Abstract
Wearable smart sensors are emerging technology for daily monitoring of vital signs with the reducing discomfort and interference with normal human activities. The main objective of this study was to review the applied wearable smart sensors for disease control and vital signs monitoring in epidemics outbreaks. A comprehensive search was conducted in Web of Science, Scopus, IEEE Library, PubMed and Google Scholar databases to identify relevant studies published until June 2, 2020. Main extracted specifications for each paper are publication details, type of sensor, disease, type of monitored vital sign, function and usage. Of 277 articles, 11 studies were eligible for criteria. 36% of papers were published in 2020. Articles were published in 10 different journals and only in the Journal of Medical Systems more than one article was published. Most sensors were used to monitor body temperature, heart rate and blood pressure. Wearable devices (like a helmet, watch, or cuff) and body area network sensors were popular types which can be used monitoring vital signs for epidemic trending. 65% of total papers (n = 6) were conducted by the USA, Malaysia and India. Applying appropriate technological solutions could improve control and management of epidemic disease as well as the application of sensors for continuous monitoring of vital signs. However, further studies are needed to investigate the real effects of these sensors and their effectiveness.
Keywords: Wearable sensors, Vital signs monitoring, Epidemics outbreak, Body area network
Introduction
Health services due to information technology development have great changes, especially in remote monitoring (Li et al. 2019). Focusing on disease prevention and early detection of high-risk disease disabilities is one of the main goals of using physical sensor networks (Majumder et al. 2017). Todays, the smart systems and developed tools have significantly increased for the instant monitoring among the patients and controlling their conditions (Gries et al. 2018). The ability of such smart systems in storing and transferring data is of great importance in different branches of healthcare (e.g. Telemedicine) (Ha et al. 2018). Wearable systems are mainly used for monitoring the symptoms and status of patients, follow up, telemedicine, monitoring of nursing and medical team systems, surgery robots, and many other systems (Lin et al. 2018; Majumder and Deen 2019). However, wearable sensors have received tremendous attention over the past decade, mainly concentrated in the healthcare industry. Such products attempt to apply physical signals such as heart rate, blood pressure, skin temperature, respiratory rate and body motion to extract clinically relevant information (Nag et al. 2019). Wireless body sensor networks (WBAN) include a number of heterogeneous biological sensors (Richesson et al. 2019). The sensors of such networks are placed on different areas of the body and these sensors can be worn or implanted on the body of the person. Each of these sensors requires specific requirements to identify and record symptoms (Rajan et al. 2018; Rezayi et al. 2019).
Since many diseases and disabilities require continuous monitoring in the present era, the continuity of patient monitoring for timely intervention seems essential (Dahiya et al. 2019; Richesson et al. 2019). As such, one of the most important areas of application of wearable technologies in healthcare field is utilizing WBANs to monitor patients. In epidemic outbreaks or under EMS (emergency medical service) conditions, patient monitoring is so sensitive and important (Ha et al. 2018). In these situations, the momentary monitoring of patients helps the medical team to take the necessary measures without delay. Patient monitoring announces the threatening events to caretakers, and most of such systems use the physiological input data for the direct control of support tools (Baskar et al. 2020; Kristoffersson and Lindén 2020). Anyhow, considering the present global conditions, the smart wearable sensors for patients̓ s monitoring have the capacity and potential to be a major breakthrough in efforts to control the epidemics. An epidemic is defined by the Centers for Disease Control and Prevention (CDC) as a sudden increase in the number of cases of an infectious disease within a community or geographic area during a specific time period (Edoh 2019; Rahman et al. 2020).
Over the years, many outbreaks of infectious diseases have occurred and spread across the world (Kristoffersson and Lindén 2020). According to the points which were mentioned above, the way of public health surveillance could enlighten by using wearable device data. Since time and speed of operation in disease outbreaks control are so critical, patient monitoring (respiratory rate, temperature rate, blood pressure, ECG, heart rate, SPo2) in the prevalence of epidemics can be considered as an important phase for control and monitor real-time and accurate data (Zhu et al. 2020).
A riches of novel innovative technologies in the form of smart wearable technologies is achieving to greaten global precision and becoming accessible for the main aims of like preventing, monitoring and controlling the infectious diseases. The aim of this systematic review is provide a comprehensive investigation about applying wearable smart sensors for disease control and vital signs monitoring in infection epidemic outbreaks.
Methods
This systematic review was performed based on the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) method (Moher et al. 2009). This method was introduced by Moher et al. and it is one of the best methods that authors can done their systematic reviews.
Literature search
In this review, a search of Web of Science, Scopus, IEEE Library, PubMed and Google Scholar databases was performed to identify relevant studies published until June 2, 2020.
The search strategy included a compressive combined keywords and mesh terms related to wearable smart sensors, patient monitoring and epidemics. The detailed search strategy for each database was presented in Table 1.
Table 1.
Search strategy for each databases
| Database | Search strategy |
|---|---|
| PubMed |
(“Wearable Electronic Devices“[MeSH Terms] OR “Wearable sensor” OR “Wearable device” OR “biosensor” OR “BAN” OR “body sensor network” OR “BSN” OR “biomedical sensor” OR “IoT”) AND (“disease Outbreaks“[MeSH Terms] OR “Epidemics“[MeSH Terms] OR “Outbreak” OR “epidemic”) AND (“monitoring, physiologic“[MeSH Terms] OR “Monitoring, Physiologic” OR “Patient Monitoring” OR “Physiological Monitoring” OR “vital sign monitoring” OR “monitor” OR “monitoring”) Results = 54 |
| IEEE Library |
((“Wearable Devices” OR “Wearable sensor” OR “Wearable device” OR “biosensor” OR “BAN” OR “body sensor network” OR “BSN” OR “biomedical sensor” OR “IoT” OR “wireless wearable technology” OR “wireless wearable” OR “Wearable Electronic Devices” ) AND (“Disease Outbreaks” OR “Epidemics” OR “Outbreak” OR “epidemic”) AND ( “Monitoring, Physiologic” OR “Patient Monitoring” OR “Physiological Monitoring” OR “vital sign monitoring” OR “monitor” OR “monitoring” )) Results = 25 |
| Web of Science |
TS=((“Wearable Devices” OR “Wearable sensor” OR “Wearable device” OR “biosensor” OR “BAN” OR “body sensor network” OR “BSN” OR “biomedical sensor” OR “IoT” OR “wireless wearable technology” OR “wireless wearable” OR “Wearable Electronic Devices”) AND (“Disease Outbreaks” OR “Epidemics” OR “Outbreak” OR “epidemic”) AND (“Monitoring, Physiologic” OR “Patient Monitoring” OR “Physiological Monitoring” OR “vital sign monitoring” OR “monitor” OR “monitoring” )) Results: 54 |
| Scopus |
TITLE-ABS-KEY ((“Wearable Devices” OR “Wearable sensor” OR “Wearable device” OR “biosensor” OR “BAN” OR “body sensor network” OR “BSN” OR “biomedical sensor” OR “IoT” OR “wireless wearable technology” OR “wireless wearable” OR “Wearable Electronic Devices”) AND (“Disease Outbreaks” OR “Epidemics” OR “Outbreak” OR “epidemic”) AND ( "Monitoring, Physiologic" OR “Patient Monitoring" OR “Physiological Monitoring" OR “vital sign monitoring" OR “monitor" OR “monitoring" )) Results = 132 |
| Google Scholar |
All in title: (“wearable sensor” OR “sensor” OR “BAN” OR “wireless sensor”) AND (“epidemics” OR “outbreak disease” OR “epidemic”) Results = 12 |
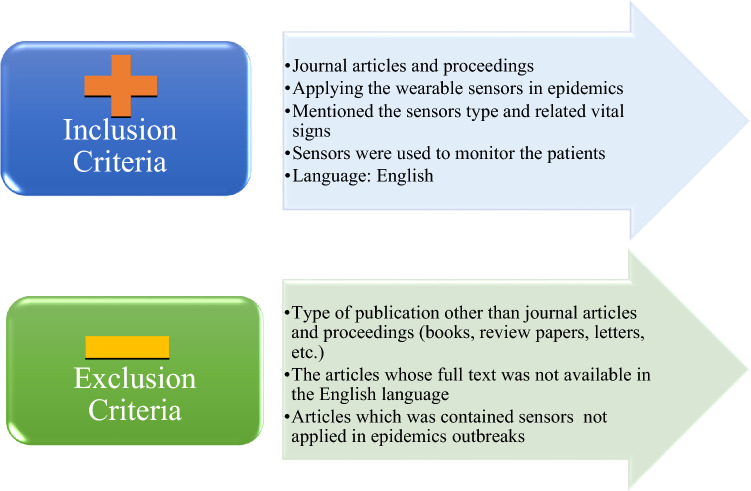
Inclusion and exclusion criteria
The academic selected papers were screened based on inclusion and exclusion criteria that have been displayed in Fig. 1.
Fig. 1.
Exclusion and inclusion criteria to select eligible papers
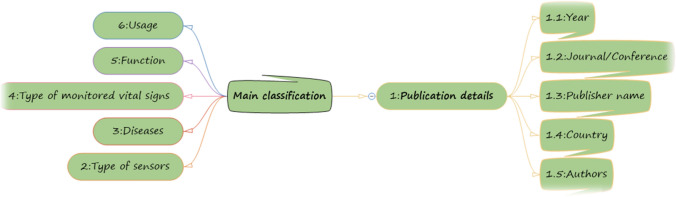
Data extraction phase
In scientific searching 277 papers were retrieved based on some inclusion and exclusion criteria which were performed for selecting eligible articles. In this phase, the main classification of included articles was independently determined by three authors. These three authors (MG, SS and SR) synthesis the main characteristics and specifications of selected papers. They extracted main specification of papers. The next author (NM) evaluated the extracted information; she validated the main elements.
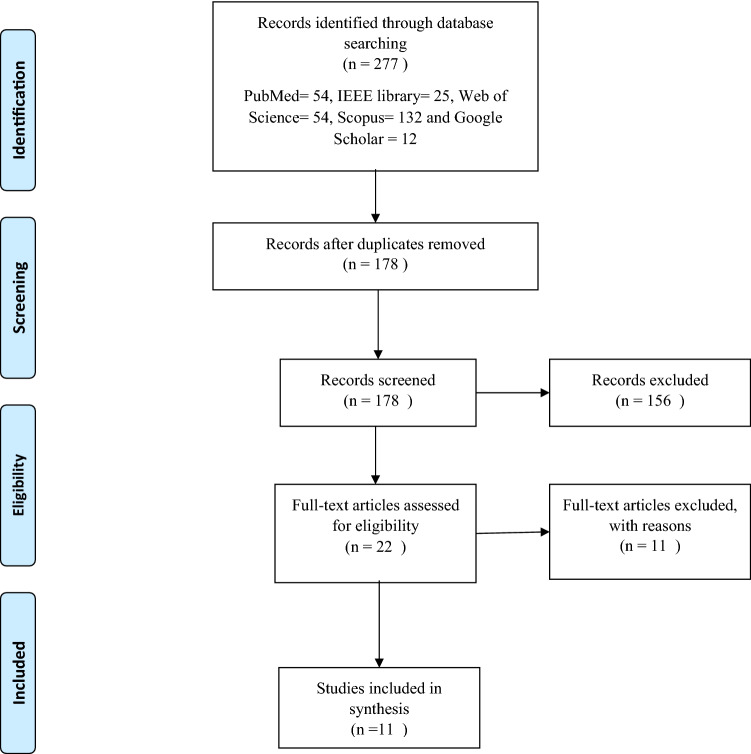
Three reviewers screened the abstract and full titles of papers independently. Another reviewer screened the selected studies randomly. These critical items are imported into a spreadsheet in Excel. The procedure of screening and selecting papers is presented in Fig. 2 based on PRISMA method. However, we presented the main characteristics and elements of included papers in Fig. 3.
Fig. 2.
Flow diagram of the literature search and study selection
Fig. 3.
The main specifications of selected papers
Results
In searching databases phase, 277 relevant papers were retrieved. We removed duplicate studies, 178 citations remained. In the last phase of screening, only 11 relevant papers met our inclusion criteria. Our summary of papers is presented in Table 2. The author's main keywords for selecting papers are displayed by word cloud figure. In the presented figure, we demonstrate the main words with their importance weight; Fig. 4 is our word cloud schema.
Table 2.
The characteristics of reviewed articles
| Author | Country | Main approach | Type of sensor | Disease | Type of monitored vital sign | Function | Applied intelligent methods | Usage |
|---|---|---|---|---|---|---|---|---|
| Mohammed et al. (2020) | Malaysia | Proposing the design of system that has capability to detect the coronavirus automatically from the thermal image with less human interactions using smart helmet | Image processing module: smart helmet | COVID-19 | The data of people’s face and temperature |
Facial-recognition technology can also display the pedestrian’s personal information which can automatically take pedestrians’ temperatures. Optical camera and infrared thermal camera which provided information about the temperature at which the different focuses of interest were found |
Cascade Classification algorithm + Viola–Jones algorithm | This helmet can help to people to screen infected persons; this allows persons with increased body temperature to be identified quickly and reliably, and to be isolated for more exact testing |
| Chung et al. (2020) | Taiwan | Providing the HEARThermo to continuously monitor body surface temperature and heart rate to trigger the reminders sent by chatbots | Watch-like wearable device | COVID-19 | Body surface temperature and heart rate | Body temperature measurements once daily for healthcare workers and twice daily for people in isolation or quarantine are important measures to reduce the risk of cross infections | Not mentioned | The HEARThermo, as a wearable physiological monitor for remotely monitoring the health status of people under risk of infection, provides real-time data and decision support for healthcare providers and public health agencies |
| Hassan et al. (2018) | Malaysia | Proposing a conceptual IoT-based patient monitoring sensor for predicting and controlling dengue outbreak | Body area network: patient worn sensors | Dengue: mosquito-borne virus | Body temperature, heart-beat, blood pressure |
The patient's vital signs and physiological information were monitored by 3 type of sensor These data received from sensors and then analyzed by analytical tools for better and effective decision making |
Cloud computing algorithm: cloud machine learning platform |
The analyzed data and proposed sensors will be used by the medical officer in healthcare organization for decision making. they can be visualized in dashboard to update the predictive factors and controlling the dengue outbreak. Also it can provide right medical support for predicting and controlling dengue |
| Lorence and Wu (2012) | USA | Proposing one promising model for using a combination of emerging systems-based technologies in multi sensor cartridges | Monitoring device worn as an arm cuff | Potential epidemics | Pulse, Blood pressure, or analyte detection |
All data about users may be automatically gathered and stored at the remote server, those data may be used for elaboration of medical prognoses, epidemic trends, and/or risk calculations The server may include a computer program for data processing |
Not mentioned | Where this system can be linked to multiple analyte measures and recorded continuously in real time, the integrated system can serve as an effective public health or clinical application, where there is need for immediate collection |
| Valsalan et al. (2019, 2020) | Oman | Designing and implementation of a smart patient health tracking system that uses sensors to track patient health | Body area network: patient worn sensors | Potential epidemics: rural areas | Pulse rate and body temperature |
These sensors are connected to a control unit, calculates the values of the sensors. These values are then transmitted through a IoT cloud to the base station Based on the temperature and heart beat values, the doctor can decide the state of the patient and appropriate measures can be taken |
Rule-based machine learning algorithm | A remote health monitoring system using IoT is proposed where the authorized personal can access these data stored using any IoT platform and based on these values received, the diseases are diagnosed accurately by the doctors from a distance |
| Radin et al. (2020) | USA | Proposing a predefined wearable sensor and evaluating the retrieved data to improve the ability to enact quick outbreak | A Fitbit wearable device | Respiratory infections: such as influenza | Total RHR (resting heart rate) and sleep measures |
According to Fitbit, RHR is calculated as follows: periods of still activity during the day are identified by looking at the accelerometer signal provided by the device If inactivity is observed for a sufficiently long time, then it is assumed that the person is in a resting state, and their heart rate at that time is used to estimate their RHR |
Mathematical model + association rule mining | By accessing these data, it could be possible to improve real-time and geographically refined influenza surveillance. This information could be vital to enact timely outbreak response measures to prevent further transmission of influenza cases effectively |
| De and Mukherjee (2015) | India | Taking proper action for curing the patient based on the health parameters’ values | Body area sensor network: patient worn sensors | Infectious diseases | Blood pressure, blood sugar level, respiration rate, body temperature, ECG |
In this system health data of a user is captured by body sensor network and then sent to the user’s mobile device which is registered under a femtocell Using a database maintained at femtocell, captured health data are verified and if abnormality is detected, the data are sent to the cloud through the femtocell for storage |
Markov chain model + Laplace estimation + Bayesian approach | Analyzing the health status of a number of patients affected by an infectious disease in a particular region, epidemic trends can be detected and then to aware people alert messages are sent over social networking sites |
| Edoh (2018) | Germany | To protect the population against emerging infectious diseases, request permanent crowd surveillance., particularly in high-risk regions | Optical sensor (fiber-optic sensors) | Ebola and infectious disease | Body temperature | The sense bio-signals using optical sensors of individuals within (ad-hoc) crowd with the objectives to monitor risks of emerging infectious diseases | Pedestrian detection method as a machine learning method to detect pedestrians | According to the results of the conducted experiment, the concept has the potential to improve the conventional epidemiological data collection. The measurement is reliable, and the recorded data are valid. The measurement error rates are about 8% |
| Sareen et al. (2018) | Guinea, Liberia and Sierra Leone | Proposing a model for remote monitoring of infected patients in real time using cloud computing | RFID | Ebola | Body temperature, blood pressure |
Through RFID attached to the user’s body, the vital signs are captured through WBAN and is transmitted to the mobile phone via Bluetooth, from where the data is forwarded to the cloud server using WiFi 3G/4G in real time At the same time, users can enter their secondary and advanced symptoms through the interface provided by the mobile application |
Cloud computing + decision tree-based algorithm (J48 decision tree) + SEIHR model | The vital body symptoms and social interactions are captured using WBAN and RFID respectively. The proposed model provided 94% accuracy for the classification and 92% of the resource utilization |
| Steinhubl et al. (2016) | Sierra Leone | Proposing a sensors based system for creating automated alerting of early changes in patient status | Wearable sensor | Ebola | Heart rate, heart rate variability, activity, respiratory rate, pulse transit time, uncalibrated skin temperature and posture |
The researcher developed a modular wireless patient monitoring system (MWPMS) and conducted a proof of concept study in an Ebola treatment centre (ETC) The system was built around a wireless, multiparametric ‘band-aid’ patch sensor for continuous vital sign |
Machine learning technology known as similarity-based modelling (SBM) | It can provide high-acuity monitoring with a continuous, objective measure of physiological status of all patients that is achievable in virtually any healthcare setting, anywhere in the world |
| Sood and Mahajan (2017) | India | Proposing fog based health monitoring system for real time monitoring and analysis of user’s health statistics and related events such as health data | Wearable IoT sensor | Chikungunya | Body temp, joint pain, headache, body pain, red eyes, rashes on the body, nausea, muscle pain and vomiting |
Wearable IoT sensor layer collects data in real-time from various health sensors, location sensors, drug sensors, environmental sensors and meteorological sensors The acquired data is transmitted to the fog layer for real time processing and diagnosing possibly infected users from CHV. After diagnosing the CHV, fog layer immediately generates alerts to the user’s mobile |
Fog computing | On the basis of health severity, emergency alerts are generated for delivering event information to user’s mobile on time through fog network. It will help uninfected residents to take immediate precautions to prevent the outbreak of these viruses and government healthcare agencies to control the problem effectively |
Fig. 4.
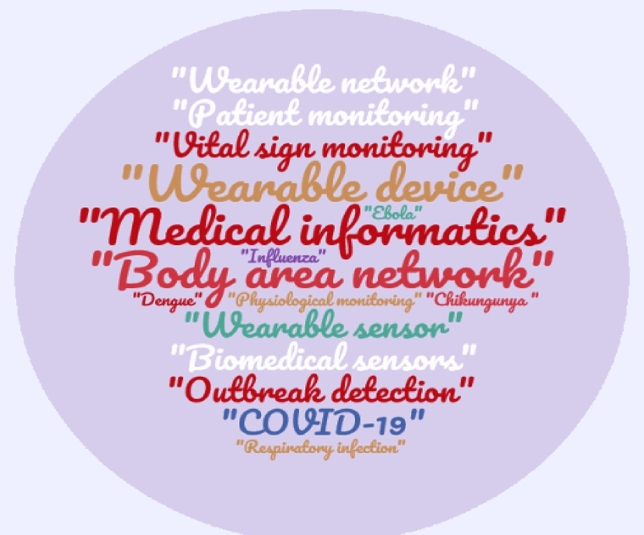
Word cloud of core keywords in included papers
Illustration of papers
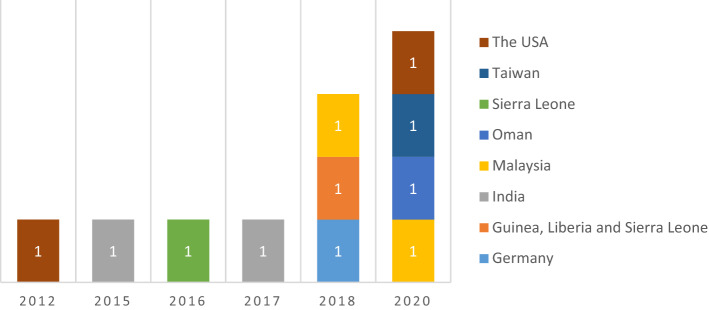
The distribution of papers based on countries and year of publication
The included papers based on their country and year of publication are presented in Fig. 5. As we can see, from 11 included papers, four papers were published in 2020 by different countries and 3 papers were published in 2018. The remained papers were published from 2012 up to 2017.
Fig. 5.
The distribution of articles based on countries and year
The distribution of included articles based on publisher names
The selected papers (n = 11) were retrieved from 10 different journals. The total number of papers for each journal is displayed in Table 3. Two of 11 papers were published by Journal of medical systems. From these 11 included papers, none of them were published by conferences.
Table 3.
Distribution of studies based on their publishers
| Journal name | Count of papers |
|---|---|
| Journal of Medical System | 2 |
| BMJ Global Health | 1 |
| Computers in Industry | 1 |
| International Journal of Grid and Distributed Computing | 1 |
| International Journal of Psychosocial Rehabilitation | 1 |
| Journal of Ambient Intelligent Humanized Computing | 1 |
| Journal of Critical Reviews | 1 |
| Journal of Medical Imaging and Health Informatics | 1 |
| Journal of Microbiology, Immunology, and Infection | 1 |
| The Lancet Digital Health | 1 |
| Grand total | 11 |
The distribution of monitored vital signs based on the wearable sensors
The types of detected physiological vital signs based on the different wearable sensors is displayed in Table 4. As it is clear, wearable devices like a cuff or watch and wearable body area network sensors are popular for patient monitoring in epidemics controlling. However, the critical vital signs for patient monitoring in the mentioned condition is body temperature, heart rate and blood pressure. Table 3 is presented the details of this analysis.
Table 4.
The distribution of monitored vital signs based on the wearable sensors
| Vital signs | BAN | RFID | Optical sensor | Wearable device | Wearable IoT sensor |
|---|---|---|---|---|---|
| Body temperature | *** | * | * | *** | * |
| Hear rate | *** | *** | |||
| Blood pressure | ** | * | |||
| Facial-recognition | * | ||||
| resting heart rate | * | ||||
| Blood sugar level | * | ||||
| Respiration rate | * | * | |||
| Myalgia | * | ||||
| Red eyes | * | ||||
| Rash | * | ||||
| Neusea | * |
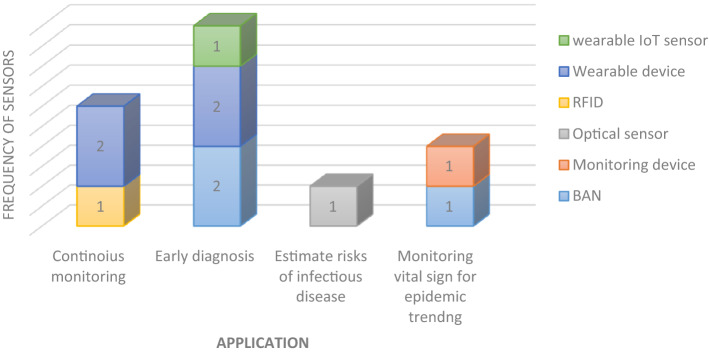
The distribution of papers based on their main application and type of sensors
In Fig. 6, as we can see wearable devices (like a helment, watch or cuff) are used for continuous monitoring and early detection. In addition, body area network sensors are a popular type which can used monitoring vital signs for epidemic trending. The details of each category are presented in mentioned figure.
Fig. 6.
The distribution of papers based on their main application and type of sensors
The distribution of papers based on countries
The reviewed papers based on their counties is presented in Fig. 7. As it is clear, approximately 65% total papers (n = 6) were conducted by the USA, Malaysia and India. The other countries have relatively equal number of published articles.
Fig. 7.
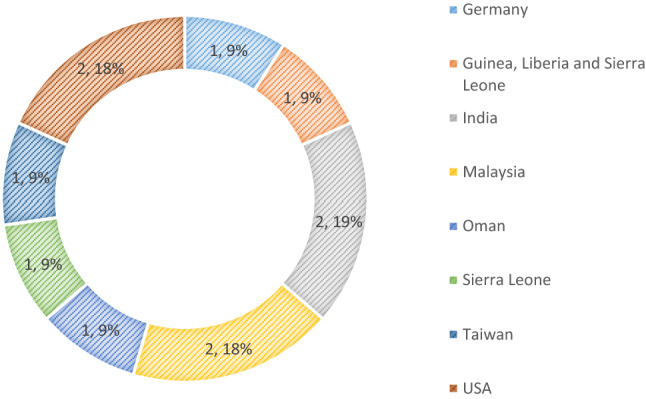
The distribution of articles based on their conducted countries
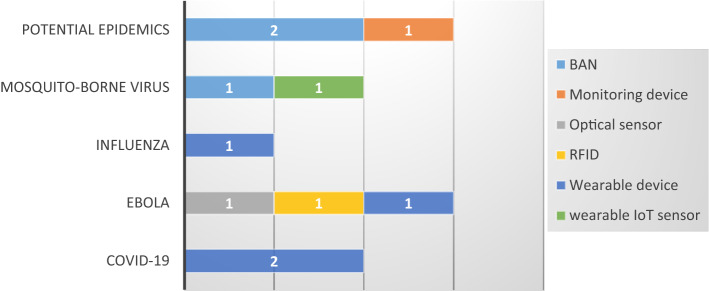
The distribution of papers based on their disease and types of sensors
As we can see in drawn figure, wearable devices are appropriate technologies for patients with COVID-19. For Ebola epidemic RFID, wearable devices and optical sensors were used too. However, in Fig. 8 for each disease we can see applied different types of wearable sensors in detail respectively.
Fig. 8.
The distribution of papers based on their disease and types of sensors
The distribution of papers based on applied intelligent algorithms or AI oriented approaches
In this section, we described the intelligent techniques and approaches used in the reviewed papers. Out of 11 citations, in 9 papers the applied AI oriented approaches were reported; most sensors designed to monitor patients in epidemic conditions (in reviewed papers) use intelligent methods to generate knowledge and information. But in 2 reviewed papers, intelligent algorithms were not applied or not reported in text. However, based on citations the smart developed sensors in addition to being able to record the vital signs of individuals, can analyze and learn using artificial intelligence algorithms. Consequently, according to the reviewed articles, sensors will be able to raise the ability obtaining massive amounts of information or big data and enhance precision and accuracy. These sensors or mini devices also reflect the developmental tendency of modern sensors. Moreover, artificial intelligence is a novel stimulus for smart sensors, which gets sensors to think and learn and feed more efficient results back. Some of the applied algorithms by sensors or devices in papers are mathematical methods, rule-based algorithm, Bayesian approach, J48 decision tree and so on.
Discussion
According to our results, emerging wearable technologies have potential and capacity to control patients physiological vital signs in epidemic outbreaks. Wearable sensors are appropriate technologies that make easier continuous monitoring and control of the patients conditions for healthcare provider like physicians, nurses and specialists. The main objective of this review was identifying and analyzing the studies which conducted on the applying wearable sensors in epidemics outbreaks for patient monitoring.
According to studies, smart wearable sensors are designed to monitor patients in a variety of epidemics, such as Ebola, COVID-19 and Influenza. Contrary to researchers ‘expectations, a small number of studies looked at the designing of wearable sensors to monitor vital signs such as body temperature, heart rate, blood pressure and a number of other studies to monitor patients’ condition in the epidemics (Breteler et al. 2020). Anyway, Given that these tools can reduce the presence of patients outside the home due to the possibility of patient care at home and reduce patient traffic to the hospital and thus reduce interactions between people and also have great potential to identify, these tools are expected to be widely used in this area (Mohammed et al. 2020). Given the high cost of manufacturing and networking sensors, it can be argued that one of the main reasons for the low number of studies in this field is to provide funding for the construction of sensors and body networks (Dias and Paulo Silva Cunha 2018; Steinhubl et al. 2016).
Studies included in this review indicated that among communicable diseases, sensors were most applicable in infectious diseases. Such sensors could be applied for early diagnosis and continuous monitoring (Dias and Paulo Silva Cunha 2018). It is due to sensors have the potential to monitor and record vital signs of patients continuously and analyzed them. The most commonly used sensors in our study are wearable devices and BAN sensors. However, the evidence concerning the effectiveness of different types of smart sensors to control epidemic disease was almost inadequate.
As we expected, the majority of these devices recorded and monitored body temperature and heart rate as the most frequent vital signs for early detection and early response to stop the spread of communicable diseases (Chung et al. 2020; Edoh 2018; Mohammed et al. 2020; Radin et al. 2020; Sood and Mahajan 2017; Valsalan et al. 2019). In these type of smart devices, real-time data sent to healthcare providers simultaneously to track patients (Al-Janabi et al. 2017). Besides, with the new pandemic of COVID-19, researchers used wearable sensors for early detection of infected patients. In reviewed articles, two kinds of sensors were introduced (Chung et al. 2020; Mohammed et al. 2020). Researches applied wearable sensors to detect vital signs of patients, especially body temperature and respiratory rate. Consistent and accurate recording of vital signs in patients who suffered from COVID-19 is essential due to drastic changes in patients’ signs and symptoms (Wang et al. 2020). The application of such sensors empowered clinicians for early diagnosis of new coronavirus to decrease its mortality. According to the positive outcomes of using sensors in similar pandemic diseases such as Ebola, it seems that using wearable sensors could be beneficial in patients who are hospitalized at home for remote vital sign monitoring to pass undesired changes to their physicians immediately.
The critical vital signs for patient monitoring in the epidemic disease in this review were body temperature, heart rate and blood pressure. Dias and Paulo Silva Cunha conducted a study of vital signs that are necessary for monitoring and concluded that heart rate, blood pressure, respiratory rate, blood oxygen saturation and body temperature are valuable vital signs (Dias and Paulo Silva Cunha 2018). These vital signs are essential for assessing a person’s health status and can be used to identify clinical deterioration. In patients with COVID-19, fever is one of the most common symptoms in these patients (Tabata et al. 2020). Fever is one of the common clinical symptoms that appear when infectious diseases occur. It can be very helpful in diagnosing infectious diseases (Plaza et al. 2016). Heart rate is a standard vital sign that its monitoring can provide information about the body’s physiological state (Plaza et al. 2016). Blood pressure monitoring is one of the most important indicators in determining a person’s cardiovascular status (Dalvi et al. 2020). Wearable sensors can be used to monitor these vital signs and help determine the health status of patients and thus can be effective in diagnosing diseases, especially in measuring body temperature in infectious diseases and they can be very helpful to patients and health care providers.
The study had several strengths, including searches on various databases; Web of Science, Scopus, IEEE Library, PubMed, and Google Scholar. We also did not impose any time constraints on the article search process, and the articles presented at the conferences were also reviewed. The limitation of this study was to exclude non-English language studies.
Conclusion
This systematic review highlights the usage of different types of sensors to improve epidemic disease control. By applying a systematic approach, the authors provide a wide overview to use sensors that could monitor vital signs and disease progression through the epidemic. The survey showed that wearable sensors had the greatest potential in controlling and diagnosing the early signs of the disease in relation to epidemic diseases. Hence, applying appropriate technological solutions could improve control and management epidemic disease as well as the application of sensors for continuous monitoring vital signs. However, further studies are needed to investigate the real effects of these sensors and their effectiveness.
Funding
In this paper, we didn’t have any financial sponsor.
Availability of data and material
All data generated or analyzed during this study are included in this published article.
Compliance with ethical standards
Conflict of interest
The authors declare that there is no conflict of interest regarding the publication of this article.
Ethical approval
This article does not contain any studies with human participants performed by any of the authors.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Al-Janabi S, Al-Shourbaji I, Shojafar M, Shamshirband S. Survey of main challenges (security and privacy) in wireless body area networks for healthcare applications. Egypt Inform J. 2017;18:113–122. doi: 10.1016/j.eij.2016.11.001. [DOI] [Google Scholar]
- Baskar S, Shakeel PM, Kumar R, Burhanuddin MA, Sampath R. A dynamic and interoperable communication framework for controlling the operations of wearable sensors in smart healthcare. Appl Comput Commun. 2020;149:17–26. doi: 10.1016/j.comcom.2019.10.004. [DOI] [Google Scholar]
- Breteler MJM, et al. Vital signs monitoring with wearable sensors in high-risk surgical patients a clinical validation study anesthesiology. J Am Soc Anesthesiol. 2020;132:424–439. doi: 10.1097/ALN.0000000000003029. [DOI] [PubMed] [Google Scholar]
- Chung Y-T, et al. Continuous temperature monitoring by a wearable device for early detection of febrile events in the SARS-CoV-2 outbreak in Taiwan, 2020. J Microbiol Immunol Infect. 2020;53:503. doi: 10.1016/j.jmii.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahiya AS, et al. Energy autonomous wearable sensors for smart healthcare: a review. J Electrochem Soc. 2019;167:037516. doi: 10.1149/2.0162003JES. [DOI] [Google Scholar]
- Dalvi C, Lamego MM, Kiani MJE, Poeze J, Vo H (2020) Blood pressure monitor with valve-chamber assembly. Google Patents
- De D, Mukherjee A. Femto-cloud based secure and economic distributed diagnosis and home health care system. J Med Imaging Health Inform. 2015;5:435–447. doi: 10.1166/jmihi.2015.1437. [DOI] [Google Scholar]
- Dias D, Paulo Silva Cunha J. Wearable health devices—vital sign monitoring, systems and technologies. Sensors. 2018;18:2414. doi: 10.3390/s18082414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edoh T. Risk prevention of spreading emerging infectious diseases using a hybrid crowd sensing paradigm, optical sensors, and smartphone. J Med Syst. 2018;42:91. doi: 10.1007/s10916-018-0937-2. [DOI] [PubMed] [Google Scholar]
- Edoh TO (2019) Internet-of-things-enabled pre-screening for diseases: a novel approach for improving the conventional methodology and paradigm for screening for non-communicable diseases. In: Pre-screening systems for early disease prediction, detection, and prevention. IGI Global, pp 1–49
- Gries A, Seekamp A, Wrede C, Dodt C. Zusatz-Weiterbildung Klinische Akut-und. Notfallmedizin Deutschland Der Anaesth. 2018;67:895–900. doi: 10.1007/s00101-018-0515-5. [DOI] [PubMed] [Google Scholar]
- Ha M, Lim S, Ko H. Wearable and flexible sensors for user-interactive health-monitoring devices. J Mater Chem B. 2018;6:4043–4064. doi: 10.1039/C8TB01063C. [DOI] [PubMed] [Google Scholar]
- Hassan NH, Salwana E, Drus SM, Maarop N, Samy GN, Ahmad NA. Proposed conceptual IoT-based patient monitoring sensor for predicting and controlling dengue. Int J Grid Distrib Comput. 2018;11:127–134. doi: 10.14257/ijgdc.2018.11.4.11. [DOI] [Google Scholar]
- Kristoffersson A, Lindén M. A systematic review on the use of wearable body sensors for health monitoring: a qualitative synthesis. Sensors. 2020;20:1502. doi: 10.3390/s20051502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J, Ma Q, Chan AHS, Man SS. Health monitoring through wearable technologies for older adults: smart wearables acceptance model. Appl Ergon. 2019;75:162–169. doi: 10.1016/j.apergo.2018.10.006. [DOI] [PubMed] [Google Scholar]
- Lin W-Y, Ke H-L, Chou W-C, Chang P-C, Tsai T-H, Lee M-Y. Realization and technology acceptance test of a wearable cardiac health monitoring and early warning system with multi-channel MCGs and ECG. Sensors. 2018;18:3538. doi: 10.3390/s18103538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorence D, Wu J. Computerized disease profiling using GPS-linked multi-function sensor cartridges. J Med Syst. 2012;36:2537–2545. doi: 10.1007/s10916-011-9726-x. [DOI] [PubMed] [Google Scholar]
- Majumder S, Deen MJ. Smartphone sensors for health monitoring diagnosis. Sensors. 2019;19:2164. doi: 10.3390/s19092164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Majumder S, Mondal T, Deen MJ. Wearable sensors for remote health monitoring. Sensors. 2017;17:130. doi: 10.3390/s17010130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohammed MN, Syamsudin H, Al-Zubaidi S, Aks RR, Yusuf E. Novel COVID-19 detection and diagnosis system using IOT based smart helmet. Int J Psychosoc Rehabil. 2020;24:7. [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009 doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nag A, Mukhopadhyay SC, Kosel J. Conclusion, challenges and future work printed flexible sensors. Cham: Springer; 2019. pp. 193–198. [Google Scholar]
- Plaza JJG, Hulak N, Zhumadilov Z, Akilzhanova A. Fever as an important resource for infectious diseases research. Intract Rare Dis Res. 2016;5:97–102. doi: 10.5582/irdr.2016.01009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radin JM, Wineinger NE, Topol EJ, Steinhubl SR. Harnessing wearable device data to improve state-level real-time surveillance of influenza-like illness in the USA: a population-based study. Lancet Digit Health. 2020;2(2):e85–e93. doi: 10.1016/S2589-7500(19)30222-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman MS, Peeri NC, Shrestha N, Zaki R, Haque U, Ab Hamid SHA. Defending against the novel Coronavirus (COVID-19) outbreak: how can the Internet of Things (IoT) help to save the world? Health Policy Technol. 2020;9:136–138. doi: 10.1016/j.hlpt.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajan K, Garofalo E, Chiolerio A. Wearable intrinsically soft, stretchable, flexible devices for memories and computing. Sensors (Basel, Switzerland) 2018 doi: 10.3390/s18020367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rezayi S, Safaei AA, Mohammadzadeh N. Requirement specification and modeling a wearable smart blanket system for monitoring patients in ambulance. J Med Signals Sens. 2019;9:234. doi: 10.4103/jmss.JMSS_55_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richesson RL, Andrews JE, Hollis KF. Introduction to clinical research informatics. In Clinical research informatics. Cham: Springer; 2019. pp. 3–15. [Google Scholar]
- Sareen S, Sood SK, Gupta SK. IoT-based cloud framework to control Ebola virus outbreak. J Ambient Intell Humaniz Comput. 2018;9:459–476. doi: 10.1007/s12652-016-0427-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sood SK, Mahajan I. Wearable IoT sensor based healthcare system for identifying and controlling chikungunya virus. Comput Ind. 2017;91:33–44. doi: 10.1016/j.compind.2017.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinhubl SR, Feye D, Levine AC, Conkright C, Wegerich SW, Conkright G. Validation of a portable, deployable system for continuous vital sign monitoring using a multiparametric wearable sensor and personalised analytics in an Ebola treatment centre. BMJ Glob Health. 2016;1:e000070. doi: 10.1136/bmjgh-2016-000070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabata S et al (2020) The clinical characteristics of COVID-19: a retrospective analysis of 104 patients from the outbreak on board the Diamond Princess cruise ship in Japan. medRxiv:2020.2003.2018.20038125. 10.1101/2020.03.18.20038125
- Valsalan P, Baomar TAB, Baabood AHO. IOT based health monitoring system. J Crit Rev. 2019;7:2020. [Google Scholar]
- Wang S, Zhou X, Zhang T, Wang Z. The need for urogenital tract monitoring in COVID-19. Nat Rev Urol. 2020;17:314–315. doi: 10.1038/s41585-020-0319-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu G, et al. Learning from large-scale wearable device data for predicting epidemics trend of COVID-19. Discrete Dyn Nat Soc. 2020;2020:6152041. doi: 10.1155/2020/6152041. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.