Abstract
Objective
A systematic review of mental health outcomes and needs of children and families during past pandemics was conducted based on the PRISMA protocol. The objectives were to evaluate the quality of existing studies on this topic, determine what is known about mental health outcomes and needs of children and families, and provide recommendations for how COVID-19 policies can best support children and families.
Methods
Seventeen studies were identified through a search of PsycINFO, PubMed, Scopus, Web of Science, and Google Scholar.
Results
Studies examining child outcomes indicate that social isolation and quarantining practices exert a substantial negative impact on child anxiety, post-traumatic stress disorder, and fear symptoms. Potential risk factors such as living in rural areas, being female, and increasing grade level may exacerbate negative mental health outcomes for children. Studies examining parental and family outcomes indicate that parents experience high stress, anxiety, and financial burden during pandemics. The age of the parent and family socioeconomic status (SES) appeared to mitigate negative outcomes, where older parents and higher SES families had lower rates of mental health problems. Parents’ fear over the physical and mental health of their children, concerns over potential job loss and arranging childcare contributes to elevated stress and poorer well-being.
Conclusions
Findings from this review suggest current gaps in COVID-19 policies and provide recommendations such implementing “family-friendly” policies that are inclusive and have flexible eligibility criteria. Examples include universal paid sick leave for parents and financial supports for parents who are also frontline workers and are at an elevated risk for contracting the disease.
Keywords: child, COVID-19, families, infectious disease outbreaks, mental health, pandemics, parents, policy
Introduction
As the number of individuals infected with the novel coronavirus began increasing at a rapid rate across the globe, the World Health Organization officially declared the COVID-19 virus a pandemic on March 11, 2020 (World Health Organization, 2020). Pandemics are infectious disease outbreaks that pose a significant public health risk, contributing to morbidity and mortality on a global scale. COVID-19 has spread to more than 200 countries, with over 6.5 million infected and upwards of 300,000 confirmed deaths worldwide (Al Jazeera, 2020). Immediate public health action took place in response to the crisis, imposing travel restrictions, infection control measures, non-essential business closures, and quarantine policies (Canadian Government, 2020).
In the initial stages of the outbreak, health authorities focused on containing the spread of the virus and researchers raced to find treatments and vaccines. Now, a few months following worldwide quarantine and social distancing measures, we are beginning to turn our attention to the psychological toll of this crisis. This is when governments must begin to consider balancing social isolation to reduce COVID-19 deaths and mental health needs to mitigate psychosocial ramifications such as child abuse, family violence, depression, substance misuse, and suicide.
As we prepare to face the challenges of the “psychosocial wave” of COVID-19, research on previous pandemics can help inform policymakers about the most prevalent mental health conditions to expect and specific measures that can be taken to mitigate negative outcomes for children and families. An example of a policy implemented in Canada during COVID-19 include the Canada Emergency Response Benefit (CERB) which was initiated to support workers laid off during COVID-19 (Canadian Government, 2020). In the United States, the CARES Act provided the Administration for Children and Families (ACF) with additional funding to aid in supporting families during the current pandemic (U.S Department of Health and Human Services, 2020). A review of the literature on previous pandemics may help identify gaps in current policies implemented during COVID-19 as they relate to children and families and contribute to informing policy-making decisions.
During emergency crisis situations, such as pandemics and other infectious disease outbreaks, parents1 must meet high demands requiring their time, energy, and access to resources to ensure the safety of their children and families. In the midst of high uncertainty, panic, and fear, parents play a crucial role in providing a stable, secure environment for their children. Responsibilities include, but are not limited to, balancing work and childcare responsibilities, providing home education, and managing infection control within their household. Beyond meeting the basic needs of their families, caregivers must also provide emotional and psychological support for their children during these challenging times. Coping with social isolation and being cut off from previously relied upon supports in the school and community may be especially difficult.
There has been a breadth of research focused on mental health impacts of natural disasters for children and families. A systematic review of 72 studies by Lai et al. (2014) found depression rates following natural disasters to range from 2% to 69% compared to rates of 1–9% found in the general population. However, the evidence for the persistence of these symptoms over time is mixed. A systematic review of ten studies conducted by Terasaka et al. (2015) found that post-traumatic stress disorder (PTSD) symptoms decrease during the first two years after a natural disaster. On the other hand, more recent studies have found that PTSD symptoms remain stable after a 6-month (Yeung et al., 2018) and 30-month follow-up (Tang et al., 2017). Researchers in this area note that more longitudinal studies are needed to make firm conclusions regarding the lasting impact of natural disasters on mental health. This body of research on the impacts of natural disasters on children and families suggests that mediators and moderators play a role and that it is not just the presence of disasters that elicit negative outcomes. Factors such as sociodemographic factors, exposure characteristics, the accumulation of negative events, personality traits, and the experience of death among close family and friends are likely to impact a child’s functioning and adaptation.
Though there are a few similarities between natural disasters and infectious disease outbreaks, there are also important distinctions. In comparison to natural disasters, pandemics involve extensive disease containment measures necessitating quarantine and social isolation measures. Furthermore, during natural disasters, recovery efforts involve communities and foreign aid working together to support those affected. In contrast, the survival of individuals and communities during pandemics requires just the opposite, social distancing and isolation, in order to reduce disease transmission. Indeed, the majority of studies examining the psychological impact of quarantine have been assessed in health care workers (Robertson et al., 2004). These studies have shown that it is a highly stressful and even traumatic experience for adults. One exception that examined the impact of quarantine on children found that children being isolated were four times more likely to show PTSD symptoms compared to families who were not isolated (Sprang & Silman, 2013). Thus, the impact of pandemics on the mental health outcomes of children and their families must be explored as a distinct phenomenon apart from natural disaster research. Because the repercussions of pandemics can be attenuated through timely interventions, there are strong ethical and public health reasons to understand the potential negative impacts and the most effective ways to intervene.
To examine the impact of pandemics on mental health outcomes of children between the ages of 0–18 years and their parents, we reviewed quantitative, qualitative, and mixed methods studies. An evaluation of the quality of studies and risk of bias was also conducted. We conclude with evidence-based recommendations on how policymakers can improve their efforts to mitigate the negative psychological effects of COVID-19.
Methods
Design
A systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guidelines (Moher et al., 2009). The review protocol was registered in advance on PROSPERO (Record ID 179437).
Search Strategy
The current study included quantitative, qualitative, and mixed methods studies published in English originating from a wide range of countries. The search was restricted to include studies published in the last 20 years from 2000 to 2020 in order to examine the most relevant research in this area (Dray et al., 2015). The first author conducted the initial search using the following databases: PsycInfo [2000—Present], PubMed [2000—Present], Scopus [2000—Present], Web of Science [2000—Present], and Google Scholar [2000—Present] on April 7, 2020. A second search was done by the first author and a university librarian on April 15 without language restrictions. The search criteria and results were verified by V. Fong, A. Chan, and A.V. Depending on the database and database-appropriate syntax, the following MeSH terms or keywords included: “child” OR “infant” OR “adol*” OR “youth” OR “pediatric” OR “paediatric” combination with “parent” OR “caregiver” OR “mother” OR “father” OR “famil*” OR “household” AND “infectious disease outbreak” OR “pandemic” OR “epidemic” OR “COVID-19” OR “H1N1” OR “swine flu” OR “H5N9” OR “coronavirus” OR “avian flu” OR “SARS” OR “severe acute respiratory syndrome” OR “coronavirus”. Articles were screened by V. Fong, A. Chan, and A. Vega on the title and abstract.
Inclusion/Exclusion Criteria
The review studied the impacts of pandemics on child and/or parent mental health and families’ information needs. Studies were included if they described empirical research with a focus on child and/or parent mental health outcomes and their information needs during pandemics, specifically COVID-19, SARS, H1N1, and H5N1. All studies utilizing qualitative, quantitative, and mixed methods study designs were considered. Studies were included from all regions of the world. Research that investigated attitudes toward immunizations or did not report on child or parent outcomes were excluded. Furthermore, single-subject case studies, reviews, studies addressing other viruses, and mathematical modeling studies were excluded.
Data Extraction
Data extraction was conducted on the 17 included studies by the first author (V. Fong) using a standardized form on Microsoft Excel. Data were extracted from each study on: (a) the location of the study and pandemic (country where the study was conducted and the type of pandemic studied); (b) quality assessment scores and risk of bias (percentages were determined based on the MMAT and items failing to meet criteria were reported); (c) population and sampling technique (whether participants were children, parents or both, method for selecting participants); (d) age of the child and/or parent; (e) timing of the assessment (dates when data collection occurred); (f) control of comparison group; (g) research type/study design (study methodology, data collection methods); (h) primary outcome measures (the name or type of scale used and the mental health outcome assessed); (i) main findings (predictors of mental health outcomes, mitigating factors identified); (j) recommendations suggestions by the authors for how to minimize negative impacts on children and/or parents. Duplicate extraction by an independent research assistant (A. Chan) was used to reduce the risk of bias and mistakes during data collection. Disagreements at this stage were resolved via consensus.
Data Synthesis
All studies were evaluated using a combination of techniques such as vote counting, presenting data in tables, and narrative synthesis. This approach was chosen due to the methodological variability across studies where meta-analysis was not feasible.
Quality Assessment and Risk of Bias
The Mixed Methods Appraisal Tool, version 2018 (MMAT; Hong et al., 2018) was utilized to assess the quality of each study included in the review. This tool has been validated and is widely used in systematic reviews including both qualitative and quantitative studies. Two reviewers (V. Fong, A.V.) independently completed the quality assessment on each article meeting inclusion criteria. The MMAT was appropriate for the current study as it allows for the evaluation of study quality and risk of bias for all empirical literature (qualitative, quantitative, and mixed methods). There are 5 sets of criteria for each study methodology and each criterion are rated on a pass (1) or fail (0) basis. For example, the criteria for qualitative studies were as follows: (a) Is the qualitative approach appropriate to answer the research question? (b) Are the qualitative data collection methods adequate to address the research question? (c) Are the findings adequately derived from the data? (d) Is the interpretation of results sufficiently substantiated by data? (e) Is there coherence between qualitative data sources, collection, analysis and interpretation? For a full description of criteria for each study methodology refer to Hong et al. (2018). The quality of a particular study was determined by calculating the percentage of criteria met (e.g., if a study met 4/5 of the MMAT criteria it would receive a total score of 80%). The authors of this tool do not provide cutoff scores that differentiate high- versus low-quality studies but recommend that reviewers conducting quality assessments define their own parameters. Given the relatively recent development of the MMAT and the lack of research on this tool specifically in mental health outcomes of children and families, any study receiving a score of 60% or more was considered satisfactory. Based on this cutoff, there were no studies excluded from the current review. Each study’s quality score percentage and unmet criteria are reported in Table I and discussed in the results.
Table I.
Study Characteristics and Main Findings
| Study | Location and pandemic | Study quality score and missing items | Population and sampling technique | Age of child and/or parent | Timing of assessment | Control or comparison group? | Research type/study design | Primary outcome measures | Main findings | Recommendations |
|---|---|---|---|---|---|---|---|---|---|---|
| Koller et al. (2006) | Toronto, Canada; SARS | 100% | Pediatric patients admitted to hospital for suspected SARS; purposive sampling | Children (N = 5) aged 6–18 years; parents (N = 10) | A month after hospital discharge during the SARS outbreak in 2003 | No | Qualitative study; interviews | Interviews focused on knowledge of SARS, understanding of infection policies, and coping; Thematic analysis was used. | Themes identified in the interviews related to negative emotional impacts, communication difficulties, and changes in parental and professional roles. | Despite isolation, family members need to make use of technology to keep in contact with their social networks. Emphasis on family-centered care and shared decision making between health care professionals and parents. |
| Dodgson et al. (2010) | Hong Kong; SARS | 80%; missing detailed information about data analysis methods | Chinese mothers who delivered healthy infants during the SARS outbreak; purposive sampling | Mothers (N = 8) aged between 28 and 38 years; infants had a mean age of 38.36 weeks | Specific date not provided but occurred during the outbreak | No | Qualitative study: interviews | Interviews focused on mothers’ experiences of parenting and the impact of the pandemic on post-partum mothering; thematic analysis was used. | Themes identified were living with uncertainty, heightened vigilance, financial burden, and isolation. | Parents expressed a need for information regarding how to care for themselves and their children during pandemics. Health care providers need to address parents’ anxieties and fears that impact the quality of life of their children, family, and themselves. |
| Fung and Loke (2010) | Hong Kong; SARS | 60%; sample representativeness; lack of validated measures | Hong Kong families with young children; convenience sampling | The majority of parents (N = 198) were aged 26–35 years; children aged 1–15 years | Between March and September in 2008 | No | Quantitative study; cross-sectional | Parent-reported questionnaire: disaster preparedness, sources of information. | Families’ information needs prioritize how to keep their families safe during emergency crisis situations. Families report the television and radio as major sources of their information. | Many parents feel unprepared during these times. Public health agencies need to provide information to families on how to adequately prepare and should use checklists and guidelines to support decision-making. |
| Effler et al. (2010) | Perth, Western Australia; H1N1 | 60%; non-response bias and lack of validated measures | Parents of children who experienced school closures in response to the pandemic; stratified sampling | Parents (N = 233) of children aged 5–13 years | June 22, 2009 to July 3, 2009 | No | Quantitative study; cross-sectional | Parent-reported questionnaire: the need for special childcare arrangements due to school closure, child’s compliance with social distancing. | 90% of parents reported that the pandemic caused minimal or no anxiety for their children. Based on parent reports, children exhibited low compliance with social distancing recommendations (25%). 50% of parents reported missing work. | Given low compliance of social distancing in children, public health officials need to inform parents about why quarantine during school closures is essential for the survival and health of the community. |
| Kavanagh et al. (2011) | Melbourne, Australia; H1N1 | 60%; non-response bias; lack of validated measures | Parents of children who experienced school closures in response to the pandemic; stratified sampling | Parents (N = 314) of school age children | November to December 2009 | No | Quantitative study; cross-sectional | Parent-reported questionnaire: understanding of quarantine recommendations, information sources, perceptions of usefulness of information, and child’s compliance with social distancing. | Major sources of parents’ information come from the schools, health department, and the media. | Consistent messages across media sources is crucial. The government should work collaboratively with the media to provide clear, accurate, and consistent information. |
| Chen et al. (2011) | Taiwan; H1N1 | 60%; non-response bias; lack of validated measures | Caregivers of children who experienced school closures in response to the pandemic; convenience sampling | Caregivers (N = 232) of children in one randomly selected class in each grade from kindergarten to grade 6. | June 1, 2009 | No | Quantitative study; cross-sectional | Caregiver-reported questionnaire: child’s compliance with social distancing, childcare arrangements, economic impact of workplace absenteeism, wage loss, childcare expenses. | Parents reported workplace absence (27%), wage loss (18%), and expenses related to childcare (2%). They also reported concerns over their child’s education and missed school work. | Despite school closures, teachers may support families by continuing with remote teaching and monitoring of children during this time. |
| Remmerswaal and Muris (2011) | Netherlands; H1N1 | 80%; non-response bias | Parents of children from 3 primary schools in the Netherlands; convenience sampling | Parents and their children (N = 223) aged 7–12 years | November 2009 at the peak of the Swine Flu | No | Quantitative study; cross-sectional | Parent and child-reported on the following measures: Fear of Swine Flu Questionnaire (FSFQ), Sources of Information about the Swine Flu Scale (SISFS), and the Fear Survey Schedule for Children-Revised (FSSC-R). | Parent and child fear of the H1N1 were positively correlated. Parent delivery of threat information was positively correlated with children’s fear even after controlling for other sources (e.g. friends, media, school). | Parents need to be cognizant of the developmental level of their child when they communicate potentially threatening information about pandemics in their households. |
| Basurto-Dávila et al. (2013) | Argentina; H1N1 | 60%; non-response bias; lack of validated measures | Households of children who experienced school closures in response to the pandemic; convenience sampling | Parents (N = 266) of children aged 6–15 years | September 7–18, 2009 | No | Quantitative study; cross-sectional | Parent-reported questionnaire: childcare arrangements and costs, wage loss, and child compliance with social distancing. | Families report a substantial financial burden as a result of pandemics. Non-childcare expenses and loss of wages were more common in low SES families. Parents are very concerned about their child’s education during school closures. | Distance learning may be more feasible in middle- and high-income households. Policies need to address the disproportionate impact on low SES families in their strategies. |
| Sprang and Silman (2013) | United States and Mexico; H1N1 | 60%; limited reporting and description of qualitative analytic methods and results | Parents from 8 sample states; “Follow the virus” sampling method with an emphasis on areas most severely impacted by H1N1 | Parents (N = 398) aged 18–67 years | Spring 2009 | Yes; comparison group from Toronto, Canada | Mixed Methods; interviews, focus groups, surveys | Parent-reported questionnaire: experiences and anticipated needs during the pandemic, experiences with isolation, sources of trust in information, UCLA Posttraumatic Stress Disorder Reaction Index (PTSD-RI), PTSD Check List-Civilian Version (PCL-C); interviews focused on psychosocial impact on children and parents. | Children and parents who were quarantined were more likely to meet clinical criteria for PTSD. Parent and child PTSD symptoms were found to be correlated. | Social isolation and quarantine measures need to ensure they minimize negative mental health impacts in children and families. Screening for PTSD may be required in both children and their parents. |
| Mizumoto et al. (2013) | Japan; H1N1 | 60%; response rate was not provided; lack of validated measures | Parents of children who experienced school closures during the pandemic; respondent-driven sampling | Parents (N = 181) of children aged 4–17 years | October 2009 to May 2010 | No | Quantitative study; cross-sectional | Parent-reported questionnaire: child compliance with social distancing, parental absenteeism, childcare arrangements. | Families with younger children were more likely to be absent from work for a longer duration especially those requiring special childcare arrangements. | Government policies need to support families especially with younger children by providing a paid leave of absence during school closures. |
| King et al. (2018) | Sydney, Australia; H1N1 | 60%; non-response bias; lack of validated measures | Parents from childcare centers were surveyed and interviewed; convenience sampling | 37 parents participated in the interviews; 431 parents completed the survey; majority of parents aged between 31 and 40 years; children aged 6 months–5 years |
Survey: November—December 2009 Interview: June 2009—May 2011 |
No | Mixed methods; surveys and interviews | Parent-reported questionnaire: parental information seeking, trusted sources and information needs; interviews focused on parental experiences of the pandemic. | Doctors and nurses were among the “trusted” sources of information. The interviews revealed themes around information needs (preference for checklists for symptoms) and impacts of the pandemic on their well-being. | Need for telephone hotlines supervised by doctors and nurses may help disseminate accurate and helpful information. |
| Chan et al. (2007) | Hong Kong; SARS | 80%; missing detail about analysis procedures | Parents of children hospitalized in a pediatric outpatient clinic in Hong Kong; convenience sampling | Parents (N = 8) of children aged 3–14 years | July 2003 | No | Qualitative study; semi-structured interviews | Interviews focused on parents’ needs at and during their child’s hospitalization, perceptions of the care provided, and other experiences of parenting during the pandemic. | Four themes were identified: fear of immediate isolation and infection control procedures, sources of anxiety, coping, and experience with health care professionals. | Measures should be taken to alleviate parental uncertainty and anxiety during future infectious disease outbreaks. Importance of technology to facilitate coping for children isolated from caregivers. |
| Xie et al. (2020) | Hubei, China; COVID-19 | 100% | Students in grades 2 through 6 from Wuhan and Huangshi were invited to complete the survey; purposive sampling | Huangshi: Children (N = 1109) in grades 2 to 6; Wuhan: children (N = 675) in grades 2 to 6 | February 28 to March 5, 2020 | Yes; comparisons made between children from Wuhan (epicenter) and Huangshi | Quantitative study; cross-sectional | Children self-reported on the following measures: Children’s Depression Inventory-Short Form (CDI-S) and the Screen for Child Anxiety Related Emotional Disorders. | 22.6% of students reported depressive symptoms, while 18.9% reported anxiety symptoms. Students in Wuhan reported higher depression scores than those in Huangshi. Students in Wuhan stayed in isolation for a longer period of time, starting quarantine earlier and ending it later. | In order to structure interventions around quarantine-related mental health issues in children, it is advisable to develop a greater understanding about how severe epidemics like COVID-19 impact students’ mental health. |
| Oosterhoff et al. (2020) | United States; COVID-19 | 80%; response rate not provided | Adolescents were recruited via social media from across the US; voluntary response sampling | Adolescents (N = 683) aged 13–18 years | March 29 to March 30, 2020 | No | Quantitative study; cross-sectional | Adolescents self-reported on the following measures: social distancing behaviors and motivation, anxiety and depression as measured by the Patient-Reported Outcomes Measurement Information System. | Those who engaged in social distancing due to a personal fear of becoming ill reported higher levels of anxiety, as did those who did so in order to avoid social judgment. | Parents, teachers, and policy makers can play an important role in motivating youth to comply with social distancing guidelines while still finding ways to reduce anxiety and depressive symptoms. |
| Saurabh and Ranjan (2020) | India; COVID-19 | 60%; response rate not provided; missing demographic information | Adolescents who did and did not quarantine during COVID-19 in India; convenience sampling | Adolescents (N = 121) aged 9–18 years who were quarantined | Date not provided (during COVID-19) | Yes; 131 adolescents who were not quarantined | Qualitative study; interviews | Interviews focused on child and parent understanding and compliance of quarantine measures and the psychological impacts of quarantining. | Adolescents in quarantine reported more negative psychological effects, specifically anxiety, annoyance, boredom, insomnia, sadness, and helplessness compared to non-quarantined adolescents. Low compliance with quarantine guidelines. | Social media platforms can help quarantined individuals stay in touch with family and friends virtually, while comic books and videos can be useful in disseminating disease-related information to children and adolescents, which can help reduce their psychological symptoms. |
| Seçer and Ulaş, (2020) | Turkey; COVID-19 | 60%; sample representativeness; missing demographic information | Adolescents from all 7 regions of Turkey were invited to participate; convenience sampling | Adolescents (N = 598) aged 14–18 years | Date not provided; data collection completed over a span of 15 days during the COVID-19 pandemic | No | Quantitative study; cross-sectional | Adolescents self-reported on the following measures: Obsessive Compulsive Inventory-Child Version, Emotional Reactivity Scale, Depression and Anxiety Scale for Children, The Fear of COVID-19 Scale, and the Experiential Avoidance Questionnaire. | A greater fear of COVID-19 is associated with higher levels of anxiety and depression, which is also linked to an increase in OCD-like behaviors. Negative emotional reactivity exacerbates negative outcomes. Experiential avoidance (wariness toward experiencing negative situations) mediates the relationship between COVID-19 and symptoms of OCD. | The elevated risk for OCD symptoms in adolescents due to COVID-19 indicates that interventions should address virus-related fears and depression, which could trigger OCD, as well as help individuals find a balance between taking necessary safety precautions and engaging in unhealthy avoidance behaviors. |
| Zhou et al. (2020) | China; COVID-19 | 80%; response rate was not provided | Junior and senior high school students across 21 provinces in China were invited to participate; voluntary response sampling | Adolescents (N = 8079) aged 12–18 years | March 8 to March 15, 2020 | Yes; adolescents from Hubei region | Quantitative study; cross-sectional | Adolescents self-reported on the following measures: Patient Health Questionnaire (PHQ-9) to measure depressive symptoms and the Generalized Anxiety Disorder scale (GAD-7) to assess anxiety symptoms. | Elevated rates for depression and anxiety were found among female students, those living in rural areas and Hubei province, and students in higher-grade levels. A protective factor appeared to be greater awareness of COVID-19 (knowledge, prevention, control measures, and projections of COVID-19). | Awareness of COVID-19 and how to prevent/manage it can be a protective factor against mental health problems. Measures should be taken to increase adolescents’ understanding of the virus in order to reduce their risk of depression and anxiety. |
Results
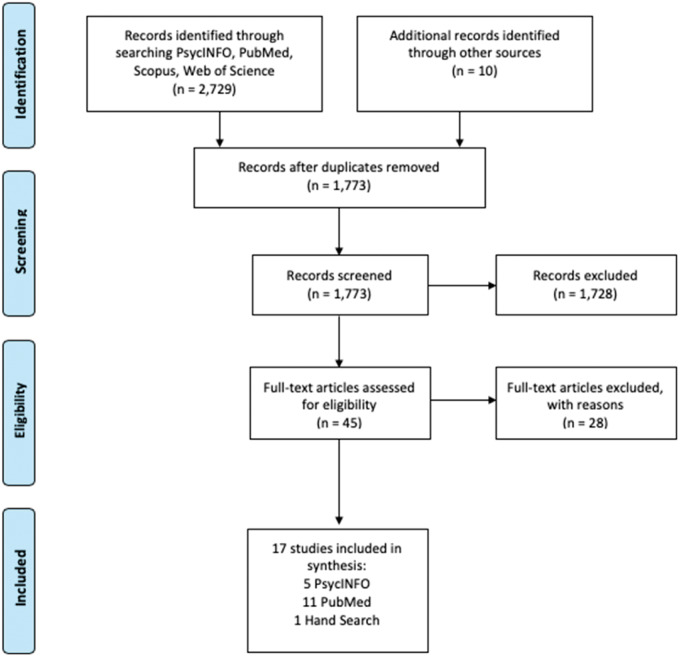
A total of 2,729 articles were identified after our database search of PsycInfo, PubMed, Scopus, and Web of Science. An additional 10 studies were identified from our search of the grey literature. Once duplicates were removed, there were 1,773 articles remaining which were then screened for inclusion criteria through title and abstract, and full article review stages. Each stage involved three independent raters assessing the articles for inclusion. Disagreements were resolved through discussion and consensus by all three raters. Of the 1,773 studies initially screened, there were 19 disagreements yielding a total interrater reliability of 98%. In total, 17 articles were deemed to have met the inclusion criteria. See Figure 1 for a flow diagram of the PRISMA process.
Figure 1.
PRISMA diagram outlining the process used to search and select articles.
Characteristics of Included Studies and Participants
Studies included in the review examined mental health outcomes and information needs during the COVID-19, SARS, and H1N1 pandemics. Study designs were qualitative (n = 4), quantitative (n = 11), and mixed methods (n = 2). Quantitative research studies had greater samples (M = 1,721) compared to qualitative (M = 36) or mixed-method studies (M = 433). The majority of studies (35.3%) were conducted in China. Three studies were conducted in Australia, two in the United States, and one each in India, Turkey, Japan, Argentina, the Netherlands, and Canada. A minority of studies (n = 4) included some type of comparison group. The timing of assessment was primarily during the outbreak (n = 12); however, two studies assessed participants after the pandemic, and two studies did not report the date of assessment but most likely occurred during the pandemic.
The samples ranged in size from 8 to 8,079 participants. The majority of studies analyzed data based on parent or caregiver reports (n = 10). Child self-report data was examined in five studies and two studies included mixed child and parent reports. Seven studies did not report the age of the parent. Most studies did not report on family income (64.7%) or education level (52.9%).
Study Quality
The average score across all three study designs was 70.6% with a range of 60–100%. Two studies passed all MMAT criteria receiving an overall methodological rigor score of 100%. The most consistent rating on the MMAT for studies included in the review was 60% where 10 studies received this score. The most frequent unmet criterion in the quality assessment for quantitative studies related to the risk of non-response bias and lack of validated measures. For qualitative studies, the most common unmet criterion related to a lack of detailed information about the methods and data analysis.
Child Mental Health Outcomes
Table II summarizes identified mental health outcomes for children during pandemics and identified risk and protective factors for child mental health functioning. A total of eight studies examined children’s anxiety, depressive, OCD, PTSD, and fear symptoms (Effler et al., 2010; Oosterhoff et al., 2020; Remmerswaal & Muris, 2011; Saurabh & Ranjan, 2020; Seçer & Ulaş, 2020; Sprang & Silman, 2013; Xie et al., 2020; Zhou et al., 2020). Rates of anxiety and depressive symptoms varied substantially depending on the informant. Parent reports of anxiety in their children suggested lower rates (10%) (Effler et al., 2010), whereas child self-reports indicated higher rates of depressive (22%) and anxiety (19%) symptoms (Xie et al., 2020). Risk factors for higher anxiety and depressive symptoms in children and adolescents were geographic location, gender, grade level, and fear of the pandemic. Higher rates of anxiety and depressive symptoms were found in rural areas compared to cities (Zhou et al., 2020) and closer proximity to the epicenter of the pandemic in Wuhan, China (Xie et al., 2020). Females between the ages of 12–18 years and students in higher grade levels reported higher rates of anxiety and depression (Zhou et al., 2020). For younger children aged 7–12 years, girls exhibited significantly greater levels of fear compared to boys (Remmerswaal & Muris, 2011). Measuring adolescents’ fear of COVID-19 revealed that a greater level of fear was linked to higher levels of anxiety, depression, and OCD symptoms (Seçer & Ulaş, 2020). A risk factor for PTSD in children was experiencing quarantine and parents’ elevated levels of PTSD symptoms (Sprang & Silman, 2013). A qualitative study by Saurabh and Ranjan (2020) explored the psychological impacts of quarantine which included anxiety, annoyance, boredom, insomnia, sadness, and helplessness. Two studies found that parent and child mental health functioning were correlated (Remmerswaal & Muris, 2011; Sprang & Silman, 2013).
Table II.
Summary of Identified Mental Health Outcomes and Information Needs for Children, Parents, and Families During Pandemics
| Article | Method | Child outcomes |
Parent and family outcomes |
Information needs | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Anxiety | Depression | PTSD | Fear, worry | OCD | Impact of quarantine | Anxiety | Depression | PTSD | Fear, worry | Impact of quarantine | Financial burden | |||
| Saurabh and Ranjan (2020) | Qualitative | X | ||||||||||||
| Seçer and Ulaş, (2020) | Quantitative | X | X | X | X | |||||||||
| Xie et al. (2020) | Quantitative | X | X | X | ||||||||||
| Zhou et al. (2020) | Quantitative | X | X | |||||||||||
| Sprang and Silman (2013) | Mixed methods | X | X | X | X | |||||||||
| Effler et al. (2010) | Quantitative | X | X | |||||||||||
| Oosterhoff et al. (2020) | Quantitative | X | X | X | ||||||||||
| Remmerswaal and Muris (2011) | Quantitative | X | X | |||||||||||
| Basurto-Dávila et al. (2013) | Quantitative | X | ||||||||||||
| Chan et al. (2007) | Qualitative | X | X | X | X | |||||||||
| Chen et al. (2011) | Quantitative | X | X | |||||||||||
| Dodgson et al. (2010) | Qualitative | X | X | X | X | |||||||||
| King et al. (2018) | Mixed methods | X | X | |||||||||||
| Koller et al. (2006) | Qualitative | X | ||||||||||||
| Mizumoto et al. (2013) | Quantitative | X | ||||||||||||
| Fung and Loke (2010) | Quantitative | X | ||||||||||||
| Kavanagh et al. (2011) | Quantitative | X | ||||||||||||
Potential moderators and mediators of mental health outcomes were children’s motivations for social distancing (Oosterhoff et al., 2020), optimism about pandemic projections (Xie et al., 2020), emotional reactivity (Seçer & Ulaş, 2020), experiential avoidance (Seçer & Ulaş, 2020), and knowledge of COVID-19 (Zhou et al., 2020). Adolescents who engaged in social distancing because they wanted to avoid judgment or because a friend advised them to, reported greater anxiety and depressive symptoms, respectively (Oosterhoff et al., 2020). Youth who were not optimistic about the projections of the pandemic reported higher depressive symptoms (Xie et al., 2020). Individual characteristics of the child such as negative emotional reactivity and greater experiential avoidance exacerbated negative mental health outcomes for children such as PTSD (Seçer & Ulaş, 2020). Greater awareness of COVID-19, specifically factual information about the disease, prevention measures, and projections of COVID-19, was a protective factor for negative mental health outcomes in children (Zhou et al., 2020). It is important to note that all studies reporting on child mental health outcomes were cross-sectional and that without longitudinal data, these results are correlational and should be interpreted cautiously.
Parent and Family Mental Health Outcomes
Table II summarizes identified mental health outcomes for parents and families during pandemics. Seven studies examined parental and family mental health outcomes (Basurto-Dávila et al., 2013; Chan et al., 2007; Chen et al., 2011; Dodgson et al., 2010; King et al., 2018; Koller et al., 2006; Mizumoto et al., 2013; Sprang & Silman, 2013). The majority of studies assessing mental health outcomes in parents used qualitative methods (n = 3) or interviews from mixed methods studies (n = 2). Only one study evaluated mental health outcomes using a validated PTSD scale (Sprang & Silman, 2013). Results revealed that parents experienced a range of negative psychological impacts as a result of pandemics, specifically heightened vigilance (Dodgson et al., 2010), excessive worry and fear (King et al., 2018; Koller et al., 2006), anxiety (Chan et al., 2007), and PTSD (Sprang & Silman, 2013). Common sources of stress and anxiety for parents included concerns over the short- and long-term health impacts on their child (King et al., 2018), and their child’s education and missed schoolwork during school closures (Basurto-Dávila et al., 2013; Chen et al., 2011). Similar to the results for children regarding the impact of quarantine, parents who were quarantined were more likely to meet clinical criteria for PTSD (Sprang & Silman, 2013) and perceived this to have a detrimental impact on their well-being (King et al., 2018). Mitigating factors, such as the age of the parent, family socioeconomic status (SES), and proximity to individuals personally infected by the disease, were found to impact parent and family outcomes. Older parents reported lower rates of PTSD (Sprang & Silman, 2013) and higher SES families were less negatively impacted by additional childcare expenses and loss of wages (Basurto-Dávila et al., 2013). Less fear and anxiety around the pandemic was related to a greater proximity to areas affected by outbreaks or lack of personal or immediate contact with those infected by the disease (King et al., 2018).
Five studies reported on the financial burden of pandemics on families (Basurto-Dávila et al., 2013; Chen et al., 2011; Dodgson et al., 2010; Effler et al., 2010; Mizumoto et al., 2013). Work absenteeism was positively correlated with the length of school closures (Effler et al., 2010; Fang et al., 2011; Mizumoto et al., 2013), whereas loss of wages was negatively correlated with the age of the child. There were no quantitative studies on the impact of the financial burden on mental health outcomes, but a qualitative study by Dodgson indicated that this was a major source of stress for parents, impacting their mental health and well-being. All of the studies reporting on parent and family mental health outcomes utilized cross-sectional designs, thus, these results are correlational and should be interpreted cautiously.
Only one study included in this review explored resilience in families during pandemics (Koller et al., 2006). In this qualitative study, parents articulated that communication with loved ones during quarantine exerted a powerful impact on families’ well-being despite isolation. Several parents expressed that despite many of the negative impacts of SARS, there were positive outcomes on their families following the outbreak. For example, some parents observed that family members were more openly affectionate with one another than before the pandemic occurred. Others perceived positive changes in their parenting, mentioning that they had made more of an effort to spend time with their families once the outbreak ended and regular routines were in place. This greater appreciation for family and modifications in their parenting behaviors more generally reflected transformations in their perspective and outlook on life.
Information Needs
Five studies reported on the main and most trusted sources of information for families, and their information needs during pandemics (Dodgson et al., 2010; Fung & Loke, 2010; Kavanagh et al., 2011; King et al., 2018; Koller et al., 2006). Parents most heavily relied on information about the pandemic from their child’s school, health department, and media. Rates of parents’ reliance on the media were similar across studies and ranged from 44% (Kavanagh et al., 2011) to 50% (Fung & Loke, 2010). However, despite the media being one of the major sources of information, only a minority of parents found this source to be trustworthy and useful. Qualitative data from Dodgson et al. (2010) suggest that a perceived lack of trust in the media may stem from conflicting and changing messages across news sources. Koller et al. (2006) further corroborated this finding, revealing that parents report an excess of changing information and recommendations which contribute to their overall confusion and stress. In contrast, the majority of parents found that information provided by health departments, schools, doctors, and nurses to be useful and trusted (Kavanagh et al., 2011; King et al., 2018). One study assessing information needs of families during pandemics found that parents prioritized information around safety protocols and expressed the need for clear guidelines and checklists to support them in their decision-making (Fung & Loke, 2010).
Discussion
What Have We Learned From Previous Pandemics That Can Help Children and Families Better Cope With COVID-19?
Child Outcomes
Findings from the studies that reported on children’s anxiety, depressive symptoms, PTSD, and fear symptoms following previous pandemics indicate a significant negative impact of social isolation and quarantining. Results also suggest potential mitigating factors that may attenuate or exacerbate the fear and anxiety children experience. Gender was found to be a risk factor for depression and anxiety symptoms in high school students, with higher rates of both were found in females. This finding is consistent with preliminary reports indicating that pandemics impact females and males differently by exacerbating existing inequalities for the former (UNFPA, 2020), placing them at an elevated risk for gender-based violence, exploitation, and child labor (Plan International, 2020).
The way in which threatening information about infectious disease outbreaks are communicated to children impacts their ability to adjust. Moderating factors such as the age of the child were shown to influence a child’s level of fear and anxiety with younger children showing elevated levels. These findings suggest that parents should provide information to their children that is accurate and appropriate for the child’s age and developmental level.
The correlation between parent and child PTSD scores highlight the reciprocal nature of parent and child mental health and suggest that mental health providers should screen for caregiver mental health disorders and that the presence of mental illness should signal assessments in other family members and children. More studies are required to fully understand the mediators and moderators impacting the link between pandemics and mental health outcomes. Future studies will benefit from using validated measures to assess child and family characteristics and their outcomes. Longitudinal designs are also needed to verify current findings.
Parent and Family Outcomes
Results from the studies that examined parental and family outcomes suggest that parents and caregivers experience high stress, anxiety, and financial burden during pandemics. The needs of caregivers should not be overlooked given that their capacity to support and protect their children ultimately depends on their own coping abilities and well-being. Similar to children, parents also experience anxiety, PTSD, fear and emotional distress. This body of research indicates that not only do parents experience excessive fear over the physical and mental health of their children but that concerns over losing their jobs and finding childcare exacerbate their anxiety, having a negative impact on their well-being.
Information Needs
A review of the literature has also shed light on the most trusted sources of information for families during pandemics. The majority of parents perceived their schools and health departments to be reliable and found the information from these sources useful. Mental health providers can help facilitate and promote health literacy by collaborating with schools and local community leaders to develop resource information sheets informing parents of common signs and symptoms of mental health problems to look out for in their children as well as resources and supports available. Findings also indicate that despite substantial reliance on the media for information, many parents do not trust or perceive this source as reliable. More studies are needed to fully understand the scope of parents’ information needs during pandemics in order to provide support for families in planning for future infectious disease outbreaks and to help inform the design of future information campaigns.
What Should Policy Makers Consider Moving Forward With the Management of COVID-19?
Child Outcomes
Findings from this review suggest that policies need to be in place to reduce barriers to access parent and child mental health services. This review has shown that children experiencing social isolation are at a high risk for developing PTSD and anxiety-related symptoms. When school-based and in-person mental health services are interrupted or discontinued, other remote, technology-based interventions are urgently needed, especially for vulnerable children. This is especially true for families from low-income households who are less likely to have access to reliable internet services and technology equipment. Governments should consider legislation to provide province or statewide resources to remove this barrier. This will also help address inequalities when it comes to remote learning and educational support for low-income families. This review suggests that health care professionals can address children’s mental health preventatively, which may be more cost-effective and successful in the long term. Providing free resources and psychoeducation to parents and teachers to help them identify early warning signs of mental health deterioration in their children will also help mitigate negative outcomes of the pandemic. As previous research by Prime et al. (2020) indicates, recognizing pathways to resilience and supporting parents and professionals who work with children is crucial to strengthening both child and family mental health and well-being.
Parent and Family Outcomes
A significant source of stress for parents is the financial impact of having to miss work and concerns over losing their job. To address this, policies such as universal paid sick leave would allow parents to stay home if they become infected with the virus without having to worry about finances or losing their jobs. Policies are needed that emphasize flexibility for the diversity of childcare needs, easy and quick access to government relief funding to prevent financial burden and help ease the transition back to work, and child care support programs that allow parents to better cope with their responsibilities during the pandemic. These measures may help mitigate negative outcomes for children and their families. Additionally, it is important that governments protect and support civil society organizations and communities who play a critical role in implementing policies, protecting public health, and providing access to needed supplies, medical care, and social services.
A World Health Organization report found that 70% of health care workers are both women and parents (Boniol et al., 2019). Better protection is needed for these individuals both because they serve on the front line and are more physically vulnerable to infection but also because they are vulnerable due to elevated stress levels they experience on a daily basis and its impact on the entire family’s well-being. Policies need to address the concerns of parents who are simultaneously balancing the need to financially provide while keeping their children healthy and safe. Providing medical and mental health care as well as financial security to workers with an elevated risk of contracting the disease is crucial in light of findings from the review highlighting this as a major concern and need for parents.
Other families who are “at risk”, meaning that they may have been living under stressful conditions prior to COVID-19, should also be considered as their stress would likely have risen to intolerable levels during the pandemic. These are families coping with domestic violence, youth protection issues, mental health concerns, and disabilities. These families have particular needs that cannot be put on hold during a pandemic. The removal of the essential supports that they rely on daily may be enough to provoke a crisis. Policies need to balance the need to protect the public as a whole and also vulnerable individuals.
Information Needs
The safety of public health depends on quick, accessible, and accurate information. It is essential that governments provide up-to-date and evidence-based information about the threat of the virus and measures the public should take to keep healthy and safe. Free access to high-speed broadband internet is needed, especially for low-income families, to prevent inequities. When banning misinformation is not possible, governments need to support and advocate rigorous fact-checking and professional journalism.
Despite the abundance of information on how to support children during COVID-19, the research on child and family experiences during pandemics is scarce. Government funding supporting research in this area in open access scientific journals is critical during this time. It allows researchers to take advantage of the natural and universal conditions of adversity brought on by pandemics to study a host of risk and protective factors and the impact on child and family outcomes. Of particular interest is what child and family resilience can teach us about overcoming, and even thriving, in the face of adversity.
Mitigating Negative Impacts of Social Isolation
Lastly, a greater emphasis on ensuring policies are in place not only to protect frontline staff from contracting the disease by providing a safe workplace environment and adequate supply of protective equipment, but also, from psychosocial adversity by mitigating its effects on domestic violence, depression, drug addiction, alcohol abuse, and suicide. A recent article found a 50% drop in reports of child abuse in Illinois after schools were forced to close (Eldeib, 2020). This decline was attributed to a decrease in access to mandated reporters such as teachers, pediatricians, and mental health workers, rather than a decrease in abuse. Although school closures and social distancing measures have helped contain the spread of the virus, other unanticipated consequences of social isolation policies, such as the shutdown of supportive services, has left vulnerable individuals at risk. Government action and federal policies are needed to address the psychosocial effects of COVID-19. In particular, individuals and families at risk need immediate attention by providing shelters for women and children escaping domestic violence, outreach and counseling for those with addiction and mental health difficulties, and specialized support for those living with disabilities.
Critique of the Literature
The existing research in this area is scarce and though a number of studies were of high quality, the majority were of low to moderate quality. A number of quantitative studies included large sample sizes, however, the main outcomes relied on survey-based single-item measures of mental health. The majority of these studies also lacked a comparison group collecting data on pre- and post-pandemic outcomes. For qualitative studies, the most common unmet criteria related to a lack of detailed information about methods and data analysis. For all three study designs less than a quarter were theory driven. Utilizing existing theories, such as Bronfenbrenner’s (1979) Ecological Systems Theory and Family Stress Theory (Conger & Conger, 2002), to inform research in this area is crucial in light of the growing evidence suggesting the reciprocal nature of family processes and child adaptation (Prime et al., 2020). Another limitation of the existing studies on this topic relates to the lack of information regarding the child’s current health status. Future studies should assess this in order to determine the additional impact of having a chronic health condition on mental health.
Limitations of the Review
It should be noted that while the review had a number of strengths, including the high agreement between reviewers who screened papers and use of a validated critical appraisal tool, there are also a number of limitations that must be considered. Due to the lack of research in this area, our review only identified a small number of papers meeting inclusion criteria. Therefore, the risk and mitigating factors identified should not be considered exhaustive or definitive. Given that there are a range of tools for assessing study quality and risk of bias, it is possible that the MMAT may not have fully captured all potential methodological issues relevant to each study design. Lastly, all studies included in this review were cross-sectional in nature and therefore causal links between risk factors and mental health outcomes cannot be determined.
Conflicts of interest: None declared.
Acknowledgments
The authors would like to thank Alyssa Chan (AC) and Alanna de la Vega (AV) for assisting with the interrater reliability and study quality/risk of bias assessments.
Appendix
PsycINFO (EBSCO) search strategy
S4 S1 AND S2 AND S3 Limiters: Publication Year: 2000-2020; Publication Type: Peer Reviewed Journal; English 144
S3 (famil* OR parent* OR child* OR adolescent* OR teenage*) 1,445,663
S2 (DE “Social Health” OR DE “Mental Health” OR DE “Mental Status” OR DE “Posttraumatic Stress Disorder” OR DE “Complex PTSD” OR DE “DESNOS”) 106,365
S1 (DE “Disease Outbreaks” OR DE “Epidemics” OR DE “Pandemics” OR DE “Coronavirus” OR DE “Severe Acute Respiratory Syndrome” OR DE “Swine Influenza” OR epidemic* OR pandemic* OR COVID-19 OR SARS OR H1N1) 17,913
Footnotes
“Parents” is inclusive of all caregivers of children.
References
- Jazeera A. (2020). Coronavirus: Which countries have confirmed cases? Retrieved April 20, 2020, from https://www.aljazeera.com/news/2020/01/countries-confirmed-cases-coronavirus-200125070959786.html
- Basurto-Dávila R., Garza R., Meltzer M. I., Carlino O. L., Albalak R., Orellano P. W., Uez O., Shay D. K., Santandrea C., Weis M. d C., Averhoff F., Widdowson M.-A. (2013). Household economic impact and attitudes toward school closures in two cities in Argentina during the 2009 influenza A (H1N1) pandemic. Influenza and Other Respiratory Viruses, 7, 1308–1315. 10.1111/irv.12054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boniol M, McIsaac M, Xu L, Wuliji T, Diallo K, Campbell J. Gender equity in the health workforce: analysis of 104 countries. Working paper 1. Geneva: World Health Organization; 2019 (WHO/HIS/HWF/Gender/WP1/2019.1).Licence: CC BY-NC-SA 3.0 IGO.
- Bronfenbrenner U. (1979). The ecology of human development: Experiments by nature and design. Harvard University Press. [Google Scholar]
- Canadian Government. (2020). Coronavirus disease (COVID-19): Travel restrictions, exemptions and advice. Retrieved May 30, 2020, [Google Scholar]
- Canadian Government (2020). Canada Emergency Response Benefit. Retrieved May 30, 2020, from https://www.canada.ca/en/services/benefits/ei/cerb-application.html
- Chan S. S. C., Leung D., Chui H., Tiwari A. F. Y., Wong E. M. Y., Wong D. C. N., Barnsteiner J. H., Lau Y.-L. (2007). Parental response to child’s isolation during the SARS outbreak. Ambulatory Pediatrics, 7, 401–404. http://proxy.lib.sfu.ca/login?url=https://search.ebscohost.com/login.aspx?direct=true&db=mnh&AN=17870650&site=ehost-live [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen W.-C., Huang A. S., Chuang J.-H., Chiu C.-C., Kuo H.-S. (2011). Social and economic impact of school closure resulting from pandemic influenza A/H1N1. Journal of Infection, 62, 200–203. 10.1016/j.jinf.2011.01.007 [DOI] [PubMed] [Google Scholar]
- Conger R. D., Conger K. J. (2002). Resilience in Midwestern families: Selected findings from the first decade of a prospective, longitudinal study. Journal of Marriage and Family, 64, 361–373. 10.1111/j.1741-3737.2002.00361.x [DOI] [Google Scholar]
- Dodgson J., Tarrant M., Chee Y., Watkins A. (2010). New mothers’ experiences of social disruption and isolation during the severe acute respiratory syndrome outbreak in Hong Kong. Nursing & Health Sciences, 12, 198–204. 10.1111/j.1442-2018.2010.00520.x [DOI] [PubMed] [Google Scholar]
- Dray J., Bowman J., Wolfenden L., Campbell E., Freund M., Hodder R., Wiggers J. (2015). Systematic review of universal resilience interventions targeting child and adolescent mental health in the school setting: Review protocol. Systematic Reviews, 4(1), 186. 10.1186/s13643-015-0172-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Effler P. V., Carcione D., Giele C., Dowse G. K., Goggin L., Mak D. B. (2010). Household responses to pandemic (H1N1) 2009-related school closures, Perth, Western Australia. Emerging Infectious Diseases, 16, 205–211. 10.3201/eid1602.091372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eldeib D. (2020, June 7). Calls to Illinois’ Child Abuse Hotline Dropped by Nearly Half Amid the Spread of Coronavirus. Here’s Why That’s Not Good News. ProPublica Illinois https://www.propublica.org/article/illinois-dcfs-child-abuse-hotline-calls-coronavirus
- Fang P., Han X., Chen J., Feng L., Tang S., Yu H. (2011). How many working days would be missed due to moderate or severe influenza pandemic in China? Scandinavian Journal of Public Health, 39, 656–664. 10.1177/1403494810396401 [DOI] [PubMed] [Google Scholar]
- Fung O., Loke A. (2010). Disaster preparedness of families with young children in Hong Kong. Scandinavian Journal of Public Health, 38, 880–888. 10.1177/1403494810382477 [DOI] [PubMed] [Google Scholar]
- Hong Q. N., Gonzalez-Reyes A., Pluye P. (2018). Improving the usefulness of a tool for appraising the quality of qualitative, quantitative and mixed methods studies, the Mixed Methods Appraisal Tool (MMAT). Journal of Evaluation in Clinical Practice, 24, 459–467. 10.1111/jep.12884 [DOI] [PubMed] [Google Scholar]
- Kavanagh A. M., Bentley R. J., Mason K. E., McVernon J., Petrony S., Fielding J., LaMontagne A. D., Studdert D. M. (2011). Sources, perceived usefulness and understanding of information disseminated to families who entered home quarantine during the H1N1 pandemic in Victoria, Australia: A cross-sectional study. BMC Infectious Diseases, 11(1), 2. 10.1186/1471-2334-11-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- King C. L., Chow M. Y. K., Wiley K. E., Leask J. (2018). Much ado about flu: A mixed methods study of parental perceptions, trust and information seeking in a pandemic. Influenza and Other Respiratory Viruses, 12, 514–521. 10.1111/irv.12547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koller D. F., Nicholas D. B., Goldie R. S., Gearing R., Selkirk E. K. (2006). When family-centered care is challenged by infectious disease: Pediatric health care delivery during the SARS outbreaks. Qualitative Health Research, 16(1), 47–60. 10.1177/1049732305284010 [DOI] [PubMed] [Google Scholar]
- Lai B., Auslander B., Fitzpatrick S., Podkowirow V. (2014). Disasters and depressive symptoms in children: A review. Child & Youth Care Forum, 43, 489–504. 10.1007/s10566-014-9249-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mizumoto K., Yamamoto T., Nishiura H. (2013). Contact behaviour of children and parental employment behaviour during school closures against the pandemic influenza A (H1N1-2009) in Japan. Journal of International Medical Research, 41, 716–724. 10.1177/0300060513478061 [DOI] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D. G. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Annals of Internal Medicine, 151, 264. 10.7326/0003-4819-151-4-200908180-00135 [DOI] [PubMed] [Google Scholar]
- Oosterhoff B., Palmer C. A., Wilson J., Shook N. (2020). Adolescents’ motivations to engage in social distancing during the COVID-19 pandemic: Associations with mental and social health. Journal of Adolescent Health, 67, 179–185. 10.1016/j.jadohealth.2020.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plan International (2020). “Shadow Pandemic” Unfolding as Girls’ Health, Rights, and Freedoms Erode https://plan-international.org/news/2020-05-27-shadow-pandemic-unfolding-srhr
- Prime H., Wade M., Browne D. T. (2020). Risk and resilience in family well-being during the COVID-19 pandemic. American Psychologist, 75, 631–643. 10.1037/amp0000660 [DOI] [PubMed] [Google Scholar]
- Remmerswaal D., Muris P. (2011). Children’s fear reactions to the 2009 Swine Flu pandemic: The role of threat information as provided by parents. Journal of Anxiety Disorders, 25, 444–449. 10.1016/j.janxdis.2010.11.008 [DOI] [PubMed] [Google Scholar]
- Robertson E., Hershenfield K., Grace S. L., Stewart D. E. (2004). The psychosocial effects of being quarantined following exposure to SARS: A qualitative study of Toronto health care workers. The Canadian Journal of Psychiatry, 49, 403–407. [DOI] [PubMed] [Google Scholar]
- Saurabh K., Ranjan S. (2020). Compliance and psychological impact of quarantine in children and adolescents due to Covid-19 pandemic. The Indian Journal of Pediatrics, 87, 532–536. 10.1007/s12098-020-03347-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seçer İ., Ulaş S. (2020). An investigation of the effect of COVID-19 on OCD in youth in the context of emotional reactivity, experiential avoidance, depression and anxiety. International Journal of Mental Health and Addiction, 1–14. 10.1007/s11469-020-00322-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sprang G., Silman M. (2013). Posttraumatic stress disorder in parents and youth after health-related disasters. Disaster Medicine and Public Health Preparedness, 7(1), 105–110. 10.1017/dmp.2013.22 [DOI] [PubMed] [Google Scholar]
- Tang B., Deng Q., Glik D., Dong J., Zhang L. (2017). A meta-analysis of risk factors for post-traumatic stress disorder (PTSD) in adults and children after earthquakes. International Journal of Environmental Research and Public Health, 14, 1537. 10.3390/ijerph14121537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terasaka A., Tachibana Y., Okuyama M., Igarashi T. (2015). Post-traumatic stress disorder in children following natural disasters: A systematic review of the long-term follow-up studies. International Journal of Child, Youth and Family Studies, 6(1), 111–133. 10.18357/ijcyfs.61201513481 [DOI] [Google Scholar]
- U.S Department of Health and Human Services (2020). ACF-COVID-19-Stimulus. Retrieved May 30, 2020, from https://www.acf.hhs.gov/coronavirus/acf-covid-19-stimulus
- UNFPA (2020). COVID-19: A gender lens—protecting sexual and reproductive health and rights, and promoting gender equality. New York, NY. https://www.unfpa.org/sites/default/files/resource-pdf/COVID-19_A_Gender_Lens_Guidance_Note.pdf
- World Health Organization (2020). WHO Director-General’s opening remarks at the media briefing on COVID-19.
- Xie X., Xue Q., Zhou Y., Zhu K., Liu Q., Zhang J., Song R. (2020). Mental health status among children in home confinement during the coronavirus disease 2019 outbreak in Hubei Province, China. JAMA Pediatrics, 174, 898. 10.1001/jamapediatrics.2020.1619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeung N. C. Y., Lau J. T. F., Yu N. X., Zhang J., Xu Z., Choi K. C., Zhang Q., Mak W. W. S., Lui W. W. S. (2018). Media exposure related to the 2008 Sichuan earthquake predicted probable PTSD among chinese adolescents in Kunming, China: A longitudinal study. Psychological Trauma: Theory, Research, Practice, and Policy, 10, 253–262. 10.1037/tra0000121 [DOI] [PubMed] [Google Scholar]
- Zhou S.-J., Zhang L.-G., Wang L.-L., Guo Z.-C., Wang J.-Q., Chen J.-C., Liu M., Chen X., Chen J.-X. (2020). Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. European Child & Adolescent Psychiatry, 29, 749–758. 10.1007/s00787-020-01541-4 [DOI] [PMC free article] [PubMed] [Google Scholar]