Abstract
Calcific aortic valve stenosis (CAVS), the most common heart valve disease, is characterized by the slow progressive fibro-calcific remodeling of the valve leaflets, leading to progressive obstruction to the blood flow. CAVS is an increasing health care burden and the development of an effective medical treatment is a major medical need. To date, no effective pharmacological therapies have proven to halt or delay its progression to the severe symptomatic stage and aortic valve replacement represents the only available option to improve clinical outcomes and to increase survival. In the present report, the current knowledge and latest advances in the medical management of patients with CAVS are summarized, placing emphasis on lipid-lowering agents, vasoactive drugs, and anti-calcific treatments. In addition, novel potential therapeutic targets recently identified and currently under investigation are reported.
Keywords: aortic valve, stenosis, calcification, valvular interstitial cells, calcific aortic valve disease
1. Introduction
Calcific aortic valve stenosis (CAVS) is the most common heart valve disease in the Western World and the third cause of cardiovascular disease after coronary artery disease and systemic arterial hypertension [1]. The prevalence increases with advancing age, reaching 12% in the elderly (>75 years) [2,3]. Its prevalence and impact on public health are expected to increase due to higher life expectancy and the rapid aging of populations worldwide [4]. The disease remains asymptomatic until it reaches the severe stage, where it manifests with syncope, angina, and heart failure, and requires the substitution of the valve [5].
To date, there are no effective medical therapies to halt or delay CAVS progression and the only available option to treat subjects with symptomatic severe CAVS remains surgical or transcatheter aortic valve replacement (AVR) with a mechanical or bioprosthetic valve. However, the two techniques are associated with significant complications: the implantation of a mechanical valve increases the risk of thrombosis and requires a life-long anticoagulation therapy. On the other hand, the bioprosthetic valves are subject to deterioration, which limits their durability and can lead to reoperation in less than 15 years [6]. The development of an effective medical treatment is a major medical need in order to reverse the progression of CAVS, to improve clinical outcomes, and to reduce the need for AVR.
2. Methods
The PubMed, Scopus, and Google Scholar databases were searched by using the key terms “calcific aortic valve disease”, “aortic valve stenosis”, and “valvular interstitial cells”, selecting the most relevant articles. The clinical trials were searched in the clinicaltrial.gov database by selecting “aortic valve stenosis” as the disease. In addition, the proposed treatments were searched in databases associated with the key terms “aortic stenosis”, “vascular calcification”, and “atherosclerosis”. Reference lists from these papers were then searched to identify previous studies. This review focuses on patients with a tricuspid aortic valve, except when otherwise specified.
3. Pathophysiology of CAVS
CAVS is the slowly progressive fibro-calcific remodeling of the valve leaflets, resulting in reduced mobility, gradual narrowing of the valve, and progressive obstruction to the blood flow. Traditionally, it was considered an age-related degenerative process caused by passive calcium deposition in the valve. Nowadays, its pathophysiology has been further investigated and its disease progression has been related to active processes involving cellular and molecular pathways.
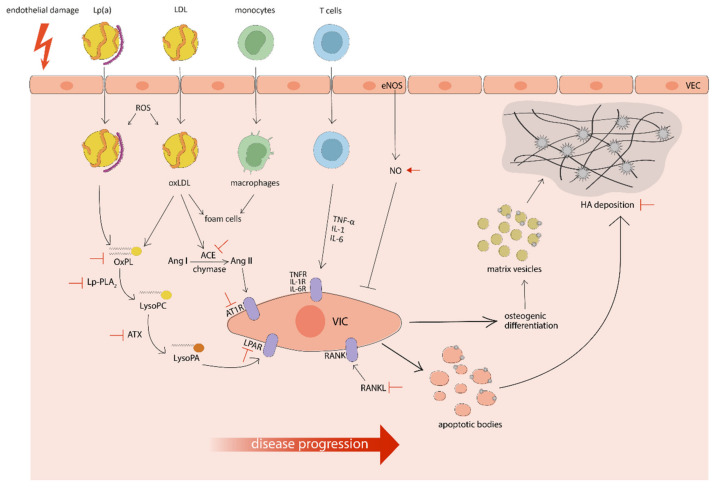
CAVS is a multi-step disease that can be divided in two distinct phases: an early initiation phase and a later propagation phase, each characterized by different mechanisms. The initiation phase, termed aortic sclerosis, shows similarities with atherosclerosis and both conditions share common risk factors (age, male gender, smoking, hypertension, dyslipidemia, metabolic syndrome) [7]. The initiating event is represented by an endothelial damage on the aortic side of the valve, due to increased mechanical stress and reduced shear stress. The loss of endothelial integrity facilitates the infiltration of monocytes, mast cells, T cells, and lipoproteins (such as low density lipoprotein (LDL), lipoprotein(a)), promoting inflammation and lipid accumulation [8]. Once in the subendothelium, monocytes are activated to macrophages, T cells release pro-inflammatory cytokines (interleukin (IL)-1, IL-6, tumor necrosis factor (TNF)-α) and LDL undergo oxidation to oxidized LDL (oxLDL), which are recognized by macrophage scavenger receptors and give rise to foam cells. These processes induce further oxidative stress and inflammatory response. Although inflammation and lipid deposition may be important in establishing the disease, their role becomes less prominent in the propagation phase, which is mainly characterized by fibrosis and calcification [9].
Valvular interstitial cells (VICs) distributed throughout the three extracellular matrix (ECM) layers are the predominant population of cells in the aortic valve (AV) and play a role in the progression of CAVS [10]. The tissue is surrounded by a monolayer of valvular endothelial cells (VECs), which also seem to be involved in disease development [11]. Physiologically, VICs are in a quiescent state, but they can be activated by transforming growth factor β (TGF-β) and pro-inflammatory cytokines to a myofibroblast-like phenotype [12]. The activation of VICs leads to an increased production and deposition of the ECM components, in particular collagen fibers. The excessive accumulation of disorganized collagen fibers results in fibrotic remodeling of the tissue, increasing the stiffness of the leaflets [1]. In this phase, VICs can also undergo apoptosis, releasing apoptotic bodies that act as nucleation sites for microcalcification [13]. Another important process of the propagation phase is valvular calcification, promoted by two different mechanisms: dystrophic calcification and biomineralization. The first process consists of a passive deposition of amorphous hydroxyapatite (HA) crystals, composed of calcium and phosphate ions, on apoptotic bodies and in the degraded ECM. The second process is similar to skeletal bone formation and is driven by the osteogenic differentiation of VICs, promoted by several signaling pathways including RANK/RANKL [14], ENPP1 [15], and Wnt/β-catenin [16]. The osteoblast-like phenotype, characterized by increased expression of osteogenic markers (such as RUNX2, BMPs, osteocalcin, osteopontin, and bone sialoprotein) [17], can release phosphate- and calcium-rich matrix vesicles, which progressively aggregate and act as scaffolds for HA crystals deposition [18]. In addition, these vesicles contain ectonucleotidases, which generate inorganic phosphate ions from endogenous sources promoting further formation of HA crystals. Concurrent dystrophic calcification and biomineralization result in massive deposition of bone-like minerals in the valvular ECM [19] (see Figure 1).
Figure 1.
A simplified schematic representation of the pathophysiology of calcific aortic valve stenosis with targets under investigation for medical treatments and potential interventions (in red). The regular arrow means “activation”, the T-shaped arrow stands for “inhibition”.
4. Purpose
The development of an effective pharmacological treatment for CAVS is an urgent medical need, considering the prevalence of the disease and the current lack of medical therapies. Several preclinical studies and clinical trials have been performed in recent years to assess the potential beneficial effects of medical treatments. The present review summarizes the current knowledge and latest advances in the medical management of patients with CAVS, placing emphasis on the drug classes with the most relevant and recent preclinical and clinical data, including lipid-lowering interventions, vasoactive drugs, and anti-calcific agents. In addition, the physiopathology of CAVS has been deepened in recent years and several novel targets have been discovered. Among them, the present review reports the targets with preclinical evidence for the development of innovative therapeutic approaches.
5. Lipid-Lowering Interventions
5.1. Statins
5.1.1. Current Evidence
Statins are 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase inhibitors that reduce the hepatic synthesis of cholesterol, lowering its intracellular levels. In response to the reduction in intracellular cholesterol, LDL receptor (LDL-R) expression increases on hepatocytes, enhancing LDL uptake and decreasing LDL cholesterol (LDL-C) plasma levels. Statins are prescribed in the primary and secondary prevention of atherosclerotic disease, where their effectiveness and established benefits are attributed to pleiotropic effects such as anti-inflammatory response, improved endothelial function, and increased plaque stability [20]. For the similarities in the pathophysiology of atherosclerosis and CAVS, pharmacological strategies effective in atherosclerosis might also modulate CAVS progression.
Statins have been shown to prevent osteogenic differentiation and to reduce calcium deposition in cultured human VICs [21]. In addition, atorvastatin administration reduces AV calcification and expression of osteogenic markers in an animal model of CAVS [22].
Several retrospective studies, involving patients with various severity of CAVS, associated statin treatment with slower progression of CAVS [23,24]. These first encouraging results were confirmed by the RAAVE trial, a prospective nonrandomized study that showed the beneficial effects of statin therapy for patients with asymptomatic moderate to severe CAVS, providing rationale for multiple trials [25]. Unfortunately, none of the randomized controlled trials (SALTIRE, TASS, ASTRONOMER, PROCAS) supported the hypothesis that statin treatment would reduce the progression of CAVS [26,27,28,29]. In the SEAS trial, a long-term co-administration of simvastatin and ezetimibe did not halt CAVS progression or the risk of associated cardiovascular (CV) events [30]. TASS, PROCAS, and SALTIRE might have been too small (less than 200 patients) and with too short follow-up (2 years) for conclusive results. On the other hand, SEAS and ASTRONOMER, larger trials with longer follow-up (4 years) and enrolling of patients (respectively, 1873 and 269) with various severity of CAVS, were powered enough to obtain significant results but they did not detect any treatment effects [31]. A meta-analysis of the above-reported clinical trials concluded that the protective effect of statins in CAVS patients was detected by low-quality (retrospective or nonrandomized) studies, but it was not confirmed by high-quality (prospective or randomized) studies, where the treatment failed to show any significant improvement in clinical outcomes [32]. More recently, a post hoc analysis of three large-scale clinical trials (TNT, IDEAL, and SPARCL) has observed that high-dose atorvastatin treatment for patients without known CAVS does not reduce the incidence of clinical disease compared with low-dose statin or placebo [33]. Taken together, clinical data have clearly shown the lack of efficacy of a lipid-lowering therapy with statins in halting disease progression or preventing the onset. As a consequence of the negative findings, the prescription of statins is not recommended for the treatment or prevention of CAVS in the American and European guidelines [34,35].
5.1.2. Future Perspectives
Recently, a secondary analysis of the SEAS trial has correlated simvastatin–ezetimibe treatment with slower disease progression and reduced need for AVR only in patients with mild CAVS and high pre-treatment LDL cholesterol levels [36], suggesting the conditions for an effective lipid-lowering therapy. It is possible that previous findings failed to show beneficial effects due to the enrolment of patients with well-established CAVS, in whom the disease was too advanced or the atherosclerotic-like process was not the central mechanism of disease progression. Moreover, an in vitro study detected a pro-calcific effect of statins if administered in differentiated VICs, further supporting the hypothesis that the efficacy of the treatment is dependent on the stage of CAVS [37].
As suggested by a recent systematic review, large and high-quality trials should first of all identify patients at high risk for developing CAVS and then, investigate whether early statin treatment can prevent disease progression in these subjects [38]. Currently, the BICATOR trial (NCT02679261) is investigating whether atorvastatin is effective in reducing CAVS progression in patients with bicuspid AV and moderate valve dysfunction [39]. If successful, it could provide a rationale in the use of statins for the prevention of CAVS or the treatment of AV sclerosis.
5.2. Lp(a)-Lowering Therapies
5.2.1. Current Evidence
Lipoprotein(a) (Lp(a)) is a cholesterol-rich particle composed of an LDL-like moiety and an apolipoprotein(a) (apo(a)) covalently bound to an apolipoprotein B-100 (apo-B100) through a disulfide bond. Lp(a) acts as atherogenic and prothrombotic lipoprotein but the mechanisms responsible for its pathogenicity are poorly understood. Probably, as an LDL-like particle, Lp(a) secreted in circulation can infiltrate the endothelium and accumulate in arterial and AV subendothelium, where it is recognized by LDL-R and provides a substrate for inflammation and lipid peroxidation [40].
In recent years, the association between Lp(a) and CAVS development has been deeply assessed in several experimental and clinical studies. Lp(a) and its associated pro-inflammatory molecules, including apo(a), oxidized phospholipids (oxPLs), and autotaxin (ATX), are overexpressed in the plasma and AV leaflets of patients with mild to moderate CAVS [41]. A treatment with Lp(a) has been shown to induce VICs osteogenic differentiation, apoptosis, calcium deposition, and ROS production, demonstrating in vitro the causal relationship between Lp(a) and CAVS development [42].
Plasma Lp(a) concentration is primarily (more than 90%) genetically determined by variation in the LPA locus, which encodes the apo(a) component of Lp(a) in the hepatocytes. In particular, the two single nucleotide polymorphisms (rs10455872 and rs3798220) responsible for genetically increased Lp(a) levels have been strongly associated with AV calcification, risk of coronary artery disease, and clinical CAVS, reaching genome-wide significance [43,44]. Very recently, Lp(a) levels have been correlated to AV microcalcification in patients without known CAVS and it has been proposed to measure this parameter in subjects with high Lp(a) levels to detect early events of CAVS before the onset of clinically manifested disease [45]. Furthermore, Lp(a) levels have been linearly associated with faster CAVS progression and increased need for AVR in patients with pre-existing mild to moderate CAVS [46] and in elderly patients with advanced CAVS [42], providing stronger rationale for targeting Lp(a). Taken together, these findings support the need to measure plasma Lp(a) concentration for identifying subjects at higher risk for CAVS and in CAVS patients for surveillance of progression, as suggested by several guidelines [47,48]. The measurement of Lp(a) or genetic diagnosis should be done to better define subjects who are more likely to benefit from specific Lp(a)-lowering drugs.
There is a lack of pharmacological agents that specifically lower Lp(a) levels. Statin treatment does not lower plasma Lp(a) concentrations and might even raise them [49]. A non-specific Lp(a)-lowering treatment is niacin, which has been associated to a significant mean Lp(a) reduction of about 23% in a meta-analysis of randomized trials [50]. Despite its established effectiveness in lowering lipid levels, treatment with extended-release niacin has failed to show any clinical benefit in patients with atherosclerosis and background statin therapy, while it increases the frequency of serious adverse effects [51,52]. Thus, niacin therapy is not considered the optimal Lp(a)-lowering therapy and is not recommended by the latest guidelines [47].
A more specific approach to target Lp(a) is the RNA-targeted therapy, which employs small interfering RNA (siRNA) and antisense oligonucleotides (ASOs) to halt Lp(a) hepatic synthesis. In recent years, three ASOs targeting hepatic LPA RNA have been developed to specifically reduce apo(a) production and Lp(a) assembly: ISIS-APO(a)Rx, IONIS-APO(a)-LRx, and AKCEA-APO(a)-LRx. In recent preclinical and clinical studies, they have been shown to lower human Lp(a) and apo(a) levels in a selective, potent, and dose-dependent manner, suggesting a novel effective, tolerable, and specific Lp(a)-lowering therapy [53].
The precise mechanism by which Lp(a) promotes CAVS progression is still poorly defined but there is growing evidence that its effect is determined by the ability to deliver oxPLs to the AV [54]. OxPLs on Lp(a) are present in the lipid phase of Lp(a) as well as covalently bound to apo-B100 and apo(a) [55]. Elevated plasma levels of oxPLs have been correlated to the presence and progression of atherosclerosis, higher risk of CV events, and increased incidence of stroke, providing strong evidence that oxPLs are major contributors to the pathogenicity of Lp(a) [56]. In addition, high oxPLs levels have been strongly associated with faster CAVS progression and more frequent need for AVR in patients with pre-existing CAVS [57]. Taken together, these data confirm the hypothesis that Lp(a) mediates pro-calcific and pro-inflammatory responses in CAVS through its oxPLs content. OxPLs play an important role in the uptake of lipoproteins by macrophages: in particular, macrophage scavenger receptors recognize the phosphocholine headgroup of oxidized but not native phospholipids. This epitope is also specifically recognized by the IgM monoclonal antibody E06, which inhibits osteogenic differentiation of VICs [42]. In vivo, its expression has been correlated with reduced atherosclerotic development and decreased AV calcification [58], providing an effective possibility to reduce the pro-inflammatory potential of oxPLs. These preliminary data suggest that novel therapies targeting oxPLs may be useful in slowing CAVS progression, but more preclinical research is needed to test this hypothesis.
OxPLs on Lp(a) can be hydrolyzed into oxidized free fatty acid and lysophosphatidylcholine (LysoPC), a strong pro-inflammatory molecule that promotes osteoblastic differentiation of human VICs [59]. LysoPC can be further hydrolyzed in lysophosphatidic acid (LysoPA) by ATX, a lysophospholipase D that is transported in the AV by apo(a) or apoB of Lp(a) and is also secreted by VICs [60]. There is recent evidence of LysoPA and ATX involvement in the pathogenesis of CAVS. ATX, overexpressed in stenotic AVs and more enzymatically active in patients with CAVS, can be a predictor of the disease [61]. LysoPA, generated by ATX, has been shown to promote the osteogenic differentiation of cultured VICs and to favor the development of CAVS in a mouse model [60]. LysoPA/ATX signaling axis could represent a novel target and may be halted at different levels through ATX inhibitors or by blocking the LysoPA-induced pathway. The first-in-class ATX inhibitor GLPG1690 has displayed safety, tolerability, and good pharmacokinetic profile in healthy subjects [62] and preliminary efficacy in patients with idiopathic pulmonary fibrosis [63], but its safety and efficacy have not been assessed in patients with CV diseases. LysoPA seems to exert pro-calcific effects by binding on VICs’ surfaces to its receptor LPAR1, overexpressed in stenotic AVs, which activates the NF-κB/IL-6/BMP-2 pathway [64]. Pharmacological blockade of LPAR1 with the receptor antagonist Ki16425 prevents the LysoPA-mediated mineralization of cultured VICs [60] and platelet-induced mineralization of the AV in a mouse model [65]. Taken together, these data suggest that blocking LPAR1 could represent a novel strategy for CAVS that warrants further research.
The enzyme responsible for the hydrolysis of oxPLs into LysoPC is the lipoprotein-associated phospholipase A2 (Lp-PLA2), carried in the plasma by LDL and Lp(a) and increased in stenotic AVs [59]. Increased Lp-PLA2 activity has been correlated to faster progression of CAVS in patients with mild CAVS, providing evidence for Lp-PLA2 involvement in the early development of the disease and a rationale for randomized trials targeting Lp-PLA2 activity [66]. The inhibition of Lp-PLA2 with darapladib might be a valuable approach for patients in early stages of CAVS. Darapladib has proven to slow the development of atherosclerosis in animal models [67], but its anti-atherogenic effect has not been confirmed in randomized trials [68]. Although the pathophysiological processes of atherosclerosis are similar to CAVS, these findings cannot be directly transposed and proper investigations on CAVS patients are required to assess whether Lp-PLA2 inhibition could be considered a novel therapeutic strategy for CAVS.
5.2.2. Future Perspectives
Several different strategies for reducing Lp(a) levels have been detected and could be further investigated, including the targeting of LPA, oxPLs, ATX, LPAR1, and Lp-PLA2. Even the PCSK9-lowering strategies could be used to reduce Lp(a) levels. However, it remains unclear whether the lowering of Lp(a) can reduce the risk of developing CAVS and improve CV outcomes in subjects with elevated plasma Lp(a) concentration. Thus, future trials should focus on this fundamental aspect.
Currently, the ongoing EAVaLL trial (NCT02109614) is investigating whether a treatment with extended-release niacin in patients with mild CAVS and elevated Lp(a) could lower plasma Lp(a) levels and slow disease progression [69] (see Table 1). If successful, this study could be the first step for trials with other Lp(a)-lowering treatments. A more specific approach for lowering Lp(a) levels is now in development: AMG890, a first-in-class candidate siRNA which targets LPA RNA. Its safety, tolerability, and efficacy are now being assessed in a phase I trial (NCT03626662) involving healthy volunteers with elevated levels of Lp(a) [70] and in a phase II trial (NCT04270760) in patients with atherosclerotic CV disease [71].
Table 1.
Ongoing clinical trials involving patients with calcific aortic valve stenosis (CAVS).
| Trial Name | NCT | Treatment | Phase | Population | Enrolment (No. of Patients) | Primary Outcome |
|---|---|---|---|---|---|---|
| EAVaLL | NCT02109614 | Extended-release niacin vs. placebo | I | Aortic sclerosis or mild CAVS | 238 | Calcium score progression measured by cardiac CT at 2 years |
| NCT03051360 | PCSK9 inhibitor vs. placebo | II | Mild to moderate CAVS | 140 | Calcium score progression measured by cardiac CT and by NaF PET at 2 years | |
| NCT02481258 | Ataciguat vs. placebo | II | Moderate CAVS | 35 | Changes in AV calcium levels at 6 months | |
| SALTIRE II | NCT02132026 | Alendronate/denosumab vs. placebo | II | Peak aortic jet velocity >2.5 m/s and grade 2–4 calcification of the AV on echocardiography | 150 | Change in AV calcium score at 6 months and 2 years |
| AVADEC | NCT03243890 | Menaquinone-7 vs. placebo | - | AV calcification score above 300, but without clinical CAVS | 389 | Change in AV calcification at 2 years |
| BASIK2 | NCT02917525 | Vitamin K2 vs. placebo | II | Bicuspid AV and mild to moderate CAVS on prior echocardiography | 44 | Change in AV calcium metabolism measured by NaF PET at 6 months |
5.3. PCSK9 Inhibitors
5.3.1. Current Evidence
Proprotein convertase subtilisin/kexin type 9 (PCSK9) is a circulating plasma protein primarily produced and secreted by the liver that promotes LDL-R lysosomal degradation, decreasing its density on hepatocytes’ surfaces. LDL-R is responsible for the internalization of LDL and Lp(a) and its depletion increases plasma levels of these lipoproteins. An increase in PCSK9 plasma levels, due to mutations in the PCSK9 gene and to pathophysiological determinants [72], causes dyslipidemia and hypercholesterolemia, risk factors for the development of CV diseases [73]. The correlation between PCSK9 levels and CAVS has been investigated in recent years: a cross sectional study has detected an increase in plasma PCSK9 concentration in patients with CAVS, in particular in the early stage, finding a correlation between circulating PCSK9 levels and the presence but not severity of the disease [74]. PCSK9, infiltrated from the blood stream and locally secreted by VICs, is significantly increased in human calcified AVs, where it correlates positively with the extent of calcification [75]; conversely, PCSK9 deficiency reduces the calcification potential [76]. These recent studies have found a direct effect of PCSK9 on the development and progression of CAVS, providing a rationale for a therapeutic strategy based on its inhibition. PCSK9 can be inhibited at the protein level with specific antibodies or at the RNA level by targeting PCSK9 RNA with siRNA.
Evolocumab and alirocumab, humanized monoclonal anti-PCSK9 antibodies, have been designed to increase LDL-R on hepatocytes, reducing LDL and Lp(a) plasma concentration. In vitro, treatment with anti-PCSK9 antibody significantly reduces calcium accumulation in VICs cultures [75]. There is growing clinical evidence that the subcutaneous administration of alirocumab and evolocumab in statin-intolerant patients is a safe, tolerable, and effective treatment for hypercholesterolemia, leading to great and persistent reduction in LDL-C levels [77,78]. Recently, the FOURIER trial has demonstrated that the addition of evolocumab to background statin therapy decreases the risk of CV events in patients with established atherosclerotic CV disease, lowering LDL-C levels by at least 30% in 99% of subjects and Lp(a) levels by a median of 27% [79,80]. In the FLOREY trial involving healthy men, evolocumab has proven to lower plasma Lp(a) levels up to 36% with two mechanisms: by decreasing Lp(a) production as monotherapy and by increasing Lp(a) catabolism in combination with atorvastatin [81]. However, analysis of the plaque composition has demonstrated that evolocumab does not change the calcium volume of coronary atherosclerotic plaques [82]. Recently, the ODYSSEY OUTCOMES trial has detected a reduction in the risk of major adverse CV events after addition of alirocumab to background statin therapy in patients with recent acute coronary syndrome [83], confirming the additional beneficial effect of this lipid-lowering therapy.
5.3.2. Future Perspectives
The above-described recent data focus on the capability of PCSK9-lowering treatments to reduce lipoproteins levels, but clinical evidence evaluating their potential effects on patients with CAVS is lacking. Currently, a randomized, placebo-controlled trial (NCT03051360) is assessing whether the administration of an anti-PCSK9 antibody to patients with mild to moderate CAVS can slow disease progression by decreasing Lp(a) and LDL-C levels [84] (see Table 1). If successful, it could support the design of other trials to further investigate this pharmacological therapy.
Another novel approach to lower PCSK9 concentration is the blocking of hepatic synthesis with inclisiran, a siRNA targeting PCSK9 RNA. Inclisiran, administered subcutaneously every 6 months, is an effective PCSK9- and LDL-lowering treatment with good patient tolerability [85]. Very recently, three pivotal phase III trials (ORION-9, ORION-10, ORION-11) have detected a persistent reduction in LDL-C levels by approximately 50% with inclisiran in patients with atherosclerotic CV disease or familial hypercholesterolemia [86,87]. These promising results provide a rationale for clinical trials involving CAVS patients to assess whether this lipid-lowering treatment can reduce disease progression.
6. RAAS Blockade
6.1. ACE Inhibitors/ARBs
6.1.1. Current Evidence
Systemic arterial hypertension is a frequent comorbidity in CAVS, affecting at least 30% of symptomatic patients [88]. High systemic pressure increases the mechanical forces, favoring an endothelial lesion in the aortic side of the leaflets, and alters the expression of markers involved in inflammation (VCAM-1, IL-6), ECM remodeling (MMPs, collagen), and calcification (osteopontin) [89], increasing the progression rate of CAVS. The stenotic valve and the systemic vascular resistance represent two resistances in series, both contributing to pressure overload in the left ventricle (LV) [90]. In patients with CAVS, hypertension increases LV hypertrophic remodeling and afterload, resulting in higher incidence of clinical CV events [91]. Treating hypertension could be useful to improve the clinical outcomes of CAVS patients. Traditionally, an antihypertensive treatment was contraindicated because it would decrease systemic vascular resistance without increasing cardiac output, with the risk of severe hypotension and lower myocardial perfusion [92]. However, recent trials have reported no change in heart rate or evident adverse effects in patients with CAVS treated with antihypertensive treatments [93]. To date, the most studied class of antihypertensive for the management of hypertensive patients with CAVS is the renin–angiotensin–angiotensinogen system (RAAS)-blocking therapy.
RAAS regulates arterial blood pressure at different levels. Angiotensinogen is hydrolyzed by renin into the inactive precursor angiotensin I, further hydrolyzed by the angiotensin-converting enzyme (ACE) into the active angiotensin II (Ang II). In addition to ACE, the enzyme chymase is involved in the production of Ang II. Ang II binds to its Ang II type 1 receptor (AT1R) inducing inflammation, oxidative stress, fibrosis, and vasoconstriction [94]. In addition, ACE promotes the inactivation of bradykinin, required for the synthesis of NO, limiting its vasodilator effect. RAAS overactivation leads to hypertension; its blockade through ACE inhibitors (ACEI) or Ang II receptor blockers (ARBs) is a common antihypertensive strategy. There is evidence of RAAS involvement in CAVS progression: Ang II has been shown to increase IL-6 production, to promote cardiac fibrosis, and to induce osteogenic differentiation of cultured VICs [95,96]. Human stenotic AVs are characterized by an overexpression of chymase, AT1R, and ACE, providing evidence of a local activation of RAAS in the valve [97]. Moreover, ACE is colocalized with lipoproteins in the valve lesions, suggesting that ACE is delivered in the AV by LDL [98]. Based on these recent findings, the blockade of RAAS could give cardioprotective and beneficial effects; clinical trials with ACEI and ARBs have been performed to test the hypothesis.
ACEI therapy was well tolerated in patients with various severity of CAVS [99,100] and its effects were assessed in some small-size trials. The first one failed to show any beneficial hemodynamic effect of ACEI in monotherapy or in combination with statins [23]. In contrast, ACEI were associated with lower AV calcification, hemodynamic benefits, and slower progression of mild CAVS in consequent trials [101,102]. More recently, two small randomized trials (ACCESS and RIAS), involving patients with moderate to severe CAVS, have detected hemodynamic improvement and progressive reduction in LV hypertrophy with ACEI [103,104]. These studies were not powered enough for relevant clinical outcomes; therefore, the preliminary promising findings should be confirmed by larger clinical trials.
ARBs were tested in patients with severe CAVS because AT1R are activated and involved in the AV remodeling and fibrosis, a later stage of CAVS. In the prospective ROCK-AS trial, candesartan was well tolerated but failed to show efficacy [105]. In contrast, two consequent studies associated the treatment with ARBs (but not with ACEI) to a reduction in AV remodeling, inflammation, IL-6 expression, and fibrosis score, suggesting that ARBs could halt the fibrotic process by lowering tissue inflammation [106,107]. It is likely that a large amount of Ang II is produced by chymase instead of ACE and the most effective way to reduce AV remodeling is the downstream blocking of AT1R through ARBs.
The effect of RAAS blockade with ACEI and ARBs was also investigated in larger trials with promising findings. An observational population-based study correlated ACEI and ARBs with higher survival and lower risk of CV events in patients with various degrees of CAVS [108]. A large retrospective study of patients included in the SEAS trial confirmed previous data, detecting that RAAS blockade did not increase the risk of CV and all-cause mortality and reduced LV mass progression [109]. The JAAS prospective analysis concluded that ACEI and ARBs may be beneficial before or early after the development of CAVS [110].
6.1.2. Future Perspectives
The above-described studies, reporting conflicting results, only partially demonstrated the efficacy of ACEI and ARBs in reducing AV remodeling and CAVS progression. Currently, two clinical trials are ongoing to further investigate the potential beneficial effects of ARBs, in particular fimasartan (ALFA trial, NCT01589380) and losartan (NCT03666351), in hypertensive patients with moderate to severe CAVS [111,112]. However, these studies evaluate the change in hemodynamic parameters and LV remodeling; they are not specifically designed to determine the effects of the treatment on valvular calcification.
Further large-scale randomized trials are required to determine whether a RAAS-blocking therapy can delay the need for AVR, halt disease progression, and lower the mortality rate in patients with moderate to severe CAVS, as suggested by a recent review [113]. The current American and European guidelines recommend treating coexisting systemic hypertension in patients with asymptomatic CAVS or at high risk for developing CAVS by choosing an antihypertensive drug that avoids hypotension [34,35], but they do not specify which treatment should be used. To date, trials are missing on different classes of antihypertensive drugs, the RAAS-blocking therapies represent the treatment of choice, and the above-reported studies suggest targeting RAAS not as a CAVS-specific treatment, but for treating CAVS-related comorbidities.
In recent years, several trials have been performed to assess the effects of a postoperative RAAS blockade on clinical outcomes. Post-AVR treatment has been associated with improved long-term outcomes [114] and a lower risk of all-cause and CV mortality [115,116]. The global cardiovascular protective effect might be partially explained by a positive LV remodeling; a randomized trial (ARISTOTE, NCT03315832) is ongoing to confirm this hypothesis [117]. Taken together, these recent clinical data suggest treating patients who underwent AVR with a postoperative RAAS-blocking therapy to improve the prognosis. Based on this evidence, a RAAS-blocking therapy seems to be more effective if prescribed after surgical or transcatheter AVR.
6.2. Mineralocorticoid Receptor Antagonists
6.2.1. Current Evidence
An alternative approach to reduce RAAS activation is the administration of mineralocorticoid receptor antagonists (eplerenone and spironolactone), used for the treatment of hypertension. Spironolactone has been shown to prevent vascular calcification in vitro and to improve CV clinical outcomes [118]; however, its effects have never been assessed in clinical trials involving patients with CAVS. Eplerenone has proven to halt the process of vascular calcification in vitro [119] and to exert an anti-atherosclerotic effect in vivo [120]. Moreover, it reduces LV hypertrophy in hypertensive subjects [121] and improves clinical outcomes among patients with systolic heart failure [122]. A study in hypercholesterolemic rabbits has shown the presence of mineralocorticoid receptors in the AV and has reported the beneficial effects of a selective antagonism with eplerenone in the early stage of CAVS [123]. Despite the promising preclinical findings, the only clinical trial involving CAVS patients has failed to show efficacy of eplerenone in reducing CAVS progression or LV dysfunction [124].
6.2.2. Future Perspectives
To our knowledge, no ongoing studies have been designed to evaluate the potential effects of the mineralocorticoid receptor antagonists on the progression of CAVS. An early phase I trial (NCT03923530) is currently investigating whether a postoperative eplerenone treatment can improve the outcomes and the quality of life among patients with hypertension and abnormal hemodynamics after TAVR [125]. In the case of positive outcomes, it would confirm the hypothesis that RAAS blockade is more effective if administered after AVR. However, it remains unclear and to be evaluated in future studies whether the modulation of the mineralocorticoid receptor could give a protective effect on the progression of CAVS.
7. Modulators of Nitric Oxide Pathway
7.1. Current Evidence
Nitric oxide (NO) is a potent vasodilator mainly produced by endothelial NO synthase (eNOS) and secreted by endothelial cells. Endothelial-derived NO binds to the heme group of intracellular soluble guanylyl cyclase (sGC), increasing the production of cGMP. The activation of the NO/sGC/cGMP pathway plays a central role in many physiological mechanisms, such as vasodilation, inhibition of platelet aggregation, anti-inflammatory, and anti-fibrotic processes. In the aortic valve, NO released by VECs prevents matrix calcification and osteoblastic differentiation of VICs, exerting protective effects [126]. In pathological conditions, eNOS downregulation and uncoupling lead to increased ROS production, enhanced oxidative stress, and decreased NO bioavailability, promoting the progression of CAVS [127].
NO donors, currently used for the management of acute heart failure, could offer an advantage in patients with severe CAVS and concomitant congestive heart failure or LV dysfunction, a high-risk population with worse clinical outcomes and higher mortality rate. Although conventionally, they were contraindicated in CAVS due to the risk of severe hypotension, they could be a useful treatment for patients with cardiac comorbidities for their ability to reduce LV consumption of oxygen, filling pressure and afterload, and improving cardiac perfusion and functionality [91].
In addition to the effects on the vasculature, NO donors seem to act directly in the valve; for example, L-Arginine and nitroprusside have been shown to inhibit osteogenic differentiation of cultured VICs [128,129]. This anti-calcific effect seems to be mediated by sGC activators (such as BAY and YC-1) or by agents increasing intracellular cGMP levels, while it is prevented by sGC inhibitors (such as ODQ), suggesting that the protective action of NO on VICs is probably dependent on the activation of the sGC/cGMP pathway [130,131]. Collectively, these findings motivate potential therapeutic strategies based on the activation of the NO/sGC/cGMP pathway, providing a rationale for clinical trials with NO donors and sGC activators to test this hypothesis.
To date, the effects of NO donors have been assessed in some small-size trials involving patients with severe CAVS and concomitant CV diseases. These studies detected an improvement in cardiac output and a beneficial decrease in LV afterload and filling pressure without increasing the risk of hypotension [132,133]. However, the aim of the trials was the management of patients with heart failure and concomitant CAVS; they were not designed to assess the effects of NO donors on CAVS progression and future studies should investigate these aspects.
Another pharmacological approach to activate the NO/sGC/cGMP pathway is the inhibition of phosphodiesterase type 5 (PDE5), the enzyme responsible for hydrolysis of cGMP to GMP. The PDE5 inhibitor sildenafil, an oral vasodilator widely used for erectile dysfunction, is also effective for pulmonary arterial hypertension, where PDE5 is upregulated [134]. The potential beneficial effects of PDE5 inhibition for the treatment of CV diseases have been investigated in several trials. At the cardiac level, sildenafil improves hemodynamic parameters, cardiac output and LV diastolic function in patients with heart failure [135]. An overexpression of myocardial PDE5 has been also observed in patients with severe CAVS or LV dysfunction [136] and its inhibition could provide a beneficial effect, but to date, only two small-size trials have been performed on CAVS patients. The first pilot study (ASPEN trial, NCT01275339), involving subjects with moderate to severe CAVS, was terminated without results for difficulty of enrolling patients [137]. In the second trial, a short-term treatment with sildenafil to patients with severe symptomatic CAVS was safe, well tolerated, and effective in improving hemodynamic parameters [138]. However, the study was not designed to evaluate the effects of the treatment on CAVS progression.
7.2. Future Perspectives
The above-reported clinical data provided evidence for the safety of NO donors and PDE5 inhibitors in CAVS, but no convincing data are available on their long-term use and clinical efficacy. In addition, these trials were specifically focused on the change in hemodynamic parameters and LV remodeling. Thus, long-term and larger randomized trials are required to confirm preliminary findings and future studies should investigate the effects of the treatments on CAVS progression.
Concerning sGC activators, a potential candidate is ataciguat (HMR1766), which preferentially binds to the oxidized state of sGC, increasing its enzymatic activity independently of NO release. Ataciguat induces NO production in endothelial cells [139], improves vascular functions in an animal model of heart failure [140], and reverses hemodynamic changes in experimental pulmonary hypertension [141]. The safety and effects of ataciguat are currently being assessed in two studies involving patients with mild to moderate CAVS. The first trial (NCT02049203) is evaluating the safety of the treatment [142]; the second one (NCT02481258) aims to determine the long-term efficacy in reducing LV dysfunction and slowing disease progression [143] (see Table 1). If successful, they could provide a rationale for larger randomized trials.
8. Anti-Calcific Agents
The calcification of the valve plays a central role in driving disease progression and can represent a key target for novel therapies. The mechanisms involved in valvular calcification are similar to those of skeletal bone formation and inhibitors of pathological mineralization (bisphosphonates, denosumab, and vitamin K) could provide an effective strategy to reduce ectopic calcification. Their effects are being assessed in experimental studies and clinical trials.
8.1. Inhibitors of Bone Resorption
8.1.1. Current Evidence
Bisphosphonates and denosumab are pharmacological treatments widely used for bone diseases characterized by excessive osteoclast-mediated bone resorption, such as osteoporosis. Bisphosphonates are inhibitors of osteoclast differentiation and activity on bone surface; denosumab is a human monoclonal antibody that targets the receptor activator of nuclear factor kappa B ligand (RANKL), avoiding its binding to its transmembrane receptor RANK on different cell types. In bone, RANK activation on pre-osteoclasts’ surfaces induces their differentiation to osteoclasts, increasing the availability of calcium and phosphate ions in the blood. The process can be counteracted by osteoprotegerin (OPG), a soluble decoy that targets RANKL preventing RANK activation. There is growing evidence of the local activation of the OPG/RANK/RANKL pathway in the CV system and AV in particular. OPG exerts a protective effect in the vasculature and AV [144], confirmed by the fact that OPG-deficient mice develop osteoporosis and vascular calcification [145]. Calcified arteries and stenotic AVs are characterized by decreased expression of OPG and increased levels of RANKL [146]. There is recent evidence of an upregulation of RANKL expression in circulating mononuclear cells of patients with CAVS, favoring ectopic calcification. In addition, the treatment with RANKL promotes matrix calcification and osteoblastic differentiation of cultured cells [14,147]. Based on these data, RANK seems to be also expressed on VICs’ surfaces, where its activation promotes CAVS progression.
Several cross-sectional and longitudinal studies have reported a strong inverse correlation between bone mineral density and valvular/vascular calcification [148,149]. This phenomenon, which is referred to as the “calcification paradox”, may be explained by common pathways with reciprocal effects on bone and vasculature simultaneously (including the OPG/RANK/RANKL axis) and suggests that treatments for osteoporosis might have a beneficial effect on vascular/valvular calcification while maintaining appropriate bone density.
Concerning denosumab, only preclinical data are available. Denosumab reduces vascular calcification in glucocorticoid-induced osteoporotic mice [150] and inhibits calcium deposition in porcine VICs cultures [151].
Bisphosphonates were developed as more stable analogues of inorganic pyrophosphate and their effects have been investigated in several preclinical and clinical studies. They have been shown to prevent the osteogenic differentiation of cultured cells [152] and to inhibit valvular/vascular calcification in mice at doses comparable to those used for osteoporosis [153]. In a recent study on an experimental model of CAVS, local delivery of zoledronate at the level of AV has shown safety and efficacy in inhibiting the progression of AV calcification [154]. In addition to reducing bone resorption, the beneficial effects of bisphosphonates in the CV system could be related to the extra-skeletal properties, including the decrease in cytokines secretion, the downregulation of adhesion molecules, and the reduction in circulating monocytes and LDL-C [155]. Several retrospective studies investigated the extra-skeletal effects of bisphosphonates. The first small-size clinical trials, involving dialysis patients with end-stage renal disease and concomitant CV calcification, detected a decrease in arterial calcification after treatment with etidronate, improving long-term outcomes [156,157]. Several recent trials have assessed the effects of bisphosphonates on CV calcification: a large multi-ethnic study (MESA) associated the bisphosphonate treatment with decreased prevalence of CV calcification in older women with subclinical CV diseases [158]; some observational retrospective studies reported an increase in AV area and slower disease progression in patients with CAVS treated with bisphosphonates [159,160]. In contrast, a large retrospective study involving older women with mild to moderate CAVS did not observe any significant impact of bisphosphonates on the progression of the disease [161].
8.1.2. Future Perspectives
The main limitation of the above-reported studies was the prescription of bisphosphonates only to patients with concomitant osteoporosis, which has an additional effect on the development of CAVS and could be a major confounder [162]. Prospective data are lacking and the potential efficacy of the treatment should be further evaluated in large randomized controlled trials involving patients without bone diseases. Currently, the ongoing SALTIRE II trial (NCT02132026) has randomized 150 patients with mild CAVS and no concomitant osteoporosis to denosumab, alendronate, or placebo [163] (see Table 1). If successful, it will be the first study to determine whether osteogenic drugs can reduce disease progression in patients without bone diseases. The study has been completed and is currently in analysis.
8.2. Vitamin K
8.2.1. Current Evidence
Vitamin K is a liposoluble vitamin naturally found as vitamin K1 (phylloquinone) in vegetables and vitamin K2 (menaquinones) in fermented food. Vitamin K serves as a cofactor for the activation of vitamin K-dependent proteins, including matrix Gla protein (MGP), through the γ-carboxylation of Glu residues. The active form of MGP functions as potent inhibitor of soft-tissue calcification by binding calcium ions and avoiding the formation of HA crystals [164]. Active MGP can also interact with bone morphogenetic protein-2 (BMP-2), reducing its osteogenic activity [165]. A beneficial anti-calcific role of MGP in the CV system is supported by experimental evidence: inhibition of MGP gene induces osteoblastic differentiation of human VICs [166] and Mgp-deficient mice develop arterial calcification [167]. MGP expression was significantly reduced in VICs isolated from stenotic valves [168]. MGP activity can be modulated by vitamin K and its antagonists: a low intake of vitamin K or the assumption of vitamin K-antagonists (warfarin) lead to vitamin K-insufficiency and therefore, lower activation of MGP [169]. There is preclinical and clinical evidence that vitamin K-antagonists accelerate osteoblastic differentiation of cultured VICs, increase vascular/valvular calcification, and promote AV degeneration [170,171]. These findings suggest that vitamin K-independent oral anticoagulants (such as thrombin inhibitors or factor Xa inhibitors) are preferable for patients with early CAVS.
The supplementation of vitamin K has been proposed as a novel strategy to reduce CV calcification by enhancing MGP activity. Vitamin K has also proven to exert an anti-inflammatory effect: vitamin K2 reduces the expression of pro-inflammatory cytokines in cell cultures [172] and the dietary supplementation of vitamin K1 has a similar effect in animal models [173]. The MESA study has found an inverse correlation between serum levels of vitamin K1 and circulating inflammation markers, such as ICAM-1, C-reactive protein, and IL-6 [174]. In addition, vitamin K2 decreases cholesterol biosynthesis and increases LDL-R, reducing plasma lipid levels [175]. The anti-inflammatory and lipid-lowering properties of vitamin K, independent of γ-carboxylation, may also contribute to the inhibition of ectopic calcification and provide a rationale for clinical trials with vitamin K supplementation.
The effects of oral vitamin K assumption have been investigated in some prospective randomized controlled trials with conflicting outcomes. In the CACK2 and Vitacal trials, vitamin K2 administration did not decrease the progression of vascular calcification in patients with chronic kidney disease and diabetes [176,177]. These studies were limited by short-term follow up and small sample size. In a long-term trial, daily supplementation of vitamin K1 for 3 years showed beneficial effects in healthy elderly people with pre-existing vascular calcification [178]. An inverse correlation between vitamin K2 intake and risk of coronary heart disease was also detected in two large population-based studies [179,180].
8.2.2. Future Perspectives
The iPACK-HD, VitaVasK, and VitaK-CAC trials are currently assessing the potential efficacy of vitamin K assumption for reducing coronary artery calcification in hemodialysis patients and in subjects with coronary heart disease [181,182,183].
Vitamin K has also been supplemented in recent clinical trials to assess the potential effects on AV calcification. The first randomized controlled trial involving CAVS patients has associated the supplementation of vitamin K1 with slower progression of AV calcification [184]. The ongoing AVADEC (NCT03243890) and BASIK2 (NCT02917525) randomized trials are investigating the effects of vitamin K2 (menaquinone-7) supplementation on the progression of AV calcification, respectively, in patients without clinically significant CAVS or with bicuspid AV and mild to moderate CAVS [185,186] (see Table 1). If successful, they would provide as effective treatment for CAVS a simple, safe, and readily available compound that can be easily supplemented in patients. However, larger phase 3 clinical trials are required to confirm this preliminary hypothesis.
9. Emerging Targets
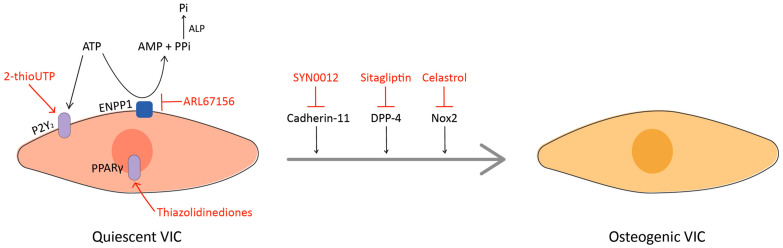
In recent years, a better understanding of the pathophysiology has led to the identification of several interesting targets for the development of novel therapeutic approaches (see Figure 2). In this chapter, we focused on the role of some innovative targets that have already collected preclinical in vivo evidence (see Table 2). Nevertheless, several other cellular pathways with potentiality for future in vivo application are currently under investigation [187,188,189].
Figure 2.
A simplified schematic representation of potential novel targets (in black) and corresponding treatments (in red). The regular arrow means “activation”, the T-shaped arrow stands for “inhibition”.
Table 2.
Potential novel targets for CAVS and corresponding treatments with in vivo evidence.
| Target | Treatment | Effects | Model | Ref. |
|---|---|---|---|---|
| Nox2 | Celastrol | Nox2 inhibition mitigates the severity of aortic valve fibrosis, calcification, and stenosis | rabbit | [190] |
| ENPP1 | ARL67156 | The inhibition of ENPP1 prevents the development of CAVS | rat | [191] |
| P2Y2 | 2-thioUTP | P2Y2 agonist promotes the regression of CAVS | mouse | [192] |
| DPP-4 | Sitagliptin | DPP-4 inhibition prevents CAVS development | rabbit | [193] |
| Cadherin-11 | SYN0012 | Cad-11-blocking antibody prevents Notch1-mediated CAVS | mouse | [194] |
| PPARγ | Pioglitazone | PPARγ agonist attenuates the progression of aortic valve calcification | rabbit | [195] |
| PPARγ agonist attenuates lipid deposition, calcification, and apoptosis in aortic valves | mouse | [196] |
9.1. Nox2
NADPH oxidase 2 (Nox2) is a ROS-generating enzyme upregulated in human stenotic AVs and associated with osteoblastic differentiation of cultured VICs [190]. The selective Nox2 inhibitor celastrol is a natural compound used in traditional Chinese medicine for cancer, neurodegeneration, chronic inflammatory, and autoimmune diseases because of its antioxidant property [197]. It also exerts pleiotropic effects, including inhibition of pro-inflammatory cytokines production, reduction in osteoclast formation, and decrease in bone resorption [198]. There is recent evidence that celastrol prevents calcium deposition in cultured VICs and reduces ROS generation, fibrosis, LV remodeling, and calcification without side effects in a rabbit model of CAVS, suggesting the safety and therapeutic effectiveness of the treatment [190]. Despite the promising findings, additional long-term preclinical studies are needed to confirm the potential beneficial properties before entering clinical trials, as suggested by Yeang and colleagues [199].
9.2. ENPP1 and P2Y2
Ectonucleotide pyrophosphatase/phosphodiesterase 1 (ENPP1) is a membrane-bound member of the ectonucleotidases family, which hydrolyzes extracellular ATP to generate pyrophosphate, a potent inhibitor of vascular/valvular calcification [200]. When ENPP1 is overexpressed, it also increases the levels of inorganic phosphate with a pro-calcific effect [201]. ENPP1 is upregulated in calcific AVs, where it promotes the mineralization of cultured VICs [15]. The pro-mineralizing effect of ENPP1 can be also related to the decrease in ATP levels: in fact, ATP exerts a protective effect on VICs by binding to the purinergic receptor P2Y2, which activates the PI3K/Akt pathway [202]. Based on this evidence, inhibitors of ENPP1 or agonists of P2Y2 might prevent the mineralization of the valve and the development of CAVS. ARL67156, an inhibitor of ectonucleotidases, and 2-thioUTP, an agonist of P2Y2, have been shown, respectively, to prevent disease development and to promote its regression in experimental models of CAVS [191,192], providing evidence that the pathologic mineralization of the valve is a reversible process. The promising preclinical findings should be confirmed in clinical trials to determine the effectiveness of the treatments.
9.3. DPP-4
Dipeptidyl peptidase 4 (DPP-4) is a multifunctional enzyme that cleaves the N-terminal dipeptides of several substrates, including chemokines, neuropeptides, and regulatory peptides [203]. DPP-4 expression is increased in the AV after endothelial dysfunction and can induce VICs osteogenic differentiation, while the inhibition of its enzymatic activity with sitagliptin halts the process in vitro [193]. Selective DPP-4 inhibitors, including sitagliptin, are a new class of oral hypoglycemics approved for the treatment of type II diabetes because they avoid the inactivation of glucagon-like peptide 1 (GLP-1) [203]. There is recent evidence that the administration of sitagliptin reduces AV calcification and disease progression in animal models of CAVS [194], suggesting that the repositioning of DDP-4 inhibitors could be a novel strategy for the treatment of CAVS. This hypothesis, further supported by the anti-atherosclerotic and anti-inflammatory properties of DPP-4 inhibitors [204], should be tested in additional preclinical and clinical studies.
The pro-calcific action of DPP-4 seems to be related to the inactivation of insulin-like growth factor-1 (IGF-1), a growth hormone with protective effects on the CV system [205]. There is in vitro evidence of IGF-1 anti-calcific affect in vascular and valvular cells [206], but additional experiments are warranted to confirm its relationship with DPP-4.
9.4. Cadherin-11
Cadherin-11 (Cad-11) is a specialized cell–cell adhesion protein related to proper embryonic valve formation and remodeling, but it may also contribute to CAVS pathogenesis if expressed in adulthood [207]. The overexpression of Cad-11 leads to dystrophic calcific nodules in vitro and calcification in mature heart valves by upregulating RhoA and Sox9 expression [208,209]. Conversely, Cad-11-/- adult mice do not develop AV calcification [210] and the treatment with SYN0012 (a Cad-11-blocking antibody) reduces calcification, pro-inflammatory signals, and leaflet stiffening in Notch+/− mice [194]. Taken together, these preclinical data suggest targeting Cad-11 as a novel pharmacological strategy for preventing disease progression in CAVS patients. Very recently, SYN0012 treatment has proven to improve cardiac function and to reduce inflammation-driven fibrotic remodeling of the myocardium in mice, suggesting that blocking Cad-11 might also prevent cardiac fibrosis and heart failure, common comorbidities in CAVS patients [211].
9.5. PPARγ
Peroxisome proliferator-activated receptor-gamma (PPARγ) is a nuclear receptor of the PPARs family, regulating the transcription of several genes. The downregulation of PPARγ expression has been associated with atherosclerosis, hypertension, and vascular calcification [212]. Conversely, its activation reduces inflammation, inhibits apoptosis, and improves endothelial function [213], making PPARγ agonists an interesting therapeutic option for the treatment of dyslipidemia, atherosclerosis, and CV diseases. PPARγ agonists are insulin sensitizers for the treatment of type II diabetes, but their use is limited because of safety concerns. Among them, the most used and safer agonist is pioglitazone, which has been shown to reduce lipid deposition, apoptosis, and AV calcification in animal models [195,196], providing a rationale for clinical trials with PPARγ agonists for CAVS treatment. There is recent evidence that the anti-calcific effect of pioglitazone is mediated by the inhibition of the Wnt/β-catenin signaling pathway [214], but more experiments are required to elucidate its mechanism of action on VICs. Although the promising preclinical findings encourage the use of PPARγ agonists for CAVS, the adverse effects (such as bone loss and increased risk of heart failure) limit the application of this therapy [215]. The benefit–risk ratio should be investigated in future preclinical studies.
10. Conclusions
Calcific aortic valve stenosis represents an increasing health care burden, but there is no effective pharmacological therapy to avoid the progression towards surgery. Despite some promising data, the above-reported medical treatments have not yet been convincingly shown to slow disease progression or to improve clinical outcomes. Thus, they are currently prescribed for treating CAVS-related comorbidities, not as CAVS-specific treatments. Statins have failed to show effectiveness in halting disease progression or preventing the onset; RAAS blockade has only partially demonstrated efficacy in reducing CAVS progression and RAAS-blocking therapy seems to be more effective if prescribed after AVR. Concerning Lp(a)-lowering therapies, modulators of the NO pathway, and anti-calcific agents, the efficacy of these treatments has not yet been determined in clinical studies or should be further assessed in larger randomized trials. The growing experimental evidence and understanding of the pathophysiology indicate that, although CAVS shares pathophysiological features with atherosclerosis and vascular calcification, it is a specific valvular disease. Moreover, it has been recently revealed that the progression, prognosis, and outcomes of CAVS are sex-dependent; for example, women have lower density of AV calcium, reduced fibrosis, and less inflammatory response compared to men [216,217]. Therefore, novel medical treatments should target valve-specific and sex-related signaling pathways to be more effective. Nowadays, several molecular targets (including Nox2, ENPP1, P2Y2, DPP-4, cadherin-11, and PPARγ) are under current investigation for the development of novel therapeutic strategies.
Author Contributions
Conceptualization, M.R.; Writing—original draft, M.D. and M.R.; Writing—review and editing, N.F., M.G.L. and E.F. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the Ministero della Salute (RF-2013-02358024 to M.R.).
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Lindman B.R., Clavel M.A., Mathieu P., Iung B., Lancellotti P., Otto C.M., Pibarot P. Calcific aortic stenosis. Nat. Rev. Dis. Primers. 2016;2:16006. doi: 10.1038/nrdp.2016.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Osnabrugge R.L.J., Mylotte D., Head S.J., Nkomo V.T., LeReun C.M., Bogers A.J., Piazza N., Kappetein A.P. Aortic stenosis in the elderly: Disease prevalence and number of candidates for transcatheter aortic valve replacement: A meta-analysis and modeling study. J. Am. Coll. Cardiol. 2013;62:1002–1012. doi: 10.1016/j.jacc.2013.05.015. [DOI] [PubMed] [Google Scholar]
- 3.Nkomo V.T., Gardin J.M., Skelton T.N., Gottdiener J.S., Scott C.G., Enriquez-Sarano M. Burden of valvular heart diseases: A population-based study. Lancet. 2006;368:1005–1011. doi: 10.1016/S0140-6736(06)69208-8. [DOI] [PubMed] [Google Scholar]
- 4.Ancona R., Comenale Pint S. Epidemiology of aortic valve stenosis (AS) and of aortic valve incompetence (AI): Is the prevalence of AS/AI similar in different parts of the world? Eur. J. Cardiol. Pract. 2020;18:10–12. [Google Scholar]
- 5.Myasoedova V.A., Ravani A.L., Frigerio B., Valerio V., Moschetta D., Songia P., Poggio P. Novel pharmacological targets for calcific aortic valve disease: Prevention and treatments. Pharmacol. Res. 2018;136:74–82. doi: 10.1016/j.phrs.2018.08.020. [DOI] [PubMed] [Google Scholar]
- 6.Head S.J., Çelik M., Kappetein A.P. Mechanical versus bioprosthetic aortic valve replacement. Eur. Heart J. 2017 doi: 10.1093/eurheartj/ehx141. [DOI] [PubMed] [Google Scholar]
- 7.Chen H.Y., Engert J.C., Thanassoulis G. Risk factors for valvular calcification. Curr. Opin. Endocrinol. Diabetes Obes. 2019;26:96–102. doi: 10.1097/MED.0000000000000471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hulin A., Hego A., Lancellotti P., Oury C. Advances in Pathophysiology of Calcific Aortic Valve Disease Propose Novel Molecular Therapeutic Targets. Front. Cardiovasc. Med. 2018;5:21. doi: 10.3389/fcvm.2018.00021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Peeters F.E.C.M., Meex S.J.R., Dweck M.R., Aikawa E., Crijns H.J.G.M., Schurgers L.J., Kietselaer B.L.J.H. Calcific aortic valve stenosis: Hard disease in the heart: A biomolecular approach towards diagnosis and treatment. Eur. Heart J. 2018;39:2618–2624. doi: 10.1093/eurheartj/ehx653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Perrucci G.L., Zanobini M., Gripari P., Songia P., Alshaikh B., Tremoli E., Poggio P. Pathophysiology of aortic stenosis and mitral regurgitation. Compr. Physiol. 2017;7:799–818. doi: 10.1002/cphy.c160020. [DOI] [PubMed] [Google Scholar]
- 11.Tao G., Kotick J.D., Lincoln J. Heart Valve Development, Maintenance, and Disease. The Role of Endothelial Cells. Volume 100. Elsevier Inc.; Amsterdam, The Netherlands: 2012. [DOI] [PubMed] [Google Scholar]
- 12.Rutkovskiy A., Malashicheva A., Sullivan G., Bogdanova M., Kostareva A., Stensløkken K.O., Fiane A., Vaage J. Valve interstitial cells: The key to understanding the pathophysiology of heart valve calcification. J. Am. Heart Assoc. 2017;6:e006339. doi: 10.1161/JAHA.117.006339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pawade T.A., Newby D.E., Dweck M.R. Calcification in aortic stenosis: The skeleton key. J. Am. Coll. Cardiol. 2015;66:561–577. doi: 10.1016/j.jacc.2015.05.066. [DOI] [PubMed] [Google Scholar]
- 14.Kaden J.J., Bickelhaupt S., Grobholz R., Haase K.K., Sarikoç A., Kiliç R., Brueckmann M., Lang S., Zahn I., Vahl C., et al. Receptor activator of nuclear factor κB ligand and osteoprotegerin regulate aortic valve calcification. J. Mol. Cell Cardiol. 2004;36:57–66. doi: 10.1016/j.yjmcc.2003.09.015. [DOI] [PubMed] [Google Scholar]
- 15.Côté N., El Husseini D., Pépin A., Guauque-Olarte S., Ducharme V., Bouchard-Cannon P., Audet A., Fournier D., Gaudreault N., Derbali H., et al. ATP acts as a survival signal and prevents the mineralization of aortic valve. J. Mol. Cell Cardiol. 2012;52:1191–1202. doi: 10.1016/j.yjmcc.2012.02.003. [DOI] [PubMed] [Google Scholar]
- 16.Zhou Y., Li J., Zhou K., Liao X., Zhou X., Shen K. The methylation of Notch1 promoter mediates the osteogenesis differentiation in human aortic valve interstitial cells through Wnt/β-catenin signaling. J. Cell Physiol. 2019;234:20366–20376. doi: 10.1002/jcp.28638. [DOI] [PubMed] [Google Scholar]
- 17.Rattazzi M., Iop L., Faggin E., Bertacco E., Zoppellaro G., Baesso I., Puato M., Torregrossa G., Fadini G.P., Agostini C., et al. Clones of interstitial cells from bovine aortic valve exhibit different calcifying potential when exposed to endotoxin and phosphate. Arterioscler. Thromb. Vasc. Biol. 2008;28:2165–2172. doi: 10.1161/ATVBAHA.108.174342. [DOI] [PubMed] [Google Scholar]
- 18.Blaser M.C., Aikawa E. Roles and Regulation of Extracellular Vesicles in Cardiovascular Mineral Metabolism. Front. Cardiovasc. Med. 2018;5:187. doi: 10.3389/fcvm.2018.00187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kostyunin A.E., Yuzhalin A.E., Ovcharenko E.A., Kutikhin A.G. Development of calcific aortic valve disease: Do we know enough for new clinical trials? J. Mol. Cell Cardiol. 2019;132:189–209. doi: 10.1016/j.yjmcc.2019.05.016. [DOI] [PubMed] [Google Scholar]
- 20.Lim S.Y. Role of statins in coronary artery disease. Chonnam Med. J. 2013;49:1–6. doi: 10.4068/cmj.2013.49.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jarrett M.J., Yao Q., Venardos N., Weyant M.J., Reece T.B., Meng X., Fullerton D.A. Simvastatin down-regulates osteogenic response in cultured human aortic valve interstitial cells. J. Thorac. Cardiovasc. Surg. 2020 doi: 10.1016/j.jtcvs.2019.10.081. [DOI] [PubMed] [Google Scholar]
- 22.Rajamannan N.M., Subramaniam M., Stock S.R., Stone N.J., Springett M., Ignatiev K.I., McConnell J.P., Singh R.J., Bonow R.O., Spelsberg T.C. Atorvastatin inhibits calcification and enhances nitric oxide synthase production in the hypercholesterolaemic aortic valve. Heart. 2005;91:806–810. doi: 10.1136/hrt.2003.029785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rosenhek R., Rader F., Loho N., Gabriel H., Heger M., Klaar U., Schemper M., Binder T., Maurer G., Baumgartner H. Statins but not angiotensin-converting enzyme inhibitors delay progression of aortic stenosis. Circulation. 2004;110:1291–1295. doi: 10.1161/01.CIR.0000140723.15274.53. [DOI] [PubMed] [Google Scholar]
- 24.Bellamy M.F., Pellikka P.A., Klarich K.W., Tajik A.J., Enriquez-Sarano M. Association of cholesterol levels, hydroxymethylglutaryl coenzyme-A reductase inhibitor treatment, and progression of aortic stenosis in the community. J. Am. Coll. Cardiol. 2002;40:1723–1730. doi: 10.1016/S0735-1097(02)02496-8. [DOI] [PubMed] [Google Scholar]
- 25.Moura L.M., Ramos S.F., Zamorano J.L., Barros I.M., Azevedo L.F., Rocha-Gonçalves F., Rajamannan N.M. Rosuvastatin Affecting Aortic Valve Endothelium to Slow the Progression of Aortic Stenosis. J. Am. Coll. Cardiol. 2007;49:554–561. doi: 10.1016/j.jacc.2006.07.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cowell S.J., Newby D.E., Prescott R.J., Bloomfield P., Reid J., Northridge D.B., Boon N.A. A Randomized Trial of Intensive Lipid-Lowering Therapy in Calcific Aortic Stenosis. N. Engl. J. Med. 2005;352:2389–2397. doi: 10.1056/NEJMoa043876. [DOI] [PubMed] [Google Scholar]
- 27.Dichtl W., Alber H.F., Feuchtner G.M., Hintringer F., Reinthaler M., Bartel T., Süssenbacher A., Grander W., Ulmer H., Pachinger O., et al. Prognosis and Risk Factors in Patients With Asymptomatic Aortic Stenosis and Their Modulation by Atorvastatin (20 mg) Am. J. Cardiol. 2008;102:743–748. doi: 10.1016/j.amjcard.2008.04.060. [DOI] [PubMed] [Google Scholar]
- 28.Chan K.L., Teo K., Dumesnil J.G., Ni A., Tam J. Effect of Lipid Lowering With Rosuvastatin on Progression of Aortic Stenosis. Circulation. 2010;121:306–314. doi: 10.1161/CIRCULATIONAHA.109.900027. [DOI] [PubMed] [Google Scholar]
- 29.Van Der Linde D., Yap S.C., Van Dijk A.P.J., Budts W., Pieper P.G., van der Burgh P.H., Mulder B.J., Witsenburg M., Cuypers J.A., Lindemans J., et al. Effects of rosuvastatin on progression of stenosis in adult patients with congenital aortic stenosis (PROCAS Trial) Am. J. Cardiol. 2011;108:265–271. doi: 10.1016/j.amjcard.2011.03.032. [DOI] [PubMed] [Google Scholar]
- 30.Rossebø A.B., Pedersen T.R., Boman K., Brudi P., Chambers J.B., Egstrup K., Gerdts E., Gohlke-Bärwolf C., Holme I., Kesäniemi Y.A., et al. Intensive Lipid Lowering with Simvastatin and Ezetimibe in Aortic Stenosis. N. Engl. J. Med. 2008;359:1343–1356. doi: 10.1056/NEJMoa0804602. [DOI] [PubMed] [Google Scholar]
- 31.Teo K.K., Corsi D.J., Tam J.W., Dumesnil J.G., Chan K.L. Lipid Lowering on Progression of Mild to Moderate Aortic Stenosis: Meta-analysis of the Randomized Placebo-Controlled Clinical Trials on 2344 Patients. Can. J. Cardiol. 2011;27:800–808. doi: 10.1016/j.cjca.2011.03.012. [DOI] [PubMed] [Google Scholar]
- 32.Parolari A., Tremoli E., Cavallotti L., Trezzi M., Kassem S., Loardi C., Veglia F., Ferrari G., Pacini D., Alamanni F. Do statins improve outcomes and delay the progression of non-rheumatic calcific aortic stenosis? Heart. 2011;97:523–529. doi: 10.1136/hrt.2010.215046. [DOI] [PubMed] [Google Scholar]
- 33.Arsenault B.J., Boekholdt S.M., Mora S., DeMicco D.A., Bao W., Tardif J.C., Amarenco P., Pedersen T., Barter P., Waters D.D. Impact of high-dose atorvastatin therapy and clinical risk factors on incident aortic valve stenosis in patients with cardiovascular disease (from TNT, IDEAL, and SPARCL) Am. J. Cardiol. 2014;113:1378–1382. doi: 10.1016/j.amjcard.2014.01.414. [DOI] [PubMed] [Google Scholar]
- 34.Nishimura R.A., Otto C.M., Bonow R.O., Carabello B.A., Erwin J.P., Guyton R.A., O’Gara P.T., Ruiz C.E., Skubas N.J., Sorajja P., et al. 2014 AHA/ACC Guideline for the Management of Patients with Valvular Heart Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129:2440–2492. doi: 10.1161/CIR.0000000000000029. [DOI] [PubMed] [Google Scholar]
- 35.Baumgartner H., Falk V., Bax J.J., De Bonis M., Hamm C., Holm P.J., Iung B., Lancellotti P., Lansac E., Rodriguez Muñoz D., et al. 2017 ESC/EACTS Guidelines for the Management of Valvular Heart Disease. Eur. Heart J. 2017;38:2739–2791. doi: 10.1093/eurheartj/ehx391. [DOI] [PubMed] [Google Scholar]
- 36.Greve A.M., Bang C.N., Boman K., Egstrup K., Kesäniemi Y.A., Ray S., Pedersen T.R., Wachtell K. Relation of Lipid-Lowering Therapy to Need for Aortic Valve Replacement in Patients With Asymptomatic Mild to Moderate Aortic Stenosis. Am. J. Cardiol. 2019;124:1736–1740. doi: 10.1016/j.amjcard.2019.08.037. [DOI] [PubMed] [Google Scholar]
- 37.Monzack E.L., Masters K.S. A time course investigation of the statin paradox among valvular interstitial cell phenotypes. Am. J. Physiol. Heart Circ. Physiol. 2012;303:903–909. doi: 10.1152/ajpheart.00263.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Thiago L., Tsuji S.R., Nyong J., Puga M.E., Gois A.F., Macedo C.R., Valente O., Atallah Á.N. Statins for aortic valve stenosis. Cochrane Database Syst. Rev. 2016 doi: 10.1002/14651858.CD009571.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. NCT02679261. Evaluating the Effectiveness of Atorvastatin on the Progression of Aortic Dilatation and Valvular Degeneration in Patients With Bicuspid Aortic Valve. [(accessed on 6 October 2020)]; Available online: https://clinicaltrials.gov/show/nct02679261.
- 40.Borrelli M.J., Youssef A., Boffa M.B., Koschinsky M.L. New Frontiers in Lp(a)-Targeted Therapies. Trends Pharmacol. Sci. 2019;40:212–225. doi: 10.1016/j.tips.2019.01.004. [DOI] [PubMed] [Google Scholar]
- 41.Torzewski M., Ravandi A., Yeang C., Yeang C., Edel A., Bhindi R., Kath S., Twardowski L., Schmid J., Yang X., et al. Lipoprotein(a)-Associated Molecules Are Prominent Components in Plasma and Valve Leaflets in Calcific Aortic Valve Stenosis. JACC Basic Transl. Sci. 2017;2:229–240. doi: 10.1016/j.jacbts.2017.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zheng K.H., Tsimikas S., Pawade T., Kroon J., Jenkins W.S.A., Doris M.K., White A.C., Timmers N.K.L.M., Hjortnaes J., Rogers M.A., et al. Lipoprotein(a) and Oxidized Phospholipids Promote Valve Calcification in Patients With Aortic Stenosis. J. Am. Coll. Cardiol. 2019;73:2150–2162. doi: 10.1016/j.jacc.2019.01.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ozkan U., Ozcelik F., Yildiz M., Budak M. Lipoprotein(a) Gene Polymorphism Increases a Risk Factor for Aortic Valve Calcification. J. Cardiovasc. Dev. Dis. 2019;6:31. doi: 10.3390/jcdd6030031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chen H.Y., Dufresne L., Burr H., Ambikkumar A., Yasui N., Luk K., Ranatunga D.K., Whitmer R.A., Lathrop M., Engert J.C., et al. Association of LPA variants with aortic stenosis a large-scale study using diagnostic and procedural codes from electronic health records. JAMA Cardiol. 2018;3:18–23. doi: 10.1001/jamacardio.2017.4266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Després A.A., Perrot N., Poulin A., Tastet L., Shen M., Chen H.Y., Bourgeois R., Trottier M., Tessier M., Guimond J., et al. Lipoprotein(a), Oxidized Phospholipids, and Aortic Valve Microcalcification Assessed by 18F-Sodium Fluoride Positron Emission Tomography and Computed Tomography. CJC Open. 2019;1:131–140. doi: 10.1016/j.cjco.2019.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Capoulade R., Yeang C., Chan K.L., Pibarot P., Tsimikas S. Association of Mild to Moderate Aortic Valve Stenosis Progression with Higher Lipoprotein(a) and Oxidized Phospholipid Levels: Secondary Analysis of a Randomized Clinical Trial. JAMA Cardiol. 2018;3:1212–1217. doi: 10.1001/jamacardio.2018.3798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mach F., Baigent C., Catapano A.L., Koskinas K.C., Casula M., Badimon L., Chapman M.J., De Backer G.G., Delgrado V., Ference B.A., et al. 2019 ESC/EAS guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk. Atherosclerosis. 2019;290:140–205. doi: 10.1016/j.atherosclerosis.2019.08.014. [DOI] [PubMed] [Google Scholar]
- 48.Wilson D.P., Jacobson T.A., Jones P.H., Koschinsky M.L., McNeal C.J., Nordestgaard B.G., Orringer C.E. Use of Lipoprotein(a) in clinical practice: A biomarker whose time has come. A scientific statement from the National Lipid Association. J. Clin. Lipidol. 2019;13:374–392. doi: 10.1016/j.jacl.2019.04.010. [DOI] [PubMed] [Google Scholar]
- 49.Yeang C., Hung M.Y., Byun Y.S., Clopton P., Yang X., Witztum J.L., Tsimikas S. Effect of therapeutic interventions on oxidized phospholipids on apolipoprotein B100 and lipoprotein(a) J. Clin. Lipidol. 2016;10:594–603. doi: 10.1016/j.jacl.2016.01.005. [DOI] [PubMed] [Google Scholar]
- 50.Sahebkar A., Reiner Ž., Simental-Mendía L.E., Ferretti G., Cicero A.F.G. Effect of extended-release niacin on plasma lipoprotein(a) levels: A systematic review and meta-analysis of randomized placebo-controlled trials. Metabolism. 2016;65:1664–1678. doi: 10.1016/j.metabol.2016.08.007. [DOI] [PubMed] [Google Scholar]
- 51.Landray M.J., Haynes R., Hopewell J.C., Parish S., Aung T., Tomson J., Wallendszus K., Craig M., Jiang L., Collins R., et al. Effects of extended-release niacin with laropiprant in high-risk patients. N. Engl. J. Med. 2014;371:203–212. doi: 10.1056/NEJMoa1300955. [DOI] [PubMed] [Google Scholar]
- 52.Boden W.E., Probstfield J.L., Anderson T., Chaitman B.R., Desvignes-Nickens P., Koprowicz K., McBride R., Teo K., Weintraub W. Niacin in patients with low HDL cholesterol levels receiving intensive statin therapy. N. Engl. J. Med. 2011;371:203–212. doi: 10.1056/NEJMoa1107579. [DOI] [PubMed] [Google Scholar]
- 53.Langsted A., Nordestgaard B.G. Antisense Oligonucleotides Targeting Lipoprotein(a) Curr. Atheroscler. Rep. 2019;21:30. doi: 10.1007/s11883-019-0792-8. [DOI] [PubMed] [Google Scholar]
- 54.Tsimikas S. Potential Causality and Emerging Medical Therapies for Lipoprotein(a) and Its Associated Oxidized Phospholipids in Calcific Aortic Valve Stenosis. Circ. Res. 2019;124:405–415. doi: 10.1161/CIRCRESAHA.118.313864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Leibundgut G., Scipione C., Yin H., Schneider M., Boffa M.B., Green S., Yang X., Dennis E., Witztum J.L., Koschinsky M.L., et al. Determinants of binding of oxidized phospholipids on apolipoprotein (a) and lipoprotein (a) J. Lipid Res. 2013;54:2815–2830. doi: 10.1194/jlr.M040733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tsimikas S., Willeit P., Willeit J., Santer P., Mayr M., Xu Q., Mayr A., Witztum J.L., Kiechl S. Oxidation-specific biomarkers, prospective 15-year cardiovascular and stroke outcomes, and net reclassification of cardiovascular events. J. Am. Coll. Cardiol. 2012;60:2218–2229. doi: 10.1016/j.jacc.2012.08.979. [DOI] [PubMed] [Google Scholar]
- 57.Capoulade R., Chan K.L., Yeang C., Mathieu P., Bossé Y., Dumesnil J.G., Tam J.W., Teo K.K., Mahmut A., Yang X., et al. Oxidized phospholipids, lipoprotein(a), and progression of calcific aortic valve stenosis. J. Am. Coll. Cardiol. 2015;66:1236–1246. doi: 10.1016/j.jacc.2015.07.020. [DOI] [PubMed] [Google Scholar]
- 58.Que X., Hung M.Y., Yeang C., Gonen A., Prohaska T.A., Sun X., Diehl C., Määttä A., Gaddis D.E., Bowden K., et al. Oxidized phospholipids are proinflammatory and proatherogenic in hypercholesterolaemic mice. Nature. 2018;558:301–306. doi: 10.1038/s41586-018-0198-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Mahmut A., Boulanger M.C., El Husseini D., Fournier D., Bouchareb R., Després J.P., Pibarot P., Bossé Y., Mathieu P. Elevated expression of lipoprotein-associated phospholipase A2 in calcific aortic valve disease: Implications for valve mineralization. J. Am. Coll. Cardiol. 2014;63:460–469. doi: 10.1016/j.jacc.2013.05.105. [DOI] [PubMed] [Google Scholar]
- 60.Bouchareb R., Mahmut A., Nsaibia M.J., Boulanger M.C., Dahou A., Lépine J.L., Laflamme M.H., Hadji F., Couture C., Trahan S., et al. Autotaxin derived from lipoprotein(a) and valve interstitial cells promotes inflammation and mineralization of the aortic valve. Circulation. 2015;132:677–690. doi: 10.1161/CIRCULATIONAHA.115.016757. [DOI] [PubMed] [Google Scholar]
- 61.Nsaibia M.J., Mahmut A., Boulanger M.C., Arsenault B.J., Bouchareb R., Simard S., Witztum J.L., Clavel M.A., Pibarot P., Bossé Y., et al. Autotaxin interacts with lipoprotein(a) and oxidized phospholipids in predicting the risk of calcific aortic valve stenosis in patients with coronary artery disease. J. Intern. Med. 2016;280:509–517. doi: 10.1111/joim.12519. [DOI] [PubMed] [Google Scholar]
- 62.Van der Aar E., Fagard L., Desrivot J., Dupont S., Heckmann B., Blanque R., Gheyle L., Ralic J., Vanhoutte F. Favorable human safety, pharmacokinetics and pharmacodynamics of the autotaxin inhibitor GLPG1690, a potential new treatment in COPD. Eur. Respir. J. 2015;304:OA484. doi: 10.1183/13993003.congress-2015.oa484. [DOI] [Google Scholar]
- 63.Maher T.M., van der Aar E.M., Van de Steen O., Allamassey L., Desrivot J., Dupont S., Fagard L., Ford P., Fieuw A., Wuyts W. Safety, tolerability, pharmacokinetics, and pharmacodynamics of GLPG1690, a novel autotaxin inhibitor, to treat idiopathic pulmonary fibrosis (FLORA): A phase 2a randomised placebo-controlled trial. Lancet Respir. Med. 2018;6:627–635. doi: 10.1016/S2213-2600(18)30181-4. [DOI] [PubMed] [Google Scholar]
- 64.Mathieu P., Boulanger M.C. Autotaxin and Lipoprotein Metabolism in Calcific Aortic Valve Disease. Front. Cardiovasc. Med. 2019;6:18. doi: 10.3389/fcvm.2019.00018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Bouchareb R., Boulanger M.C., Tastet L., Mkannez G., Nsaibia M.J., Hadji F., Dahou A., Messadeq Y., Arsenault B.J., Pibarot P., et al. Activated platelets promote an osteogenic programme and the progression of calcific aortic valve stenosis. Eur. Heart J. 2019;40:1362–1373. doi: 10.1093/eurheartj/ehy696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Capoulade R., Mahmut A., Tastet L., Arsenault M., Bédard É., Dumesnil J.G., Després J.P., Larose É., Arsenault B.J., Bossé Y., et al. Impact of plasma Lp-PLA2 activity on the progression of aortic stenosis: The PROGRESSA study. JACC Cardiovasc. Imaging. 2015;8:26–33. doi: 10.1016/j.jcmg.2014.09.016. [DOI] [PubMed] [Google Scholar]
- 67.Wihastuti T.A., Heriansyah T., Hanifa H., Andarini S., Sholichah Z., Sulfia Y.H., Adam A.A., Refialdinata J., Lutfiana N.C. Darapladib inhibits atherosclerosis development in type 2 diabetes mellitus Sprague-Dawley rat model. Endocr. Regul. 2018;52:69–75. doi: 10.2478/enr-2018-0008. [DOI] [PubMed] [Google Scholar]
- 68.Choi W.G., Prasad M., Lennon R., Gulati R., Prasad A., Lerman L.O., Lerman A. Long-term darapladib use does not affect coronary plaque composition assessed using multimodality intravascular imaging modalities: A randomized-controlled study. Coron Artery Dis. 2018;29:104. doi: 10.1097/MCA.0000000000000573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. NCT02109614. Early Aortic Valve Lipoprotein(a) Lowering Trial. [(accessed on 6 October 2020)]; Available online: https://clinicaltrials.gov/ct2/show/NCT02109614.
- 70. NCT03626662. Safety, Tolerability, Pharmacokinetics and Pharmacodynamics Study of AMG 890 in Subjects with Elevated Plasma Lipoprotein(a) [(accessed on 6 October 2020)]; Available online: https://clinicaltrials.gov/ct2/show/NCT03626662.
- 71. NCT04270760. Randomized Study to Evaluate Efficacy, Safety, and Tolerability of AMG 890 in Subjects With Elevated Lipoprotein(a) [(accessed on 6 October 2020)]; Available online: https://clinicaltrials.gov/ct2/show/NCT04270760.
- 72.Ferri N., Ruscica M., Coggi D., Bonomi A., Amato M., Frigerio B., Sansaro D., Ravani A., Veglia F., Capra N., et al. Sex-specific predictors of PCSK9 levels in a European population: The IMPROVE study. Atherosclerosis. 2020;309:39–46. doi: 10.1016/j.atherosclerosis.2020.07.014. [DOI] [PubMed] [Google Scholar]
- 73.Warden B.A., Fazio S., Shapiro M.D. The PCSK9 revolution: Current status, controversies, and future directions: The PCSK9 revolution. Trends Cardiovasc. Med. 2020;30:179–185. doi: 10.1016/j.tcm.2019.05.007. [DOI] [PubMed] [Google Scholar]
- 74.Wang W.G., He Y.F., Chen Y.L., Zhao F.M., Song Y.Q., Zhang H., Ma Y.H., Guan X., Zhang W.Y., Chen X.L., et al. Proprotein convertase subtilisin/kexin type 9 levels and aortic valve calcification: A prospective, cross sectional study. J. Int. Med. Res. 2016;44:865–874. doi: 10.1177/0300060516648030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Perrot N., Valerio V., Moschetta D., Boekholdt S.M., Dina C., Chen H.Y., Abner E., Martinsson A., Manikpurage H.D., Rigade S., et al. Genetic and In Vitro Inhibition of PCSK9 and Calcific Aortic Valve Stenosis. JACC Basic Transl. Sci. 2020;5:649–661. doi: 10.1016/j.jacbts.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Poggio P., Songia P., Cavallotti L., Barbieri S.S., Zanotti I., Arsenault B.J., Valerio V., Ferri N., Capoulade R., Camera M. PCSK9 Involvement in Aortic Valve Calcification. J. Am. Coll. Cardiol. 2018;72:3225–3227. doi: 10.1016/j.jacc.2018.09.063. [DOI] [PubMed] [Google Scholar]
- 77.Nissen S.E., Stroes E., Dent-Acosta R.E., Rosenson R.S., Lehman S.J., Sattar N., Preiss D., Bruckert E., Ceška R., Lepor N., et al. Efficacy and tolerability of evolocumab vs ezetimibe in patients with muscle-related statin intolerance: The GAUSS-3 randomized clinical trial. JAMA J. Am. Med. Assoc. 2016;315:1580–1590. doi: 10.1001/jama.2016.3608. [DOI] [PubMed] [Google Scholar]
- 78.Cho L., Dent R., Stroes E.S.G., Stein E.A., Sullivan D., Ruzza A., Flower A., Somaratne R., Rosenson R.S. Persistent Safety and Efficacy of Evolocumab in Patients with Statin Intolerance: A Subset Analysis of the OSLER Open-Label Extension Studies. Cardiovasc. Drugs Ther. 2018;32:365–372. doi: 10.1007/s10557-018-6817-7. [DOI] [PubMed] [Google Scholar]
- 79.O’Donoghue M.L., Fazio S., Giugliano R.P., Stroes E.S.G., Kanevsky E., Gouni-Berthold I., Im K., Lira Pineda A., Wasserman S.M., Češka R., et al. Lipoprotein(a), PCSK9 Inhibition, and Cardiovascular Risk. Circulation. 2019;139:1483–1492. doi: 10.1161/CIRCULATIONAHA.118.037184. [DOI] [PubMed] [Google Scholar]
- 80.Qamar A., Giugliano R.P., Keech A.C., Kuder J.F., Murphy S.A., Kurtz C.E., Wasserman S.M., Sever P.S., Pedersen T.R., Sabatine M.S. Interindividual Variation in Low-Density Lipoprotein Cholesterol Level Reduction with Evolocumab: An Analysis of FOURIER Trial Data. JAMA Cardiol. 2019;4:59–63. doi: 10.1001/jamacardio.2018.4178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Watts G.F., Chan D.C., Somaratne R., Wasserman S.M., Scott R., Marcovina S.M., Barrett P.H.R. Controlled study of the effect of proprotein convertase subtilisin-kexin type 9 inhibition with evolocumab on lipoprotein(a) particle kinetics. Eur. Heart J. 2018;39:2577–2585. doi: 10.1093/eurheartj/ehy122. [DOI] [PubMed] [Google Scholar]
- 82.Nicholls S.J., Puri R., Anderson T., Ballantyne C.M., Cho L., Kastelein J.J.P., Koenig W., Somaratne R., Kassahun H., Yang J., et al. Effect of Evolocumab on Coronary Plaque Composition. J. Am. Coll. Cardiol. 2018;72:2012–2021. doi: 10.1016/j.jacc.2018.06.078. [DOI] [PubMed] [Google Scholar]
- 83.Schwartz G.G., Steg P.G., Szarek M., Bhatt D.L., Bittner V.A., Diaz R., Edelberg J.M., Goodman S.G., Hanotin C., Harrington R.A., et al. Alirocumab and cardiovascular outcomes after acute coronary syndrome. N. Engl. J. Med. 2018;379:2097–2107. doi: 10.1056/NEJMoa1801174. [DOI] [PubMed] [Google Scholar]
- 84. NCT03051360. PCSK9 Inhibitors in the Progression of Aortic Stenosis. [(accessed on 6 October 2020)]; Available online: https://clinicaltrials.gov/show/NCT03051360.
- 85.Fitzgerald K., White S., Borodovsky A., Bettencourt B.R., Strahs A., Clausen V., Wijngaard P., Horton J.D., Taubel J., Brooks A., et al. A highly durable RNAi therapeutic inhibitor of PCSK9. N. Engl. J. Med. 2017;376:41–51. doi: 10.1056/NEJMoa1609243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Ray K.K., Wright R.S., Kallend D., Koenig W., Leiter L.A., Raal F.J., Bisch J.A., Richardson T., Jaros M., Wijngaard P.L.J., et al. Two Phase 3 Trials of Inclisiran in Patients with Elevated LDL Cholesterol. N. Engl. J. Med. 2020;382:1507–1519. doi: 10.1056/NEJMoa1912387. [DOI] [PubMed] [Google Scholar]
- 87.Raal F.J., Kallend D., Ray K.K., Turner T., Koenig W., Wright R.S., Wijngaard P.L.J., Curcio D., Jaros M.J., Leiter L.A., et al. Inclisiran for the Treatment of Heterozygous Familial Hypercholesterolemia. N. Engl. J. Med. 2020;382:1520–1530. doi: 10.1056/NEJMoa1913805. [DOI] [PubMed] [Google Scholar]
- 88.Antonini-Canterin F., Huang G., Cervesato E., Faggiano P., Pavan D., Piazza R., Nicolosi G.L. Symptomatic aortic stenosis: Does systemic hypertension play an additional role? Hypertension. 2003;41:1268–1272. doi: 10.1161/01.HYP.0000070029.30058.59. [DOI] [PubMed] [Google Scholar]
- 89.Arjunon S., Rathan S., Jo H., Yoganathan A.P. Aortic valve: Mechanical environment and mechanobiology. Ann. Biomed. Eng. 2013;41:1331–1346. doi: 10.1007/s10439-013-0785-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Rassa A., Zahr F. Hypertension and Aortic Stenosis: A Review. Curr. Hypertens Rev. 2018;14:6–14. doi: 10.2174/1573402114666180416161326. [DOI] [PubMed] [Google Scholar]
- 91.Capoulade R., Clavel M.A., Mathieu P., Côté N., Dumesnil J.G., Arsenault M., Bédard E., Pibarot P. Impact of hypertension and renin-angiotensin system inhibitors in aortic stenosis. Eur. J. Clin. Investig. 2013;43:1262–1272. doi: 10.1111/eci.12169. [DOI] [PubMed] [Google Scholar]
- 92.Poggio P., Folesani G., Raffa G.M., Songia P., Valenti V., Myasoedova V., Parolari A. Antihypertensive Treatments in Patients Affected by Aortic Valve Stenosis. Curr. Pharm. Des. 2017;23:1188–1194. doi: 10.2174/1381612823666161123144534. [DOI] [PubMed] [Google Scholar]
- 93.Lindman B.R., Otto C.M. Time to treat hypertension in patients with aortic stenosis. Circulation. 2013;128:1281–1283. doi: 10.1161/CIRCULATIONAHA.113.005275. [DOI] [PubMed] [Google Scholar]
- 94.Balakumar P., Jagadeesh G. A century old renin-angiotensin system still grows with endless possibilities: AT1 receptor signaling cascades in cardiovascular physiopathology. Cell Signal. 2014;26:2147–2160. doi: 10.1016/j.cellsig.2014.06.011. [DOI] [PubMed] [Google Scholar]
- 95.Xie C., Shen Y., Hu W., Chen Z., Li Y. Angiotensin II promotes an osteoblast-like phenotype in porcine aortic valve myofibroblasts. Aging Clin. Exp. Res. 2016;28:181–187. doi: 10.1007/s40520-015-0408-2. [DOI] [PubMed] [Google Scholar]
- 96.Ma F., Li Y., Jia L., Han Y., Cheng J., Li H., Qi Y., Du J. Macrophage-stimulated cardiac fibroblast production of IL-6 is essential for TGF β/Smad activation and cardiac fibrosis induced by angiotensin II. PLoS ONE. 2012;7:1–9. doi: 10.1371/journal.pone.0035144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Helske S., Lindstedt K.A., Laine M., Mäyränpää M., Werkkala K., Lommi J., Turto H., Kupari M., Kovanen P.T. Induction of local angiotensin II-producing systems in stenotic aortic valves. J. Am. Coll. Cardiol. 2004;44:1859–1866. doi: 10.1016/j.jacc.2004.07.054. [DOI] [PubMed] [Google Scholar]
- 98.O’Brien K.D., Shavelle D.M., Caulfield M.T., McDonald T.O., Olin-Lewis K., Otto C.M., Probstfield J.L. Association of angiotensin-converting enzyme with low-density lipoprotein in aortic valvular lesions and in human plasma. Circulation. 2002;106:2224–2230. doi: 10.1161/01.CIR.0000035655.45453.D2. [DOI] [PubMed] [Google Scholar]
- 99.Chockalingam A., Venkatesan S., Subramaniam T., Jagannathan V., Elangovan S., Alagesan R., Gnanavelu G., Dorairajan S., Krishna B.P., Chockalingam V. Safety and efficacy of angiotensin-converting enzyme inhibitors in symptomatic severe aortic stenosis: Symptomatic Cardiac Obstruction-Pilot Study of Enalapril in Aortic Stenosis (SCOPE-AS) Am. Heart J. 2004;147:740. doi: 10.1016/j.ahj.2003.10.017. [DOI] [PubMed] [Google Scholar]
- 100.O’Brien K.D., Zhao X.Q., Shavelle D.M., Caulfield M.T., Letterer R.A., Kapadia S.R., Probstfield J.L., Otto C.M. Hemodynamic effects of the angiotensin-converting enzyme inhibitor, ramipril, in patients with mild to moderate aortic stenosis and preserved left ventricular function. J. Investig. Med. 2004;52:185. doi: 10.1136/jim-52-03-33. [DOI] [PubMed] [Google Scholar]
- 101.Wakabayashi K., Tsujino T., Naito Y., Ezumi A., Lee-Kawabata M., Nakao S., Goda A., Sakata Y., Yamamoto K., Daimon T., et al. Administration of angiotensin-converting enzyme inhibitors is associated with slow progression of mild aortic stenosis in Japanese patients. Heart Vessels. 2011;26:252–257. doi: 10.1007/s00380-010-0052-x. [DOI] [PubMed] [Google Scholar]
- 102.Jiménez-Candil J., Bermejo J., Yotti R., Cortina C., Moreno M., Cantalapiedra J.L., García-Fernández M.A. Effects of angiotensin converting enzyme inhibitors in hypertensive patients with aortic valve stenosis: A drug withdrawal study. Heart. 2005;91:1311–1318. doi: 10.1136/hrt.2004.047233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Dalsgaard M., Iversen K., Kjaergaard J., Grande P., Goetze J.P., Clemmensen P., Hassager C. Short-term hemodynamic effect of angiotensin-converting enzyme inhibition in patients with severe aortic stenosis: A placebo-controlled, randomized study. Am. Heart J. 2014;167:226–234. doi: 10.1016/j.ahj.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 104.Bull S., Loudon M., Francis J.M., Joseph J., Gerry S., Karamitsos T.D., Prendergast B.D., Banning A.P., Neubauer S., Myerson S.G. A prospective, double-blind, randomized controlled trial of the angiotensin-converting enzyme inhibitor Ramipril in Aortic Stenosis (RIAS trial) Eur. Heart J. Cardiovasc. Imaging. 2015;16:834–841. doi: 10.1093/ehjci/jev043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Helske-Suihko S., Laine M., Lommi J., Kaartinen M., Werkkala K., Kovanen P.T., Kupari M. Is blockade of the renin-angiotensin system able to reverse the structural and functional remodeling of the left ventricle in severe aortic stenosis? J. Cardiovasc. Pharmacol. 2015;65:233–240. doi: 10.1097/FJC.0000000000000182. [DOI] [PubMed] [Google Scholar]
- 106.Côté N., Couture C., Pibarot P., Després J.P., Mathieu P. Angiotensin receptor blockers are associated with a lower remodelling score of stenotic aortic valves. Eur. J. Clin. Investig. 2011;41:1172–1179. doi: 10.1111/j.1365-2362.2011.02522.x. [DOI] [PubMed] [Google Scholar]
- 107.Côté N., Mahmut A., Fournier D., Boulanger M.C., Couture C., Després J.P., Trahan S., Bossé Y., Pagé S., Pibarot P., et al. Angiotensin receptor blockers are associated with reduced fibrosis and interleukin-6 expression in calcific aortic valve disease. Pathobiology. 2013;81:15–24. doi: 10.1159/000350896. [DOI] [PubMed] [Google Scholar]
- 108.Nadir M.A., Wei L., Elder D.H.J., Libianto R., Lim T.K., Pauriah M., Pringle S.D., Doney A.D., Choy A.M., Struthers A.D., et al. Impact of renin-angiotensin system blockade therapy on outcome in aortic stenosis. J. Am. Coll. Cardiol. 2011;58:570–576. doi: 10.1016/j.jacc.2011.01.063. [DOI] [PubMed] [Google Scholar]
- 109.Bang C.N., Greve A.M., Køber L., Rossebø A.B., Ray S., Boman K., Nienaber C.A., Devereux R.B., Wachtell K. Renin-angiotensin system inhibition is not associated with increased sudden cardiac death, cardiovascular mortality or all-cause mortality in patients with aortic stenosis. Int. J. Cardiol. 2014;175:492–498. doi: 10.1016/j.ijcard.2014.06.013. [DOI] [PubMed] [Google Scholar]
- 110.Yamamoto K., Yamamoto H., Takeuchi M., Kisanuki A., Akasaka T., Ohte N., Hirano Y., Yoshida K., Nakatani S., Takeda Y., et al. Risk factors for progression of degenerative aortic valve disease in the Japanese—The Japanese aortic stenosis study (JASS) prospective analysis. Circ. J. 2015;79:2050–2057. doi: 10.1253/circj.CJ-15-0499. [DOI] [PubMed] [Google Scholar]
- 111. NCT01589380. A Randomized Trial of Angiotensin Receptor bLocker, Fimasartan, in Aortic Stenosis (ALFA Trial) [(accessed on 6 October 2020)]; Available online: https://clinicaltrials.gov/show/nct01589380.
- 112. NCT03666351. Study to Evaluate the Effect on Improvement of LVH by the Control of BP in Hypertension Patients With AV Disease. [(accessed on 6 October 2020)]; Available online: https://clinicaltrials.gov/ct2/show/NCT03666351.
- 113.Andersson C., Abdulla J. Is the use of renin-angiotensin systeminhibitors in patients with aortic valve stenosis safe and of prognostic benefit? A systematic review and meta-analysis. Eur. Heart J. Cardiovasc. Pharmacother. 2017;3:21–27. doi: 10.1093/ehjcvp/pvw027. [DOI] [PubMed] [Google Scholar]
- 114.Magne J., Guinot B., Le Guyader A., Bégot E., Marsaud J.P., Mohty D., Aboyans V. Relation Between Renin-Angiotensin System Blockers and Survival Following Isolated Aortic Valve Replacement for Aortic Stenosis. Am. J. Cardiol. 2018;121:455–460. doi: 10.1016/j.amjcard.2017.11.013. [DOI] [PubMed] [Google Scholar]
- 115.Rodriguez-Gabella T., Catalá P., Muñoz-García A.J., Nombela-Franco L., Del Valle R., Gutiérrez E., Regueiro A., Jimenez-Diaz V.A., Ribeiro H.B., Rivero F., et al. Renin-Angiotensin System Inhibition Following Transcatheter Aortic Valve Replacement. J. Am. Coll. Cardiol. 2019;74:631–641. doi: 10.1016/j.jacc.2019.05.055. [DOI] [PubMed] [Google Scholar]
- 116.Chen S., Redfors B., Nazif T., Kirtane A., Crowley A., Ben-Yehuda O., Kapadia S., Finn M.T., Goel S., Lindman B.R., et al. Impact of renin-angiotensin systeminhibitors on clinical outcomes in patients with severe aortic stenosis undergoing transcatheter aortic valve replacement: An analysis of from the PARTNER 2 trial and registries. Eur. Heart J. 2020;41:943–954. doi: 10.1093/eurheartj/ehz769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. NCT03315832. Efficacy of Angiotensin Receptor Blocker Following aortIc Valve Intervention for Aortic STenOsis: A Randomized mulTi-cEntric Double-blind Phase II Study. [(accessed on 6 October 2020)]; Available online: https://clinicaltrials.gov/show/NCT03315832.
- 118.Wang P., Quan Z., Luo D., Chen W., Peng D. Spironolactone dose-dependently alleviates the calcification of aortic rings cultured in hyperphosphatemic medium with or without hyperglycemia by suppressing phenotypic transition of VSMCs through downregulation of Pit-1. Mol. Med. Rep. 2019;49:3622–3632. doi: 10.3892/mmr.2019.10039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Zhu D., Rashdan N.A., Chapman K.E., Hadoke P.W., MacRae V.E. A novel role for the mineralocorticoid receptor in glucocorticoid driven vascular calcification. Vasc. Pharmacol. 2016;86:87–93. doi: 10.1016/j.vph.2016.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Rajagopalan S., Duquaine D., King S., Pitt B., Patel P. Mineralocorticoid receptor antagonism in experimental atherosclerosis. Circulation. 2002;105:2212–2216. doi: 10.1161/01.CIR.0000015854.60710.10. [DOI] [PubMed] [Google Scholar]
- 121.Pitt B., Reichek N., Willenbrock R., Zannad F., Phillips R.A., Roniker B., Kleiman J., Krause S., Burns D., Williams G.H. Effects of Eplerenone, Enalapril, and Eplerenone/Enalapril in Patients with Essential Hypertension and Left Ventricular Hypertrophy: The 4E-Left Ventricular Hypertrophy Study. Circulation. 2003;108:1831–1838. doi: 10.1161/01.CIR.0000091405.00772.6E. [DOI] [PubMed] [Google Scholar]
- 122.Jolobe O.M.P. Evolving strategies for the use of spironolactone in cardiovascular disease. Eur. J. Intern. Med. 2013;24:303–309. doi: 10.1016/j.ejim.2012.11.007. [DOI] [PubMed] [Google Scholar]
- 123.Gkizas S., Koumoundourou D., Sirinian X., Rokidi S., Mavrilas D., Koutsoukos P., Papalois A., Apostolakis E., Alexopoulos D., Papadaki H. Aldosterone receptor blockade inhibits degenerative processes in the early stage of calcific aortic stenosis. Eur. J. Pharmacol. 2010;642:107–112. doi: 10.1016/j.ejphar.2010.05.048. [DOI] [PubMed] [Google Scholar]
- 124.Stewart R.A.H., Kerr A.J., Cowan B.R., Young A.A., Occleshaw C., Richards A.M., Edwards C., Whalley G.A., Freidlander D., Williams M., et al. A randomized trial of the aldosterone-receptor antagonist eplerenone in asymptomatic moderate-severe aortic stenosis. Am. Heart J. 2008;156:348–355. doi: 10.1016/j.ahj.2008.03.012. [DOI] [PubMed] [Google Scholar]
- 125. NCT03923530. Pressure Assessment to Improve Outcomes After TAVR: A Registry. [(accessed on 6 October 2020)]; Available online: https://clinicaltrials.gov/ct2/show/NCT03923530.
- 126.Bosse K., Hans C.P., Zhao N., Koenig S.N., Huang N., Guggilam A., LaHaye S., Tao G., Lucchesi P.A., Lincoln J., et al. Endothelial nitric oxide signaling regulates Notch1 in aortic valve disease. J. Mol. Cell Cardiol. 2013;60:27–35. doi: 10.1016/j.yjmcc.2013.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Miller J.D., Chu Y., Brooks R.M., Richenbacher W.E., Peña-Silva R., Heistad D.D. Dysregulation of Antioxidant Mechanisms Contributes to Increased Oxidative Stress in Calcific Aortic Valvular Stenosis in Humans. J. Am. Coll. Cardiol. 2008;52:843–850. doi: 10.1016/j.jacc.2008.05.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Bertacco E., Renato M., Arrigoni G., Faggin E., Iop L., Puato M., Tessari P., Pauletto P., Rattazzi M. Proteomic analysis of clonal interstitial aortic valve cells acquiring a pro-calcific profile. J. Proteome Res. 2010;9:5913–5921. doi: 10.1021/pr100682g. [DOI] [PubMed] [Google Scholar]
- 129.Kennedy J.A., Hua X., Mishra K., Murphy G.A., Rosenkranz A.C., Horowitz J.D. Inhibition of calcifying nodule formation in cultured porcine aortic valve cells by nitric oxide donors. Eur. J. Pharmacol. 2009;602:28–35. doi: 10.1016/j.ejphar.2008.11.029. [DOI] [PubMed] [Google Scholar]
- 130.Richards J., El-Hamamsy I., Chen S., Sarang Z., Sarathchandra P., Yacoub M.H., Chester A.H., Butcher J.T. Side-specific endothelial-dependent regulation of aortic valve calcification: Interplay of hemodynamics and nitric oxide signaling. Am. J. Pathol. 2013;182:1922–1931. doi: 10.1016/j.ajpath.2013.01.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Rattazzi M., Donato M., Bertacco E., Millioni R., Franchin C., Mortarino C., Faggin E., Nardin C., Scarpa R., Cinetto F., et al. L-Arginine prevents inflammatory and pro-calcific differentiation of interstitial aortic valve cells. Atherosclerosis. 2020;298:27–35. doi: 10.1016/j.atherosclerosis.2020.02.024. [DOI] [PubMed] [Google Scholar]
- 132.Claveau D., Piha-Gossack A., Friedland S.N., Afilalo J., Rudski L. Complications Associated with Nitrate Use in Patients Presenting with Acute Pulmonary Edema and Concomitant Moderate or Severe Aortic Stenosis. Ann. Emerg. Med. 2015;66:355–362.e1. doi: 10.1016/j.annemergmed.2015.03.027. [DOI] [PubMed] [Google Scholar]
- 133.Lloyd J.W., Nishimura R.A., Borlaug B.A., Eleid M.F. Hemodynamic Response to Nitroprusside in Patients With Low-Gradient Severe Aortic Stenosis and Preserved Ejection Fraction. J. Am. Coll. Cardiol. 2017;70:1339–1348. doi: 10.1016/j.jacc.2017.07.736. [DOI] [PubMed] [Google Scholar]
- 134.Lewis G.D., Shah R., Shahzad K., Camuso J.M., Pappagianopoulos P.P., Hung J., Tawakol A., Gerszten R.E., Systrom D.M., Bloch K.D., et al. Sildenafil improves exercise capacity and quality of life in patients with systolic heart failure and secondary pulmonary hypertension. Circulation. 2007;116:1555–1562. doi: 10.1161/CIRCULATIONAHA.107.716373. [DOI] [PubMed] [Google Scholar]
- 135.Zhuang X.D., Long M., Li F., Hu X., Liao X.X., Du Z.M. PDE5 inhibitor sildenafil in the treatment of heart failure: A meta-analysis of randomized controlled trials. Int. J. Cardiol. 2014;172:581–587. doi: 10.1016/j.ijcard.2014.01.102. [DOI] [PubMed] [Google Scholar]
- 136.Vandenwijngaert S., Pokreisz P., Hermans H., Gillijns H., Pellens M., Bax N.A., Coppiello G., Oosterlinck W., Balogh A., Papp Z., et al. Increased Cardiac Myocyte PDE5 Levels in Human and Murine Pressure Overload Hypertrophy Contribute to Adverse LV Remodeling. PLoS ONE. 2013;8:e58841. doi: 10.1371/journal.pone.0058841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137. NCT01275339. Aortic Stenosis and PhosphodiEsterase Type 5 iNhibition (ASPEN): A Pilot Study. [(accessed on 6 October 2020)]; Available online: https://ClinicalTrials.gov/show/NCT01275339.
- 138.Lindman B.R., Zajarias A., Madrazo J.A., Shah J., Gage B.F., Novak E., Johnson S.N., Chakinala M.M., Hohn T.A., Saghir M., et al. Effects of phosphodiesterase type 5 inhibition on systemic and pulmonary hemodynamics and ventricular function in patients with severe symptomatic aortic stenosis. Circulation. 2012;125:2353–2362. doi: 10.1161/CIRCULATIONAHA.111.081125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Martinelli A., Rodrigues C., Moraes T., Rodrigues G. In Endothelial Cells, the Activation or Stimulation of Soluble Guanylyl Cyclase Induces the Nitric Oxide Production by a Mechanism Dependent of Nitric Oxide Synthase Activation. J. Pharm. Pharm. Sci. 2018;21:38–45. doi: 10.18433/jpps29578. [DOI] [PubMed] [Google Scholar]
- 140.Schäfer A., Fraccarollo D., Werner L., Bauersachs J. Guanylyl cyclase activator ataciguat improves vascular function and reduces platelet activation in heart failure. Pharmacol. Res. 2010;62:432–438. doi: 10.1016/j.phrs.2010.06.008. [DOI] [PubMed] [Google Scholar]
- 141.Weissmann N., Hackemack S., Dahal B.K., Pullamsetti S.S., Savai R., Mittal M., Fuchs B., Medebach T., Dumitrascu R., Eickels M.V., et al. The soluble guanylate cyclase activator HMR1766 reverses hypoxia-induced experimental pulmonary hypertension in mice. Am. J. Physiol. Lung Cell Mol. Physiol. 2009;297:658–665. doi: 10.1152/ajplung.00189.2009. [DOI] [PubMed] [Google Scholar]
- 142. NCT02049203. Safety of Ataciguat in Patients with Moderate Calcific Aortic Valve Stenosis. [(accessed on 6 October 2020)]; Available online: https://clinicaltrials.gov/show/nct02049203.
- 143. NCT02481258. A Study Evaluating the Effects of Ataciguat (HMR1766) on Aortic Valve Calcification. [(accessed on 6 October 2020)]; Available online: https://clinicaltrials.gov/show/nct02481258.
- 144.Weiss R.M., Lund D.D., Chu Y., Brooks R.M., Zimmerman K.A., El Accaoui R., Davis M.K., Hajj G.P., Zimmerman M.B., Heistad D.D. Osteoprotegerin Inhibits Aortic Valve Calcification and Preserves Valve Function in Hypercholesterolemic Mice. PLoS ONE. 2013;8:e65201. doi: 10.1371/journal.pone.0065201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Bucay N., Sarosi I., Dunstan C.R., Morony S., Tarpley J., Capparelli C., Scully S., Tan H.L., Xu W., Lacey D.L., et al. Osteoprotegerin-deficient mice develop early onset osteoporosis and arterial calcification. Genes Dev. 1998;12:1260–1268. doi: 10.1101/gad.12.9.1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Buso G., Faggin E., Pauletto P., Rattazzi M. Osteoprotegerin in Cardiovascular Disease: Ally or Enemy? Curr. Pharm. Des. 2014;20:5862–5869. doi: 10.2174/1381612820666140212195711. [DOI] [PubMed] [Google Scholar]
- 147.Rattazzi M., Faggin E., Bertacco E., Buso R., Puato M., Plebani M., Zaninotto M., Condotta D., Zoppellaro G., Tarantini G., et al. RANKL Expression Is Increased in Circulating Mononuclear Cells of Patients with Calcific Aortic Stenosis. J. Cardiovasc. Transl. Res. 2018;11:329–338. doi: 10.1007/s12265-018-9804-2. [DOI] [PubMed] [Google Scholar]
- 148.Persy V., D’Haese P. Vascular calcification and bone disease: The calcification paradox. Trends Mol. Med. 2009;15:405–416. doi: 10.1016/j.molmed.2009.07.001. [DOI] [PubMed] [Google Scholar]
- 149.Pfister R., Michels G., Sharp S.J., Luben R., Wareham N.J., Khaw K.T. Inverse association between bone mineral density and risk of aortic stenosis in men and women in EPIC-Norfolk prospective study. Int. J. Cardiol. 2015;178:29–30. doi: 10.1016/j.ijcard.2014.10.065. [DOI] [PubMed] [Google Scholar]
- 150.Helas S., Goettsch C., Schoppet M., Zeitz U., Hempel U., Morawietz H., Kostenuik P.J., Erben R.G., Hofbauer L.C. Inhibition of receptor activator of NF-κB ligand by denosumab attenuates vascular calcium deposition in mice. Am. J. Pathol. 2009;175:473–478. doi: 10.2353/ajpath.2009.080957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Lerman D.A., Prasad S., Alotti N. Denosumab could be a Potential Inhibitor of Valvular Interstitial Cells Calcification in vitro. Int. J. Cardiovasc. Res. 2015;5:1–19. doi: 10.4172/2324-8602.1000249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Elmariah S., Cimmino G., Fuster V., Badimon J.J. Bisphosphonates Prevent Oxidized Low-Density Lipoprotein-Induced Expression of Osteogenic Markers in Aortic Valve Myofibroblasts. J. Am. Coll. Cardiol. 2010;55:A149–E1398. doi: 10.1016/S0735-1097(10)61399-X. [DOI] [Google Scholar]
- 153.Price P.A., Faus S.A., Williamson M.K. Bisphosphonates alendronate and ibandronate inhibit artery calcification at doses comparable to those that inhibit bone resorption. Arterioscler. Thromb Vasc. Biol. 2001;21:817–824. doi: 10.1161/01.ATV.21.5.817. [DOI] [PubMed] [Google Scholar]
- 154.Synetos A., Toutouzas K., Drakopoulou M., Koutagiar I., Benetos G., Kotronias R., Anousakis-Vlachochristou N., Latsios G., Karanasos A., Agrogiannis G., et al. Inhibition of Aortic Valve Calcification by Local Delivery of Zoledronic Acid—An Experimental Study. J. Cardiovasc. Transl. Res. 2018;11:192–200. doi: 10.1007/s12265-018-9802-4. [DOI] [PubMed] [Google Scholar]
- 155.Corrado A., Santoro N., Cantatore F.P. Extra-skeletal effects of bisphosphonates. Jt. Bone Spine. 2007;74:32–38. doi: 10.1016/j.jbspin.2006.06.005. [DOI] [PubMed] [Google Scholar]
- 156.Hashiba H., Aizawa S., Tamura K., Kogo H. Inhibition of the progression of aortic calcification by etidronate treatment in hemodialysis patients: Long-term effects. Ther. Apher. Dial. 2006;10:59–64. doi: 10.1111/j.1744-9987.2006.00345.x. [DOI] [PubMed] [Google Scholar]
- 157.Ariyoshi T., Eishi K., Sakamoto I., Matsukuma S., Odate T. Effect of etidronic acid on arterial calcification in dialysis patients. Clin. Drug Investig. 2006;26:215–222. doi: 10.2165/00044011-200626040-00006. [DOI] [PubMed] [Google Scholar]
- 158.Elmariah S., Delaney J.A.C., O’Brien K.D., Budoff M.J., Vogel-Claussen J., Fuster V., Kronmal R.A., Halperin J.L. Bisphosphonate use and prevalence of valvular and vascular calcification in women: MESA (The Multi-Ethnic Study of Atherosclerosis) J. Am. Coll. Cardiol. 2010;56:1752–1759. doi: 10.1016/j.jacc.2010.05.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Innasimuthu A.L., Katz W.E. Effect of bisphosphonates on the progression of degenerative aortic stenosis. Echocardiography. 2011;28:1–7. doi: 10.1111/j.1540-8175.2010.01256.x. [DOI] [PubMed] [Google Scholar]
- 160.Sterbakova G., Vyskocil V., Linhartova K. Bisphosphonates in calcific aortic stenosis: Association with slower progression in mild disease—A pilot retrospective study. Cardiology. 2011;117:184–189. doi: 10.1159/000321418. [DOI] [PubMed] [Google Scholar]
- 161.Aksoy O., Cam A., Goel S.S., Houghtaling P.L., Williams S., Ruiz-Rodriguez E., Menon V., Kapadia S.R., Tuzcu E.M., Blackstone E.H., et al. Do bisphosphonates slow the progression of aortic stenosis? J. Am. Coll. Cardiol. 2012;59:1452–1459. doi: 10.1016/j.jacc.2012.01.024. [DOI] [PubMed] [Google Scholar]
- 162.Dweck M.R., Newby D.E. Osteoporosis is a major confounder in observational studies investigating bisphosphonate therapyin aortic stenosis. J. Am. Coll. Cardiol. 2012;60:1027. doi: 10.1016/j.jacc.2012.04.048. [DOI] [PubMed] [Google Scholar]
- 163. NCT02132026. Study Investigating the Effect of Drugs Used to Treat Osteoporosis on the Progression of Calcific Aortic Stenosis. [(accessed on 6 October 2020)]; Available online: https://clinicaltrials.gov/ct2/show/NCT02132026.
- 164.Schurgers L.J., Uitto J., Reutelingsperger C.P. Vitamin K-dependent carboxylation of matrix Gla-protein: A crucial switch to control ectopic mineralization. Trends Mol. Med. 2013;19:217–226. doi: 10.1016/j.molmed.2012.12.008. [DOI] [PubMed] [Google Scholar]
- 165.Zebboudj A.F., Imura M., Boström K. Matrix GLA protein, a regulatory protein for bone morphogenetic protein-2. J. Biol. Chem. 2002;277:4388–4394. doi: 10.1074/jbc.M109683200. [DOI] [PubMed] [Google Scholar]
- 166.Chiyoya M., Seya K., Yu Z., Daitoku K., Motomura S., Imaizumi T., Fukuda I., Furukawa K.I. Matrix Gla protein negatively regulates calcification of human aortic valve interstitial cells isolated from calcified aortic valves. J. Pharmacol. Sci. 2018;136:257–265. doi: 10.1016/j.jphs.2018.03.004. [DOI] [PubMed] [Google Scholar]
- 167.Luo G., Ducy P., McKee M.D., Pinero G.J., Loyer E., Behringer R.R., Karsenty G. Spontaneous calcification of arteries and cartilage in mice lacking matrix GLA protien. Nature. 1997;386:78–81. doi: 10.1038/386078a0. [DOI] [PubMed] [Google Scholar]
- 168.Venardos N., Bennett D., Weyant M.J., Reece T.B., Meng X., Fullerton D.A. Matrix Gla protein regulates calcification of the aortic valve. J. Surg. Res. 2015;199:1–6. doi: 10.1016/j.jss.2015.04.076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Schurgers L.J., Cranenburg E.C.M., Vermeer C. Matrix Gla-protein: The calcification inhibitor in need of vitamin K. Thromb. Haemost. 2008;100:593–603. doi: 10.1160/TH08-02-0087. [DOI] [PubMed] [Google Scholar]
- 170.Yamamoto K., Koretsune Y., Akasaka T., Kisanuki A., Ohte N., Takenaka T., Takeuchi M., Yoshida K., Iwade K., Okuyama Y., et al. Effects of vitamin K antagonist on aortic valve degeneration in non-valvular atrial fibrillation patients: Prospective 4-year observational study. Thromb. Res. 2017;160:69–75. doi: 10.1016/j.thromres.2017.10.027. [DOI] [PubMed] [Google Scholar]
- 171.Rattazzi M., Faggin E., Bertacco E., Nardin C., Pagliani L., Plebani M., Cinetto F., Guidolin D., Puato M., Pauletto P. Warfarin, but not rivaroxaban, promotes the calcification of the aortic valve in ApoE−/− mice. Cardiovasc. Ther. 2018;36:e12438. doi: 10.1111/1755-5922.12438. [DOI] [PubMed] [Google Scholar]
- 172.Pan M.H., Maresz K., Lee P.S., Wu J.C., Ho C.T., Popko J., Mehta D.S., Stohs S.J., Badmaev V. Inhibition of TNF-α, IL-1α, and IL-1β by Pretreatment of Human Monocyte-Derived Macrophages with Menaquinone-7 and Cell Activation with TLR Agonists in Vitro. J. Med. Food. 2016;19:663–669. doi: 10.1089/jmf.2016.0030. [DOI] [PubMed] [Google Scholar]
- 173.Ohsaki Y., Shirakawa H., Hiwatashi K., Furukawa Y., Mizutani T., Komai M. Vitamin K suppresses lipopolysaccharide-induced inflammation in the rat. Biosci. Biotechnol. Biochem. 2006;70:926–932. doi: 10.1271/bbb.70.926. [DOI] [PubMed] [Google Scholar]
- 174.Shea M.K., Cushman M., Booth S.L., Burke G.L., Chen H., Kritchevsky S.B. Associations between vitamin k status and haemostatic and inflammatory biomarkers in community-dwelling adults: The multi-ethnic study of atherosclerosis. Thromb. Haemost. 2014;112:438–444. doi: 10.1160/TH13-12-1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Lupo M.G., Biancorosso N., Brilli E., Tarantino G., Adorni M.P., Vivian G., Salvalaio M., Dall’Acqua S., Sut S., Neutel C., et al. Cholesterol-lowering action of a novel nutraceutical combination in uremic rats: Insights into the molecular mechanism in a hepatoma cell line. Nutrients. 2020;12:436. doi: 10.3390/nu12020436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Zwakenberg S.R., De Jong P.A., Bartstra J.W., van Asperen R., Westerink J., de Valk H., Slart R.H.J.A., Luurtsema G., Wolterink J.M., de Borst G.J., et al. The effect of menaquinone-7 supplementation on vascular calcification in patients with diabetes: A randomized, double-blind, placebo-controlled trial. Am. J. Clin. Nutr. 2019;110:883–890. doi: 10.1093/ajcn/nqz147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Kurnatowska I., Grzelak P., Masajtis-Zagajewska A., Kaczmarska M., Stefańczyk L., Vermeer C., Maresz K., Nowicki M. Effect of Vitamin K2 on progression of atherosclerosis and vascular calcification in nondialyzed patients with chronic kidney disease stages 3-5. Pol. Arch. Med. Wewn. 2015;125:631–640. doi: 10.20452/pamw.3041. [DOI] [PubMed] [Google Scholar]
- 178.Shea M.K., O’Donnell C.J., Hoffmann U., Dallal G.E., Dawson-Hughes B., Ordovas J.M., Price P.A., Williamson M.K., Booth S.L. Vitamin K supplementation and progression of coronary artery calcium in older men and women. Am. J. Clin. Nutr. 2009;89:1799–1807. doi: 10.3945/ajcn.2008.27338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Geleijnse J.M., Vermeer C., Grobbee D.E., Schurgers L., Knapen M.H., van der Meer I.M., Hofman A., Witteman J.C. Dietary Intake of Menaquinone Is Associated with a Reduced Risk of Coronary Heart Disease: The Rotterdam Study. J. Nutr. 2004;134:3100–3105. doi: 10.1093/jn/134.11.3100. [DOI] [PubMed] [Google Scholar]
- 180.Gast G.C.M., de Roos N.M., Sluijs I., Bots M.L., Beulens J.W., Geleijnse J.M., Witteman J.C., Grobbee D.E., Peeters P.H., van der Schouw Y.T. A high menaquinone intake reduces the incidence of coronary heart disease. Nutr. Metab. Cardiovasc. Dis. 2009;19:504–510. doi: 10.1016/j.numecd.2008.10.004. [DOI] [PubMed] [Google Scholar]
- 181.Holden R.M., Booth S.L., Day A.G., Clase C.M., Zimmerman D., Moist L., Shea M.K., McCabe K.M., Jamal S.A., Tobe S., et al. Inhibiting the progression of arterial calcification with vitamin K in HemoDialysis patients (iPACK-HD) trial: Rationale and study design for a randomized trial of vitamin K in patients with end stage kidney disease. Can. J. Kidney Health Dis. 2015;2:53. doi: 10.1186/s40697-015-0053-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Krueger T., Schlieper G., Schurgers L., Cornelis T., Cozzolino M., Jacobi J., Jadoul M., Ketteler M., Rump L.C., Stenvinkel P., et al. Vitamin K1 to slow vascular calcification in haemodialysis patients (VitaVasK trial): A rationale and study protocol. Nephrol. Dial. Transplant. 2014;29:1633–1638. doi: 10.1093/ndt/gft459. [DOI] [PubMed] [Google Scholar]
- 183.Vossen L.M., Schurgers L.J., van Varik B.J., Kietselaer B.L., Vermeer C., Meeder J.G., Rahel B.M., van Cauteren Y.J., Hoffland G.A., Rennenberg R.J., et al. Menaquinone-7 supplementation to reduce vascular calcification in patients with coronary artery disease: Rationale and study protocol (VitaK-CAC Trial) Nutrients. 2015;7:8905–8915. doi: 10.3390/nu7115443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Brandenburg V.M., Reinartz S., Kaesler N., Krüger T., Dirrichs T., Kramann R., Peeters F., Floege J., Keszei A., Marx N., et al. Slower progress of aortic valve calcification with Vitamin K supplementation: Results from a prospective interventional proof-of-concept study. Circulation. 2017;135:2081–2083. doi: 10.1161/CIRCULATIONAHA.116.027011. [DOI] [PubMed] [Google Scholar]
- 185.Lindholt J.S., Frandsen N.E., Fredgart M.H., Øvrehus K.A., Dahl J.S., Møller J.E., Folkestad L., Urbonaviciene G., Becker S.W., Lambrechtsen J., et al. Effects of menaquinone-7 supplementation in patients with aortic valve calcification: Study protocol for a randomised controlled trial. BMJ Open. 2018;8:e22019. doi: 10.1136/bmjopen-2018-022019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Peeters F.E.C.M., Van Mourik M.J.W., Meex S.J.R., Bucerius J., Schalla S.M., Gerretsen S.C., Mihl C., Dweck M.R., Schurgers L.J., Wildberger J.E., et al. Bicuspid aortic valve stenosis and the effect of vitamin K2 on calcification using 18F-sodium fluoride positron emission tomography/magnetic resonance: The BASIK2 rationale and trial design. Nutrients. 2018;10:386. doi: 10.3390/nu10040386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Perrucci G.L., Songia P., Moschetta D., Barbagallo V.A., Valerio V., Myasoedova V.A., Alfieri V., Massaiu I., Roberto M., Malešević M., et al. Cyclophilin A inhibition as potential treatment of human aortic valve calcification. Pharmacol. Res. 2020;158:104888. doi: 10.1016/j.phrs.2020.104888. [DOI] [PubMed] [Google Scholar]
- 188.Chen Z., Gordillo-Martinez F., Jiang L., He P., Hong W., Wei X., Staines K.A., Macrae V.E., Zhang C., Yu D., et al. Zinc ameliorates human aortic valve calcification through GPR39 mediated ERK1/2 signalling pathway. Cardiovasc. Res. 2020 doi: 10.1093/cvr/cvaa090. [DOI] [PubMed] [Google Scholar]
- 189.Artiach G., Carracedo M., Seime T., Plunde O., Laguna-Fernandez A., Matic L., Franco-Cereceda A., Bäck M. Proteoglycan 4 is Increased in Human Calcified Aortic Valves and Enhances Valvular Interstitial Cell Calcification. Cells. 2020;9:684. doi: 10.3390/cells9030684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Liu H., Wang L., Pan Y., Wang X., Ding Y., Zhou C., Shah A.M., Zhao G., Zhang M. Celastrol Alleviates Aortic Valve Calcification Via Inhibition of NADPH Oxidase 2 in Valvular Interstitial Cells. JACC Basic Transl. Sci. 2020;5:35–49. doi: 10.1016/j.jacbts.2019.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Côté N., El Husseini D., Pépin A., Bouvet C., Gilbert L.A., Audet A., Fournier D., Pibarot P., Moreau P., Mathieu P. Inhibition of ectonucleotidase with ARL67156 prevents the development of calcific aortic valve disease in warfarin-treated rats. Eur. J. Pharmacol. 2012;689:139–146. doi: 10.1016/j.ejphar.2012.05.016. [DOI] [PubMed] [Google Scholar]
- 192.Bouchareb R., Côté N., Boulanger M.C., Le Quang K., El Husseini D., Asselin J., Hadji F., Lachance D., Shayhidin E.E., Mahmut A., et al. Carbonic anhydrase XII in valve interstitial cells promotes the regression of calcific aortic valve stenosis. J. Mol. Cell Cardiol. 2015;82:104–115. doi: 10.1016/j.yjmcc.2015.03.002. [DOI] [PubMed] [Google Scholar]
- 193.Choi B., Lee S., Kim S.M., Lee E.J., Lee S.R., Kim D.H., Jang J.Y., Kang S.W., Lee K.U., Chang E.J., et al. Dipeptidyl peptidase-4 induces aortic valve calcifcation by inhibiting insulin-like growth factor-1 signaling in valvular interstitial cells. Circulation. 2017;135:1935–1950. doi: 10.1161/CIRCULATIONAHA.116.024270. [DOI] [PubMed] [Google Scholar]
- 194.Clark C.R., Bowler M.A., Snider J.C., David Merryman W. Targeting Cadherin-11 Prevents Notch1-Mediated Calcific Aortic Valve Disease. Circulation. 2017;135:2448–2450. doi: 10.1161/CIRCULATIONAHA.117.027771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Li F., Cai Z., Chen F., Shi X., Zhang Q., Chen S., Shi J., Wang D.W., Dong N. Pioglitazone attenuates progression of aortic valve calcification via down-regulating receptor for advanced glycation end products. Basic Res. Cardiol. 2012;107 doi: 10.1007/s00395-012-0306-0. [DOI] [PubMed] [Google Scholar]
- 196.Chu Y., Lund D.D., Weiss R.M., Brooks R.M., Doshi H., Hajj G.P., Sigmund C.D., Heistad D.D. Pioglitazone attenuates valvular calcification induced by hypercholesterolemia. Arterioscler. Thromb. Vasc. Biol. 2013;33:523–532. doi: 10.1161/ATVBAHA.112.300794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Chen S.R., Dai Y., Zhao J., Lin L., Wang Y., Wang Y. A mechanistic overview of triptolide and celastrol, natural products from Tripterygium wilfordii Hook F. Front. Pharmacol. 2018;9:104. doi: 10.3389/fphar.2018.00104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Cascão R., Fonseca J.E., Moita L.F. Celastrol: A spectrum of treatment opportunities in chronic diseases. Front. Med. 2017;4:69. doi: 10.3389/fmed.2017.00069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Yeang C., Tsimikas S. Ancient Remedy for a Modern Disease: Will Celastrol Become a Treatment for Aortic Valve Stenosis? JACC Basic Transl. Sci. 2020;5:50–52. doi: 10.1016/j.jacbts.2019.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Rattazzi M., Bertacco E., Iop L., D’Andrea S., Puato M., Buso G., Causin V., Gerosa G., Faggin E., Pauletto P. Extracellular pyrophosphate is reduced in aortic interstitial valve cells acquiring a calcifying profile: Implications for aortic valve calcification. Atherosclerosis. 2014;237:568–576. doi: 10.1016/j.atherosclerosis.2014.10.027. [DOI] [PubMed] [Google Scholar]
- 201.Villa-Bellosta R. New insights into endogenous mechanisms of protection against arterial calcification. Atherosclerosis. 2020;306:68–74. doi: 10.1016/j.atherosclerosis.2020.03.007. [DOI] [PubMed] [Google Scholar]
- 202.El Husseini D., Boulanger M.C., Mahmut A., Bouchareb R., Laflamme M.H., Fournier D., Pibarot P., Bossé Y., Mathieu P. P2Y2 receptor represses IL-6 expression by valve interstitial cells through Akt: Implication for calcific aortic valve disease. J. Mol. Cell Cardiol. 2014;72:146–156. doi: 10.1016/j.yjmcc.2014.02.014. [DOI] [PubMed] [Google Scholar]
- 203.Mulvihill E.E., Drucker D.J. Pharmacology, physiology, and mechanisms of action of dipeptidyl peptidase-4 inhibitors. Endocr. Rev. 2014;35:992–1019. doi: 10.1210/er.2014-1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Shah Z., Kampfrath T., Deiuliis J.A., Zhong J., Pineda C., Ying Z., Xu X., Lu B., Moffatt-Bruce S., Durairaj R., et al. Long-term dipeptidyl-peptidase 4 inhibition reduces atherosclerosis and inflammation via effects on monocyte recruitment and chemotaxis. Circulation. 2011;124:2338–2349. doi: 10.1161/CIRCULATIONAHA.111.041418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Varennes O., Mary A., Bricca G., Kamel S., Bellien J. Dipeptidyl Peptidase-4 Inhibition Prevents Vascular Calcification by Potentiating the Insulin-Like Growth Factor-1 Signaling Pathway. JACC Basic Transl. Sci. 2019;4:113–115. doi: 10.1016/j.jacbts.2018.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Radcliff K., Tang T.B., Lim J., Zhang Z., Abedin M., Demer L.L., Tintut Y. Insulin-like growth factor-I regulates proliferation and osteoblastic differentiation of calcifying vascular cells via extracellular signal-regulated protein kinase and phosphatidylinositol 3-kinase pathways. Circ. Res. 2005;96:398–400. doi: 10.1161/01.RES.0000157671.47477.71. [DOI] [PubMed] [Google Scholar]
- 207.Zhou J., Bowen C., Lu G., Knapp C., Recknagel A., Norris R.A., Butcher J.T. Cadherin-11 expression patterns in heart valves associate with key functions during embryonic cushion formation, valve maturation and calcification. Cells Tissues Organs. 2014;198:300–310. doi: 10.1159/000356762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Hutcheson J.D., Chen J., Sewell-Loftin M.K., Ryzhova L.M., Fisher C.I., Su Y.R., Merryman W.D. Cadherin-11 regulates cell-cell tension necessary for calcific nodule formation by valvular myofibroblasts. Arterioscler. Thromb. Vasc. Biol. 2013;33:114–120. doi: 10.1161/ATVBAHA.112.300278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Sung D.C., Bowen C.J., Vaidya K.A., Zhou J., Chapurin N., Recknagel A., Zhou B., Chen J., Kotlikoff M., Butcher J.T. Cadherin-11 Overexpression Induces Extracellular Matrix Remodeling and Calcification in Mature Aortic Valves. Arterioscler. Thromb. Vasc. Biol. 2016;36:1627–1637. doi: 10.1161/ATVBAHA.116.307812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Bowen C.J., Zhou J., Sung D.C., Butcher J.T. Cadherin-11 coordinates cellular migration and extracellular matrix remodeling during aortic valve maturation. Dev. Biol. 2015;407:145–157. doi: 10.1016/j.ydbio.2015.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Schroer A.K., Bersi M.R., Clark C.R., Zhang Q., Sanders L.H., Hatzopoulos A.K., Force T.L., Majka S.M., Lal H., Merryman W.D. Cadherin-11 blockade reduces inflammation-driven fibrotic remodeling and improves outcomes after myocardial infarction. JCI Insight. 2019;4:e131545. doi: 10.1172/jci.insight.131545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Liu L., Liu Y., Zhang Y., Bi X., Nie L., Liu C., Xiong J., He T., Xu X., Yu Y., et al. High phosphate-induced downregulation of PPARγ contributes to CKD-associated vascular calcification. J. Mol. Cell Cardiol. 2018;114:264–275. doi: 10.1016/j.yjmcc.2017.11.021. [DOI] [PubMed] [Google Scholar]
- 213.Ivanova E.A., Parolari A., Myasoedova V., Melnichenko A.A., Bobryshev Y.V., Orekhov A.N. Peroxisome proliferator-activated receptor (PPAR) gamma in cardiovascular disorders and cardiovascular surgery. J. Cardiol. 2015;66:271–278. doi: 10.1016/j.jjcc.2015.05.004. [DOI] [PubMed] [Google Scholar]
- 214.Gao M., Chen T., Wu L., Zhao X., Mao H., Xing C. Effect of pioglitazone on the calcification of rat vascular smooth muscle cells through the downregulation of the Wnt/β-catenin signaling pathway. Mol. Med. Rep. 2017;16:6208–6213. doi: 10.3892/mmr.2017.7308. [DOI] [PubMed] [Google Scholar]
- 215.Arnold S.V., Inzucchi S.E., Echouffo-Tcheugui J.B., Tang F., Lam C.S.P., Sperling L.S., Kosiborod M. Understanding contemporary use of thiazolidinediones an analysis from the diabetes collaborative registry. Circ. Heart Fail. 2019;12:e005855. doi: 10.1161/CIRCHEARTFAILURE.118.005855. [DOI] [PubMed] [Google Scholar]
- 216.Summerhill V.I., Moschetta D., Orekhov A.N., Poggio P., Myasoedova V.A. Sex-specific features of calcific aortic valve disease. Int. J. Mol. Sci. 2020;21:5620. doi: 10.3390/ijms21165620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Myasoedova V.A., Di Minno A., Songia P., Massaiu I., Alfieri V., Valerio V., Moschetta D., Andreini D., Alamanni F., Pepi M., et al. Sex-specific differences in age-related aortic valve calcium load: A systematic review and meta-analysis. Ageing Res. Rev. 2020;61:101077. doi: 10.1016/j.arr.2020.101077. [DOI] [PubMed] [Google Scholar]