Abstract
Aims
To elucidate the prognostic role of monocytes in the immune response of patients with coronary artery disease (CAD) at risk for life-threatening heart and lung injury as major complications of SARS-CoV-2 infection.
Methods and Results
From February to April 2020, we prospectively studied a cohort of 96 participants comprising 47 consecutive patients with CAD and acute SARS-CoV-2 infection (CAD+SARS-CoV-2), 19 CAD patients without infections, and 30 healthy controls. Clinical assessment included blood sampling, echocardiography, and electrocardiography within 12 hours of admission. Respiratory failure was stratified by the Horovitz Index (HI) as moderately/severely impaired when HI ≤ 200 mmHg. The clinical endpoint (EP) was defined as HI ≤ 200 mmHg with subsequent mechanical ventilation within a follow-up of 30 days.
The numbers of CD14dimCD16+ non-classical monocytes in peripheral blood were remarkably low in CAD+SARS-CoV-2 compared to CAD patients without infection and healthy controls (p < 0.0001). Moreover, these CD14dimCD16 monocytes showed decreased expression of established markers of adhesion, migration, and T cell activation (CD54, CD62L, CX3CR1, CD80, HLA-DR). Decreased numbers of CD14dimCD16+ monocytes were associated with the occurrence of EP. Kaplan-Meier curves illustrate that CAD+SARS-CoV-2 patients with numbers below the median of CD14dimCD16+ monocytes (median 1443 cells/mL) reached EP significantly more often compared to patients with numbers above the median (log-rank 5.03, p = 0.025).
Conclusion
Decreased numbers of CD14dimCD16+ monocytes are associated with rapidly progressive respiratory failure in CAD+SARS-CoV-2 patients. Intensified risk assessments comprising monocyte sub- and phenotypes may help to identify patients at risk for respiratory failure.
Translational Perspective
Patients with coronary artery disease (CAD) are at risk of life-threatening heart and lung injury accelerated by the pro-inflammatory and pro-thrombotic immune response during SARS-CoV-2 infection. We found substantially low numbers of CD14dimCD16+ non-classical monocytes with an altered phenotype suggesting impaired migration behaviour and T cell activation capacity in peripheral blood of SARS-CoV-2 patients with CAD, compared to CAD patients without infection or healthy controls. Decreased numbers of CD14dimCD16+ monocytes predicted rapidly progressive respiratory failure (Horovitz index ≤ 200 mmHg) with subsequent mechanical ventilation. Therefore, early sub- and phenotyping of CD14dimCD16+ monocytes using simple flow cytometry might predict worsening of respiratory failure at an early stage of SARS-CoV-2 infection in high-risk CAD patients, who require an extensive heart failure and anti-thrombotic therapy to improve their clinical outcome.
Keywords: Coronary artery disease, SARS-CoV-2 infection, respiratory failure, immuno-response, non-classical monocytes
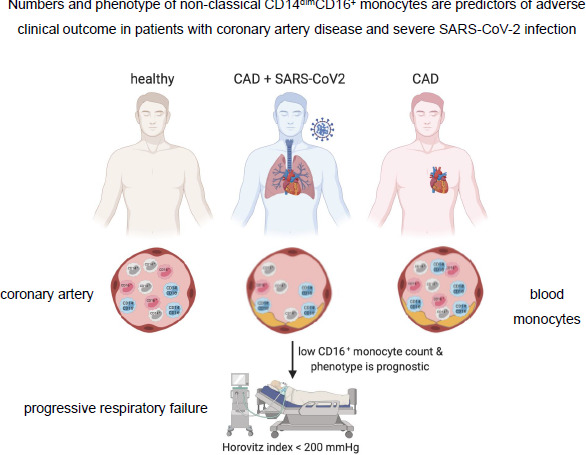
Graphical Abstract
Graphical Abstract.