Abstract
Soaring gold prices have created an almost impossible void in the Dental Materials supply reserves for affordable patient posterior crowns. Fortunately, aerotech fiber-reinforced composite (FRC) materials in use for many diverse structural applications can be developed for dentistry to replace gold with computer-assisted design/computer-assisted manufacture (CAD/CAM) technology. Current dental ceramics or high-strength oxide ceramics like alumina and zirconia available for CAD/CAM have extremely poor fracture-toughness properties and can propagate microscopic cracks rapidly to sudden adverse brittle failure. As a highly promising alternative, exceptional FRC fracture toughness properties counteract brittle failure with high-strength fibers that act as major barriers to crack propagation. In addition, excellent rapid FRC CAD/CAM machining can offer one-patient appointments for single crowns. FRCs have high-strength fibers coupled into a polymer matrix with the ability to form strong covalent bonds with resin adhesives whereas ceramics do not bond well and oxide ceramics have non-reactive inert surfaces making resin bonding extremely difficult. Prominent adhesive free-radical covalent bonding by FRCs then provides a great opportunity to achieve a crown marginal reline directly on the patienťs clinical tooth for possible near zero-gap defect tolerances. To place crown gingival marginal defects in proper perspective, gaps between the tooth and crown expose luting cements that can wash out and provide space for microbial plaque growth. Bacterial toxins released from a crown-tooth interface can subsequently produce secondary decay, gingival inflammation and eventually under severe plaque environments breed periodontal disease with bone loss.
Keywords: Fiber-Reinforced Composite, Margins, Surface Roughness, Hydrophobic, Bacterial Adhesion, Gingival Recession
Introduction
Because of soaring gold prices, new dental substitute materials have been in extensive development since the early 1970s primarily to replace gold crowns [1]. Nevertheless, materials sold commercially to replace gold have generally created inferior clinical crowns for our patients [1]. Problems encountered with newer gold substitute materials are primarily related to clinically unacceptable marginal defect tolerances that have increased significantly from values down at about 39 micrometers common in the 1960s era for occlusal gold margins [2]. Although clinically acceptable interproximal and subgingival gold margin defects in the same era were much higher at 74 micrometers [2], current acceptable marginal defect tolerance standards range up toward about 120 micrometers [3–5]. Subsequent increases in marginal defects then create conditions that favor bacterial colonization to increase the probability of secondary decay [6] in addition to periodontal inflammation and possible bone loss [7–11].
Ceramic developments as gold substitute materials went forward with much enthusiasm when fused to metal as a prevalent preferred means to overcome inferior clinical restorative marginal results with non-noble metals primarily by furnishing patients with increased esthetics. Alternatively, newer computer-assisted design/computer-assisted manufacture (CAD/CAM) technology afforded the opportunity to examine advanced industrial-style ceramics and oxide ceramics like alumina and zirconia for dental crowns [1,12]. Nevertheless, current commercial CAD/CAM materials produce less accurate crown marginal outcomes than the 60s-era gold restorations [1].
Ceramics are extremely prone to detrimental brittle failures due to poor fracture-toughness properties [1,13] and with low energy adsorption are limited in structural applications [1,13]. In fact, ceramic materials have a tendency to break without any plastic deformation at yield equivalent to maximum strength and resilience equal to work of fracture (WOF) [1,13]. Ceramic cracks tend to grow from small microscopic flaws that act as stress concentrations when molecular bonds break between atoms in the crystalline lattice during moderately minor loading conditions [1,12–15]. Resulting ceramic stress concentrators then amplify loading forces as active locations for crack initiation [13–15]. When internal bonds break to generate crack growth, potential ceramic energy is released at much greater speeds than metals or extensively greater speeds than polymers reinforced with high-strength fibers [14]. Consequently, ceramic crack-forming energy can propel fracture completely through the material and generally into multiple pieces [1]. Conversely, fiber-reinforced composite [FRC] fibers act as major barriers to block crack propagation [1,12,14]. As a result, following critical or maximum load FRCs maintain parts in a whole state without full fracture through the material [1]. The critical stress intensity factor (KIc) can be calculated by Equations 1 and 2 so that the critical initiating crack at maximum load (a) can be determined as the length of a surface crack or half the crack length of an internal crack by Equation 3 [14].
| Equation 1: |
| Equation 2: |
| Equation 3: |
Where: E is the modulus, SIc is the critical strain energy release that describes rapid crack propagation after maximum load and σ is the maximum strength. Table 1 provides the minimum precision cut sample thickness without fracture and CAD/CAM ceramic material data [1,12] to calculate critical starter crack flaw length [14] from Equation 3.
Table 1:
Critical flaw size.
| CAD/CAM Ceramic Materials | Minimum Sample Thickness (mm) | Flexural Strength (MPa) [14] | KIc (MPa*m1/2) [14] | a (um) |
|---|---|---|---|---|
| Vita Mark II® |
0.74 (±0.01) |
103.8 (17.0) |
1.24 (0.25) |
45.5 (9.5) |
| ProCAD® Leucite |
1.16 (±0.20) |
129.7 (14.3) |
1.11 (0.14) |
25.6 (9.4) |
| InCeram® Spinel |
1.02 (±0.18) |
339.5 (16.1) |
1.94 (1.25) |
17.6 (4.6) |
| InCeram® Alumina |
0.86 (±0.19) |
314.0 (124.9) |
2.53 (0.43) |
23.7 (7.9) |
| InCeram® Zirconia |
1.06 (±0.29) |
248.6 (102.7) |
1.93 (1.01) |
18.8 (7.7) |
| Alumina Coors® |
0.82 (±0.30) |
231.8 (71.7) |
2.59 (1.20) |
37.9 (15.2) |
The high rate of ceramic bond-energy release reaches a surface critical flaw size for the minimum precision cut flexural sample thickness with complete crown fracture calculated between just 17.6 um and 45.5 um from the CAD/CAM ceramics in table 1. Alternatively, an internal critical crack length is calculated at twice the length of a surface crack between about 35.2 um and 91.0 um. Of major concern, ceramic flaws can grow slowly over time from less than applied maximum strength values to reach critical flaw size and fracture at much lower loads [13–15]. Conversely, FRCs now in CAD/CAM development are much stronger and extensively much tougher than ceramics [1,12]. Moreover, critical flaw size for an FRC is not of great concern following maximum load because high-strength fibers extensively block crack propagation so that fracture is contained to a large extent within the fiber network of multiple stacked woven plys. As a result, crack propagation does not proceed directly through an FRC part into multiple pieces like all brittle materials such as ceramics [1,16–18]. Consequently, common brittle ceramic failure from low fracture toughness now appears practically almost impossible clinically when examining an initial FRC crown fracture loading test average of 5118N [1]. By comparison, average maximum-bite-force recordings are exceedingly much lower from several literature sources: Maximum bite forces range from 200 – 540N, 400 – 800N, 600 – 1200N and an average of 700N; also by gender differences for a female average of 430 N or male average of 587 N; and ranges for females 340 – 391N or males 539 – 608N [15,19–25]. Decline in use of gold crowns for patients resulted in porcelain fused-to-metal [PFM] crown development as the new posterior standard [26] accepting non-nobel nickle chromium copings with ceramic overlays that fracture by delamination shear. Nonetheless, a non-precious PFM crown tested during protracted ceramic development for average maximum failure load at a lightly respectable 1494N [27] when compared to a CAD/CAM polymethylmethacrylate temporary crown maximum loading average of 1854N.
The FRC crown loading test average of 5118N with average crown marginal thickness of 1.09 mm [1] has produced average maximum forces at higher levels than monolithic yttrium-stabilized zirconia YZT crowns of 4550N that are approximately 3 times thicker and break into multiple fragments on fracture [1,28]. Previously fully sintered zirconia crowns were machined as copings over the abutment and then veneered with ceramic. But, ceramic veneers commonly chipped critically so that easily machined yttrium stabilized zirconia was subsequently introduced and then sintered after milling as a current monolithic material [28]. By better comparison, the higher-loaded FRC material axial wall thickness was close to about 10% of the average crown cross-sectional length whereas the YZT zirconia crown thickness was about l/3rd of the crown cross-sectional distance. In regard to the highest routine maximum crown loading, the type of ceramic or oxide ceramic material and ceramic thickness are both of great importance [29]. Also, for maximum crown loading a critical thickness at around 1.5 mm appears to greatly increase fracture resistance of silicate based ceramics [29] apparently by helping to reduce the influence of stress concentrators that propagate cracks from microscopic flaws [13,14].
Maximum CAD/CAM crown fracture loads are furnished to distinguish the FRC average load of 5118N with several monolithic crowns of varying thickness to include: Vita Zirconia YZT (4550N); Alumina InCeram (2717N); Lithium Disilicate e.max CAD (998N); polymer infiltrated feldspare ceramic (506N) and Feldspare ceramic Mark II (260N) [28]; and Everest F1PC ZrSiO4 Zircon [1622N and 1957N] [30]; Alternatively, several veneering systems tested by bridge-pontic flexural 3-point bend include: a Lava Zirconia fracture [1966N and 2581N] or Lava Zirconia with veneering ceramic delamination [928N or 1076N] [26,31]; and Procera Zirconia fracture [2071N] or Procera Zirconia with veneering ceramic delamination [415N] [26].
Ceramics based on silica (SiO2) have some bonding potential with resin cements [32,33]. But, oxide ceramics with low silica content like alumina and especially zirconia are extremely difficult to bond with resin cements [32–36]. Fortunately, FRCs have active polymer matrix sites for excellent free-radical covalent adhesive bonding with resin cements [1,12]. Cementation can greatly increase fracture resistance of weaker monolithic ceramics by supporting the space between the crown and the tooth [28]. Subsequent high contacts between a crown and tooth that create stress raisers to initiate crack propagation are removed by filling in space with cement [28]. However, cementation does not influence higher strength monolithic oxide ceramics like zirconia or alumina crown-fracture maximum loads [28]. Further, inert highly-crystalline zirconia does not allow etching with hydrofluoric acid to create a micromechanical bond [33,34,35]. Nevertheless, sandblasting of internal zirconia crown surfaces can provide micromechanical retention that in turn creates micro-crack defects to reduce strength [32,34,37].
Current work on CAD/CAM FRC gold-substitute material has been developed on standards created by the United States Department of Defense (DoD) based on Total Quality Management or TQM. Highly successful TQM practices were initially developed at the most demanding levels to protect our National Security. Consequently, TQM was soon introduced into important Industrial Complex areas of most vital interest. DoD Continuous Improvement or Cl principles have also been employed to ensure that the final CAD/CAM FRC dental crowns produced will meet all current requirements for Non-Significant Risk (NSR). Accordingly, the following improvements were developed with the initial preliminary CAD/CAM FRC material to meet requirements on NSR when comparing current standards for Food and Drug Administration (FDA) approved polymeric or ceramic materials used with dental crowns:
Increased FRC Strengths provide much higher maximum loads and are related to increased fracture toughness [1,12].
Greatly increased FRC Fracture Toughness properties eliminate problems with brittle ceramic catastrophic failures. Much higher fracture toughness properties in turn provide thinner crowns for less detrimental tooth reductions common with aggressive ceramic tooth preparations that may produce pain or pulpal exposure [1,12].
Lower FRC Modulus (approximately stiffness) more similar to dentin for better bone stress-transfer that becomes critical when using dental crowns over bone implants [1,12].
FRC aerotech materials adhesively bond well so that a marginal-crown reline has been extensively developed to ensure that the new FRC dental crowns will provide the lowest defect tolerances ever conceived for any crown [1,12]. Expected improvements include lower plaque retention with much less chance of secondary decay, gingival inflammation, and destructive periodontal gingival attachment involvement or bone loss. In addition, after proper crown seating to the prepared tooth, the new crown-margin reline can easily produce a tighter more retentive fit of the crown to the tooth.
Excellent FRC adhesive bonding [1,12] includes free-radical covalent bonding with resin luting cements. FRC adhesive bonding then also offers the convenience for fabricating a crown with an occlusal escape vent to relieve hydraulic cement pressures that prevent complete seating onto the tooth margin [38–40]. Subsequent filling of the vent hole can then be easily facilitated with high success using an advanced FRC molding compound [41–46].
FRC polymer matrices provide design options with specialty additives or resins to develop hydrophobic materials and the opportunity to incorporate the efficacious and hydrophobic Triclosan antimicrobial [47–49].
Acceptable FRC white esthetics are currently available for posterior crowns and matching tooth shades are being developed for anterior crowns [1,12].
Lower thermal FRC conductivity than metals or ceramic provides better protection to the dental pulp [13].
Patient time has been reduced with CAD/CAM technology and FRC quick machinability from the standard two-patient appointment down to a one-patient appointment [1,12]. Also, subsequent FRC CAD/CAM costs can be reduced for milling equipment considerably [1,12].
Biocompatible FRC polymer-matrix with estrogenic properties bestows highly significant tissue healing better than metal titanium [50–52].
For an unequaled pertinent NSR contrast, thermoplastic PEEK polymers are approved by the FDA for crowns, bridges, fixed-removal implant retained dental frameworks [53–55] and spinal fusion implants [56] with PEEK tensile strengths of only 70.3–103.5 MPa [57]. To distinguish exceptional improvement, the tensile strength on the lower flexural mechanical test side for the initial preliminary FRC crown material was an exceedingly much stronger 575.7 MPa [1,12]. In addition, the same FRC material greatly exceeded all seven of the commercial CAD/CAM ceramics or alumina and zirconia oxide ceramics initially tested for maximum strength [1,12]. Further, FRC fracture toughness properties for resilience (in kJ/m2), WOF (in kJ/m2) and KIc (in MPa*m1/2) tested correspondingly to one of the strongest solid materials known with tungsten carbide [1,12]. The same FRC even produced a much higher value than tungsten carbide for critical strain energy release (SIc) in common kJ/m2 fracture toughness units. Subsequent properties for SIc then measure resistance to unstable rapid crack propagation after critical maximum load [1,12].
Of concern to the National Academy of Sciences (NAS), all fracture toughness properties were accurately measured as requested by bulk-material testing without artificial man-made initiating cracks [1,12,14,17,58,59]. Multiple fracture toughness test methods for KIc have been used with different sample sizes, sample dimensions and testing fixtures so that comparative analysis between laboratories is a genuine concern due to differences in results of data, difficulty in the duplication of identical test procedures and even experimental inaccuracy making most KIc tests unreliable [58]. The NAS considers KIc testing with artificial cracks to be entirely undependable [1,12,14,17,59]. In fact, the NAS through an important ceramics-materials advisory board on high-temperature engines has even requested that limitations be imposed on reporting KIc data [59]. Of import, SIc is the fracture toughness property of most regard needed to calculate KIc scaled in the unusual units of MPa*m1/2 [1,14]. In turn, SIc can be obtained for accurate close repeatable results by NAS-requested bulk-material testing without artificial cracks [1,12,14,17,59]. Also, KIc supplies one other measurement advantage to calculate the comparative relative critical flaw size from Griffith Crack Theory as in table 1 [14].
In terms of the overall risk for FRCs, the probability of crown failure is greatly diminished and expected crown longevity extensively increased when comparing current ceramic or oxide ceramic crowns with the FRC crown. Therefore, the benefits far outweigh the possibilities of even the most-minor conceivable risks. Process control was initiated early in development to reduce small porosity in the final FRC part that could decrease detrimental water initiating defects and increase fiber bonding with the polymer matrix for increased stress transfer through the composite. In fact, with TQM and CI product development plans went forward with hydrophobic resins to reduce risks from water adsorption and polymer degradation that could reduce ultimate clinical crown mechanical properties and decrease crown longevity for patient clinical service. More recently shade esthetics have been worked on extensively to move the gold-substitute white posterior crowns forward to be used eventually for anterior teeth.
Marginal fit
Historically marginal adaptation has been one of the most important variables for dental crown success, but also one of the most common problems encountered in failure [8,11,60–63]. Location of the crown margin has been questioned in the past such that many studies show more gingival inflammation for subgingival margins compared to supragingival margins [8,64,65]. In the subgingival sulcus or intracrevicular crevice, open margins support bacterial microleakage with cement dissolution [10,11]. With increasing levels of marginal discrepancies, cement dissolution then increases [11,66]. Subsequent subgingival marginal defects are sources for periodontal tissue inflammation [10,11] that have generated significant heightened differences when comparing gap size with periodontal tissue inflammation, p < 0.001 [10]. Further, subgingival margin defect sizes are associated with bone loss [7,9]. In addition, margin overhangs are defective extensions of a restoration beyond the confines of the tooth margin and are consistently present to generally contribute toward the severity of bacterial plaque retention as a factor for gingivitis, periodontal disease and possibly periodontal attachment loss [67–74]. Bone loss increased in the presence of larger overhangs, p < 0.01 and a larger overhang defect appeared to increase the severity of the tissue disease [75,76]. Also, bacterial microleakage at a restorative margin noted from histopathology analysis contributes to pulpal inflammation [77]. The secondary decay that commonly originates from margins of a crown is due to marginal defects and plaque accumulation where plaque pH decreases as cariogenic bacteria such as Streptococcus mutans and Lactobacilli increase [6,78].
Regarding favorable recommendations for subgingival margins, extension of a margin into the gingival sulcus has been considered a preventive measure to reduce recurrent caries [64,79]. Scanning electron microscopy (SEM) imaging has presented observations for bacterial microorganism accumulations inside marginal gaps from 5 – 30 micrometers wide that are well below visual detection [80]. Therefore, excellence in the quality of fit and finish become a concern of more importance when considering margins placed subgingivally [81]. Many experienced clinicians comparing motivated patients from more well-controlled private practice environments to mostly dental school studies or VA hospitals agree that placement location of the margins had limited validity on periodontal gingival inflammation [82]. With excellence in the quality of fit and finish during more difficult placement of subgingival margins, similar gingival inflammation was seen when compared to supragingival margins or non-restored teeth [81,82]. Further, normal gingival capillary loop formation around full crowns indicated that proficient marginal adaptation was necessary combined with good oral hygiene [83]. Although supragingival margins are considered much easier to place, nevertheless subgingival margins are indicated for anterior facing esthetics, better retention for short clinical crowns, old restorations with subgingival margins and subgingival caries, erosion or abrasion [8,10,74,81]. However, crown margin defect gap sizes increase with longer walls and less taper of the prepared tooth [2].
Several other problems contribute to decreased sealing of the crown-tooth interface by gap defects at the margins of all crowns. Crown marginal openings increase with the film thickness of the luting cement [2,64] because of hydraulic forces contained inside the crown during seating [10,38,39,61,84,85]. In fact, marginal gaps increase significantly after cementation, p < 0.05 [30,40]. Possible cement exposure at the margin and excess extrusion into the gingiva have been considered a link to inflammation of the tissues [86]. To overcome difficult cement hydraulic pressures, the use of occlusal vent holes has been widely recommended and considered necessary to attain better seating of the crown with less margin discrepancies [38,39,40,64,86]. Venting has shown statistically significant improvement for marginal fit with zirconia copings, p < 0.05 [40]. Vented ceramic crowns seated statistically significantly better than non-vented crowns, p < 0.05 [87]. However, drilling vent holes into ceramic crowns has been shown to reduce fracture resistance [39]. Further, crowns seat better, faster and with less force when space is provided between the tooth and crown [84,88], whereas relief space is negatively related to crown retentive fit [88]. Subsequent marginal gaps between the cement layer and prepared tooth then create microleakage of fluids and bacteria [62]. Also, excess crown cement extruded into the surrounding tissues is associated with peri-implant disease of the soft tissue and progression into bone because of bacterial retention by cement [89].
Resin cements appear to aid in seating of a crown compared to the other cements tested that interfered with crown seating, p < 0.05 [87]. Microleakage has been known to be reduced with the resin cements [90], but still biodegradation of the resin-tooth interface increases bacterial microleakage [91]. In addition, some resins appear to release the common low-viscosity monomer triethylene-glycol-dimethacrylate [TEGDMA] that has even been shown to increase bacterial growth [92]. As the crown margin gap size increases, greater cement dissolution occurs with increasing secondary caries and loosening of the crown [66].
Photos are provided through previous interest in ceramic crown fractures (Figure 1). From a completely random selection of all other non-fractured crown areas imaged, note that all marginal interfaces show some light generalized gingival recession below the crown margins. Of importance, the patients were from a private practice under close supervision and instruction to provide excellent tissue health with no signs of any gingival inflammation.
Figure 1:
Generalized light gingival recession below crown margins. (A) Fracture of 2nd premolar crown with gingival recession of adjacent molar crown on left and premolar crown on right. (B) Fracture of cuspid crown with apical gingival recession and gingival recession on both bicuspid crowns to the left and lateral incisor crown on right. (C) Fracture of lateral incisor with apical gingival recession and gingival recession on central incisor crown to the right. (D) Fracture of central incisor crown with apical gingival recession and gingival recession on central incisor crown to the right.
Plaque accumulation in margin defects
Clinical quality of the margin especially with significant large discrepancies between the crown and tooth can be compared as a measure for plaque accumulation, bacterial adhesion and microbial retention [93]. Plaque growth is a major etiologic basis for caries and periodontal disease [64,94–98]. Plaque is observed with increasing concern when comparing visually observable pit and fissures to smooth enamel surfaces [99–101]. Occlusal surfaces with deeply irregular invaginations generally about 0.1 mm wide [100] represent approximately 13% of all tooth surfaces [102], but caries occurs most frequently in pit and fissures at a rate eight times greater than on smooth surfaces [100,101]. Initial bacterial colonization of tooth surfaces occurs in uneven surface irregularities, pits and fissure grooves that shelter bacteria from detachment forces [99,103–107]. Even on the lingual surface, detachment-shearing forces of the tongue could not prevent bacterial colonization of dental material test samples in microgrooves of only a few micrometers that provide subsequent time to promote bacteria adhesion [103]. The pit and fissure sealant was developed by Buonocore and commercialized in 1971 as a liquid material that would fill into deep occlusal pits and fissures to create a protective layer capable of preventing bacterial colonization and caries initiation. The liquid sealant could be either chemically cured or photocured after acid etching as a mechanically bonded caries preventive overlay [108]. Since then pit and fissure sealant coatings have proven considerably effective in preventing pit and fissure caries by making deep occlusal surface irregularities inaccessible for plaque accumulation [102,108]. By similar argument, bacterial attachment and plaque growth necessary for caries initiation and periodontal disease can be several hundred cells thick [98] to emphasize the need for reducing current accepted marginal gap tolerances that now extend upward to about 120 um [3,4].
Surface roughness and bacterial adhesion
At a more refined level, surface roughness (Ra) measured in single digit micrometers down to 100 nanometers is associated with bacterial adhesion and colonization accompanied by subsequent biofilm growth and plaque retention [104–111]. Bacterial colonization of subgingival surfaces is higher on rougher surfaces than smoother surfaces [104–107]. Resultant higher Ra accordingly protects bacteria from shearing forces to promote biofilm-plaque formation [107]. Microbial colonization has been shown to significantly increase with increasing Ra, p < 0.05 [112]. Further, dental oral plaque has been shown to significantly increase with increasing Ra, p < 0.05 [113]. A lower Ra along the marginal line may prevent secondary caries, staining, plaque accumulation and periodontal inflammation [110]. In addition, with increasing Ra escalating growth of the plaque biofilm is a major factor in periodontal disease [110].
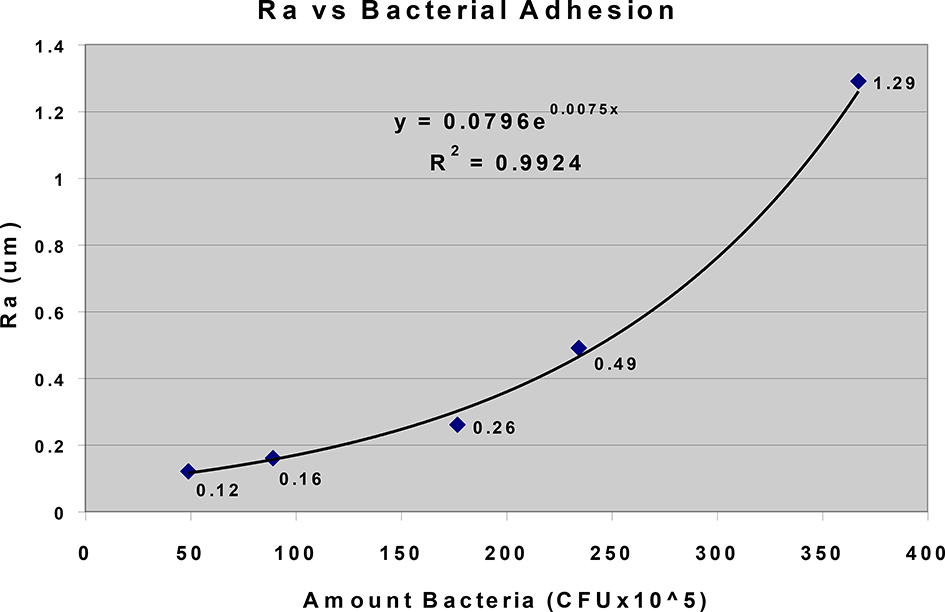
Amount bacterial adhesion increased with accelerating Ra that was documented by Kamonwanon., et al. [111]. In fact, Ra from 0.12 um to 1.29 um could explain 99% of the variability for the amount of bacterial adherence measured in colony forming units (CFU) using an exponential regression with the coefficient of variability (R2) = 0.99 (Figure 2). On the other hand, R2 = 0.87 for the linear regression. The lower threshold limit for bacterial adhesion extrapolates toward about 0.10 um. However, others have considered the lower threshold limit for bacterial adhesion and plaque growth on supragingival and subgingival surfaces to be an Ra of 0.2 um [104–106]. Subsequent increasing Ra above 0.2 um was then associated with increasing periodontal inflammation and caries [104–106].
Figure 2:
Chart with exponential regression demonstrates that 99% of the variability for Amount Bacteria Adhesion is explained by increasing Ra with a lower threshold limit approaching approximately 0.10 um (data from Kamonwanon., et al. [111]).
As a strong exponential regression, data in figure 2 appear to be related through association as a corollary of the Marcus Theory for electron transfer by the outer valence electrons during covalent bonding [114]. However instead, weak secondary bonding forces by bacterial fimbriae or appendages increase bacterial adhesion amounts with the increasing surface areas available by exponentially increasing Ra. But, an upper limit for bacterial growth somewhere above 400 × 105 CFUs at a much higher Ra appears to occur due to a restriction on the amount of available space also with some possible negative metabolic toxic effects.
Other data in past laboratory testing obtained for Marcus Theory observation includes outer-valence covalent exponential increasing reaction rates with increasing cross-linking free-radical concentrations, R2 = 1.00 whereas in the linear regression R2 = 0.76 [115]. Further, increasing overall covalent polymerization shrinkage that plateaus by natural logarithmic growth over time as reactants are consumed gave multiple R2 values between 0.94 to 0.99 whereas linear regressions produced much lower R2 values from 0.77 to 0.88 respectively [115]. Conventional stabilized electron covalent-bond pairing indicates attraction forces between individual electron species with electron surface interactions could indeed form exponential or natural logarithmic relationships as active electron-species concentrations increase or are consumed within a reaction environment. Also, electron interactions with secondary-bonding environments occur when bacteria are forming initial bond-adhesion attachments with the substrate material. From a practical standpoint, increasing bacterial adhesion with exponential increasing Ra suggests that efforts to eliminate rough surfaces and instead create smoothest surfaces toward the lower threshold limits could be invaluable in future biomaterials development. Further, as biomaterial surfaces possibly roughen over time, the importance of interventional clinical surface smoothing should be considered by conventional polishing methods.
Surface free energy interaction
The initial bacterial surface adhesion occurs by secondary weak van der Waals forces-of-attraction at distances of approximately 50 nm [104–107]. Subsequent weak bacterial binding occurs at about 10–15 nm from the surface [105]. Extracellular bacterial filamentous fimbriae appendages most likely less than 50 nm in diameter are more susceptible to van der Waals forces at smaller sizes. Fimbriae appendages then form stable attachments with adhesion molecules that are generally glycoproteins or lipoproteins [98,105]. An increase in the surface free energy (SFE) attracts more microorganisms with a high-binding force [116], increases the adhesion of microorganisms [117] and increases biofilm formation [107]. Increasing SFE increases surface hydrophilic water-loving interactions that are termed polar with unequal molecular charge distributions [98]. Water has a negative charge on the oxygen region and positive charge on the hydrogen region to act as a solvent toward dissociating polar molecules like salts and act in reactions with hydrogen ions and hydroxide ions [98]. A water surface layer is considered essential to promoting bacterial life [98]. On the other hand, the bacterial appendages are hydrophobic so that water removal dehydrates the substrate surface [104,107,118] for irreversible attachment by covalent, ionic or hydrogen bonding [107,118]. Conversely overall, hydrophobic or nonpolar surfaces that represent lower SFEs can reduce bacterial adhesion and plaque biofilm accumulation [111,117,119,120]. But, a higher SFE then creates a polar water surface layer needed for bacterial life-sustaining survival [98]. In fact, under conditions of desiccation with low SFE microorganisms cannot grow or reproduce [98].
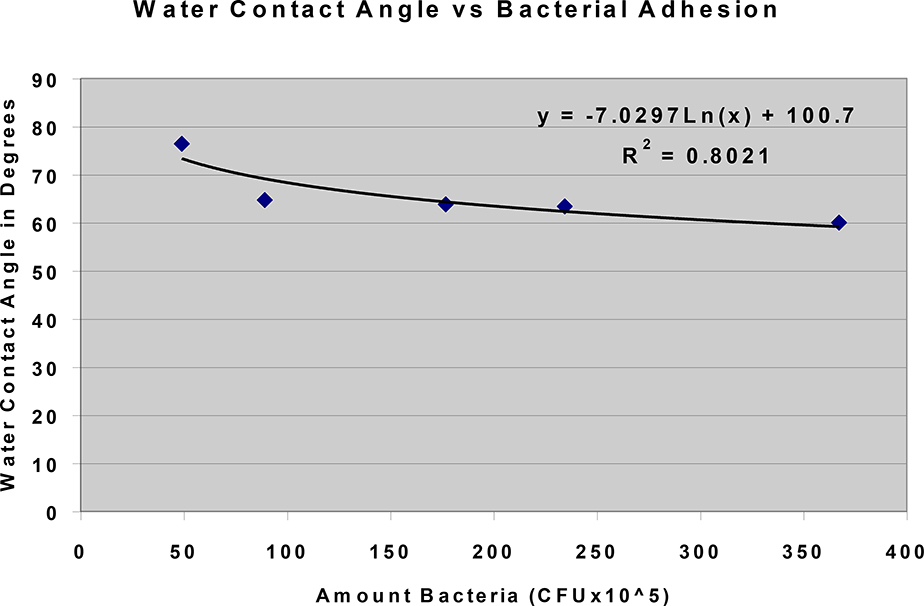
Bacterial adhesion that increased with decreasing water contact angle measurements was documented by Kamonwanon., et al. [111] (Figure 3). By some possible association in relation to figure 2 for amount bacterial adhesion with a lower Ra threshold of 0.1 um, a surface Ra less than 0.1 um has no effect on increasing the water contact angle for a more hydrophobic lower SFE [107]. Water contact angle is considered a sign of the energy between the water and substrate surfaces where an angle larger than 90 degrees suggests the surface is hydrophobic [111]. In fact, lowering water contact angle as a relationship with higher SFE could explain 80% of the variability for the amount of bacterial adherence measured in CFUs using a natural log regression, R2 = 0.80 (Figure 3). In contrast, R2 = 0.63 for the linear regression. In other testing, a separate Marcus Theory corollary provided alternate data with natural log associations for weak secondary resin bonding/chain entanglements between lowering viscosities and increasing amounts of resin diluent monomer R2 = 0.92 and 0.99 [121]. On the other hand, linear regressions were R2 = 0.47 and 0.67 respectively [121]. Weak attraction forces by electron surface interactions increase with a polar molecule like water [98]. In turn, large electron surface interactions with high SFEs decrease with hydrophobic water-repelling materials. Because small decreases in water contact angle below 70 degrees greatly increase amounts of bacterial adhesion (Figure 3), the need for use of nonpolar or hydrophobic materials with low SFEs to reduce bacterial attachments is emphasized for future biomaterials development. However, when moving toward more hydrophobic materials some balance is needed for the provision of sufficient electron interactions with FRC bonding active sites and the crown reline material to eliminate critical marginal defects. Further, active FRC bonding sites are needed for the final luting cementation to secure the crown with superior tooth-crown retention.
Figure 3:
Chart with natural log regression demonstrates that 80% of the variability for Amount Bacteria Adhesion is explained by decreasing Water Contact Angle as a measurement for the relationship with higher SFE or more hydrophilic material (data from Kamonwanon., etal. [111]).
Gingivitis and periodontal disease
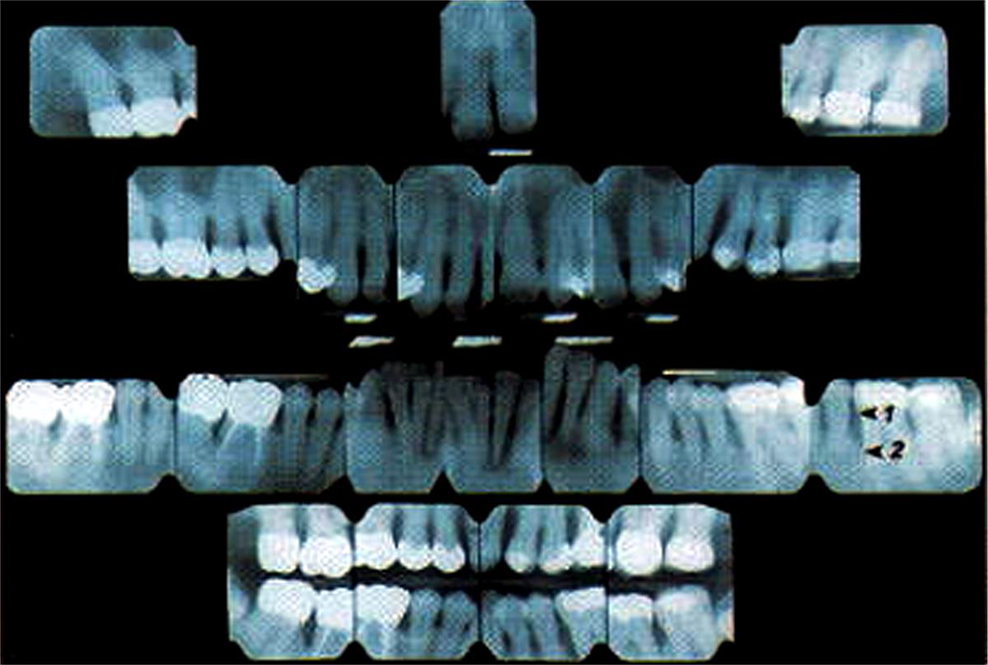
Bacterial attachment and plaque growth necessary for caries initiation and periodontal disease [64,68–71,73–76,94–98] with association to retentive irregular rough restorative surfaces [68–71,73–76,94] highlight the need for eliminating marginal gap tolerances that can promote microorganism biofilm. The critical area of any crown margin defect with plaque accumulation is particularly susceptible to release of bacterial toxins into the gingival tissues. Bacterial toxins can then cause an inflammation as gingivitis with bleeding during brushing [98]. Gingivitis can advance to periodontitis where toxins degrade tissue and force the gingiva to recede [98]. Further, bacterial toxins can eventually destroy bone to form pockets surrounding the teeth [98], x-rays (Figure 4). The junctional epithelium is in contact with the tooth surface to form a barrier between the bottom of the gingival sulcus and the periodontal soft tissues with underlying bone [122,123]. The conversion of the junctional epithelium to defective pocket epithelium may not provide an effective barrier seal to bacteria [122,123]. Subsequent loss of the junctional epithelium intercellular barrier seal is then a penetrating stage in periodontal pocket formation and highly associated with the assault of bacteria and toxins related to plaque build up [122,123].
Figure 4:
Radiographic appearance of a 57-year-oid patient with generalized advanced chronic periodontitis, generalized bone loss ranging from 15 to 100%. 1, expected location of alveolar bone height in health; 2, actual alveolar bone height demonstrating ~60% bone loss (Authored and published by the National Center for Biotechnology Information).
Human gingival epithelium keratinocytes cultured on smooth substrates with Ra = 121.3 ± 13.4 nm developed tight intercellular junctions [123]. However, human gingival epithelium keratinocytes cultured on rougher substrates with Ra values in the 500 – 800 nm ranges formed wide intercellular gaps that can increase rapid destruction of the cell junction during periods of calcium deficiency [123]. Further, deficient junctional epitheliums develop less stable barriers to bacterial penetration on rougher surfaces and are more susceptible to host inflammatory defenses [123]. Therefore, Ra values surrounding the crown marginal line in the submicron range potentially have the ability to adversely influence the development of an ineffective protective junctional epithelium barrier that is more susceptible to periodontal disease during excessive plaque biofilm growth. Subsequent proteolytic bacterial enzymes entering the junctional epithelium may then start pocket formation to provide access for bacteria that can penetrate deeper into tissue toward more well-developed periodontal disease and possible bone loss [122,123]. On the other hand, smoother surfaces are considered to be a more biocompatible environment for reducing bacterial adhesion or inflammation in the periodontal ligament and better increase fibroblast attachment [96].
F-actin lies beneath the plasma cell membrane that supplies high modulus intracellular fiber structural support to increase cell stiffness [124–126], However, tight gingival intercellular junctions were suppressed increasingly on rough surfaces where f-actin did not disassemble to allow pliable cell spreading [123]. Conversely, f-actin disappeared in the areas of cell membrane lamellipodia extension development on smooth surfaces to allow high levels of filipodia formation with tight junctional epithelium and no intercellular gaps [123]. Subsequent filipodia are small membrane focal adhesion proteins thought to provide cell mobility by bond formation with bond contractions at the leading edge of the cell [124–126]. In turn, adhesive filopodia proteins would be inclined to promote tight junctional epithelium barrier seals by forming adhesive covalent or secondary bonds between cells and with the tooth surface.
Normal cells have relatively smoother more-even round membranes with smooth nuclei compared to cancer cells that reflect free-radical oxidative stress with uneven distorted borders, membrane ruffling and irregularly shaped nuclei [124–126]. As a possible related interest, in cancer cells f-actin also disassembles intracellularly under the plasma cell membrane to create a highly pliable cell with low modulus that can squeeze between narrow gaps like openings in the blood vessel endothelium [124–126]. Low-modulus flexible cancer cells may possibly represent progressive free-radical disease related to creating intercellular membrane contacts that form smooth even interactions to disassemble f-actin. Nevertheless, unsaturated membrane lipids cross-linked during free-radical oxidative stress need invagination of the rounder cell membrane as bonds contract to create the distorted uneven cancer cell membrane [124–126]. Further, during metastasis intracellular f-actin fibers in cancer cells reorganize by free-radical polymerization to form spike-like stiff membrane extensions that can apply leverage between gaps to force narrow intercellular openings further apart toward invasive cell movement into adjacent tissue [124–126].
Conclusion
Altogether, the crown FRC margin relines have the potential to supply essentially near zero-gap defects with smooth flush surfaces accompanied by low Ra and low SFE hydrophobic surfaces providing ideal plaque detachment removal in addition to preventing bacterial attraction and bacterial adherence. FRC margin reline material has been extensively advanced to ensure that the new FRC dental crowns will provide the lowest defect tolerances and smoothest margins ever conceived for any crown [1,12]. TQM and CI practices are constantly employed toward hydrophobic and crystalline materials that do not attract or retain microorganisms. Further, nonpolar triclosan has been under intensive development in polymer matrix FRCs as a highly efficacious hydrophobic antimicrobial that entangles into the polymer chain for long-term retention with effective mechanomolecular surface vibrations to interfere with bacterial adhesion and cell division [47–49]. With expected FRC crown marginal improvements, clinical benefits include lower plaque retention with much less chance of secondary decay, gingival inflammation, and destructive periodontal gingival attachment involvement or bone loss. In addition, after proper crown seating to the prepared tooth, with a bonded margin reline a tighter more retentive fit of the crown to the tooth can be easily achieved. Further, FRCs have exceptional fracture toughness properties where critical flaw size is not of great concern following maximum load because high-strength fibers extensively block crack propagation. Consequently, FRC fracture is constrained largely within the woven fiber network. As a result, crack propagation does not proceed directly through a part into multiple pieces like all brittle materials such as ceramics. In fact, brittle ceramic failure from low fracture toughness now appears practically impossible when comparing the FRC crown fracture maximum loading test average of 5118N that is extensively well above all average maximum bite force recordings published in a range from 200 – 1200N.
Acknowledgements
Support in part from funding through the National Institutes of Health grant numbers T32DE07042 and T32DE014300.
Abbreviations
- CAD/CAM
Computer Assisted Design/Computer Assisted Manufacture
- FRCs
Fiber-Reinforced Composites
- KIc
Critical Stress Intensity Factor
- a
Critical Initiating Crack as the Length of a Surface Crack or Half the Crack Length of an Internal Crack
- SIc
Critical Strain Energy Release
- WOF
Work of Fracture
- PFM
Porcelain Fused-To-Metal
- DoD
Department of Defense
- TQM
Total Quality Management
- CI
Continuous Improvement
- NSR
Non-Significant Risk
- FDA
Food and Drug Administration
- NAS
National Academy of Sciences
- SEM
Scanning Electron Microscopy
- TEGDMA
Triethylene-Glycol-Dimethacrylate
- Ra
Surface Roughness
- SFE
Surface Free Energy
- CFU
Colony Forming Units
- R2
Coefficient of Variability
Footnotes
Conflict of Interest
Authors declare no conflicts of interest.
Bibliography
- 1.Petersen RC., et al. "Fiber-reinforced composites for computer assisted design/computer assisted manufacture of dental crowns". EC Dental Science 18.7 (2019): 1654–1672. [Google Scholar]
- 2.Christensen GJ. "Marginal fit of gold inlay castings". Journal of Prosthetic Dentistry 16.2 (1966): 297–305. [DOI] [PubMed] [Google Scholar]
- 3.Beuer F., et al. "Marginal and internal fits of fixed dental prostheses zirconia retainers". Dental Materials 25 (2009): 94–102. [DOI] [PubMed] [Google Scholar]
- 4.Vojdani M., et al. "Comparison the marginal and internal fit of metal copings cast from wax patterns fabricated by CAD/CAM and conventional wax up techniques". Journal of Dentistry, Shiraz University of Medical Sciences 14.3 (2013): 118–129. [PMC free article] [PubMed] [Google Scholar]
- 5.Ha S-J and Cho J-H. "Comparison of the fit accuracy of zirconia-based prostheses generated by two CAD/CAM systems". Journal of Advanced Prosthodontics 8 (2016): 439–448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tanaka J., et al. "Relationship between cariogenic bacteria and pH of dental plaque at margin of fixed prostheses". International Journal of Dentistry Volume 2012 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bjorn AL., et al. "Marginal fit of restorations and its relation to periodontal bone level". Odontologisk Revy 21.3 (1970): 337–346. [PubMed] [Google Scholar]
- 8.Gardner FM. "Margins of complete crowns-Literature review". Journal of Prosthetic Dentistry 48.4 (1982): 396–114. [DOI] [PubMed] [Google Scholar]
- 9.Sorenson SE., et al. "Gingival and alveolar bone reaction to marginal fit of subgingival crown margins". Scandinavian Journal of Dental Research 94 (1986): 109–114. [DOI] [PubMed] [Google Scholar]
- 10.Felton DA., et al. "Effect of in vivo crown margin discrepancies on periodontal health". Journal of Prosthetic Dentistry 65 (1991): 357–364.. [DOI] [PubMed] [Google Scholar]
- 11.Riccitiello F., et al. "In vitro evaluation of the marginal fit and internal adaptation of Zirconia and Lithium Di-silicate single crowns: Micro-CT comparison between different manufacturing procedures". The Open Dentistry Journal 12 (2018): 160–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Petersen RC and Liu P-R. "3D-woven fiber-reinforced composite for CAD/CAM dental application". Society for Advanced Materials and Process Engineering, Sampe Journal (2016). [PMC free article] [PubMed] [Google Scholar]
- 13.Callister WD Jr. Brittle Fracture of Ceramics pages 397–399; Appendix Table C.7 Thermal Conductivity pages 791–793. Materials Science and Engineering 4th Edition. New York: John Wiley and Sons, Inc, (1997): 13.7. [Google Scholar]
- 14.Petersen RC. "Accurate critical stress intensity factor Griffith crack theory measurements by numerical techniques". Society for the Advancement of Material and Process Engineering. SAMPE 2013 Proceedings. Long Beach, California. (2013): 737–752. [PMC free article] [PubMed] [Google Scholar]
- 15.Anusavice KJ., et al. "Chapter 21 Dental Ceramics". In: Phillips' Science of Dental Materials 11th edition. St. Louis: Elsevier Saunders. (2003): 655–719. [Google Scholar]
- 16.Petersen RC., et al. "Stress-transfer micromechanics for fiber length in a photocure vinyl ester composite". Polymer Composites 27 (2006): 153–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Petersen RC., et al. "Fracture toughness micromechanics by energy methods with a photocure fiber-reinforced composite". Polymer Composites 28 (2007): 311–324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Petersen RC., et al. "Micromechanics for fiber volume percent with a photocure vinyl ester composite". Polymer Composites 28 (2007): 294–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Attia A and Kern M. "Fracture strength of all-ceramic crowns luted using two bonding methods". Journal of Prosthetic Dentistry 91 (2004):247–252. [DOI] [PubMed] [Google Scholar]
- 20.Baig MR., et al. "Evaluation of the marginal fit of a zirconia ceramic computer-aided machined (CAD) crown system". Journal of Prosthetic Dentistry 104 (2010):216–227. [DOI] [PubMed] [Google Scholar]
- 21.Zhang Y., et al. "Edge chipping and flexural resistance of monolithic ceramics". Dental Materials 29.12 (2013): 1201–1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Peck CC. "Biomechanics of occlusion-implications for oral rehabilitation". Oral Rehabilitation 43 (2016): 205–214. [DOI] [PubMed] [Google Scholar]
- 23.Ferrario VF., et al. "Maximal bite forces in healthy young adults as predicted by surface electromyography". Journal of Dentistry 32 (2004): 451–457. [DOI] [PubMed] [Google Scholar]
- 24.Calceron PdS., et al. "The influence of gender and bruxism on the human maximum bite force". Journal of Applied Oral Science 14.6 (2006): 448–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pereira-Cenci T et al. "Maximal bite force and its association with temporomandibular disorders". Brazilian Dental Journal 18.1 (2007): 65–68. [DOI] [PubMed] [Google Scholar]
- 26.Lopez-Suarez C., et al. "Fracture resistance and failure mode of posterior fixed dental prostheses fabricated with two zirconia CAD/ CAM systems". Journal of Clinical and Experimental Dentistry 12 (2015): e250–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Probster L. "Compressive strength of two modern all-ceramic crowns". International Journal of Prosthodontics 5.5 (1992): 409–414. [PubMed] [Google Scholar]
- 28.Rohr N., et al. "Correlations between fracture load of zirconia implant supported single crowns and mechanical properties of restorative material and cement". Dental Materials Journal 37.2 (2018): 222–228. [DOI] [PubMed] [Google Scholar]
- 29.Zimmermann M., et al. "Influence of material thickness on fractural strength of CAD/CAM fabricated ceramic crowns". Dental Materials Journal 36.6 (2017): 778–783. [DOI] [PubMed] [Google Scholar]
- 30.Okutan M., et al. "Fracture load and marginal fit of shrinkage-free ZrSiO4 all-ceramic crowns after chewing simulation". Journal of Oral Rehabilitation 33 (2006): 827–832. [DOI] [PubMed] [Google Scholar]
- 31.Lopez-Suarez C., et al. "Comparative fracture behavior of monolithic and veneered zirconia posterior fixed dental prostheses". Dental Materials Journal 36.6 (2017): 816–821. [DOI] [PubMed] [Google Scholar]
- 32.Li RWL., et al. "Ceramic dental biomaterials and CAD/CAM technology: State of the art". Journal of Prosthodontic Research 58 (2014): 208–216. [DOI] [PubMed] [Google Scholar]
- 33.Luthra R and Kaur P. "An insight into current concepts and techniques in resin bonding to high strength ceramics". Australian Dental Journal 61 (2016):163–173. [DOI] [PubMed] [Google Scholar]
- 34.Wang C., et al. "Bonding of resin cement to zirconia with high pressure primer coatings". PLOS ONE 9.7 (2014): 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kasraei S., et al. "Bond strength of resin cement to Co2 and Er:YAG laser-treated zirconia ceramic". Restorative Dentistry and Endodontics 39.4 (2014): 296–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bona AD., et al. "Zirconia as a dental biomaterial". 8 (2015): 4978–4991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yin L et al. "A review of engineered zirconia surfaces in biomedical applications". Procedia CIRP 65 (2017): 284–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fusayama T., et al. "Relief of resistance of cement of full cast crowns". Journal of Prosthetic Dentistry 14 (1964): 95–105. [Google Scholar]
- 39.Sallustio FW., et al. "The effect of venting on the strength of Dicor and Hi-Ceram ceramic crowns". The International Journal of Prosthodontics 5.5 (1992): 463–468. [PubMed] [Google Scholar]
- 40.Habib SR., et al. "Effect of cementation, cement type and ventholes on fit of zirconia coping". Saudi Dental Journal 31 (2019): 45–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Petersen RC., et al. "Fiber-reinforced composites: A breakthrough in practical clinical applications with advanced wear resistance for Dental Materials". EC Dental Science 17.5 (2018): 430–459. [PMC free article] [PubMed] [Google Scholar]
- 42.Petersen RC. "Important dental fiber-reinforced composite molding compound breakthroughs". EC Dental Science (2017): 52–58. [PMC free article] [PubMed] [Google Scholar]
- 43.Petersen RC., "Advancing discontinuous fiber-reinforced composites above critical length for replacing current dental composites and amalgam". Journal of Nature and Science 3.2 (2017): e321. [PMC free article] [PubMed] [Google Scholar]
- 44.Petersen RC and Perng-Ru Liu. "Mechanical properties comparing composite fiber length to amalgam ". Journal of Composites 2016 (2016): 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Petersen RC. "Discontinuous fiber-reinforced composites above critical length" Journal of Dental Research 84.4 (2005): 365–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Petersen RC and Wenski EG. "Mechanical testing of a photocured chopped fiber-reinforced composite”. Society for Advanced Materials and Process Engineering, SAMPE 2002 Affordable Materials Technology-Platform to Global Value and Performance, Long Beach (2002): 380–395. [Google Scholar]
- 47.Petersen RC. "Computational conformational antimicrobial analysis developing mechanomolecular theory for polymer biomaterials in Materials Science and Engineering". International Journal of Computational Materials Science and Engineering 3.1 (2014): 48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Petersen RC. "Triclosan computational conformational chemistry analysis for antimicrobial properties in polymers". Journal of Nature and Science 13 (2015): e547. [PMC free article] [PubMed] [Google Scholar]
- 49.Petersen RC. "Triclosan antimicrobial polymers". AIMS Molecular Science 3.1 (2016): 88–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Petersen RC. "Carbon fiber biocompatibility for implants". Fibers 4.1 (2016): 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Petersen RC. "Titanium implant osseointegration problems with alternate solutions using epoxy/carbon-fiber-reinforced composite". Metals 4.1 (2014): 549–569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Petersen RC. "Bisphenyl-polymer/carbon-fiber-reinforced composite compared to titanium alloy bone implant". International Journal of Polymer Science Polymeric Biomaterials for Tissue Engineering Applications annual focus/special issue (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Jarman-Smith M. "Advantages of PEEK dental prosthetic frameworks over metal". Invibio Biomaterial Solutions INSIDER Annually (2017): 22–23. [Google Scholar]
- 54.Jarman-Smith M and Siewert B. "A retrospective, single centre clinical evaluation using PEEK frameworks for full arch implant supported prosthetics". Invibio Biomaterial Solutions INSIDER Annually (2017): 24–25. [Google Scholar]
- 55.Jarman-Smith M. "Changing the face of prosthetic dentistry". Invibio Biomaterial Solutions INSIDER Annually (2017): 26–27. [Google Scholar]
- 56.Valentine C "FDA reclassification paves regulatory pathway for Invibio PEEK-Optima spinal rods". Invibio Biomaterial Solutions INSIDER Annually (2017): 14–15. [Google Scholar]
- 57.Callister WD. "Materials Science and Engineering 4th edition". John Wiley and Sons, New York: (1997): appendix c Table C.4: 785. [Google Scholar]
- 58.Quinn GD. "Fractographic analysis and the Army flexure test method". Advances in Ceramics 22 (1988): 319–333. [Google Scholar]
- 59.Bortz S. National Materials Advisory Board. "Reliability of ceramics for heat engine applications". Chapter 4 Materials Characterization. National Academy of Sciences, Washington DC: (1980): 445–473. [Google Scholar]
- 60.Rosner D. "Function, placement, and reproduction of bevels for gold castings". Journal of Prosthetic Dentistry 13.6 (1963): 1160–1166.. [Google Scholar]
- 61.Moore JA., et al. "Marginal distortion of cast restorations induced by cementation". Journal of Prosthetic Dentistry 54.3 (1985): 336–340.. [DOI] [PubMed] [Google Scholar]
- 62.Medic V., et al. "In Vitro evaluation of microleakage of various types of dental cements". Srpski Arhiv Za Celokupno Lekarstvo 138.3–4 (2010): 143–149. [DOI] [PubMed] [Google Scholar]
- 63.Contrepois M., et al. "Marginal adaptation of ceramic crowns: A systematic review". Journal of Prosthetic Dentistry 110 (2013):447–454.. [DOI] [PubMed] [Google Scholar]
- 64.Paloma F and Peden J. "Periodontal considerations of restorative procedures". Journal of Prosthetic Dentistry 36.4 (1976): 387–394. [DOI] [PubMed] [Google Scholar]
- 65.Silness J. "Fixed prosthodontics and periodontics". Dental Clinics of North America 24.2 (1980): 317–329. [PubMed] [Google Scholar]
- 66.Jacobs MS and Windeler AS. "An investigation of dental luting cement solubility as a function of the marginal gap". Journal of Prosthetic Dentistry 65.3 (1991): 436–442. [DOI] [PubMed] [Google Scholar]
- 67.Than A., et al. "Relationship between restorations and the level of the periodontal attachment". Journal of Clinical Periodontology 9.3 (1982): 193–202. [DOI] [PubMed] [Google Scholar]
- 68.Lang NR, et al. "Clinical and microbiological effects of subgingival restorations with overhanging or clinically perfect margins". Journal of Clinical Periodontology 10 (1983): 563–578. [DOI] [PubMed] [Google Scholar]
- 69.Chen J-TJ., et al. "Periodontal attachment loss asociated with proximal tooth restorations". Journal of Prosthetic Dentistry 57.4 (1987): 416–420. [DOI] [PubMed] [Google Scholar]
- 70.Brunsvold MA and Lane JJ. "The prevalences of overhanging dental restorations and their relationship to periodontal disease". Journal of Clinical Periodontology 17.2 (1990): 67–72. [DOI] [PubMed] [Google Scholar]
- 71.Kells BE and Linden GJ. "Overhanging amalgam restorations in young adults attending a periodontal department". Journal of Dentistry 20 (1992): 85–89. [DOI] [PubMed] [Google Scholar]
- 72.Axelsson P. "New ideas and advancing technology in prevention and nonsurgical treatment of periodontal disease". International Dental Journal 43.3 (1993): 223–238. [PubMed] [Google Scholar]
- 73.Jansson L., et al. "Proximal restorations and periodontal status". Journal of Clinical Periodontology 21.9 (1994): 577–582. [DOI] [PubMed] [Google Scholar]
- 74.Padbury A Jr., et al. "Interactions between the gingiva and the margin of restorations". Journal of Clinical Periodontology 30 (2003): 379–385. [DOI] [PubMed] [Google Scholar]
- 75.Gilmore N and Sheiham A. "Overhanging dental restorations and periodontal disease". Journal of Periodontology 42.1 (1971): 8–12. [DOI] [PubMed] [Google Scholar]
- 76.Jeffcoat MK and Howell TH. "Alveolar bone destruction due to overhanging amalgam in periodontal disease". Journal of Periodontology 51.10 (1980): 599–602. [DOI] [PubMed] [Google Scholar]
- 77.Bergenholtz G., et al. "Bacterial leakage around dental restorations: Its effect on the dental pulp". Journal of Oral Pathology 11 (1982): 439–450. [DOI] [PubMed] [Google Scholar]
- 78.Kohler B and Hager B. "Influence of salivary levels of mutans streptococci on colonization of crown margins: A longitudinal study". Journal of Prosthetic Dentistry 69 (1993): 524–528. [DOI] [PubMed] [Google Scholar]
- 79.Karlsen K. "Gingival reactions to dental restorations". Acta odontologia Scandinavica 28.6 (1970): 895–904. [DOI] [PubMed] [Google Scholar]
- 80.Saltzberg DS., et al. "Scanning electron microscope study of the junction between restorations and gingival cavosurface margins". Journal of Prosthetic Dentistry 36.5 (1976): 517–522. [DOI] [PubMed] [Google Scholar]
- 81.Richter WA and Ueno H. "Relationship of crown margin placement to gingival inflammation". Journal of Prosthetic Dentistry 30.2 (1973): 156–161. [DOI] [PubMed] [Google Scholar]
- 82.Koth DL. "Full crown restorations and gingival inflammation in a controlled population". Journal of Prosthetic Dentistry 48.6 (1982): 681–684. [DOI] [PubMed] [Google Scholar]
- 83.Maruyama T., et al. "Morphology of gingival capillaries adjacent to complete crowns". Journal of Prosthetic Dentistry 35.2 (1976): 179–184. [DOI] [PubMed] [Google Scholar]
- 84.Patel MG. "The effect of electrochemical milling on margins of MOD inlays". Journal of Prosthetic Dentistry 23 (1973): 66–73. [DOI] [PubMed] [Google Scholar]
- 85.Webb EL., et al. "Effects of preparation relief and flow channels on seating full coverage castings during cementation". Journal of Prosthetic Dentistry 49.6 (1983): 777–780. [DOI] [PubMed] [Google Scholar]
- 86.Rodriquez LC., et al. "A finite element analysis of novel vented dental abutment geiometries for cement-retained crown restorations", Clinical and Experimental Dental Research 2.2 (2016): 136–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Clark MT., et al. "Seating accuracy and fracture strength of vented and nonvented ceramic crowns luted with three cements". Journal of Prosthetic Dentistry 74.1 (1995): 18–24. [DOI] [PubMed] [Google Scholar]
- 88.Carter SM and Wilson PR. "The effects of die-spacing on post-cementation crown elevation and retention". Australian Dental Journal 42.3 (1997): 192–198. [DOI] [PubMed] [Google Scholar]
- 89.Wilson TG. "The positive relationship between excess cement and peri-implant disease: a prospective clinical endoscopic study". Journal of Periodontology 80 (2009): 1388–1392. [DOI] [PubMed] [Google Scholar]
- 90.Albert FE and El-Mowafy OM. "Marginal adaptation and microleakage of Procera AllCeram crowns with four cements". International Journal of Prosthodontics 17 (2004): 529–535. [PubMed] [Google Scholar]
- 91.Kermanshahi S., et al. "Biodegradation of resin-dentin interfaces increases bacterial microleakage". Journal of Dental Research 89.90 (2010): 996–1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Hansel C., et al. "Effects of various resin composite (co)monomers and extracts on two caries-associated micro-organisms in vitro". Journal of Dental Research 77.1 (1998): 60–67. [DOI] [PubMed] [Google Scholar]
- 93.Hunter AJ and Hunter AR. "Gingival margins for crowns: A review and discussion. Part II: Discrepancies and configurations". Journal of Prosthetic Dentistry 64.6 (1990): 636–642. [DOI] [PubMed] [Google Scholar]
- 94.Matthews DC and Tabesh M. "Detection of localized tooth related factors that predispose to periodontal infections". Periodontology 2000 34 (2004): 136–150. [DOI] [PubMed] [Google Scholar]
- 95.Drisko CH. "Nonsurgical periodontal therapy". Periodontology 2000 25 (2001): 77–88. [DOI] [PubMed] [Google Scholar]
- 96.Hagi TT., et al. "A biofilm pocket model to evaluate different non-surgical periodontal treatment modalities in terms of biofilm removal and reformation, surface alterations and attachment of periodontal ligament fibroblasts". PLOS ONE (2015): 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Yaghini et al. "Root surface roughness after scaling and root planing with Er:YAG laser compared to hand and ultrasonic instruments by profilometry ". Journal of Dentistry, Tehran University of Medical Sciences 12.12 (2015): 899–905. [PMC free article] [PubMed] [Google Scholar]
- 98.Tortora GJ., et al. "Inorganic Compounds-Water", "Desiccation", "Interaction between Microbes and Hosts-Adherence" and "Bacterial diseases of the mouth". In: Microbiology 9th edition. Pearson Benjamin Cummings, San Francisco: (2007): 747–750. [Google Scholar]
- 99.Nyvad B and Fejerskov O. "Scanning electron microscopy of early microbial colonization of human enamel and root surfaces in vivo". Scandinavian Journal of Dental Research 95 (1987): 287–296. [DOI] [PubMed] [Google Scholar]
- 100.Juric H. "Current possibilities in occlusal caries management". Acta Medica Academica 42.2 (2013): 216–222. [DOI] [PubMed] [Google Scholar]
- 101.Sreedevi A and Mohamed S. "Sealants, pit and fissure." StatPearls StatPearls Publishing, Treasure Island, FL: (2017): 9. [PubMed] [Google Scholar]
- 102.Eskandarian T., et al. "Comparison of clinical success of applying a kind of fissure sealant on the lower permanent molar teeth in dry and wet conditions". Journal of Dentistry, Tehran University of Medical Sciences 16.3 (2015):162–168. [PMC free article] [PubMed] [Google Scholar]
- 103.Hannig M. "Transmission electron microscopy of early plaque formation on dental materials in vivo". European Journal of Oral Sciences 107 (1999): 55–64. [DOI] [PubMed] [Google Scholar]
- 104.Quirynen M and Bollen CML. "The influence of surface roughness and surface-free energy on supra- and subgingival plaque formation in man". Journal of Periodontoiogy 22 (1995): 1–14. [DOI] [PubMed] [Google Scholar]
- 105.Bollen CML., et al. "The influence of abutment surface roughness on plaque accumulation and peri-implant mucositis". Clinical Oral Implants Research 7 (1996): 201–211. [DOI] [PubMed] [Google Scholar]
- 106.Bollen CML., et al. "Comparison of surface roughness of oral hard materials to the threshold surface roughness for bacterial plaque retention: A review of the literature". Dental Materials 13 (1997): 258–269. [DOI] [PubMed] [Google Scholar]
- 107.Teughels W., et al. "Effect of material characteristics and/or surface topography on biofilm development". Clinical Oral Implants Research 17.2 (2006): 68–81. [DOI] [PubMed] [Google Scholar]
- 108.Simonsen RJ and Neal RC. "A review of the clinical application and performance of pit and fissure sealants". Australian Dental Journal 56.1 (2011): 45–58. [DOI] [PubMed] [Google Scholar]
- 109.Mourouzis P. "Effects of sonic scaling on the surface roughness of restorative materials". Journal of Oral Science 51.4 (2009): 607–614. [DOI] [PubMed] [Google Scholar]
- 110.Eid HA., et al. "Surface topography of composite restorative materials following ultrasonic scaling and its impact on bacterial plaque accumulation. An in-vitro study". Journal of International Oral Health 5.3 (2013): 13–19. [PMC free article] [PubMed] [Google Scholar]
- 111.Kamonwanon P., et al. "SiO2-nanocomposite film coating of CAD/CAM composite resin blocks improves surface hardness and reduces susceptibility to bacterial adhesion". Dental Materials 36.1 (2017): 88–94. [DOI] [PubMed] [Google Scholar]
- 112.Leknes KN., et al. "Influence of tooth instrumentation roughness on subgingival microbial colonization". Journal of Periodontoiogy 65 (1994): 303–308. [DOI] [PubMed] [Google Scholar]
- 113.Eick S., et al. "Adherence of Streptococcus mutans to various restorative materials in continuous flow system". Journal of Oral Rehabilitation 31 (2004): 278–285. [DOI] [PubMed] [Google Scholar]
- 114.Marcus RA and Sutin N. "Electron transfers in chemistry and biology" Biochimica et Biophysica Acta 811 (1985): 265–322. [Google Scholar]
- 115.Petersen RC. "Reactive secondary sequence oxidative pathology polymer model and antioxidant tests". International Research Journal of Pure and Applied Chemistry 2.4 (2012): 247–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Quirynen M., et al. "The influence of surface free-energy on planimetric plaque growth in man". Journal of Dental Research 68.5 (1989): 796–799. [DOI] [PubMed] [Google Scholar]
- 117.Van Dijk J., et al. "Surface-free energy and bacterial adhesion". Journal of Clinical Periodontoiogy 14 (1987): 300–304. [DOI] [PubMed] [Google Scholar]
- 118.Weerkamp AH., et al. "Effect of zeta potential and surface energy on bacterial adhesion to uncoated and saliva-coated human enamel and dentin". Journal of Dental Research 67.12 (1988): 1483–1487. [DOI] [PubMed] [Google Scholar]
- 119.Rolla G., et al. "Enhancement and inhibition of dental plaque formation-Some old and new concepts". Biofouling 3.3 (1991): 175–181. [Google Scholar]
- 120.Koseki H., et al. "Early Staphylococcal biofilm formation on solid orthopedic implant materials: In vitro study". PLOS ONE 9.10 (2014): e107588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Petersen RC. "Appendix D-Hydrophobic Low-Viscosity Styrene-Free Vinyl Ester Resin Systems. In: Micromechanics/Electron Interactions for Advanced Biomedical Research". LAP LAMBERT Academic Publishing Gmbh and Co. KG Saarbrücken Germany: (2011): 499–504. [Google Scholar]
- 122.Bosshardt DD and Lang NP. "The junctional epithelium: from health to disease". Journal of Dental Research 84.1 (2005): 9–20. [DOI] [PubMed] [Google Scholar]
- 123.Chengbiao J., et al. "Substrate roughness induces the development of defective E-cadherin junctions in human gingival keratinocytes". Journal of Periodontal and Implant Science 47.2 (2017): 116–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Petersen RC. "Free-radical polymer science structural cancer model: A review". Scientifica (2013): 143589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Petersen RC. "Free radicals and advanced chemistries involved in cell membrane organization influence oxygen diffusion and pathology treatment". AIMS Biophysics 4.2 (2017): 240–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Petersen RC., et al. "Advancements in free-radical pathologies and an important treatment solution with a free-radical inhibitor". SF Journal of Biotechnology and Biomedical Engineering 1.1 (2018): 1003. [PMC free article] [PubMed] [Google Scholar]