Abstract
Backgound
Santiago, Chile underwent two separate periods of crisis over the past year. The first period, the ‘social crisis,’ extended over thirteen weeks in late 2019 into early 2020 due to protests over income inequality and the government response to social unrest. The second period, the ‘health crisis,’ began in March 2020 with Chile’s first case of COVID-19 and escalated rapidly to include ‘stay at home orders,’ traffic restrictions, and the shuttering of most businesses. We wished to evaluate the impact of these crisis periods on trauma epidemiology.
Methods
We performed a retrospective review of the South-East Metropolitan Health Service Trauma Registry. Trauma admissions, operative volume, and in-hospital mortality were evaluated during the crisis period and the year prior.
Results
The social crisis saw increased levels of trauma, both blunt and penetrating, relative to the time period immediately preceding. The health crisis saw an increase in penetrating trauma with a concomitant decline in blunt trauma. Both crisis periods had decreased levels of trauma, overall, compared to the year prior. There were no statistically significant differences in in-hospital trauma mortality.
Conclusion
Different crises may have different patterns of trauma. Crisis periods that include extended periods of lockdown and curfew may lead to increasing penetrating trauma volume. Governments and health officials should anticipate the aggregate impact of these measures on public health and develop strategies to actively mitigate them.
Level of evidence
III
Introduction
Santiago, Chile underwent two separate periods of crisis over the past year. The first period, the ‘social crisis,’ started in mid-October 2019 and extended for thirteen weeks through early January 2020. It started with mass street protests for income inequality, and was characterized by vandalization, rioting, and violent clashes between police and protesters. The weeks following were characterized by nighttime curfews, traffic restrictions, and military patrols. The second period, the ‘health crisis,’ began in early March with Chile’s first case of the COVID-19 pandemic. Within weeks, a new curfew was initiated with ‘stay at home orders’ for commuters, traffic restrictions, the shuttering of most businesses except for ‘essential’ services for most of Santiago’s residents.
A lockdown is a political or public health measure imposed in crisis situations to control riots or reduce the spread of infectious disease. Multiple reports have shown decreased overall visits to the hospital during crisis periods, but its impact on trauma epidemiology is less well understood [1]. Some early studies report fewer injury-related admissions with significant reductions seen in major traumatic injuries while others report an increase in violence, especially gunshot injuries [2, 3].
Sotero Del Rio is a 900-bed hospital located in the heart of south-east Santiago, an area with a population of 1.7 million, sixty times the rate of poverty, and less than 1/8th the health spending per capita than other parts of the city. Sotero Del Rio also houses the South-East Metropolitan Health Service Trauma Registry (SEMHSTR), which was established in 2017 through a combination of public and private funding and collects prospective information on trauma patients at two public trauma hospitals serving the south-east Santiago [4]. We sought to understand the impact of curfews from two national crises, the “social crisis” and the “health crisis,” on trauma epidemiology through the SEMHSTR.
Methods
Study design and setting
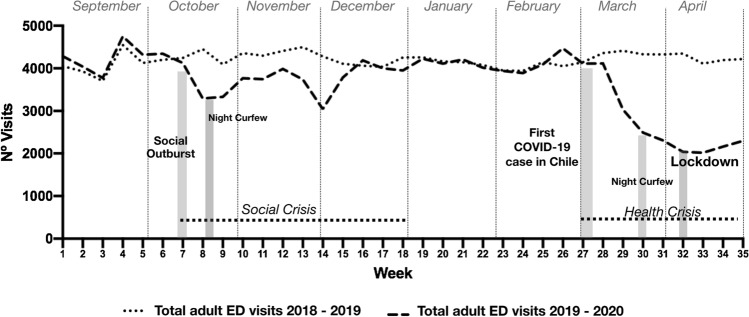
We performed a retrospective review of the South-East Metropolitan Health Service Trauma Registry (SEMHSTR), extracting data for 35 weeks between September 1, 2019 and May 1, 2020. We defined the time period for the ‘social crisis’ as beginning on October 14, 2019 and continuing in varied intensity for the next 13 weeks, though a nightly curfew was in place for most of that time. We defined the time period for the ‘health crisis’ as beginning with the first confirmed case of COVID-19 on March 3, 2020. Official social distancing recommendations began on this day, though formal ‘stay-at-home’ orders and more restrictive measures, including curfews, were not initiated until additional cases were registered several weeks later. We confirmed the length of these crisis periods by evaluating total medical, surgical, and trauma visits to the adult emergency department through a separate internal hospital registry. These visits declined sharply during these time periods and returned to baseline in the intervening period between the two crises, compared to the year prior (Fig. 1), thus providing further confirmation of the ‘crisis’ periods of interest.
Fig. 1.
Number of weekly visits in the emergency department in the period 2018–2019 (baseline period) and in 2019–2020 (crisis period)
Participants
Patients older than 15 years and admitted to the hospital with a traumatic injury were included in the SEMHSTR registry. Traumatic injuries were defined as penetrating, blunt, and burn injuries of any part of the body including the brain and extremities proximal to the wrist. Injuries to the hand were only included if ligaments, bone, and vascular systems were affected.
Variables and dataset
We extracted data from the SEMHSTR registry on hospital admissions for penetrating and blunt trauma, the number of patients who underwent a trauma operations, and the number of patients who died each week from September 1, 2019 to May 1, 2020, encompassing both crisis periods. We also extracted this information from the registry from September 1, 2018 to May 1, 2019 to serve as a baseline. This study was approved by the ethics committee of the South-East Metropolitan Health Services.
Data analysis
We performed a descriptive analysis presenting categorical variables as proportions and continuous variables as means with standard deviations. A student’s t-test was performed comparing means of continuous variables, and we used a two-tailed p-value of less than 0.05 to classify as statistically significant. We used R Studio 1.2 (www.rstudio.com) for statistical analysis.
Results
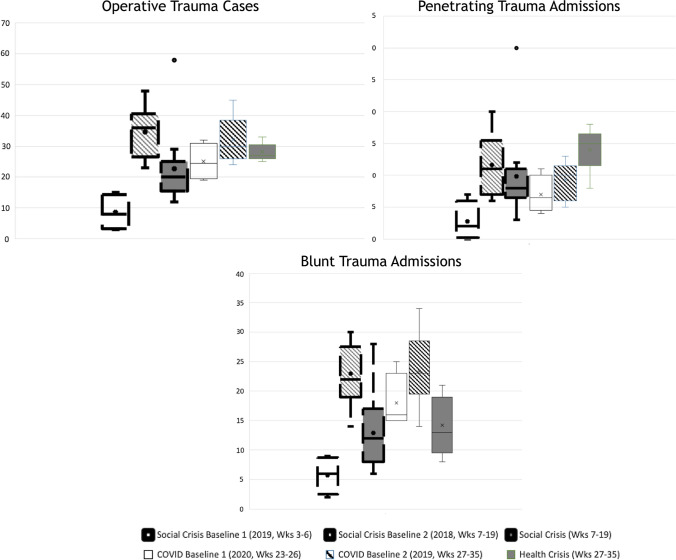
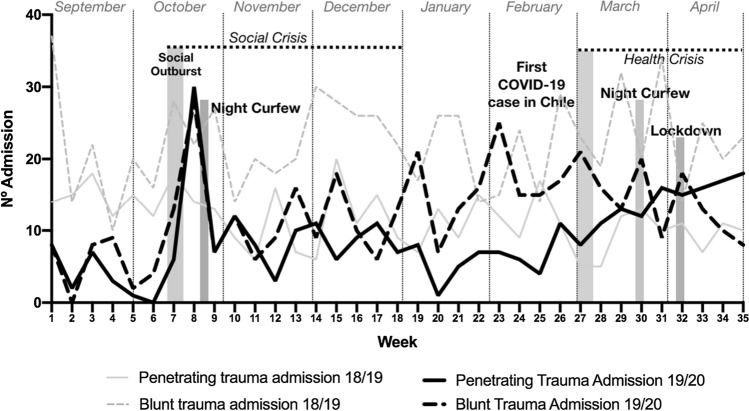
There were a total of 14614 emergency department visits for surgical complaints from September 1, 2019 to May 1, 2020, averaging 3783 visits per week during the social crisis and 2729 visits per week during the health crisis. In comparison, there was an average of 4257 visits per week and 4721 visits per week in the same time periods in 2018 and 2019, respectively (Fig. 1). Averages for blunt and penetrating trauma, operative trauma, and trauma deaths during these crisis periods are summarized in Table 1. We observed a sharp increase in trauma admissions, including both penetrating and blunt trauma, at the onset of the social crisis that remained higher, on average, than during the immediate weeks preceding the social crisis (Table 1, Fig. 2). However, we do not see differences between the periods analyzed with respect to age, ISS or type of transfer to the hospital center or damage control surgery requirements. In contrast, there was a progressive increase in cases of penetrating trauma along with a decrease in blunt trauma as weeks of health crisis continued. In the later weeks of the health crisis, penetrating trauma was more common than blunt trauma. (Fig. 3). Penetrating trauma volume, blunt trauma volume, and overall trauma volume were depressed during the social crisis and health crisis relative to their respective baseline periods from the previous year with the exception of penetrating trauma, which was higher during the health crisis compared to its previous year’s baseline.
Table 1.
Comparison of both crisis (Social and COVID) with the baseline period 2018–2019
| Social crisis (weeks 7-19) mean (SD) | Baseline (weeks 7-19) mean (SD) | P valuea | COVID crisis (weeks 27-35) mean (SD) | Baseline (weeks 27-35) mean (SD) | P valuea | |
|---|---|---|---|---|---|---|
| Total ED visits | 3783 (363.4) | 4257 (149.0) | < 0.001 | 2729 (841.6) | 4271 (105.7) | < 0.001 |
| Blunt Trauma admissions | 12.9 (6.4) | 22.9 (4.7) | < 0.001 | 14.2 (4.8) | 23.3 (6.3) | 0.004 |
| Penetrating Trauma admissions | 9.8 (6.5) | 11.6 (4.7) | 0.43 | 14.0 (3.2) | 9.3 (3.0) | 0.006 |
| Ageb | 32 (3.5) | 31 (3.8) | 0.31 | 32 (4.1) | 32 (3.9) | 0.33 |
| ISSb | 13 (2,1) | 14 (3.1) | 0.25 | 14 (2.9) | 14 (3.3) | 0.37 |
| Prehospital careb | 5,1 (3.5) | 5.7 (4.0) | 0.21 | 6.1 (3.8) | 5.2 (3.5) | 0.14 |
| Operative Trauma cases | 8.9 (3.5) | 18.6 (3.0) | < 0.001 | 11.3 (3.3) | 19.4 (3.2) | < 0.001 |
| Damage control surgery | 2.9 (4.5) | 3.0 (3.5) | 0.56 | 2.6 (3.8) | 2.2 (3.1) | 0.45 |
| Trauma deaths | .89 (.55) | .76 (.72) | 0.76 | 1.1 (1.9) | .89 (.92) | 0.76 |
| Trauma mortality rate (Trauma deaths/Trauma cases) | .043 (.033) | .026 (.018) | .11 | .036(.058) | .041(.077) | .90 |
SD Standard deviation, ISS Injury severity score
aT-Test was adjusted to assess the differences between the two time periods, both the baseline (2018–2019) and the crisis period (2019–2020). Significance level at 0.05.
bVariable referring to hospitalized patients
Fig. 2.
Box-and-whisker plots of operative trauma case, blunt trauma admissions, and penetrating trauma admissions during the social and health crises (solid, dark boxes) with the baseline time period of the year prior (striped boxes) and the weeks immediately preceding the crises (white box) as comparison
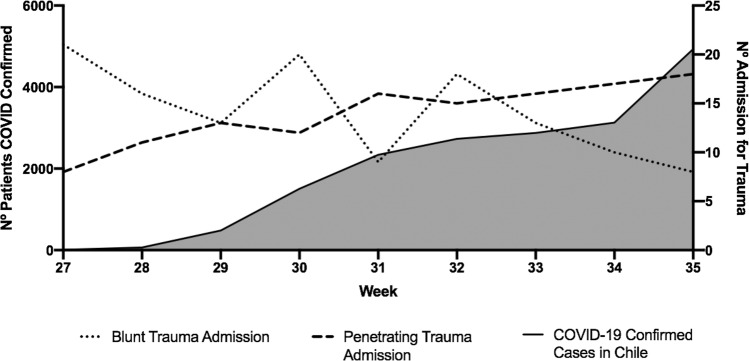
Fig. 3.
Number of weekly admissions for penetrating and blunt trauma during the period of health and social crisis
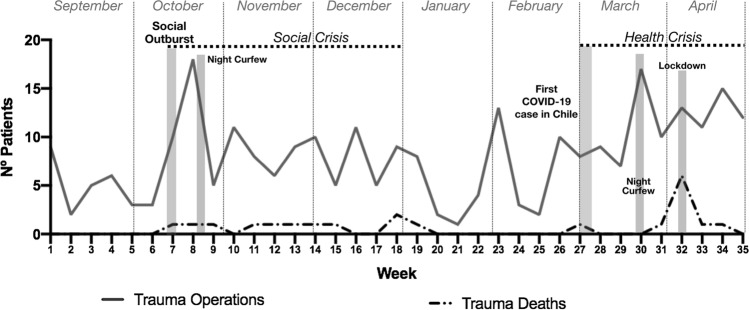
We found that operative trauma volume remained higher in both crisis periods compared to the weeks immediately preceding them, but they were both substantially lower than the year prior (Fig. 4). There were slight increases in the number of deaths amongst admitted trauma patients during both the social crisis and the health crisis relative to the year prior, but these differences were not statistically significant.
Fig. 4.
Number of weekly patients requiring surgery due to traumatic event and number of patients dying from trauma during crises
Discussion
Two crises events in Santiago over a single year presented a unique opportunity to explore the impact of social lockdowns on trauma epidemiology. Crisis periods were associated with depressed emergency department visits, and that while there were spikes in trauma volume during both crises, overall it was much lower than the previous year’s baseline. Strikingly, penetrating trauma increased relative to blunt trauma during the health crisis but not during the social crisis. Interestingly, we found that the severity of the patients, when observing the ISS and damage control surgery requirements, is not affected between the periods. We believe that this is determined by the great interpersonal violence that exists in the urban area analyzed.
The spike in trauma volume at the onset of the social crisis can be explained by rioting and violent clashes between police and protesters. Soon thereafter, confinement measures began with a night curfew, replete with military patrols and traffic restrictions, and these measures seemed to reduce the number of individuals who visited emergency departments or were brought in as victims of trauma. As the health crisis began, another “lockdown” was initiated. This included shuttering of most nonessential businesses in addition to curfews and traffic restrictions and mandates for social distancing. Consequently, ED visits declined even further than during the social crisis, as did overall trauma volume relative to the year prior. This suggests that that the combination of restrictive measures imposed by the government with many individuals’ desire to avoid hospitals in the setting of COVID contributed in reduced access of hospital facilities for emergency visits and trauma. These findings align well with recent literature during the global COVID pandemic showing that patients suffering from a wide variety of ailments, from acute coronary syndromes to strokes, are arriving to the hospital in less frequency during COVID lockdowns [1, 5].
Interestingly, we found penetrating trauma volume increased during the health crisis and there were (Fig. 5), more penetrating injuries during the health crisis than the year prior. Simultaneously, blunt traumatic injuries decreased during this time period (and compared to the year prior). Other studies have shown that curfew measures, such as the stay-at-home orders and traffic restrictions imposed during the health crisis in Santiago, increase rates of interpersonal violence including domestic violence [6]. Further, the risk of death increases five times when there is a weapon at home [7]. Southeastern Santiago is the location of the city’s most violent trauma and is known for high levels of gang violence. This finding suggests, that communities that have a high underlying level of interpersonal violence may be predisposed to increased penetrating trauma with curfews.
Fig. 5.
Number of confirmed COVID-19 patients in the country during week 27 and week 35. Number of admissions for both penetrating and blunt trauma during the health crisis due to COVID-19
Recent literature from Philadelphia also shows increasing gun violence [8] in the setting of overall fewer trauma admissions during the COVID crisis. Similarly, trauma data from New Orleans shows steady penetrating volume in the setting of reduced blunt volume [3].
Notably, divergent trends with increasing penetrating injuries and decreasing blunt trauma was not observed during the curfew period of the social crisis. While there was a slight uptick of penetrating trauma cases at the later stages of the social crisis, blunt trauma also increased. This may be explained by the social crisis curfew being initially very restrictive but progressing to a night-time curfew only where businesses were open, and most individuals were not restricted from leaving to work. The burden of traffic collisions and occupational injuries increased as restrictive measures decreased. Future research will be needed to further explore this relationship.
Our data were limited in that our registry did not distinguish between violence-related and violence unrelated traumatic injury. We used penetrating trauma as a proxy for violence-related trauma given data completeness in the registry, though we recognize that not all penetrating trauma is the product of violence nor is all blunt trauma nonviolent. Further, because our registry did not include trauma visits that did not result in admission, our data only speak to the most severe of trauma seen during the crisis periods.
In summary, this study suggests that confinement measures such as curfews and lockdowns to deal with crisis situations effectively decrease emergency hospital visits and trauma volume. Penetrating trauma may increase in the setting of prolonged, restrictive confinement measures in communities with high preexisting levels of firearm possession and baseline violence. Blunt trauma likely decreases with the reduction of road traffic collisions, fewer occupational accidents, and possible difficulty accessing health facilities. In the future, governments considering a confinement measure to deal with a crisis should consider the impact on community health to reallocate resources and design strategies to mitigate interpersonal violence [9]. Reducing trauma burden during these crisis periods is particularly important because of limited hospital resources, availability of critical care unit beds, blood products, personal protective equipment and healthcare staff.
Dr. Juan Pablo Ramos Perkis
was born and raised in Santiago, Chile. He completed his surgical residency at the Dr. Sótero del Río Hospital, where he then joined the faculty as an Assistant Professor. His clinical interest is in Trauma and acute care surgery, with an emphasis on the development of trauma systems. Dr. Ramos is one of the founders of the trauma and emergency unit at the Dr. Sótero del Río Hospi-tal and creator of the first trauma registry in his country. In his spare time, he stands out as a mountaineer in the American Andes.
Authors contribution
JPR: Study conception, literature search and writing. PAT: Study conception, data interpretation and writing. NR: Study conception, literature search and writing. AZA: data interpretation and writing. POL: Study conception and critical revision. CMA: data collection and a data analysis. JCP: Study conception and critical revision.
Funding
None from NIH/Wellcome trust/HHM.
Compliance with ethical standards
Conflict of interest
All authors declare no conflict of interest in the preparation of or writing of this manuscript.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Juan Pablo Ramos Perkis, Email: jramos.med@gmail.com.
Pablo Achurra Tirado, Email: achurrapablo@gmail.com.
Nakul Raykar, Email: raykarnp@upmc.edu.
Analía Zinco Acosta, Email: analia.zinco5@gmail.com.
Carolina Muñoz Alarcon, Email: caritomunozalarcon@gmail.com.
Juan Carlos Puyana, Email: puyajc@upmc.edu.
Pablo Ottolino Lavarte, Email: ottolinopablo@gmail.com.
References
- 1.O. De Filippo, F. D'Ascenzo, F. Angelini, et al. 2020 Reduced rate of hospital admissions for ACS during Covid-19 outbreak in northern Italy.N Engl J Med. Epub ahead of print, NEJMc2009166 [DOI] [PMC free article] [PubMed]
- 2.Christey G, Amey J, Campbell A, Smith A. Variation in volumes and characteristics of trauma patients admitted to a level one trauma centre during national level 4 lockdown for COVID-19 in New Zealand. N Z Med J. 2020;133(1513):81–88. [PubMed] [Google Scholar]
- 3.Ninokawa S, Nordham K, Tatum D, Duchesne J 2020 Effects of social distancing on the incidence of traumatic injuries. PAJT. Open Access. https://www.panamtrauma.net/resources/Resources/PAJT%202020%20perspectives%202.pdf
- 4.Ramos Perkis J, Ottolino Lavarte P, Muñoz Alarcón C, Ruiz Cabrera J, Arenas Ponce C, Salazar Moreira F, Calderón Ramirez L, Achurra Tirado P, Diaz Fernadez A (2020) Primer registro de trauma en Chile. Análisis de 2 años en un hospital público. Rev Cirugia. 73(1). 10.35687/s2452-45492021001703. Accessed 11 Nov 2020
- 5.Kazdin AE. Conceptualizing the challenge of reducing interpersonal violence. Psychol Violence. 2011;1(3):166–187. doi: 10.1037/a0022990. [DOI] [Google Scholar]
- 6.Aljuboori Z, Sieg E. The early effects of social distancing resultant from covid-19 on admission to a level I trauma center. Injury. 2020 Jun 25. doi: 10.1016/j.injury.2020.06.036 [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 7.Campbell JC, Webster D, Koziol-McLain J, et al. Risk factors for femicide in abusive relationships: results from a multisite case control study. Am J Public Health. 2003;93(7):1089–97. doi: 10.2105/AJPH.93.7.1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hatchimonji J, Swendiman R, Seamon M, Nance M. Trauma does not quarantine: violence during the Covid-19 pandemic. Epub: Annals of surgery; 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hyman I, Vahabi M, Bailey A, et al. Taking action on violence through research, policy, and practice. Glob Health Res Policy. 2016 doi: 10.1186/s41256-016-0006-7. [DOI] [PMC free article] [PubMed] [Google Scholar]