Abstract
Background
Although coronavirus disease 2019 (COVID-19) disproportionally affects older adults, the use of conventional triage tools in acute care settings ignores the key aspects of vulnerability.
Objective
This study aimed to determine the usefulness of adding a rapid vulnerability screening to an illness acuity tool to predict mortality in hospitalised COVID-19 patients.
Design
Cohort study.
Setting
Large university hospital dedicated to providing COVID-19 care.
Participants
Participants included are 1,428 consecutive inpatients aged ≥50 years.
Methods
Vulnerability was assessed using the modified version of PRO-AGE score (0–7; higher = worse), a validated and easy-to-administer tool that rates physical impairment, recent hospitalisation, acute mental change, weight loss and fatigue. The baseline covariates included age, sex, Charlson comorbidity score and the National Early Warning Score (NEWS), a well-known illness acuity tool. Our outcome was time-to-death within 60 days of admission.
Results
The patients had a median age of 66 years, and 58% were male. The incidence of 60-day mortality ranged from 22% to 69% across the quartiles of modified PRO-AGE. In adjusted analysis, compared with modified PRO-AGE scores 0–1 (‘lowest quartile’), the hazard ratios (95% confidence interval) for 60-day mortality for modified PRO-AGE scores 2–3, 4 and 5–7 were 1.4 (1.1–1.9), 2.0 (1.5–2.7) and 2.8 (2.1–3.8), respectively. The modified PRO-AGE predicted different mortality risk levels within each stratum of NEWS and improved the discrimination of mortality prediction models.
Conclusions
Adding vulnerability to illness acuity improved accuracy of predicting mortality in hospitalised COVID-19 patients. Combining tools such as PRO-AGE and NEWS may help stratify the risk of mortality from COVID-19.
Keywords: COVID-19, triage, geriatric assessment, prognosis, mortality, older people
Key points
The use of conventional triage tools in acute care settings ignores the key aspects of vulnerability.
Several screening tools have been developed to capture vulnerability and estimate the prognosis in acutely ill older patients.
Adding vulnerability to illness acuity improved the accuracy of predicting mortality in hospitalised COVID-19 patients.
The vulnerability worked as an independent predictor of mortality in hospitalised patients with COVID-19.
Introduction
The rapid spread of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has burdened most healthcare systems worldwide [1]. Although most individuals with coronavirus disease 2019 (COVID-19) are asymptomatic or oligosymptomatic, one in five persons develop severe forms of the disease; as of September 2020, about 1 million people have died of COVID-19 [2]. In this context, frontline health workers are constantly challenged to determine the severity and prognosis of COVID-19 cases to provide high-quality care and efficiently allocate resources [3].
In past decades, various screening tools have been incorporated into the triage systems to identify patients at a higher risk of clinical deterioration in acute care settings [4, 5]. These instruments use physiological parameters, such as vital signs, to measure illness acuity (general level of patient illness, urgency for clinical intervention and intensity of resource utilisation) [6]. Previous studies have shown that tools such as the National Early Warning Score (NEWS) and the quick Sequential Sepsis-Related Organ Failure Assessment (SOFA) can be used to identify patients with infection who are at a higher risk of mortality in the hospital [4, 7].
However, ageing appears to decrease the predictive accuracy of illness acuity screening tools [8]. That is unfortunate, as multiple factors possibly increase the older adults’ risk of experiencing complications from COVID-19, including physiological changes that affect vital signs (e.g. absence of fever), multimorbidity, cognitive impairment, sensory deficits and atypical presentations of disease [9, 10]. Because conventional screening tools often fail to capture the key elements of risk in older persons (e.g. frailty, functional decline and cognitive impairment), they can misclassify illness severity in patients aged 65 years and older [10, 11]. Such inaccuracies are particularly problematic in the context of COVID-19 since almost half of the admissions and up to 80% of deaths from the infection occur in older adults [12, 13].
Several geriatric screening tools have been developed to estimate the prognosis in acutely ill older patients [14, 15]. These easy-to-use vulnerability screening tools allow the quick assessment of geriatric conditions in acute care settings [9, 10]. Previous studies have demonstrated that tools like the Identification of Seniors at Risk (ISAR) and the PRO-AGE scoring system can provide valuable prognostic information by identifying factors that are rarely contemplated in routine medical assessments [15, 16]. Nevertheless, unlike physiological parameters, the usefulness of geriatric screening tools in the risk stratification of COVID-19 patients remains unknown. We aimed to assess whether measuring vulnerability, in addition to an illness acuity tool and other conventional risk factors, improves the prognostication of COVID-19 patients admitted to the hospital.
Methods
Study design and population
Our cohort is part of an ongoing study investigating COVID-19 patients admitted to a tertiary university hospital located in São Paulo. This hospital is the largest academic medical complex in Latin America. On 30 March 2020, the main hospital building was converted to a COVID-19-only facility, becoming the major centre for the treatment of SARS-CoV-2-infected patients in Brazil. A total of 900 beds allotted for COVID-19 admissions, which were centrally regulated by the State of São Paulo. Overall, the hospital received severely ill patients from 85 cities and 278 secondary hospitals statewide, although they mostly supported the metropolitan area of São Paulo (Appendix Figure S1).
We assessed the eligibility of all patients aged ≥50 years consecutively admitted to the hospital between 30 March and 30 June 2020. We included those with confirmed (detection of the new coronavirus using reverse transcription-polymerase chain reactions) cases of SARS-CoV-2 infection.
The local institutional review board approved the study and authorised the researchers to secure verbal consent in the follow-up interviews during the study.
Data collection
Trained medical investigators collected the study information using standardised electronic case report forms. Data were extracted from electronic medical and nursing records using the enterprise electronic health record reporting database (SOUL System; MV Hospitalar®). Whenever necessary, investigators supplemented the data from electronic records by conducting structured telephone interviews with patients or their proxies. Thus, we were able to obtain data on patient’s demographic characteristics (age, sex, self-reported race or ethnicity and years of formal education), comorbidities, medications used, previous hospitalisations, vital signs, level of consciousness, need for supplemental oxygen and acute symptoms of the disease on admission. We computed the Charlson comorbidity score to measure the disease burden [17]. We examined evidence of delirium on admission using the CHART-DEL instrument [18]. Data regarding patients’ functional status and other geriatric syndromes (need for assistance in performing activities of daily living, memory complaints, sensory deficits, falls, weight loss and fatigue) were also documented.
Screening tools
For each of our domains of interest, vulnerability and illness acuity, we examined two possible assessment tools and selected those that can more accurately predict mortality.
To measure illness acuity, the NEWS [19] and quick SOFA [20] were assessed. The NEWS (0–20; higher = worse) comprises seven physiological variables that often integrate early warning systems to identify high-risk patients in acute care settings [7]. The quick SOFA combines three dichotomous criteria (hypotension, dyspnoea and altered level of consciousness), with scores ranging from 0 to 3 (higher = worse) [20].
To measure vulnerability, we evaluated the modified version of the PRO-AGE scoring system [15] and ISAR [21]. The ISAR, a geriatric screening tool widely used in acute care settings, includes six concise questions on functional status, previous hospitalisations, presence of visual and memory complaints and polypharmacy [21]. The PRO-AGE scoring system is a validated mnemonic method used to assess vulnerability and predict hospital admission, prolonged length of stay and death in older adults at the emergency department [15]. It is used to evaluate P = physical impairment (acute functional decline), R = recent hospitalisation (hospitalisation in the previous 6 months), O = older age (≥90 years), A = acute mental status change (as a surrogate measure of delirium), G = getting thinner (weight loss ≥ 5% in the previous year) and E = exhaustion (fatigue) [15]. In our study, we wanted to control for age separately in the statistical models as the age of ≥90 years as a cut-off may not be clinically meaningful [22]. Therefore, we removed ‘older age’ from the PRO-AGE equation, resulting in a modified version of the tool with scores ranging from 0 to 7 (higher = worse).
Details of the operational and scoring instructions for the screening tools are shown in Appendix Tables S1 and S2.
Outcome measures
Our primary outcomes were time-to-death within 30 and 60 days of hospital admission. We registered the dates of admission and discharge or death, and then followed those who were discharged for up to 60 days. Investigators blinded to the baseline data conducted a series of follow-up via telephone interviews to assess all-cause mortality. Participants who survived at the end of the 60 days were censored.
Statistical analysis
We estimated the accuracy of each screening tool to predict 60-day mortality using the area under the receiver operating characteristic curve (AUROC). We compared the differences in AUROC between illness acuity tools (NEWS versus quick SOFA) and between geriatric screening tools (ISAR versus modified PRO-AGE).
We used Cox proportional hazards models to estimate whether the vulnerability measure was a predictor of time-to-death within 30 and 60 days. We also studied sociodemographic factors (age and sex), Charlson comorbidity score and illness acuity as predictors of time-to-death. For analysis purposes, we categorised the measures with no standard cut-off values according to quartiles.
We calculated the Spearman’s rank correlation between illness acuity and vulnerability to explore the relationship between these measures. We also investigated whether adding vulnerability to illness acuity improved the risk stratification of death. For this analysis, we combined the two lower and two higher quartiles of the vulnerability screening tool, obtaining two levels of vulnerability. Then, we calculated the Kaplan–Meier survival curves over the 60-day follow-up according to quartiles of the illness acuity tool, stratified based on the two levels of vulnerability. We also fitted Cox proportional hazards models for time-to-death within 60 days using quartiles of the illness acuity tool, stratified based on the two levels of vulnerability as the predictor.
Finally, we examined whether the vulnerability measure improved the discrimination of 30-day and 60-day mortality models based on age, sex and Charlson comorbidity score, on an illness acuity tool and on both models by comparing the AUROC.
The analyses were performed using Stata 15.1 (StataCorp, College Station, TX, USA). All statistical tests were two-tailed and accepted significance at alpha levels < 0.05.
Results
We screened 2,078 people aged ≥50 years who were admitted to the hospital between March and June 2020. We excluded patients without laboratory-confirmed diagnosis of COVID-19 (N = 599) and readmitted patients who were already included in the study (N = 51), resulting in a final sample of 1,428 SARS-CoV-2-infected patients. The participants had a median age of 66 years, and 58% were male (Table 1). Delirium was identified in 222 (16%) patients on admission using the CHART-DEL instrument and was associated with illness acuity and vulnerability (Appendix Table S3).
Table 1.
Baseline characteristics of patients admitted to hospital with COVID-19 (N = 1,428)
| Characteristics | N (%) or median (IQR) |
|---|---|
| Sociodemographic factors | |
| Age (years) | 66 (59, 74) |
| Age | |
| 50–64 years old | 646 (45) |
| 65–79 years old | 587 (41) |
| ≥80 years old | 195 (14) |
| Men | 825 (58) |
| Race or ethnicity | |
| White | 898 (63) |
| Black | 127 (9) |
| Mixed | 361 (25) |
| Other | 42 (3) |
| Education (years) | 5 (4, 8) |
| Comorbidities | |
| Chronic obstructive pulmonary disease | 114 (8) |
| Asthma | 53 (4) |
| Hypertension | 995 (70) |
| Heart failure | 225 (16) |
| Coronary artery disease | 196 (14) |
| Diabetes | 634 (44) |
| Chronic kidney disease (moderate to severe) | 240 (17) |
| Cerebrovascular disease | 122 (8) |
| Dementia | 70 (5) |
| Cancer | 208 (15) |
| Charlson comorbidity score | 1 (0, 4) |
| Behaviour measure | |
| Smoking status | |
| Never | 983 (69) |
| Former | 370 (26) |
| Current | 75 (5) |
| Illness acuity screening tools | |
| The National Early Warning Score (NEWS; 0–20) | 7 (5, 10) |
| The quick Sepsis-related Organ Failure Assessment (quick SOFA; 0–3) | 1 (1, 2) |
| Vulnerability screening tools | |
| The Identification of Seniors at Risk (ISAR; 0–6) | 2 (1, 3) |
| The modified PRO-AGE score (0–7) | 3 (2, 4) |
IQR, interquartile range.
During the 60-day follow-up, 605 (42%) patients died (564 [39%] in the hospital and 41 [3%] after discharge). Excluding 31 (2%) patients who were still hospitalised at the end of the 60 days, the median length of hospital stay was 13 days (interquartile range = 8–20 days). Of the 833 patients who were discharged from the hospital, 722 (87%) returned home and 111 (13%) were transferred to a post-acute care setting. The NEWS showed a significantly higher accuracy in predicting 60-day mortality compared with quick SOFA (AUROC = 0.71 versus 0.67; P < 0.001). Likewise, the modified PRO-AGE was superior to ISAR (AUROC = 0.70 versus 0.62, P < 0.001) (Appendix Figure S2).
The cumulative incidence of 30-day and 60-day mortality ranged from 16% and 22% to 63% and 69% across the quartiles of modified PRO-AGE scores, respectively (Table 2). The higher modified PRO-AGE score levels were significantly associated with time-to-death within 30 and 60 days, even after adjusting for age, sex, Charlson comorbidity score and NEWS (Table 2).
Table 2.
Association between risk factors and mortality in hospitalised patients with COVID-19
| Time-to-death within 30 days | Time-to-death within 60 days | |||||
|---|---|---|---|---|---|---|
| Hazard ratio (95% CI) | Hazard ratio (95% CI) | |||||
| N died/N total (%) | Crude | Adjusted | N died/N total (%) | Crude | Adjusted | |
| Age | ||||||
| 50–64 years old | 172/646 (27) | (reference) | (reference) | 212/646 (33) | (reference) | (reference) |
| 65–79 years old | 244/587 (42) | 1.7 (1.4–2.1) | 1.5 (1.2–1.8) | 276/587 (47) | 1.6 (1.4–1.9) | 1.4 (1.2–1.7) |
| ≥ 80 years old | 110/195 (56) | 2.8 (2.2–3.6) | 2.3 (1.8–3.0) | 117/195 (60) | 2.5 (2.0–3.2) | 2.1 (1.7–2.6) |
| Sex | ||||||
| Female | 204/603 (34) | (reference) | (reference) | 234/603 (39) | (reference) | (reference) |
| Male | 322/825 (39) | 1.2 (1.0–1.4) | 1.3 (1.1–1.6) | 371/825 (45) | 1.2 (1.0–1.4) | 1.4 (1.1–1.6) |
| Charlson score | ||||||
| 0 points | 101/379 (27) | (reference) | (reference) | 124/379 (33) | (reference) | (reference) |
| 1 point | 111/340 (33) | 1.3 (1.0–1.7) | 1.2 (0.9–1.6) | 123/340 (36) | 1.2 (0.9–1.5) | 1.1 (0.9–1.4) |
| 2–3 points | 129/340 (38) | 1.6 (1.3–2.1) | 1.5 (1.2–2.0) | 151/340 (45) | 1.6 (1.2–2.0) | 1.5 (1.2–1.9) |
| ≥ 4 points | 185/369 (50) | 2.4 (1.8–3.0) | 2.3 (1.7–2.9) | 207/369 (56) | 2.2 (1.8–2.7) | 2.2 (1.7–2.7) |
| NEWS | ||||||
| 0–5 points | 66/387 (17) | (reference) | (reference) | 81/387 (21) | (reference) | (reference) |
| 6–7 points | 98/340 (29) | 1.9 (1.4–2.5) | 1.9 (1.4–2.6) | 120/340 (35) | 1.9 (1.4–2.5) | 1.9 (1.4–2.5) |
| 8–9 points | 140/331 (42) | 3.0 (2.2–4.0) | 3.3 (2.5–4.4) | 161/331 (49) | 2.9 (2.2–3.8) | 3.2 (2.4–4.2) |
| ≥ 10 points | 222/370 (60) | 4.8 (3.6–6.3) | 4.1 (3.1–5.5) | 243/370 (66) | 4.6 (3.5–5.9) | 4.0 (3.1–5.2) |
| PRO-AGEa | ||||||
| 0–1 point | 54/328 (16) | (reference) | (reference) | 71/328 (22) | (reference) | (reference) |
| 2–3 points | 146/500 (29) | 1.9 (1.4–2.6) | 1.6 (1.1–2.1) | 170/500 (34) | 1.7 (1.3–2.3) | 1.4 (1.1–1.9) |
| 4 points | 139/301 (46) | 3.4 (2.5–4.6) | 2.1 (1.5–3.0) | 159/301 (53) | 3.1 (2.3–4.1) | 2.0 (1.5–2.7) |
| 5–7 points | 187/299 (63) | 5.4 (4.0–7.3) | 3.0 (2.2–4.1) | 205/299 (69) | 4.8 (3.6–6.3) | 2.8 (2.1–3.8) |
aWe used a modified version of the PRO-AGE score, excluding ‘older age (≥90 years old)’ from the algorithm.
Estimates were calculated using Cox proportional hazards models. Quartiles defined the categories of Charlson, NEWS and modified PRO-AGE scores. CI, confidence interval.
Meanwhile, NEWS and modified PRO-AGE scores were weakly associated (Spearman coefficient = 0.33; 95% CI = 0.29–0.38), suggesting that they capture different clinical phenomena (Appendix Figure S3). Accordingly, survival over 60 days varied significantly within the same quartile of NEWS, depending on the level of vulnerability (Figure 1). Similarly, classifying patients by vulnerability levels improved the prediction of time-to-death within 60 days across the quartiles of NEWS (Table 3).
Figure 1.
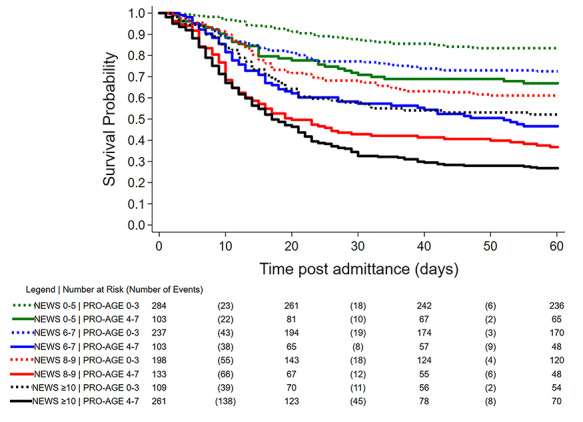
Kaplan–Meier survival curves over 60 days based on the levels of NEWS (illness acuity) and modified PRO-AGE score (vulnerability). We used a modified version of the PRO-AGE score, excluding ‘older age (≥90 years old)’ from the algorithm. Quartiles defined the categories of NEWS and modified PRO-AGE scores. For the modified PRO-AGE score, we combined the two lower and two higher quartiles, resulting in two levels of vulnerability. We censored 12 patients between 31 and 43 days of follow-up because we were unable to complete the 60 days. All pairwise comparisons between modified PRO-AGE scores: 0–3 versus 4–7 within the same stratum of NEWS resulted in a log-rank test with a P-value < 0.001.
Table 3.
Mortality in patients hospitalised with COVID-19 according to levels of NEWS (illness acuity) and modified PRO-AGE score (vulnerability)
| NEWS | PRO-AGE scoresa | Time-to-death within 60 days | ||||
|---|---|---|---|---|---|
| N died/N total (%) | Hazard ratio (95% CI) | ||||
| Crude model | P-valueb | Adjusted model | P-valueb | ||
| NEWS 0–5 | PRO-AGE 0–3 | 47/284 (17) | (reference) | (reference) | ||
| NEWS 0–5 | PRO-AGE 4–7 | 34/103 (33) | 2.3 (1.5–3.5) | <0.001 | 1.9 (1.2–2.9) | 0.005 |
| NEWS 6–7 | PRO-AGE 0–3 | 65/237 (27) | 1.8 (1.3–2.7) | 1.9 (1.3–2.7) | ||
| NEWS 6–7 | PRO-AGE 4–7 | 55/103 (53) | 4.1 (2.8–6.1) | <0.001 | 3.6 (2.4–5.3) | <0.001 |
| NEWS 8–9 | PRO-AGE 0–3 | 77/198 (39) | 2.7 (1.9–3.9) | 3.2 (2.2–4.6) | ||
| NEWS 8–9 | PRO-AGE 4–7 | 84/133 (63) | 5.7 (4.0–8.2) | <0.001 | 5.8 (4.0–8.3) | <0.001 |
| NEWS ≥ 10 | PRO-AGE 0–3 | 52/109 (48) | 3.7 (2.5–5.4) | 4.1 (2.7–6.1) | ||
| NEWS ≥10 | PRO-AGE 4–7 | 191/261 (73) | 7.2 (5.2–10.0) | <0.001 | 7.3 (5.3–10.1) | <0.001 |
Estimates were calculated using Cox proportional hazards models. The adjusted model included age, sex and Charlson comorbidity score. CI, confidence interval.
aWe used a modified version of the PRO-AGE score, excluding ‘older age (≥90 years old)’ from the algorithm. Quartiles defined the categories of NEWS and modified PRO-AGE scores; for the modified PRO-AGE score, we combined the two lower and two higher quartiles, resulting in two levels of vulnerability.
bPairwise comparisons between modified PRO-AGE scores: 0–3 versus 4–7 within the same stratum of NEWS.
Of note, in the three different prognostic models we analysed, inclusion of the modified PRO-AGE score markedly increased the accuracy in identifying those patients at high risk of mortality (Table 4).
Table 4.
Impact of the modified PRO-AGE score on the discrimination accuracy of mortality models (N = 1,428)
| Area under the ROC curve (95% CI) | |||
|---|---|---|---|
| Area under the ROC curve (95% CI) | |||
| Prognostic model | Without PRO-AGEa | With PRO-AGEa | |
| Base model = age, sex and Charlson comorbidity score | 30-day mortality | 0.66 (0.64–0.69) | 0.74 (0.71–0.76) |
| 60-day mortality | 0.66 (0.63–0.69) | 0.73 (0.71–0.76) | |
| National Early Warning Score (NEWS) | 30-day mortality | 0.71 (0.68–0.74) | 0.75 (0.73–0.78) |
| 60-day mortality | 0.71 (0.68–0.73) | 0.75 (0.73–0.78) | |
| Base model + NEWS | 30-day mortality | 0.77 (0.74–0.79) | 0.79 (0.76–0.81) |
| 60-day mortality | 0.77 (0.74–0.79) | 0.79 (0.76–0.81) | |
The ROC curve for the model including only the modified PRO-AGE score was 0.70 (95% CI = 0.68–0.73) for both 30-day and 60-day mortality. All pairwise comparisons of the ROC curves of the models with and without the modified PRO-AGE score resulted in a P-value ≤ 0.001. ROC, receiver operating characteristic; CI, confidence interval.
aWe used a modified version of the PRO-AGE score, excluding ‘older age (≥90 years old)’ from the algorithm.
Discussion
In this study, we determined that the modified version of the PRO-AGE score, a rapid vulnerability screening tool, was a strong predictor of mortality in patients with severe SARS-CoV-2 infection. Moreover, predictive models incorporating the modified PRO-AGE were more accurate than those that did not contemplate vulnerability. Our results underscore the need to assess vulnerability alongside illness acuity and other commonly used risk factors when estimating prognosis in hospitalised patients with COVID-19.
The COVID-19 pandemic has prompted the need to pay particular attention to the health of older adults, given that they account for the majority of severe cases and deaths from the SARS-CoV-2 infection [13, 23]. Nevertheless, the geriatric population is heterogeneous, and individuals can run markedly divergent courses of COVID-19 [24]. Thus, the early recognition of those who have a higher risk of mortality is challenging and depends on the adequate assessment of a broad spectrum of vulnerabilities (i.e. social, functional, cognitive and psychological issues) that often influence how older patients react to an infectious disease [11, 25]. Although the healthcare workers are already attentive to the elements of risk, such as physiological parameters, which are included in screening tools like the NEWS [8], they should capture elements of underlying vulnerability as well [9, 26]. Our results suggest that this strategy might help providers in establishing a fuller picture of COVID-19 prognosis in hospitalised older patients.
Previous studies suggested that geriatric screening tools have the potential to refine the prognostic performance of routine assessments in acute care settings [10, 27]. Similar to what we now report, these studies have shown that the combination of measures of illness acuity and vulnerability can better explain the variability of adverse outcomes in acutely ill older patients [10, 27, 28]. For example, Blomaard et al. [10] examined adults aged ≥70 years in four Dutch hospitals and showed that those with the highest vulnerability had a three-fold increase in their mortality as compared with low-vulnerability patients, independently from the Manchester Triage System categories [10]. In our study, we compared the predictive accuracy of different illness acuity tools and geriatric screening tools and confirmed the ability of the modified PRO-AGE score to identify different levels of mortality risk within the NEWS strata.
Use of the parameters measured by the NEWS and the modified PRO-AGE is also potentially advantageous because they do not require the conduct of laboratory tests or complicated computations [29]. Most items can be extracted from medical records or assessed during a brief medical evaluation. Thus, they could be particularly useful in fast-paced medical settings, where providers are hard-pressed by limited time and resources [14]. The ultimate value of our risk stratification model during the pandemic still needs to be tested. We must admit the possibility that high-risk scores could be used as a basis to move patients to end-of-life care in a biased way. However, this is a danger that resides in most prognostic assessments: measures of poor prognosis are often used to justify both the increased use of medical resources and the limitation of their use. This does not mean that we should not strive for more accurate prognostic measures. On the contrary, we must help providers make informed clinical decisions [10]. We believe that our study offers an improved framework to evaluate prognosis in patients who are hospitalised with COVID-19. It guides providers towards evaluating aspects of geriatric health on admission that are not commonly contemplated, along with other more conventional triage measures. With such information, patients and families will be better educated on what to expect during the pandemic, and health professionals will be better prepared to make recommendations [30].
Our results should be interpreted in the context of our limitations. We completed a single-centre investigation in an academic hospital from a low-to-middle income country. Also, despite our positive results adding the PRO-AGE score to the NEWS, we cannot reject the possibility that other prognostic screening tools might have even greater accuracy in COVID-19 patients. Additionally, admissions to our hospital were centrally regulated by a governmental agency, and we prioritised patients with severe cases of COVID-19. Therefore, our findings still need to be tested and validated in different settings and populations. Even so, we were able to study a large number of individuals, with minimum missing information, and our conclusions suggest that other COVID-19 patients admitted to the hospital should require early screening for detection of vulnerability.
In conclusion, vulnerability was an independent predictor of mortality in hospitalised patients with COVID-19. Providers in fast-paced acute care settings should be aware that adding information from a rapid geriatric screening tool to an illness acuity tool can improve their capacity to stratify mortality risk on admission.
Providers should be aware that combining tools such as PRO-AGE score and NEWS may help stratify the risk of death from COVID-19.
Supplementary Material
Acknowledgements
This work is part of the CO-FRAIL Study registered in the Brazilian Clinical Trials Registry (ReBEC), accessible on http://www.ensaiosclinicos.gov.br/rg/RBR-7w5zhr/. We thank the members of the CO-FRAIL Study Group and COVID-19 Study Group (C19SS) for their efforts in collecting data for our work.
Contributor Information
Márlon Juliano Romero Aliberti, Laboratorio de Investigacao Medica em Envelhecimento (LIM-66), Servico de Geriatria, Hospital das Clinicas HCFMUSP, Faculdade de Medicina, Universidade de Sao Paulo, Brazil; Research Institute, Hospital Sirio-Libanes, Sao Paulo, Brazil.
Kenneth E Covinsky, Division of Geriatrics, University of California, San Francisco, California, USA; Veterans Affairs Medical Center, San Francisco, California, USA.
Flavia Barreto Garcez, Laboratorio de Investigacao Medica em Envelhecimento (LIM-66), Servico de Geriatria, Hospital das Clinicas HCFMUSP, Faculdade de Medicina, Universidade de Sao Paulo, Brazil.
Alexander K Smith, Division of Geriatrics, University of California, San Francisco, California, USA; Veterans Affairs Medical Center, San Francisco, California, USA.
Pedro Kallas Curiati, Laboratorio de Investigacao Medica em Envelhecimento (LIM-66), Servico de Geriatria, Hospital das Clinicas HCFMUSP, Faculdade de Medicina, Universidade de Sao Paulo, Brazil; Research Institute, Hospital Sirio-Libanes, Sao Paulo, Brazil.
Sei J Lee, Division of Geriatrics, University of California, San Francisco, California, USA; Veterans Affairs Medical Center, San Francisco, California, USA.
Murilo Bacchini Dias, Laboratorio de Investigacao Medica em Envelhecimento (LIM-66), Servico de Geriatria, Hospital das Clinicas HCFMUSP, Faculdade de Medicina, Universidade de Sao Paulo, Brazil.
Victor José Dornelas Melo, Laboratorio de Investigacao Medica em Envelhecimento (LIM-66), Servico de Geriatria, Hospital das Clinicas HCFMUSP, Faculdade de Medicina, Universidade de Sao Paulo, Brazil.
Otávio Fortes do Rego-Júnior, Laboratorio de Investigacao Medica em Envelhecimento (LIM-66), Servico de Geriatria, Hospital das Clinicas HCFMUSP, Faculdade de Medicina, Universidade de Sao Paulo, Brazil.
Valéria de Paula Richinho, Laboratorio de Investigacao Medica em Envelhecimento (LIM-66), Servico de Geriatria, Hospital das Clinicas HCFMUSP, Faculdade de Medicina, Universidade de Sao Paulo, Brazil.
Wilson Jacob-Filho, Laboratorio de Investigacao Medica em Envelhecimento (LIM-66), Servico de Geriatria, Hospital das Clinicas HCFMUSP, Faculdade de Medicina, Universidade de Sao Paulo, Brazil.
Thiago J Avelino-Silva, Laboratorio de Investigacao Medica em Envelhecimento (LIM-66), Servico de Geriatria, Hospital das Clinicas HCFMUSP, Faculdade de Medicina, Universidade de Sao Paulo, Brazil.
Declaration of Sources of Funding
This work was supported by Hospital das Clinicas HCFMUSP, Faculdade de Medicina, Universidade de Sao Paulo, Brazil, from donations of the #HCComvida campaign. The funders had no role in the design of the study; collection, management, analysis and interpretation of the data; and preparation, review or approval of the manuscript.
Declaration of Conflicts of Interest
None.
References
- 1. Zhu N, Zhang D, Wang W et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med 2020;382:727–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Clark A, Jit M, Warren-Gash C et al. Global, regional, and national estimates of the population at increased risk of severe COVID-19 due to underlying health conditions in 2020: a modelling study. Lancet Glob Health 2020;8:e1003–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Farrell TW, Ferrante LE, Brown T et al. AGS position statement: resource allocation strategies and age-related considerations in the COVID-19 era and beyond. J Am Geriatr Soc 2020;68:1136–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kim I, Song H, Kim HJ et al. Use of the National Early Warning Score for predicting in-hospital mortality in older adults admitted to the emergency department. Clin Exp Emerg Med 2020;7:61–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Usman OA, Usman AA, Ward MA. Comparison of SIRS, qSOFA, and NEWS for the early identification of sepsis in the emergency department. Am J Emerg Med 2019;37:1490–7. [DOI] [PubMed] [Google Scholar]
- 6. Yiadom M, Baugh CW, Barrett TW et al. Measuring emergency department acuity. Acad Emerg Med 2018;25:65–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Liu VX, Lu Y, Carey KA et al. Comparison of early warning scoring Systems for Hospitalized Patients with and without infection at risk for in-hospital mortality and transfer to the intensive care unit. JAMA Netw Open 2020;3:e205191. doi: 10.1001/jamanetworkopen.2020.5191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hu H, Yao N, Qiu Y. Comparing rapid scoring Systems in Mortality Prediction of critically ill patients with novel coronavirus disease. Acad Emerg Med 2020;27:461–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Carpenter CR, Mooijaart SP. Geriatric screeners 2.0: time for a paradigm shift in emergency department vulnerability research. J Am Geriatr Soc 2020;68:1402–5. [DOI] [PubMed] [Google Scholar]
- 10. Blomaard LC, Speksnijder C, Lucke JA et al. Geriatric screening, triage urgency, and 30-day mortality in older emergency department patients. J Am Geriatr Soc 2020;68:1755–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Aw D, Woodrow L, Ogliari G, Harwood R. Association of Frailty with mortality in older inpatients with Covid-19: a cohort study. Age Ageing 2020. doi: 10.1093/ageing/afaa184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Zhou F, Yu T, Du R et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020;395:1054–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Guo Y, Liu X, Deng M et al. Epidemiology of COVID-19 in older persons, Wuhan, China. Age Ageing 2020;49:706–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Heeren P, Devriendt E, Wellens NIH et al. Old and new geriatric screening tools in a Belgian emergency department: a diagnostic accuracy study. J Am Geriatr Soc 2020;68:1454–61. [DOI] [PubMed] [Google Scholar]
- 15. Curiati PK, Gil-Junior LA, Morinaga CV, Ganem F, Curiati JAE, Avelino-Silva TJ. Predicting hospital admission and prolonged length of stay in older adults in the emergency department: the PRO-AGE scoring system. Ann Emerg Med 2020;76:255–65. [DOI] [PubMed] [Google Scholar]
- 16. Salvi F, Morichi V, Grilli A et al. Predictive validity of the identification of seniors at risk (ISAR) screening tool in elderly patients presenting to two Italian emergency departments. Aging Clin Exp Res 2009;21:69–75. [DOI] [PubMed] [Google Scholar]
- 17. Frenkel WJ, Jongerius EJ, Mandjes-van Uitert MJ, Munster BC, Rooij SE. Validation of the Charlson comorbidity index in acutely hospitalized elderly adults: a prospective cohort study. J Am Geriatr Soc 2014;62:342–6. [DOI] [PubMed] [Google Scholar]
- 18. Garcez FB, Aliberti MJR, Poco PCE et al. Delirium and adverse outcomes in hospitalized patients with COVID-19. J Am Geriatr Soc 2020. doi: 10.1111/jgs.16803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Smith GB, Prytherch DR, Meredith P, Schmidt PE, Featherstone PI. The ability of the National Early Warning Score (NEWS) to discriminate patients at risk of early cardiac arrest, unanticipated intensive care unit admission, and death. Resuscitation 2013;84:465–70. [DOI] [PubMed] [Google Scholar]
- 20. Churpek MM, Snyder A, Han X et al. Quick sepsis-related organ failure assessment, systemic inflammatory response syndrome, and early warning scores for detecting clinical deterioration in infected patients outside the intensive care unit. Am J Respir Crit Care Med 2017;195:906–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. McCusker J, Bellavance F, Cardin S, Trepanier S, Verdon J, Ardman O. Detection of older people at increased risk of adverse health outcomes after an emergency visit: the ISAR screening tool. J Am Geriatr Soc 1999;47:1229–37. [DOI] [PubMed] [Google Scholar]
- 22. Richardson S, Hirsch JS, Narasimhan M et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA 2020. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wu ZY, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA 2020;323:1239–42. [DOI] [PubMed] [Google Scholar]
- 24. Hewitt J, Carter B, Vilches-Moraga A et al. The effect of frailty on survival in patients with COVID-19 (COPE): a multicentre, European, observational cohort study. Lancet Public Health 2020;5:e444–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Aliberti MJR, Covinsky KE, Apolinario D et al. 10-minute targeted geriatric assessment predicts disability and hospitalization in fast-paced acute care settings. J Geront Ser A, Biol Sci Med Sci 2019;74:1637–42. [DOI] [PubMed] [Google Scholar]
- 26. Zerah L, Baudouin E, Pepin M et al. Clinical characteristics and outcomes of 821 older patients with SARS-Cov-2 infection admitted to acute care geriatric wards. J Geront Ser A, Biol Sci Med Sci 2020. doi: 10.1093/gerona/glaa210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Pulok MH, Theou O, Valk AM, Rockwood K. The role of illness acuity on the association between frailty and mortality in emergency department patients referred to internal medicine. Age Ageing 2020;1:9. doi: 10.1093/ageing/afaa089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Romero-Ortuno R, Wallis S, Biram R, Keevil V. Clinical frailty adds to acute illness severity in predicting mortality in hospitalized older adults: an observational study. Eur J Intern Med 2016;35:24–34. [DOI] [PubMed] [Google Scholar]
- 29. Liang W, Liang H, Ou L et al. Development and validation of a clinical risk score to predict the occurrence of critical illness in hospitalized patients with COVID-19. JAMA Intern Med 2020. doi: 10.1001/jamainternmed.2020.2033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Farrell TW, Francis L, Brown T et al. Rationing limited health care resources in the COVID-19 era and beyond: ethical considerations regarding older adults. J Am Geriatr Soc 2020. doi: 10.1111/jgs.16539. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


