Abstract
T-cell acute lymphoblastic leukemia (T-ALL) is one of the hematological malignancies. With the applications of chemotherapy regimens and allogeneic hematopoietic stem cell transplantation, the cure rate of T-ALL has been significantly improved. However, patients with relapsed and refractory T-ALL still lack effective treatment options. Gene mutations play an important role in T-ALL. The NOTCH1 gene mutation is the important one among these genetic mutations. Since the mutation of NOTCH1 gene is considered as a driving oncogene in T-ALL, targeting the NOTCH1 signaling patheway may be an effective option to overcome relapsed and refractory T-ALL. This review mainly summarizes the recent research advances of targeting on NOTCH1 signaling pathway in T-ALL.
Keywords: T-cell acute lymphoblastic leukemia, NOTCH1, γ-Secretase inhibitors, SERCA inhibitors, Monoclonal antibody
Background
T-cell acute lymphoblastic leukemia (T-ALL) is a hematological malignancy originating from T-lymphocytes in bone marrow. In recent years, with the advances of chemotherapy and the application of allogeneic hematopoietic stem cell transplantation in the management of T-ALL, the outcomes of this disease have been significantly improved. At the same time, the use of chimeric antigen receptor modified T cell (CAR-T) therapy also provides new and effective immunotherapy for T-ALL [1]. However, some T-ALL patients are refractory to induction therapy, and others responding to induction therapy may relapse and become refractory to salvage therapy. There are no effective treatment options for those patients with poor prognosis. Thus the underlying molecular mechanisms and therapy for refractory and relapsed T-ALL are the main focuses of current researches. With the advance of state-of-art molecular technology such as next generation DNA sequencing, studies have found that germline or somatic mutations of some genes may play important roles in the occurrence, development, and drug-resistance of T-ALL [2]. The mutation in NOTCH1 gene is one of the important genetic mutations in T-ALL [3, 4]. Studies have shown that NOTCH1 mutations play a role in carcinogenesis or tumor suppression under different cell backgrounds [5, 6]. In T-ALL, NOTCH1 is a driving oncogene, and the dominant active mutations induce the development of pre-T cells to leukemia [7–9]. Therefore, further understandings of the NOTCH1 mutation in T-ALL will shed light on developing targeting therapy for T-ALL patients. Targeting the NOTCH1 signaling pathway may be an optimal management for the treatment of relapsed and refractory T-ALL carrying NOTCH1 mutation.
NOTCH1 gene and the signaling pathways
NOTCH1 gene is a member of a highly conserved NOTCH gene family (NOTCH1-4), located on chromosome 9q34.3, and encodes a NOTCH1 transmembrane signal protein. The NOTCH1 receptor protein is composed of three regions/subunits: (1) The extracellular region consisting of the epidermal growth factor (EGF)-like repeats, the negative regulatory region (NRR) composed of 3 cysteine-rich Lin12-Notch repeats (LNR) and a heterodimerization domain (HD); (2) The transmembrane region that includes the site of action for ADAM protease and γ-secretase; (3) The intracellular region consisting of a proline/glutamic acid/serine/threonine enriched motif (PEST) domain, which is primarily responsible for producing NOTCH1 active component ICN1 [10–12].
The mature NOTCH1 receptor protein containing the heterodimerization domain is transported to the cell surface. The EGF-like repeats in the extracellular region combine with NOTCH ligands (Jag1, Jag2, Dll1, Dll3, etc.) in neighboring cells, leading to the exposure of S2 site and S3 site in NRR region near the cell membrane. As a result, this conformation change triggers the proteolytic function of the ADAM protease in S2 site and the γ-secretase in S3 site, leading to the release of the intracellular region ICN1. ICN1 enters the nucleus and interacts with the DNA-binding protein continuous spontaneous localization (CSL) and the Mastermind-like (MAML) family proteins, resulting in the formation of a transient ICN1-CSL-MAML complex and activation of downstream gene transcription. Finally, the PEST region binds to the FBXW7 that includes E3 ubiquitin ligase. The NOTCH-FBXW7 complex recognizes and degrades ICN1 to terminate the signaling pathway [12–14].
Agents target on NOTCH1 pathway
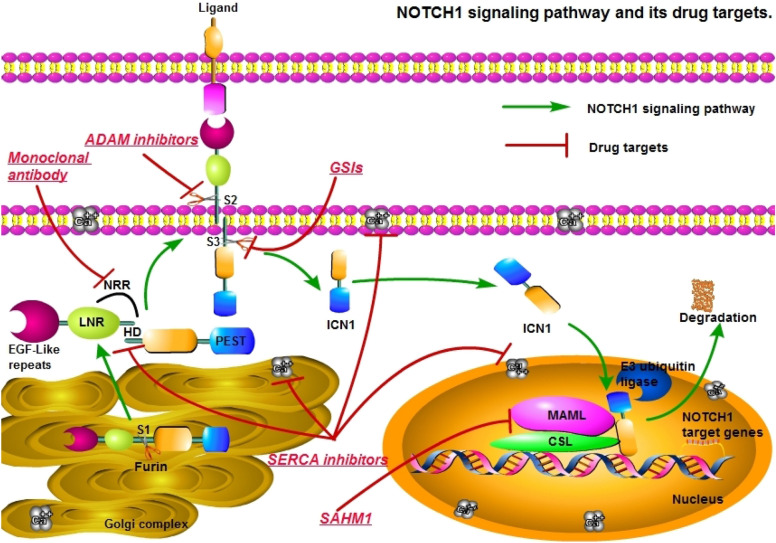
There have been many small molecules tested in the targeted therapy on NOTCH1 pathway in T-ALL [15, 16], which can be divided into the following categories (Fig. 1).
Fig. 1.
NOTCH1 signaling pathway and drug targets. Agent categories and their targets: ADAM inhibitors prevent ADAM protease S2 site digestion; γ-secretase inhibitors (GSIs) prevent the cleavage of S3 site of γ-secretase; Monoclonal antibody prevent the conformational change of the negative regulatory region (NRR) from exposing the S2 and S3 cleavage sites; SERCA inhibitors include Ca2+ ATPase inhibitors prevent transportation process of NOTCH1 and the formation of heterodimerization domain (HD); SAHM1 prevent the formation of ICN1-CSL-MAML complex
γ-Secretase inhibitors (GSIs)
γ-Secretase is a key enzyme in the activation process of NOTCH pathway. Inhibiting its activity can induce G0/G1 cell cycle arrest and inhibit cell proliferation.
The original GSI trial drug was MK-0752. Seven patients with T-ALL received MK-0752 for 56 days. One of the patients showed a certain anti-leukemia effect to the drug, but the response was transient. Most patients developed gastrointestinal toxicity (mainly diarrhea) at a dose of 300 mg/m2, which lead to the termination of the trial [17]. The GSI may block NOTCH1 and NOTCH2 at the same time and disturbs the normal function of physiological NOTCH signals. As a result, serious imbalance of digestive tract homeostasis is considered as the main reason of diarrhea [2, 18].
PF-03084014 is an oral, non-competitive, reversible, selective γ-secretase inhibitor. In a HPB-ALL (a subset of human T-ALL) cell line, cells in S-G2-M phase were suppressed after 7 days of PF-03084014 treatment, while cells in G0-G1 phase were accumulated. The ICN1 protein was completely inhibited, and the expression of Notch target genes Hes-1 and cMyc were down-regulated in these cells [19]. PF-03084014 was well tolerated in mice at dose levels below 100 mg/kg. HPB-ALL xenotransplanted mice were tested at 150 mg/kg with different intermittent treatment schedules: continuous treatment, 3 days treatment/4 days withdrawal, 7 days treatment/7 days withdrawal. The PF-03084014 at 7-day treatment/7-day withdrawal schedule exerted the best anti-cancer efficacy and the least toxicity in HPB-ALL xenotransplanted mice [19]. In a phase I study, eight patients with T-ALL or T-cell lymphoblastic lymphoma (5 T-cell lymphoblastic lymphoma and 3 T-ALL) received PF-03084014 at 150 mg twice daily [20]. All eight patients had previously received systemic treatment and relapsed. One of the T-ALL patients achieved complete remission lasting about 3 months, and then relapsed. The HES4 gene expression level was suppressed during remission and was higher than the baseline level when the disease relapsed in this case. The most common adverse effects were nausea and vomiting [20].
BMS-906024, another small molecule γ-secretase inhibitor was screened by efficacy/tolerance profile. The efficacy of BMS-906024 was dose-dependent, and the lowest effective dose was 1 mg/kg/day in xenotransplantation mice [21]. At higher doses, a significant delay in tumor growth can be observed even after the administration was complete. And no significant toxicity such as weight loss of mice was observed [21]. A clinical trial of the agent allowed a 53-year-old male patient with relapsed and refractory early T-cell progenitor acute lymphoblastic leukemia to reach complete remission with a deep molecular response [22]. In a Phase I clinical trial, BMS-906024 was administered in 25 children with T-ALL or T-cell lymphoblastic lymphoma at 4–6 mg weekly. One-third of cases (32%) showed at least a 50% reduction in bone marrow blasts and had tolerable side effects [23].
MRK-560, a precise selective γ-secretase inhibitor, mainly targets PSEN1 in the γ-secretase complex in T-ALL cell lines [24]. MRK-560 was used to treat T-ALL patient-derived xenograft mouse models with different NOTCH1 mutations. The anti-tumor activity and improved survival were observed in all mice with various response. And the mice administered with MRK-560 did not show obvious gastrointestinal pathological changes and thymus T cell development defects [24].
There are currently a variety of GSIs in the experimental stage [5]. But overall, GSI has a limited anti-tumor effect, mostly manifested as transient growth arrest rather than cell death, and a single agent seems to be insufficient to eradicate T-ALL blasts [25]. Combining GSI with other agents that can trigger cell death may be an alternative option to treatment of NOTCH1-mutant T-ALL [26, 27]. Chloroquine (CQ) can increase the accumulation of reactive oxygen species in T-ALL, activate DNA damage, enhance GSI-induced cell cycle arrest in T-ALL, and interfere with ligand-independent NOTCH1 transportation and localization [28]. In addition, it can also reduce the concentration of GSI with less side effects [28]. The combination therapy of GSIs and CQ showed excellent synergistic effect in vitro on T-ALL cell line [28]. Because there is PI3K/mTOR pathway activation in T-ALL [29], some researchers have conducted experiments using GSI and mTOR inhibitor rapamycin in mouse model [30]. T-ALL xenograft mice were divided into 4 treatment groups: control group, GSI group, rapamycin group and combination group. The average survival time of the combination group was significantly longer than that of the single agent group and the control group. The combined treatment increased the mean survival time of mice by more than 50 days [30]. These results suggest that the combination of GSI and mTOR inhibitors have synergistic inhibitory effect on T-ALL blasts. The addition of glucocorticoid to GSI can overcome the severe gastric-intestinal toxicity of GSI in a xenograft mice model [19]. The xenograft mice were treated with PF-03084014 (150 mg/kg, twice a day) or PF-03084014 plus dexamethasone (15 mg/kg, once a day) [19]. After euthanizing of mice at day 14, the duodenum in combined treatment mice had similar number of goblet cells to that in untreated animals assayed by histology, which demonstrated that dexamethasone had a protective effect on gastrointestinal toxicity caused by PF-03084014 [19]. Furthermore, the application of GSI can reverse glucocorticoid resistance of T-ALL [31]. In the highly resistant human T-ALL cell line with glucocorticoids, when treated with dexamethasone concentrations as high as 1 × 10–5 M, cells only showed the minimum loss of cell viability. However, the addition of GSI to dexamethasone showed a synergistic dose-dependent response and could effectively reduce cell viability, with a 50% inhibitory concentration value of 7.7 × 10–8 M for dexamethasone in the presence of GSI. The addition of glucocorticoids antagonists can reverse the synergistic effect of combination therapy [32]. There are also other combination options tested. For example, protein kinase CK2 inhibitor CX-4945 combined with GSI can destroy the stability of NOTCH1, reduce the growth and survival of human T-ALL cells [33, 34]. The combined application of cyclin D-dependent kinase CD4 inhibitor and GSI made ALL cells more sensitive to GSI, with a synergistic effects on cell cycle arrest and cell death [35, 36]. Therefore, it is promising to apply GSI with other agents combining with chemotherapy in the management of T-ALL cases.
Currently, no GSI has been approved for the clinical use in treatment of T-ALL. In addition to gastrointestinal toxicity and limited anti-leukemia effects, researchers also found that there are differences in the degree of inhibition of NOTCH1 cleavage by various GSIs and a lack of bioequivalence [37]. Further study found that some T-ALL cells are resistant to GSIs, which may be related to PTEN inactivating mutations [26, 38]. Therefore, further researches on GSIs with different agents are necessary to guarantee the effective management of T-ALL cases with NOTCH1 mutation.
ADAM inhibitors
Notch receptor activation requires ADAM protease (ADAM10 or ADAM17) cleavage at the S2 site. Inhibition of the ADAM protease may block the Notch receptor activation. Therefore, G1254023X, an ADAM10 inhibitor has been investigated in T-ALL. The proliferative rate of Jurkat cells decreased significantly in a dose-dependent manner after treated with 20 μmoL/L G1254023X for 48 h. At the same time, 20 µmoL/L G1254023X has a stronger apoptosis-inducing effect than 10 µmoL/L G1254023X. Significantly higher level of intracellular NOTCH1 protein and lower level of cleaved NOTCH1 protein was observed in the treated cells as compared to the untreated cells. The transcription of Hes-1, one of the target genes of NOTCH1, was reduced by 80–90%. The results suggest that G1254023X induce apoptosis and inhibit proliferation by inhibiting the activation of NOTCH1 signaling pathway in Jurkat cells [39]. This data provide evidences for further exploration of ADAM10 inhibitor in T-ALL with NOTCH1 mutation.
Monoclonal antibody targeting NOTCH1
OMP-52M51 is a monoclonal antibody produced by mice immunized by human NOTCH1 protein fragments [40]. It can bind to the negative regulatory region of NOTCH1 and prevent ligand-free activation of NOTCH1 receptors. OMP-52M51 reduces the level of NOTCH1 intracellular domain in T-ALL cell line in vitro and significantly inhibits T-ALL cell growth in xenograft models [40]. Agnusdai and colleagues [40] reported seven T-ALL xenograft mice (4 NOTCH1 mutants and 3 NOTCH1 wild types) treated with OMP-52M51. All of the T-ALL xenograft mice carrying NOTCH1-mutant had reduced circulating leukemia cells, while the animals carrying NOTCH1 wild-type had no response to OMP-52M51 treatment. The survival time of NOTCH1-mutant T-ALL mice were significantly prolonged in comparison to the animals carrying NOTCH1 wild-type after treatment with OMP-52M51(mean 44 days vs. 15 days). Leukemia burden were reduced by 90% in animals with NOTCH1-mutant by administration of OMP-52M51. At necropsy, the spleen size was significantly reduced in mice treated with anti-NOTCH1 antibody compared to that in the untreated group. Ki67 staining showed a significant reduction after anti-NOTCH1 antibody administration. Similar to GSIs, the combined application of OMP-52M51 and dexamethasone enhances the anti-NOTCH1 efficacy [40]. However, some T-ALL xenografts developed resistance to OMP-52M51. And gene sequencing analysis suggested that OMP-52M51 resistant mice mostly carried two activation mutations of NOTCH1 gene: p.Q1584H and p.L1585P [41]. Therefore, T-ALL patients with p.Q1584H and p.L1585P mutations of NOTCH1 gene may not benefit from OMP-52M51. However, there are no further clinical trials to support this hypothesis, and further research is needed.
Ankur and colleagues generated a monoclonal antibody mAb604.107 against the negative regulatory region of NOTCH1 [42]. At low concentrations (1–2 μg/mL), it can distinguish the conformation of the NRR region between mutated NOTCH1 and wild-type NOTCH1. T-ALL leukemia-initiating cells were inhibited by mAb604.107. The mAb604.107 can increase the sensitivity of the chemotherapy drug doxorubicin in an animal model [42]. Therefore, mAb604.107 may be a promising monoclonal antibody targeting NOTCH1-mutant in T-ALL.
Direct inhibition of NOTCH1 transcription factor complex
ICN1 combines with CSL to form a long and shallow groove in cell nucleus, which serves as the binding surface of MAML. A synthetic cell-permeable α-helix peptide, SAHM1, targets the ternary complex of ICN1-CSL-MAML in NOTCH signaling pathway [43]. The α-helical peptide SAHM1 competes with MAML1 to bind to the ICN1-CSL complex, and blocks the formation of ICN1-CSL-MAML ternary complex, thus leading to the inhibition of NOTCH1 target gene expression. In the T-ALL mouse model, cell proliferation was significantly reduced after SAHM1 treatment, while mRNA levels of Heyl, Hes1, Myc, Dtx1 and Nrarp were significantly reduced [43]. And the animals treated with SAHM1 showed that the weight of the spleen and the absolute number of donor-derived circulating lymphoblasts were significantly reduced. Histopathological examination of bone marrow and spleen showed a significant reduction in leukemia infiltration. The T-ALL bioluminescent mouse model was treated with intraperitoneal injection of SAHM1 or placebo, once daily (35 mg/kg) or twice daily (30 mg/kg). The control mice experienced progressive disease, and 8/9 of them showed higher bioluminescence within 5 days. The mice treated with SAHM1 had less bioluminescence and fewer animals with progressive disease (4/6). These data suggest that targets in the complex of NOTCH signaling pathway may be an alternative option in management of T-ALL with over activation of NOTCH signals.
SERCA inhibitors
The formation of the NOTCH1 receptor protein HD region and the transport process of NOTCH1 require the participation of calcium ions [17]. The NOTCH1 signal is related to the intracellular Ca2+ homeostasis in T-ALL [44]. In a NOTCH1-dependent model of T-ALL, the absence of Ca2+ channel activators STIM1 and STIM2 can significantly prolong the survival of these animals [45]. Ca2+ ATPase (SERCA) regulates the calcium ion concentration. Therefore, some studies explore the role of SERCA inhibitors in activation of NOTCH1 signaling pathway.
The compound thapsigargicin was screened from a series of SERCA inhibitors. The study in vitro showed that thapsigargicin induced cellular apoptosis by depletion of endoplasmic reticulum calcium ions and oxidative stress. The inhibitory effect of thapsigargicin on T-ALL was evaluated in cell lines and mouse model [46]. Thapsigargicin inhibits NOTCH1 mutated T-ALL cells more specifically than NOTCH1 wild-type T-ALL cells. However, severe dose-limited cardiotoxicity was observed, which limited the clinical application [47]. The folate conjugate named as JQ-FT combines folic acid with thapsigargicin through a cleavable bond to achieve leukemia-specific delivery of thapsigargicin. JQ-FT is a NOTCH1 inhibitor with a dual selectivity, targeting both NOTCH1 mutations and leukemia cells. In the xenograft model, JQ-FT inhibits NOTCH1-mutated T-ALL growth in vivo. And the sensitivity of JQ-FT to cells in NOTCH1-mutated T-ALL is higher than that of NOTCH1 wild-type cells [47].
Clerodane diterpene casearin J (CJ), a natural SERCA inhibitor, mainly targets NOTCH1 HD domain mutant in T-ALL. Experiments in cell lines show that CJ can induce T-ALL cell death in the low molar concentration [48]. CJ reduces the level of ICN1 in T-ALL cells carrying NOTCH1 HD domain mutations, and this effect was significantly reduced in the cells with normal NOTCH alleles and juxtamembrane expansion mutations [49]. CJ can also cause slight activation of NF-κB. The combined treatment of CJ and NF-κB inhibitor, parthenolide, resulted in significant synergistic death of T-ALL cells [48].
Recently, Marchesini and colleagues identified an oral SERCA inhibitor, CAD204520 [50]. The toxicity of CAD204520 to off-target calcium ions is significantly reduced. T-ALL xenograft mice treated with CAD204520 by oral gavage (dose 45 mg/kg, twice a day, 8 h apart, for 4 days) showed that the percentages of circulating leukemia cells were 56-fold reduced compared to the control group. Leukemia infiltration in the spleen also decreased significantly. There were no weight loss, no adverse effects on behavior, and no signs of acute cardiotoxicity or gastrointestinal metaplasia observed in mice treated with CAD204520. The complete blood count of the treatment group had no significant difference from control group. There were no general pathological abnormalities in internal organs, including heart, lung, liver, brain and kidney at 21 days after the treatment. These data demonstrated that CAD204520 is a promising option in the management of T-ALL with NOTCH mutation due to its high efficacy and tolerable toxicities.
Other agents
In addition to the above studies, there are other experimental protocols targeting NOTCH1 [51, 52], such as the proteasome inhibitor (bortezomib) [53], histone deacetylase inhibitor (panobinostat) [54], HSP90 inhibitor [55, 56], insecticide (mebendazole) [57], geranylgeranyl diphosphate synthase inhibition (digeranyl bisphosphonate, DGBP) [58], and the antibody Rova-T against its ligand DLL3 [59]. Other natural anti-NOTCH compounds have been shown to inhibit NOTCH1 mutant T-ALL cells, such as plant polyphenol flavonoids [60], artemisinin [61], etc. However, all of the currently investigated agents targeting on Notch signaling pathway are waiting to be approved for clinical application in the management of T-ALL patients [2].
Conclusion and prospect
NOTCH1 gene plays an important role in lymphocyte differentiation, development and proliferation [62, 63]. Mutations in NOTCH1 gene play a key role in the occurrence and progression of ALL, especially T-ALL [64, 65]. Therefore, targeting the NOTCH1 signaling pathway in T-ALL has been a research focus in recent years. The complex mechanism of NOTCH1 and its signaling pathway in T-ALL also provides many treatment options for this disease (Table 1). Researchers have developed GSIs, ADAM10 inhibitors, monoclonal antibodies, SERCA inhibitors, a-helical peptides that inhibit NOTCH1 transcription factor complex, and other agents to interfere with the NOTCH signaling pathway. Although the clinical trials of GSIs alone have shown limited anti-tumor efficacy and dose-limiting toxicity, the development in GSIs and the combination with other agents showed some promising therapeutic effects. Meanwhile, other agents in preclinical trials targeting NOTCH1 signaling pathway have shown efficacy against T-ALL. Since each agents has its own limitations (Table 2), none of the agents targeting NOTCH1 signaling pathway in T-ALL is currently applied in clinical practice. But it is undeniable that targeted therapy on NOTCH1 signaling pathway is showing promises for a breakthrough in T-ALL management. It is expected that further investigation in the field will significantly benefit the T-ALL patients.
Table 1.
Agents targeting NOTCH1 pathway in T-ALL
| Name | Target | Mechanism | Type of cancer | Phase | NCT number/publication date | Assessment |
|---|---|---|---|---|---|---|
| MK-0752 | γ-Secretase | Induce G0/G1 cell cycle arrest and inhibit cell proliferation | T-ALL | I | 2006 | Transient anti-leukemia effect but severe diarrhea |
| PF-03084014 | γ-Secretase | Inhibit ICN1 levels and the expression of Notch target genes | T-ALL or T-cell lymphoblastic lymphoma | I | NCT00878189 | 1/8 achieved complete remission lasting about 3 months and the most common adverse effects were nausea and vomiting |
| BMS-906024 | γ-Secretase | γ-Secretase inhibitor screened by efficacy/tolerance profile | T-ALL or T-cell lymphoblastic lymphoma | I | NCT01363817 | 32% showed at least a 50% reduction in bone marrow blasts and had tolerable side effects |
| MRK-560 | PSEN1 of γ-Secretase | Selective γ-Secretase inhibitor, mainly target PSEN1 in the γ-secretase complex | T-ALL | Preclinical | July 1, 2019 | Improved survival and did not show obvious gastrointestinal pathological |
| G1254023X | ADAM | Prevent ADAM protease cleavage Notch receptor at the S2 site | T-ALL | Preclinical | August 20, 2015 | Inhibited the activation of NOTCH1 signaling pathway and induce apoptosis |
| OMP-52M51 | NRR | Prevent ligand-free activation of NOTCH1 receptors | T-ALL | Preclinical | July 23, 2013 | Prolonged survival time but had drug resistance |
| MAb 604.107 | NRR | Distinguish the conformation of the NRR region between mutant NOTCH1 and wild-type NOTCH1 | T-ALL | Preclinical | June 5, 2015 | Inhibited T-ALL leukemia-initiating cells |
| SAHM1 | ICN1-CSL-MAML complex | Block the formation of ICN1-CSL-MAML complex, and inhibit the activation of NOTCH1 target gene expression | T-ALL | Preclinical | November 12, 2009 | Inhibited leukemic progression and NOTCH1 signaling |
| Thapsigargicin | SERCA | Induce the depletion of endoplasmic reticulum calcium ions and oxidative stress, which ultimately leads to apoptosis | T-ALL | Preclinical | March 18, 2013 | Effective but severe cardiotoxicity |
| JQ-FT | SERCA | Combine folic acid and thapsigargicin with a cleavable bond to achieve leukemia-specific delivery of thapsigargicin | T-ALL | Preclinical | January 2, 2018 | Dual selectivity: targeting NOTCH1 mutations and targeting leukemia cells, but Complex process and poor practicality |
| CJ | SERCA | Target NOTCH1 HD domain mutant T-ALL, induce T-ALL cell death | T-ALL | Preclinical | January 28, 2016 | Mainly target NOTCH1 HD domain mutation but weak effect on cells with mutations in other domains of NOTCH1 |
| CAD204520 | SERCA | Retain the anti-NOTCH1 tumor characteristics while inhibiting thapsigargicin-resistant cell lines | T-ALL | Preclinical | June 18, 2020 | Effective and had tolerable side effects |
Table 2.
Adverse events for each agent
| Type of agents | Agents | Adverse events |
|---|---|---|
| γ-Secretase inhibitors (GSIs) | MK-0752 | Gastrointestinal toxicity (mainly diarrhea) |
| PF-03084014 | Nausea and vomiting | |
| BMS-906024 | Tolerable gastrointestinal toxicity | |
| MRK-560 | Did not show obvious gastrointestinal pathological changes and thymus T cell development defects | |
| ADAM inhibitors | G1254023X | No records of adverse events related to the drug found in the literature |
| Monoclonal antibody targeting NOTCH1 | OMP-52M51 | May be resistant to T-ALL of carried two activation mutations of NOTCH1 gene: p.Q1584H and p.L1585P |
| mAb604.107 | No records of adverse events related to the drug found in the literature | |
| Direct inhibition of NOTCH1 transcription factor complex | SAHM1 | No records of adverse events related to the drug found in the literature |
| SERCA inhibitors | Thapsigargicin | Severe dose-limited cardiotoxicit |
| JQ-FT | Complex process and poor practicality | |
| Clerodane diterpene casearin J (CJ) | No records of adverse events related to the drug found in the literature | |
| CAD204520 | No weight loss, no adverse effects on behavior, and no signs of acute cardiotoxicity or gastrointestinal metaplasia |
Acknowledgements
We are grateful for the English editing by Dr. Yajun Liu from the Department of Orthopaedics, Brown University, Warren Alpert Medical School/Rhode Island Hospital, Rhode Island, the United States.
Abbreviations
- T-ALL
T-cell acute lymphoblastic leukemia
- CAR-T
Chimeric antigen receptor modified T
- EGF
Epidermal growth factor
- NRR
Negative regulatory region
- LNR
Lin12-Notch repeats
- HD
Heterodimerization domain
- PEST domain
Proline/glutamic acid/serine/threonine enriched motif
- ADAM
A disintergrin and metalloprotease
- GSI
γ-Secretase inhibitor
- ICN1
Intracellular domain of NOTCH1
- CQ
Chloroquine
- CSL
C-promoter binding factor 1 CBF-1, suppressor of hairless, lag
- MAML
Mastermind-like
- SERCA
Ca2+ ATPase
- CJ
Clerodane diterpene casearin J
Authors’ contributions
RZ and ML drafted the manuscript. SW and YL participated in the design and revision of the manuscript. All authors read and approved the final manuscript.
Funding
The study is partly supported by the National Natural Science Foundation of China (Grant Numbers 81800137).
Availability of data and materials
The material supporting the conclusion of this review has been included within the article.
Ethics approval and consent to participate
This is not applicable for this review.
Consent for publication
This is not applicable for this review.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Ruyue Zheng and Menglin Li contributed equally to this work
Contributor Information
Ruyue Zheng, Email: asmoonzheng123@163.com.
Menglin Li, Email: bjyx1197695396@163.com.
Shujuan Wang, Email: fccwangsj1@zzu.edu.cn.
Yanfang Liu, Email: fccliuyf1@zzu.edu.cn.
References
- 1.Gomes-Silva D, Srinivasan M, Sharma S, Lee CM, Wagner DL, Davis TH, Rouce RH, Bao G, Brenner MK, Mamonkin M. CD7-edited T cells expressing a CD7-specific CAR for the therapy of T-cell malignancies. Blood. 2017;130(3):285–296. doi: 10.1182/blood-2017-01-761320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Katoh M, Katoh M. Precision medicine for human cancers with Notch signaling dysregulation (Review) Int J Mol Med. 2020;45(2):279–297. doi: 10.3892/ijmm.2019.4418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liu H, Chiang MY, Pear WS. Critical roles of NOTCH1 in acute T-cell lymphoblastic leukemia. Int J Hematol. 2011;94(2):118–125. doi: 10.1007/s12185-011-0899-3. [DOI] [PubMed] [Google Scholar]
- 4.Salah A. Significance of NOTCH1 mutations detections in T-acute lymphoblastic leukemia patients. Cancer Biomark Sect A Dis Mark. 2020;27(2):157–162. doi: 10.3233/CBM-190967. [DOI] [PubMed] [Google Scholar]
- 5.Meurette O, Mehlen P. Notch signaling in the tumor microenvironment. Cancer Cell. 2018;34(4):536–548. doi: 10.1016/j.ccell.2018.07.009. [DOI] [PubMed] [Google Scholar]
- 6.Chiang MY, Radojcic V, Maillard I. Oncogenic notch signaling in T-cell and B-cell lymphoproliferative disorders. Curr Opin Hematol. 2016;23(4):362–370. doi: 10.1097/MOH.0000000000000254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tan SH, Bertulfo FC, Sanda T. Leukemia-initiating cells in T-cell acute lymphoblastic leukemia. Front Oncol. 2017;7:218. doi: 10.3389/fonc.2017.00218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Garcia-Peydro M, Fuentes P, Mosquera M, Garcia-Leon MJ, Alcain J, Rodriguez A, et al. The NOTCH1/CD44 axis drives pathogenesis in a T cell acute lymphoblastic leukemia model. J Clin Investig. 2018;128(7):2802–2818. doi: 10.1172/JCI92981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kimura S, Seki M, Yoshida K, Shiraishi Y, Akiyama M, Koh K, et al. NOTCH1 pathway activating mutations and clonal evolution in pediatric T-cell acute lymphoblastic leukemia. Cancer Sci. 2019;110(2):784–794. doi: 10.1111/cas.13859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guruharsha KG, Kankel MW, Artavanis-Tsakonas S. The Notch signalling system: recent insights into the complexity of a conserved pathway. Nat Rev Genet. 2012;13(9):654–666. doi: 10.1038/nrg3272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhong FF, Yang Y, Liu WJ. Progress in research on childhood T-cell acute lymphocytic leukemia, Notch1 signaling pathway, and its inhibitors: a review. Bosn J Basic Med Sci. 2020;4687:1–9. doi: 10.17305/bjbms.2020.4687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hori K, Sen A, Artavanis-Tsakonas S. Notch signaling at a glance. J Cell Sci. 2013;126(Pt 10):2135–2140. doi: 10.1242/jcs.127308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Garcia-Leon MJ, Fuentes P, de la Pompa JL, Toribio ML. Dynamic regulation of NOTCH1 activation and Notch ligand expression in human thymus development. Development. 2018;16:dev165597. doi: 10.1242/dev.165597. [DOI] [PubMed] [Google Scholar]
- 14.Kopan R, Ilagan MXG. The canonical notch signaling pathway: unfolding the activation mechanism. Cell. 2009;137(2):216–233. doi: 10.1016/j.cell.2009.03.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Adolfo F. Can one target T-cell ALL? Best practice & research. Clin Haematol. 2018;31(4):361–366. doi: 10.1016/j.beha.2018.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tosello V, Ferrando AA. The NOTCH signaling pathway: role in the pathogenesis of T-cell acute lymphoblastic leukemia and implication for therapy. Ther Adv Hematol. 2013;4(3):199–210. doi: 10.1177/2040620712471368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sorrentino C, Cuneo A, Roti G. Therapeutic targeting of notch signaling pathway in hematological malignancies. Mediterr J Hematol Infect Dis. 2019;11(1):e2019037. doi: 10.4084/mjhid.2019.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yang Y, Li XM, Wang T, Guo QQ, Xi T, Zheng LF. Emerging agents that target signaling pathways in cancer stem cells. J Hematol Oncol. 2020;13(1):60. doi: 10.1186/s13045-020-00901-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wei P, Walls M, Qiu M, Ding R, Denlinger RH, Wong A, et al. Evaluation of selective gamma-secretase inhibitor PF-03084014 for its antitumor efficacy and gastrointestinal safety to guide optimal clinical trial design. Mol Cancer Ther. 2010;9(6):1618–1628. doi: 10.1158/1535-7163.MCT-10-0034. [DOI] [PubMed] [Google Scholar]
- 20.Papayannidis C, DeAngelo DJ, Stock W, Huang B, Shaik MN, Cesari R, et al. A phase 1 study of the novel gamma-secretase inhibitor PF-03084014 in patients with T-cell acute lymphoblastic leukemia and T-cell lymphoblastic lymphoma. Blood Cancer J. 2015;5:e350. doi: 10.1038/bcj.2015.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gavai AV, Quesnelle C, Norris D, Han WC, Gill P, Shan WF, et al. Discovery of clinical candidate BMS-906024: a potent pan-notch inhibitor for the treatment of leukemia and solid tumors. ACS Med Chem Lett. 2015;6(5):523–527. doi: 10.1021/acsmedchemlett.5b00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Knoechel B, Bhatt A, Pan L, Pedamallu CS, Severson E, Gutierrez A, et al. Complete hematologic response of early T-cell progenitor acute lymphoblastic leukemia to the γ-secretase inhibitor BMS-906024: genetic and epigenetic findings in an outlier case. Cold Spring Harbor Lab Press. 2015;1(1):a000539. doi: 10.1101/mcs.a000539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zweidler-McKay P DD, Douer D. The safety and activity of BMS- 906024, a gamma secretase inhibitor (GSI) with anti-notch activity, in patients with relapsed T-cell acute lymphoblastic leukemia (T-ALL): initial results of a phase I trial [abstract]. Blood. 2014;121(21):Abstract 968.
- 24.Maria GB. Adjusting the focus on γ-secretase inhibition. Nat Rev Cancer. 2019;19(8):419. doi: 10.1038/s41568-019-0174-0. [DOI] [PubMed] [Google Scholar]
- 25.Sanchez-Martin M, Ambesi-Impiombato A, Qin Y, Herranz D, Bansal M, Girardi T, et al. Synergistic antileukemic therapies in NOTCH1 -induced T-ALL. Proc Natl Acad Sci USA. 2017;114(8):2006–2011. doi: 10.1073/pnas.1611831114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lisa MG. Inhibition of γ-secretase activity synergistically enhances tumour necrosis factor-related apoptosis-inducing ligand induced apoptosis in T-cell acute lymphoblastic leukemia cells via upregulation of death receptor 5. Oncol Lett. 2016;12(4):2900–2905. doi: 10.3892/ol.2016.5011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mendes RD, Canté-Barrett K, Pieters R, Meijerink JPP. The relevance of PTEN-AKT in relation to NOTCH1-directed treatment strategies in T-cell acute lymphoblastic leukemia. Haematologica. 2016;101(9):1010–1017. doi: 10.3324/haematol.2016.146381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hounjet J, Habets R, Schaaf MB, Hendrickx TC, Barbeau L, Yahyanejad S, et al. The anti-malarial drug chloroquine sensitizes oncogenic NOTCH1 driven human T-ALL to γ-secretase inhibition. Oncogene. 2019;38(27):5457–5468. doi: 10.1038/s41388-019-0802-x. [DOI] [PubMed] [Google Scholar]
- 29.Tasian SK, Teachey DT, Rheingold SR. Targeting the PI3K/mTOR pathway in pediatric hematologic malignancies. Front Oncol. 2014;4:108. doi: 10.3389/fonc.2014.00108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cullion K, Draheim KM, Hermance N, Tammam J, Sharma VM, Ware C, et al. Targeting the Notch1 and mTOR pathways in a mouse T-ALL model. Blood. 2009;113(24):6172–6181. doi: 10.1182/blood-2008-02-136762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Real PJ, Ferrando AA. NOTCH inhibition and glucocorticoid therapy in T-cell acute lymphoblastic leukemia. Leukemia. 2009;23(8):1374–1377. doi: 10.1038/leu.2009.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Real PJ, Tosello V, Palomero T, Castillo M, Hernando E, De SE, et al. Gamma-secretase inhibitors reverse glucocorticoid resistance in T cell acute lymphoblastic leukemia. Nat Med. 2009;15(1):50–58. doi: 10.1038/nm.1900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lian HW, Li D, Zhou Y, Landesman-Bollag E, Zhang G, Anderson NM, et al. CK2 inhibitor CX-4945 destabilizes NOTCH1 and synergizes with JQ1 against human T-acute lymphoblastic leukemic cells. Haematologica. 2017;102(1):e17–e21. doi: 10.3324/haematol.2016.154013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Silva A, Jotta PY, Silveira AB, Ribeiro D, Brandalise SR, Yunes JA, et al. Regulation of PTEN by CK2 and Notch1 in primary T-cell acute lymphoblastic leukemia: rationale for combined use of CK2- and gamma-secretase inhibitors. Haematologica. 2010;95(4):674–678. doi: 10.3324/haematol.2009.011999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rao SS, O'Neil J, Liberator CD, Hardwick JS, Dai XD, Zhang T, et al. Inhibition of NOTCH signaling by gamma secretase inhibitor engages the RB pathway and elicits cell cycle exit in T-cell acute lymphoblastic leukemia cells. Can Res. 2009;69(7):3060–3068. doi: 10.1158/0008-5472.CAN-08-4295. [DOI] [PubMed] [Google Scholar]
- 36.Joshi I, Minter LM, Telfer J, Demarest RM, Capobianco AJ, Aster JC, et al. Notch signaling mediates G1/S cell-cycle progression in T cells via cyclin D3 and its dependent kinases. Blood. 2009;113(8):1689–1698. doi: 10.1182/blood-2008-03-147967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yong R. γ-Secretase inhibitors in cancer clinical trials are pharmacologically and functionally distinct. EMBO Mol Med. 2017;9(7):950–966. doi: 10.15252/emmm.201607265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Palomero T, Dominguez M, Ferrando AA. The role of the PTEN/AKT pathway in NOTCH1-induced leukemia. Cell Cycle. 2008;7(8):965–970. doi: 10.4161/cc.7.8.5753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ma S, Xu J, Wang X, Wu QY, Cao J, Li ZY, et al. Effect of ADAM10 Inhibitor GI254023X on proliferation and apoptosis of acute T-lymphoblastic leukemia jurkat cells in vitro and its possible mechanisms. J Exp Hematol. 2015;23(4):950–955. doi: 10.7534/j.issn.1009-2137.2015.04.008. [DOI] [PubMed] [Google Scholar]
- 40.Agnusdei V, Minuzzo S, Frasson C, Grassi A, Axelrod F, Satyal S, et al. Therapeutic antibody targeting of Notch1 in T-acute lymphoblastic leukemia xenografts. Leukemia. 2014;28(2):278–288. doi: 10.1038/leu.2013.183. [DOI] [PubMed] [Google Scholar]
- 41.Valentina A, Sonia M, Marica P, Alessandra G, Laura P, Agnese AA, et al. Dissecting molecular mechanisms of resistance to NOTCH1-targeted therapy in T-cell acute lymphoblastic leukemia xenografts. Haematologica. 2020;105(5):1317–1328. doi: 10.3324/haematol.2019.217687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ankur S, Rupali AG, Satthenapalli VR, Krishnanand P, Davanam SM, Lakshmi D, et al. A novel monoclonal antibody against notch1 targets leukemia-associated mutant notch1 and depletes therapy resistant cancer stem cells in solid tumors. Sci Rep. 2015;5:11012. doi: 10.1038/srep11012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Moellering RE, Cornejo M, Davis TN, Del BC, Aster JC, Blacklow SC, et al. Direct inhibition of the NOTCH transcription factor complex. Nature. 2009;462(7270):182–188. doi: 10.1038/nature08543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gachet S, Genescà E, Passaro D, Irigoyen M, Alcalde H, Clémenson C, et al. Leukemia-initiating cell activity requires calcineurin in T-cell acute lymphoblastic leukemia. Leukemia. 2013;27(12):2289–2300. doi: 10.1038/leu.2013.156. [DOI] [PubMed] [Google Scholar]
- 45.Fleur-Lominy SS, Maus M, Vaeth M, Lange I, Zee I, Suh D, et al. STIM1 and STIM2 mediate cancer-induced inflammation in T cell acute lymphoblastic leukemia. Cell Rep. 2018;24(11):3045–3060. doi: 10.1016/j.celrep.2018.08.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Giovanni R, Anne C, Kenneth NR, Michele M, Kostandin P, Angela HS, et al. Complementary genomic screens identify SERCA as a therapeutic target in NOTCH1 mutated cancer. Cancer Cell. 2013;23(3):390–415. doi: 10.1016/j.ccr.2013.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Giovanni R, Jun Q, Samuel K, Marta SM, Amy SC, Anthony CV, et al. Leukemia-specific delivery of mutant NOTCH1 targeted therapy. J Exp Med. 2018;215(1):197–216. doi: 10.1084/jem.20151778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.De FC, Heidersdorf B, Haun F, Murillo R, Friedrich T, Borner C, et al. The clerodane diterpene casearin J induces apoptosis of T-ALL cells through SERCA inhibition, oxidative stress, and interference with Notch1 signaling. Cell Death Dis. 2016;7:e2070. doi: 10.1038/cddis.2015.413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sara CL, Sabine S. Complexity of NOTCH1 juxtamembrane insertion mutations in T-cell acute lymphoblastic leukemia. Leukemia Lymphoma. 2016;57(5):1219–1222. doi: 10.3109/10428194.2015.1080366. [DOI] [PubMed] [Google Scholar]
- 50.Marchesini M, Gherli A, Montanaro A, Patrizi L, Sorrentino C, Pagliaro L, et al. Blockade of oncogenic NOTCH1 with the SERCA inhibitor CAD204520 in T cell acute lymphoblastic leukemia. Cell Chem Biol. 2020;27:1–20. doi: 10.1016/j.chembiol.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Diana B, Rocco P, Pia FM, Isabella S, Saula C. Notch signaling as a therapeutic target for acute lymphoblastic leukemia. Expert Opin Ther Targets. 2018;22(4):331–342. doi: 10.1080/14728222.2018.1451840. [DOI] [PubMed] [Google Scholar]
- 52.Hefazi M, Litzow MR. Recent advances in the biology and treatment of T cell acute lymphoblastic leukemia. Curr Hematol Malig Rep. 2018;13(4):265–274. doi: 10.1007/s11899-018-0455-9. [DOI] [PubMed] [Google Scholar]
- 53.Koyama D, Kikuchi J, Hiraoka N, Wada T, Kurosawa H, Chiba S, et al. Proteasome inhibitors exert cytotoxicity and increase chemosensitivity via transcriptional repression of Notch1 in T-cell acute lymphoblastic leukemia. Leukemia. 2014;28(6):1216–1226. doi: 10.1038/leu.2013.366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wai BM, Vervoort SJ, Kong IY, Heinzel S, Ramsbottom KM, Martin BP, et al. Epigenetic targeting of Notch1-driven transcription using the HDACi panobinostat is a potential therapy against T-cell acute lymphoblastic leukemia. Leukemia. 2018;32(1):237–241. doi: 10.1038/leu.2017.282. [DOI] [PubMed] [Google Scholar]
- 55.Wang Z, Hu Y, Xiao D, Wang J, Liu C, Xu Y, et al. Stabilization of Notch1 by the Hsp90 chaperone is crucial for T-cell leukemogenesis. Clin Cancer Res. 2017;23(14):3834–3846. doi: 10.1158/1078-0432.CCR-16-2880. [DOI] [PubMed] [Google Scholar]
- 56.Sanda T, Li XY, Gutierrez A, Ahn Y, Neuberg DS, O'Neil J, et al. Interconnecting molecular pathways in the pathogenesis and drug sensitivity of T-cell acute lymphoblastic leukemia. Blood. 2010;115(9):1735–1745. doi: 10.1182/blood-2009-07-235143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wang XL, Lou KY, Song XD, Ma HJ, Zhou XY, Xu H, et al. Mebendazole is a potent inhibitor to chemoresistant T cell acute lymphoblastic leukemia cells. Toxicol Appl Pharmacol. 2020;396:115001. doi: 10.1016/j.taap.2020.115001. [DOI] [PubMed] [Google Scholar]
- 58.Agabiti SS, Li J, Dong W, Poe MM, Wiemer AJ. Regulation of the Notch-ATM-abl axis by geranylgeranyl diphosphate synthase inhibition. Cell Death Dis. 2019;10(10):733. doi: 10.1038/s41419-019-1973-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Leonetti A, Facchinetti F, Minari R, Cortellini A, Rolfo CD, Giovannetti E, et al. Notch pathway in small-cell lung cancer: from preclinical evidence to therapeutic challenges. Cell Oncol (Dordrecht) 2019;42(3):261–273. doi: 10.1007/s13402-019-00441-3. [DOI] [PubMed] [Google Scholar]
- 60.Zhu W, Zhu Y, Xu H, Wang T, Wang J, Meng M, et al. Flavone inhibited proliferation of T-ALL by promoting c-Cbl-induced ubiquitinylation and degradation of Notch1. Biochem Biophys Res Commun. 2020;522(3):684–689. doi: 10.1016/j.bbrc.2019.11.148. [DOI] [PubMed] [Google Scholar]
- 61.Ohtaka M, Itoh M, Tohda S. BMI1 inhibitors down-regulate NOTCH signaling and suppress proliferation of acute leukemia cells. Anticancer Res. 2017;37(11):6047–6053. doi: 10.21873/anticanres.12052. [DOI] [PubMed] [Google Scholar]
- 62.Brandstadter JD, Maillard I. Notch signalling in T cell homeostasis and differentiation. Open Biol. 2019;9(11):190187. doi: 10.1098/rsob.190187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Medyouf H, Gao X, Armstrong F, Gusscott S, Liu Q, Gedman AL, et al. Acute T-cell leukemias remain dependent on Notch signaling despite PTEN and INK4A/ARF loss. Blood. 2010;115(6):1175–1184. doi: 10.1182/blood-2009-04-214718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Aifantis I, Vilimas T, Buonamici S. Notches, NFkappaBs and the making of T cell leukemia. Cell Cycle. 2007;6(4):403–406. doi: 10.4161/cc.6.4.3858. [DOI] [PubMed] [Google Scholar]
- 65.Choi SH, Severson E, Pear WS, Liu XS, Aster JC, Blacklow SC. The common oncogenomic program of NOTCH1 and NOTCH3 signaling in T-cell acute lymphoblastic leukemia. PLoS ONE. 2017;12(10):e0185762. doi: 10.1371/journal.pone.0185762. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The material supporting the conclusion of this review has been included within the article.