Highlights
-
•
We examined psychological impact of the COVID-19 pandemic on the general population in south korea where the spread of the virus has been controlled but there have been signs of population-wide distress.
-
•
An online study was conducted to investigate the relationship between mental health, social factors and demographic variables in 400 south korean residents.
-
•
Clinical levels of depression, anxiety or stress were reported by 45% of the respondents. Elevated psychosis-risk was present in 12.8%. These represent a drastic increase above the base rate prior to the pandemic.
-
•
Loneliness, but not social network size contributed to deteriorating mental health.
-
•
The extent of the psychological distress in the general population despite successful mitigation of the pandemic is disconcerting. There is an urgent need to prepare for a potential mental illness epidemic in the near future.
Keywords: COVID-19, Loneliness, Psychosis, Depression, Stress, Anxiety
Abstract
South Korea was able to successfully control the spread of COVID-19 without nationwide lockdowns or drastic social distancing efforts, but pandemic-related psychological outcome of the general population remains unknown. Between March and June 2020, 400 South Korean residents participated in an online study of depression, anxiety, stress, psychosis-risk and loneliness, as well as indices of social network, physical health and demographics. Clinical levels of depression, anxiety or stress were reported by 45% of the respondents, and psychosis-risk was present in 12.8%; a drastic increase above the base rate reported by previous studies conducted in South Korea prior to the pandemic. Subjective feelings of loneliness, but not the size of the social network accounted for poor mental health. Women were especially at increased risk for mental health problems. Thus, despite effective mitigation of the pandemic, there was a striking deterioration of mental health. As the psychological burden of the continuing pandemic accrues, the probability of an impending mental health crisis is increasing, especially in countries with greater infection and death rates than South Korea. Comprehensive efforts to address the psychological aftermath of the pandemic are urgently needed.
1. Introduction
As of August 2020, COVID‐19 has infected more than 22 million people worldwide (ecdc.europa.eu ). However, successful mitigation of the pandemic has been achieved in many countries owing to their nationwide efforts to administer and manage public health policies based on science. The case of South Korea (population of 50 million) is particularly illuminating in this respect. After reporting the first case of COVID-19 on January 20th, 2020 (Gralinski, and Menachery, 2020; Hyun et al., 2020), South Korea experienced exponential growth of confirmed COVID-19 cases in the next two months (Kuhn, 2020; Shim et al., 2020). To take control of the pandemic, widespread testing and contact tracing began almost immediately (Kang et al., 2020) through a well-coordinated partnership between the government and private sectors. Novel test settings were launched (e.g., drive-through screening, Kwon et al., 2020) and fast tracking of infected cases with transparent disclosure of information was made available (Park et al., 2020). Although extremely restrictive measures such as immigration control or nationwide lockdowns were not enacted, South Korea brought the pandemic under control through an extraordinarily large volume of testing, efficient contact tracing, monitored quarantines for those who were exposed or suspected to have been exposed to the virus and universal adherence to science-based public health policies by the general public (Park et al., 2020; AL‐Rousan and AL‐Najjar, 2020). There was near-universal compliance with mask use, self-quarantine protocols and social distancing rules. With daily cases dropping below 50 (Kang et al., 2020) and a very low mortality rate (Her, 2020) by June, the vast majority had been spared of the disease.
While the mitigation of COVID-19 nationwide is undoubtedly a success story, the psychological wellbeing of the population during this period has not yet been closely examined. Outcome data from previous epidemics (e.g. Severe Acute Respiratory Syndrome in 2003, and the Middle East Respiratory Syndrome in 2012) forewarn adverse psychiatric consequences (Chan, and Chan, 2004; Sim et al., 2004; Mak et al. 2009; H.C. Kim et al., 2018, Lee et al., 2018). For example, the risk for post-traumatic stress disorder (PTSD) increased for both the survivors of these diseases and healthcare workers (Lee et al., 2018) and psychiatric symptoms remained elevated up to six months after the end of the quarantine period (Jeong et al., 2016). Furthermore, the psychological consequences of pandemics can be extensive across the general population regardless of exposure to the disease itself. Past research indicates that, although the vast majority of the population was never infected, there was a significant psychological toll on the general population (Park and Yu, 2020).
Given the severity and the scale of the current pandemic, a worldwide mental health crisis is expected in the near future (see Holmes et al., 2020; Yao et al., 2020). In addition to chronically elevated levels of stress, anxiety and fear that interfere with daily functioning due to the pandemic (Jung, and Jun, 2020), public health strategies designed to curb the spread of the virus may have an unintended negative impact on mental health. Lockdowns, quarantines and social distancing protocols protect the public but these measures also separate individuals from their regular social networks. Prolonged social isolation is associated with exacerbation of stress, panic, depression, anxiety and psychosis (Bo et al., 2020; ; Rossi et al., 2020; Wang et al., 2020; Zhang, and Ma, 2020; Selten et al., 2017). Social isolation and loneliness have long been linked to poor mental and physical health outcomes (see Leigh-Hunt et al., 2017 for a review). Importantly, it has been shown that the subjective feelings of loneliness rather than objective measures of social contact or network contribute to psychosis-risk (Badcock et al., 2020; Michael and Park, 2016; Benson and Park, 2019). Indeed, the national lockdown enacted earlier this year to stem the spread of COVID-19 may have already resulted in increased psychosis risk in the general population in Italy (D'Agostino et al., 2020).
Although Korea was able to avoid a nationwide lockdown, the widespread closure of public spaces, educational institutions, places of worship and other social venues have been disruptive, especially among young people whose social world collapsed when schools and colleges shut down. Social isolation and disconnection due to the pandemic are likely to be even more burdensome to vulnerable individuals. Indeed, as early as mid-March of 2020, mental illness was the third most frequent underlying condition of those who died of COVID-19 in South Korea (Kang, 2020; ).
A recent survey of Hong Kong residents underscores the pivotal role of loneliness in extraordinarily high levels of psychiatric distress during the pandemic, with almost two-thirds of the respondents reporting depression or anxiety disorders and about a quarter meeting the criteria for psychosis-risk (Tso and Park, 2020). Similar to South Korea, Hong Kong was not severely affected by COVID-19 owing to its early and successful public health efforts to limit the spread of the disease. In contrast to Koreans, Hong Kong residents were forced to undergo a complete lockdown leading to extreme social isolation. Furthermore, Hong Kong had been under prolonged political turmoil and uncertainties that were already generating high levels of stress before the COVID-19 pandemic hit (Ni et al., 2020). Thus, one might expect the psychiatric impact of COVID-19 to be less severe in Korea than in Hong Kong.
The major aim of the present study was to survey mental health and social wellbeing during the COVID-19 pandemic among the general population in South Korea where effective public health strategies and high compliance by the residents were able to successfully stop the spread of the virus. By investigating psychological consequences of the pandemic in a country, which largely escaped the ravages of the COVID-19, we sought to observe mental health outcomes under the best case scenario. In particular, we wanted to elucidate demographic factors (e.g., age, gender, living situation) associated with increased risk or protective factors for psychiatric conditions. Moreover, we hypothesized that there would be adverse psychological consequences of living under the pandemic conditions in relation to social disconnection.
2. Methods
2.1. Participants
Four hundred three participants viewed the introduction page of the online survey in Korean from March 22, 2020 to June 31, 2020. Among those, 400 (99.2%) met the criteria for the survey by their self-reported age (i.e., over 18) and current residence in South Korea at the time of the survey). All 400 respondents completed the survey.
2.2. Procedure
All participants completed the survey in Korean using the Google Form platform (available at https://forms.gle/4zkooaXm4ZfYznUYA). The survey link was disseminated using social media, local online communities, websites and by word-of-mouth in South Korea. This study did not collect any personal or identifying information, such as name, date of birth, contact information, IP address, ethnicity or other potentially identifying information, guaranteeing the total anonymity and privacy of the respondent, and therefore received an exempt status from the Vanderbilt University Institutional Review Board (IRB# 201,000).
2.3. Measures
Participants were asked to respond to questions about their demographic information (age, sex, education level, occupation, marital status), 4 levels of concern about the COVID-19 pandemic from “not at all concerned” to “extremely concerned”, general physical health status, mental health, loneliness and social network. For general physical health, participants reported their health status on a 5-point Likert scale, from “poor” to “excellent”. Subjects also reported the number of days in the past month that they experienced health problems with respect to physical and mental health, disturbances in daily activities, alcohol and tobacco use, pain and worry.
The 42-item version of the Depression Anxiety Stress Scale (DASS; Lovibond, and Lovibond, 1995) and the 16-item version of the Prodromal Questionnaire (PQ-16; Ising et al., 2012; Kim et al., 2018b) were used to assess the mental health of the respondents. DASS was used to assess depression, anxiety and stress levels, classifying the severity from “normal” to “extremely severe”. PQ-16 assessed psychosis risk with a total score of 6 or higher indicating high-risk status (Ising et al., 2012). In addition to PQ-16, there were two items that asked directly about dissociative experiences (out-of-body experience) and voice-hearing. The UCLA Loneliness Scale (Russell, 1996) was utilized to measure subjective feelings of loneliness. The size and the diversity of social network of the respondents were collected to obtain an objective index of social isolation using the Social Network Index (SNI; Cohen, 1997).
2.4. Statistical analysis
First, descriptive data for demographics, general health questions and mental health items were examined. Then, we compared physical and mental health status between demographic subgroups. We used independent t-tests to compare participants in terms of age (old vs. young), sex, employment status and occupation (healthcare worker vs. non-healthcare worker).
Family relationships play an outsized role in the quality of life of South Koreans. The majority of South Koreans live with their families until marriage, and often after marriage as well (see Yang, 2003). We classified family and living arrangement across the whole sample with three groups: married couples (or cohabiting partners), singles living with family and singles living alone. We expected the singles living alone to fare worse during COVID-19 since they are the most likely to be socially disconnected. A series of one-way ANCOVAs, controlling for age and sex, were used to examine family and living arrangement differences.
A series of hierarchical linear regression analysis was used to examine the contributions of loneliness and social network size on physical and mental health variables. In the first step, independent variables for age, sex and concern for COVID-19 were used to form the basic model. In the second step, loneliness, social network diversity and social network size were included in the full model. For each dependent variable (e.g., self-reported health, days physically ill, days when physical and mental health limited engagement in usual activities, days in which pain limited functioning, days mentally ill, days feeling anxious, DASS and PQ-scores), the change in R2 between the basic model and full model was used to examine whether the addition of loneliness and social network explained more of the variance in each physical or mental health variable, after controlling for age, sex and COVID concern. Bonferroni correction of p < .0045 was applied to minimize Type I errors.
3. Results
3.1. Demographics
The majority of the respondents (71.75%) identified as female, 27.5% as male and 0.75% as other or preferred not to answer. Mean age was 31.68 years (SD =12.31; range, 18–72). Mean years of education was 14.83 (SD =3.01). 68.25% were single, 29.75% were married or cohabiting with a partner and the rest preferred not to answer. 30.5% were employed and 62.5% were unemployed (7% preferred not to answer). Only 6% (n = 24) of the total sample were healthcare workers, who made up 9.6% of the total number of employed participants. Please see Table 1 for details.
Table 1.
Demographic information.
| Demographics (n = 400) | M (SD) |
| Age | 31.68 (12.31) |
| Years of Education | 14.83 (3.01) |
| N (%) | |
| Sex | |
| Female | 110 (27.50%) |
| Male | 287 (71.75%) |
| Other | 0 |
| Prefer not to answer | 3 (0.75%) |
| Marital status and living situation | |
| Married | 119 (29.75%) |
| Single but live with family | 176 (44.00%) |
| Single and live alone | 98 (24.50%) |
| Prefer not to answer | 7 (1.75%) |
| Employment | |
| Employed | 122 (30.50%) |
| Unemployed | 250 (62.50%) |
| Prefer not to answer | 28 (7%) |
| Work in Healthcare | 24 (6%) |
3.2. General health
No respondent reported a diagnosis of COVID-19. One participant was in self-quarantine due to suspected exposure to COVID-19 but was asymptomatic. The mean rating for self-reported overall health (Excellent =5; Very good = 4; Good =3; Fair =3; Poor=1) was 3.07 (SD = 0.93), with 69.5% reporting 4 (Good) or above. Forty-percent of the respondents reported one or more of the following types of illnesses in the past 30 days: head cold or chest cold (11.75%); gastrointestinal illness with vomiting or diarrhea (16.75%); flu, pneumonia or ear infections (6.75%); or an ongoing or chronic medical condition (4.75%). Only 6.75% smoked (M = 0.45 packs/day, SD = 0.39) but 49.5% drank alcohol (M = 2.13 drinks/week, SD = 1.64). Among the smokers and drinkers, 25.9% reported smoking and 16.2% endorsed drinking more than usual in the past 30 days.
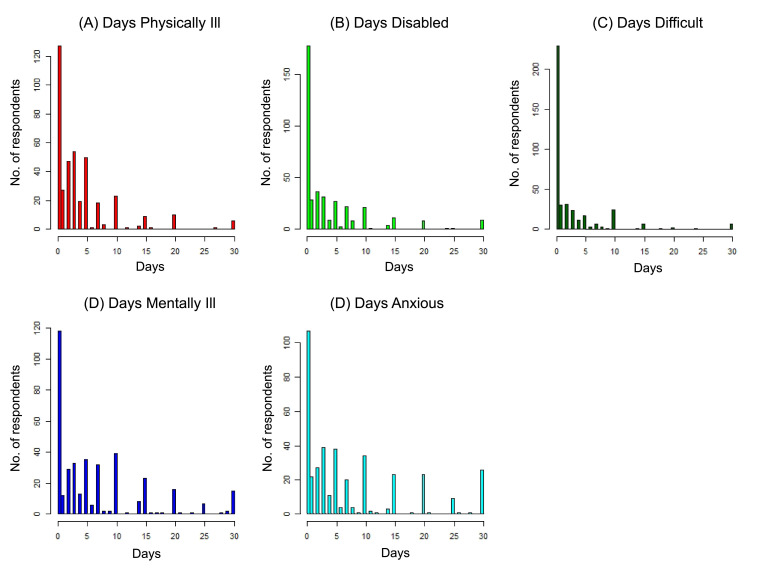
Fig. 1 represents the number of days (in the past month) during which participants reported experiencing significant health problems. Psychological problems (i.e., poor mental health, or feeling worried, anxious or tense) were responsible for more days lost to illness or disability than physical health issues (i.e., poor physical health or pain). See Fig. 1.
Fig. 1.
Number of days (in the past month) in which the respondents experienced these problems
A) Days of Physical Illness: mean = 4.0 days (SD = 5.5)
B) Days of Disability: mean = 3.8 days (SD = 6.2)
C) Days of Difficulty due to pain: mean = 2.6 (SD = 5.3)
D) Days of Mental Illness: mean = 6.7 days (SD = 7.9
E) Days of feeling worried, anxious, or tense: mean = 7.4 days (SD = 8.9).
3.3. Psychological symptoms
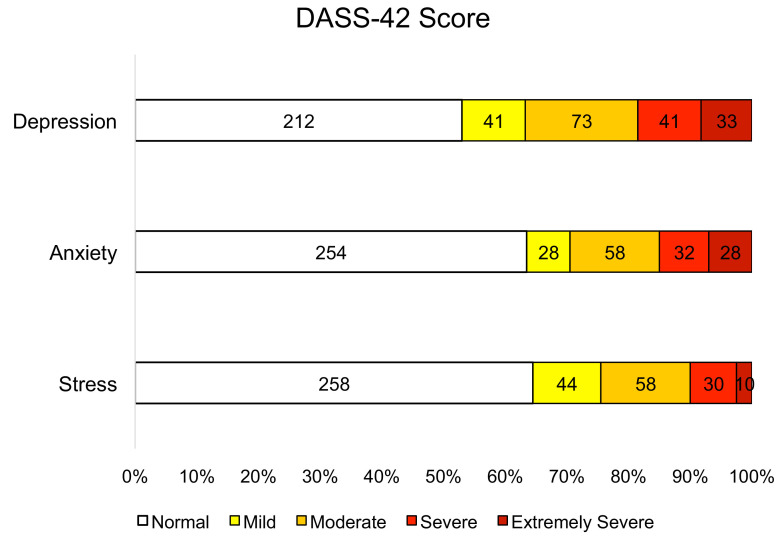
Depression, anxiety, and stress (DASS-42). The mean subscale scores were 11.66 (median = 9, SD = 9.89) for depression; 7.34 (median = 5, SD = 7.18) for anxiety; 12.19 (median = 11, SD = 9.05) for stress. We used the published cut-off scores (Crawford, and Henry, 2003) to determine the proportion of participants experiencing at least moderate levels of depression, anxiety and stress. Depression was present in 36.75%, anxiety in 29.5%, and stress in 24.5% of the participants. Furthermore, 45% (n = 180, 95% CI [40.12%, 49.87%]) of the respondents endorsed moderate or higher symptoms on one or more of the subscales. See Fig. 2 .
Fig. 2.
Levels of depression, anxiety, and stress.
The numbers of respondents scoring at different severity levels of Depression, Anxiety, and Stress on the DASS-42 and corresponding%.
Prodromal Psychosis (PQ-16). Mean endorsed items was 2.6 (median = 2, SD = 2.67, range = 0 – 14). Mean distress score was 3.69 (median= 2, SD = 5.59, range = 0 – 45). According to the published cut-off score of 6 or more endorsed items (Ising et al., 2012; S.W. Kim et al., 2018b), 12.75% (n= 51, 95% CI [9.48%, 16.02%]) of the respondents were at increased risk for psychosis. In addition to the PQ-16, there were two items that asked directly about the presence of out-of-body experience (OBE) or auditory hallucinations. 7% reported experiencing OBEs, and 16.25% reported having auditory hallucinations.
3.4. Loneliness and social network
Loneliness. On the UCLA Loneliness Scale, the mean score of the 400 respondents was 43.28 (median = 42; SD = 12.47), comparable to the reported norms of the North American (Russell, 1996), and validated norms from South Korean (O. Kim, 1999a; ; Kim, 1999b) samples.
Social Network Index. The mean number of high-contact social roles was 4.45 (median = 4, SD = 2.03, range = 0 – 12). The mean number of people with whom the respondents had regular contact (i.e., at least once every 2 weeks) was 13.49 (median = 13, SD = 8.64, range = 0 – 62).
3–5. Physical and mental health status in relation to demographic characteristics
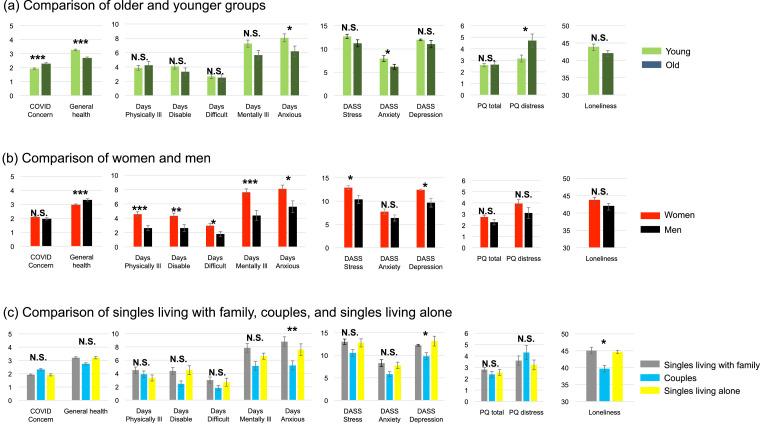
We examined the effect of age by splitting participants into two groups about the mean (M = 31.68, SD = 12.31). Older participants reported greater concern for COVID-19 (t 398 = 4.29, p < .001) and worse general physical health (t 311.42 = −6.37, p < .001). There were no differences in age groups for days of physical health (t 397 = 0.63, p = .53), days of mental health (t 397 = −1.93, p = .06), days when usual activities affected by health problems (t 394 = −1.16, p = .25), or pain (t 396 = −0.31, p = .75). Younger respondents endorsed more days of feeling worried, anxious or tense (t 396 = 2.02, p = .04). Younger people also scored higher on DASS anxiety (t 327.90 = 2.48, p = .01), but the two groups did not differ with regard to DASS depression (t 398 = 0.89, p = .38) or DASS stress (t 398 = 1.55, p = .12). There was no difference in the PQ-16 total score between the old and young groups (t 223.19 = 0.13, p = .90), but older people reported greater distress (t 211.55 = 2.40, p = .02). See Fig. 3 .
Fig. 3.
Physical and mental health status of demographic subgroups
• COVID Concern: self-reported concern for COVID-19 in 5-point Likert-like scale (1=not at all concerned to 5= very concerned)
• General health: self-reported general health in 5-point Likert scale (1=Poor to 5= Excellent health)
• Days Physically Ill: the number of days physical health was not good in the past month
• Days Disable: the number of days usual activities were affected due to health problems in the past month
• Days Difficult: the number of days usual activities were affected due to pain in the past month
• Days Mentally Ill: the number of days mental health was not good in the past month
• Days Anxious: the number of days felt worried, anxious, or tense in the past month
• DASS: the 42-item version of the Depression Anxiety Stress Scale
• PQ: the 16-item version of the Prodromal Questionnaire
• Loneliness: a total score on the UCLA Loneliness Scale.
There were significant differences between women and men on most physical and mental health variables. Women reported worse general health ratings (t 395 = −3.39, p = .001), more days of physical (t 308.10 = 3.80, p < .001) and mental health problems (t 213.38 = 3.84, p < .001), more days when their usual activities were affected by health problems (t 258.68 = 2.78, p < .01) or pain (t 324.37 = 2.41, p = .02), and more days when they felt worried, anxious or tense (t 393 = 2.53, p = .01). Men and women did not differ on the levels of concern for COVID-19 (t 395 = 1.46, p = .15). On the DASS subscales, women scored higher than men on stress (t 395 = 2.48, p = .01) and depression (t 395 = 2.50, p = .01) but not on anxiety (t 395 = 1.68, p = .09). More women (40.4%) reported clinical levels of depression than men (26.4%) (χ 2 = 6.78, df = 1, p < 0.01). Clinical levels of one or more of the DASS subscales were reported by 46.1% of women compared to 36.4% of men (χ 2= 4.42, df = 1, p = 0.04), indicating heightened emotional distress in women during the pandemic. There were no sex differences in the PQ-16 scores (total: t 395 = 1.56, p = .12; distress: t 395 = 1.35, p = .18) and loneliness (t 395 = 1.24, p = .22). See Fig. 3.
With regard to family and living arrangements, there were no differences between family groups in terms of COVID concern, self-reported general health, days physically ill, days when usual activities were affected by health problems, days affected by pain, days mentally ill, DASS-stress, DASS-anxiety and PQ-16. There were significant differences between singles living with family, married couples, and singles living alone for days feeling worried, anxious or tense (F 2, 388 = 4.45, p = .01), DASS depression (F 2, 390 = 3.39, p = .03), and UCLA loneliness (F 2, 390 = 3.72, p = .03). Post-hoc comparisons using a Tukey HSD correction showed that singles living with family experienced more days of worry than people who were married. There was a marginal difference between for days feeling worried between singles living alone and married couples. Single people living alone and with family reported experiencing more depression and loneliness than married people. There were no differences between singles living alone or with family in terms of depression and loneliness. Detailed information can be found in the supplementary Table S1.
Employment, education and healthcare worker status did not have a significant effect on any of the physical or mental health variables.
3.6. Predictors of physical and mental health status
Hierarchical linear regression was used to examine the effect of loneliness and social network on general health and mental health ratings. Each full model showed a significant change in the magnitude of R2, suggesting that loneliness and social networks explained some of the variance in general health and mental health variables. When individual estimates were examined within each model, loneliness but not the size of social network was solely responsible for the change in R2, ranging from 5.1% to 45.4%. See Table 2 and Supplementary Table S2.
Table 2.
Predictors of Physical and Mental Health.
| Physical health/mental health measures | ||||||||
| Basic Model | Full Model | |||||||
| df | R2 (95% C.I.) | F | p | df | ΔR2 (95% C.I.) | ΔF | p | |
| General health rating (1–5) | 3, 391 | 10.3% (4.7 - 15.8%) | 14.90 | <0.0001* | 6, 388 | 8.6% (5.8 - 11.3%) | 0.12 | <0.0001* |
| Days of Physical Illness | 3, 390 | 2.9% (−0.3 - 6.2%) | 3.93 | .0087 | 6, 387 | 5.1% (2.9 - 7.2%) | 1.68 | <0.0001* |
| Days of Disability | 3, 387 | 3.0% (−0.3 - 6.3%) | 4.04 | .0076 | 6, 384 | 14.2% (10.8 - 17.6%) | 9.28 | <0.0001* |
| Days of Difficulty due to Pain | 3, 389 | 1.5% (−0.8 - 3.9%) | 2.04 | .011 | 6, 386 | 7.8% (5.2 - 10.4%) | 4.61 | <0.0001* |
| Days of Mental Illness | 3, 390 | 5.2% (1.0 - 9.4%) | 7.09 | .0001* | 6, 387 | 15.5% (12.0 - 19.1%) | 9.73 | <0.0001* |
| Days of feeling worried, anxious, tense | 3, 389 | 3.3% (−0.1 - 6.7%) | 4.40 | .0046 | 6, 386 | 12.9% (9.6 - 16.2%) | 8.03 | <0.0001* |
| Depression, Anxiety, Stress and Psychosis-risk | ||||||||
| Dependent variable | Basic Model | Full Model | ||||||
| df | R2 (95% C.I.) | F | p | df | ΔR2 (95% C.I.) | ΔF | p | |
| DASS Depression | 3, 391 | 2.7% (−0.4 - 5.7%) | 3.56 | .014 | 6, 388 | 45.4% (40.5 - 50.3%) | 56.21 | <0.0001* |
| DASS Anxiety | 3, 391 | 3.5% (0.0 - 7.0%) | 4.76 | .0028* | 6, 388 | 25.3% (21.1 - 29.6%) | 21.44 | <0.0001* |
| DASS Stress | 3, 391 | 4.3% (0.4 - 8.1%) | 5.79 | .0007* | 6, 388 | 29.7% (25.2 - 34.2%) | 27.46 | <0.0001* |
| PQ-16 Total | 3, 391 | 2.1% (−0.6 - 4.9%) | 2.84 | .038 | 6, 388 | 10.2% (7.3 - 13.2%) | 6.28 | <0.0001* |
| PQ-16 Distress | 3, 391 | 3.2% (−0.2 - 6.6%) | 4.35 | .0050 | 6, 388 | 13.7% (10.3 - 17.1%) | 8.82 | <0.0001* |
* Bonferroni correction for the significance test was adopted (α < 0.0045).
General health ratings: self-reported general health (ratings from 1 to 5).
Days of physical Illness: the number of days physical health was not good.
Days of mental Illness: the number of days mental health was not good.
Days of disability: the number of days usual activities were affected due to health problems.
Days of difficulty due to pain: the number of days when usual activities were affected due to pain.
Days of feeling worried, Anxious or tense.
4. Discussion
The primary goal of the current study was to investigate the psychological wellbeing of South Korean residents during the COVID-19 pandemic. Successful management of COVID-19 in South Korea was achieved by proactive, nationwide interventions conducted by the government and the high compliance of the general public (AL‐Rousan and AL‐Najjar, 2020). However, the results of the present study indicate signs of psychological distress. Many respondents reported suffering from mental health issues and feeling worried, anxious or tense 7 days out of 30 on average. Importantly, clinical levels of depression, anxiety or stress were reported by nearly half of the respondents. These numbers vastly exceed previously reported 12-month prevalence rates of depression (1.5%) and generalized anxiety disorder (0.4%), surveyed by the Korean ministry of health and welfare using a similar measure, prior to the current pandemic (see Hong et al., 2016). Psychosis-risk was elevated in a noticeably higher proportion of the population during the COVID-19 pandemic compared with the prevalence of 6.6% reported in a validation study of the Korean version of the Prodromal Questionnaire (Kim et al., 2018b). Overall, these findings suggest a significant psychological impact of the COVID-19 pandemic on the mental health and social wellbeing in South Korean, with high rates of depression, anxiety, stress and psychosis-risk.
We observed significant sex differences in psychological and physical wellbeing; physical and psychological suffering were greatly exacerbated in women. Women reported significantly more days with physical and mental health problems and higher levels of stress and depression than men. According to the Korean government, the 12-month prevalence rates of depression and anxiety prior to the pandemic were higher for women than men but the difference was small. However, our data indicate a stark and concerning sex difference in mental health outcomes of women during the pandemic. This observed gender disparity in our study may reflect the fact that gender inequality in South Korea is consistently ranks as one of the worst in the world despite the fact that women are well-educated, participate in the workforce and have excellent healthcare. The gender pay gap, already one of the worst among the industrialized nations (The World Economic Forum, 2017) got much worse during the pandemic as the unemployment rate among women disproportionately skyrocketed (Kim, 2020). These disparities are layered upon cultural expectations that place disproportionate burden of housework and childcare on women, which may greatly compound the pandemic-related distress. However, to better understand these findings, more comprehensive investigations of women's mental health are warranted and our findings underscore the importance of developing targeted strategies for supporting women during the pandemic.
Loneliness was not significantly elevated above the reported pre-pandemic norms from North American (Russell, 1996) or South Korean (Kim, 1999a;Kim, 1999b) studies. However, the majority of the respondents (75%) lived with their families and there was no nationwide lockdown in Korea. Thus, a partial maintenance of social life was possible for most people even though schools, colleges and many workplaces were closed for a prolonged period. Nevertheless, loneliness emerged as a significant predictor for the self-reported general health ratings and mental health variables, even after controlling for age, sex and the degree of concern for COVID-19. In contrast, objective measures of social isolation (e.g. social network size) did not significantly predict physical or mental health variables. These findings underscore the importance of loneliness in the context of public health but it is crucial to understand how and why loneliness might arise.
It is commonly assumed that living with family would reduce loneliness. Families are often sources of emotional, social and financial support but some families are also fraught with hostilities, conflict and distress. We found that marital status and family living arrangement played a significant role in loneliness and depression. In Korea, single adults (i.e., unmarried or without long-term romantic partner) usually live with their families rather than alone. We asked if singles who live with their families fare better than singles who live alone. Singles, regardless of their living arrangements fared worse than couples especially with respect to depression and loneliness but surprisingly, there was no difference in mental health outcome between singles living alone versus singles living with family. In other words, living alone itself was not necessarily detrimental to mental health during this period. However, the quality and type of relationships mattered more than physical proximity to family members. For example, singles living with family reported more days spent worrying than did married couples. Here, the concept of expressed emotion (EE) may be relevant (see Hooley, 2007). EE is a measure of family environment that captures the degree of hostility and negative emotions. Importantly, high EE predicts worse clinical outcomes across a wide range of psychological conditions (Hooley, 2007). During the pandemic when Korean residents suffered a significant narrowing of their usual social life, time spent at home increased dramatically. Extended contact with family members may reduce social isolation but could also increases exposure to high EE. We do not have data on family dynamics but anecdotally, we observed that out of 13 participants who reported experiencing some form of abuse (verbal or physical) recently, the majority were singles living with family. Whilst this sample is too small to draw any conclusions, this observation underscores the complex relationships among family dynamics, loneliness and mental health. Future research could further elucidate individual differences and family environment that may contribute to increased risk for mental illness. Overall, the impact of loneliness on mental health needs to be interpreted in the context of family structures and culture as each society struggles to adapt to the pandemic.
Compared to a recent study in Hong Kong (Tso, & Park, 2020), the psychological impact of COVID-19 appears to be milder in South Korea. Fewer people met the clinical levels of depression, anxiety, stress and psychosis-risk in South Korea. Moreover, the average number of days the respondents reported feeling worried, anxious or tense was half (7.4 days) of that reported by those in Hong Kong (14.1 days). South Korea's adoption of less restrictive social distancing measures might be a factor, but the greater severity of psychological distress reported by Hong Kong residents might also reflect ongoing civil unrest that had already traumatized the city (Ni et al., 2020). Sociopolitical unrest is widespread, with many countries including the United States experiencing violent conflicts. Mental health consequences of COVID-19 should be examined within the social and political context of each nation in order to implement culturally appropriate interventions.
There are several caveats. First, a large number of the respondents were young university students and was disproportionately made up of women, which limits generalizability to the whole South Korean population. Second, the results of this study convey a snapshot of a highly organized and efficient country meeting the unprecedented challenges of a global catastrophe; sociocultural aspects of the response to the pandemic may not generalize to other countries. Fourth, this cross-sectional design does not allow us to track psychological wellbeing over time. Future studies are needed to build a fuller picture of the psychological impact of COVID-19 as the pandemic settles into a chronic situation. Nevertheless, the results of this study clearly indicate that successful management of the pandemic is insufficient to protect the general public from disconcerting deterioration of mental health.
Since the beginning of the COVID-19 pandemic, many have predicted future mental health crises (Holmes et al., 2020). Whilst COVID-19 might have a greater psychological impact on individuals with existing psychiatric disorders (Kang, 2020; ), our findings indicate that the general public is also at elevated risk for psychiatric disorders even when the pandemic is under control. It is important to reduce loneliness, improve the quality of social relationships and provide targeted support for women. As COVID-19 continues to disrupt the lives of billions of people, comprehensive public health efforts must be implemented to meet the difficult challenges of prolonged psychological distress.
Funding information
This work was supported in part by the Gertrude Conaway Vanderbilt Endowment.
CRediT authorship contribution statement
Hyeon-Seung Lee: Methodology, Formal analysis, Investigation, Data curation, Visualization, Writing - original draft, Writing - review & editing. Derek Dean: Formal analysis, Writing - original draft, Writing - review & editing. Tatiana Baxter: Methodology, Data curation, Writing - original draft, Writing - review & editing. Taylor Griffith: Methodology, Data curation, Writing - original draft, Writing - review & editing. Sohee Park: Conceptualization, Methodology, Writing - original draft, Writing - review & editing, Resources, Supervision, Project administration, Funding acquisition.
Declaration of Competing Interest
None
Acknowledgement(s).
We would like to thank Lnie Torregrossa, Hafsah Diakhate, Jason Scott, Sunil Shenoy, Iris Kim and Catherine Martinez for their helpful comments and support.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.psychres.2020.113570.
Appendix. Supplementary materials
References
- AL‐Rousan N., AL‐Najjar H. Data analysis of coronavirus COVID‐19 epidemic in South Korea based on recovered and death cases. J. Med. Virol. 2020 doi: 10.1002/jmv.25850. jmv.25850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Badcock J.C., Adery L.H., Park S. Loneliness in psychosis: a practical review and critique for clinicians. Clinical Psychology: Science and Practice. 2020:e12345. [Google Scholar]
- Benson T., Park S. Increased plasticity of bodily self-experiences in individuals who may carry latent liability for schizophrenia. Schizophr. Res. 2019;207:58–62. doi: 10.1016/j.schres.2018.05.004. PMID 29793817. [DOI] [PubMed] [Google Scholar]
- Bo H.X., Li W., Yang Y., Wang Y., Zhang Q., Cheung T., Wu X., Xiang Y.T. Posttraumatic stress symptoms and attitude toward crisis mental health services among clinically stable patients with COVID-19 in China. Psychol Med. 2020:1–2. doi: 10.1017/S0033291720000999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan A.O.M., Chan Y.H. Psychological impact of the 2003 severe acute respiratory syndrome outbreak on health care workers in a medium size regional general hospital in Singapore. Occup Med (Chic Ill) 2004;54(3):190–196. doi: 10.1093/occmed/kqh027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crawford J.R., Henry J.D. The Depression Anxiety Stress Scales (DASS): normative data and latent structure in a large non-clinical sample. British Journal of Clinical Psychology. 2003;42(2):111–131. doi: 10.1348/014466503321903544. [DOI] [PubMed] [Google Scholar]
- D’Agostino A., D’Angelo S., Giordano B., Cigognini A.C., Chirico M.L., Redaelli C., Gambini O. Brief Psychotic Disorder during the national lockdown in Italy: an emerging clinical phenomenon of the coronavirus pandemic. Schizophr Bull. 2020 doi: 10.1093/schbul/sbaa112. sbaa112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gralinski L.E., Menachery V.D. Return of the coronavirus: 2019-nCoV. Viruses. 2020;12(2):1–8. doi: 10.3390/v12020135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Her M. How is COVID-19 affecting South Korea? What is our current strategy? Disaster Med Public Health Prep. 2020:68–70. doi: 10.1017/dmp.2020.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes E.A., O’Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., Ballard C., Christensen H., Cohen Silver R., Everall I., Ford T., John A., Kabir T., King K., Madan I., Michie S., Przybylski A.K., Shafran R., Sweeney A., Bullmore E. Vol. 7. Elsevier Ltd; 2020. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science; pp. 547–560. (The Lancet Psychiatry). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong J.P., Lee D.W., Ham B.J., Lee S.H., Sung S.J., Yoon T. Ministry of Health and Welfare (Korea); Seoul: 2016. Survey of Mental Disorders in Korea. 2017 April (No. 11-1352, pp. 000-000564). Report. [Google Scholar]
- Hooley J.M. Expressed emotion and relapse of psychopathology. Annu. Rev. Clin. Psychol. 2007;3:329–352. doi: 10.1146/annurev.clinpsy.2.022305.095236. [DOI] [PubMed] [Google Scholar]
- Hyun J.H., Kim J.H., Lee H.Y. Contact tracing results of the first confirmed COVID-19 case in the Republic of Korea. Public Health Weekly Report, Korean Centers for Disease Control and Prevention. 2020;13(7):352–358. [Google Scholar]
- Ising H.K., Veling W., Loewy R.L., Rietveld M.W., Rietdijk J., Dragt S., Klaassen R.M.C., Nieman D.H., Wunderink L., Linszen D.H., Van Der Gaag M. The Validity of the 16-Item Version of the Prodromal Questionnaire (PQ-16) to Screen for Ultra High Risk of Developing Psychosis in the General Help-Seeking Population. Schizophr Bull. 2012;38(6):1288–1296. doi: 10.1093/schbul/sbs068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeong H., Yim H.W., Song Y.J., Ki M., Min J.A., Cho J., Chae J.H. Mental health status of people isolated due to Middle East Respiratory Syndrome. Epidemiol Health. 2016;38 doi: 10.4178/epih.e2016048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jung S.J., Jun J.Y. Mental health and psychological intervention amid COVID-19 outbreak: perspectives from South Korea. Yonsei Med. J. 2020;61(4):271–272. doi: 10.3349/ymj.2020.61.4.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang J.H., Jang Y.Y., Kim J.H., Han S.H., Lee K.R., Kim M., Eom J.S. South Korea’s responses to stop the COVID-19 pandemic. Am J Infect Control. 2020;000:1–7. doi: 10.1016/j.ajic.2020.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang Y.J. Mortality rate of infection with COVID-19 in Korea from the perspective of underlying disease. Disaster Med Public Health Prep. 2020:50–52. doi: 10.1017/dmp.2020.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim H.C., Yoo S.Y., Lee B.H., Lee S.H., Shin H.S. Psychiatric findings in suspected and confirmed middle east respiratory syndrome patients quarantined in hospital: a retrospective chart analysis. Psychiatry Investig. 2018;15(4):355–360. doi: 10.30773/pi.2017.10.25.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim O. Mediation effect of social support between ethnic attachment and loneliness in older Korean immigrants. Research in Nursing and Health. 1999;22(2):169–175. doi: 10.1002/(sici)1098-240x(199904)22:2<169::aid-nur8>3.0.co;2-f. 10.1002/(SICI)1098-240X(199904)22:2<169::AID-NUR8>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- Kim O. The effects of loneliness on alcohol drinking, smoking, and health perception in college students. J Korean Acad Nurs. 1999;29(1):107–116. [Google Scholar]
- Kim, S. (2020). Widest Gender Pay Gap in OECD Set to Worsen With Pandemic. September, 11th 2020. www.Bloomberg.com.
- Kim S.W., Chung Y.C., Kang Y.S., Kim J.K., Jang J.E., Jhon M., Lee J.Y., Kim J.M., Shin I.S., Yoon J.S. Validation of the Korean version of the 16-item prodromal questionnaire in a non-help-seeking college population. Psychiatry Investig. 2018;15(2):111–117. doi: 10.30773/pi.2017.04.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuhn A. Secretive church sect at the center of South Korea's coronavirus outbreak. NPR. 2020 https://www.npr.org/sections/goatsandsoda/2020/02/24/808914718/secretive-church-sect-at-the-center-of-south-koreas-coronavirus-outbreak available at. [Google Scholar]
- Kwon K.T., Ko J.H., Shin H., Sung M., Kim J.Y. Drive-through screening center for covid-19: a safe and efficient screening system against massive community outbreak. J. Korean Med. Sci. 2020;35(11):2–5. doi: 10.3346/jkms.2020.35.e123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S.M., Kang W.S., Cho A.R., Kim T., Park J.K. Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Compr Psychiatry. 2018;87:123–127. doi: 10.1016/j.comppsych.2018.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leigh-Hunt N., Bagguley D., Bash K., Turner V., Turnbull S., Valtorta N., Caan W. An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health. 2017;152:157–171. doi: 10.1016/j.puhe.2017.07.035. [DOI] [PubMed] [Google Scholar]
- Lovibond P.F., Lovibond S.H. THE STRUCTURE OF NEGATIVE EMOTIONAL STATES: COMPARISON OF THE DEPRESSION ANXIETY STRESS SCALES (DASS) WITH THE BECK DEPRESSION AND ANXIETY INVENTORIES. BehaP. Res. Ther. 1995;33(Issue 3) doi: 10.1016/0005-7967(94)00075-u. [DOI] [PubMed] [Google Scholar]
- Michael J., Park S. Anomalous bodily experiences and perceived social isolation in schizophrenia: an extension of the Social Deafferentation Hypothesis. Schizophr. Res. 2016;176(2–3) doi: 10.1016/j.schres.2016.06.013. (392-7)PMID 27344986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ni M.Y., Yao X.I., Leung K.S.M., Yau C., Leung C.M.C., Lun P., Flores F.P., Chang W.C., Cowling B.J., Leung G.M. Depression and post-traumatic stress during major social unrest in Hong Kong: a 10-year prospective cohort study. The Lancet. 2020;395(10220):273–284. doi: 10.1016/S0140-6736(19)33160-5. [DOI] [PubMed] [Google Scholar]
- Park S., Choi G.J., Ko H. Information Technology-Based Tracing Strategy in Response to COVID-19 in South Korea - Privacy Controversies. JAMA - Journal of the American Medical Association. 2020;323(21):2129–2130. doi: 10.1001/jama.2020.6602. [DOI] [PubMed] [Google Scholar]
- Park Hyunbong, Yu Soyoung. Mental healthcare policies in South Korea during the COVID-19 epidemic. Health Policy Technol. 2020;9(3):279–280. doi: 10.1016/j.hlpt.2020.06.006. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7297166/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossi R., Socci V., Talevi D., Mensi S., Niolu C., Pacitti F., Marco A.Di, Rossi A., Siracusano A., Lorenzo G.Di. COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. An N=18147 web-based survey. MedRxiv. 2020;20057802 doi: 10.1101/2020.04.09.20057802. 2020.04.09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell D.W. UCLA Loneliness Scale (Version 3): reliability, validity, and factor structure. J Pers Assess. 1996;66(1):20–40. doi: 10.1207/s15327752jpa6601_2. [DOI] [PubMed] [Google Scholar]
- Selten J.P., Booij J., Buwalda B., Meyer-Lindenberg A. Biological mechanisms whereby social exclusion may contribute to the etiology of psychosis: a narrative review. Schizophr Bull. 2017;43(2):287–292. doi: 10.1093/schbul/sbw180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shim E., Tariq A., Choi W., Lee Y., Chowell G. Transmission potential and severity of COVID-19 in South Korea. International Journal of Infectious Diseases. 2020;93:339–344. doi: 10.1016/j.ijid.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sim K., Phui N.C., Yiong H.C., Soon W.S.W. Severe acute respiratory syndrome-related psychiatric and posttraumatic morbidities and coping responses in medical staff within a primary health care setting in Singapore. Journal of Clinical Psychiatry. 2004;65(8):1120–1127. doi: 10.4088/JCP.v65n0815. [DOI] [PubMed] [Google Scholar]
- Tso I., Park S. Alarming Mental Health Status Among Hong Kong Residents During the COVID-19 Epidemic: role of Loneliness. Psychiatry Res. 2020 doi: 10.1016/j.psychres.2020.113423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int J Environ Res Public Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The World Economic Forum (2017). The Global Gender Gap Report. ISBN 978-1-944835-12-5.
- Yang O.K. Family Structure and Relations. In: Shin D.C., Rutkowski C.P., Park C.M., editors. Vol. 14. Springer; 2003. 10.1007/978-94-017-0281-2_7. [Google Scholar]
- Yao H., Chen J.H., Xu Y.F. Patients with mental health disorders in the COVID-19 epidemic. The Lancet Psychiatry. 2020;7(4):e21. doi: 10.1016/S2215-0366(20)30090-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y., Ma Z.F. Impact of the COVID-19 Pandemic on Mental Health and Quality of Life among Local Residents in Liaoning Province, China: a Cross-Sectional Study. Int J Environ Res Public Health. 2020;17(7):2381. doi: 10.3390/ijerph17072381. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.