Abstract
Cancer is one of the highest prevalent diseases in humans. The chances of surviving cancer and its prognosis are very dependent on the affected tissue, body location, and stage at which the disease is diagnosed. Researchers and pharmaceutical companies worldwide are pursuing many attempts to look for compounds to treat this malignancy. Most of the current strategies to fight cancer implicate the use of compounds acting on DNA damage checkpoints, non-receptor tyrosine kinases activities, regulators of the hedgehog signaling pathways, and metabolic adaptations placed in cancer. In the last decade, the finding of a lipid peroxidation increase linked to 15-lipoxygenases isoform 1 (15-LOX-1) activity stimulation has been found in specific successful treatments against cancer. This discovery contrasts with the production of other lipid oxidation signatures generated by stimulation of other lipoxygenases such as 5-LOX and 12-LOX, and cyclooxygenase (COX-2) activities, which have been suggested as cancer biomarkers and which inhibitors present anti-tumoral and antiproliferative activities. These findings support the previously proposed role of lipid hydroperoxides and their metabolites as cancer cell mediators. Depletion or promotion of lipid peroxidation is generally related to a specific production source associated with a cancer stage or tissue in which cancer originates. This review highlights the potential therapeutical use of chemical derivatives to stimulate or block specific cellular routes to generate lipid hydroperoxides to treat this disease.
Keywords: cancer, peroxides, LOX, COX, Fenton reaction, iron, ferroptosis, nanoparticles
1. Introduction
Oxidative stress and inflammation are linked to cancer development [1,2]. Mutations in the DNA, phosphorylation of kinases, or inactivation of phosphatases can alter the cell growth, cellular control of the division, cell death, cell fate, and cell motility, which are altered in angiogenesis, inflammation, and fuel cancer progression [3,4,5,6]. A progressive increase of reactive oxygen species (ROS) marks the transition steps from a healthy tissue towards an invasive carcinoma [7]. This trend is owed to cancer cells’ metabolic aberrations to adapt strategies to escape from cell death. It occurs in the presence of compensatory upregulation of the genes coding antioxidant enzymes, preventing ROS induced cell death [2,5]. Therefore, a blockage of the antioxidant cellular defenses or pro-oxidant therapies’ stimulation is suggested as potential strategies to fight against cancer [8,9]. In general, lipids’ ability to participate in anti-inflammatory and/or pro-inflammatory signaling cascades is defined by: the length of the fatty acyl chain, the number of unsaturations, and the place where the oxidation account [10]. During lipid peroxidation, oxygen molecules are added to the unsaturated fatty acyl chain of non-polar lipids, increasing their water solubility and diffusion towards the membrane surface. Cyclooxygenases or lipoxygenases accessibility for their substrates is boosted, the generation of lipid metabolites linked to inflammation is prompted, and the interaction of specific proteins and receptors recognizing lipid oxidation products is promoted [11,12,13,14,15]. All of these actions are part of the lipid-dependent inflammatory cascade. Moreover, these arrangements prevent the accumulation of lipid peroxides into the membrane, which might functionally damage membrane components such as proteins by induction of covalent modifications, which might compromise membrane permeability [16,17]. In general, free fatty acids can be released from phospholipids by phospholipases, and this pathway is essential in inflammation, since it counterparts the activities of lipoxygenases and cyclooxygenases [18]. Polyunsaturated fatty acids (PUFA) and their related phospholipids are very well-known signaling molecules with pro-inflammatory and anti-inflammatory functions, but also sensitive substrates for peroxidation [19,20,21,22,23,24,25,26,27,28]. PUFA can promote cell life or cell death through complex signaling cascades related to the fatty acid structure and their oxidation products [29,30]. In cancer, the connection of some of these pathways with inflammation is unveiled by identifying a group of lipid oxidation products, known as lipid pro-resolving mediators, which can resolve the inflammation [31,32,33]. Their discovery opens the opportunity to identify new potential drugs in cancer therapy [32]. Some lipid oxidation products have also gained attention since they are suggested as biomarkers for cancer development and recurrence [34,35]. In general, lipids’ ability to participate in anti-inflammatory or pro-inflammatory signaling cascades depends on the lipid’s nature and its degree of oxidation. In this review, we dissect the lipid hydroperoxides and metabolites sources found in cancer research to better define proper actions to treat the malignancy and highlight those stimulated pathways found in tumors from those triggered in strategies to kill cancer cells.
2. Lipid Peroxidation: Non-Enzymatic Reactions vs. Enzymatic Reactions
Cellular lipid peroxidation can occur through different reactions, but they can be categorized into enzyme and non-enzyme dependent reactions. The primary substrates in lipid peroxidation reactions are polyunsaturated lipids since carbon-carbon double bonds are susceptible to reactive oxygen species, such as the hydroxyl radical (HO•), which is a key radical that participates in peroxidation reactions.
2.1. Non-Enzyme-Dependent Lipid Peroxidation
In the non-enzymatic reactions, the Fenton and Haber–Weiss reactions producing HO• are dependent on transition metals (i.e., iron [36,37]), for the initiation of the radical chain reactions required for lipid peroxidation. In addition to this radical formation, some authors have suggested that for initiation of lipid peroxidation, the formation of a complex between iron and the lipids is required [38]. In general, it is accepted that the initiation reaction starts when a hydrogen atom is abstracted from lipid, forming an alkyl radical [39]. HO• is preferred over other radicals to performed this abstraction [38,39,40,41,42,43]. Once the alkyl radical is formed, the chain-carrying a carbon radical reacts with oxygen, leading to an alkyl peroxyl radical formation. This radical can abstract hydrogen from an organic substrate, which can be another lipid, to form a hydroperoxide plus an organic radical or be added to alkenes, such as those present in the fatty acyl chains of PUFA present in phospholipids, which provide isolated double bonds [44]. This last reaction leads to the formation of a lipid hydroperoxide with a conjugated double bond. By reaction with metals, lipid radical reactions leading to lipid peroxidation can be reinitiated as part of the propagating radical reactions [45,46]. This process occurs when the hydroperoxides react with an oxidized metal forming an alkoxyl radical. In case the reaction involves a reduced metal, e.g., Fe2+, an alkyl peroxyl radical is generated, which also contributes to the propagation of the reaction. PUFA are lipid molecules priming the Fenton’s reaction, as previously indicated. Arachidonic acid (AA) and the phospholipids containing this fatty acid are essential molecules since they are precursors of pro- and anti-inflammatory mediators, sometimes enriched at cellular locations identified as signaling platforms, such as the plasma membrane lipid rafts [47,48]. Lipid oxidation at this location during the inflammation process is relevant since lipid rafts are platforms required for cell activation in the immune system [49].
2.2. Radiation Inducing Lipid Peroxidation
HO• can also be generated by ionizing radiation [38], which is generally used and applied in patients to treat cancer. As previously indicated, HO• is a very reactive radical, leading to the generation of lipid hydroperoxides and oxidizing other biomolecules, including the DNA. Radiation exposition leads to peroxides generation in membranes enriched with PUFA. Indeed, this fact should not be discarded as a relevant factor for cancer therapy’s success in these patients [50,51,52,53]. Noteworthy, more efforts are required to shed light on the role that ionizing radiation generating lipid peroxides have in cancer cell death vs. other targets. These investigations could help in the characterization of pharmacological drugs prompting the cancer cell sensitivity to lipid hydroperoxides generated by ionizing radiation (i.e., glutathione peroxidase 4 (GPX4) inhibitors) and, therefore, better define or reduce the patient’s exposure to ionizing radiation that can also damage non-tumoral tissues.
2.3. Enzyme-Dependent Lipid Peroxidation
The enzyme-dependent reactions are executed by peroxidases, which have been elegantly classified by Vlasova [54]. Based on this classification, lipids can be oxidized by proteins that possess a true peroxidase activity, such as lipoxygenases (LOX), cyclooxygenases (COX), and cytochrome P450, or by proteins that do not have a peroxidase activity but acquire a pseudo-peroxidase activity under certain conditions, i.e., cytochrome c [55,56,57,58,59] upon binding to cardiolipin or other hemeproteins in defined conditions [60,61,62,63]. The coordinated iron or iron associated with the heme group is key in these enzymes’ catalytic center. Compound I, compound II, and sometimes compound III are generally typical and associated with different iron valences [64]. The function of real peroxidases might depend upon the existence of binding pockets where substrates can settle and interact with the enzyme catalytic center, and upon electrons donated by organic molecules, which might be protein amino acids acting as electron donors [54]. In heme-dependent pseudo-peroxidases, substrates accessibility to the enzyme coordinating sphere depends upon the catalytic center flexibility to swift from a metal hexa- to penta-coordination, a feature that can be influenced by the redox state or the interaction with a ligand, i.e., cytochrome c upon cardiolipin binding to the protein [55]. The main enzymes using AA to generate lipid hydroperoxides and derived metabolites as signaling molecules in cancer are cyclooxygenases (COX), lipoxygenases (LOX), and P450 families [29,30,47,65]. COX-1 is constitutively expressed in many tissues and cell types, whereas COX-2 is an inducible cyclooxygenase isoform which activation has been reported in tumoral tissues [66,67,68,69,70,71]. Some studies have also pointed out that other peroxidases (like myeloperoxidase and eosinophil peroxidase) released from infiltrating neutrophils and eosinophils in the tumor microenvironment [72,73,74,75] or from infiltrated macrophages can also generate lipid hydroperoxide [76]. Although myeloperoxidases are potential sources of lipid peroxides and some myeloperoxidases polymorphisms, have been correlated with a higher risk of suffering pulmonary, ovarian, and gastric cancer [77,78,79], there is no correlation between their activity and the lipid peroxides derived from it with disease development.
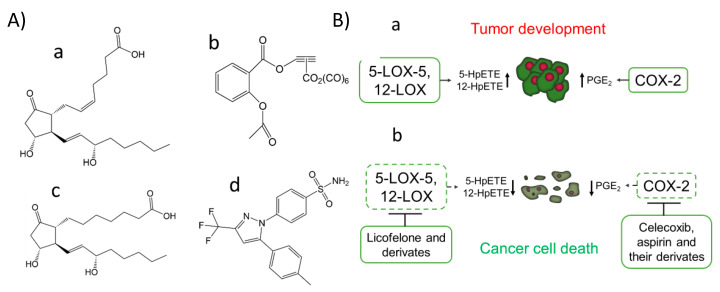
In contrast, anti-inflammatory drugs have been linked to a decreased risk of cancer development and decreased tumor growth rate [28]. Notably, in this context, overexpression of enzymes generating eicosanoids in breast, lung, and pancreas cancer has been reported [28]. In particular, prostaglandins (PGs) can stimulate mitogenesis by directly affecting fibroblasts, osteoblasts, and mammary cells. The production of the proinflammatory PG named prostaglandin E2 (PGE2) (Figure 1A) through COX-2 activity can be found in mutagenesis, angiogenesis, and cell migration processes associated with cancer (Table 1). An activation mechanism for COX-2 has been proposed using human colorectal HT-29 and the human prostate carcinoma DU145 cell lines [80]. A correlation between the production of PGE2 with the resistance of cancer cells to apoptosis has been found through activation of the P2Y2/Src/p38 signaling pathway, which lead to AA release from the membranes by overexpression of some PLA2 isoforms, and the overexpression of COX-2 with the subsequent PGE2 production [80].
Figure 1.
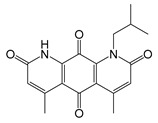
COX-2 inhibitors, PGE1, and PGE2 chemical structure (A). The prostaglandin E2 (PGE2) (pro-cancer) (a), the aspirin derivate named [2-acetoxy-(2-propynyl)benzoate]hexacarbonyldicobalt (Co-ASS) (b), the prostaglandin E1 (PGE1) (anticancer) (c) and the COX-2 selective inhibitor named celecoxib, (p-(5-p-Tolyl-3-(trifluoromethyl) pyrazol-1-yl)benzenesulfonamide) (d). Expression of COX-2, 5-LOX, and 12-LOX in cancer and the effect of inhibitors against these targets (B). Activation of 5-LOX-5, 12-LOX, and COX-2 has been reported in the development and progress of tumors from different tissues associated with the production of specific lipid peroxides and metabolites, such as PGE2 (a). Some inhibitors of these LOX isoforms and COX-2 have emerged as potential therapeutical agents for cancer treatment, modulating the production of previously commented metabolites and by induction of cancer cell death (b).
Table 1.
Correlation between COX-2 level and other biomarkers found in tumoral tissues
| Tissue Location and Type of Cancer | Correlation with Other Biomarkers |
|---|---|
| Colon cancer [66], primary tumors and metastatic lymph nodes resections for colorectal adenocarcinoma [93], stage II and III colorectal cancer patients [94] | High levels of COX-2 correlates with high levels of MMP-2 and VEGF expression and shorter survival time [93,94]. |
| Cervical cancer [67] | Multivariate analysis of COX-2 levels in tumor/stromal compartments. The proportion of CD3+, CD4+, and CD25+ cells was lower in tumors with high tumor/stroma ratios, but in these tumors, mast cells were increased [67]. |
| Ovarian cancer [95,96,97] | No correlation between COX-2 expression and EGFR, and HER-2/neu status [96]. |
| Human breast cancer cell lines and tumors [26,98,99,100] | Elevated COX-2 expression associated with a large tumor size, a high histological grade, a negative hormone receptor status, a high proliferation rate, high p53 expression, and the presence of HER-2 oncogene amplification along with axillary node metastases and a ductal type of histology [98]. COX-2 inhibition may potentially prevent the development of ER-positive and ER-negative breast cancers [98]. Expression of PGE2 and IL-8 [101]. COX-2 over-expression induces an oncogenic microRNA (miR655) in human breast cancer cells by activation of EP4 [102]. |
| Ductal carcinoma in situ (DCIS) [103,104,105] | COX-2 expression stabilizes survivin, an inhibitor of apoptosis (IAP) [103]. CacyBP expression was significantly negatively associated with the COX expression [104]. |
| Non-small cell lung cancer [68,69] | Correlation between HER-2, EGFR, and COX-2 expression in patients of non-small cell lung cancer at different degrees [69] |
| Laryngeal cancer [71] | Cox-2 overexpression was significantly associated with radioresistant tumors [71]. |
| Papillary thyroid cancer [106] | The expression of COX-2 is increased with age in papillary thyroid cancer [106]. Immunohistochemically, expression of COX-2 and VEGF-C correlated strongly, and both were induced by the tumor promoter phorbol 12-myristate 13-acetate [107]. |
| Endometrial hyperplasia and carcinoma [108,109,110] | No correlation between COX-2 expression with estrogen (ER) or progesterone receptor (PR), p53, and neu [110]. Correlation between COX-2 (59%) and aromatase (65%) expression but not estrogen and progesterone receptor [111]. |
| Invasive gallbladder cancer [112] | COX-2, c-Met, β-catenin, c-erbB2 and EGFR were over-expressed in 80%, 74%, 71%, 62%, and 11% of invasive gallbladder cancers, respectively [112]. |
| Prostate cancer Metastatic primary prostate carcinoma compared to non-metastatic cancers [113,114,115,116] |
COX-2 and Ki-67 antigen co-expression in 42.9% and 67% of the prostate cancer patients [113]. Patients with PSA > 7 ng/mL and high COX-2 expression had the highest probability of recurrence [114]. The expressions of COX-2 and E-cadherin are very firmly and inversely correlated as prognostic indicators. [115]. High expression of COX-2, TGF-beta, and Ki67 in metastatic primary prostate carcinoma was associated with death from prostate carcinoma [116]. |
| Gastric cancer [117,118] | A positive correlation between COX-2 and K-ras expression with the depth of invasion and lymph node metastasis in gastric cancer [117]. Epithelial MMP-2 expression in gastric cancer is associated with aggressive forms, COX-2 expression, and poor survival [118]. |
| Cervical cancer [119] | DNA hypermethylation of the COX-2 gene may be a potential prognostic marker in the early stages of cervical cancer [119]. |
| Pancreatic cancer [120,121] Anaplastic pancreatic cancer [122] |
Tumor COX-2 expression portends a poor prognosis for patients with resected adenocarcinoma of the pancreas, particularly in tumors > or = 3 cm [121]. Expression of L1CAM, COX-2, and EGFR in the majority of undifferentiated pancreatic carcinomas [122]. |
To define the role of lipid peroxidation in signaling, the type of lipid hydroperoxide generated should be finely characterized. In the metal-mediated lipid peroxidation based on the Fenton and Haber–Weiss reactions, random lipid peroxides are generated and differentiated from those formed by specialized enzymes that produce specific lipid signatures that can be used as fingerprints of enzymatic activities [58,81,82]. Many efforts are being made to find specific inhibitors that can provide a specific modulation of lipid hydroperoxide production that could act as mediators in signaling cascades [58,83]. For example, aspirin, which has beneficial effects in some cancer types, has been proposed to play that role [82,84,85]. Its implication in cancer has been associated with COX inhibition via acetylation of the active site, where AA binds. This accounts for COX-1 isozyme inhibition, while in COX-2, aspirin binding produces a structural rearrangement shifting the cyclooxygenase towards the lipoxygenase activity [86,87]. Therefore, AA oxygenation and cyclization to form a 15R-Prostaglandin endoperoxide is promoted, which favors the production of Prostaglandin D2 (PGD2) (with has a suggested function in inflammation resolution) instead of PGE2 [88]. Recent studies have also shown the potential therapeutically effect of aspirin organometallic derivatives as anticancer agents targeting COX-2 [89], such as the 4-[5-(4-Chlorophenyl)-3-(trifluoromethyl)-1H-pyrazol-1-yl]-benzenesulfonamide (SC-236) and [2-acetoxy-(2-propynyl)benzoate]hexacarbonyldicobalt (Co-ASS) (Figure 1A), which open a promising field in the search for inhibitors derived from aspirin [90,91,92].
2.4. Lipid Peroxidation Derived Products and Biological Targets
Lipid hydroperoxides generated via enzyme or non-enzyme-dependent reactions can be further oxidized to form highly reactive species and lipid autoxidation products. Acrolein, malonaldehyde, and 4-hydroxynonenal can covalently modify proteins leading to functional and structural changes in proteins [123,124,125]. Lipid autoxidation products mainly react with primary amines and lysines, histidine, and cysteine residues from proteins to induce covalent crosslinking and prompt protein aggregation [125]. The amino acid residues mentioned above are also the primary targets for several protein post-transductional modifications, such as acylation, acetylation, phosphorylation, methylation, glycation, and S-nitrosylation, among other modifications [126,127]. Therefore, it can be presumed that the reaction of essential amino acid residues with lipid autoxidation products will also induce changes in the signaling pathways in which these proteins are involved. The generation of lipid autoxidation products has been reported in cancer development, angiogenesis, and invasiveness [128,129,130,131,132]. Some autoxidation products, such as 4-hydroxynonenal, have been implicated in DNA modifications that generate cancer-linked mutations [1].
2.5. Antioxidants against Lipid Radical Reactions and Peroxidases
Antioxidants play a central role to counteract lipid peroxidation. In the non-enzyme-dependent reactions, the radical chain reactions can terminate when antioxidants react with the alkyl peroxyl or the alkoxyl radicals. Tocopherol is the main membrane antioxidant in charge of reacting with these radicals and one of the primary membrane antioxidants against reactions generating lipid peroxides, in general [133]. Consequently, a lipid hydroperoxide or the alcohol and the radical antioxidant are products of the reaction between the lipid radical with the antioxidant. In the particular case of the tocopheroxyl radical, it can be reduced back to tocopherol by its reaction with other antioxidants, such as ascorbate and ubiquinol [134], or by enzymes in charge of reducing the antioxidant radical [135,136]. Indirectly or directly, the enzymatic activities that reduce the radicals derived from antioxidants are essential to keep optimal alpha-tocopherol levels in the membrane [135,137,138]. Other types of enzymes, such as glutathione peroxidases, can reduce lipid hydroperoxides to alcohols at the expense of glutathione (GSH). GPX4 is a pharmacological target in cancer [139,140,141], and its inhibition has been found to induce cancer cell death by the accumulation of lipid hydroperoxides [140].
3. Lipid Hydroperoxides Generated by Stimulated Lipoxygenases (LOXs), Cyclooxygenases (COXs), and the Role of Their Metabolites in Cancer
3.1. COXs
The main AA oxidation products of COXs activity are PGs. Prostaglandin H2 (PGH2) is a PG generated by both COX-1 and -2 using AA as a substrate, which acts as a precursor for the generation of other PGs such as the thromboxane A2 (TxA2) and the PGs named PGI2, PGD2, PGE2, and PGF2α [142]. PGs are important in the early inflammatory response, and their production is increased in the inflamed tissue mainly by stimulation of COX-2 activity [143]. In addition to COXs, other pathways have been implicated in the generation of PGs in cancer, such as those dependent upon prostaglandin synthetases that might be functionally coupled to COX-2 activity and, in some cases, might also be dependent upon glutathione [23,144,145]. In general, raised levels of COX-2 and 12-lipoxygenase (12-LOX) in patients who developed metastatic disease or local recurrence and/or died have been found in other studies and, therefore, these enzymes have been proposed as biomarkers in cancer [146,147]. COX-2 in combination with other biomarkers has also been used in cancer prognosis (Table 1). In addition, a strong correlation between the production of PGE2 and cancer development has been observed [34,35].
For the generation of PGE2 by COXs, a peroxidation and cyclooxygenation reaction of the substrate is required. On the distal side from the heme moiety, an array of amino acids provides the site for hydroperoxides to bind and assists the heme-dependent reduction of hydroperoxides to alcohols [148]. Therefore, the formation of the PG involved in cancer named PGE2 requires several steps for its production [23]. First, the formation of unstable endoperoxide intermediate named prostaglandin G2 (PGG2) through COX activity using AA as a substrate. This PG can be further metabolized to a second unstable endoperoxide intermediate named PGH2, which can be enzymatically broken down to generate the PGE2 [23,24,25,26,27,28].
PGE2 acts binding to any of the specific G-coupled receptors belonging to four subclasses, EP1-EP4, which have specific signal transduction activities, tissue localization, and regulation [149]. The activation of each of the different receptors and downstream signaling cascades makes PGE2 activity highly dependent on the specific docking receptor [150]. The role of each EP receptor in malignant behavior is complex, but their signaling cascades have been found linked to different stages of tumoral and immune processes [151].
Moreover, downstream metabolites derived from PGE2 are compounds, such as 15-keto-PGE2, generated by 15-hydroxyprostaglandin dehydrogenase [152,153]. This compound ligates to the transcription factor peroxisome proliferator-activator receptor gamma (PPARγ), which regulation has been found to regulate genes with anti-proliferative and anti-inflammatory effects and play a protective role against tumor development [154,155]. Some PPARγ agonists, including 15-keto-PGE2 and thiazolidinediones, have been proposed as potential pharmacological therapeutical drugs in cancer [156,157,158,159]. However, it is still unclear whether PPARs act as bona fide tumor suppressor or as an oncogene, and more studies are needed to understand their role in cancer for the development of efficient and safe chemotherapeutic agents targeting these molecules [154]. Other AA derived metabolites, such as 15-deoxy-delta-12,14-prostaglandin-J2 (15d-PGJ2), are also known as PPARγ agonists. Besides, PGD2, PGJ2, Δ12-PGJ2 are also known to induce the apoptosis of tumoral cells [160,161].
3.2. The Use of COX Inhibitors to Induce Cancer Cell Death
The possibility of product formation modulation by altering the substrate availability has traditionally been the primary COX activity regulation approach. Some substrates of COX-2 activity other than AA, such as γ-linolenic acid and dihomo-γ-linolenic acid, have been demonstrated to pose anti-cancer effects and have been proposed as promising dietary supplements for cancer prevention since they increase the formation of PGE1 (Figure 1A) and related metabolites, which have anti-inflammatory properties [19,20,21,22]. Additionally, pharmacological drugs targeting the COX/LOX have been identified. Combined inhibition of 5-LOX/COX-2 has been used to treat some types of cancer [162,163,164,165,166]. COX-2 inhibitors such as celecoxib (Figure 1A,B), aspirin, diosgenin, and ibuprofen have been proposed to have anti-tumor activities, being useful in preventing and treating several cancer types [99,167,168,169,170]. Noteworthy, in some instances, a lack of response to COX-2 inhibitors, such as aspirin in some types of cancer at low concentrations, has been reported despite the potential noted benefit among individual patients population with stage I tumors [171,172]. However, some reports have evidenced a lack of effectiveness of this compound due to the upregulation of 15-LOX-1 that might be induced to compensate the lack of some lipid oxidation products [173].
3.3. LOXs
This group of enzymes is named based on the place of the carbon chain where the oxidation occurs. Six functional LOX genes (ALOX5, ALOX12, ALOX15, ALOX15B, ALOX12B, and ALOXE3) have been identified in humans [174]. Historically, mammalian LOXs are classified based on the position where AA oxygenation occurs [175]. Classification of genes, expression, and tissue location can be found in Table 2.
Table 2.
Human lipoxygenases (LOXs) genes classification and expression in cells and tissues.
| ALOX Gene | Name | Cell and Tissue Location |
|---|---|---|
| ALOX5 PubMed Gene ID: 240 |
arachidonate 5-lipoxygenase or 5-lipoxygenase (5-LOX) |
Monocytes, macrophages, B lymphocytes cells [175] and appendix, bone marrow, gall bladder, lung, lymph node, spleen, and urinary bladder [176]. |
| ALOX12 PubMed Gene ID: 239 |
arachidonate 12-lipoxygenase, 12S type or 12-lipoxygenase (12-LOX) |
Esophagus and skin [176]. |
| ALOX15 PubMed Gene ID: 246 |
arachidonate 15-lipoxygenase or platelet type platelet lipoxygenase or 15-lipoxygenase-1 (15-LOX-1) | Reticulocytes, eosinophils [175] and lung, small intestine, testis urinary bladder [176]. |
| ALOX15B PubMed Gene ID: 247 |
arachidonate 15-lipoxygenase type B or 15-lipoxygenase-2 (15-LOX-2) | Human skin [175] and prostate, lung, and esophagus [176]. |
| ALOX12B PubMed Gene ID: 242 |
arachidonate 12-lipoxygenase, 12R type or 12R-lipoxygenase (12R-LOX) | Skin and esophagus [176]. |
| ALOXE3 PubMed Gene ID: 59344 |
arachidonate lipoxygenase 3, lipoxygenase, epidermis type (eLOX3) | Skin, tongue, prostate, tonsils [175,176]. |
The 12-LOX utilizes AA to synthesize 12(S)-hydroperoxyeicosatetraenoic acid (12(S)-HpETE), which is converted to the end-product named 12(S)-hydroxyeicosatetraenoic acid (12(S)-HETE) implicated in the promotion of tumorigenesis, proliferation, and metastasis by stimulation of the vascular endothelial growth factor (VEGF), and some integrins expression and controlling the cell cycle [177,178,179,180]. Besides 12(S)-HETE, metabolites generated from 5-LOX such as 5-hydroxyeicosatetraenoic acid (5(S)-HETE), which precursor is 5(S)-HpETE, have been implicated in the stimulation of prostate cancer cell growth [181]. Upregulation of 5-LOX and 12-LOX activities in cancer contrast with the decrease in 15-lipoxygenase (15-LOX) isoform 1 (15-LOX-1) function, as well as in the metabolites generated from linoleic acid oxidation, such as 13–hydroperoxyoctadecadienoic acid (13(S)-HpODE) [178] and 13-S-hydroxyoctadecadienoic acid (13-S-HODE), which are reported in human colorectal and esophageal cancers [173]. These effects might be related to a downregulation of the 15-LOX-1 gene expression or its inactivation, as demonstrated for colon cancer [182,183,184,185], where the transcription factor GATA-6 is responsible for this effect [183]. Other derived hydroperoxides from 15-LOX-1, such as hydroperoxyoctadecatrienoic acid (13-HpOTrE), 13-HpODE, and 15-hydroperoxyeicosatetraenoic acid (15-HpETE) have been reported as inhibitors of breast, colon, prostate, lung, and leukemia cancer growth in conventional cell studies in vitro [186], supporting that stimulation of this 15-LOX-1 could be potentially used for therapeutical purposes. Among these compounds, 13-HpOTrE is reported to be the most active hydroperoxide regarding cytotoxicity and apoptosis induction in cell culture experiments [184,186]. Notably, other than in the two-dimensional (2D) culture experiments, 13-HpOTrE treatments for as long as a week did not show significant effects on cell viability in 3D cell culture experiments of tumor cells but resulted in decreased IL-6 release [186]. These results support the specific role of some lipid hydroperoxides as pro-survival or cell death signals in cancer that could be modulated by a specific tissue microenvironment and linked to the specific LOX isoforms.
Moreover, 15-LOX-1 activity is elevated when ferroptosis is induced in cancer cells [139]. Some of the main phospholipids acting as substrates for 15-LOX-1 in the context of ferroptosis are phosphatidylethanolamines (PE) containing PUFA in their fatty acyl chain, which generates lipid hydroperoxide and other PE oxidation products as ferroptosis signals [187]. This target specificity is associated with phosphatidylethanolamine-binding protein 1 (PEBP1) activity that acts as a scaffold protein inhibitor of protein kinase cascades that can form a complex with some 15-LOX isoforms [188].
3.4. The Use of LOX Inhibitors to Induce Cancer Cell Death
The nonsteroidal anti-inflammatory drugs acting as inhibitors of COX/LOX named tepoxalin [189], and licofelone [190] have been successfully used to halt the progression of gastric cancer and colon cancer cells, respectively, in tumor xenograft mice. These results suggest that inhibition of certain LOXs that have been found stimulated in cancer might be used to block cancer development. The most potent inhibitor of 12-LOX, named Zyflamend, presents cancer antiproliferative activity in human prostate cancer PC3 cells [191]. Peptides against 12-LOX, such as the one formed by tyrosine, tryptophan, cysteine and serine residues (YWCS), have also been developed and suggested for breast cancer treatment, and specific 12-LOX inhibitors, such as baicalein, due to their tumor-suppressive and anti-angiogenesis effects [192,193]. Other therapeutical approaches have demonstrated the efficacy of 12-LOX inhibition in vitro and in vivo experiments using human prostate cancer cells [194,195]. To summarize, it seems that the combinatorial effect of these enzyme inhibitors with those of COX-2 can prevent the generation of tumorigenic signaling molecules derived from 5-LOX and 12-LOX, whose synthesis is induced in some types of cancers with pathological consequences (Figure 1B).
4. Stimulation of Peroxidases to Induce Cancer Cell Death: The Case of 15-LOX-1 Activity in Ferroptosis
In cancer, lipid peroxidation became interesting for researchers since its involvement, and implication in cancer cell ferroptosis was discovered [196]. Many well-written reviews are describing this type of cell death [82,197,198]. Essentially this process can be summarized as a cell-regulated iron-dependent form of non-apoptotic cell death derived from lipid hydroperoxide accumulation [199], more predominantly phosphatidylethanolamine hydroperoxides [187]. In ferroptosis, iron chelators, lipophilic antioxidants, lipid peroxidation inhibitors, and depletion of polyunsaturated fatty acids (PUFAs) can block this cell death process [200]. Inhibition of GPX4 activates ferroptosis, and since this enzyme function is dependent upon GSH that acts as a substrate for this activity, those processes that limit GSH biosynthesis are essential and also to trigger this type of cell death [200,201]. For example, inhibition of the cystine/glutamate antiporter system xc- regulates the transsulfuration pathway, in charge of cysteine biosynthesis, and limits the synthesis of glutathione [200,201]. In correlation with this point, glutamate and glutamine deficiency also regulate ferroptosis [202]. Besides GPX4 activity depletion, suppression of some non-steroidogenic metabolites of the mevalonate pathway enhances some ferroptosis inducers’ sensitivity, such as the ferroptosis activator named FIN56, which acts independently of GPX4 degradation [203]. From this pathway, ubiquinone has emerged as an essential molecule that could modulate ferroptosis [203], which correlates with the early described function as one of the major cellular antioxidants against lipid peroxidation [204,205,206,207]. Ferroptosis is also dependent upon stimulation of several other enzymatic processes, such as the biosynthesis of PUFA-containing phospholipids that are the primary substrate for selective oxygenation by lipoxygenases, the acyl-CoA synthetase long-chain family member 4 (ACSL4), in charge of free fatty acids conversion into fatty CoA esters, and the lysophosphatidylcholine acyltransferase 3 (LPCAT3), which is involved in phospholipid biosynthesis [200]. Iron can also mediate the activation of ferroptosis, and processes and iron import, export, storage, and iron turnover impact the cell sensitivity to ferroptosis [200]. These processed should be summed to the fact that iron is an enzyme effector for non-heme dependent enzymes such as LOXs in charge of the generation of lipid peroxidation products [187,208,209]. Although iron chelators and genetic inhibition of cellular iron uptake can block ferroptosis [210,211], the increase in H2O2 production dependent upon iron can not only be attributed to Fenton’s chemistry [199]. All 15-LOX isoforms, but 15-LOX-1, significantly [187,209], play a crucial role in generating lipid hydroperoxides associated with ferroptosis. Iron has also been implicated in this process since iron chelators can rescue cells from experimental induction of ferroptosis [210,211]. Therefore, there is some controversy on the relative role of enzymatic and non-enzymatic metal-dependent reactions in the generation of lipid hydroperoxides. The combined activity of 15-LOX and iron-binding proteins in ferroptosis are likely to be required to generate phospholipid autoxidation products that participate in the initiation-propagation of the lipid radical chains implicated in the modification of cellular regulatory proteins driving ferroptosis [82,212,213]. Moreover, the activity of the phosphorylase kinase G2 (PHKG2), a key enzyme in the control of cellular iron levels, is necessary to induce ferroptosis in the erastin-induced model, where LOX induced formation of lipid hydroperoxides has been demonstrated as one of the main inducer mechanism of ferroptosis [209].
5. Blockage of Antioxidant Enzymes to Increase Lipid Peroxidation in Tumoral Cells
5.1. GPX4
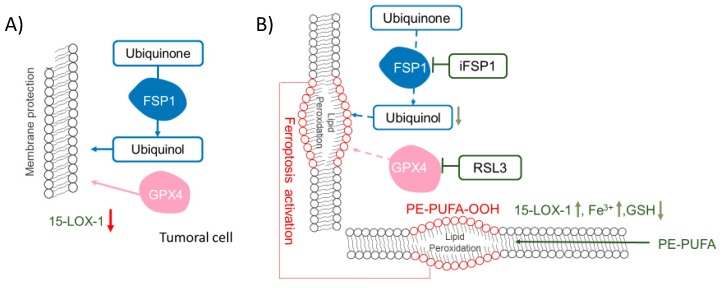
Ferroptosis can be triggered by inhibition of GPX4 (Figure 2), a peroxidase in charge of reducing lipid peroxides at the expense of GSH [140]. Therefore, ferroptosis in cancer can be triggered by inhibition of this enzyme [140], and some efforts have been made to find specific inhibitors; (1S,3R)-RSL-3 (RSL3) was the first described irreversible inhibitor of GPX4 [140,199,209]. Other inhibitors, such as ML210 and ML162, are mesenchymal state-targeting compounds inhibiting GPX4 [214]. Due to GPX4 dependence upon GSH, compounds downregulating cellular GSH levels (such as erastin and sorafenib [199], as well as inhibitors of the xc-cystine/glutamate exchanger system that limits the novo synthesis of GSH [215]), can also promote ferroptosis. GSH depletion also leads to ferroptosis activation in cancer cells and the accumulation of lipid hydroperoxides [216]. Moreover, the ferroptosis suppressor protein 1 (FSP1), an enzyme in charge of ubiquinone reduction, has emerged as a potential pharmacological target to inhibit cellular ferroptosis resistance in the GPX4 deficiency model (Figure 2) [217].
Figure 2.
Glutathione peroxidase 4 (GPX4) and ferroptosis suppressor protein 1 (FSP1) function in cancer cells. Role of ubiquinone reduction through FSP1 and GPX4 in the protection of the membrane against lipid peroxidation in cancer cells (A). In cancer cells, the antioxidant enzymes GPX4 and FSP1, which act on reducing lipid hydroperoxides, would protect them against cell death. Lipid peroxidation and stimulation and ferroptosis induction by the FSP1 and GPX4 inhibitors’ such as iFSP1 and RSL3, respectively (B). By the blockage of these enzymes and stimulation of LOXs, such as 15-LOX-1, lipid peroxidation is prompted. Moreover, substrates of these enzymes and mediators such as GSH and iron could stimulate ferroptosis in cancer cells.
5.2. Quinone Reductases (QRs)
Several recent studies have recently evidenced the role of QRs in cancer cells using a GPX4 deficiency model and have highlighted the potential of ubiquinol and, therefore, QRs as novel targets for cancer treatment (Figure 2). Their role in cancer seems to be related to their capacity to reduce ubiquinone. Reduced ubiquinone is necessary to recycle oxidized alpha-tocopherol and protect membranes from lipid hydroperoxides [204]. Studies using inhibitors of the mevalonate pathway, blocking the ubiquinone synthesis, have evidenced the ubiquinone role in this type of cell death [203]. Some QRs, including the NAD(P)H Quinone Dehydrogenase 1 (NQO1), have been shown to work with a Km value for quinones in the same range reported for FSP1 [217]. Although it is known that NQO1 cannot compete with FSP1 in the reaction with hydrophilic peroxides, the situation is reversed when the substrate is lipid hydroperoxides. Other QRs, with similar or higher Km values for quinones, are also putative targets for cancer treatment combined with GPX4 inhibitors. We proposed a list of described mammalian QRs with reported Km values, the name and structure of the specific inhibitors available for these enzymes, and the IC50 value reported for cancer cells as potential targets to inhibit to promote ferroptosis in conjunction with GPX4 inhibitors (Table 3).
Table 3.
Summary of enzymes with Quinone Reductases (QR) activity, reported kinetic properties, and implication in cancer.
| Name | Km (CoQ) (µM) | Specific Inhibitor with Anti-Cancer Properties | IC50 (µM) and Cancer Cell Line | Structure |
|---|---|---|---|---|
| FSP1 (AFM2) |
12 [217] | 1-amino-3-(4-methylphenyl)-pyrido [1,2-a]benzimidazole-2,4-dicarbonitrile (iFSP1) [217] | ≈1 variety of human cancer cell lines co-treatment with RSL3 [217] |
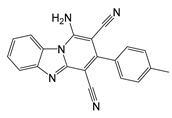
|
| TrxR | 22 [218] | 5-methoxy-1-methyl-3-[(2,4,6-trifluorophenoxy)methyl]indole-4,7-dione [219] | 0.034 (MIA PaCa-2) Human pancreatic cancer [219] |
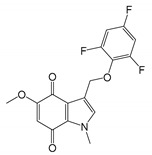
|
| NQO1 | 0.79 [217] | 1-isobutyl-4,6-dimethylpyrido[3,2-g]quinoline-2,5,8,10(1H,9H)-tetraone (IB-DNQ) [220] | 0.08 (A549) Human Lung Cancer [220] |
|
| Cb5R | 625 [221] | N.D. | N.D. | |
| NADH:ubiquinone reductase Complex I |
10 [222] | Rotenone [223] | 0.5 > (MBA-MD-231) Triple negative breast cancer [223] |
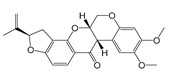
|
| Succinate-quinone oxidoreductase Complex II |
0.3 [224] | 7-chloro-3-methyl-4H-1,2,4-benzothiadiazine 1,1-dioxide (Idra-21) [225] | 0.87 [226] |
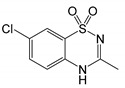
|
| DLD | 5 [227] | Huzhangoside A [228] | 1.5 (A549) Human Lung Cancer [228] |
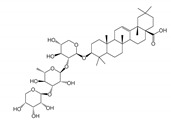
|
| DHODH | 14 [229] | 2-(4-(2,6-difluorophenoxy)-3-isopropoxy-5-methyl-1H-pyrazol-1-yl)-5-ethylpyrimidine (BDBM50070908) [230] | 0.02 (Jurkat cells) Human lymphocytes [231] |
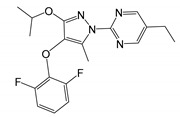
|
Kinetic parameters were obtained from BRENDA enzyme database [89]. N.D. Non-determined.
6. The Future of Nanoparticles (NP) for Cancer Targeting and Tissue Specificity
In the last decade, NPs have emerged as tools for delivering compounds for cancer treatment. Up to date, attempts to generate NPs loaded with lipid hydroperoxides have been hampered due to the high reactivity and instability of lipid hydroperoxides, hindering the proper delivery of intact peroxides into cancer cells. Noteworthy, and based on the evidence accumulated using the pharmacological targets reviewed here, the use of NPs to facilitate the distribution of drugs modulating lipid hydroperoxide generation in cancer patients seems to be of potential pharmacological interest. NPs can incorporate molecules on their surface that preferentially target cancer cells (i.e., folate [232] and 5-(4-hydroxyphenyl)-10,15,20-triphenylporphyrin [233]). The successful delivery of anticancer drugs can be achieved through this strategy [234,235,236,237].
Some recent advances have been made regarding the synthesis of NPs loaded with metals, mainly with iron, which can facilitate lipid peroxidation in cancer cells [234,238,239]. As previously indicated, iron overload produces an increase in random peroxidation products that is entirely unspecific and could lead to harmful oxidative stress in non-cancer cells. Ferroptosis induction has been indirectly associated with the use of pharmacological inhibitors of this type of cell death. However, in some cases, the mechanism of action that induces ferroptosis is unknown and does not seem mediated by inhibition of antioxidant enzymes [237]. Due to iron’s high reactivity, GSH oxidation induced by the metal should be considered a therapeutical approach and could be the main triggering factor leading to ferroptosis activation. Some reports have been published describing ferroptosis induction thought combination therapy where iron NPs are conjugated with ferroptosis inducers, such as the xc-cystine-glutamate exchanger’s inhibitor Sorafenib, that induces glutathione depletion [240], as well as with drugs promoting lysosomes disruption [241,242].
Regarding COX inhibitors, the use of nebulized colloidal poly d,l-lactide-co-glycolide (PLGA) nanoparticles co-encapsulating a COX-2 inhibitor (celecoxib) and a herbal compound (naringenin) has shown promising results for lung cancer treatment in in vitro studies [243]. A similar strategy for the treatment of tumoral glial cells has been reported [244]. As pertaining to LOX inhibitors, we did not find specific reports on their use in combination with NPs to treat cancer. Although some authors reported the photodynamic therapeutic effect of indocyanine green entrapped nanoparticles in skin cancer and the inhibition of COX-2 and 5-LOX, the inhibition mechanism involved remains unknown. More efforts should be made to evaluate the potential applications of NPs to deliver LOX inhibitors for cancer treatment.
Author Contributions
All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Ministerio de Ciencia e Innovación grant number RTI2018-093864-B-I00 and the European Union’s Horizon 2020 Research and Innovation Programme MSCA GA 721236-TREATMENT.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bartsch H., Nair J. Chronic inflammation and oxidative stress in the genesis and perpetuation of cancer: Role of lipid peroxidation, DNA damage, and repair. Langenbeck’s Arch. Surg. 2006;391:499–510. doi: 10.1007/s00423-006-0073-1. [DOI] [PubMed] [Google Scholar]
- 2.Klaunig J.E., Kamendulis L.M. The Role of Oxidative Stress in Carcinogenesis. Annu. Rev. Pharmacol. Toxicol. 2004;44:239–267. doi: 10.1146/annurev.pharmtox.44.101802.121851. [DOI] [PubMed] [Google Scholar]
- 3.Taniguchi K., Karin M. NF-κB, inflammation, immunity and cancer: Coming of age. Nat. Rev. Immunol. 2018;18:309–324. doi: 10.1038/nri.2017.142. [DOI] [PubMed] [Google Scholar]
- 4.Elinav E., Nowarski R., Thaiss C.A., Hu B., Jin C., Flavell R.A. Inflammation-induced cancer: Crosstalk between tumours, immune cells and microorganisms. Nat. Rev. Cancer. 2013;13:759–771. doi: 10.1038/nrc3611. [DOI] [PubMed] [Google Scholar]
- 5.Gorrini C., Harris I.S., Mak T.W. Modulation of oxidative stress as an anticancer strategy. Nat. Rev. Drug Discov. 2013;12:931–947. doi: 10.1038/nrd4002. [DOI] [PubMed] [Google Scholar]
- 6.Sever R., Brugge J.S. Signal transduction in cancer. Cold Spring Harb. Perspect. Med. 2015;5:a006098. doi: 10.1101/cshperspect.a006098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chaiswing L., St Clair W.H., St Clair D.K. Redox Paradox: A Novel Approach to Therapeutics-Resistant Cancer. Antioxid. Redox Signal. 2018;29:1237–1272. doi: 10.1089/ars.2017.7485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sznarkowska A., Kostecka A., Meller K., Bielawski K.P. Inhibition of cancer antioxidant defense by natural compounds. Oncotarget. 2016;8:15996. doi: 10.18632/oncotarget.13723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Perillo B., Di Donato M., Pezone A., Di Zazzo E., Giovannelli P., Galasso G., Castoria G., Migliaccio A. ROS in cancer therapy: The bright side of the moon. Exp. Mol. Med. 2020;52:192–203. doi: 10.1038/s12276-020-0384-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Colombo S., Melo T., Martínez-López M., Carrasco M.J., Domingues M.R., Pérez-Sala D., Domingues P. Phospholipidome of endothelial cells shows a different adaptation response upon oxidative, glycative and lipoxidative stress. Sci. Rep. 2018;8:12365. doi: 10.1038/s41598-018-30695-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hazen S.L. Oxidized phospholipids as endogenous pattern recognition ligands in innate immunity. J. Biol. Chem. 2008;283:15527–15531. doi: 10.1074/jbc.R700054200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dennis E.A. Liberating Chiral Lipid Mediators, Inflammatory Enzymes, and LIPID MAPS from Biological Grease. J. Biol. Chem. 2016;291:24431–24448. doi: 10.1074/jbc.X116.723791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Freigang S. The regulation of inflammation by oxidized phospholipids. Eur. J. Immunol. 2016;46:1818–1825. doi: 10.1002/eji.201545676. [DOI] [PubMed] [Google Scholar]
- 14.Miller Y.I., Shyy J.Y.J. Context-Dependent Role of Oxidized Lipids and Lipoproteins in Inflammation. Trends Endocrinol. Metab. 2017;28:143–152. doi: 10.1016/j.tem.2016.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dias I.H.K., Milic I., Heiss C., Ademowo O.S., Polidori M.C., Devitt A., Griffiths H.R. Inflammation, Lipid (Per)oxidation, and Redox Regulation. Antioxid. Redox Signal. 2020;33:166–190. doi: 10.1089/ars.2020.8022. [DOI] [PubMed] [Google Scholar]
- 16.Van der Paal J., Neyts E.C., Verlackt C.C.W., Bogaerts A. Effect of lipid peroxidation on membrane permeability of cancer and normal cells subjected to oxidative stress. Chem. Sci. 2016;7:489–498. doi: 10.1039/C5SC02311D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Catalá A. Lipid peroxidation modifies the picture of membranes from the “Fluid Mosaic Model” to the “Lipid Whisker Model”. Biochimie. 2012;94:101–109. doi: 10.1016/j.biochi.2011.09.025. [DOI] [PubMed] [Google Scholar]
- 18.Mouchlis V.D., Dennis E.A. Phospholipase A(2) catalysis and lipid mediator lipidomics. Biochim. Biophys. Acta. Mol. Cell Biol. Lipids. 2019;1864:766–771. doi: 10.1016/j.bbalip.2018.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Xu Y., Qian S.Y. Anti-cancer activities of ω-6 polyunsaturated fatty acids. Biomed. J. 2014;37:112–119. doi: 10.4103/2319-4170.131378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Anderson D.W., Crowle A.J. Regression and differentiation of neuroblastoma tumors in mice treated with differentiating agents-prostaglandin E1 and a phosphodiesterase inhibitor, RO 20-1724. Cancer Lett. 1982;16:287–295. doi: 10.1016/0304-3835(82)90009-X. [DOI] [PubMed] [Google Scholar]
- 21.Hanazaki K., Kajikawa S., Fujimori Y., Nakata S., Shimozawa N., Koide N., Adachi W., Amano J. Effects of prostaglandin E1 administration during hepatectomy for cirrhotic hepatocellular carcinoma. Hepatogastroenterology. 2000;47:461–464. [PubMed] [Google Scholar]
- 22.Wang X., Lin H., Gu Y. Multiple roles of dihomo-γ-linolenic acid against proliferation diseases. Lipids Health Dis. 2012;11:25. doi: 10.1186/1476-511X-11-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Davies P., Bailey P.J., Goldenberg M.M., Ford-Hutchinson A.W. The Role of Arachidonic Acid Oxygenation Products in Pain and Inflammation. Annu. Rev. Immunol. 1984;2:335–357. doi: 10.1146/annurev.iy.02.040184.002003. [DOI] [PubMed] [Google Scholar]
- 24.Castellone M.D., Teramoto H., Williams B.O., Druey K.M., Gutkind J.S. Prostaglandin E2 promotes colon cancer cell growth through a Gs-axin-beta-catenin signaling axis. Science. 2005;310:1504–1510. doi: 10.1126/science.1116221. [DOI] [PubMed] [Google Scholar]
- 25.Pai R., Soreghan B., Szabo I.L., Pavelka M., Baatar D., Tarnawski A.S. Prostaglandin E2 transactivates EGF receptor: A novel mechanism for promoting colon cancer growth and gastrointestinal hypertrophy. Nat. Med. 2002;8:289–293. doi: 10.1038/nm0302-289. [DOI] [PubMed] [Google Scholar]
- 26.Schrey M.P., Patel K.V. Prostaglandin E2 production and metabolism in human breast cancer cells and breast fibroblasts. Regulation by inflammatory mediators. Br. J. Cancer. 1995;72:1412–1419. doi: 10.1038/bjc.1995.523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Uotila P. Inhibition of prostaglandin E2 formation and histamine action in cancer immunotherapy. Cancer Immunol. Immunother. 1993;37:251–254. doi: 10.1007/BF01518519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang D., Dubois R.N. Eicosanoids and cancer. Nat. Rev. Cancer. 2010;10:181–193. doi: 10.1038/nrc2809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tachtsis B., Whitfield J., Hawley J.A., Hoffman N.J. Omega-3 Polyunsaturated Fatty Acids Mitigate Palmitate-Induced Impairments in Skeletal Muscle Cell Viability and Differentiation. Front. Physiol. 2020;11 doi: 10.3389/fphys.2020.00563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Magtanong L., Ko P.J., Dixon S.J. Emerging roles for lipids in non-apoptotic cell death. Cell Death Differ. 2016;23:1099–1109. doi: 10.1038/cdd.2016.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Khadge S., Sharp J.G., McGuire T.R., Thiele G.M., Talmadge J.E. Lipid Inflammatory Mediators in Cancer Progression and Therapy. In: Kalinski P., editor. Tumor Immune Microenvironment in Cancer Progression and Cancer Therapy. Springer International Publishing; Cham, Switzerland: 2017. pp. 145–156. [DOI] [PubMed] [Google Scholar]
- 32.Zhang Q., Zhu B., Li Y. Resolution of Cancer-Promoting Inflammation: A New Approach for Anticancer Therapy. Front. Immunol. 2017;8:71. doi: 10.3389/fimmu.2017.00071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ungaro F., D’Alessio S., Danese S. The Role of Pro-Resolving Lipid Mediators in Colorectal Cancer-Associated Inflammation: Implications for Therapeutic Strategies. Cancers. 2020;12:2060. doi: 10.3390/cancers12082060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rigas B., Goldman I.S., Levine L. Altered eicosanoid levels in human colon cancer. J. Lab. Clin. Med. 1993;122:518–523. [PubMed] [Google Scholar]
- 35.Wang D., DuBois R.N. Cyclooxygenase-2: A potential target in breast cancer. Semin. Oncol. 2004;31:64–73. doi: 10.1053/j.seminoncol.2004.01.008. [DOI] [PubMed] [Google Scholar]
- 36.Koppenol W.H. The centennial of the Fenton reaction. Free Radic. Biol. Med. 1993;15:645–651. doi: 10.1016/0891-5849(93)90168-T. [DOI] [PubMed] [Google Scholar]
- 37.Koppenol W.H. The Haber-Weiss cycle—70 years later. Redox Rep. 2001;6:229–234. doi: 10.1179/135100001101536373. [DOI] [PubMed] [Google Scholar]
- 38.Halliwell B., Gutteridge J.M.C. Free Radicals in Biology and Medicine. 4th ed. Oxford University Press; Oxford, UK: 2007. [Google Scholar]
- 39.Johnson D.R., Decker E.A. The Role of Oxygen in Lipid Oxidation Reactions: A Review. Annu. Rev. Food Sci. Technol. 2015;6:171–190. doi: 10.1146/annurev-food-022814-015532. [DOI] [PubMed] [Google Scholar]
- 40.Schafer F.Q., Qian S.Y., Buettner G.R. Iron and free radical oxidations in cell membranes. Cell Mol. Biol. 2000;46:657–662. [PMC free article] [PubMed] [Google Scholar]
- 41.Qian S.Y., Buettner G.R. Iron and dioxygen chemistry is an important route to initiation of biological free radical oxidations: An electron paramagnetic resonance spin trapping study. Free Radic. Biol. Med. 1999;26:1447–1456. doi: 10.1016/S0891-5849(99)00002-7. [DOI] [PubMed] [Google Scholar]
- 42.Minotti G., Aust S.D. The role of iron in the initiation of lipid peroxidation. Chem. Phys. Lipids. 1987;44:191–208. doi: 10.1016/0009-3084(87)90050-8. [DOI] [PubMed] [Google Scholar]
- 43.Reis A., Spickett C.M. Chemistry of phospholipid oxidation. Biochim. Biophys. Acta (BBA)-Biomembr. 2012;1818:2374–2387. doi: 10.1016/j.bbamem.2012.02.002. [DOI] [PubMed] [Google Scholar]
- 44.Pratt D.A., Tallman K.A., Porter N.A. Free radical oxidation of polyunsaturated lipids: New mechanistic insights and the development of peroxyl radical clocks. Acc Chem. Res. 2011;44:458–467. doi: 10.1021/ar200024c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Repetto M.G., Ferrarotti N.F., Boveris A. The involvement of transition metal ions on iron-dependent lipid peroxidation. Arch. Toxicol. 2010;84:255–262. doi: 10.1007/s00204-009-0487-y. [DOI] [PubMed] [Google Scholar]
- 46.Repetto M., Boveris A. Transition Metals: Bioinorganic and Redox Reactions in Biological Systems. Nova Science Publishers Inc.; New York, NY, USA: 2011. pp. 349–370. Transition Metals: Characteristics, Properties and Uses. [Google Scholar]
- 47.Pike L.J., Han X., Chung K.-N., Gross R.W. Lipid Rafts Are Enriched in Arachidonic Acid and Plasmenylethanolamine and Their Composition Is Independent of Caveolin-1 Expression: A Quantitative Electrospray Ionization/Mass Spectrometric Analysis. Biochemistry. 2002;41:2075–2088. doi: 10.1021/bi0156557. [DOI] [PubMed] [Google Scholar]
- 48.Gutierrez-Merino C., Marques-da-Silva D., Fortalezas S., Samhan-Arias A.K. The critical role of lipid rafts nanodomains in the cross-talk between calcium and reactive oxygen and nitrogen species in cerebellar granule neurons apoptosis by extracellular potassium deprivation. Aims. Mol. Sci. 2016;3:12–29. doi: 10.3934/molsci.2016.1.12. [DOI] [Google Scholar]
- 49.Yaqoob P. Fatty acids as gatekeepers of immune cell regulation. Trends Immunol. 2003;24:639–645. doi: 10.1016/j.it.2003.10.002. [DOI] [PubMed] [Google Scholar]
- 50.Tyurina Y.Y., Tyurin V.A., Kapralova V.I., Amoscato A.A., Epperly M.W., Greenberger J.S., Kagan V.E. Mass-Spectrometric Characterization of Phospholipids and Their Hydroperoxide Derivatives In Vivo: Effects of Total Body Irradiation. In: Armstrong D., editor. Lipidomics: Volume 2: Methods and Protocols. Humana Press; Totowa, NJ, USA: 2010. pp. 153–183. [DOI] [PubMed] [Google Scholar]
- 51.Stark G. The effect of ionizing radiation on lipid membranes. Biochim. Biophys. Acta (BBA)-Rev. Biomembr. 1991;1071:103–122. doi: 10.1016/0304-4157(91)90020-W. [DOI] [PubMed] [Google Scholar]
- 52.Corre I., Niaudet C., Paris F. Plasma membrane signaling induced by ionizing radiation. Mutat. Res. Rev. Mutat. Res. 2010;704:61–67. doi: 10.1016/j.mrrev.2010.01.014. [DOI] [PubMed] [Google Scholar]
- 53.Emerit J., Klein J.M., Coutellier A., Congy F. [Free radicals and lipid peroxidation in cell biology: Physiopathologic prospects] Pathol. Biol. (Paris) 1991;39:316–327. [PubMed] [Google Scholar]
- 54.Vlasova I.I. Peroxidase Activity of Human Hemoproteins: Keeping the Fire under Control. Molecules. 2018;23:2561. doi: 10.3390/molecules23102561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kagan V.E., Tyurin V.A., Jiang J., Tyurina Y.Y., Ritov V.B., Amoscato A.A., Osipov A.N., Belikova N.A., Kapralov A.A., Kini V., et al. Cytochrome c acts as a cardiolipin oxygenase required for release of proapoptotic factors. Nat. Chem. Biol. 2005;1:223–232. doi: 10.1038/nchembio727. [DOI] [PubMed] [Google Scholar]
- 56.Ji J., Kline A.E., Amoscato A., Samhan-Arias A.K., Sparvero L.J., Tyurin V.A., Tyurina Y.Y., Fink B., Manole M.D., Puccio A.M., et al. Lipidomics identifies cardiolipin oxidation as a mitochondrial target for redox therapy of brain injury. Nat. Neurosci. 2012;15:1407–1413. doi: 10.1038/nn.3195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Atkinson J., Kapralov A.A., Yanamala N., Tyurina Y.Y., Amoscato A.A., Pearce L., Peterson J., Huang Z., Jiang J., Samhan-Arias A.K., et al. A mitochondria-targeted inhibitor of cytochrome c peroxidase mitigates radiation-induced death. Nat. Commun. 2011;2:497. doi: 10.1038/ncomms1499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Samhan-Arias A.K., Tyurina Y.Y., Kagan V.E. Lipid antioxidants: Free radical scavenging versus regulation of enzymatic lipid peroxidation. J. Clin. Biochem. Nutr. 2011;48:91–95. doi: 10.3164/jcbn.11-009FR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Belikova N.A., Tyurina Y.Y., Borisenko G., Tyurin V., Samhan Arias A.K., Yanamala N., Furtmuller P.G., Klein-Seetharaman J., Obinger C., Kagan V.E. Heterolytic reduction of fatty acid hydroperoxides by cytochrome c/cardiolipin complexes: Antioxidant function in mitochondria. J. Am. Chem. Soc. 2009;131:11288–11289. doi: 10.1021/ja904343c. [DOI] [PubMed] [Google Scholar]
- 60.Samhan-Arias A.K., Cordas C.M., Carepo M.S., Maia L.B., Gutierrez-Merino C., Moura I., Moura J.J.G. Ligand accessibility to heme cytochrome b5 coordinating sphere and enzymatic activity enhancement upon tyrosine ionization. J. Biol. Inorg. Chem. A Publ. Soc. Biol. Inorg. Chem. 2019;24:317–330. doi: 10.1007/s00775-019-01649-2. [DOI] [PubMed] [Google Scholar]
- 61.Samhan-Arias A.K., Maia L.B., Cordas C.M., Moura I., Gutierrez-Merino C., Moura J.J.G. Peroxidase-like activity of cytochrome b5 is triggered upon hemichrome formation in alkaline pH. Biochim. Biophys. Acta Proteins Proteom. 2018;1866:373–378. doi: 10.1016/j.bbapap.2017.09.010. [DOI] [PubMed] [Google Scholar]
- 62.Ascenzi P., Coletta M., Wilson M.T., Fiorucci L., Marino M., Polticelli F., Sinibaldi F., Santucci R. Cardiolipin–cytochrome c complex: Switching cytochrome c from an electron-transfer shuttle to a myoglobin- and a peroxidase-like heme-protein. Iubmb Life. 2015;67:98–109. doi: 10.1002/iub.1350. [DOI] [PubMed] [Google Scholar]
- 63.Beckerson P., Svistunenko D., Reeder B. Effect of the distal histidine on the peroxidatic activity of monomeric cytoglobin. F1000Res. 2015;4:87. doi: 10.12688/f1000research.5971.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Poulos T.L. Heme enzyme structure and function. Chem. Rev. 2014;114:3919–3962. doi: 10.1021/cr400415k. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ayala A., Muñoz M.F., Argüelles S. Lipid Peroxidation: Production, Metabolism, and Signaling Mechanisms of Malondialdehyde and 4-Hydroxy-2-Nonenal. Oxidative Med. Cell. Longev. 2014;2014:360438. doi: 10.1155/2014/360438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Eberhart C.E., Coffey R.J., Radhika A., Giardiello F.M., Ferrenbach S., Dubois R.N. Up-regulation of cyclooxygenase 2 gene expression in human colorectal adenomas and adenocarcinomas. Gastroenterology. 1994;107:1183–1188. doi: 10.1016/0016-5085(94)90246-1. [DOI] [PubMed] [Google Scholar]
- 67.Ferrandina G., Lauriola L., Zannoni G.F., Distefano M.G., Legge F., Salutari V., Gessi M., Maggiano N., Scambia G., Ranelletti F.O. Expression of cyclooxygenase-2 (COX-2) in tumour and stroma compartments in cervical cancer: Clinical implications. Br. J. Cancer. 2002;87:1145–1152. doi: 10.1038/sj.bjc.6600578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Tian F., Wang T.Y., Gong M., Lu X.M., Hu J., Wang J., Zhang C.H. [Overexpression of COX-2 and its clinical significance in non-small cell lung cancer] Zhonghua Wai Ke Za Zhi. 2003;41:407–410. [PubMed] [Google Scholar]
- 69.Brattstrom D., Wester K., Bergqvist M., Hesselius P., Malmstrom P.U., Nordgren H., Wagenius G., Brodin O. HER-2, EGFR, COX-2 expression status correlated to microvessel density and survival in resected non-small cell lung cancer. Acta Oncol. 2004;43:80–86. doi: 10.1080/02841860310017441. [DOI] [PubMed] [Google Scholar]
- 70.Liao Z., Milas L. COX-2 and its inhibition as a molecular target in the prevention and treatment of lung cancer. Expert Rev. Anticancer Ther. 2004;4:543–560. doi: 10.1586/14737140.4.4.543. [DOI] [PubMed] [Google Scholar]
- 71.Nix P., Lind M., Greenman J., Stafford N., Cawkwell L. Expression of Cox-2 protein in radioresistant laryngeal cancer. Ann. Oncol. 2004;15:797–801. doi: 10.1093/annonc/mdh185. [DOI] [PubMed] [Google Scholar]
- 72.Panagopoulos V., Leach D.A., Zinonos I., Ponomarev V., Licari G., Liapis V., Ingman W.V., Anderson P., DeNichilo M.O., Evdokiou A. Inflammatory peroxidases promote breast cancer progression in mice via regulation of the tumour microenvironment. Int. J. Oncol. 2017;50:1191–1200. doi: 10.3892/ijo.2017.3883. [DOI] [PubMed] [Google Scholar]
- 73.Tabariès S., Ouellet V., Hsu B.E., Annis M.G., Rose A.A.N., Meunier L., Carmona E., Tam C.E., Mes-Masson A.-M., Siegel P.M. Granulocytic immune infiltrates are essential for the efficient formation of breast cancer liver metastases. Breast Cancer Res. 2015;17:45. doi: 10.1186/s13058-015-0558-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Samoszuk M., Lin F., Rim P., Strathearn G. New marker for blood vessels in human ovarian and endometrial cancers. Clin. Cancer Res. 1996;2:1867–1871. [PubMed] [Google Scholar]
- 75.Cormier S.A., Taranova A.G., Bedient C., Nguyen T., Protheroe C., Pero R., Dimina D., Ochkur S.I., O’Neill K., Colbert D., et al. Pivotal Advance: Eosinophil infiltration of solid tumors is an early and persistent inflammatory host response. J. Leukoc. Biol. 2006;79:1131–1139. doi: 10.1189/jlb.0106027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Hou Z., Falcone D.J., Subbaramaiah K., Dannenberg A.J. Macrophages induce COX-2 expression in breast cancer cells: Role of IL-1beta autoamplification. Carcinogenesis. 2011;32:695–702. doi: 10.1093/carcin/bgr027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Mustea A., Heinze G., Sehouli J., Koensgen D., Wolf A., Gutu L., Sofroni D., Pirvulescu C., Braicu E.I., Schuster E., et al. The -463G/A polymorphism in myeloperoxidase gene and cervical cancer. Anticancer Res. 2007;27:1531–1535. [PubMed] [Google Scholar]
- 78.Zhu H., Yang L., Zhou B., Yu R., Tang N., Wang B. Myeloperoxidase G-463A polymorphism and the risk of gastric cancer: A case-control study. Carcinogenesis. 2006;27:2491–2496. doi: 10.1093/carcin/bgl121. [DOI] [PubMed] [Google Scholar]
- 79.London S.J., Lehman T.A., Taylor J.A. Myeloperoxidase genetic polymorphism and lung cancer risk. Cancer Res. 1997;57:5001–5003. [PubMed] [Google Scholar]
- 80.Limami Y., Pinon A., Leger D.Y., Pinault E., Delage C., Beneytout J.-L., Simon A., Liagre B. The P2Y2/Src/p38/COX-2 pathway is involved in the resistance to ursolic acid-induced apoptosis in colorectal and prostate cancer cells. Biochimie. 2012;94:1754–1763. doi: 10.1016/j.biochi.2012.04.006. [DOI] [PubMed] [Google Scholar]
- 81.Berger S., Weichert H., Porzel A., Wasternack C., Kuhn H., Feussner I. Enzymatic and non-enzymatic lipid peroxidation in leaf development. Biochim. Biophys. Acta. 2001;1533:266–276. doi: 10.1016/S1388-1981(01)00161-5. [DOI] [PubMed] [Google Scholar]
- 82.Stoyanovsky D.A., Tyurina Y.Y., Shrivastava I., Bahar I., Tyurin V.A., Protchenko O., Jadhav S., Bolevich S.B., Kozlov A.V., Vladimirov Y.A., et al. Iron catalysis of lipid peroxidation in ferroptosis: Regulated enzymatic or random free radical reaction? Free Radic. Biol. Med. 2019;133:153–161. doi: 10.1016/j.freeradbiomed.2018.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Noguchi N., Yamashita H., Hamahara J., Nakamura A., Kuhn H., Niki E. The specificity of lipoxygenase-catalyzed lipid peroxidation and the effects of radical-scavenging antioxidants. Biol. Chem. 2002;383:619–626. doi: 10.1515/BC.2002.064. [DOI] [PubMed] [Google Scholar]
- 84.Drew D.A., Cao Y., Chan A.T. Aspirin and colorectal cancer: The promise of precision chemoprevention. Nat. Rev. Cancer. 2016;16:173–186. doi: 10.1038/nrc.2016.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Elwood P.C., Morgan G., Pickering J.E., Galante J., Weightman A.L., Morris D., Kelson M., Dolwani S. Aspirin in the Treatment of Cancer: Reductions in Metastatic Spread and in Mortality: A Systematic Review and Meta-Analyses of Published Studies. PLoS ONE. 2016;11:e0152402. doi: 10.1371/journal.pone.0152402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Dong L., Anderson A.J., Malkowski M.G. Arg-513 and Leu-531 Are Key Residues Governing Time-Dependent Inhibition of Cyclooxygenase-2 by Aspirin and Celebrex. Biochemistry. 2019;58:3990–4002. doi: 10.1021/acs.biochem.9b00659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Lucido M.J., Orlando B.J., Vecchio A.J., Malkowski M.G. Crystal Structure of Aspirin-Acetylated Human Cyclooxygenase-2: Insight into the Formation of Products with Reversed Stereochemistry. Biochemistry. 2016;55:1226–1238. doi: 10.1021/acs.biochem.5b01378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Giménez-Bastida J.A., Boeglin W.E., Boutaud O., Malkowski M.G., Schneider C. Residual cyclooxygenase activity of aspirin-acetylated COX-2 forms 15 R-prostaglandins that inhibit platelet aggregation. FASEB J. Off. Publ. Fed. Am. Soc. Exp. Biol. 2019;33:1033–1041. doi: 10.1096/fj.201801018R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Jeske L., Placzek S., Schomburg I., Chang A., Schomburg D. BRENDA in 2019: A European ELIXIR core data resource. Nucleic Acids Res. 2018;47:D542–D549. doi: 10.1093/nar/gky1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Fan X.M., Zheng F.S., Liu H.Y., Ma Y.H., Wong B.C. [Mechanism of apoptosis induced by specific COX-2 inhibitor SC236 in gastric cancer cells] Zhonghua Zhong Liu Za Zhi. 2005;27:145–147. [PubMed] [Google Scholar]
- 91.Ott I., Schmidt K., Kircher B., Schumacher P., Wiglenda T., Gust R. Antitumor-Active Cobalt−Alkyne Complexes Derived from Acetylsalicylic Acid: Studies on the Mode of Drug Action. J. Med. Chem. 2005;48:622–629. doi: 10.1021/jm049326z. [DOI] [PubMed] [Google Scholar]
- 92.Zanellato I., Bonarrigo I., Ravera M., Gabano E., Gust R., Osella D. The hexacarbonyldicobalt derivative of aspirin acts as a CO-releasing NSAID on malignant mesothelioma cells. Met. Integr. Biometal Sci. 2013;5:1604–1613. doi: 10.1039/c3mt00117b. [DOI] [PubMed] [Google Scholar]
- 93.Soumaoro L.T., Uetake H., Takagi Y., Iida S., Higuchi T., Yasuno M., Enomoto M., Sugihara K. Coexpression of VEGF-C and Cox-2 in human colorectal cancer and its association with lymph node metastasis. Dis. Colon Rectum. 2006;49:392–398. doi: 10.1007/s10350-005-0247-x. [DOI] [PubMed] [Google Scholar]
- 94.Peng Z.H., Wan D.S., Li L.R., Chen G., Lu Z.H., Wu X.J., Kong L.H., Pan Z.Z. Expression of COX-2, MMP-2 and VEGF in stage II and III colorectal cancer and the clinical significance. Hepatogastroenterology. 2011;58:369–376. [PubMed] [Google Scholar]
- 95.Ferrandina G., Lauriola L., Zannoni G.F., Fagotti A., Fanfani F., Legge F., Maggiano N., Gessi M., Mancuso S., Ranelletti F.O., et al. Increased cyclooxygenase-2 (COX-2) expression is associated with chemotherapy resistance and outcome in ovarian cancer patients. Ann. Oncol. 2002;13:1205–1211. doi: 10.1093/annonc/mdf207. [DOI] [PubMed] [Google Scholar]
- 96.Ferrandina G., Ranelletti F.O., Lauriola L., Fanfani F., Legge F., Mottolese M., Nicotra M.R., Natali P.G., Zakut V.H., Scambia G. Cyclooxygenase-2 (COX-2), epidermal growth factor receptor (EGFR), and Her-2/neu expression in ovarian cancer. Gynecol. Oncol. 2002;85:305–310. doi: 10.1006/gyno.2002.6620. [DOI] [PubMed] [Google Scholar]
- 97.Denkert C., Köbel M., Pest S., Koch I., Berger S., Schwabe M., Siegert A., Reles A., Klosterhalfen B., Hauptmann S. Expression of Cyclooxygenase 2 Is an Independent Prognostic Factor in Human Ovarian Carcinoma. Am. J. Pathol. 2002;160:893–903. doi: 10.1016/S0002-9440(10)64912-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Ristimäki A., Sivula A., Lundin J., Lundin M., Salminen T., Haglund C., Joensuu H., Isola J. Prognostic Significance of Elevated Cyclooxygenase-2 Expression in Breast Cancer. Cancer Res. 2002;62:632–635. [PubMed] [Google Scholar]
- 99.Mazhar D., Ang R., Waxman J. COX inhibitors and breast cancer. Br. J. Cancer. 2006;94:346–350. doi: 10.1038/sj.bjc.6602942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Fulton A.M., Heppner G.H. Relationships of Prostaglandin E and Natural Killer Sensitivity to Metastatic Potential in Murine Mammary Adenocarcinomas. Cancer Res. 1985;45:4779–4784. [PubMed] [Google Scholar]
- 101.Singh B., Berry J.A., Vincent L.E., Lucci A. Involvement of IL-8 in COX-2-mediated bone metastases from breast cancer. J. Surg. Res. 2006;134:44–51. doi: 10.1016/j.jss.2006.03.018. [DOI] [PubMed] [Google Scholar]
- 102.Majumder M., Dunn L., Liu L., Hasan A., Vincent K., Brackstone M., Hess D., Lala P.K. COX-2 induces oncogenic micro RNA miR655 in human breast cancer. Sci. Rep. 2018;8:327. doi: 10.1038/s41598-017-18612-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Barnes N., Haywood P., Flint P., Knox W.F., Bundred N.J. Survivin expression in in situ and invasive breast cancer relates to COX-2 expression and DCIS recurrence. Br. J. Cancer. 2006;94:253–258. doi: 10.1038/sj.bjc.6602932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Nie F., Yu X.L., Wang X.G., Tang Y.F., Wang L.L., Ma L. Down-regulation of CacyBP is associated with poor prognosis and the effects on COX-2 expression in breast cancer. Int. J. Oncol. 2010;37:1261–1269. doi: 10.3892/ijo_00000777. [DOI] [PubMed] [Google Scholar]
- 105.Li E.X., Wu Y.Y., Shi F., Wu Y., Guo J.J., Dong D.F. [Relationship between serum VEGF level and VEGF, COX-2 and MVD expression in breast cancer tissues] Zhonghua Zhong Liu Za Zhi. 2007;29:522–525. [PubMed] [Google Scholar]
- 106.Siironen P., Ristimäki A., Nordling S., Louhimo J., Haapiainen R., Haglund C. Expression of COX-2 is increased with age in papillary thyroid cancer. Histopathology. 2004;44:490–497. doi: 10.1111/j.1365-2559.2004.01880. [DOI] [PubMed] [Google Scholar]
- 107.Siironen P., Ristimaki A., Narko K., Nordling S., Louhimo J., Andersson S., Haapiainen R., Haglund C. VEGF-C and COX-2 expression in papillary thyroid cancer. Endocr. Relat. Cancer. 2006;13:465–473. doi: 10.1677/erc.1.01114. [DOI] [PubMed] [Google Scholar]
- 108.Fujiwaki R., Iida K., Kanasaki H., Ozaki T., Hata K., Miyazaki K. Cyclooxygenase-2 expression in endometrial cancer: Correlation with microvessel count and expression of vascular endothelial growth factor and thymidine phosphorylase. Hum. Pathol. 2002;33:213–219. doi: 10.1053/hupa.2002.31292. [DOI] [PubMed] [Google Scholar]
- 109.Landen C.N., Mathur S.P., Richardson M.S., Creasman W.T. Expression of cyclooxygenase-2 in cervical, endometrial, and ovarian malignancies. Am. J. Obstet. Gynecol. 2003;188:1174–1176. doi: 10.1067/mob.2003.284. [DOI] [PubMed] [Google Scholar]
- 110.Ferrandina G., Ranelletti F.O., Gallotta V., Martinelli E., Zannoni G.F., Gessi M., Scambia G. Expression of cyclooxygenase-2 (COX-2), receptors for estrogen (ER), and progesterone (PR), p53, ki67, and neu protein in endometrial cancer. Gynecol. Oncol. 2005;98:383–389. doi: 10.1016/j.ygyno.2005.04.024. [DOI] [PubMed] [Google Scholar]
- 111.Fowler J.M., Ramirez N., Cohn D.E., Kelbick N., Pavelka J., Ben-Shachar I., Morrison C. Correlation of cyclooxygenase-2 (COX-2) and aromatase expression in human endometrial cancer: Tissue microarray analysis. Am. J. Obstet. Gynecol. 2005;192:1262–1271. doi: 10.1016/j.ajog.2005.01.009. [DOI] [PubMed] [Google Scholar]
- 112.Moon W.S., Park H.S., Lee H., Pai R., Tarnawski A.S., Kim K.R., Jang K.Y. Co-expression of cox-2, C-met and beta-catenin in cells forming invasive front of gallbladder cancer. Cancer Res. Treat. 2005;37:171–176. doi: 10.4143/crt.2005.37.3.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Rubio J., Ramos D., Lopez-Guerrero J.A., Iborra I., Collado A., Solsona E., Almenar S., Llombart-Bosch A. Immunohistochemical expression of Ki-67 antigen, cox-2 and Bax/Bcl-2 in prostate cancer; prognostic value in biopsies and radical prostatectomy specimens. Eur. Urol. 2005;48:745–751. doi: 10.1016/j.eururo.2005.06.014. [DOI] [PubMed] [Google Scholar]
- 114.Cohen B.L., Gomez P., Omori Y., Duncan R.C., Civantos F., Soloway M.S., Lokeshwar V.B., Lokeshwar B.L. Cyclooxygenase-2 (COX-2) expression is an independent predictor of prostate cancer recurrence. Int. J. Cancer. 2006;119:1082–1087. doi: 10.1002/ijc.21749. [DOI] [PubMed] [Google Scholar]
- 115.Rao D.S., Gui D., Koski M.E., Popoviciu L.M., Wang H., Reiter R.E., Said J.W. An Inverse Relation Between COX-2 and E-cadherin Expression Correlates With Aggressive Histologic Features in Prostate Cancer. Appl. Immunohistochem. Mol. Morphol. 2006;14:375–383. doi: 10.1097/01.pai.0000210417.61117.6c. [DOI] [PubMed] [Google Scholar]
- 116.Richardsen E., Uglehus R.D., Due J., Busch C., Busund L.T. COX-2 is overexpressed in primary prostate cancer with metastatic potential and may predict survival. A comparison study between COX-2, TGF-beta, IL-10 and Ki67. Cancer Epidemiol. 2010;34:316–322. doi: 10.1016/j.canep.2010.03.019. [DOI] [PubMed] [Google Scholar]
- 117.Li M., Liu W., Zhu Y.F., Chen Y.L., Zhang B.Z., Wang R. Correlation of COX-2 and K-ras expression to clinical outcome in gastric cancer. Acta Oncol. 2006;45:1115–1119. doi: 10.1080/02841860601043066. [DOI] [PubMed] [Google Scholar]
- 118.Mrena J., Wiksten J.P., Nordling S., Kokkola A., Ristimäki A., Haglund C. MMP-2 but not MMP-9 associated with COX-2 and survival in gastric cancer. J. Clin. Pathol. 2006;59:618–623. doi: 10.1136/jcp.2005.033761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Jo H., Kang S., Kim J.W., Kang G.H., Park N.H., Song Y.S., Park S.Y., Kang S.B., Lee H.P. Hypermethylation of the COX-2 gene is a potential prognostic marker for cervical cancer. J. Obs. Gynaecol. Res. 2007;33:236–241. doi: 10.1111/j.1447-0756.2007.00517.x. [DOI] [PubMed] [Google Scholar]
- 120.Matsumoto G., Muta M., Tsuruta K., Horiguchi S., Karasawa K., Okamoto A. Tumor size significantly correlates with postoperative liver metastases and COX-2 expression in patients with resectable pancreatic cancer. Pancreatology. 2007;7:167–173. doi: 10.1159/000104241. [DOI] [PubMed] [Google Scholar]
- 121.Matsubayashi H., Infante J.R., Winter J., Klein A.P., Schulick R., Hruban R., Visvanathan K., Goggins M. Tumor COX-2 expression and prognosis of patients with resectable pancreatic cancer. Cancer Biol. 2007;6:1569–1575. doi: 10.4161/cbt.6.10.4711. [DOI] [PubMed] [Google Scholar]
- 122.Bergmann F., Moldenhauer G., Herpel E., Gaida M.M., Strobel O., Werner J., Esposito I., Muerkoster S.S., Schirmacher P., Kern M.A. Expression of L1CAM, COX-2, EGFR, c-KIT and Her2/neu in anaplastic pancreatic cancer: Putative therapeutic targets? Histopathology. 2010;56:440–448. doi: 10.1111/j.1365-2559.2010.03499.x. [DOI] [PubMed] [Google Scholar]
- 123.Yin H., Porter N.A. New Insights Regarding the Autoxidation of Polyunsaturated Fatty Acids. Antioxid. Redox Signal. 2004;7:170–184. doi: 10.1089/ars.2005.7.170. [DOI] [PubMed] [Google Scholar]
- 124.Russell G.A. Deuterium-isotope Effects in the Autoxidation of Aralkyl Hydrocarbons. Mechanism of the Interaction of PEroxy Radicals1. J. Am. Chem. Soc. 1957;79:3871–3877. doi: 10.1021/ja01571a068. [DOI] [Google Scholar]
- 125.Pizzimenti S., Ciamporcero E., Daga M., Pettazzoni P., Arcaro A., Cetrangolo G., Minelli R., Dianzani C., Lepore A., Gentile F., et al. Interaction of aldehydes derived from lipid peroxidation and membrane proteins. Front. Physiol. 2013;4 doi: 10.3389/fphys.2013.00242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Lee M.J., Yaffe M.B. Protein Regulation in Signal Transduction. Cold Spring Harb. Perspect. Biol. 2016;8:a005918. doi: 10.1101/cshperspect.a005918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Rahimi N., Costello C.E. Emerging roles of post-translational modifications in signal transduction and angiogenesis. Proteomics. 2015;15:300–309. doi: 10.1002/pmic.201400183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Tomko N., Kluever M., Wu C., Zhu J., Wang Y., Salomon R.G. 4-Hydroxy-7-oxo-5-heptenoic acid lactone is a potent inducer of brain cancer cell invasiveness that may contribute to the failure of anti-angiogenic therapies. Free Radic. Biol. Med. 2020;146:234–256. doi: 10.1016/j.freeradbiomed.2019.11.009. [DOI] [PubMed] [Google Scholar]
- 129.Sousa B.C., Ahmed T., Dann W.L., Ashman J., Guy A., Durand T., Pitt A.R., Spickett C.M. Short-chain lipid peroxidation products form covalent adducts with pyruvate kinase and inhibit its activity in vitro and in breast cancer cells. Free Radic. Biol. Med. 2019;144:223–233. doi: 10.1016/j.freeradbiomed.2019.05.028. [DOI] [PubMed] [Google Scholar]
- 130.Sakuma S., Sumi H., Kohda T., Arakawa Y., Fujimoto Y. Effects of Lipid Peroxidation-Derived Products on the Growth of Human Colorectal Cancer Cell Line HT-29. J. Clin. Biochem. Nutr. 2009;45:171–177. doi: 10.3164/jcbn.09-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Gasparovic A.C., Milkovic L., Sunjic S.B., Zarkovic N. Cancer growth regulation by 4-hydroxynonenal. Free Radic. Biol. Med. 2017;111:226–234. doi: 10.1016/j.freeradbiomed.2017.01.030. [DOI] [PubMed] [Google Scholar]
- 132.Rossin D., Calfapietra S., Sottero B., Poli G., Biasi F. HNE and cholesterol oxidation products in colorectal inflammation and carcinogenesis. Free Radic. Biol. Med. 2017;111:186–195. doi: 10.1016/j.freeradbiomed.2017.01.017. [DOI] [PubMed] [Google Scholar]
- 133.Tappel A.L. Vitamin E as the Biological Lipid Antioxidant. In: Harris R.S., Wool I.G., Marrian G.F., Thimann K.V., editors. Vitamins & Hormones. Volume 20. Academic Press; New York, NY, USA: 1962. pp. 493–510. [Google Scholar]
- 134.Buettner G.R. The pecking order of free radicals and antioxidants: Lipid peroxidation, alpha-tocopherol, and ascorbate. Arch. Biochem. Biophys. 1993;300:535–543. doi: 10.1006/abbi.1993.1074. [DOI] [PubMed] [Google Scholar]
- 135.Samhan-Arias A.K., Duarte R.O., Martin-Romero F.J., Moura J.J., Gutierrez-Merino C. Reduction of ascorbate free radical by the plasma membrane of synaptic terminals from rat brain. Arch. Biochem. Biophys. 2008;469:243–254. doi: 10.1016/j.abb.2007.10.004. [DOI] [PubMed] [Google Scholar]
- 136.Scarpa M., Rigo A., Maiorino M., Ursini F., Gregolin C. Formation of alpha-tocopherol radical and recycling of alpha-tocopherol by ascorbate during peroxidation of phosphatidylcholine liposomes. An electron paramagnetic resonance study. Biochim. Biophys. Acta. 1984;801:215–219. doi: 10.1016/0304-4165(84)90070-9. [DOI] [PubMed] [Google Scholar]
- 137.Buettner G.R., Jurkiewicz B.A. Catalytic metals, ascorbate and free radicals: Combinations to avoid. Radiat. Res. 1996;145:532–541. doi: 10.2307/3579271. [DOI] [PubMed] [Google Scholar]
- 138.Mendiratta S., Qu Z.C., May J.M. Enzyme-dependent ascorbate recycling in human erythrocytes: Role of thioredoxin reductase. Free Radic. Biol. Med. 1998;25:221–228. doi: 10.1016/S0891-5849(98)00060-4. [DOI] [PubMed] [Google Scholar]
- 139.Schneider M., Wortmann M., Mandal P.K., Arpornchayanon W., Jannasch K., Alves F., Strieth S., Conrad M., Beck H. Absence of glutathione peroxidase 4 affects tumor angiogenesis through increased 12/15-lipoxygenase activity. Neoplasia. 2010;12:254–263. doi: 10.1593/neo.91782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Yang W.S., SriRamaratnam R., Welsch M.E., Shimada K., Skouta R., Viswanathan V.S., Cheah J.H., Clemons P.A., Shamji A.F., Clish C.B., et al. Regulation of ferroptotic cancer cell death by GPX4. Cell. 2014;156:317–331. doi: 10.1016/j.cell.2013.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Hangauer M.J., Viswanathan V.S., Ryan M.J., Bole D., Eaton J.K., Matov A., Galeas J., Dhruv H.D., Berens M.E., Schreiber S.L., et al. Drug-tolerant persister cancer cells are vulnerable to GPX4 inhibition. Nature. 2017;551:247–250. doi: 10.1038/nature24297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Bakhle Y.S. COX-2 and cancer: A new approach to an old problem. Br. J. Pharm. 2001;134:1137–1150. doi: 10.1038/sj.bjp.0704365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Ricciotti E., FitzGerald G.A. Prostaglandins and inflammation. Arter. Thromb. Vasc. Biol. 2011;31:986–1000. doi: 10.1161/ATVBAHA.110.207449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Murakami M., Naraba H., Tanioka T., Semmyo N., Nakatani Y., Kojima F., Ikeda T., Fueki M., Ueno A., Oh-ishi S., et al. Regulation of Prostaglandin E2 Biosynthesis by Inducible Membrane-associated Prostaglandin E2 Synthase That Acts in Concert with Cyclooxygenase-2. J. Biol. Chem. 2000;275:32783–32792. doi: 10.1074/jbc.M003505200. [DOI] [PubMed] [Google Scholar]
- 145.Jakobsson P.J., Thorén S., Morgenstern R., Samuelsson B. Identification of human prostaglandin E synthase: A microsomal, glutathione-dependent, inducible enzyme, constituting a potential novel drug target. Proc. Natl. Acad. Sci. USA. 1999;96:7220–7225. doi: 10.1073/pnas.96.13.7220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Jiang W.G., Douglas-Jones A., Mansel R.E. Levels of expression of lipoxygenases and cyclooxygenase-2 in human breast cancer. Prostaglandinsleukotrienes Essent. Fat. Acids. 2003;69:275–281. doi: 10.1016/S0952-3278(03)00110-8. [DOI] [PubMed] [Google Scholar]
- 147.Nassar A., Radhakrishnan A., Cabrero I.A., Cotsonis G., Cohen C. COX-2 expression in invasive breast cancer: Correlation with prognostic parameters and outcome. Appl. Immunohistochem. Mol. Morphol. 2007;15:255–259. doi: 10.1097/01.pai.0000213130.63417.b3. [DOI] [PubMed] [Google Scholar]
- 148.Li W., Wu S., Ahmad M., Jiang J., Liu H., Nagayama T., Rose M.E., Tyurin V.A., Tyurina Y.Y., Borisenko G.G., et al. The cyclooxygenase site, but not the peroxidase site of cyclooxygenase-2 is required for neurotoxicity in hypoxic and ischemic injury. J. Neurochem. 2010;113:965–977. doi: 10.1111/j.1471-4159.2010.06674.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Markovič T., Jakopin Ž., Dolenc M.S., Mlinarič-Raščan I. Structural features of subtype-selective EP receptor modulators. Drug Discov. Today. 2017;22:57–71. doi: 10.1016/j.drudis.2016.08.003. [DOI] [PubMed] [Google Scholar]
- 150.Sugimoto Y., Narumiya S. Prostaglandin E receptors. J. Biol. Chem. 2007;282:11613–11617. doi: 10.1074/jbc.R600038200. [DOI] [PubMed] [Google Scholar]
- 151.Reader J., Holt D., Fulton A. Prostaglandin E2 EP receptors as therapeutic targets in breast cancer. Cancer Metastasis Rev. 2011;30:449–463. doi: 10.1007/s10555-011-9303-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Lu D., Han C., Wu T. 15-PGDH inhibits hepatocellular carcinoma growth through 15-keto-PGE2/PPARγ-mediated activation of p21WAF1/Cip1. Oncogene. 2014;33:1101–1112. doi: 10.1038/onc.2013.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Tai H.H., Cho H., Tong M., Ding Y. NAD+-linked 15-hydroxyprostaglandin dehydrogenase: Structure and biological functions. Curr. Pharm. Des. 2006;12:955–962. doi: 10.2174/138161206776055958. [DOI] [PubMed] [Google Scholar]
- 154.Tachibana K., Yamasaki D., Ishimoto K., Doi T. The Role of PPARs in Cancer. Ppar. Res. 2008;2008:102737. doi: 10.1155/2008/102737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Savage D.B. PPARγ as a metabolic regulator: Insights from genomics and pharmacology. Expert Rev. Mol. Med. 2005;7:1–16. doi: 10.1017/S1462399405008793. [DOI] [PubMed] [Google Scholar]
- 156.Robbins G.T., Nie D. PPAR gamma, bioactive lipids, and cancer progression. Front. Biosci. 2012;17:1816–1834. doi: 10.2741/4021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Zhang Z., Xu H., Ji J., Shi X., Lyu J., Zhu Y., Yu H., Wang F. Heterogeneity of PTEN and PPAR-gamma in cancer and their prognostic application to bladder cancer. Exp. Med. 2019;18:3177–3183. doi: 10.3892/etm.2019.7879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Dana N., Vaseghi G., Haghjooy Javanmard S. PPAR gamma agonist, pioglitazone, suppresses melanoma cancer in mice by inhibiting TLR4 signaling. J. Pharm. Pharm. Sci. 2019;22:418–423. doi: 10.18433/jpps30626. [DOI] [PubMed] [Google Scholar]
- 159.Sawayama H., Ishimoto T., Watanabe M., Yoshida N., Sugihara H., Kurashige J., Hirashima K., Iwatsuki M., Baba Y., Oki E., et al. Small molecule agonists of PPAR-gamma exert therapeutic effects in esophageal cancer. Cancer Res. 2014;74:575–585. doi: 10.1158/0008-5472.CAN-13-1836. [DOI] [PubMed] [Google Scholar]
- 160.Forman B.M., Tontonoz P., Chen J., Brun R.P., Spiegelman B.M., Evans R.M. 15-Deoxy-Δ12,14-Prostaglandin J2 is a ligand for the adipocyte determination factor PPARγ. Cell. 1995;83:803–812. doi: 10.1016/0092-8674(95)90193-0. [DOI] [PubMed] [Google Scholar]
- 161.De Jong E., Winkel P., Poelstra K., Prakash J. Anticancer effects of 15d-prostaglandin-J2 in wild-type and doxorubicin-resistant ovarian cancer cells: Novel actions on SIRT1 and HDAC. PLoS ONE. 2011;6:e25192. doi: 10.1371/journal.pone.0025192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Pommery N., Taverne T., Telliez A., Goossens L., Charlier C., Pommery J., Goossens J.F., Houssin R., Durant F., Henichart J.P. New COX-2/5-LOX inhibitors: Apoptosis-inducing agents potentially useful in prostate cancer chemotherapy. J. Med. Chem. 2004;47:6195–6206. doi: 10.1021/jm0407761. [DOI] [PubMed] [Google Scholar]
- 163.Ye Y.N., Wu W.K., Shin V.Y., Bruce I.C., Wong B.C., Cho C.H. Dual inhibition of 5-LOX and COX-2 suppresses colon cancer formation promoted by cigarette smoke. Carcinogenesis. 2005;26:827–834. doi: 10.1093/carcin/bgi012. [DOI] [PubMed] [Google Scholar]
- 164.Goossens L., Pommery N., Henichart J.P. COX-2/5-LOX dual acting anti-inflammatory drugs in cancer chemotherapy. Curr. Top. Med. Chem. 2007;7:283–296. doi: 10.2174/156802607779941369. [DOI] [PubMed] [Google Scholar]
- 165.Che X.H., Chen C.L., Ye X.L., Weng G.B., Guo X.Z., Yu W.Y., Tao J., Chen Y.C., Chen X. Dual inhibition of COX-2/5-LOX blocks colon cancer proliferation, migration and invasion in vitro. Oncol. Rep. 2016;35:1680–1688. doi: 10.3892/or.2015.4506. [DOI] [PubMed] [Google Scholar]
- 166.Chang J., Tang N., Fang Q., Zhu K., Liu L., Xiong X., Zhu Z., Zhang B., Zhang M., Tao J. Inhibition of COX-2 and 5-LOX regulates the progression of colorectal cancer by promoting PTEN and suppressing PI3K/AKT pathway. Biochem. Biophys. Res. Commun. 2019;517:1–7. doi: 10.1016/j.bbrc.2018.01.061. [DOI] [PubMed] [Google Scholar]
- 167.Sarkar F.H., Adsule S., Li Y., Padhye S. Back to the future: COX-2 inhibitors for chemoprevention and cancer therapy. Mini Rev. Med. Chem. 2007;7:599–608. doi: 10.2174/138955707780859431. [DOI] [PubMed] [Google Scholar]
- 168.Sun L., Zhao Y., Wang L., Song M., Song J. [Suppression of COX-2 protein to cell apoptosis in non-small cell lung cancer] Zhongguo Fei Ai Za Zhi. 2007;10:188–191. doi: 10.3779/j.issn.1009-3419.2007.03.06. [DOI] [PubMed] [Google Scholar]
- 169.Bocca C., Bozzo F., Bassignana A., Miglietta A. Antiproliferative effects of COX-2 inhibitor celecoxib on human breast cancer cell lines. Mol. Cell. Biochem. 2011;350:59–70. doi: 10.1007/s11010-010-0682-4. [DOI] [PubMed] [Google Scholar]
- 170.Lepage C., Léger D.Y., Bertrand J., Martin F., Beneytout J.L., Liagre B. Diosgenin induces death receptor-5 through activation of p38 pathway and promotes TRAIL-induced apoptosis in colon cancer cells. Cancer Lett. 2011;301:193–202. doi: 10.1016/j.canlet.2010.12.003. [DOI] [PubMed] [Google Scholar]
- 171.Holmes M.D., Chen W.Y., Schnitt S.J., Collins L., Colditz G.A., Hankinson S.E., Tamimi R.M. COX-2 expression predicts worse breast cancer prognosis and does not modify the association with aspirin. Breast Cancer Res. Treat. 2011;130:657–662. doi: 10.1007/s10549-011-1651-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Frisk G., Ekberg S., Lidbrink E., Eloranta S., Sund M., Fredriksson I., Lambe M., Smedby K.E. No association between low-dose aspirin use and breast cancer outcomes overall: A Swedish population-based study. Breast Cancer Res. 2018;20:142. doi: 10.1186/s13058-018-1065-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Wu J., Xia H.H., Tu S.P., Fan D.M., Lin M.C., Kung H.F., Lam S.K., Wong B.C. 15-Lipoxygenase-1 mediates cyclooxygenase-2 inhibitor-induced apoptosis in gastric cancer. Carcinogenesis. 2003;24:243–247. doi: 10.1093/carcin/24.2.243. [DOI] [PubMed] [Google Scholar]
- 174.Haeggström J.Z., Funk C.D. Lipoxygenase and Leukotriene Pathways: Biochemistry, Biology, and Roles in Disease. Chem. Rev. 2011;111:5866–5898. doi: 10.1021/cr200246d. [DOI] [PubMed] [Google Scholar]
- 175.Krieg P., Fürstenberger G. The role of lipoxygenases in epidermis. Biochim. Biophys. Acta (BBA)-Mol. Cell Biol. Lipids. 2014;1841:390–400. doi: 10.1016/j.bbalip.2013.08.005. [DOI] [PubMed] [Google Scholar]
- 176.Fagerberg L., Hallström B.M., Oksvold P., Kampf C., Djureinovic D., Odeberg J., Habuka M., Tahmasebpoor S., Danielsson A., Edlund K., et al. Analysis of the human tissue-specific expression by genome-wide integration of transcriptomics and antibody-based proteomics. Mol. Cell. Proteom. MCP. 2014;13:397–406. doi: 10.1074/mcp.M113.035600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Nie D., Krishnamoorthy S., Jin R., Tang K., Chen Y., Qiao Y., Zacharek A., Guo Y., Milanini J., Pages G., et al. Mechanisms regulating tumor angiogenesis by 12-lipoxygenase in prostate cancer cells. J. Biol. Chem. 2006;281:18601–18609. doi: 10.1074/jbc.M601887200. [DOI] [PubMed] [Google Scholar]
- 178.Pidgeon G.P., Kandouz M., Meram A., Honn K.V. Mechanisms Controlling Cell Cycle Arrest and Induction of Apoptosis after 12-Lipoxygenase Inhibition in Prostate Cancer Cells. Cancer Res. 2002;62:2721–2727. [PubMed] [Google Scholar]
- 179.Pidgeon G.P., Tang K., Cai Y.L., Piasentin E., Honn K.V. Overexpression of Platelet-type 12-Lipoxygenase Promotes Tumor Cell Survival by Enhancing αvβ3 and αvβ5 Integrin Expression. Cancer Res. 2003;63:4258–4267. [PubMed] [Google Scholar]
- 180.Nie D., Hillman G.G., Geddes T., Tang K., Pierson C., Grignon D.J., Honn K.V. Platelet-Type 12-Lipoxygenase in a Human Prostate Carcinoma Stimulates Angiogenesis and Tumor Growth. Cancer Res. 1998;58:4047–4051. [PubMed] [Google Scholar]
- 181.Ghosh J., Myers C.E. Arachidonic Acid Stimulates Prostate Cancer Cell Growth: Critical Role of 5-Lipoxygenase. Biochem. Biophys. Res. Commun. 1997;235:418–423. doi: 10.1006/bbrc.1997.6799. [DOI] [PubMed] [Google Scholar]
- 182.Na Y.J., Kim B.R., Kim J.L., Kang S., Jeong Y.A., Park S.H., Jo M.J., Kim J.Y., Kim H.J., Oh S.C., et al. Deficiency of 15-LOX-1 Induces Radioresistance through Downregulation of MacroH2A2 in Colorectal Cancer. Cancers (Basel) 2019;11:1776. doi: 10.3390/cancers11111776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Shureiqi I., Zuo X., Broaddus R., Wu Y., Guan B., Morris J.S., Lippman S.M. The transcription factor GATA-6 is overexpressed in vivo and contributes to silencing 15-LOX-1 in vitro in human colon cancer. Faseb J. 2007;21:743–753. doi: 10.1096/fj.06-6830com. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Wu Y., Mao F., Zuo X., Moussalli M.J., Elias E., Xu W., Shureiqi I. 15-LOX-1 suppression of hypoxia-induced metastatic phenotype and HIF-1alpha expression in human colon cancer cells. Cancer Med. 2014;3:472–484. doi: 10.1002/cam4.222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Zuo X., Morris J.S., Broaddus R., Shureiqi I. 15-LOX-1 transcription suppression through the NuRD complex in colon cancer cells. Oncogene. 2009;28:1496–1505. doi: 10.1038/onc.2008.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Wolff C., Zoschke C., Kalangi S.K., Reddanna P., Schäfer-Korting M. Tumor microenvironment determines drug efficacy in vitro-apoptotic and anti-inflammatory effects of 15-lipoxygenase metabolite, 13-HpOTrE. Eur. J. Pharm. Biopharm. 2019;142:1–7. doi: 10.1016/j.ejpb.2019.06.003. [DOI] [PubMed] [Google Scholar]
- 187.Kagan V.E., Mao G., Qu F., Angeli J.P.F., Doll S., Croix C.S., Dar H.H., Liu B., Tyurin V.A., Ritov V.B., et al. Oxidized arachidonic and adrenic PEs navigate cells to ferroptosis. Nat. Chem. Biol. 2017;13:81–90. doi: 10.1038/nchembio.2238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Wenzel S.E., Tyurina Y.Y., Zhao J., St. Croix C.M., Dar H.H., Mao G., Tyurin V.A., Anthonymuthu T.S., Kapralov A.A., Amoscato A.A., et al. PEBP1 Wardens Ferroptosis by Enabling Lipoxygenase Generation of Lipid Death Signals. Cell. 2017;171:628–641.e626. doi: 10.1016/j.cell.2017.09.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Lu X., Huang L., Zhang W., Ning X. Tepoxalin a dual 5-LOX-COX inhibitor and erlotinib an EGFR inhibitor halts progression of gastric cancer in tumor xenograft mice. Am. J. Transl. Res. 2018;10:3847–3856. [PMC free article] [PubMed] [Google Scholar]
- 190.Tavolari S., Bonafe M., Marini M., Ferreri C., Bartolini G., Brighenti E., Manara S., Tomasi V., Laufer S., Guarnieri T. Licofelone, a dual COX/5-LOX inhibitor, induces apoptosis in HCA-7 colon cancer cells through the mitochondrial pathway independently from its ability to affect the arachidonic acid cascade. Carcinogenesis. 2008;29:371–380. doi: 10.1093/carcin/bgm265. [DOI] [PubMed] [Google Scholar]
- 191.Yang P., Cartwright C., Chan D., Vijjeswarapu M., Ding J., Newman R.A. Zyflamend®-mediated inhibition of human prostate cancer PC3 cell proliferation: Effects on 12-LOX and Rb protein phosphorylation. Cancer Biol. Ther. 2007;6:228–236. doi: 10.4161/cbt.6.2.3624. [DOI] [PubMed] [Google Scholar]
- 192.Singh A.K., Singh R., Naz F., Chauhan S.S., Dinda A., Shukla A.A., Gill K., Kapoor V., Dey S. Structure based design and synthesis of peptide inhibitor of human LOX-12: In vitro and in vivo analysis of a novel therapeutic agent for breast cancer. PLoS ONE. 2012;7:e32521. doi: 10.1371/journal.pone.0032521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Wong B.C.Y., Wang W.P., Cho C.H., Fan X.M., Lin M.C.M., Kung H.F., Lam S.K. 12-Lipoxygenase inhibition induced apoptosis in human gastric cancer cells. Carcinogenesis. 2001;22:1349–1354. doi: 10.1093/carcin/22.9.1349. [DOI] [PubMed] [Google Scholar]
- 194.Lovey J., Nie D., Tovari J., Kenessey I., Kandouz M., Timar J., Kasler M., Honn K.V. [Selective 12-lipoxygenase inhibition potentiates the effect of radiation on human prostate cancer cells in vitro and in vivo] Magy. Onkol. 2014;58:211–218. [PubMed] [Google Scholar]
- 195.Lovey J., Nie D., Tovari J., Kenessey I., Timar J., Kandouz M., Honn K.V. Radiosensitivity of human prostate cancer cells can be modulated by inhibition of 12-lipoxygenase. Cancer Lett. 2013;335:495–501. doi: 10.1016/j.canlet.2013.03.012. [DOI] [PubMed] [Google Scholar]
- 196.Skouta R., Dixon S.J., Wang J., Dunn D.E., Orman M., Shimada K., Rosenberg P.A., Lo D.C., Weinberg J.M., Linkermann A., et al. Ferrostatins inhibit oxidative lipid damage and cell death in diverse disease models. J. Am. Chem. Soc. 2014;136:4551–4556. doi: 10.1021/ja411006a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Lei P., Bai T., Sun Y. Mechanisms of Ferroptosis and Relations With Regulated Cell Death: A Review. Front. Physiol. 2019;10:139. doi: 10.3389/fphys.2019.00139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Li J., Cao F., Yin H.-l., Huang Z.-j., Lin Z.-t., Mao N., Sun B., Wang G. Ferroptosis: Past, present and future. Cell Death Dis. 2020;11:88. doi: 10.1038/s41419-020-2298-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Dixon S.J., Lemberg K.M., Lamprecht M.R., Skouta R., Zaitsev E.M., Gleason C.E., Patel D.N., Bauer A.J., Cantley A.M., Yang W.S., et al. Ferroptosis: An iron-dependent form of nonapoptotic cell death. Cell. 2012;149:1060–1072. doi: 10.1016/j.cell.2012.03.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Stockwell B.R., Friedmann Angeli J.P., Bayir H., Bush A.I., Conrad M., Dixon S.J., Fulda S., Gascón S., Hatzios S.K., Kagan V.E., et al. Ferroptosis: A Regulated Cell Death Nexus Linking Metabolism, Redox Biology, and Disease. Cell. 2017;171:273–285. doi: 10.1016/j.cell.2017.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Hayano M., Yang W.S., Corn C.K., Pagano N.C., Stockwell B.R. Loss of cysteinyl-tRNA synthetase (CARS) induces the transsulfuration pathway and inhibits ferroptosis induced by cystine deprivation. Cell Death Differ. 2016;23:270–278. doi: 10.1038/cdd.2015.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Gao M., Monian P., Quadri N., Ramasamy R., Jiang X. Glutaminolysis and Transferrin Regulate Ferroptosis. Mol. Cell. 2015;59:298–308. doi: 10.1016/j.molcel.2015.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Shimada K., Skouta R., Kaplan A., Yang W.S., Hayano M., Dixon S.J., Brown L.M., Valenzuela C.A., Wolpaw A.J., Stockwell B.R. Global survey of cell death mechanisms reveals metabolic regulation of ferroptosis. Nat. Chem. Biol. 2016;12:497–503. doi: 10.1038/nchembio.2079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Kagan V., Serbinova E., Packer L. Antioxidant effects of ubiquinones in microsomes and mitochondria are mediated by tocopherol recycling. Biochem. Biophys. Res. Commun. 1990;169:851–857. doi: 10.1016/0006-291X(90)91971-T. [DOI] [PubMed] [Google Scholar]
- 205.Forsmark P., Åberg F., Norling B., Nordenbrand K., Dallner G., Ernster L. Inhibition of lipid peroxidation by ubiquinol in submitochondrial particles in the absence of vitamin E. Febs Lett. 1991;285:39–43. doi: 10.1016/0014-5793(91)80720-N. [DOI] [PubMed] [Google Scholar]
- 206.Frei B., Kim M.C., Ames B.N. Ubiquinol-10 is an effective lipid-soluble antioxidant at physiological concentrations. Proc. Natl. Acad. Sci. USA. 1990;87:4879–4883. doi: 10.1073/pnas.87.12.4879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Kagan V.E., Tiurin V.A., Kitanova S.A., Serbinova E.A., Quinn P.J. [The action of a homologous series of ubiquinols on lipid peroxidation in brain mitochondrial and synaptosomal membranes] Biull. Eksp. Biol. Med. 1989;107:420–422. doi: 10.1007/BF00842378. [DOI] [PubMed] [Google Scholar]
- 208.Seiler A., Schneider M., Förster H., Roth S., Wirth E.K., Culmsee C., Plesnila N., Kremmer E., Rådmark O., Wurst W., et al. Glutathione Peroxidase 4 Senses and Translates Oxidative Stress into 12/15-Lipoxygenase Dependent- and AIF-Mediated Cell Death. Cell Metab. 2008;8:237–248. doi: 10.1016/j.cmet.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 209.Yang W.S., Kim K.J., Gaschler M.M., Patel M., Shchepinov M.S., Stockwell B.R. Peroxidation of polyunsaturated fatty acids by lipoxygenases drives ferroptosis. Proc. Natl. Acad. Sci. USA. 2016;113:E4966–E4975. doi: 10.1073/pnas.1603244113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Yagoda N., von Rechenberg M., Zaganjor E., Bauer A.J., Yang W.S., Fridman D.J., Wolpaw A.J., Smukste I., Peltier J.M., Boniface J.J., et al. RAS–RAF–MEK-dependent oxidative cell death involving voltage-dependent anion channels. Nature. 2007;447:865–869. doi: 10.1038/nature05859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Yang W.S., Stockwell B.R. Synthetic lethal screening identifies compounds activating iron-dependent, nonapoptotic cell death in oncogenic-RAS-harboring cancer cells. Chem. Biol. 2008;15:234–245. doi: 10.1016/j.chembiol.2008.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Shah R., Shchepinov M.S., Pratt D.A. Resolving the Role of Lipoxygenases in the Initiation and Execution of Ferroptosis. Acs Cent. Sci. 2018;4:387–396. doi: 10.1021/acscentsci.7b00589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Stadtman E.R. Oxidation of free amino acids and amino acid residues in proteins by radiolysis and by metal-catalyzed reactions. Annu. Rev. Biochem. 1993;62:797–821. doi: 10.1146/annurev.bi.62.070193.004053. [DOI] [PubMed] [Google Scholar]
- 214.Viswanathan V.S., Ryan M.J., Dhruv H.D., Gill S., Eichhoff O.M., Seashore-Ludlow B., Kaffenberger S.D., Eaton J.K., Shimada K., Aguirre A.J., et al. Dependency of a therapy-resistant state of cancer cells on a lipid peroxidase pathway. Nature. 2017;547:453–457. doi: 10.1038/nature23007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Dixon S.J., Patel D.N., Welsch M., Skouta R., Lee E.D., Hayano M., Thomas A.G., Gleason C.E., Tatonetti N.P., Slusher B.S., et al. Pharmacological inhibition of cystine–glutamate exchange induces endoplasmic reticulum stress and ferroptosis. eLife. 2014;3:e02523. doi: 10.7554/eLife.02523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Friedmann Angeli J.P., Schneider M., Proneth B., Tyurina Y.Y., Tyurin V.A., Hammond V.J., Herbach N., Aichler M., Walch A., Eggenhofer E., et al. Inactivation of the ferroptosis regulator Gpx4 triggers acute renal failure in mice. Nat. Cell. Biol. 2014;16:1180–1191. doi: 10.1038/ncb3064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Doll S., Freitas F.P., Shah R., Aldrovandi M., da Silva M.C., Ingold I., Grocin A.G., Xavier da Silva T.N., Panzilius E., Scheel C.H., et al. FSP1 is a glutathione-independent ferroptosis suppressor. Nature. 2019;575:693–698. doi: 10.1038/s41586-019-1707-0. [DOI] [PubMed] [Google Scholar]
- 218.Xia L., Nordman T., Olsson J.M., Damdimopoulos A., Björkhem-Bergman L., Nalvarte I., Eriksson L.C., Arnér E.S.J., Spyrou G., Björnstedt M. The Mammalian Cytosolic Selenoenzyme Thioredoxin Reductase Reduces Ubiquinone: A novel mechanism for defense against oxidative stress. J. Biol. Chem. 2003;278:2141–2146. doi: 10.1074/jbc.M210456200. [DOI] [PubMed] [Google Scholar]
- 219.Yan C., Shieh B., Reigan P., Zhang Z., Colucci M.A., Chilloux A., Newsome J.J., Siegel D., Chan D., Moody C.J., et al. Potent activity of indolequinones against human pancreatic cancer: Identification of thioredoxin reductase as a potential target. Mol. Pharmacol. 2009;76:163–172. doi: 10.1124/mol.109.055855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Parkinson E.I., Hergenrother P.J. Deoxynyboquinones as NQO1-Activated Cancer Therapeutics. Acc. Chem. Res. 2015;48:2715–2723. doi: 10.1021/acs.accounts.5b00365. [DOI] [PubMed] [Google Scholar]
- 221.Navarro F., Villalba J.M., Crane F.L., Mackellar W.C., Navas P. A phospholipid-dependent NADH-coenzyme Q reductase from liver plasma membrane. Biochem. Biophys. Res. Commun. 1995;212:138–143. doi: 10.1006/bbrc.1995.1947. [DOI] [PubMed] [Google Scholar]
- 222.Nakashima Y., Shinzawa-Itoh K., Watanabe K., Naoki K., Hano N., Yoshikawa S. Steady-state kinetics of NADH:coenzyme Q oxidoreductase isolated from bovine heart mitochondria. J. Bioenerg. Biomembr. 2002;34:11–19. doi: 10.1023/A:1013862502185. [DOI] [PubMed] [Google Scholar]
- 223.Reda A., Refaat A., Abd-Rabou A.A., Mahmoud A.M., Adel M., Sabet S., Ali S.S. Role of mitochondria in rescuing glycolytically inhibited subpopulation of triple negative but not hormone-responsive breast cancer cells. Sci. Rep. 2019;9:13748. doi: 10.1038/s41598-019-50141-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Grivennikova V.G., Gavrikova E.V., Timoshin A.A., Vinogradov A.D. Fumarate reductase activity of bovine heart succinate-ubiquinone reductase. New assay system and overall properties of the reaction. Biochim. Biophys. Acta (BBA)-Bioenerg. 1993;1140:282–292. doi: 10.1016/0005-2728(93)90067-P. [DOI] [PubMed] [Google Scholar]
- 225.Ralph S.J., Moreno-Sánchez R., Neuzil J., Rodríguez-Enríquez S. Inhibitors of Succinate: Quinone Reductase/Complex II Regulate Production of Mitochondrial Reactive Oxygen Species and Protect Normal Cells from Ischemic Damage but Induce Specific Cancer Cell Death. Pharm. Res. 2011;28:2695. doi: 10.1007/s11095-011-0566-7. [DOI] [PubMed] [Google Scholar]
- 226.Wang A., Lim H., Cheng S.-Y., Xie L. ANTENNA, a Multi-Rank, Multi-Layered Recommender System for Inferring Reliable Drug-Gene-Disease Associations: Repurposing Diazoxide as a Targeted Anti-Cancer Therapy. bioRxiv. 2017:192385. doi: 10.1109/TCBB.2018.2812189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Olsson J.M., Xia L., Eriksson L.C., Björnstedt M. Ubiquinone is reduced by lipoamide dehydrogenase and this reaction is potently stimulated by zinc. Febs Lett. 1999;448:190–192. doi: 10.1016/S0014-5793(99)00363-4. [DOI] [PubMed] [Google Scholar]
- 228.Kwak C.H., Lee J.H., Kim E.Y., Han C.W., Kim K.J., Lee H., Cho M., Jang S.B., Kim C.H., Chung T.W., et al. Huzhangoside A Suppresses Tumor Growth through Inhibition of Pyruvate Dehydrogenase Kinase Activity. Cancers (Basel) 2019;11:712. doi: 10.3390/cancers11050712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Ullrich A., Knecht W., Fries M., Loffler M. Recombinant expression of N-terminal truncated mutants of the membrane bound mouse, rat and human flavoenzyme dihydroorotate dehydrogenase. A versatile tool to rate inhibitor effects? Eur. J. Biochem. 2001;268:1861–1868. doi: 10.1046/j.1432-1327.2001.02061.x. [DOI] [PubMed] [Google Scholar]
- 230.Madak J.T., Bankhead A., Cuthbertson C.R., Showalter H.D., Neamati N. Revisiting the role of dihydroorotate dehydrogenase as a therapeutic target for cancer. Pharmacol. Ther. 2019;195:111–131. doi: 10.1016/j.pharmthera.2018.10.012. [DOI] [PubMed] [Google Scholar]
- 231.Lucas-Hourani M., Munier-Lehmann H., El Mazouni F., Malmquist N.A., Harpon J., Coutant E.P., Guillou S., Helynck O., Noel A., Scherf A., et al. Original 2-(3-Alkoxy-1H-pyrazol-1-yl)azines Inhibitors of Human Dihydroorotate Dehydrogenase (DHODH) J. Med. Chem. 2015;58:5579–5598. doi: 10.1021/acs.jmedchem.5b00606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Bahrami B., Mohammadnia-Afrouzi M., Bakhshaei P., Yazdani Y., Ghalamfarsa G., Yousefi M., Sadreddini S., Jadidi-Niaragh F., Hojjat-Farsangi M. Folate-conjugated nanoparticles as a potent therapeutic approach in targeted cancer therapy. Tumor Biol. 2015;36:5727–5742. doi: 10.1007/s13277-015-3706-6. [DOI] [PubMed] [Google Scholar]
- 233.Bretin L., Pinon A., Bouramtane S., Ouk C., Richard L., Perrin M.L., Chaunavel A., Carrion C., Bregier F., Sol V., et al. Photodynamic Therapy Activity of New Porphyrin-Xylan-Coated Silica Nanoparticles in Human Colorectal Cancer. Cancers (Basel) 2019;11:1474. doi: 10.3390/cancers11101474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Jasim K.A., Gesquiere A.J. Ultrastable and Biofunctionalizable Conjugated Polymer Nanoparticles with Encapsulated Iron for Ferroptosis Assisted Chemodynamic Therapy. Mol. Pharm. 2019;16:4852–4866. doi: 10.1021/acs.molpharmaceut.9b00737. [DOI] [PubMed] [Google Scholar]
- 235.Thomas R.G., Moon M.J., Lee H., Sasikala A.R., Kim C.S., Park I.K., Jeong Y.Y. Hyaluronic acid conjugated superparamagnetic iron oxide nanoparticle for cancer diagnosis and hyperthermia therapy. Carbohydr. Polym. 2015;131:439–446. doi: 10.1016/j.carbpol.2015.06.010. [DOI] [PubMed] [Google Scholar]
- 236.Emami M., Shamsipur M., Saber R., Irajirad R. An electrochemical immunosensor for detection of a breast cancer biomarker based on antiHER2-iron oxide nanoparticle bioconjugates. Analyst. 2014;139:2858–2866. doi: 10.1039/C4AN00183D. [DOI] [PubMed] [Google Scholar]
- 237.Kim S.E., Zhang L., Ma K., Riegman M., Chen F., Ingold I., Conrad M., Turker M.Z., Gao M., Jiang X., et al. Ultrasmall nanoparticles induce ferroptosis in nutrient-deprived cancer cells and suppress tumour growth. Nat. Nanotechnol. 2016;11:977–985. doi: 10.1038/nnano.2016.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Alarifi S., Ali D., Alkahtani S., Alhader M.S. Iron Oxide Nanoparticles Induce Oxidative Stress, DNA Damage, and Caspase Activation in the Human Breast Cancer Cell Line. Biol. Trace Elem. Res. 2014;159:416–424. doi: 10.1007/s12011-014-9972-0. [DOI] [PubMed] [Google Scholar]
- 239.Jaganjac M., Borovic Sunjic S., Zarkovic N. Utilizing Iron for Targeted Lipid Peroxidation as Anticancer Option of Integrative Biomedicine: A Short Review of Nanosystems Containing Iron. Antioxidants. 2020;9:191. doi: 10.3390/antiox9030191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Sang M., Luo R., Bai Y., Dou J., Zhang Z., Liu F., Feng F., Xu J., Liu W. Mitochondrial membrane anchored photosensitive nano-device for lipid hydroperoxides burst and inducing ferroptosis to surmount therapy-resistant cancer. Theranostics. 2019;9:6209–6223. doi: 10.7150/thno.36283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Abrams R.P., Carroll W.L., Woerpel K.A. Five-Membered Ring Peroxide Selectively Initiates Ferroptosis in Cancer Cells. Acs Chem. Biol. 2016;11:1305–1312. doi: 10.1021/acschembio.5b00900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Shen Z., Song J., Yung B.C., Zhou Z., Wu A., Chen X. Emerging Strategies of Cancer Therapy Based on Ferroptosis. Adv. Mater. 2018;30:1704007. doi: 10.1002/adma.201704007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Said-Elbahr R., Nasr M., Alhnan M.A., Taha I., Sammour O. Nebulizable colloidal nanoparticles co-encapsulating a COX-2 inhibitor and a herbal compound for treatment of lung cancer. Eur. J. Pharm. Biopharm. 2016;103:1–12. doi: 10.1016/j.ejpb.2016.03.025. [DOI] [PubMed] [Google Scholar]
- 244.Kim T.-H., Jeong Y.-I., Jin S.-G., Pei J., Jung T.-Y., Moon K.-S., Kim I.-Y., Kang S.-S., Jung S. Preparation of polylactide-co-glycolide nanoparticles incorporating celecoxib and their antitumor activity against brain tumor cells. Int. J. Nanomed. 2011;6:2621–2631. doi: 10.2147/IJN.S19497. [DOI] [PMC free article] [PubMed] [Google Scholar]