Abstract
Objectives
Driving cessation is associated with adverse social and health outcomes including increased mortality risk. Some former drivers resume driving. Do resumed drivers have a different mortality risk compared to former drivers or continued drivers?
Method
We analyzed National Health and Aging Trends Study (2011–2015) data of community-dwelling self-responding ever drivers (n = 6,189) with weighted stratified life tables and discrete time logistic regression models to characterize mortality risk by driving status (continued, resumed, former), adjusting for relevant sociodemographic and health variables.
Results
Overall, 14% (n = 844) of participants died and 52% (n = 3,209) completed Round 5. Former drivers had the highest mortality (25%), followed by resumed (9%) and continued (6%) drivers. Former drivers had 2.4 times the adjusted odds of mortality compared with resumed drivers (adjusted odds ratio [aOR] = 2.41; 95% confidence interval [CI] = 1.51, 3.83), with no difference between continued and resumed drivers (aOR = 1.22; 95% CI = 0.74, 1.99).
Discussion
Those who resumed driving had better survival than those who did not. Practice implications include driver rehabilitation and retraining to safely promote and prolong driving.
Keywords: Driving cessation, Longitudinal cohort, Survival analysis, Transportation
The United States is undergoing a demographic shift as the number and proportion of Americans aged 65 and older grows. This subpopulation is expected to reach 88 million by 2050 (Colby & Ortman, 2015). Shifting demographics have social and economic implications, including health care, public health, and transportation. Driving serves an important function in maintaining mobility and meeting basic needs (Chihuri et al., 2016). Most older adults do not plan for a time when they cannot drive and expect to drive into their 90s (Harmon, Babulal, Vivoda, Zikmund-Fisher, & Carr, 2018; Naumann, West, & Sauber-Schatz, 2014). A 2002 study found that American men aged 70–74 are expected to live past driving cessation by 6–7 years, and women by 10–11 years (Foley, Heimovitz, Guralnik, & Brock, 2002).
Conceptually, change in driving status has been viewed as a progression from unrestricted driving to driving reduction (self-regulation and lifestyle changes), and cessation (Dellinger, Sehgal, Sleet, & Barrett-Conner, 2001; Dickerson et al., 2017; Rudman, Friedland, Chipman, & Sciortino, 2006). Driving reduction includes changes in frequency, distance, time of day, weather conditions, roadways (e.g., unfamiliar roads, intersections), and speed (Forrest, Bunker, Songer, Coben, & Cauley, 1997). Studies of driving behavior have typically classified individuals by degree of self-regulation (Bergen et al., 2017) or as drivers, former drivers (stopped driving completely), and never drivers. Alternatively, studies may dichotomize as driver versus not driver, but such broad categories fail to distinguish the complexities of driving behaviors (Pristavec, 2018). For example, a portion of former drivers resume driving (return to driving), often within a few years of cessation (Jette & Branch, 1992; Johnson, 2008; Ratnapradipa, Wang, Berg-Weger, & Schootman, 2018).
The Transtheoretical Model has been used to explain driving cessation (Kowalski, Jeznach, & Tuokko, 2014; Stalvey & Owsley, 2003). Within this context, driving resumption may be considered a “relapse” from cessation. Alternatively, Coxon and Keay (2015) used the Precaution Adoption Process Model to create messages targeting behavior change stage by identifying potential barriers to maintaining cessation: lack of alternatives, convenience, and sense of identity associated with car. Cessation is the target behavior for both models. New approaches are needed to examine changes in driving behavior and to accommodate bidirectional movement between driving and cessation.
Driving cessation is associated with several adverse outcomes (e.g., increased risk of dependence, depression, long-term care placement, mortality; Chihuri et al., 2016). As older adults transition driving behavior, the effect, if any, driving resumption has on health outcomes is unknown. Because driving resumption has received limited attention, mortality risk has not been studied within an expanded classification including driving resumption. This study aims to determine whether resumed drivers had a different mortality risk compared with former drivers and continued drivers when controlling for sociodemographic and health variables.
Method
Data and Sample
The National Health and Aging Trends Study (NHATS) is sponsored by the National Institute on Aging (grant number NIA U01AG032947) through a cooperative agreement with the Johns Hopkins Bloomberg School of Public Health, described elsewhere (Kasper & Freedman, 2016; Montaquila, Freedman, Edwards, & Kasper, 2012). Data are from public use files (2011–2015). At baseline, NHATS provided a nationally representative sample of Medicare beneficiaries aged 65 years and older living in the contiguous United States. Our study was limited to community-dwelling self-respondents who had ever driven (n = 6,189; N. G. Choi & DiNitto, 2016; Ratnapradipa et al., 2018).
Measures
Variables were selected based on driving cessation literature (Chihuri et al., 2016) and available in NHATS. Classification of categorical variables was based on response distributions among resumed drivers.
Event
Rounds 2–5 had a flag variable for death based on proxy reporting through the NHATS Last Month of Life questionnaire, indicating that the participant died between previous and current rounds. NHATS did not compare proxy-reported deaths to the National Death Index. Censoring (loss to follow-up) occurred when participants not flagged for death lacked any responses for the current round of data collection, or at Round 5.
Driving status
As a time-dependent variable, driving status was set at baseline from a series of questions, including driving frequency in the past month and drove since last interview. The variable was updated each round based on prior classification (Ratnapradipa et al., 2018). Baseline driving status consisted of current driver (drove in past month) or former driver (not a current driver but did not identify as never driving; N. G. Choi & DiNitto, 2016). Four categories captured subsequent changes in driving status based on whether the respondent drove in the past year: continued driver, resumed driver, new former driver, and continued former driver. Although driving resumption was a potentially repeated event, only 15 participants had more than one resumption. Three categories of driving status were classified: driver (continued to drive until last follow-up; n = 4,209), resumed (any instance of resumed driving; n = 290), and former (stopped driving, did not resume during study period; n = 1,690).
Sociodemographic variables
Variables included: sex, baseline age group, race/ethnicity (non-Hispanic white, non-Hispanic black, other), birth in the United States, high school diploma or above, living arrangement (with spouse/partner, with someone not spouse/partner, alone), Medicaid recipient, vehicle ownership, and social network size (0–5).
Health
Self-rated health was dichotomized (good-to-excellent vs poor-to-fair). Number of chronic health conditions (0–9) was based on reporting of individual conditions: heart attack/heart disease, high blood pressure, arthritis, osteoporosis, diabetes, lung disease, stroke, dementia, and cancer. Overnight hospitalization in the past year, surgery (knee, hip, back, or heart) in the past year, and vision impairment (based on self-report questions about the ability to see across the street, across the room, and close-up) were dichotomized. Depressive symptom severity (2–8, with higher number indicating increased severity) was based on the Patient Health Questionnaire 2. Memory was measured as immediate word recall score (0–10, with higher numbers indicating better recall) and dichotomized self-rated memory (good-to-excellent vs poor-to-fair).
Statistical Analysis
Survival analyses were performed using (a) stratified life tables to estimate survival curves using the Kaplan–Meier method and to compare survival distributions by driving status and sociodemographic variables using the simple log-rank test, and (b) discrete time logistic regression to model the relationship between independent variables and survival time. The Tukey–Kramer adjustment for multiple comparisons of percentage of censored/failed cases was used for the categorical variables with more than two categories. Both survival analyses incorporated survey design effects. The purposeful selection method was used for model building (Hosmer, Lemeshow, & Sturdivant, 2013) by first fitting univariate models, followed by the multivariable model including all statistically significant variables selected from the univariate models. The backward elimination procedure was then used to exclude variables one at a time that were not statistically significant.
All analyses were conducted using SAS software, Version 9.4. Statistical significance used two-tailed testing with P<0.05. Missing data (fewer than 5% of observations) was addressed by casewise exclusion.
This study was exempt from Institutional Review Board oversight.
Results
Continued drivers were 68% (n = 4,209), representing 75% of the national study population; 5% (n = 290) were resumed drivers representing 4% of the population, and 27% of participants (n = 1,690) were former drivers (who never resumed driving) representing 21% of the population. All weighted baseline characteristics differed significantly by driving status (Supplementary Table 1). Overall, 14% (n = 844) of participants died by Round 5, and 52% participated in all five rounds of data collection.
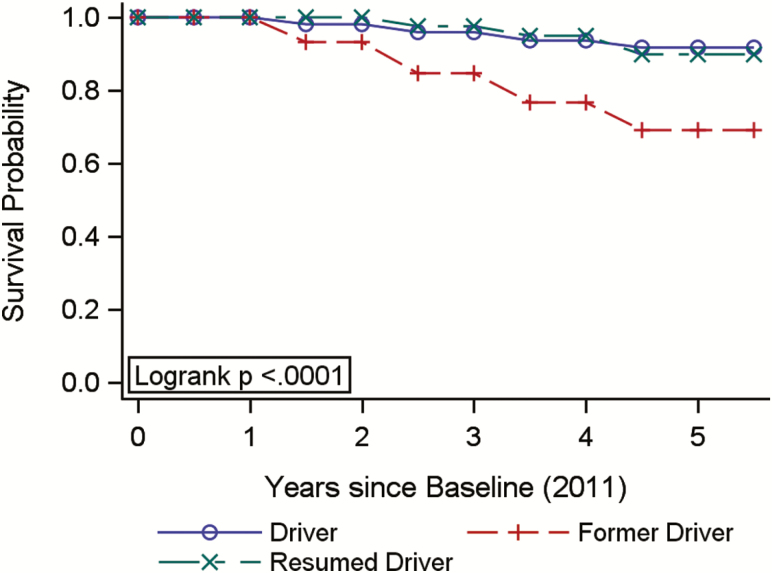
Kaplan–Meier survival curves by driving status over time were estimated from lifetables (Figure 1). The survival probabilities changed over time for each driving status category. Former drivers consistently had the poorest survival, with difference increasing over time. Graphs were similar between unweighted and weighted analysis (results not shown). The weighted log-rank test estimated from lifetables was used to test for equality by driving status and other categorical variables (Supplementary Table 2). All pairwise comparisons were statistically significant.
Figure 1.
Weighted life table survival function, stratified by driving status, NHATS (2011–2015).
For driving status, the percentage of censored/failed cases differed significantly overall and for each paired comparison. The younger age categories had better survival probabilities than older age categories. Survival probability for those aged 65–69 did not differ significantly compared with those 70–74 (p = .32), and those 70–74 did not differ significantly from those 75–79 (p = .11) but all other age comparisons were statistically significant. Survival curves stratified by race showed interaction over time. The curves were similar at the beginning and end of the study, but those in the other category had better survival between Rounds 3 and 4 compared with non-Hispanic whites and non-Hispanic blacks. The survival probabilities of all other stratified categorical variables were statistically significant. Those with better survival included: females, born outside the United States, high school diploma, living with spouse versus alone versus with others, not receiving Medicaid, car owners, good-to-excellent self-rated health, not hospitalized, no vision impairment, and good-to-excellent self-rated memory.
Discrete time logistic regression modeled the relationship between independent variables and survival time. Race was not statistically significant in univariate analysis (p = .30) and therefore excluded. The crude odds ratio of person-year was 0.83, that is, the odds of death decreased by 17% for each additional year that a participant remained in the study. After adjusting for sociodemographic and health variables (Table 1), continued and resumed drivers did not have statistically significant differences in odds of mortality (adjusted odds ratio [aOR] = 1.22; 95% confidence interval [CI] = 0.74, 1.99). However, the odds of death were 2.4 times greater for former versus resumed drivers (aOR = 2.41; 95% CI = 1.51, 3.83).
Table 1.
Adjusted Odds of Mortality, Final Logistic Model, NHATS (2011–2015)
| Variable | aOR | CI |
|---|---|---|
| Person-years*** | 0.87 | 0.82, 0.91 |
| Continued driver vs resumed driver | 1.22 | 0.74, 1.99 |
| Former driver vs resumed driver*** | 2.41 | 1.51, 3.83 |
| Sex (male vs female)*** | 1.60 | 1.32, 1.93 |
| Age: 70–74 vs 65–69 | 1.52 | 0.98, 2.36 |
| Age: 75–79 vs 65–69** | 1.76 | 1.17, 2.67 |
| Age: 80–84 vs 65–69*** | 2.85 | 2.04, 3.98 |
| Age: 85+ vs 65–69*** | 5.33 | 3.56, 7.98 |
| High school diploma (no vs yes) | 0.94 | 0.75, 1.18 |
| Car owner (no vs yes) | 1.08 | 0.88, 1.33 |
| Living with others vs spouse/partner | 1.20 | 0.93, 1.54 |
| Living alone vs spouse/partner | 1.00 | 0.83, 1.20 |
| Medicaid (yes vs no) | 1.04 | 0.78, 1.38 |
| Social network size (0–5, per unit increase in number of contacts) | 0.95 | 0.88, 1.03 |
| Self-rated health (good-to-excellent vs poor-to-fair)*** | 0.51 | 0.41, 0.64 |
| No. chronic conditions (0–9, per unit increase in number of conditions)*** | 1.15 | 1.08, 1.22 |
| Hospitalization in past year (yes vs no)*** | 1.54 | 1.22, 1.96 |
| Depressive symptoms | 1.07 | 1.00, 1.15 |
| Vision impairment (yes vs no) | 0.97 | 0.83, 1.14 |
| Self-rated memory (good-to-excellent vs poor-to-fair) | 1.20 | 0.96, 1.49 |
| Immediate Word Recall Score (0–10, per each additional word recalled)*** | 0.88 | 0.83, 0.93 |
Note: aOR = adjusted odds ratio; CI = 95% confidence interval.
*p < .05. **p < .01. ***p < .001.
Discussion
This study determined whether individuals who stopped and resumed driving had a different mortality risk compared with those who ceased driving altogether and those who continued driving. Our results show that resumed drivers had better survival compared with continued former drivers. There was no statistically significant difference in mortality between resumed and continued drivers in adjusted analysis.
Previous research has found accelerated declines in health and function associated with driving cessation (M. Choi, Lohman, & Mezuk, 2014; Edwards, Lunsman, Perkins, Rebok, & Roth, 2009), as well as increased risk of depression following driving cessation (Chihuri et al., 2016). Reduced driving frequency has been associated with decreased social participation (Pristavec, 2018) as well, although this appears to be moderated by access to rides and alternative transportation. Returning to driving may also serve to mitigate these adverse health effects.
Because driving resumption has received limited attention in the literature, it was not possible to ascertain why certain individuals resumed driving. Two scenarios for driving resumption have been proposed: intended temporary cessation and inability to maintain intended permanent cessation (Ratnapradipa et al., 2018). Therefore, reason for driving resumption may have differential impacts on driving reduction behaviors as well as overall health.
Strengths of this study include the explicit recognition of driving resumption as a driving status category, thus expanding the focus of driving cessation literature. Modeling utilized 5 years of data from a large, nationally representative sample of older adults, suggesting the results are generalizable to the older adult population in the United States.
Study limitations relate to secondary data analysis and availability of variables in the public-use NHATS data files. Death and change in driving status were postulated as time varying variables that could change at any point in time in a given year. Therefore, ideally, information on them at continuous time points would allow for accurate prediction of mortality by using continuous time survival model, when compared with the discrete time survival model conducted in this article due to the discrete nature of driving status. Flagged proxy-reported response at yearly intervals was used to identify deaths, and NHATS lacked the ability to detect changes in driving patterns in less than yearly intervals. Among older adult women who intended to stop driving but resumed, this occurred within 6–9 months of cessation (Johnson, 2008). Therefore, studies with continuous time measurements would be more likely to capture both the changes in driving patterns and the timing of adverse health conditions and allow more accurate survival analysis to predict morality risk. Likewise, NHATS did not collect information about driving ability or fitness to drive, driving history, use of driver rehabilitation services, or reasons for changes in driving status. Another potential limitation was the relatively small number of resumed drivers. Although inclusion at baseline was limited to self-respondents, proxy status in subsequent rounds was not assessed in this analysis, therefore creating the potential for misclassification for time-independent variables.
Cause of death was not available in the public-use data files, so we were unable to ascertain what proportion of study participant deaths were traffic-related, although this is expected to be low. Driving self-regulation was not modeled because it only pertained to those who drove within the past month.
Areas for additional study include the need for refined time-to-event to fully model the effects of driving status on survival, as well as using time-dependent driving status to model the effects of the length of time between cessation and resumption. Ideally, driving status would be monitored continuously (or at least multiple times/year) to capture nuanced changes in driving habits.
Driving is a valued activity often associated with sense of identity and independence (Coxon & Keay, 2015). In this study, among individuals who stopped driving, those who resumed had better survival than those who did not. Implications for practice include driver rehabilitation and retraining, which may enable some former drivers to safely resume driving and thus avoid the increased health risks associated with cessation.
Conflict of Interest
None reported.
Author Contributions
K. L. Ratnapradipa planned the study, acquired the data, conducted the analysis, interpreted results and drafted the article. All authors made substantial contributions to the study design and made critical revisions to the article.
Supplementary Material
Acknowledgments
Data were made available through the National Health and Aging Trends Study (NHATS) Public Use files, sponsored by the National Institute on Aging (grant number NIA U01AG032947) through a cooperative agreement with the Johns Hopkins Bloomberg School of Public Health. The authors bear sole responsibility for the analysis and interpretations presented here.
References
- Bergen G., West B. A., Luo F., Bird D. C., Freund K., Fortinsky R. H., & Staplin L (2017). How do older adult drivers self-regulate? Characteristics of self-regulation classes defined by latent class analysis. Journal of Safety Research, 61, 205–210. doi:10.1016/j.jsr.2017.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chihuri S., Mielenz T. J., DiMaggio C. J., Betz M. E., DiGuiseppi C., Jones V. C., & Li G (2016). Driving cessation and health outcomes in older adults. Journal of the American Geriatrics Society, 64, 332–341. doi:10.1111/jgs.13931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi N. G., & DiNitto D. M (2016). Depressive symptoms among older adults who do not drive: Association with mobility resources and perceived transportation barriers. The Gerontologist, 56(3), 432–443. doi:10.1093/geront/gnu116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi M., Lohman M. C., & Mezuk B (2014). Trajectories of cognitive decline by driving mobility: Evidence from the Health and Retirement Study. International Journal of Geriatric Psychiatry, 29(5), 447–453. doi:10.1002/gps.4024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colby S. L., & Ortman J. M (2015). Projections of the size and composition of the U.S. population: 2014 to 2060 (Current Population Reports, P25-1143). Washington, DC: US Census Bureau; Retrieved from https://www.census.gov/library/publications/2015/demo/p25-1143.html. Accessed 6 March 2019. [Google Scholar]
- Coxon K., & Keay L (2015). Behind the wheel: Community consultation informs adaptation of safe-transport program for older drivers. BMC Research Notes, 8, 764. doi:10.1186/s13104-015-1745-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dellinger A. M., Sehgal M., Sleet D. A., & Barrett-Connor E (2001). Driving cessation: What older former drivers tell us. Journal of the American Geriatrics Society, 49(4), 431–435. doi:10.1046/j.1532-5415.2001.49087.x [DOI] [PubMed] [Google Scholar]
- Dickerson A. E., Molnar L. J., Bedard M., Eby D. W., Berg-Weger M., Choi M.,…Silverstein N. M (2017). Transportation and aging: An updated research agenda to advance safe mobility among older adults transitioning from driving to non-driving. The Gerontologist, 59(2), 215–221. doi:10.1093/geront/gnx120 [DOI] [PubMed] [Google Scholar]
- Edwards J. D., Lunsman M., Perkins M., Rebok G. W., & Roth D. L (2009). Driving cessation and health trajectories in older adults. The Journals of Gerontology, Series A: Biological Sciences and Medical Sciences, 64(12), 1290–1295. doi:10.1093/gerona/glp114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foley D. J., Heimovitz H. K., Guralnik J. M., & Brock D. B (2002). Driving life expectancy of persons aged 70 years and older in the United States. American Journal of Public Health, 92(8), 1284–1289. doi:10.2105/AJPH.92.8.1284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forrest K. Y.-Z., Bunker C. H., Songer T. J., Coben J. H., & Cauley J. A (1997). Driving patterns and medical conditions in older women. Journal of the American Geriatrics Society, 45(10), 1214–1218. doi:10.1111/j.1532-5415.1997.tb03772.x [DOI] [PubMed] [Google Scholar]
- Harmon A. C., Babulal G., Vivoda J. M., Zikmund-Fisher B. J., & Carr D. B (2018). Planning for a nondriving future: Behaviors and beliefs among middle-aged and older drivers. Geriatrics, 3(2), 19. doi:10.3390/geriatrics3020019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hosmer D. W., Lemeshow S., & Sturdivant R. X (2013). Applied logistic regression (3rd ed.). Hoboken, NJ: John Wiley & Sons. doi:10.1002/9781118548387 [Google Scholar]
- Jette A. M., & Branch L. G (1992). A ten-year follow-up of driving patterns among community-dwelling elderly. Human Factors, 34(1), 25–31. doi:10.1177/001872089203400104 [DOI] [PubMed] [Google Scholar]
- Johnson J. E. (2008). Informal social support networks and the maintenance of voluntary driving cessation by older rural women. Journal of Community Health Nursing, 25(2), 65–72. doi:10.1080/07370010802017034 [DOI] [PubMed] [Google Scholar]
- Kasper J. D., & Freedman V. A (2016). National Health and Aging Trends Study user guide: Rounds 1, 2, 3, 4 & 5 beta release. Baltimore: Johns Hopkins University School of Public Health; Retrieved from www.NHATS.org. Accessed 3 February 2017. [Google Scholar]
- Kowalski K., Jeznach A., & Tuokko H. A (2014). Stages of driving behavior change within the Transtheoretical Model™. Journal of Safety Research, 50, 17–25. doi:10.1016/j.jsr.2014.01.002 [DOI] [PubMed] [Google Scholar]
- Montaquila J., Freedman V. A., Edwards B., & Kasper J. D (2012). National Health and Aging Trends Study round 1 sample design and selection (NHATS Technical Paper #1). Baltimore: Johns Hopkins University School of Public Health; Retrieved from http://nhats.org/scripts/sampleDesign.htm. Accessed 6 March 2019. [Google Scholar]
- Naumann R. B., West B. A., & Sauber-Schatz E. K (2014). At what age do you think you will stop driving? Views of older U.S. adults. Journal of the American Geriatrics Society, 62(10), 1999–2001. doi:10.1111/jgs.13050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- NHATS Public Use Data (Rounds 1–5), sponsored by the National Institute on Aging (grant number NIA U01AG032947) through a cooperative agreement with the Johns Hopkins Bloomberg School of Public Health. Retrieved from www.nhats.org. Accessed 10 May 2017.
- Pristavec T. (2018). Social participation in later years: The role of driving mobility. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 73(8), 1457–1469. doi:10.1093/geronb/gbw057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ratnapradipa K. L., Wang J., Berg-Weger M., & Schootman M (2018). Coming out of “retirement”-predictors of driving resumption among older drivers. Innovation in Aging, 2(3), igy030. doi:10.1093/geroni/igy030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudman D. L., Friedland J., Chipman M., & Sciortino P (2006). Holding on and letting go: The perspectives of pre-seniors and seniors on driving self-regulation in later life. Canadian Journal on Aging, 25(1), 65–76. doi:10.1353/cja.2006.0031 [DOI] [PubMed] [Google Scholar]
- Stalvey B. T., & Owsley C (2003). The development and efficacy of a theory-based educational curriculum to promote self-regulation among high-risk older drivers. Health Promotion Practice, 4(2), 109–119. doi:10.1177/1524839902250757 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.