Supplemental Digital Content is available in the text.
Introduction:
Asthma is the most common cause of chronic disease in children and has high healthcare utilization costs. Minority children living in poverty have a higher asthma burden. These health disparities are associated with the social determinants of health (SDH). A severe asthma clinic was implemented at Rady Children’s Hospital in San Diego to determine whether a multidisciplinary approach, including an asthma home visit addressing SDH, would lead to decreased healthcare utilization in terms of emergency department (ED) visits and hospitalizations.
Methods:
Patients with 2 or more ED visits in the past 6 months or 2 or more hospitalizations in the previous year were recruited to Rady Children’s Hospital Severe Asthma Clinic. A multidisciplinary team evaluated each patient systematically. A subset of patients on capitated Medicaid insurance plans also had a comprehensive asthma home visit with community health workers as part of the Community Approach to Severe Asthma (CASA) program.
Results:
A significant reduction in ED visits (75%, P < 0.001) and hospitalization days (73%, P < 0.001) was demonstrated in 74 Severe Asthma Clinic participants with 1 year of pre-/postdata to analyze. In a subset of 12 patients in the CASA program, further reductions in ED visits (90%, P = 0.002) were also demonstrated. Basic needs, including shelter, food, and assistance with utilities, were the most common domain of SDH identified and addressed in CASA participants.
Conclusion:
We demonstrate that a novel pediatric severe asthma clinic with a multidisciplinary approach, including actively addressing SDH, is associated with decreasing health care utilization.
INTRODUCTION
Asthma is the leading cause of chronic disease in the pediatric population in the United States, affecting over 6 million children and 8% of the population.1 It accounts for over $82 billion per year in costs associated with health care utilization.2 Children from minority ethnicities and living in poverty have higher prevalence rates of asthma and suffer from significant disparities with increased morbidity and mortality than age-matched white children.3,4 In San Diego County, asthma-related emergency department (ED) visits are 5 times higher for black children (109.6 per 10,000) and 2 times higher for Hispanic (44.7 per 100,000) children than for white children (20.9 per 10,000).5 The complex social and environmental factors that shape these health disparities are referred to as the social determinants of health (SDH) and powerfully impact chronic conditions like asthma.6 Low-income housing disproportionately exposes children to multiple indoor allergens and outdoor pollutants that can exacerbate asthma symptoms.7,8 Poor children are also exposed to higher levels of family turmoil, violence, separation, instability, and chaotic household conditions.9
Severe asthma in children is defined as persistent uncontrolled asthma despite maximal therapy. This term comprises asthma-mimicking conditions, asthma that is difficult to treat because of comorbidities, improper inhaler technique or poor therapeutic adherence, and other environmental factors, and true severe therapy-resistant asthma, as defined by the latest European Respiratory Society/American Thoracic Society definition.10
Dedicated severe asthma programs have shown efficacy in reducing asthma burden in the literature.11 Successful asthma programs, including the Community Asthma Initiative in Boston12 target high-risk patients, provide education and home environment assessment, and coordinate community, public health, and social services.13
The Severe Asthma Clinic (SAC) at Rady Children’s Hospital in San Diego began in 2015 intending to provide coordinated care to children with severe asthma and reduce health disparities. Although the SAC sees all patients with severe asthma, patients with Medicaid or California Covered Services insurance predominate, 74% (Table 1). These insurance programs are available to low-income children and funded at the federal and state level, respectively. Although multidisciplinary clinics and home visiting programs have demonstrated success in the past, they have infrequently screened SDH.14 In this novel observational retrospective analysis, we aimed to determine whether a dedicated severe asthma service in combination with a home visiting program that screened SDH would lead to a decrease in asthma-related ED visits and hospitalization days in this specific pediatric population.
Table 1.
Basic Demographics of SAC Patients
| Overall (n = 74) | |
|---|---|
| Age at first visit | 9.50 (4.49) |
| Race/ethnicity | |
| Asian | 3 (4.1%) |
| Black | 14 (18.9%) |
| Hispanic | 41 (55.4%) |
| Other | 3 (4.1%) |
| White | 13 (17.6%) |
| Insurance type | |
| CCS | 8 (10.8%) |
| Commercial | 17 (23.0%) |
| Medi-Cal | 47 (63.5%) |
| Military | 2 (2.7%) |
| Baseline ED visit | 2.97 (2.91) |
| Baseline hospitalization days | 3.15 (3.86) |
SAC baseline demographics. Age, baseline ED, and hospitalization days reported as mean (SD). Race/ethnicity and insurance type reported as count (percentage). Commercial Plans include Blue Cross, Blue Shield, Kaiser, Scripps, and United. CCS include supplemental state insurance plan for chronic illnesses.
CCS, California Covered Services.
METHODS
Inclusion criteria to SAC included children age 2–18 with 2 or more ED visits or hospitalizations in the previous 6 months due to an asthma-related episode as the primary diagnosis. Patients meeting these criteria are referred from Rady inpatient hospitalists and specialist physicians within the Allergy/Immunology and Pulmonology divisions. A multidisciplinary team, including allergy/immunology, pulmonology, clinical pharmacy, respiratory therapy, and nurse case management, sees each SAC patient. The visits focus on confirmation of diagnosis, evaluation of comorbidities, and optimization of medication and adherence. Patients have follow-up visits in SAC every 3 months; about 4 visits annually. The no-show rate for the SAC clinic is 15%.
With funding from the California Department of Public Health (CDPH), a subset of SAC patients on Rady capitated Medi-Cal plans also had an asthma home visit soon after their first SAC visit. This home visit was scheduled with Rady bilingual community health workers (CHWs) as part of the Community Approach to Severe Asthma (CASA) program. CDPH and Rady physicians, social workers, and nurses trained the CHWs on how to interact with families and perform asthma home visits. The CASA program is shaped on principles of the social-ecological model. This model emphasizes several layers of influence, including individual, interpersonal, organizational, community, and local public policy that can affect asthma management and outcomes for patients.
The program employs several quality improvement strategies to optimize success. The team, composed of CHWs, a social worker, a program coordinator, and a physician, took a Kaizen approach by holding a weekly meeting focused on making improvements to help decrease asthma-related events for our patient population.15 This team approach was chosen due to the various skills of team members. At the onset, the team invited community stakeholders to discuss how to best provide resources to families in the San Diego community with Rady Children’s Hospital Asthma Forum in November 2016. The team then performed vital informant interviews with different asthma programs throughout the United States, including Alameda Asthma Start,16 the Respira Sano project in Imperial Valley,17 the Yes We Can Urban Asthma Partnership,18 and the Boston Home Asthma Visit Collaborative19 to help shape this program and evaluation metrics.
Like these programs, the main goal was to evaluate asthma control in the patient population by demonstrating a reduction in ED visits and hospitalizations. These programs are all informed by the National Asthma Education and Prevention Program guidelines that recommend environmental trigger reduction in patients with asthma to improve asthma control.20 The team then developed the process map integrating the CASA program with the SAC with this input (Fig. 1). After initiating the program, the team performed regular Plan-Do-Study-Act cycles to ensure coordination between the SAC, CASA program, and each patient was optimized. Lastly, the recognition of CASA team members occurred at the annual Rady Children’s Hospital Research Symposium. This symposium also allowed for constructive feedback regarding the CASA program.
Fig. 1.

Patients with 2 or more ED visits in the previous 6 months and/or 2 or more hospitalizations in the last year are recruited to the SAC from the ED, ICU, and inpatient settings. A subset of patients on capitated insurance plans seen in SAC has an asthma home visit in the CASA program. ICU indicates intensive care unit; MD, physician; RN, registered nurse; RT, respiratory therapist.
At the home visit, CHWs conduct a walk-through environmental assessment for asthma triggers developed from Boston Asthma Home Visit Collaborative19 and, with assistance from the CDPH, provided CDPH recipes for simple cleaning solutions. Furthermore, the CHWs reinforce clinician SAC instructions, including medication changes, inhaler technique, and home environment recommendations such as obtaining dust mite encasements or mold abatement. They set behavioral/environmental change goals based on the social cognitive theory, which suggests that creating an environment conducive to change makes adopting positive behaviors easier. Lastly, they facilitate an opt-in link with 211-San Diego (211) to screen for SDH. The CHWs called families to remind them about upcoming SAC appointments and related patient concerns to the SAC.
The local nonprofit organization, 211, provides access to 6,000 community, health, social, and disaster services in San Diego. They developed a specific risk assessment tool for this project with 14 SDH domains based on Healthy People 2020 Strategies.21 The 211 service provided resources based on risk assessment responses and follow-up with families by phone to monitor the reduction in risk throughout 12 months. They also provided monthly reports on referrals to the CASA program allowing further follow-up and coordination with the SAC physicians in follow-up clinic visits. As the goal was improving patient outcomes, the University of California, San Diego Institutional Review Board determined this project to be a quality improvement project and waived the requirement for Institutional Review Board approval.
RESULTS
The SAC saw 86 patients from 2017 to 2019. At the time of submission, 10 patients had not followed up for 1 year postintervention data collection, and 2 had moved out of state (2.3% lost to follow-up), leaving 74 patients with 12 months of pre-/postintervention data to analyze from Rady’s electronic medical record system for a primary diagnosis of asthma-related events. A paired t test was used to analyze the change in the number of visits pre- and postintervention. McNemar test was used to analyze the change in the number of patients who had visits pre- and postintervention. A cutoff of 2 visits was used to create binary variables. All patients had poorly controlled asthma (by ERP Asthma guidelines)20 and were on inhaled corticosteroids before their first SAC visit. Nested within the SAC were 12 (16%) patients who had a home visit as part of the CASA home visit program. The patients were primarily Hispanic (55%) and black children (19%) with Medi-Cal (Medicaid) and California Covered Services insurance (74%) (Table 1). Significant reductions were seen in patients who had 2 or more ED visits in both the SAC (pre: 54, post: 13, 75% reduction, P < 0.001) and the nested CASA program (pre: 11, post: 1, 90% reduction, P = 0.002). The SAC population showed significant reductions in patients with 2 or more hospitalization days (pre: 45, post: 12, 73% reduction, P < 0.001). The CASA program demonstrated a decreasing trend (pre: 6, post: 2, 77% reduction, P = 0.125). The results are summarized in Figure 2A.
Fig. 2.
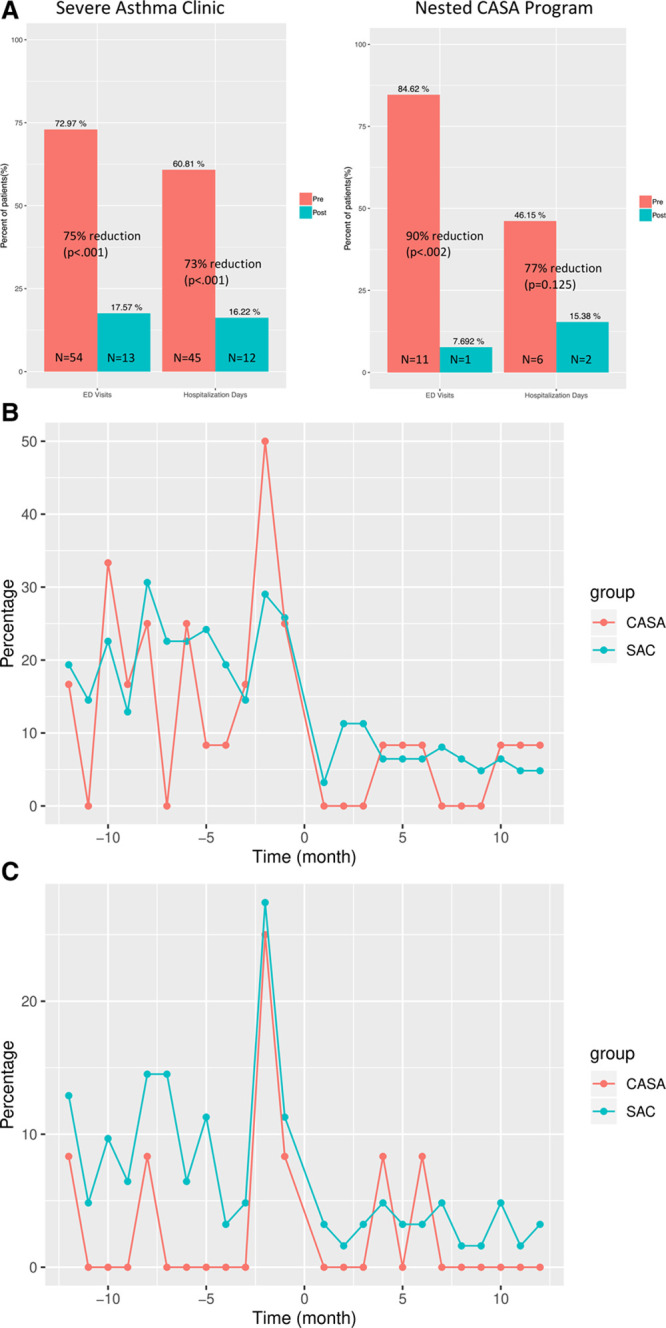
Comparison of healthcare utilization before and after intervention. A, Pre- and postchanges in ED visits (2 or more) and hospitalization days (2 or more) of subjects in SAC (N = 74) and the subset who participated in the CASA program (N = 12). Both pre- and postrecord contains each patient’s visits/hospitalization days for 12 months. B, P-chart of pre- and postintervention changes in the percentage of subjects in SAC and the CASA program who had ED visits over the 12 months before and after the intervention. C, P-chart of pre- and postintervention changes in the percentage of subjects in SAC and the CASA program who had hospitalization days over the 12 months before and after the intervention.
A P-chart was created to visually describe what percent of patients had ED visits (Fig. 2B) and/or hospitalization (Fig. 2C) each month before and after the program start for the SAC and nested CASA group. Three-sigma limits were used to calculate upper and lower control limits (Fig. 2B, C). Generally, a higher percentage of patients had ED visits and hospitalizations in the 2 to 3 months before the intervention. The percentage of patients who had ED visits and hospitalizations after the intervention remained low for 12 months postintervention.
The 211 health navigators provided a comprehensive assessment of unmet social, behavioral, and health needs. Of the 12 participants contacted by the 211 staff, 88 SDH-related needs divided into different domains were identified utilizing the telephone questionnaire risk assessment tool. Responders indicated the “Basic Needs” domain (food, shelter, and utilities) as the most common need (37%), with “utilities” most commonly being identified in the group (Table S1, Supplemental Digital Content, which shows 211 needs assessment for CASA participants. Social Determinants of Health domains are divided into a first and second level in the first and second columns, respectively. Taxonomy of resources provided are identified in the third column. Number of participants with the specific taxonomic resources provided are identified in the forth column, http://links.lww.com/PQ9/A215).
DISCUSSION
Pediatric patients seen at the SAC demonstrated a significant decrease in ED visits and hospitalizations. A multidisciplinary approach allows for the coordination of the expertise needed to manage the complexities of severe pediatric asthma.22,23 In a subset of patients in the CASA program who had a CHW asthma home visit and a 211 referral to manage their asthma further and address SDH issues, respectively, decreases in hospitalization days were demonstrated. Although the sample size is small, these findings are consistent with the literature that show decreased healthcare utilization (ED visits and hospitalizations) with CHW asthma home visit programs.2,11,12 CHW asthma home visit programs provide asthma self-management support with less time and access limitations than in the clinic setting and are increasingly being utilized in asthma management.12 Data from our P-chart analysis showed a higher percentage of ED visits and hospitalization days in the 2 to 3 months before the intervention suggesting that recruiting patients soon after an ED visit or hospitalization may increase participation in the intervention. We also demonstrated that our intervention had a sustained effect over the 12 months postintervention.
By beginning to assess SDH with the 211 partnership, the CASA program was able to identify other barriers to care, including transportation, stable housing, and access to healthy food. Based on their assessment results, the 211 health navigators established a care plan, including a direct link to services. This plan included helping families access housing lists, filling out applications, and following the progress of applications with various agencies (Table S1, Supplemental Digital Content, which shows 211 needs assessment for CASA participants. Social Determinants of Health domains are divided into a first and second level in the first and second columns, respectively. Taxonomy of resources provided are identified in the third column. Number of participants with the specific taxonomic resources provided are identified in the forth column, http://links.lww.com/PQ9/A215).
The findings in this report are subject to several limitations. First, this evaluation was not a randomized controlled trial, so the team cannot account for a placebo effect or regression to the mean. The contributions of individual components of the program to outcomes were not evaluated. The team is planning a randomized controlled trial based on results to address this limitation. Also, the administrative data may not include all patients outside of Rady’s network for emergency care. However, Rady’s electronic medical record does capture encounter level data with other institutions, which limits this possibility. Lastly, the small sample size potentially limits the interpretation of the results. Similar findings in a replicated but larger sample size would be even more compelling.
CONCLUSIONS
Based on thorough research, this SAC is thought to be the first subspecialty multidisciplinary pediatric asthma clinic to actively screen SDH domains, and the findings indicate a multidisciplinary approach to asthma with a home visit and screening of SDH will help decrease healthcare utilization in a pediatric population with severe asthma. Future research of this approach at Rady Children’s Hospital has begun and will be elucidating if similar findings are confirmed as the program is scaled up.
DISCLOSURES
Dr Phipatanakul is a consultant for Genentech, Novartis, Regeneron, GSK, AstraZeneca, Sanofi, and Teva; received additional funding support from NIH K24 AI 106822; received grant support from Genentech, Novartis, Regeneron, GSK, Kaleo, Monaghan, Alk Abello, Lincoln Diagnostics, and Thermo Fisher; and all financial relationships are unrelated to the content of this article. Dr Leibel is a consultant for Thermo Fisher and Genentech; Received grant support from Genentech; and all financial relationships are unrelated to the content of this article. Dr Geng is a consultant for Genentech, Novartis, CSL, Shire, RMS, and Diplomat; is a speaker for Regeneron, CSL, Optinose, Mead-Johnson, and Horizon; received grant support from Genentech, Novartis, GSK, and Stallergenes; and all financial relationships are unrelated to the content of this article. The other authors have no financial interest to declare.
Supplementary Material
Footnotes
Published online September 25, 2020
The Community Approach to Severe Asthma (CASA) program and partnership with 211 San Diego were funded by the California Department of Public Health and Center for Medicare and Medicaid Services’ Transforming Clinical Practice Initiative. Funding also provided by the National Institutes of Health, Grant K24 AI 106822. The Altman Clinical and Translational Research Institute (ACTRI) is partially supported by the National Institutes of Health, Grant UL1TR001442 of Clinical and Translational Science Awards (CTSA) funding. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health (NIH).
Supplemental digital content is available for this article. Clickable URL citations appear in the text.
To cite: Leibel S, Geng B, Phipatanakul W, Lee E, Hartigan P. Screening Social Determinants of Health in a Multidisciplinary Severe Asthma Clinical Program. Pediatr Qual Saf 2020;5:e360.
REFERENCES
- 1.Sullivan PW, Ghushchyan V, Navaratnam P, et al. National prevalence of poor asthma control and associated outcomes among school-aged children in the United States. J Allergy Clin Immunol Pract. 2018; 6:536–544.e1. [DOI] [PubMed] [Google Scholar]
- 2.Nurmagambetov T, Kuwahara R, Garbe P. The economic burden of asthma in the United States, 2008-2013. Ann Am Thorac Soc. 2018; 15:348–356. [DOI] [PubMed] [Google Scholar]
- 3.Forno E, Celedon JC. Asthma and ethnic minorities: socioeconomic status and beyond. Curr Opin Allergy Clin Immunol. 2009; 9:154–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Akinbami LJ, Moorman JE, Garbe PL, et al. Status of childhood asthma in the United States, 1980-2007. Pediatrics. 2009; 123suppl 3S131–S145. [DOI] [PubMed] [Google Scholar]
- 5.Office of Statewide Health Planning and Development. Asthma ED visits in San Diego County compared to California [Internet]. Office of Statewide Health Planning and Development (OSHPD). [Cited May 26, 2020.] Available at https://data.chhs.ca.gov/dataset/asthma-ed-visit-rates-lghc-indicator-07. Accessed May 26, 2020. [Google Scholar]
- 6.Marmot M, Friel S, Bell R, et al. ; Commission on Social Determinants of Health. Closing the gap in a generation: health equity through action on the social determinants of health. Lancet. 2008; 372:1661–1669. [DOI] [PubMed] [Google Scholar]
- 7.Thakur N, Oh SS, Nguyen EA, et al. Socioeconomic status and childhood asthma in urban minority youths. The GALA II and SAGE II studies. Am J Respir Crit Care Med. 2013; 188:1202–1209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guarnieri M, Balmes JR. Outdoor air pollution and asthma. Lancet. 2014; 383:1581–1592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Evans GW. The environment of childhood poverty. Am Psychol. 2004; 59:77–92. [DOI] [PubMed] [Google Scholar]
- 10.Chung KF, Wenzel SE, Brozek JL, et al. International ERS/ATS guidelines on definition, evaluation and treatment of severe asthma. Eur Respir J. 2014; 43:343–373. [DOI] [PubMed] [Google Scholar]
- 11.Gibeon D, Heaney LG, Brightling CE, et al. ; British Thoracic Society Difficult Asthma Network. Dedicated severe asthma services improve health-care use and quality of life. Chest. 2015; 148:870–876. [DOI] [PubMed] [Google Scholar]
- 12.Woods ER, Bhaumik U, Sommer SJ, et al. Community asthma initiative: evaluation of a quality improvement program for comprehensive asthma care. Pediatrics. 2012; 129:465–472. [DOI] [PubMed] [Google Scholar]
- 13.Le Cann P, Paulus H, Glorennec P, et al. Home environmental interventions for the prevention or control of allergic and respiratory diseases: what really works. J Allergy Clin Immunol Pract. 2017; 5:66–79. [DOI] [PubMed] [Google Scholar]
- 14.Williams DR, Sternthal M, Wright RJ. Social determinants: taking the social context of asthma seriously. Pediatrics. 2009; 123suppl 3S174–S184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jacobson GH, McCoin NS, Lescallette R, et al. Kaizen: a method of process improvement in the emergency department. Acad Emerg Med. 2009; 16:1341–1349. [DOI] [PubMed] [Google Scholar]
- 16.Respira Sano. 2020. Respira Sano Project. [Cited May 26, 2020] Available at http://www.respirasano.org/about. Accessed May 26
- 17.Thyne SM, Rising JP, Legion V, et al. The Yes We Can Urban Asthma Partnership: a medical/social model for childhood asthma management. J Asthma. 2006; 43:667–673. [DOI] [PubMed] [Google Scholar]
- 18.Dong Z, Nath A, Guo J, et al. Evaluation of the environmental scoring system in multiple child asthma intervention programs in Boston, Massachusetts. Am J Public Health. 2018; 108:103–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.National Asthma Education and Prevention Program. Expert panel report 3 (EPR-3): guidelines for the diagnosis and management of asthma-summary report 2007. J Allergy Clin Immunol. 2007; 1205 supplS94–S138. [DOI] [PubMed] [Google Scholar]
- 20.US Department of Health and Human Services, Office of Disease Prevention and Health Promotion Healthy People 2020 Topics and Objectives [Internet]. 2020.Washington, DC: US. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. [Cited December 30, 2019.] Available at https://www.healthypeople.gov/2020/topic/maternal-infant-and-child-health/objectives. Accessed May 26 [Google Scholar]
- 21.Pike KC, Levy ML, Moreiras J, et al. Managing problematic severe asthma: beyond the guidelines. Arch Dis Child. 2018; 103:392–397. [DOI] [PubMed] [Google Scholar]
- 22.Ramratnam SK, Bacharier LB, Guilbert TW. Severe asthma in children. J Allergy Clin Immunol Pract. 2017; 5:889–898. [DOI] [PubMed] [Google Scholar]
- 23.Campbell JD, Brooks M, Hosokawa P, et al. Community health worker home visits for medicaid-enrolled children with asthma: effects on asthma outcomes and costs. Am J Public Health. 2015; 105:2366–2372. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


