Abstract
Aims
We conducted a cross-sectional survey to estimate the prevalence and clinical manifestation of disulfiram ethanol reaction (DER) and isopropanol toxicity (IT) in patients with alcohol use disorders, on disulfiram. Alcohol-based hand rub contains either ethanol or isopropanol or both. COVID-19 pandemic has led to wide scale usage of sanitizers. Patients with alcohol use disorders, on disulfiram, might experience disulfiram ethanol like reactions with alcohol-based sanitizers.
Methods
We telephonically contacted 339 patients, prescribed disulfiram between January 2014 and March 2020. The assessment pertained to the last 3 months (i.e. third week of March to third week of June 2020).
Result
The sample consisted of middle-aged men with a mean 16 years of alcohol dependence. Among the 82 (24%) patients adherent to disulfiram, 42 (12.3%) were using alcohol-based hand rubs. Out of these, a total of eight patients (19%; 95% CI 9–33) had features suggestive of DER; four of whom also had features indicative of IT. Five patients (62.5%) had mild and self-limiting symptoms. Severe systemic reactions were experienced by three (37.5%). Severe reactions were observed with exposure to sanitizers in greater amounts, on moist skin or through inhalation.
Conclusion
Patients on disulfiram should be advised to use alternate methods of hand hygiene.
Short Summary Alcohol-based hand sanitizer may lead to both disulfiram ethanol reaction and isopropanol toxicity in patients on disulfiram. The higher amount of use and probably inhalational absorption may lead to a systemic reaction. This may affect treatment adherence. Patients on disulfiram should use alternate methods of hand hygiene.
INTRODUCTION
Disulfiram is one of the time-tested and widely used long-term pharmacotherapeutic approaches for alcohol use disorders (AUD). It was approved in Sweden and Denmark in 1949, whereas the US Food and Drug Administration approved this medication in 1951 (Suh et al., 2006; Kragh, 2008).
Alcohol is metabolized to acetaldehyde by alcohol dehydrogenase. Acetaldehyde is subsequently metabolized to acetic acid by acetaldehyde dehydrogenase (ALDH). Disulfiram blocks ALDH enzyme leading to accumulation acetaldehyde. This results in a range of unpleasant symptoms, from tachycardia, headache, flushing, nausea, vomiting to cardiac arrhythmias and seizures—disulfiram ethanol reaction (DER). DER develops within 10–30 minutes after alcohol use. As disulfiram irreversibly blocks ALDH, it can take up to 2 weeks to replenish the enzyme once the medication is stopped. DER may happen with ethanol from any sources other than the alcoholic beverages (Center for Substance Abuse Treatment, 2009). Literature suggests the development of such reactions with other lower aliphatic alcohol and solvents, which usually are metabolized by the ALDH enzyme (Haddock and Wilkin, 1982; Ehrlich et al., 2012).
Alcohol-based hand rubs are frequently used as hand hygiene measures during the COVID-19 pandemic. In many public places, the use of hand sanitizers is mandatory before entry (World Health Organization, 2020). Most of the alcohol-based hand sanitizers contain between 60 and 80% isopropanol or ethanol alone or in combination.
A case report on DER in a with alcohol-based hand sanitizer has already been published from India (De Soussa, 2020). Nevertheless, DER after application of alcohol on the intact skin is a debatable entity, as the systemic absorption of alcohol through intact skin surface is minimal. In one study, it appeared that alcohol absorption from previously moist skin might explain the possibility of DER after using alcohol-based shampoo or aftershave lotion (Haddock and Wilkin, 1982). A recent commentary raised the possibility of absorption of clinically significant amounts of alcohol from pulmonary circulation while inhaling the sanitizer after local application (Brewer and Streel, 2020). All these evidences come from individual case reports, and there is a need to conduct systematic research in this area.
We aimed to estimate the prevalence and clinical manifestations of DER and isopropanol toxicity (IT) with alcohol-based hand rubs among patients with alcohol use disorder receiving disulfiram.
MATERIAL AND METHODS
Although the first case of COVID-19 was detected on 30 January, India witnessed a rapid rise in the number of cases in the first and second week of March. The Ministry of Health, among other measures, advised using alcohol-based hand rubs to minimize the risk of infection. Within the first few weeks, the high demand for hand sanitizer depleted its stock from the market. Later, it was included in the list of essential items ensuring wider availability, access and affordability.
We conducted the study among patients with alcohol use disorder receiving disulfiram from tertiary care substance use disorder treatment centers catering to patients from the entire northern and parts of western and eastern India. This study was approved by the institutional ethical committee.
Design and sample
It was a cross-sectional survey. We assessed patients who were prescribed disulfiram for maintenance treatment for alcohol use disorder between January 2014 and March 2020. Assessments were done between 21 June and 14 July 2020.
Procedure
We identified subjects and their phone numbers through an outpatient-based register and conducted telephonic interviews. A semi-structured tool was specially designed for this study. This tool consisted of four sub-sections—socio-demographic profile, alcohol-related information, disulfiram-related information (which included adherence), information on alcohol-based hand rub use and reaction-related details (Supplementary Panel 1). Treatment adherence with disulfiram was assessed with a brief adherence rating scale (Byrley et al., 2008). Assessment pertained to the last 3 months (i.e. third week of March to third week of June 2020).
Statistical analysis
The analysis was performed using MS Excel software. Descriptive analyses were expressed by appropriate statistics—mean, standard deviation, frequency and percentages. We compared the groups with or without DER, with regard to demographic and clinical variables, using either unpaired t-test and chi-square test. The confidence interval of the estimated prevalence of DER was calculated by Wilson’s method (Brown et al., 2001).
RESULTS
We contacted a total of 339 patients who were prescribed disulfiram between January 2014 and March 2020. Eighty-two (24%) of them were adherent to disulfiram for the last 3 months. Forty-two (12.3%) of them had concurrently used hand sanitizer and disulfiram. Out of these, a total of eight patients (19%; 95% CI: 9–33) had features suggestive of DER—four of whom also had features indicative of IT along with DER (Fig. 1).
Fig. 1.
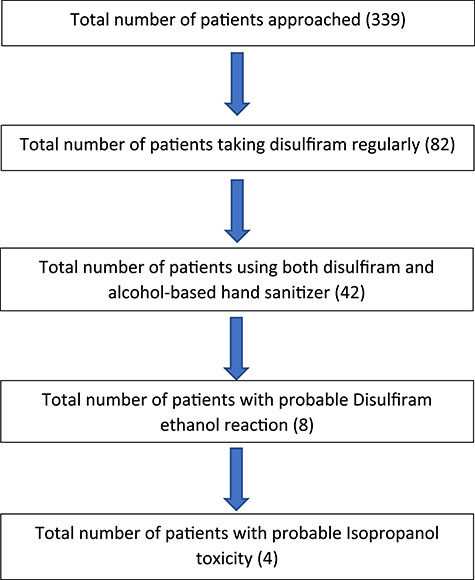
Flow diagram of recruitment of the subjects.
Clinical and demographic characteristics of the population
The population was middle-aged adult (mean age ~42 years) men with the education of up to intermediate level (mean 12.7 years). They were mostly employed (85.7%), hailing from the nuclear family (81%) and urban background (76%). On average, they had started using alcohol from their early 20s (20.4 years). The mean duration of alcohol use and dependence was 19 years (228.4 months) and 16 years (158.9 months), respectively. The average pre-treatment consumption of alcohol was around 548.7 ml of 40% alcohol. Eleven (26.2%) patients had comorbid medical illnesses. There were two cases of hypertension and one each for chronic obstructive pulmonary disease, benign prostatic hyperplasia, neuropathy, coronary artery disease (CAD), fatty liver and type 2 diabetes mellitus. The rest of the three patients had multiple physical comorbidities. Among the eight patients (19%) having comorbid psychiatric conditions, mood disorder was the most prevalent (depressive disorder in four patients and bipolar disorder in one). Two patients had comorbid anxiety spectrum disorder (one each with agoraphobia and generalized anxiety disorder), and one had a dissocial personality disorder (Supplementary Table 1). The diagnosis of comorbidities was recorded from the case files. Only three (7.1%) patients had concurrent occupational exposure to solvents and alcohol, and none of them had developed DER with hand sanitizer. The patients were using a fixed dose of 250 mg per day for a mean duration of around 1 year (54.1 weeks; median 34 weeks; range 4–260 weeks), and their mean adherence rating score was 88.3 (out of possible 100). Sixteen patients (38.1%) used predominantly liquid sanitizer, 19 patients (45.2%) used gel-based and seven patients (16.7%) used both. Eight (19%) and seven (16.7%) patients used ethanol and isopropanol-based sanitizer predominantly. Nineteen (45.2%) used both. The rest of the patients were unaware of the composition of the hand sanitizer used. On average, patients used hand sanitizer around six times per day (median, 5 times; range 1–25 times).
Clinical details of the reaction
When individual cases were examined, the usual reaction was a local irritation. In those patients, the characteristic feature was localized heat and redness usually, and on using more than the usual amount, there was a generalized reaction on the face, neck and body. One patient with pre-existing hypertensive illness had breathlessness, giddiness and confusion. Dizziness, palpitation and ataxia were standard features of IT among our patients. Five of the patients did not require medical attention. Three sought medical advice and were managed conservatively. Two of these three patients had medical comorbidity (hypertension and CAD). Treatment adherence to disulfiram was affected in three patients (37.5%). Six patients (75%) considered using alternative ways of hand sanitization (Table 1).
Table 1.
Case by case description of reaction with disulfiram
| Serial number | Age (years) | Medical comorbidity | Disulfiram ethanol reaction | Isopropanol toxicity | Need for medical attention | Sanitizer particulars | Behaviour change | Possible hypothesis | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Description | Frequency | Description | Frequency | Nature | Daily use (ml) | Change in medication adherence | Change in handwashing practice | |||||
| 1 | 51 | No | Heat and redness over face and neck, Heat and sweating all over body | Rare | NIL | NA | No | Ethanol | 6 | No | Hand wash with soap-water | Possible inhalation |
| 2 | 35 | No | More than usual amount heat and redness over hands, heat and sweating over the body | Rare | NIL | NA | No | Isopropanol | 25 | No | None | Higher amount, inhalational |
| 3 | 29 | No | Heat and sweating over hands and all over body if more amount is used, Nausea and vomiting, vertigo | Frequent | NIL | NA | No | Both | 6 | No | Hand wash with soap-water | Higher amount, inhalational |
| 4 | 37 | No | Heat and redness over hands, Occasional difficulty in breathing, Palpitations and chest discomfort, anxiety, restlessness | Frequent | NIL | NA | No | Isopropanol | 5 | Yes | Hand wash with soap-water | Usual amount—local reaction. Generalised reaction—Higher amount, inhalational |
| 5 | 41 | HTN | Difficulty in breathing, weakness, fatigue, giddiness, confusion after being sprayed with more than usual amount of sanitizer | Frequent | Dizziness, Ataxia | Rare | Yes | Isopropanol | 4 | No | Hand wash with soap-water | Higher amount and spraying inhalational |
| 6 | 42 | No | Heat and redness over face and neck, Nausea and vomiting, Difficulty in breathing, Anxiety, restlessness, Weakness, fatigue, Giddiness | Frequent | Dizziness, Palpitations | Frequent | No | Both | 15 | Yes | Hand wash with soap-water | Absorption from Moist hand |
| 7 | 40 | No | Heat and redness over hands. Self-limiting | Frequent | Dizziness, Palpitations | Frequent | No | Both | 6 | No | Non-alcoholic hand rub | Local reaction after exposure |
| 8 | 34 | CAD | Heat and redness over face and neck (no local reaction) | Once | Dizziness, palpitation, Ataxia | Once | Yes | Both | 10 | Yes | None | Systemic reaction after exposure |
We compared the group with or without any history of DER to explore potential clinical correlates. However, there were no significant differences of age, age of onset of alcohol use, age, and duration of dependence, frequencies of medical and psychiatric comorbidities.
DISCUSSION
Our study revealed that nearly one in five patients developed DER or IT with alcohol-based hand sanitizers. Forty percent of those developing reaction required medical attention. Two out of three patients who had local reactions with the usual amount of sanitizer developed more severe and systemic reactions with a higher dose, suggested a possible dose–response relationship of alcohol hand rub and disulfiram–ethanol reaction. The application of a higher dose may lead to more extensive local absorption or systemic absorption through pulmonary vasculature during the evaporation of the sanitizer. Local absorption of clinically significant amounts of alcohol from intact skin is still a debatable entity, but it may occur from moist skin (Haddock and Wilkin, 1982). This might be the etiology of reaction, at least in one of our patients. In other cases, the possible etiology may be systemic absorption of alcohol in the sanitizer, as no definite history of application on moist or breached skin was available. One of the patients was sprayed with sanitizer and developed a severe systemic reaction. A small experimental study showed that breath alcohol concentration did not rise even after 20 minutes of cutaneous exposure to alcohol-based hand sanitizer, when inhalation was restricted. However, alcohol concentration raised significantly when the subject was allowed to inhale the sanitizer after topical application (Brewer and Streel, 2020). Therefore, a possible systemic absorption of sanitizer through the pulmonary route must be avoided in patients on disulfiram. Those patients with co-existing medical disorders had greater severity of the reaction and had to seek treatment. Hence, these groups of patients should exercise caution using hand sanitizer and disulfiram (Suh et al., 2006). Clinicians might consider an alternative to disulfiram in patinets with cardiac comorbidities.
Another important finding is the presence of symptoms of isopropanol poisoning in a subgroup of patients. The common symptoms were dizziness, ataxia and palpitation. This indicates the pharmacological effect of disulfiram on the metabolism of other lower aliphatic alcohols. Literature suggests the presence of such a reaction after the local application of isopropyl alcohol, and this is more pronounced when the same is applied to hydrated skin (Haddock and Wilkin, 1982).
Nearly 40% of the patients discontinued disulfiram as a result of the reactions. Therefore, DER with hand rubs might lead to treatment non-adherence, which could trigger a subsequent relapse to alcohol.
This study has some limitations. The vast majority of patients were non-adherent to disulfiram. Although previous literature reported poor adherence, the nationwide lockdown implemented in the third week of March, too, negatively impacted treatment adherence in our patients (Williams, 2005). We could not use inferential statistics and examine the risk factors because of the overall small sample size and a lower number of patients with DER.
Nevertheless, our study had the following lessons for clinicians: (a) alcohol hand rubs can produce disulfiram ethanol like reaction in a minority, (b) of these, the majority had a mild and self-limiting response, (c) systemic response could result from inhalation of sanitizer spray, (d) higher amount of hand sanitizer use and use in moist skin would increase the risk of reaction, (e) patients with medical comorbidity should exercise special caution and (f) the experience of DER following exposure to the alcohol-based disinfectnats can increase the risk of disulfiram discontinuation putting the patients at greater risk for the resumption of alcohol use. Clinicians should inform their patients on these possibilities and advise them on use of alternate methods of hand hygiene, such as washing hands with soap water. In cases where it is not possible toavoid alcohol-based sanitizers, it is advisable to use alcohol hand rubs cautiously and preferably on dry skin. For patients, not able to adhere to the alternative hand hygiene measures, a change of medication might be considered.
Supplementary Material
Contributor Information
Abhishek Ghosh, Drug De-Addiction and Treatment CentreDepartment of Psychiatry, Post Graduate Institute of Medical Education and Research, Chandigarh, India.
Tathagata Mahintamani, Drug De-Addiction and Treatment CentreDepartment of Psychiatry, Post Graduate Institute of Medical Education and Research, Chandigarh, India.
Y P S Balhara, National Drug De-Addiction and Treatment Centre, Department of Psychiatry, All India Institute of Medical Sciences, New Delhi, India.
Fazl E Roub, Drug De-Addiction and Treatment CentreDepartment of Psychiatry, Post Graduate Institute of Medical Education and Research, Chandigarh, India.
Debashish Basu, Drug De-Addiction and Treatment CentreDepartment of Psychiatry, Post Graduate Institute of Medical Education and Research, Chandigarh, India.
Subodh BN, Drug De-Addiction and Treatment CentreDepartment of Psychiatry, Post Graduate Institute of Medical Education and Research, Chandigarh, India.
S K Mattoo, Drug De-Addiction and Treatment CentreDepartment of Psychiatry, Post Graduate Institute of Medical Education and Research, Chandigarh, India.
Eepsita Mishra, Drug De-Addiction and Treatment CentreDepartment of Psychiatry, Post Graduate Institute of Medical Education and Research, Chandigarh, India.
Babita Sharma, Drug De-Addiction and Treatment CentreDepartment of Psychiatry, Post Graduate Institute of Medical Education and Research, Chandigarh, India.
References
- Brewer C, Streel E (2020) Is alcohol in hand sanitizers absorbed through the skin or lungs? Implications for Disulfiram treatment. Alcohol Alcohol 55:354–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown, LD, Cat, TT and DasGupta, A (2001) Interval Estimation for a proportion. Statistical Science 16:101–33. [Google Scholar]
- Byerly MJ, Nakonezny PA, Rush AJ (2008) The Brief Adherence Rating Scale (BARS) validated against electronic monitoring in assessing the antipsychotic medication adherence of outpatients with schizophrenia and schizoaffective disorder. Schizophr Res 100:60–9. [DOI] [PubMed] [Google Scholar]
- Center for Substance Abuse Treatment (2009) Chapter 3 Disulfiram: How is disulfiram used In Incorporating alcohol pharmacotherapies into medical practice. Rockville, MD, 19–25. [Google Scholar]
- De Sousa A. (2020) Disulfiram ethanol reaction in a patient abstinent from alcohol caused by hand sanitizing. Alcohol Alcohol 55:349. [DOI] [PubMed] [Google Scholar]
- Ehrlich RI, Woolf DC, Kibel DA (2012) Disulfiram reaction in an artist exposed to solvents. Occup Med (Lond) 62:64–6. [DOI] [PubMed] [Google Scholar]
- Haddock NF, Wilkin JK (1982) Cutaneous reactions to lower aliphatic alcohols before and during disulfiram therapy. Arch Dermatol 118:157–9. [PubMed] [Google Scholar]
- Kragh H. (2008) From disulfiram to antabuse: The invention of a drug. Bull Hist Chem 33:82–8. [Google Scholar]
- Suh JJ, Pettinati HM, Kampman KM et al. (2006) The status of disulfiram: A half of a century later. J Clin Psychopharmacol 26:290–302. [DOI] [PubMed] [Google Scholar]
- Williams SH. (2005) Medications for treating alcohol dependence. Am Fam Physician 72:1775–80. [PubMed] [Google Scholar]
- World Health Organization (2020) Recommendations to member states to improve hand hygiene practices to help prevent the transmission of the COVID-19 virus. Interim guidance. pp. 1–3. https://www.who.int/publications/i/item/recommendations-to-member-states-to-improve-hand-hygiene-practices-to-help-prevent-the-transmission-of-the-covid-19-virus (31 July 2020, date last accessed). [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


