidence that chitosan is a promising alternative for combination therapy against Candida species and drug-resistant strains. The main issue with this treatment is that chitosan exhibits low antimicrobial activity at neutral pH. Thus, the application of chitosan in combination with fluconazole locally for skin and mucosal infections or a chitosan-based nanoparticle as a fluconazole carrier will likely provide more beneficial effects in clinical therapy. Further in vivo animal experiments to validate the in vitro findings are necessary to provide useful guidelines to develop a better method and formulation to manage fungal pathogens.
4. Materials and Methods
4.1. Strains and Media
The C. albicans and C. tropicalis strains used in this study included the sequence SC5314 strain MYA3404 [33] and clinical isolate [68] obtained from National Taiwan University Hospital. YPD, RPMI 1640 (Roswell Park Memorial Institute 1640) and RPMI 1640 supplemented with chitosan were prepared as previously described [69]. The characteristics of each chitosan used in this study are listed below (Table 6). The ~3 kDa chitosan oligomer (>85% deacetylation; cat: OC28900) was obtained from Carbosynth Ltd., United Kingdom. The ~15 kDa chitosan sample (>85% deacetylation; cat: 21161-50) was purchased from Polysciences, Inc., Warrington, PA, USA. Chitosan (20–30 kDa, >90% deacetylation) was purchased from Shin Era Technology, Taiwan (cat: CHG-87G). Low-molecular-weight (LMW) chitosan (50–190 kDa; deacetylation 75–85%; cat: 448869), medium-molecular-weight (MMW) chitosan (deacetylation 75–85%; cat: 448877), and high-molecular-weight (HMW) chitosan (310–375 kDa; deacetylation >75%; cat: 419419) were purchased from Sigma-Aldrich Co., St. Louis, MO, USA. Chitosan must be dissolved in acetic acid before being added to the medium. The final pH of each chitosan-containing medium was 6.2~6.3. Moreover, HMW chitosan required a higher acetic acid concentration for dissolution owing to its low solubility, and the final pH of the HMW chitosan medium was 4.5.
Table 6.
Chitosans used in this study. LMW, low molecular weight; MMW, medium MW; HMW, high MW.
| Chitosan | Molecular Weight | Degree of Deacetylation |
|---|---|---|
| Chitosan oligomer | 3 kDa | minimum 85% |
| ~15 kDa chitosan | avg. 15 kDa | minimum 85% |
| 20–30 kDa chitosan | 20–30 kDa | ≥90% |
| LMW chitosan | 50–190 kDa | 75–85% |
| MMW chitosan | Not available | 75–85% |
| HMW chitosan | 310–375 kDa | >75% |
4.2. MIC and Checkerboard Assays
The MICs were determined for chitosan, fluconazole, amphotericin B, and caspofungin by broth microdilution [35,70]. The MIC was defined as the concentration of the compound that reduces the turbidity of C. albicans and C. tropicalis cells by more than 50% (fluconazole) or 90% (chitosan, amphotericin B, and caspofungin) [35,71,72]. A typical synergy checkerboard assay setup was performed using a 96-well plate. Columns 1 to 11 contained twofold serial dilutions of antifungal drug, and rows A to G contained twofold serial dilutions of chitosan. Column 12 contained a serial dilution of antifungal drug alone, and row H contained a serial dilution of chitosan alone.
To test the WT C. albicans SC5314 FICindex, a checkerboard array synergy experiment was performed in which fluconazole in concentrations of 0.0015625–4 μg/mL was combined with 3 kDa chitosan at concentrations of 62.5–4000 μg/mL, 15 kDa chitosan at concentrations of 62.5–4000 μg/mL, 20–30 kDa chitosan at concentrations of 62.5–4000 μg/mL, LMW chitosan at concentrations of 62.5–4000 μg/mL, or MMW chitosan at concentrations of 15.625–1000 μg/mL. Amphotericin B (0.0015625–4 μg/mL) and caspofungin (0.00390625–1 μg/mL) in combination with each chitosan were tested. To test the FICindex of the C. albicans drug-resistance strain, fluconazole in concentrations of 1–256 μg/mL was used and combined with each chitosan at the same concentration range.
To test the FICindex of the WT C. tropicalis MYA3404, a checkerboard array synergy experiment was performed in which fluconazole in concentrations of 0.0625–16 μg/mL was combined with 3 kDa chitosan at concentrations of 62.5–4000 μg/mL, 15 kDa chitosan at concentrations of 0.15625–10 μg/mL, 20–30 kDa chitosan at concentrations of 0.3125–20 μg/mL, LMW chitosan at concentrations of 0.15625–10 μg/mL, or MMW chitosan at concentrations of 0.0117188–7.5 μg/mL. To test the FICindex of the C. tropicalis drug-resistance strain, fluconazole in concentrations of 4–1024 μg/mL was combined with 3 kDa chitosan at concentrations of 62.5–4000 μg/mL, 15 kDa chitosan at concentrations of 0.9375–60 μg/mL, 20–30 kDa chitosan at concentrations of 0.9375–60 μg/mL, LMW chitosan at concentrations of 0.9375–60 μg/mL, or MMW chitosan at concentrations of 0.15625–10 μg/mL.
An antagonist effect was defined as an FICindex of > 4 [73]. MIC and checkerboard assays were performed with three replicates. The formulas (Equations (1), (2), and (3)) for calculating the FIC indices are listed below:
| (1) |
| (2) |
| (3) |
where A represents chitosan and B represents fluconazole, amphotericin B, or caspofungin.
4.3. Disk Diffusion Assays
For the disk diffusion test, 6 mm disks with different concentrations of fluconazole, amphotericin B, and caspofungin were used according to a previous report with slight modifications [74]. Each disk was placed on the surface of the agar with or without chitosan, the plates were incubated at 37 °C for 24 h, after which images were taken.
5. Conclusion
Fungal infections have become a serious issue over the past decade; however, the limited number of antifungal drugs and the rapid emergence of drug resistance strains might lead to incurable fungal infections. Chitosan has been extensively studied for potential applications in biomedical areas. Our investigation demonstrated that the combination of chitosan with a currently available antifungal drug shows a remarkable synergistic antifungal effect. Thus, the innovative application of chitosan should be explored in the future.
Author Contributions
Conceptualization, W.-H.L., F.-S.D., C.-J.C., and C.-H.L.; methodology, W.-H.L., and F.-S.D.; validation, W.-H.L., and F.-S.D.; formal analysis, W.-H.L., F.-S.D., and C.-H.L.; investigation, W.-H.L., F.-S.D., C.-J.C., and C.-H.L.; resources, C.-H.L.; writing, C.-H.L. C.-H.L. Conceived the study, participated in its design and coordination, and finalized the draft of the manuscript. W.-H.L., and F.-S.D. Contributed equally. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by NTU-108L7813 from the National Taiwan University and by MOST-105-2628-B-002-018-MY3 from the Ministry of Science and Technology.
Conflicts of Interest
The authors declare no conflict of interest.
Sample Availability: Samples of the compounds are not available from the authors.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Achkar J.M., Fries B.C. Candida infections of the genitourinary tract. Clin. Microbiol. Rev. 2010;23:253–273. doi: 10.1128/CMR.00076-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kullberg B.J., Arendrup M.C. Invasive candidiasis. N. Engl. J. Med. 2015;373:1445–1456. doi: 10.1056/NEJMra1315399. [DOI] [PubMed] [Google Scholar]
- 3.Azuma K., Izumi R., Osaki T., Ifuku S., Morimoto M., Saimoto H., Minami S., Okamoto Y. Chitin, chitosan, and its derivatives for wound healing: Old and new materials. J. Funct. Biomater. 2015;6:104–142. doi: 10.3390/jfb9020038. reprinted in J. Funct. Biomater.2018, 9, 38. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 4.Cheung R.C.F., Ng T.B., Wong J.H., Chan W.Y. Chitosan: An update on potential biomedical and pharmaceutical applications. Mar. Drugs. 2015;13:5156–5186. doi: 10.3390/md13085156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hosseinnejad M., Jafari S.M. Evaluation of different factors affecting antimicrobial properties of chitosan. Int. J. Biol. Macromol. 2016;85:467–475. doi: 10.1016/j.ijbiomac.2016.01.022. [DOI] [PubMed] [Google Scholar]
- 6.Kong M., Chen X., Xing K., Park H.J. Antimicrobial properties of chitosan and mode of action: A state of the art review. Int. J. Food Microbiol. 2010;144:51–63. doi: 10.1016/j.ijfoodmicro.2010.09.012. [DOI] [PubMed] [Google Scholar]
- 7.Kumar M.N.R. A review of chitin and chitosan applications. React. Funct. Polym. 2000;46:1–27. doi: 10.1016/S1381-5148(00)00038-9. [DOI] [Google Scholar]
- 8.Shahidi F., Arachchi J.K.V., Jeon Y.-J. Food applications of chitin and chitosans. Trends Food Sci. Technol. 1999;10:37–51. doi: 10.1016/S0924-2244(99)00017-5. [DOI] [Google Scholar]
- 9.Schlachet I., Halamish H.M., Sosnik A. Mixed Amphiphilic polymeric nanoparticles of chitosan, poly(vinyl alcohol) and poly(methyl methacrylate) for intranasal drug delivery: A preliminary in vivo study. Molecules. 2020;25:4496. doi: 10.3390/molecules25194496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Loiseau P.M., Pomel S., Croft S.L. Chitosan contribution to therapeutic and vaccinal approaches for the control of leishmaniasis. Molecules. 2020;25:4123. doi: 10.3390/molecules25184123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lisuzzo L., Cavallaro G., Milioto S., Lazzara G. Halloysite nanotubes coated by chitosan for the controlled release of khellin. Polymers. 2020;12:1766. doi: 10.3390/polym12081766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bertolino V., Cavallaro G., Milioto S., Lazzara G. Polysaccharides/halloysite nanotubes for smart bionanocomposite materials. Carbohydr. Polym. 2020;245:116502. doi: 10.1016/j.carbpol.2020.116502. [DOI] [PubMed] [Google Scholar]
- 13.Lisuzzo L., Cavallaro G., Milioto S., Lazzara G. Layered composite based on halloysite and natural polymers: A carrier for the pH controlled release of drugs. New J. Chem. 2019;43:10887–10893. doi: 10.1039/C9NJ02565K. [DOI] [Google Scholar]
- 14.Alburquenque C., Bucarey S.A., Cabrera G., Urzúa B., Hermosilla G., Tapia C.V. Antifungal activity of low molecular weight chitosan against clinical isolates of Candida spp. Med. Mycol. 2010;48:1018–1023. doi: 10.3109/13693786.2010.486412. [DOI] [PubMed] [Google Scholar]
- 15.Baker L.G., Specht C.A., Donlin M.J., Lodge J.K. Chitosan, the deacetylated form of chitin, is necessary for cell wall integrity in Cryptococcus neoformans. Eukaryot. Cell. 2007;6:855–867. doi: 10.1128/EC.00399-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hirano S., Nagao N. Effects of chitosan, pectic acid, lysozyme, and chitinase on the growth of several phytopathogens. Agr. Bio. Chem. 1989;53:3065–3066. [Google Scholar]
- 17.Lim S.-H., Hudson S.M. Review of Chitosan and its derivatives as antimicrobial agents and their uses as textile chemicals. J. Macromol. Sci. Part C. 2003;43:223–269. doi: 10.1081/MC-120020161. [DOI] [Google Scholar]
- 18.Lin C.-H., Chien H., Lin M.-H., Chen C.-P., Shen M., Chen C.-T. Chitosan inhibits the rehabilitation of damaged microbes induced by photodynamic inactivation. Int. J. Mol. Sci. 2018;19:2598. doi: 10.3390/ijms19092598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Martínez-Camacho A., Cortez-Rocha M.O., Ezquerra-Brauer J., Graciano-Verdugo A., Rodriguez-Félix F., Castillo-Ortega M., Yépiz-Gómez M., Plascencia-Jatomea M. Chitosan composite films: Thermal, structural, mechanical and antifungal properties. Carbohydr. Polym. 2010;82:305–315. doi: 10.1016/j.carbpol.2010.04.069. [DOI] [Google Scholar]
- 20.Panwar R., Pemmaraju S.C., Sharma A.K., Pruthi V. Efficacy of ferulic acid encapsulated chitosan nanoparticles against Candida albicans biofilm. Microb. Pathog. 2016;95:21–31. doi: 10.1016/j.micpath.2016.02.007. [DOI] [PubMed] [Google Scholar]
- 21.Peña A., Sánchez N.S., Calahorra M. Effects of chitosan on Candida albicans: Conditions for its antifungal activity. BioMed Res. Int. 2013;2013:1–15. doi: 10.1155/2013/527549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Raafat D., Von Bargen K., Haas A., Sahl H.-G. Insights into the Mode of action of chitosan as an antibacterial compound. Appl. Environ. Microbiol. 2008;74:3764–3773. doi: 10.1128/AEM.00453-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rabea E.I., Badwy M.E.-T., Stevens C.V., Smagghe A.G., Steurbaut W. Chitosan as antimicrobial agent: Applications and mode of action. Biomacromolecules. 2003;4:1457–1465. doi: 10.1021/bm034130m. [DOI] [PubMed] [Google Scholar]
- 24.Sudarshan N.R., Hoover D.G., Knorr D. Antibacterial action of chitosan. Food Biotechnol. 1992;6:257–272. doi: 10.1080/08905439209549838. [DOI] [Google Scholar]
- 25.Tsai T., Chien H.-F., Wang T.-H., Huang C.-T., Ker Y.-B., Chen C. Chitosan augments photodynamic inactivation of gram-positive and gram-negative bacteria. Antimicrob. Agents Chemother. 2011;55:1883–1890. doi: 10.1128/AAC.00550-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Huang L., Dai T., Xuan Y., Tegos G.P., Hamblin M.R. Synergistic combination of chitosan acetate with nanoparticle silver as a topical antimicrobial: Efficacy against bacterial burn infections. Antimicrob. Agents Chemother. 2011;55:3432–3438. doi: 10.1128/AAC.01803-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Breser M.L., Felipe V., Bohl L.P., Orellano M.S., Isaac P., Conesa A., Rivero V.E., Correa S.G., Bianco I.D., Porporatto C. Chitosan and cloxacillin combination improve antibiotic efficacy against different lifestyle of coagulase-negative Staphylococcus isolates from chronic bovine mastitis. Sci. Rep. 2018;8:5081. doi: 10.1038/s41598-018-23521-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yang K., Han Q., Chen B., Zheng Y., Zhang K., Li Q., Wang J. Antimicrobial hydrogels: Promising materials for medical application. Int. J. Nanomed. 2018;13:2217–2263. doi: 10.2147/IJN.S154748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Labruère R., Sona A.J., Turos E. Anti–methicillin-resistant Staphylococcus aureus nanoantibiotics. Front. Pharmacol. 2019;10:1121. doi: 10.3389/fphar.2019.01121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Darwesh B., Aldawsari H.M., Aburahma M.H. Optimized chitosan/anion polyelectrolyte complex based inserts for vaginal delivery of fluconazole: In vitro/in vivo evaluation. Pharmaceutics. 2018;10:227. doi: 10.3390/pharmaceutics10040227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fitaihi R.A., Aleanizy F.S., Elsamaligy S., Mahmoud H.A., Bayomi M.A. Role of chitosan on controlling the characteristics and antifungal activity of bioadhesive fluconazole vaginal tablets. Saudi Pharm. J. 2018;26:151–161. doi: 10.1016/j.jsps.2017.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ganan M., Lorentzen S.B., Aam B.B., Eijsink V.G.H., Gaustad P., Sørlie M. Antibiotic saving effect of combination therapy through synergistic interactions between well-characterized chito-oligosaccharides and commercial antifungals against medically relevant yeasts. PLoS ONE. 2019;14:e0227098. doi: 10.1371/journal.pone.0227098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Butler G., Rasmussen M.D., Lin M.F., Santos M.A.S., Sakthikumar S., Munro C.A., Rheinbay E., Grabherr M., Forche A., Reedy J.L., et al. Evolution of pathogenicity and sexual reproduction in eight Candida genomes. Nat. Cell Biol. 2009;459:657–662. doi: 10.1038/nature08064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Falagas M.E., Roussos N., Vardakas K.Z. Relative frequency of albicans and the various non-albicans Candida spp among candidemia isolates from inpatients in various parts of the world: A systematic review. Int. J. Infect. Dis. 2010;14:e954–e966. doi: 10.1016/j.ijid.2010.04.006. [DOI] [PubMed] [Google Scholar]
- 35.Chang T.-P., Lo P.-C., Wang A.-H., Lo H.-J., Ho M.-W., Yang Y.-L., Lin P.-S. Distribution and drug susceptibilities of Candida species causing candidemia from a medical center in central Taiwan. J. Infect. Chemother. 2013;19:1065–1071. doi: 10.1007/s10156-013-0623-8. [DOI] [PubMed] [Google Scholar]
- 36.Guinea J. Global trends in the distribution of Candida species causing candidemia. Clin. Microbiol. Infect. 2014;20:5–10. doi: 10.1111/1469-0691.12539. [DOI] [PubMed] [Google Scholar]
- 37.Nagy F., Bozó A., Toth Z., Daróczi L., Majoros L., Kovács R. In vitro antifungal susceptibility patterns of planktonic and sessile Candida kefyr clinical isolates. Med. Mycol. 2017;56:493–500. doi: 10.1093/mmy/myx062. [DOI] [PubMed] [Google Scholar]
- 38.Sheehan D.J., Hitchcock C.A., Sibley C.M. Current and emerging azole antifungal agents. Clin. Microbiol. Rev. 1999;12:40–79. doi: 10.1128/CMR.12.1.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.No H.K., Park N.Y., Lee S.H., Meyers S.P. Antibacterial activity of chitosans and chitosan oligomers with different molecular weights. Int. J. Food Microbiol. 2002;74:65–72. doi: 10.1016/S0168-1605(01)00717-6. [DOI] [PubMed] [Google Scholar]
- 40.Mellegård H., Strand S., Christensen B., Granum P.E., Hardy S.P. Antibacterial activity of chemically defined chitosans: Influence of molecular weight, degree of acetylation and test organism. Int. J. Food Microbiol. 2011;148:48–54. doi: 10.1016/j.ijfoodmicro.2011.04.023. [DOI] [PubMed] [Google Scholar]
- 41.Younes I., Sellimi S., Rinaudo M., Jellouli K., Nasri M. Influence of acetylation degree and molecular weight of homogeneous chitosans on antibacterial and antifungal activities. Int. J. Food Microbiol. 2014;185:57–63. doi: 10.1016/j.ijfoodmicro.2014.04.029. [DOI] [PubMed] [Google Scholar]
- 42.Omura Y., Shigemoto M., Akiyama T., Saimoto H., Shigemasa Y., Nakamura I., Tsuchido T. Antimicrobial activity of chitosan with different degrees of acetylation and molecular weights. Biocontrol Sci. 2003;8:25–30. doi: 10.4265/bio.8.25. [DOI] [Google Scholar]
- 43.Davey J. Bringing it all together. Nat. Cell Biol. 1989;339:591. doi: 10.1038/339591b0. [DOI] [Google Scholar]
- 44.Palma-Guerrero J., Lopez-Jimenez J.A., Pérez-Berná A.J., Huang I.-C., Jansson H.-B., Salinas J., Villalaín J., Read N.D., Lopez-Llorca L.V. Membrane fluidity determines sensitivity of filamentous fungi to chitosan. Mol. Microbiol. 2010;75:1021–1032. doi: 10.1111/j.1365-2958.2009.07039.x. [DOI] [PubMed] [Google Scholar]
- 45.Kumariya R., Sood S.K., Rajput Y.S., Saini N., Garsa A.K. Increased membrane surface positive charge and altered membrane fluidity leads to cationic antimicrobial peptide resistance in Enterococcus faecalis. Biochim. Biophys. Acta Biomembr. 2015;1848:1367–1375. doi: 10.1016/j.bbamem.2015.03.007. [DOI] [PubMed] [Google Scholar]
- 46.Schneider H., Fuhrmann G.F., Fiechter A. Plasma membrane from Candida tropicalis grown on glucose or hexadecane. II. Biochemical properties and substrate-induced alterations. Biochim. Biophys. Acta Biomembr. 1979;554:309–322. doi: 10.1016/0005-2736(79)90372-9. [DOI] [PubMed] [Google Scholar]
- 47.Yano K., Yamada T., Banno Y., Sekiya T., Nozawa Y. Modification of lipid composition in a dimorphic fungus, Candida albicans during the yeast cell to hypha transformation. Jpn. J. Med. Mycol. 1982;23:159–165. doi: 10.3314/jjmm1960.23.159. [DOI] [Google Scholar]
- 48.Ghannoum M.A., Janini G., Khamis L., Radwan S.S. Dimorphism-associated variations in the lipid composition of Candida albicans. Microbiology. 1986;132:2367–2375. doi: 10.1099/00221287-132-8-2367. [DOI] [PubMed] [Google Scholar]
- 49.Tylicki A., Siemieniuk M., Dobrzyn P., Ziolkowska G., Nowik M., Czyzewska U., Pyrkowska A. Fatty acid profile and influence of oxythiamine on fatty acid content in Malassezia pachydermatis, Candida albicans and Saccharomyces cerevisiae. Mycoses. 2011;55:e106–e113. doi: 10.1111/j.1439-0507.2011.02152.x. [DOI] [PubMed] [Google Scholar]
- 50.Chaffin W.L. Candida albicans cell wall proteins. Microbiol. Mol. Biol. Rev. 2008;72:495–544. doi: 10.1128/MMBR.00032-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gow N.A.R., Latge J.-P., Munro C.A. The fungal cell wall: Structure, biosynthesis, and function. The Fungal Kingdom. 2017;5:267–292. doi: 10.1128/microbiolspec.funk-0035-2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hall R.A., Gow N.A.R. Mannosylation in Candida albicans: Role in cell wall function and immune recognition. Mol. Microbiol. 2013;90:1147–1161. doi: 10.1111/mmi.12426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Walker L.A., Munro C.A. Caspofungin induced cell wall changes of Candida species influences macrophage interactions. Front. Cell. Infect. Microbiol. 2020;10:164. doi: 10.3389/fcimb.2020.00164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Navarro-Arias M.J., Hernández-Chávez M.J., Garcia-Carnero L.C., Amezcua-Hernández D.G., E Lozoya-Pérez N., Estrada-Mata E., Martínez-Duncker I., Franco B., Mora-Montes H.M. Differential recognition of Candida tropicalis, Candida guilliermondii, Candida krusei, and Candida auris by human innate immune cells. Infect. Drug Resist. 2019;12:783–794. doi: 10.2147/IDR.S197531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Verlee A., Mincke S., Stevens C.V. Recent developments in antibacterial and antifungal chitosan and its derivatives. Carbohydr. Polym. 2017;164:268–283. doi: 10.1016/j.carbpol.2017.02.001. [DOI] [PubMed] [Google Scholar]
- 56.Kravanja G., Primožič M., Knez Ž., Leitgeb M. Chitosan-based (nano)materials for novel biomedical applications. Molecules. 2019;24:1960. doi: 10.3390/molecules24101960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Noor A., Preuss C.V. Stat Pearls. Publishing Treasure; Island, FL, USA: 2020. Amphotericin B. [Google Scholar]
- 58.Zakrzewska A., Boorsma A., Brul S., Hellingwerf K.J., Klis F.M. Transcriptional response of Saccharomyces cerevisiae to the plasma membrane-perturbing compound chitosan. Eukaryot. Cell. 2005;4:703–715. doi: 10.1128/EC.4.4.703-715.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Matsumori N., Sawada Y., Murata M. Mycosamine orientation of amphotericin B controlling interaction with ergosterol: Sterol-dependent activity of conformation-restricted derivatives with an amino-carbonyl bridge. J. Am. Chem. Soc. 2005;127:10667–10675. doi: 10.1021/ja051597r. [DOI] [PubMed] [Google Scholar]
- 60.Gray K.C., Palacios D.S., Dailey I., Endo M.M., Uno B.E., Wilcock B.C., Burke M.D. Amphotericin primarily kills yeast by simply binding ergosterol. Proc. Natl. Acad. Sci. USA. 2012;109:2234–2239. doi: 10.1073/pnas.1117280109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Palacios D.S., Dailey I., Siebert D.M., Wilcock B.C., Burke M.D. Synthesis-enabled functional group deletions reveal key underpinnings of amphotericin B ion channel and antifungal activities. Proc. Natl. Acad. Sci. 2011;108:6733–6738. doi: 10.1073/pnas.1015023108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Chen P.-Y., Chuang Y.-C., Wang J.-T., Sheng W.-H., Yu C.-J., Chu C.-C., Hsueh P.-R., Chen Y.-C., Chen Y.-C. Comparison of epidemiology and treatment outcome of patients with candidemia at a teaching hospital in Northern Taiwan, in 2002 and 2010. J. Microbiol. Immunol. Infect. 2014;47:95–103. doi: 10.1016/j.jmii.2012.08.025. [DOI] [PubMed] [Google Scholar]
- 63.Chuang Y.-C., Chen Y.-C., Chen Y.-C., Sun C.-C., Chang Y.-Y., Chen M.-L., Hsu L.-Y., Wang J.-L. Secular trends of healthcare-associated infections at a teaching hospital in Taiwan, 1981–2007. J. Hosp. Infect. 2010;76:143–149. doi: 10.1016/j.jhin.2010.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Barchiesi F., Calabrese D., Sanglard D., Di Francesco L.F., Caselli F., Giannini D., Giacometti A., Gavaudan S., Scalise G. Experimental induction of fluconazole resistance in Candida tropicalis ATCC 750. Antimicrob. Agents Chemother. 2000;44:1578–1584. doi: 10.1128/AAC.44.6.1578-1584.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Yang Y.-L., Ho Y.-A., Cheng H.-H., Ho M., Lo H.-J. Susceptibilities of Candida species to amphotericin B and fluconazole: The emergence of fluconazole resistance in Candida tropicalis. Infect. Control. Hosp. Epidemiol. 2004;25:60–64. doi: 10.1086/502294. [DOI] [PubMed] [Google Scholar]
- 66.Ford C.B., Funt J.M., Abbey D., Issi L., Guiducci C., A Martinez D., DeLorey T., Li B.Y., White T.C., Cuomo C.A., et al. The evolution of drug resistance in clinical isolates of Candida albicans. eLife. 2015;4:e00662. doi: 10.7554/eLife.00662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.McManus B.A., Coleman D.C. Molecular epidemiology, phylogeny and evolution of Candida albicans. Infect. Genet. Evol. 2014;21:166–178. doi: 10.1016/j.meegid.2013.11.008. [DOI] [PubMed] [Google Scholar]
- 68.Chien H.-F., Chen C.-P., Chen Y.-C., Chang P.-H., Tsai T., Chen C. The use of chitosan to enhance photodynamic inactivation against Candida albicans and its drug-resistant clinical isolates. Int. J. Mol. Sci. 2013;14:7445–7456. doi: 10.3390/ijms14047445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Shih P.-Y., Liao Y.-T., Tseng Y.-K., Deng F.-S., Lin C.-H. A potential antifungal effect of chitosan against Candida albicans is mediated via the inhibition of SAGA complex component expression and the subsequent alteration of cell surface integrity. Front. Microbiol. 2019;10:602. doi: 10.3389/fmicb.2019.00602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Clinical Laboratory Standard Institute . Reference Method for Broth Dilution Antifungal Susceptibility Testing of Yeasts; Approved Standard-Third Edition. Clinical Laboratory Standard Institute; Wayne, PA, USA: 2008. CLSI document M27-A3. [Google Scholar]
- 71.Ing L.Y., Zin N.M., Sarwar A., Katas H. Antifungal activity of chitosan nanoparticles and correlation with their physical properties. Int. J. Biomater. 2012;2012:1–9. doi: 10.1155/2012/632698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ahmed F., Soliman F.M., Adly M.A., Soliman H.A., El-Matbouli M., Saleh M. In vitro assessment of the antimicrobial efficacy of chitosan nanoparticles against major fish pathogens and their cytotoxicity to fish cell lines. J. Fish Dis. 2020;43:1049–1063. doi: 10.1111/jfd.13212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.White R.L., Burgess D.S., Manduru M., A Bosso J. Comparison of three different in vitro methods of detecting synergy: Time-kill, checkerboard, and E test. Antimicrob. Agents Chemother. 1996;40:1914–1918. doi: 10.1128/AAC.40.8.1914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Bonev B., Hooper J., Parisot J. Principles of assessing bacterial susceptibility to antibiotics using the agar diffusion method. J. Antimicrob. Chemother. 2008;61:1295–1301. doi: 10.1093/jac/dkn090. [DOI] [PubMed] [Google Scholar]