Abstract
The coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has rapidly grown into a pandemic. According to initial reports, the lungs were thought to be the primary target, but recent case studies have shown its reach can extend to other organs including the heart and blood vessels. The severity of cardiac complications of COVID-19 depends on multiple underlying factors, with air pollutant exposure being one of them, as reported by several recent studies. Airborne particulate matter (PM) attracts heightened attention due to its implication in various diseases, especially respiratory and cardiovascular diseases. Inhaled PM not only carries microorganisms inside the body but also elicits local and systemic inflammatory responses resulting in altering the host’s immunity and increasing susceptibility to infection. Previous and recent studies have documented that PM acts as a ‘carrier’ for the virus and aids in spreading viral infections. This review presents the mechanisms and effects of viral entry and how pollution can potentially modulate pathophysiological processes in the heart. We aimed to concisely summarize studies examining cardiovascular outcomes in COVID-19 patients and postulate on how PM can influence these outcomes. We have also reviewed evidence on the use of renin–angiotensin system inhibitors, namely angiotensin-converting enzyme inhibitors and angiotensin receptor blockers, in patients with COVID-19. The interplay of pollution and SARS-CoV-2 is essential to understanding the effects of accentuated cardiovascular effects of COVID-19 and deserves in-depth experimental investigations.
Keywords: Aerosol, Airborne transmission, SARS-CoV-2, COVID-19, Particulate matter, Air pollution, Cardiovascular diseases
1. Introduction
The outbreak of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) first emerged in the Hubei province of China in December 2019 and rapidly spread worldwide to pandemic levels. The World Health Organization (WHO) officially named the novel disease coronavirus disease 2019 (COVID-19) and declared the outbreak as a public health emergency of international concern.1 It has now been >6 months since the outbreak and, as of 31 August 2020, there have been 25 251 334 confirmed cases and 846 841 fatalities reported worldwide.2 The initial clinical reports of COVID-19 predominantly showed respiratory tract symptoms, characterized by fever, cough, fatigue, pneumonia, and acute respiratory distress syndrome.3 The lungs were initially thought to be the primary target of COVID-19; however, other clinical manifestations including cardiac complications, vascular impairment, and stroke are becoming increasingly evident.4,5 As the virus affects and damages other vital organs and tissues, COVID-19 is now regarded as a systemic disease.
In the February 2020 issue of the Lancet, Huang et al.3 reported that 12% of patients with COVID-19 were diagnosed with acute myocardial injury with elevated levels of troponin I (TnI), a cardiac-specific biomarker of myocardial injury.6 In another study, severe and critical COVID-19 patients showed elevated TnI levels and presence of arrhythmias. Other markers of cardiac inflammation, such as C-reactive protein and N-terminal probrain natriuretic peptide (NT-proBNP), were also found to be elevated7 and are probably associated with infection-induced myocarditis and ischaemia.8 In addition, COVID-19 infections have been shown to be associated with heart failure and arrhythmias.10Table 1 lists several cardiovascular complications of COVID-19 reported in recent clinical studies.
Table 1.
Cardiovascular complications/presentations of COVID-19
| Cardiovascular manifestation | Study | No. of patients | Clinical outcome |
|---|---|---|---|
| Acute cardiac injury, evidenced by elevated cardiac troponin I and/or electrocardiogram and echocardiogram changes | Huang et al.3 | 5 (out of 41 patients; 12%) | 4 out of 5 required ICU care |
| Wang et al.10 | 10 (out of 138 patients; 7.2%) | More likely to end up in ICU (exact data not provided) | |
| Shi et al.11 | 82 (out of 416 patients; 19.7%) | 42 out of 82 experienced mortality (51.2%) | |
| Zhou et al.12 | 33 (out of 191 patients; 17%) | 32 out of 33 experienced mortality | |
| Arrhythmia | Wang et al.10 | 16 (out of 36 patients in the ICU; 44.4%) | Required ICU care |
| Myocarditis | Zeng et al.13 | 1 patient | Deceased |
| Sala et al.14 | 1 patient | Recovered and discharged | |
| Kim et al.15 | 1 patient | Not reported | |
| Heart failure | Zhou et al.12 | 44 (out of 191 patients; 23%) | 28 out of 44 experienced mortality |
| Fried et al.16 | 1 patient | Required mechanical ventilation | |
| Cardiomyopathy | Arentz et al.17 | 7 (out of 21 patients; 33%) | Not reported specifically for cardiomyopathy |
| Fried et al.16 | 1 patient | Stable on mechanical ventilation | |
| Venous thrombo-embolism | Wichmann et al.18 | 7 (out of 12 patients; 58%) had a DVT | 4 out of 12 patients died directly of PE |
| Lodigiani et al.19 | 28 (out of 362 patients; 7.7%) | 8 out of the 28 cases occurred in ICU patients |
ICU, intensive care unit. DVT, deep vein thrombosis
It remains arguable whether COVID-19 infection and cardiac complications are causally linked, directly associated, or if any externally modifiable factor is influencing this correlation. In a recent study by van Doremalen, it was shown that SARS-CoV-2 can remain viable and infectious in aerosols (particulate matter; PM) for hours and on surfaces for days.20 This could partially explain the reason behind the more severe fatality and transmission rates of COVID-19, unlike those observed with influenza viral infection.8 Fine PM may damage the respiratory system by inducing oxidative stress, leading to serious health problems including decreased resistance to respiratory viral infections.21 Recent literature clearly indicated that more polluted places are likely to have increased COVID-19 mortality.22,23 These are not the first studies to highlight a substantial link between air pollution levels and deaths from viral diseases. A study published in 2003 found that SARS patients were 84% more likely to die if they lived in areas with high levels of pollution, although these results were not adjusted for important confounders, such as age, gender, and other comorbid conditions.24
A key determinant of the spread of COVID-19 has been identified as population density.25 As denser populations catalyse the spread of the virus,26 the possibility of the outbreak and transmission of the disease is higher in urban areas. However, there may be an effect from ambient air pollution as increased population density is associated with increased pollution.27 The direct or indirect correlation between COVID-19 infection, cardiovascular injury, and PM pollution is the main focus of this review as we attempt to answer the question: does PM pollution act as a cofactor for viral entry into the heart and exacerbate the susceptibility and severity of cardiovascular disease (CVD) and deaths due to COVID-19?
2. Mechanisms and pathophysiological impact of viral entry into the heart
2.1. Mechanism of SARS-CoV-2 entry
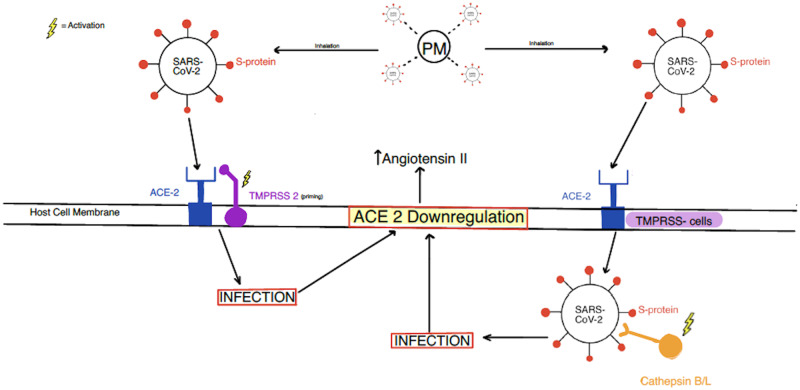
The novel coronavirus SARS-CoV-2, which is closely related to SARS-CoV, has been found to infect cardiac tissue via a similar mechanism involving angiotensin-converting enzyme 2 (ACE2).28 ACE2 is found to be expressed in a wide variety of tissues, with some of the highest levels in the lungs and heart.29,30 ACE2 converts angiotensin I and angiotensin II into potent vasodilators angiotensin 1–9 and angiotensin 1–7, respectively.31 By counteracting the vasoconstrictive actions of angiotensin II, ACE2 negatively regulates the renin–angiotensin system (RAS) and plays a role in blood pressure homoeostasis.31 The key player for viral entry into the host cells is the spike (S) protein, which is responsible for ACE2 binding and fusion to the host cell (Figure 1).28 Before the S protein can fuse, it must first be cleaved by a host cell protease known as transmembrane protease serine type 2 (TMPRSS2). This priming by TMPRSS2 is believed to be essential for cell entry by SARS-CoV-2, just as it was for SARS-CoV. In the absence of TMPRSS2, SARS-CoV was found to alternatively be primed by other host cell proteases, such as cathepsin B/L, which is also thought to be the case for SARS-CoV-2.28 Inhibition of cathepsin B/L significantly reduced SARS-CoV-2 entry, suggesting cathepsin B/L dependence. However, based on investigations of both the previous viral disease outbreaks SARS and Middle Eastern respiratory syndrome (MERS), cathepsin B/L is not believed to be essential for the viral spread and pathogenesis, unlike the priming by TMPRSS2.28
Figure 1.
Host cell entry mechanisms utilized by SARS-CoV-2. ACE2, angiotensin-converting enzyme 2; PM, particulate matter; S protein, spike protein; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; TMPRSS 2, transmembrane protease serine type 2.
2.2. Pathophysiological impact of SARS-CoV-2 on the myocardium
2.2.1. ACE2 regulation
Once SARS-CoV-2 binds to ACE2 and gains entry into the host cell, there is a subsequent down-regulation of ACE2 that results in reduced degradation of angiotensin II, a potent vasoconstrictor and culprit of endothelial damage and myocardial dysfunction.32 The resulting increased levels of circulating angiotensin II binds angiotensin II type 1 (AT1) receptors, along with sympathetic nervous system activation, are believed to contribute to the vasoconstriction and pulmonary damage that results in acute respiratory distress syndrome (ARDS).32 ACE2 can counteract the untoward effects of angiotensin II (by converting it to angiotensin 1–7) by exerting vasodilatory, anti-inflammatory, antioxidant, and antifibrotic effects.33,34 An important role for ACE2 in contributing to the cardioprotective effect was demonstrated by Loot et al.35 Their findings showed reversal of cardiac dysfunction and restoration of vascular endothelial response post-myocardial infarction (MI) after angiotensin 1–7 infusion. ACE2 gain-of-function studies revealed that it mediates favourable post-MI remodelling and recovery,36 and improved left ventricular diastolic function through reduction of oxidative stress, fibrosis, and myocardial hypertrophy.37,38 Alternatively, mice lacking ACE2 (loss of function) were more likely to develop left ventricular systolic dysfunction and heart failure with reduced ejection fraction.29
Previous experimental and clinical studies demonstrated that SARS-CoV mediates myocardial inflammation associated with ACE2 down-regulation and is likely to be responsible for the adverse cardiac outcomes in SARS patients.29 Based on previous evidence, we speculate that binding of SARS-CoV-2 is likely to alter ACE2 function, resulting in adverse cardio-respiratory effects.
2.2.2. Exaggerated immune and inflammatory response
The overwhelming inflammatory response leading to production of large quantities of cytokines, known as the ‘cytokine storm’, is an indirect mechanism by which SARS-CoV-2 damages the myocardium.9 This ‘cytokine storm’ is usually seen in more critically ill patients, such as those with ARDS and multiple organ failure.39 It has been shown that severely ill COVID-19 patients had decreased expression of interferon (IFN)-γ in CD4+ cells, along with an exaggerated release of cytokines and chemokines, resulting in damage to the host cells and tissues.40 The magnitude of the ‘cytokine storm’ strongly correlates with infection severity, as severe COVID-19 cases were found to have significantly higher levels of interleukin (IL)-6, IL-10, and tumour necrosis factor (TNF)-α, along with more severe lymphopenia compared with moderate cases.40 IL-6 not only stimulates production of other cytokines, but also contributes to vascular leakage and interstitial oedema, and has been shown to cause myocardial dysfunction.41 Indeed, inflammation has been considered as an important risk factor for long QT-syndrome (LQTS) and Torsades de pointes (TdP), primarily via direct electrophysiological effects of cytokines on the myocardium.42 A recent study revealed an association between increased levels of IL-6 and high TnI levels, indicating a ‘cytokine storm’ as a contributor to myocardial injury.43
2.2.3. Systemic effects: myocardial oxygen supply–demand mismatch
SARS-CoV-2 primarily causes pulmonary manifestations such as pneumonia and ARDS. The association between pneumonia and cardiac complications has been documented previously,44 and various studies also confirmed that extrapulmonary complications of acute respiratory infections serve as triggers of CVDs.45 Hypoxaemia and hypotension due to pulmonary dysfunction lead to insufficient oxygen supply to the myocardium. As a result of ongoing hypoxia, the cardiometabolic demand is increased in the wake of inadequate supply, further causing the imbalance between myocardial oxygen supply and demand.46 As the disease progresses, the oxygen supply–demand ratio becomes increasingly aggravated, ultimately leading to myocardial damage. Respiratory and metabolic acidosis and electrolyte and acid–base abnormalities are other systemic contributors leading to myocardial damage.47 Consequently (less cardiac output and ineffective circulating volume), the sympathetic nervous system is activated to maintain circulatory homoeostasis and perfusion to vital organs by increasing inotropy and chronotropy of the failing myocardium.48 In the long term, these mechanisms turn maladaptive by further compromising coronary perfusion49 and are responsible for disease progression leading to myocardial stunning, arrhythmias, and sudden death.50 COVID-19 = associated extra-pulmonary complications may manifest as cardiomegaly and pericardial effusion on chest computed tomography (CT) imaging.51
3. Pollution as a cofactor for increased myocardial damage in COVID-19
3.1. PM and SARS-CoV-2 interaction
Air pollution represents a serious public health issue as it ranks ninth in overall mortality worldwide,52 and hence is recognized as one of the top 10 global health burdens.53 Particularly through its impact on CVDs, it causes as many as 8.9 million premature deaths per year worldwide.54 Besides nitrogen dioxide (NO2) and ozone (O3), the current focus of research is mainly on PM (PM2.5 and PM10) as these occur frequently at elevated concentrations in large metropolitan areas. PM is comprised of solid particles and liquid droplets from various sources and are classified according to their aerodynamic diameters: coarse (PM10), fine (PM2.5), and ultrafine (PM0.1). The size, surface area, and chemical composition determine the toxicity of PM.55 According to various particle size deposition models,56,57 particles with aerodynamic diameter >10 μm deposit in the nose or extrathoracic airway, while inhaled particles of the size range 3–6 μm reach and deposit in the lower respiratory tract. Particles between 2.5 and 0.1 μm can penetrate deep into the alveolar region. In particular, PM2.5 and PM10 have been shown to act as carriers for viral spread and facilitate the prolonged survival of microorganisms,58 including viruses,59 which could partly explain the association of air pollution with the increased spread of respiratory viral infections.59 Ye et al.60 demonstrated a positive correlation between the infection rate due to respiratory syncytial virus and PM fractions (PM2.5, r = 0.446, P < 0.001; and PM10, r = 0.397, P < 0.001). Other similar studies provided evidence on the interaction between PM and viruses,61 and highlighted that an increase in PM2.5 concentration by 10 µg/m3 was associated with a higher incidence of viral infection.62
With recent studies specifically exploring the PM–SARS-CoV-2 interaction, data are now available confirming this lethal association. Experiments conducted by van Doremalen et al.20 indicated that the transmission of SARS-CoV-2 by aerosols is plausible, since it remains viable and infectious for hours and on surfaces for up to days. The first preliminary evidence showed the presence of SARS-COV-2 RNA on PM particles in Bergamo, Italy, suggesting that the virus can create clusters with the particles which can be carried and detected on PM10.63,64 The authors inferred that by creating clusters with PM, SARS-CoV-2 reduces their diffusion coefficient, which enhances the persistence of the virus in the atmosphere and could serve as an index for COVID-19 diffusion. Few other laboratory experiments on aerosol sampling have investigated the presence of SARS-CoV-2. In a recent study, Liu et al.65 analysed the presence of SARS-CoV-2 RNA in particle samples collected inside two designated hospitals in Wuhan, and quantified the copy counts of the virus using a droplet-digital-PCR-based detection method. Their data showed the presence of SARS-CoV-2 on particles of two different size ranges, one in the range of 0.25 and 1.0 μm (submicrometre) and the other >2.5 μm (supermicrometre). The authors indicated that the airborne route could be a possible pathway for contamination. Similar findings are confirmed from air samples collected at the University of Nebraska Hospital.66 The authors pointed out that SARS-CoV-2 may spread through both direct (droplet and person-to-person) and indirect mechanisms (contaminated objects and airborne transmission). More recent data from air samples collected from intensive care units to general wards of COVID-19 patients at the National Centre for Infectious Diseases, Singapore also revealed the presence of SARS-CoV-2 RNA on aerosol particles of 1–4 μm in size.67 In contrast, Ong et al.68 did not confirm the presence of airborne SARS-CoV-2 RNA, but the negative results are likely to be due to small sample size, inconsistent methodology, and dilution of the air sample because of continuous air exchanges. Based on these observations, it might be conceivable that the higher the levels of atmospheric PM, the more binding of SARS-CoV-2 and thus more chances of an individual’s exposure to the virus. These studies also underscore the need for future studies designed to detect virus RNA survivability on PM samples, especially in highly polluted countries, such as India as this vital information could serve as a biomarker for COVID-19 transmission.
3.2. PM exposure and COVID-19 lethality: supporting evidence
Several recent studies have now documented that PM acts as a medium for the aerial transport of SARS-CoV-269,70 and plays a role in exacerbating morbidity and mortality of COVID-19 patients. The Italian Society of Environmental Medicine (SIMA) was the first to hypothesize a possible link between the high COVID-19 mortality rates observed in Northern Italian regions and PM concentrations. A specific Position Paper published in March 2020 demonstrated a significant correlation between daily PM10 levels exceeding the legal limit (50 µg/m3) in the northern regions (Lombardy and in cities located in the Po valley) compared with southern regions (Rome and Southern Italy), where the diffusion and lethality of the virus were significantly lower.71 Fattorini and Regoli72 analysed the data on air pollution distribution and days exceeding regulatory limits during the last 4 years (2016–19), and years of the last decade (2010–19) in which pollution limits have been exceeded for at least 35 days. The authors highlighted that long-term air quality data were significantly correlated with cases of COVID-19 in up to 71 Italian provinces, providing further evidence that chronic exposure to atmospheric contamination may represent a favourable context for the spread of the virus. Similarly, Conticini et al.22 showed that the high levels of atmospheric pollution (PM10 and PM2.5) in Northern Italy can be considered as an additional cofactor of the high level of lethality recorded in that area. These observations corroborated the findings from China, which showed that meteorological factors, such as humidity and temperature along with air pollution, can influence COVID-19 outcomes. The authors have concluded that PM2.5 and humidity are associated with increased risk, and PM10 and temperature could substantially decrease the risk of COVID-19 incidence.73 Further, Zhu et al. demonstrated that a 10 μg/m3 increase (lag0–14: cumulative lag effect of different air pollutants from day 0 to day 14) in PM2.5, PM10, NO2, and O3 was associated with a 2.24% [95% confidence interval (CI) 1.02–3.46], 1.76% (95% CI 0.89– 2.63), 6.94% (95% CI 2.38–11.51), and 4.76% (95% CI 1.99–7.52) increase in the daily counts of COVID-19 confirmed cases, respectively.74 Similarly, a survey carried out by the Harvard School of Public Health in the USA found that an increase of 1 µg/m3 in long-term PM2.5 exposure is associated with an 8% increase in COVID-19 mortality rate.23 Yao et al.75 further found in 49 Chinese cities that COVID-19 mortality is higher where PM2.5 and PM10 concentrations were greater. In another study, Fronza et al.76 analysed PM levels in relation to COVID-19 cases from four European countries (Italy, France, Germany, and Spain) and found positive correlations between PM2.5 and infection frequency. A similar potential correlation between air pollution and COVID-19 mortality has also been described in several other studies.77,78 These initial data clearly indicated that PM not only favours the virus pathogenicity but also increased the effectiveness of virus spread (by creating a suitable microenvironment for its persistence) and mortality rates due to COVID-19. These observations also corroborate previous studies demonstrating that PM may act as a ‘carrier’ for the viral droplet nuclei, eventually leading to the spreading of viral infections.21,60
3.3. Cardiovascular effects of PM exposure
The majority of reports have focused on the pulmonary effects of PM compared with cardiovascular effects, leading to some doubt about the causal association between pollution and cardiovascular mortality. There is now convincing evidence from animal as well as human studies that PM has direct interactions at sites remote from the lungs. A study conducted in hamsters demonstrated that a substantial fraction of intratracheally instilled ultrafine particles (radiolabelled denatured albumin with diameter <100 nm) diffuses from the lungs into the systemic circulation.79 Another study in rats showed that ultrafine silver particles entered the systemic pathways after inhalation.80 Similarly, PM was shown to pass directly into the circulation in human studies.81 In contrast, a study conducted by Mills et al.82 in humans showed that inhaled carbon nanoparticles do not pass directly from the lungs into the systemic circulation. These contradictory results, therefore, show the need for more confirmatory studies. Based on the studies so far, it can be said that upon inhalation, PM particles (aerodynamic diameter 2.5–0.1 μm) travel deep into the lungs and presumably translocate into the blood stream to reach the heart. PM exposure is able to elicit indirect lung-mediated (pulmonary inflammation resulting in systemic inflammation) as well as direct cardiovascular effects (vascular dysfunction, oxidative stress, and dysregulation of calcium channels/levels) (reviewed in Tanwar et al.83). There are several experimental and epidemiological studies which have documented the deleterious direct and indirect PM-induced cardiovascular effects.84,85 In addition, positive associations between short-term air pollution and viral infections have also been reported.86 The severity of viral infections is influenced by the number of extra-pulmonary manifestations, including cardiovascular complications,87 such as myocarditis, ischaemic heart disease, and idiopathic diabetic cardiomyopathy (iDCM).87 Furthermore, due to an imbalance between increased metabolic demand and reduced cardiac reserve in the wake of viral infection, chronic CVD may become unstable.
3.4. Cardiovascular complications of COVID-19
The combined impact of (i) the PM–SARS-CoV-2 interaction, (ii) pre-existing heart conditions, and (iii) the lone effects of PM on an individual’s cardiovascular system is not yet fully elucidated. Thus, the question remains as to how PM-aided SARS-CoV-2 entry into the heart affects cardiovascular outcomes in COVID-19 patients (with or without pre-existing conditions).
Evidence from previous viral disease outbreaks, such as SARS and MERS, indicate that coronaviruses affect the cardiovascular system.88,89 Despite COVID-19’s initial categorization as a respiratory-dominant illness, many patients present with cardiovascular symptoms, such as heart palpitations and chest tightness, according to the National Health Commission of China (NHC). The NHC further stated that 11.8% of deceased COVID-19 patients without underlying CVD had evidence of substantial heart damage,9 which suggests that SARS-CoV-2 can inflict cardiac damage without any pre-existing conditions. One of the more profound effects of SARS-CoV-2 is the myocardial injury observed in some severely ill patients. One study revealed that 5 out of 41 patients with COVID-19 in Wuhan, China experienced myocardial injury, which was identified by increased levels of cardiac TnI.3 There have been more reports of acute cardiac injury evidenced by electrocardiogram and echocardiogram changes, in addition to elevated troponins.10–12,90 Additionally, there have been reports of new-onset arrhythmias particularly due to electrolyte imbalances,10,91 as well as cases of venous thrombo-embolism18,19 and cardiomyopathy.16,17 Furthermore, similar to what was seen with MERS, instances of fulminant myocarditis have also been reported in COVID-19 patients,13–15 in addition to heart failure complications.12,92
It remains unclear whether pre-existing cardiovascular conditions, such as hypertension and CVD, increase susceptibility to infection. However, there has been increasing evidence showing that severely ill COVID-19 patients have one or more pre-existing cardiovascular conditions which might have contributed to their increased susceptibility, poor prognosis, and higher mortality rates.7,93 Based on early-stage analyses of the COVID-19 outbreak in China, the Centers for Disease Control and Prevention found that the case fatality rate (CFR) for those with underlying CVD is 10.5%, the highest among all other comorbid conditions (Figure 2).94 According to the NHC, data on COVID-19 mortality cases revealed 35% of patients with a history of hypertension and 17% with underlying coronary heart disease.9 Furthermore, the systemic inflammatory response elicited by the infection, along with increased shear stress from increased coronary blood flow, can cause plaque rupture and subsequent MI in patients with underlying CAD.95 SARS-CoV-2 causes microvascular dysfunction, notably pericyte injury particularly in patients with heart failure.96 Additionally, COVID-19 infection can cause decompensation of underlying heart failure, increasing the risk for mixed shock (septic and cardiogenic).97 Further, special consideration has been suggested for those with inherited arrhythmia syndromes due to the arrhythmogenic potential of COVID-19.91 It is becoming more apparent that SARS-CoV-2 can lead to both novel cardiovascular effects and exacerbation of existing cardiovascular comorbidities, resulting in a higher rate of mortality.
Figure 2.
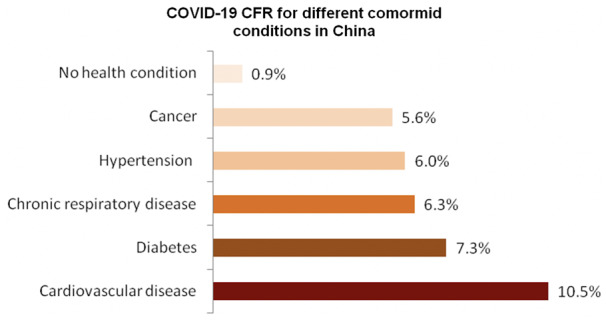
CFR for different comorbid conditions in China. The CFR is calculated by dividing the total number of deaths (n = 1023) from a disease by the number of confirmed cases (n = 44 672). The data were obtained from the Chinese Center for Disease Prevention and Control.94
3.5. Indirect (lung-mediated) cardiovascular effects of SARS-CoV-2
On both a physiological and pathological basis, a strong heart–lung connection exists. In the setting of severe pulmonary infections, the exaggerated inflammatory response induced by cytokines is thought to affect other organs, such as the heart, by ‘spilling over’ into the systemic circulation.98 This ‘spill over’ has been proposed as an indirect mechanism for myocardial injury.99 Moreover, it has also been suggested that the potential for myocardial damage seen in infected patients can be indirect due to reduced oxygen supply, severe lung failure, and/or the previously discussed cytokine storm.100 The severe hypoxia and ARDS that accompany severe respiratory infections, such as COVID-19 has been suggested as a key contributor to development of this myocardial injury,90 mainly due to oxidative stress and increased cardiometabolic demand.95 Conversely, it is proposed that the myocardial damage may be directly due to ACE2 down-regulation in the cardiac tissue,100 as discussed previously. The presence of this vigorous inflammatory response in the myocardium can also lead to myocarditis, heart failure, cardiac arrhythmias, and even sudden cardiac death.16
Despite the majority of available clinical analyses being preliminary with small sample sizes, great consideration and further investigation is warranted regarding the potential for cardiovascular complications, both direct and indirect, in COVID-19 patients.
4. Plausible mechanisms for exacerbated myocardial injury in COVID-19: role of PM exposure
First, SARS-CoV-2 infects cardiac tissue using ACE2 as ‘entry gates’ present on cardiomyocytes, pericytes, and endothelial cells96 and causes direct damage to the myocardium. It has been shown previously that chronic exposure to PM2.5 increases both pulmonary101 and circulatory ACE2 expression.102 The massive viral binding to ACE2 reduces its availability, resulting in decreased production of angiotensin 1–7 (vasodilator) and an excess of angiotensin II (vasoconstrictor). Virus-mediated depletion of ACE2 appears to be crucial in mediating cardiac injury.29,100 In an attempt to investigate how PM2.5 up-regulates ACE2 expression, Borro et al.103 recently performed a bioinformatics analysis of the ACE2 gene promoter region. The authors reported the presence of consensus sequences for the transcription factor aryl hydrocarbon receptor (AhR) in the promoter region of the ACE2 gene. AhRs primarily mediate a protective adaptive response by inducing detoxifying xenobiotic enzymes,104 microbial defence, immunity, and inflammation.105 Polycyclic aromatic hydrocarbons (PAHs) present in PM2.5 particles106 stimulate AhRs, which in turn activate the expression of target genes by binding to a DNA consensus sequence, canonical and non-canonical xenobiotic responsive elements (XRE and NC-XRE).107–109 The authors identified nine such consensus sequences in the promoter region of the ACE2 gene. Although these results provide the first evidence of pollution-induced overexpression of ACE2, the authors indicated the need for future studies to validate that AhR may control the level of ACE2 at the translational level.
We speculate that patients who were exposed to high levels of PM2.5 overexpress ACE2, which in turn facilitates more viral binding and consequent ACE2 depletion, leading to exaggerated disease response. Thus, it can be hypothesized that in areas where PM levels are high, such as Northern Italy, COVID-19 patients present with exaggerated cardiac complications.
Secondly, smaller PM particles (particles with an aerodynamic diameter ≤2.5 µm) are known to enter the heart directly via translocating into the blood stream, resulting in inflammation.83 Recent reports indicated that SARS-CoV-2 absorbs and can remain viable on the surface of PM (PM–SARS-CoV-2 interaction). The PM–SARS-CoV-2 interaction might be responsible for giving additional access to the virus in reaching distal airway/alveoli and travelling indirectly to the heart. Where exposure to PM is associated with cytokine/chemokine production and inflammation,110 SARS-CoV-2 also elicits an exaggerated host immune response.111 It is thus conceivable that both PM and SARS-CoV-2 together elicit a high grade systemic inflammatory state (‘cytokine storm’) characteristic of COVID-19.90 In this regard, the presence of myocardial inflammation and viral particles has been reported recently in the endomyocardial biopsy of a COVID-19 patient.112 Other reports in COVID-19 patients have found high viral load-induced fulminant myocarditis with inflammatory cell infiltration.41,113
Interestingly, studies have shown that inflammatory signals are capable of increasing the expression of ACE2 in the respiratory epithelium114,115 and that increased ACE2 exerts anti-inflammatory action.116–118 The crucial role of ACE2 in defending lung epithelial cells from the inflammatory action of PM2.5 has also been shown previously by Lin et al. However, in the current context, we speculate that the up-regulation of anti-inflammatory ACE2 (in response to pro-inflammatory stimuli) is unable to counteract augmented inflammation because the virus, by binding to ACE2, blocks its activity and probably contributes to severe SARS-CoV-2 infection.
Thirdly, the role of exosomes appears to be crucial in mediating COVID-19 cardiovascular pathology. Exosomes are extracellular membrane vesicles released by different cells that are capable of transferring cellular information to recipient cells. Recently, Kwon et al.119 demonstrated that secreted exosome-containing SARS-CoV-2 RNA from A549 lung epithelial cells can be taken up by human induced pluripotent stem cell-derived cardiomyocytes (hiPSC-CMs), suggesting indirect routes of viral entry into cardiomyocytes. The authors further demonstrated induction of proinflammatory genes in hiPSC-CMs, which may potentially lead to cardiac dysfunction. Supporting this observation, a recent study by Wichmann et al.18 detected SARS-CoV-2 RNA in the hearts of COVID-19 patients, which may indicate the potential involvement of exosomes in mediating viral entry into the myocardium. Interestingly, short- and long-term exposures to PM have been shown to be associated with exosome release in the lung epithelial cells120,121 and blood.122,123 Circulating exosomes are implicated in sepsis-mediated heart failure,124 whereas pulmonary exosomes mediate local and systemic inflammation.125 It is thus reasonable to propose that exosomes, released in response to PM exposure, might be serving as viral vectors carrying SARS-CoV-2 RNA to the myocardium and thus exacerbating myocardial inflammation by its own as well as virus-mediated mechanisms.
Based on the above speculations, it could be proposed that PM exposure influences the adverse cardiovascular outcomes of COVID-19 by exerting its own deleterious effects and serving as a carrier for SARS-CoV-2. Together, PM and SARS-CoV-2 exert ‘double trouble’ to the heart by altering ACE2 function and influencing the inflammatory response, thus increasing the baseline risk of complications that are known to increase the severity of viral infections (Figure 3). In a recent study, Frontera et al.126 highlighted an association between low levels of atmospheric pollution and COVID-19 presentation. The authors found that in the Italian municipality of Vo’ near Padua where atmospheric pollution levels remain relatively low (annual PM2.5 and NO2 of 19 and 14 µg/m3, respectively), an exceptionally high number of COVID-19-positive cases were present and 50–75% of the positive cases were asymptomatic. It has also been demonstrated that patients with serious COVID-19 have 60 times higher viral loads compared with mild cases, suggesting that higher viral loads might be associated with more severe clinical outcomes.127 Thus, it can be postulated that less exposure to PM2.5 could lead to lower expression of ACE2 and subsequently less viral load and mild symptoms.126
Figure 3.
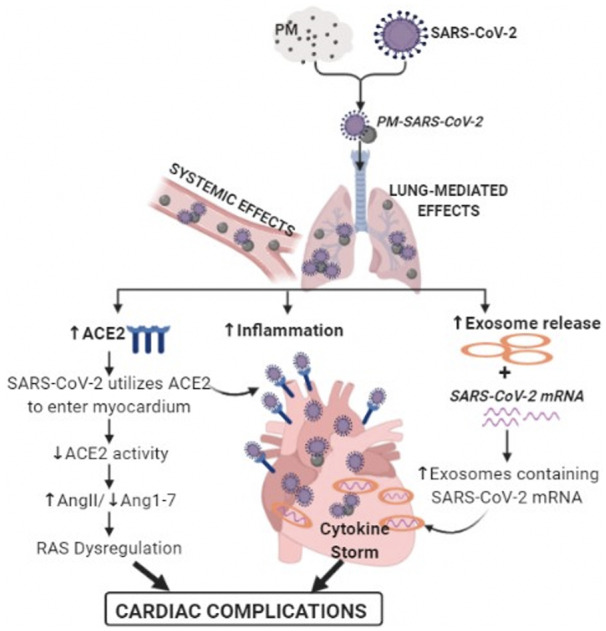
Plausible mechanisms of PM2.5-induced exacerbated cardiac injury in COVID-19. ACE2, angiotensin-converting enzyme 2; AngII, angiotensin II; Ang1-7, angiotensin 1-7; PM, particulate matter; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; RAS, renin–angiotensin system.
5. Therapeutic concern of RAS inhibitors in COVID-19
Angiotensin-converting enzyme inhibitors (ACEIs) and angiotensin II receptor blockers (ARBs) are RAS-inhibiting agents that are considered as important first-line drugs to treat hypertension, hypertrophic cardiomyopathy, and heart failure.128–130 Because of structural dissimilarity to ACE,131 RAS inhibitors do not bind and inhibit the active site of ACE2 and hence it is not their direct target. However, several clinical132–137 and laboratory studies have demonstrated increased expression of ACE2 with the use of ACEIs and ARBs,138–140 and hence they could potentially affect COVID-19 virulence in the ongoing pandemic. As uncertainty around possible associations of these drugs with COVID-19 has caused widespread debate, regulatory bodies do not support discontinuation of these medications141 and have called for outcome studies.
A retrospective study from Wuhan, China included 126 COVID-19 patients with pre-existing hypertension (43 out of 126 were on either an ACEI or an ARB) and 125 age- and sex-matched COVID-19 patients without hypertension. The clinical outcomes indicated that the use of ACEIs/ARBs is not associated with increased risk of morbidity or mortality in COVID-19 patients. Another study from China142 enrolled 1178 COVID-19 patients (362 with hypertension out of which 115 were on ACEI/ARB therapy). The results demonstrated that the percentage of patients with hypertension taking ACEIs/ARBs did not differ between those with severe and non-severe infections (32.9% vs. 30.7%; P = 0.65) nor did it differ between non-survivors and survivors (27.3% vs. 33.0%; P = 0.34). A case–control study from Lombardy, Italy, which included 6272 patients with COVID-19 and 30 759 controls showed no evidence that ACEIs or ARBs affected the risk of COVID-19.143 However, due to a higher prevalence of CVD, the use of ACEIs and ARBs was more frequent among patients with COVID-19 than among controls. A study from Spain (1139 cases and 11 390 population controls) demonstrated that RAS inhibitors do not increase the risk of COVID-19 requiring admission to hospital, including fatal cases.144 Another study using data from Danish national administrative registries concluded that prior use of ACEIs/ARBs was not significantly associated with COVID-19 diagnosis in patients with hypertension or with severe disease.145 In addition, ACEIs/ARBs were not found to be associated with COVID-19 severity in a study conducted in the USA.146 Furthermore, a few observational studies also found that ACEI/ARB use was not associated with increased severity of COVID-19 illness.142,147–154
The results from these retrospective and observational studies suggest that treatment with ACEIs or ARBs is not associated with worse outcomes in infected patients.
6. Limitations of current evidence on PM and COVID-19 association
All of the studies systemically reviewed and included in this manuscript indicate that both long- and short-term exposures to high levels of pollutants are positively correlated with increased COVID-19 contagion worldwide. However, several other critical factors responsible for the high contagiousness and fatality of COVID-19 are not considered, which could potentially have affected the end results. Hence, the analysis presented in this article may also be subject to limitations. First, in ecological75 and/or cross-sectional studies,23 (i) measures of exposure are only a proxy based in the population and, therefore, caution is required while applying grouped results to the individual level; (ii) there are potential systemic differences between areas in the measurement of exposures and recording disease frequency; (iii) there is an inability to control confounding; and (iv) there is a lack of evidence of a temporal relationship between exposure and outcomes as both are simultaneously assessed. Secondly, the presence of confounding factors may mask an actual association between the exposure and outcome. Some studies did not include variables, such as age, gender, lifestyle factors (e.g. diet or smoking habits), socio-economic status, prevalence of pre-existing conditions, such as CVD, respiratory disease, and diabetes, emotional stress, physical activity, genetic predisposition, effect of other co-pollutants and all meteorological variables, the capacity of the healthcare system, or the case identification practices (e.g. the percentage of the population that were tested and the percentage of positive tests relative to the total number of tests), which might have confounded the findings.22,72–74,102
7. Conclusion and future directions
Taken together, a compelling association between PM and SARS-CoV-2 appears to exist, and this association facilitates the longevity of virus particles in the atmosphere, increases transmission and pathogenicity, and influences the incidence and severity of COVID-19 cardiovascular outcomes. In such a context, it would be valuable to carry out additional experimental studies to (i) screen PM for virus contamination; (ii) determine the particle size to which the virus binds; (iii) confirm the presence of the SARS-CoV-2 RNA on PM; and (iv) investigate the duration for which the virus remains active and infectious in association with PM. Further investigations to study the effect of the virus within the myocardium will probably facilitate future diagnostic and therapeutic modalities that may improve treatment and management of this novel disease.
COVID-19 exerts severe pathophysiological impacts on the cardiovascular system; under this scenario, discontinuing RAS inhibitors in COVID-19 patients is unwarranted. In fact, serious complications due to discontinuation of these drugs have far more adverse consequences than the surmised adverse effects. It is likely that due to pneumonia, COVID-19 patients will experience adverse CVD outcomes in the future. Thus, follow-up studies are essential amongst survivors. Future studies also warrant detailed randomized controlled epidemiological studies in multiple geographic regions affected by COVID-19.
Conflict of interest: none declared.
Funding
This work was supported, in part, by the OSU College of Medicine Roessler Research Scholarship (J.M.A.) and National Institutes of Health R01 grants AG057046, HL139348, and ES019923 to L.E.W.
References
- 1.WHO. Novel Coronavirus—China WHO. World Health Organization. http://www.who.int/csr/don/12-january-2020-novel-coronavirus-china/en/ (24 June 2020, date last accessed).
- 2.COVID-19 pandemic. European Centre for Disease Prevention and Control. https://www.ecdc.europa.eu/en/covid-19-pandemic (24 June 2020, date last accessed).
- 3. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B.. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Avula A, Nalleballe K, Narula N, Sapozhnikov S, Dandu V, Toom S, Glaser A, Elsayegh D.. COVID-19 presenting as stroke. Brain Behav Immun 2020;87:115–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Leisman DE, Deutschman CS, Legrand M.. Facing COVID-19 in the ICU: vascular dysfunction, thrombosis, and dysregulated inflammation. Intensive Care Med 2020;46:1105–1108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Buja LM, Zehr B, Lelenwa L, Ogechukwu E, Zhao B, Dasgupta A, Barth RF.. Clinicopathological complexity in the application of the universal definition of myocardial infarction. Cardiovasc Pathol 2020;44:107153. [DOI] [PubMed] [Google Scholar]
- 7. Guo T, Fan Y, Chen M, Wu X, Zhang L, He T, Wang H, Wan J, Wang X, Lu Z.. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiol 2020;5:811–818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Madjid M, Safavi-Naeini P, Solomon SD, Vardeny O.. Potential effects of coronaviruses on the cardiovascular system: a review. JAMA Cardiol 2020;5:831–840. [DOI] [PubMed] [Google Scholar]
- 9. Zheng Y-Y, Ma Y-T, Zhang J-Y, Xie X.. COVID-19 and the cardiovascular system. Nat Rev Cardiol 2020;17:259–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, Zhao Y, Li Y, Wang X, Peng Z.. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 2020;323:1061–1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Shi S, Qin M, Shen B, Cai Y, Liu T, Yang F, Gong W, Liu X, Liang J, Zhao Q, Huang H, Yang B, Huang C.. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol 2020;5:802–810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B.. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020;395:1054–1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Zeng JH, Liu Y-X, Yuan J, Wang F-X, Wu W-B, Li J-X, Wang L-F, Gao H, Wang Y, Dong C-F, Li Y-J, Xie X-J, Feng C, Liu L.. First case of COVID-19 complicated with fulminant myocarditis: a case report and insights. Infection 2020;48:773–777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Sala S, Peretto G, Gramegna M, Palmisano A, Villatore A, Vignale D, De Cobelli F, Tresoldi M, Cappelletti AM, Basso C, Godino C, Esposito A.. Acute myocarditis presenting as a reverse Tako-Tsubo syndrome in a patient with SARS-CoV-2 respiratory infection. Eur Heart J 2020;41:1861–1862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kim I-C, Kim JY, Kim HA, Han S.. COVID-19-related myocarditis in a 21-year-old female patient. Eur Heart J 2020;41:1859–1859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Fried JA, Ramasubbu K, Bhatt R, Topkara VK, Clerkin KJ, Horn E, Rabbani L, Brodie D, Jain SS, Kirtane AJ, Masoumi A, Takeda K, Kumaraiah D, Burkhoff D, Leon M, Schwartz A, Uriel N, Sayer G.. The variety of cardiovascular presentations of COVID-19. Circulation 2020;141:1930–1936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Arentz M, Yim E, Klaff L, Lokhandwala S, Riedo FX, Chong M, Lee M.. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington State. JAMA 2020;323:1612–1614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Wichmann D, Sperhake J-P, Lütgehetmann M, Steurer S, Edler C, Heinemann A, Heinrich F, Mushumba H, Kniep I, Schröder AS, Burdelski C, de Heer G, Nierhaus A, Frings D, Pfefferle S, Becker H, Bredereke-Wiedling H, de Weerth A, Paschen H-R, Sheikhzadeh-Eggers S, Stang A, Schmiedel S, Bokemeyer C, Addo MM, Aepfelbacher M, Püschel K, Kluge S.. Autopsy findings and venous thromboembolism in patients with COVID-19. Ann Intern Med 2020;173:268–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lodigiani C, Iapichino G, Carenzo L, Cecconi M, Ferrazzi P, Sebastian T, Kucher N, Studt J-D, Sacco C, Alexia B, Sandri MT, Barco S; Humanitas COVID-19 Task Force. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb Res 2020;191:9–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN, Tamin A, Harcourt JL, Thornburg NJ, Gerber SI, Lloyd-Smith JO, de Wit E, Munster VJ.. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med 2020;382:1564–1567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ciencewicki J, Jaspers I.. Air pollution and respiratory viral infection. Inhal Toxicol 2007;19:1135–1146. [DOI] [PubMed] [Google Scholar]
- 22. Conticini E, Frediani B, Caro D.. Can atmospheric pollution be considered a co-factor in extremely high level of SARS-CoV-2 lethality in Northern Italy? Environ Pollut 2020;261:114465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wu X, Nethery R C, Sabath M B, Braun D, Dominici F. Air pollution and COVID-19 mortality in the United States: Strengths and limitations of an ecological regression analysis. Sci Adv 2020;6:eabd4049. 10.1126/sciadv.abd4049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Cui Y, Zhang Z-F, Froines J, Zhao J, Wang H, Yu S-Z, Detels R.. Air pollution and case fatality of SARS in the People’s Republic of China: an ecologic study. Environ Health 2003;2:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rocklöv J, Sjödin H. High population densities catalyse the spread of COVID-19. J Travel Med. 2020 May 18;27(3):taaa038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Rocklöv J, Sjödin H.. High population densities catalyse the spread of COVID-19. J Travel Med 2020;27:taaa038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Chen B, Kan H.. Air pollution and population health: a global challenge. Environ Health Prev Med 2008;13:94–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, Schiergens TS, Herrler G, Wu N-H, Nitsche A, Müller MA, Drosten C, Pöhlmann S.. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell 2020;181:271–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Oudit GY, Kassiri Z, Jiang C, Liu PP, Poutanen SM, Penninger JM, Butany J.. SARS-coronavirus modulation of myocardial ACE2 expression and inflammation in patients with SARS. Eur J Clin Invest 2009;39:618–625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Li M-Y, Li L, Zhang Y, Wang X-S.. Expression of the SARS-CoV-2 cell receptor gene ACE2 in a wide variety of human tissues. Infect Dis Poverty 2020;9:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Forrester SJ, Booz GW, Sigmund CD, Coffman TM, Kawai T, Rizzo V, Scalia R, Eguchi S.. Angiotensin II signal transduction: an update on mechanisms of physiology and pathophysiology. Physiol Rev 2018;98:1627–1738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Verdecchia P, Cavallini C, Spanevello A, Angeli F.. The pivotal link between ACE2 deficiency and SARS-CoV-2 infection. Eur J Intern Med 2020;76:14–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. South AM, Diz DI, Chappell MC.. COVID-19, ACE2, and the cardiovascular consequences. Am J Physiol Heart Circ Physiol 2020;318:H1084–H1090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Simões E Silva AC, Teixeira MM.. ACE inhibition, ACE2 and angiotensin-(1-7) axis in kidney and cardiac inflammation and fibrosis. Pharmacol Res 2016;107:154–162. [DOI] [PubMed] [Google Scholar]
- 35. Loot AE, Roks AJM, Henning RH, Tio RA, Suurmeijer AJH, Boomsma F, van Gilst WH.. Angiotensin-(1-7) attenuates the development of heart failure after myocardial infarction in rats. Circulation 2002;105:1548–1550. [DOI] [PubMed] [Google Scholar]
- 36. Crackower MA, Sarao R, Oudit GY, Yagil C, Kozieradzki I, Scanga SE, Oliveira-dos-Santos AJ, Costa JD, Zhang L, Pei Y, Scholey J, Ferrario CM, Manoukian AS, Chappell MC, Backx PH, Yagil Y, Penninger JM.. Angiotensin-converting enzyme 2 is an essential regulator of heart function. Nature 2002;417:822–828. [DOI] [PubMed] [Google Scholar]
- 37. Huentelman MJ, Grobe JL, Vazquez J, Stewart JM, Mecca AP, Katovich MJ, Ferrario CM, Raizada MK.. Protection from angiotensin II-induced cardiac hypertrophy and fibrosis by systemic lentiviral delivery of ACE2 in rats. Exp Physiol 2005;90:783–790. [DOI] [PubMed] [Google Scholar]
- 38. Zhong J, Basu R, Guo D, Chow FL, Byrns S, Schuster M, Loibner H, Wang X, Penninger JM, Kassiri Z, Oudit GY.. Angiotensin-converting enzyme 2 suppresses pathological hypertrophy, myocardial fibrosis, and cardiac dysfunction. Circulation 2010;122:717–728. [DOI] [PubMed] [Google Scholar]
- 39. Ye Q, Wang B, Mao J.. The pathogenesis and treatment of the ‘Cytokine Storm’ in COVID-19. J Infect 2020;80:607–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Chen G, Wu D, Guo W, Cao Y, Huang D, Wang H, Wang T, Zhang X, Chen H, Yu H, Zhang X, Zhang M, Wu S, Song J, Chen T, Han M, Li S, Luo X, Zhao J, Ning Q.. Clinical and immunological features of severe and moderate coronavirus disease 2019. J Clin Invest 2020;130:2620–2629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C, Liu S, Zhao P, Liu H, Zhu L, Tai Y, Bai C, Gao T, Song J, Xia P, Dong J, Zhao J, Wang F-S.. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med 2020;8:420–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Lazzerini PE, Capecchi PL, Laghi-Pasini F.. Systemic inflammation and arrhythmic risk: lessons from rheumatoid arthritis. Eur Heart J 2017;38:1717–1727. [DOI] [PubMed] [Google Scholar]
- 43. Santoso A, Pranata R, Wibowo A, Al-Farabi MJ, Huang I, Antariksa B.. Cardiac injury is associated with mortality and critically ill pneumonia in COVID-19: a meta-analysis. Am J Emerg Med 2020;19: doi:S0735-6757(20)30280-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Cilli A, Cakin O, Aksoy E, Kargin F, Adiguzel N, Karakurt Z, Ergan B, Mersin S, Bozkurt S, Ciftci F, Cengiz M.. Acute cardiac events in severe community-acquired pneumonia: a multicenter study. Clin Respir J 2018;12:2212–2219. [DOI] [PubMed] [Google Scholar]
- 45. Cowan LT, Lutsey PL, Pankow JS, Matsushita K, Ishigami J, Lakshminarayan K.. Inpatient and outpatient infection as a trigger of cardiovascular disease: the ARIC study. J Am Heart Assoc 2018;7:e009683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Xiong T-Y, Redwood S, Prendergast B, Chen M.. Coronaviruses and the cardiovascular system: acute and long-term implications. Eur Heart J 2020;41:1798–1800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Urso C, Brucculeri S, Caimi G.. Acid–base and electrolyte abnormalities in heart failure: pathophysiology and implications. Heart Fail Rev 2015;20:493–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Florea VG, Cohn JN.. The autonomic nervous system and heart failure. Circ Res 2014;114:1815–1826. [DOI] [PubMed] [Google Scholar]
- 49. Corrales-Medina VF, Musher DM, Shachkina S, Chirinos JA.. Acute pneumonia and the cardiovascular system. Lancet 2013;381:496–505. [DOI] [PubMed] [Google Scholar]
- 50. Packer M. Evolution of the neurohormonal hypothesis to explain the progression of chronic heart failure. Eur Heart J 1995;16: 4–6. [DOI] [PubMed] [Google Scholar]
- 51. Behzad S, Aghaghazvini L, Radmard AR, Gholamrezanezhad A.. Extrapulmonary manifestations of COVID-19: radiologic and clinical overview. Clin Imaging 2020;66:35–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, Amann M, Anderson HR, Andrews KG, Aryee M, Atkinson C, Bacchus LJ, Bahalim AN, Balakrishnan K, Balmes J, Barker-Collo S, Baxter A, Bell ML, Blore JD, Blyth F, Bonner C, Borges G, Bourne R, Boussinesq M, Brauer M, Brooks P, Bruce NG, Brunekreef B, Bryan-Hancock C, Bucello C, Buchbinder R, Bull F, Burnett RT, Byers TE, Calabria B, Carapetis J, Carnahan E, Chafe Z, Charlson F, Chen H, Chen JS, Cheng AT, Child JC, Cohen A, Colson KE, Cowie BC, Darby S, Darling S, Davis A, Degenhardt L, Dentener F, Des Jarlais DC, Devries K, Dherani M, Ding EL, Dorsey ER, Driscoll T, Edmond K, Ali SE, Engell RE, Erwin PJ, Fahimi S, Falder G, Farzadfar F, Ferrari A, Finucane MM, Flaxman S, Fowkes FG, Freedman G, Freeman MK, Gakidou E, Ghosh S, Giovannucci E, Gmel G, Graham K, Grainger R, Grant B, Gunnell D, Gutierrez HR, Hall W, Hoek HW, Hogan A, Hosgood HD, Hoy D, Hu H, Hubbell BJ, Hutchings SJ, Ibeanusi SE, Jacklyn GL, Jasrasaria R, Jonas JB, Kan H, Kanis JA, Kassebaum N, Kawakami N, Khang YH, Khatibzadeh S, Khoo JP, Kok C, Laden F, Lalloo R, Lan Q, Lathlean T, Leasher JL, Leigh J, Li Y, Lin JK, Lipshultz SE, London S, Lozano R, Lu Y, Mak J, Malekzadeh R, Mallinger L, Marcenes W, March L, Marks R, Martin R, McGale P, McGrath J, Mehta S, Mensah GA, Merriman TR, Micha R, Michaud C, Mishra V, Mohd Hanafiah K, Mokdad AA, Morawska L, Mozaffarian D, Murphy T, Naghavi M, Neal B, Nelson PK, Nolla JM, Norman R, Olives C, Omer SB, Orchard J, Osborne R, Ostro B, Page A, Pandey KD, Parry CD, Passmore E, Patra J, Pearce N, Pelizzari PM, Petzold M, Phillips MR, Pope D, Pope CA 3rd, Powles J, Rao M, Razavi H, Rehfuess EA, Rehm JT, Ritz B, Rivara FP, Roberts T, Robinson C, Rodriguez-Portales JA, Romieu I, Room R, Rosenfeld LC, Roy A, Rushton L, Salomon JA, Sampson U, Sanchez-Riera L, Sanman E, Sapkota A, Seedat S, Shi P, Shield K, Shivakoti R, Singh GM, Sleet DA, Smith E, Smith KR, Stapelberg NJ, Steenland K, Stöckl H, Stovner LJ, Straif K, Straney L, Thurston GD, Tran JH, Van Dingenen R, van Donkelaar A, Veerman JL, Vijayakumar L, Weintraub R, Weissman MM, White RA, Whiteford H, Wiersma ST, Wilkinson JD, Williams HC, Williams W, Wilson N, Woolf AD, Yip P, Zielinski JM, Lopez AD, Murray CJ, Ezzati M, AlMazroa MA, Memish ZA.. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2224–2260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Thurston G, Lippmann M.. Ambient particulate matter air pollution and cardiopulmonary diseases. Semin Respir Crit Care Med 2015;36:422–432. [DOI] [PubMed] [Google Scholar]
- 54. Lelieveld J, Klingmüller K, Pozzer A, Pöschl U, Fnais M, Daiber A, Münzel T.. Cardiovascular disease burden from ambient air pollution in Europe reassessed using novel hazard ratio functions. Eur Heart J 2019;40:1590–1596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Nel A. Atmosphere. Air pollution-related illness: effects of particles. Science 2005;308:804–806. [DOI] [PubMed] [Google Scholar]
- 56. Schroeter JD, Kimbell JS, Asgharian B.. Analysis of particle deposition in the turbinate and olfactory regions using a human nasal computational fluid dynamics model. J Aerosol Med 2006;19:301–313. [DOI] [PubMed] [Google Scholar]
- 57. Subramaniam RP, Asgharian B, Freijer JI, Miller FJ, Anjilvel S.. Analysis of lobar differences in particle deposition in the human lung. Inhal Toxicol 2003;15:1–21. [DOI] [PubMed] [Google Scholar]
- 58. Dong L, Qi J, Shao C, Zhong X, Gao D, Cao W, Gao J, Bai R, Long G, Chu C.. Concentration and size distribution of total airborne microbes in hazy and foggy weather. Sci Total Environ 2016;541:1011–1018. [DOI] [PubMed] [Google Scholar]
- 59. Silva DR, Viana VP, Müller AM, Livi FP, Dalcin PDT.. Respiratory viral infections and effects of meteorological parameters and air pollution in adults with respiratory symptoms admitted to the emergency room. Influenza Other Respi Viruses 2014;8:42–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Ye Q, Fu J-F, Mao J-H, Shang S-Q.. Haze is a risk factor contributing to the rapid spread of respiratory syncytial virus in children. Environ Sci Pollut Res Int 2016;23:20178–20185. [DOI] [PubMed] [Google Scholar]
- 61. Liang Y, Fang L, Pan H, Zhang K, Kan H, Brook JR, Sun Q.. PM2.5 in Beijing—temporal pattern and its association with influenza. Environ Health 2014;13:102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Chen G, Zhang W, Li S, Williams G, Liu C, Morgan GG, Jaakkola JJK, Guo Y.. Is short-term exposure to ambient fine particles associated with measles incidence in China? A multi-city study. Environ Res 2017;156:306–311. [DOI] [PubMed] [Google Scholar]
- 63. Setti L, Passarini F, De Gennaro G, Barbieri P, Perrone MG, Borelli M, Palmisani J, Di Gilio A, Torboli V, Fontana F, Clemente L, Pallavicini A, Ruscio M, Piscitelli P, Miani A.. SARS-Cov-2RNA found on particulate matter of Bergamo in Northern Italy: first evidence. Environ Res 2020;188:109754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Setti L, Passarini F, De Gennaro G, Barbieri P, Pallavicini A, Ruscio M, Piscitelli P, Colao A, Miani A.. Searching for SARS-COV-2 on particulate matter: a possible early indicator of COVID-19 epidemic recurrence. Int J Environ Res Public Health 2020;17:2986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Liu Y, Ning Z, Chen Y, Guo M, Liu Y, Gali NK, Sun L, Duan Y, Cai J, Westerdahl D, Liu X, Xu K, Ho K-F, Kan H, Fu Q, Lan K.. Aerodynamic analysis of SARS-CoV-2 in two Wuhan hospitals. Nature 2020;582:557–560. [DOI] [PubMed] [Google Scholar]
- 66. Santarpia JL, Rivera DN, Herrera V, Morwitzer MJ, Creager H, Santarpia GW, Crown KK, Brett-Major D, Schnaubelt E, Broadhurst MJ, Lawler JV, Reid SP, Lowe JJ.. Aerosol and surface contamination of SARS-CoV-2 observed in quarantine and isolation care. Sci Rep. 2020 Jul 29;10(1):12732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Chia PY, Coleman KK, Tan YK, Ong SWX, Gum M, Lau SK, Lim XF, Lim AS, Sutjipto S, Lee PH, Son TT, Young BE, Milton DK, Gray GC, Schuster S, Barkham T, De PP, Vasoo S, Chan M, Ang BSP, Tan BH, Leo Y-S, Ng O-T, Wong MSY, Marimuthu K; for the Singapore 2019 Novel Coronavirus Outbreak Research Team. Detection of air and surface contamination by SARS-CoV-2 in hospital rooms of infected patients. Nat Commun 2020;11:2800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Ong SWX, Tan YK, Chia PY, Lee TH, Ng OT, Wong MSY, Marimuthu K.. Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from a symptomatic patient. JAMA 2020;323:1610–1612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Contini D, Costabile F.. Does air pollution influence COVID-19 outbreaks? Atmosphere 2020;11:377. [Google Scholar]
- 70. Sasidharan M, Singh A, Torbaghan ME, Parlikad AK.. A vulnerability-based approach to human-mobility reduction for countering COVID-19 transmission in London while considering local air quality. Sci Total Environ 2020;741:140515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Setti L, Passarini F, De Gennaro G, Barbieri P, Licen S, Perrone MG, Piazzalunga A, Borelli M, Palmisani J, Di Gilio A, Rizzo E, Colao A, Piscitelli P, Miani A.. The potential role of particulate matter in the spreading of COVID-19 in Northern Italy: first evidence-based research hypotheses. BMJ Open 2020;10:e039338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Fattorini D, Regoli F.. Role of the chronic air pollution levels in the COVID-19 outbreak risk in Italy. Environ Pollut 2020;264:114732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Jiang Y, Wu X-J, Guan Y-J.. Effect of ambient air pollutants and meteorological variables on COVID-19 incidence. Infect Control Hosp Epidemiol 2020;41:1011–1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Zhu Y, Xie J, Huang F, Cao L.. Association between short-term exposure to air pollution and COVID-19 infection: evidence from China. Sci Total Environ 2020;727:138704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Yao Y, Pan J, Wang W, Liu Z, Kan H, Qiu Y, Meng X., Wang W, Association of particulate matter pollution and case fatality rate of COVID-19 in 49 Chinese cities. Science of the Total Environment 2020;741:140396. 10.1016/j.scitotenv.2020.140396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Fronza R, Lusic M, Schmidt M, Lucic B.. Spatial–temporal variations in atmospheric factors contribute to SARS-CoV-2 outbreak. Viruses 2020;12:588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Comunian S, Dongo D, Milani C, Palestini P. Air Pollution and Covid-19: The Role of Particulate Matter in the Spread and Increase of Covid-19's Morbidity and Mortality. Int J Environ Res Public Health. 2020 Jun 22;17(12):4487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Tung NT, Cheng P-C, Chi K-H, Hsiao T-C, Jones T, BéruBé K, Ho K-F, Chuang H-C.. Particulate matter and SARS-CoV-2: a possible model of COVID-19 transmission. Sci Total Environ 2021;750:141532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Nemmar A, Vanbilloen H, Hoylaerts MF, Hoet PH, Verbruggen A, Nemery B.. Passage of intratracheally instilled ultrafine particles from the lung into the systemic circulation in hamster. Am J Respir Crit Care Med 2001;164:1665–1668. [DOI] [PubMed] [Google Scholar]
- 80. Takenaka S, Karg E, Roth C, Schulz H, Ziesenis A, Heinzmann U, Schramel P, Heyder J.. Pulmonary and systemic distribution of inhaled ultrafine silver particles in rats. Environ Health Perspect 2001;109: 547–551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Nemmar A, Hoet PHM, Vanquickenborne B, Dinsdale D, Thomeer M, Hoylaerts MF, Vanbilloen H, Mortelmans L, Nemery B.. Passage of inhaled particles into the blood circulation in humans. Circulation 2002;105:411–414. [DOI] [PubMed] [Google Scholar]
- 82. Mills NL, Amin N, Robinson SD, Anand A, Davies J, Patel D, de la Fuente JM, Cassee FR, Boon NA, Macnee W, Millar AM, Donaldson K, Newby DE.. Do inhaled carbon nanoparticles translocate directly into the circulation in humans? Am J Respir Crit Care Med 2006;173:426–431. [DOI] [PubMed] [Google Scholar]
- 83. Tanwar V, Katapadi A, Adelstein JM, Grimmer JA, Wold LE.. Cardiac pathophysiology in response to environmental stress: a current review. Curr Opin Physiol 2018;1:198–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Hadei M, Naddafi K.. Cardiovascular effects of airborne particulate matter: a review of rodent model studies. Chemosphere 2020;242:125204. [DOI] [PubMed] [Google Scholar]
- 85. Dehbi H-M, Blangiardo M, Gulliver J, Fecht D, Hoogh K. D, Al-Kanaani Z, Tillin T, Hardy R, Chaturvedi N, Hansell AL.. Air pollution and cardiovascular mortality with over 25 years follow-up: a combined analysis of two British cohorts. Environ Int 2017;99:275–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Horne BD, Joy EA, Hofmann MG, Gesteland PH, Cannon JB, Lefler JS, Blagev DP, Korgenski EK, Torosyan N, Hansen GI, Kartchner D, Pope CA.. Short-term elevation of fine particulate matter air pollution and acute lower respiratory infection. Am J Respir Crit Care Med 2018;198:759–766. [DOI] [PubMed] [Google Scholar]
- 87. Sellers SA, Hagan RS, Hayden FG, Fischer WA.. The hidden burden of influenza: a review of the extra-pulmonary complications of influenza infection. Influenza Other Respir Viruses 2017;11:372–393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Yu C-M, Wong RS-M, Wu EB, Kong S-L, Wong J, Yip GW-K, Soo YOY, Chiu MLS, Chan Y-S, Hui D, Lee N, Wu A, Leung C-B, Sung JJ-Y.. Cardiovascular complications of severe acute respiratory syndrome. Postgrad Med J 2006;82:140–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Alhogbani T. Acute myocarditis associated with novel Middle east respiratory syndrome coronavirus. Ann Saudi Med 2016;36:78–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Driggin E, Madhavan MV, Bikdeli B, Chuich T, Laracy J, Biondi-Zoccai G, Brown TS, Der Nigoghossian C, Zidar DA, Haythe J, Brodie D, Beckman JA, Kirtane AJ, Stone GW, Krumholz HM, Parikh SA.. Cardiovascular considerations for patients, health care workers, and health systems during the COVID-19 pandemic. J Am Coll Cardiol 2020;75:2352–2371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Wu C-I, Postema PG, Arbelo E, Behr ER, Bezzina CR, Napolitano C, Robyns T, Probst V, Schulze-Bahr E, Remme CA, Wilde AAM.. SARS-CoV-2, COVID-19, and inherited arrhythmia syndromes. Heart Rhythm 2020;17:1456–1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Khan IH, Zahra SA, Zaim S, Harky A.. At the heart of COVID-19. J Card Surg 2020;35:1287–1294. [DOI] [PubMed] [Google Scholar]
- 93. Bonow RO, Fonarow GC, O’Gara PT, Yancy CW.. Association of coronavirus disease 2019 (COVID-19) with myocardial injury and mortality. JAMA Cardiol 2020;5:751–753. [DOI] [PubMed] [Google Scholar]
- 94.Epidemiology Working Group for NCIP Epidemic Response, Chinese Center for Disease Control and Prevention. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. Zhonghua Liu Xing Bing Xue Za Zhi 2020;41:145–151. [DOI] [PubMed] [Google Scholar]
- 95. Bansal M. Cardiovascular disease and COVID-19. Diabetes Metab Syndr 2020;14:247–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Chen L, Li X, Chen M, Feng Y, Xiong C.. The ACE2 expression in human heart indicates new potential mechanism of heart injury among patients infected with SARS-CoV-2. Cardiovasc Res 2020;116:1097–1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Goha A, Mezue K, Edwards P, Nunura F, Baugh D, Madu E.. COVID-19 and the heart: an update for clinicians. Clin Cardiol 2020;43:1216–1222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Morris A. Heart–lung interaction via infection. Annals ATS 2014;11:S52–S56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Babapoor-Farrokhran S, Gill D, Walker J, Rasekhi RT, Bozorgnia B, Amanullah A.. Myocardial injury and COVID-19: possible mechanisms. Life Sci 2020;253:117723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Guo J, Huang Z, Lin L, Lv J.. Coronavirus disease 2019 (COVID-19) and cardiovascular disease: a viewpoint on the potential influence of angiotensin-converting enzyme inhibitors/angiotensin receptor blockers on onset and severity of severe acute respiratory syndrome coronavirus 2 infection. J Am Heart Assoc 2020;9:e016219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Lin C-I, Tsai C-H, Sun Y-L, Hsieh W-Y, Lin Y-C, Chen C-Y, Lin C-S.. Instillation of particulate matter 2.5 induced acute lung injury and attenuated the injury recovery in ACE2 knockout mice. Int J Biol Sci 2018;14:253–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Wang C, Chen R, Cai J, Shi J, Yang C, Tse LA, Li H, Lin Z, Meng X, Liu C, Niu Y, Xia Y, Zhao Z, Kan H.. Personal exposure to fine particulate matter and blood pressure: a role of angiotensin converting enzyme and its DNA methylation. Environ Int 2016;94:661–666. [DOI] [PubMed] [Google Scholar]
- 103. Borro M, Di Girolamo P, Gentile G, De Luca O, Preissner R, Marcolongo A, Ferracuti S, Simmaco M.. Evidence-based considerations exploring relations between SARS-CoV-2 pandemic and air pollution: involvement of PM2.5-mediated up-regulation of the viral receptor ACE-2. Int J Environ Res Public Health 2020;17:5573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Vogel CFA, Van Winkle LS, Esser C, Haarmann-Stemmann T.. The aryl hydrocarbon receptor as a target of environmental stressors—implications for pollution mediated stress and inflammatory responses. Redox Biol 2020;34:101530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Bock KW. Aryl hydrocarbon receptor (AHR): from selected human target genes and crosstalk with transcription factors to multiple AHR functions. Biochem Pharmacol 2019;168:65–70. [DOI] [PubMed] [Google Scholar]
- 106. Wang S, Ji Y, Zhao J, Lin Y, Lin Z.. Source apportionment and toxicity assessment of PM2.5-bound PAHs in a typical iron–steel industry city in northeast China by PMF-ILCR. Sci Total Environ 2020;713:136428. [DOI] [PubMed] [Google Scholar]
- 107. Moorthy B, Chu C, Carlin DJ.. Polycyclic aromatic hydrocarbons: from metabolism to lung cancer. Toxicol Sci 2015;145:5–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Wright EJ, De Castro KP, Joshi AD, Elferink CJ.. Canonical and non-canonical aryl hydrocarbon receptor signaling pathways. Curr Opin Toxicol 2017;2:87–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Huang G, Elferink CJ.. A novel nonconsensus xenobiotic response element capable of mediating aryl hydrocarbon receptor-dependent gene expression. Mol Pharmacol 2012;81:338–347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Meng K, Wu B, Gao J, Cai Y, Yao M, Wei L, Chai T.. Immunity-related protein expression and pathological lung damage in mice poststimulation with ambient particulate matter from live bird markets. Front Immunol 2016;7:252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Shi Y, Wang Y, Shao C, Huang J, Gan J, Huang X, Bucci E, Piacentini M, Ippolito G, Melino G.. COVID-19 infection: the perspectives on immune responses. Cell Death Differ 2020;27:1451–1454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Tavazzi G, Pellegrini C, Maurelli M, Belliato M, Sciutti F, Bottazzi A, Sepe PA, Resasco T, Camporotondo R, Bruno R, Baldanti F, Paolucci S, Pelenghi S, Iotti GA, Mojoli F, Arbustini E.. Myocardial localization of coronavirus in COVID-19 cardiogenic shock. Eur J Heart Fail 2020;22:911–915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Liu K, Fang Y-Y, Deng Y, Liu W, Wang M-F, Ma J-P, Xiao W, Wang Y-N, Zhong M-H, Li C-H, Li G-C, Liu H-G.. Clinical characteristics of novel coronavirus cases in tertiary hospitals in Hubei Province. Chin Med J (Engl) 2020;133:1025–1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Yoshikawa T, Hill TE, Yoshikawa N, Popov VL, Galindo CL, Garner HR, Peters CJ, Tseng C-TK.. Dynamic innate immune responses of human bronchial epithelial cells to severe acute respiratory syndrome-associated coronavirus infection. PLoS One 2010;5:e8729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Hung Y-H, Hsieh W-Y, Hsieh J-S, Liu F-C, Tsai C-H, Lu L-C, Huang C-Y, Wu C-L, Lin C-S.. Alternative roles of STAT3 and MAPK signaling pathways in the MMPs activation and progression of lung injury induced by cigarette smoke exposure in ACE2 knockout mice. Int J Biol Sci 2016;12:454–465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Fang Y, Gao F, Liu Z.. Angiotensin-converting enzyme 2 attenuates inflammatory response and oxidative stress in hyperoxic lung injury by regulating NF-κB and Nrf2 pathways. QJM 2019;112:914–924. [DOI] [PubMed] [Google Scholar]
- 117. Shenoy V, Ferreira AJ, Qi Y, Fraga-Silva RA, Díez-Freire C, Dooies A, Jun JY, Sriramula S, Mariappan N, Pourang D, Venugopal CS, Francis J, Reudelhuber T, Santos RA, Patel JM, Raizada MK, Katovich MJ.. The angiotensin-converting enzyme 2/angiogenesis-(1-7)/Mas axis confers cardiopulmonary protection against lung fibrosis and pulmonary hypertension. Am J Respir Crit Care Med 2010;182:1065–1072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Ferreira AJ, Shenoy V, Yamazato Y, Sriramula S, Francis J, Yuan L, Castellano RK, Ostrov DA, Oh SP, Katovich MJ, Raizada MK.. Evidence for angiotensin-converting enzyme 2 as a therapeutic target for the prevention of pulmonary hypertension. Am J Respir Crit Care Med 2009;179:1048–1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Kwon Y, Nukala SB, Srivastava S, Miyamoto H, Ismail NI, Rehman J, Ong S-B, Lee WH, Ong S-G.. Detection of viral RNA fragments in human iPSC-cardiomyocytes following treatment with precipitated extracellular vesicles from SARS-CoV-2 coding-sequence-overexpressing lung epithelial cells. Stem Cell Res Ther. 2020 Nov 30;11(1):514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Bollati V, Angelici L, Rizzo G, Pergoli L, Rota F, Hoxha M, Nordio F, Bonzini M, Tarantini L, Cantone L, Pesatori AC, Apostoli P, Baccarelli AA, Bertazzi PA.. Microvesicle-associated microRNA expression is altered upon particulate matter exposure in healthy workers and in A549 cells. J Appl Toxicol 2015;35:59–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Orozco AF, Lewis DE.. Flow cytometric analysis of circulating microparticles in plasma. Cytometry A 2010;77:502–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Pergoli L, Cantone L, Favero C, Angelici L, Iodice S, Pinatel E, Hoxha M, Dioni L, Letizia M, Albetti B, Tarantini L, Rota F, Bertazzi PA, Tirelli AS, Dolo V, Cattaneo A, Vigna L, Battaglia C, Carugno M, Bonzini M, Pesatori AC, Bollati V.. Extracellular vesicle-packaged miRNA release after short-term exposure to particulate matter is associated with increased coagulation. Part Fibre Toxicol 2017;14:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Pavanello S, Bonzini M, Angelici L, Motta V, Pergoli L, Hoxha M, Cantone L, Pesatori AC, Apostoli P, Tripodi A, Baccarelli A, Bollati V.. Extracellular vesicle-driven information mediates the long-term effects of particulate matter exposure on coagulation and inflammation pathways. Toxicol Lett 2016;259:143–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Raeven P, Zipperle J, Drechsler S.. Extracellular vesicles as markers and mediators in sepsis. Theranostics 2018;8:3348–3365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Wahlund CJE, Eklund A, Grunewald J, Gabrielsson S.. Pulmonary extracellular vesicles as mediators of local and systemic inflammation. Front Cell Dev Biol 2017;5:39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Frontera A, Cianfanelli L, Vlachos K, Landoni G, Cremona G.. Severe air pollution links to higher mortality in COVID-19 patients: the ‘double-hit’ hypothesis. J Infect 2020;81:255–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Liu Y, Yan L-M, Wan L, Xiang T-X, Le A, Liu J-M, Peiris M, Poon LLM, Zhang W.. Viral dynamics in mild and severe cases of COVID-19. Lancet Infect Dis 2020;20:656–657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Romero CA, Orias M, Weir MR.. Novel RAAS agonists and antagonists: clinical applications and controversies. Nat Rev Endocrinol 2015;11:242–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, Falk V, González-Juanatey JR, Harjola V-P, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GMC, Ruilope LM, Ruschitzka F, Rutten FH, Meer PVD; ESC Scientific Document Group. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 2016;37:2129–2200. [DOI] [PubMed] [Google Scholar]
- 130. Whelton PK, Carey RM, Aronow WS, Casey DE, Collins K,D, Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA, Williamson JD, Wright JT.. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. J Am Coll Cardiol 2018;71:e127–e248. [DOI] [PubMed] [Google Scholar]
- 131. Arendse LB, Danser AHJ, Poglitsch M, Touyz RM, Burnett JC, Llorens-Cortes C, Ehlers MR, Sturrock ED.. Novel therapeutic approaches targeting the renin–angiotensin system and associated peptides in hypertension and heart failure. Pharmacol Rev 2019; 71:539–570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Sukumaran V, Veeraveedu PT, Gurusamy N, Yamaguchi K, Lakshmanan AP, Ma M, Suzuki K, Kodama M, Watanabe K.. Cardioprotective effects of telmisartan against heart failure in rats induced by experimental autoimmune myocarditis through the modulation of angiotensin-converting enzyme-2/angiotensin 1–7/mas receptor axis. Int J Biol Sci 2011;7:1077–1092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. Iwanami J, Mogi M, Tsukuda K, Wang X-L, Nakaoka H, Ohshima K, Chisaka T, Bai H-Y, Kanno H, Min L-J, Horiuchi M.. Role of angiotensin-converting enzyme 2/angiotensin-(1-7)/Mas axis in the hypotensive effect of azilsartan. Hypertens Res 2014;37:616–620. [DOI] [PubMed] [Google Scholar]
- 134. Jessup JA, Gallagher PE, Averill DB, Brosnihan KB, Tallant EA, Chappell MC, Ferrario CM.. Effect of angiotensin II blockade on a new congenic model of hypertension derived from transgenic Ren-2 rats. Am J Physiol Heart Circ Physiol 2006;291:H2166–H2172. [DOI] [PubMed] [Google Scholar]
- 135. Ishiyama Y, Gallagher PE, Averill DB, Tallant EA, Brosnihan KB, Ferrario CM.. Upregulation of angiotensin-converting enzyme 2 after myocardial infarction by blockade of angiotensin II receptors. Hypertension 2004;43:970–976. [DOI] [PubMed] [Google Scholar]
- 136. Agata J, Ura N, Yoshida H, Shinshi Y, Sasaki H, Hyakkoku M, Taniguchi S, Shimamoto K.. Olmesartan is an angiotensin II receptor blocker with an inhibitory effect on angiotensin-converting enzyme. Hypertens Res 2006;29:865–874. [DOI] [PubMed] [Google Scholar]
- 137. Soler MJ, Barrios C, Oliva R, Batlle D.. Pharmacologic modulation of ACE2 expression. Curr Hypertens Rep 2008;10:410–414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138. Karram T, Abbasi A, Keidar S, Golomb E, Hochberg I, Winaver J, Hoffman A, Abassi Z.. Effects of spironolactone and eprosartan on cardiac remodeling and angiotensin-converting enzyme isoforms in rats with experimental heart failure. Am J Physiol Heart Circ Physiol 2005;289:H1351–H1358. [DOI] [PubMed] [Google Scholar]
- 139. Burrell LM, Risvanis J, Kubota E, Dean RG, MacDonald PS, Lu S, Tikellis C, Grant SL, Lew RA, Smith AI, Cooper ME, Johnston CI.. Myocardial infarction increases ACE2 expression in rat and humans. Eur Heart J 2005;26:369–375. [DOI] [PubMed] [Google Scholar]
- 140. Tikellis C, Bialkowski K, Pete J, Sheehy K, Su Q, Johnston C, Cooper ME, Thomas MC.. ACE2 deficiency modifies renoprotection afforded by ACE inhibition in experimental diabetes. Diabetes 2008;57:1018–1025. [DOI] [PubMed] [Google Scholar]
- 141.HFSA/ACC/AHA Statement Addresses Concerns Re: Using RAAS Antagonists in COVID-19. American College of Cardiology. https://www.acc.org/latest-in-cardiology/articles/2020/03/17/08/59/hfsa-acc-aha-statement-addresses-concerns-re-using-raas-antagonists-in-covid-19 (31 August 2020, date last accessed).
- 142. Li J, Wang X, Chen J, Zhang H, Deng A.. Association of renin–angiotensin system inhibitors with severity or risk of death in patients with hypertension hospitalized for coronavirus disease 2019 (COVID-19) infection in Wuhan, China. JAMA Cardiol 2020;5:825–830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143. Mancia G, Rea F, Ludergnani M, Apolone G, Corrao G.. Renin–angiotensin–aldosterone system blockers and the risk of COVID-19. N Engl J Med 2020;382:2431–2440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144. de Abajo FJ, Rodríguez-Martín S, Lerma V, Mejía-Abril G, Aguilar M, García-Luque A, Laredo L, Laosa O, Centeno-Soto GA, Ángeles Gálvez M, Puerro M, González-Rojano E, Pedraza L, de Pablo I, Abad-Santos F, Rodríguez-Mañas L, Gil M, Tobías A, Rodríguez-Miguel A, Rodríguez-Puyol D, Barreira-Hernandez D, Zubiaur P, Santos-Molina E, Pintos-Sánchez E, Navares-Gómez M, Aparicio RM, García-Rosado V, Gutiérrez-Ortega C, Pérez C, Ascaso A, Elvira C.. MED-ACE2-COVID19 study group. Use of renin–angiotensin–aldosterone system inhibitors and risk of COVID-19 requiring admission to hospital: a case–population study. Lancet 2020;395:1705–1714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145. Fosbøl EL, Butt JH, Østergaard L, Andersson C, Selmer C, Kragholm K, Schou M, Phelps M, Gislason GH, Gerds TA, Torp-Pedersen C, Køber L.. Association of angiotensin-converting enzyme inhibitor or angiotensin receptor blocker use with COVID-19 diagnosis and mortality. JAMA 2020;324:168–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146. Reynolds HR, Adhikari S, Pulgarin C, Troxel AB, Iturrate E, Johnson SB, Hausvater A, Newman JD, Berger JS, Bangalore S, Katz SD, Fishman GI, Kunichoff D, Chen Y, Ogedegbe G, Hochman JS.. Renin–angiotensin–aldosterone system inhibitors and risk of COVID-19. N Engl J Med 2020;382:2441–2448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147. Feng Y, Ling Y, Bai T, Xie Y, Huang J, Li J, Xiong W, Yang D, Chen R, Lu F, Lu Y, Liu X, Chen Y, Li X, Li Y, Summah HD, Lin H, Yan J, Zhou M, Lu H, Qu J.. COVID-19 with different severities: a multicenter study of clinical features. Am J Respir Crit Care Med 2020;201:1380–1388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Zhang P, Zhu L, Cai J, Lei F, Qin J-J, Xie J, Liu Y-M, Zhao Y-C, Huang X, Lin L, Xia M, Chen M-M, Cheng X, Zhang X, Guo D, Peng Y, Ji Y-X, Chen J, She Z-G, Wang Y, Xu Q, Tan R, Wang H, Lin J, Luo P, Fu S, Cai H, Ye P, Xiao B, Mao W, Liu L, Yan Y, Liu M, Chen M, Zhang XJ, Wang X, Touyz RM, Xia J, Zhang BH, Huang X, Yuan Y, Loomba R, Liu PP, Li H.. Association of inpatient use of angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers with mortality among patients with hypertension hospitalized with COVID-19. Circ Res 2020;126:1671–1681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149. Meng J, Xiao G, Zhang J, He X, Ou M, Bi J, Yang R, Di W, Wang Z, Li Z, Gao H, Liu L, Zhang G.. Renin–angiotensin system inhibitors improve the clinical outcomes of COVID-19 patients with hypertension. Emerg Microbes Infect 2020;9:757–760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150. Peng YD, Meng K, Guan HQ, Leng L, Zhu RR, Wang BY, He MA, Cheng LX, Huang K, Zeng QT.. Clinical characteristics and outcomes of 112 cardiovascular disease patients infected by 2019-nCoV. Zhonghua Xin Xue Guan Bing Za Zhi 2020;48:450–455. [DOI] [PubMed] [Google Scholar]
- 151. Yang G, Tan Z, Zhou L, Yang M, Peng L, Liu J, Cai J, Yang R, Han J, Huang Y, He S. Effects of Angiotensin II Receptor Blockers and ACE (Angiotensin-Converting Enzyme) Inhibitors on Virus Infection, Inflammatory Status, and Clinical Outcomes in Patients With COVID-19 and Hypertension. Hypertension 2020;76:51–58. 10.1161/HYPERTENSIONAHA.120.15143 [DOI] [PubMed] [Google Scholar]
- 152. Zhang X, Yu J, Pan L-Y, Jiang H-Y. ACEI/ARB use and risk of infection or severity or mortality of COVID-19: A systematic review and meta-analysis. Pharmacol Res 2020;158:104927. 10.1016/j.phrs.2020.104927PMC: 32422341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Bean DM, Kraljevic Z, Searle T,Bendayan R, Kevin O’G , Pickles A, Folarin A, Roguski L, Noor K, Shek A, Zakeri R, Shah AM, Teo JTH, Dobson RJB. Angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers are not associated with severe COVID-19 infection in a multi-site UK acute hospital trust. Eur J Heart Fail. 2020 Jun;22(6):967–974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154. Rossi PG, Marino M, Formisano D, Venturelli F, Vicentini M, Grilli R; the Reggio Emilia COVID-19 Working Group. Characteristics and outcomes of a cohort of SARS-CoV-2 patients in the Province of Reggio Emilia, Italy. PLoS One 2020;15:e0238281. [DOI] [PMC free article] [PubMed] [Google Scholar]