Abstract
Background
Fluid Resistant Surgical Masks have been implemented in UK personal protective equipment (PPE) guidelines for COVID-19 for all care sites that do not include aerosol-generating procedures (AGPs). FFP3 masks are used in AGP areas. Concerns from the ENT and plastic surgery communities out with intensive care units have questioned this policy. Emerging evidence on cough clouds and health care worker deaths has suggested that a review is required.
Aims
To test the efficacy of Fluid Resistant Surgical Mask with and without adaptions for respiratory protection. To test the efficacy of FFP and FFP3 regarding fit testing and usage.
Methods
A smoke chamber test of 5 min to model an 8-h working shift of exposure while wearing UK guideline PPE using an inspiratory breathing mouthpiece under the mask. Photographic data were used for comparison.
Results
The Fluid Resistant Surgical Mask gave no protection to inhaled smoke particles. Modifications with tape and three mask layers gave slight benefit but were not considered practical. FFP3 gave complete protection to inhaled smoke but strap tension needs to be ‘just right’ to prevent facial trauma. Facial barrier creams are an infection risk.
Conclusions
Surgical masks give no protection to respirable particles. Emerging evidence on cough clouds and health care worker deaths suggests the implementation of a precautionary policy of FFP3 for all locations exposed to symptomatic or diagnosed COVID-19 patients. PPE fit testing and usage policy need to improve to include daily buddy checks for FFP3 users
Keywords: Covid-19, health care worker, occupational exposure, personal protective equipment
Key learning points.
What is already known about this subject:
Heath care worker personal protective equipment policy for SARS-CoV-2 virus had to be quickly inferred from influenza, SARS-CoV-1 and MERS-CoV-1 viruses. This provided a weak evidence base for a new infection.
Surgical masks are designed to protect the patient from the surgeon’s breath and the surgeon from splashes of bodily fluids, not the wearer from inhalation of airborne particles.
Personal protective equipment supply problems during the COVID-19 world pandemic have required policy makers to target aerosol-generating procedures as the main risk requiring FFP3 respiratory protection.
What this study adds:
A smoke chamber model was used to compare Fluid Resistant Surgical Mask, FFP2 and FFP3 industrial masks in a single subject wearing personal protective equipment as per UK policy for COVID-19.
The surgical mask offered no respiratory protection to smoke size particles. Tape adaptions to the surgical mask and FFP2 still let in smoke tracer. FFP3 gave complete protection to smoke.
FFP3 masks need skilled fit testing to prevent facial trauma and reducing doffing risks.
What impact this may have on practice or policy:
Surgical masks give inadequate respiratory protection during the COVID-19 pandemic. Cough clouds, serology and UK health care workers deaths need to be factored into revised PPE policy. The precautionary principle and COSHH assessments would suggest FFP3 for all areas where potential COVID-19 patients are being assessed or treated.
Occupational hygiene studies are urgently required in community settings such as nursing homes and symptomatic patients home bedrooms for community staff. Occupational medicine and occupational hygiene have key industrial experience to inform NHS Public Health PPE policy makers.
FFP3 Fit Testing and policy implementation in the NHS needs to be improved with understanding of mask design and industrial personal protective equipment experience. Buddy personal protective equipment systems for personal protective equipment donning and doffing could enhance worker safety and infection control.
Introduction
The World Health Organization (WHO) states that SARS-CoV-2 (COVID-19) is transmitted by: direct contact, indirect contact of contaminated surfaces and through inhalation of droplets from sneezing and coughing [1]. It is known that viral aerosols are also generated during breathing, talking and coughing [2–4]. These particles can: travel great distances (7–8 m from a cough) [5], remain suspended in air for >1 h [6] and can be inhaled to the bottom of the respiratory tree [7,8].
The Fluid Resistant Surgical Mask (FRSM) is routinely used in hospital settings to protect the Health Care Workers (HCWs) from body fluid splashes. In 2008, the UK Health and Safety Executive demonstrated that FRSMs afford the wearer a 6-fold reduction in exposure to respirable aerosol. In comparison, well-fitting disposable FFP3 masks afforded the wearer 100-fold reduction in exposure to respirable aerosols [9]. These findings have been repeated in the USA with the Occupational Health and Safety Association finding FRSM cannot be relied upon to protect workers against airborne infectious agents [10].
On 6 April 2020, WHO published interim guidance on personal protective equipment (PPE) for HCWs during the SARS-CoV-2 pandemic. These stated that FRSM should be worn by HCWs caring for SARS-CoV2 patients, with the exception of aerosol-generating procedures (AGPs) [11]. Public Health England (PHE) and PPE policies across the UK followed WHO to advise FFP3 mask protection only for AGPs [12].
The evidence for PPE policy came from a weak evidence base during flu and SARS epidemics, with a limited understanding of SARS-CoV-2 pathogenicity. The surgical community was quick to raise concerns about these recommendations, in particular, otolaryngology (ENT), maxillofacial surgery, plastic surgery and ophthalmology due to their close working proximity to patients airways. ENT UK and BAOMS (British Association of Oral and Maxillofacial Surgeons) issued a guideline at variance from PHE policy, which recommended FFP3 for all throat and nasal examinations on 23 April 2020 and was not restricted to the WHO AGP list [2,13].
In order to interrogate the effectiveness and usage of FRSM, FFP2 and FFP3 masks, we developed a novel smoke chamber model of ‘action research’ during COVID-19. Smoke particles (0.1 μm) were used to simulate SARS-CoV-2 particles (0.12 µm) [14–19]. This study was initially presented to HCWs on videos, in order to provide an accessible visual understanding of potential viral aerosol movements through respiratory PPE, with and without adaptions.
Methods
This study was aimed to contribute qualitative data to the literature by providing a visual portrayal of the level of respiratory protection granted to the UK Health and Social Care workforce during the COVID-19 pandemic. Each grade of mask and adaptations were investigated using a smoke chamber model (particle size 0.1 μm) [18,19] to simulate exposure to SARS-SoV-2 (particle size of 0.12 μm) [14,15,17,19].
The same test subject was used throughout, sitting in a resting state wearing NHS PPE according to guidelines at the time of test. The single subject and author (J.D.M.D.) recorded informed consent for the test series. Research governance is guaranteed by their GMC registration.
The smoke chamber was constructed in a converted shipping container, measuring 16.3 m3, with exhaust ventilation to clear smoke between runs (Figure 1). Purple and orange stage smoke was used with 13 g propellant in 14 mm copper tube, with a detonator, to achieve the same dose of smoke for each test run, using two doses per run. All runs were recorded on video (Canon 5D Mark III, 50 mm Lens EF 50 mm f/1.2L USM, shot at: 1/160 s at f/5.6 ISO 200).
Figure 1.
Smoke chamber design.
Five minutes of intense smoke exposure was estimated to be the equivalent of an 8-h working shift. Five minutes is 1% of the exposure time during an 8-h shift. So, the model assumes the shift particle exposure was 99-fold less than the dense dose of smoke used over 5 min. Confined space safety and emergency plans were in place throughout. A mouthpiece sensor tube was made from cardboard spirometer tubes cut to 40 mm * 30 mm diameter. It was covered in FRSM material with the inside white filter layer outermost in an exact fashion for all runs, to capture tracer smoke consistently.
The mouthpiece sensor tube was worn in the subject’s mouth against the teeth, leaving 30 mm exposed beneath the mask during all run combinations. The nostrils were plugged with gauze. Cliniderm surgical tape and Sudocrem barrier cream were used to test ‘PPE Hacks’ during short supply.
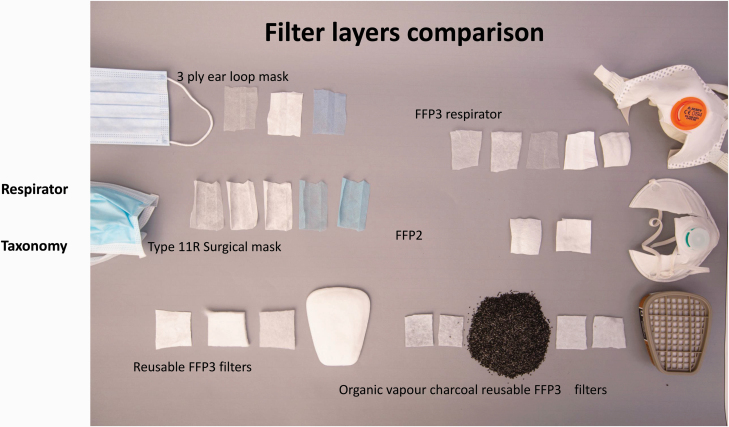
3M 8835 FFP3, Alpha Solway 3030V EN 149:2001, Cardinal Health AT74535UK Type IIR FRSM and FRP2V EN149:2001+A1:2009 FFR2R Safety Source were the masks tested. We deconstructed all the available masks to consider and record their layers and function (Figure 2).
Figure 2.
Mask taxonomy.
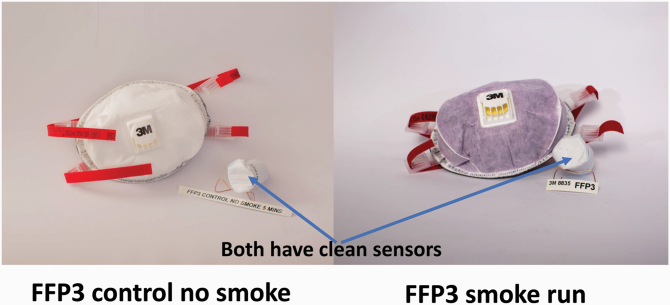
Control runs for all masks were conducted with the mouthpiece sensor below the mask for 5 min without smoke.
There was a careful routine with glove changing and a buddy to avoid cross contamination of smoke on exit and during doffing. The mouthpiece sensor was captured in a clean specimen bag for photography. No quantitative measurements were taken. The results are entirely visual, by choice, in order to inform HCWs by video image rather than complex data.
Results
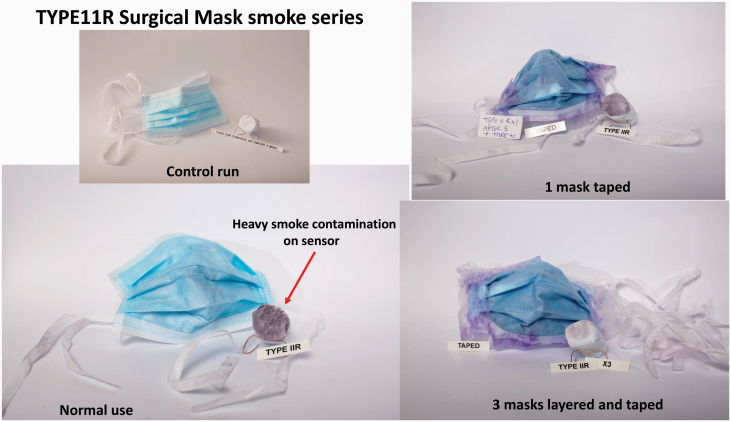
The Fluid-Resistant Surgical Mask Type 11R smoke test showed heavy contamination with smoke deposits on the mouthpiece sensor after 5-min exposure. There was only light purple smoke contamination on the front surface. This confirmed that unfiltered air is breathed in from around the edges of the surgical mask during routine clinical use as instructed in PHE PPE guidelines (Figure 3) [12].
Figure 3.
Fluid Resistant Surgical Mask Type 11R adaptions.
The control run without smoke showed no smoke deposits on the mouthpiece sensor (Figure 3).
We taped up the sides of a single FRSM with surgical tape applied to the face and mask to attempt a seal (Figure 3). This still showed heavy contamination of the mouthpiece sensor, but slightly less than the ‘no tape’ run. We also noted heavier purple smoke on the outside surface compared to the untaped runs. This would suggest that despite the smoke being drawn through the mask, that there were insufficient layers to prevent smoke getting to the sensor mouthpiece (Figures 2, 3 and 6).
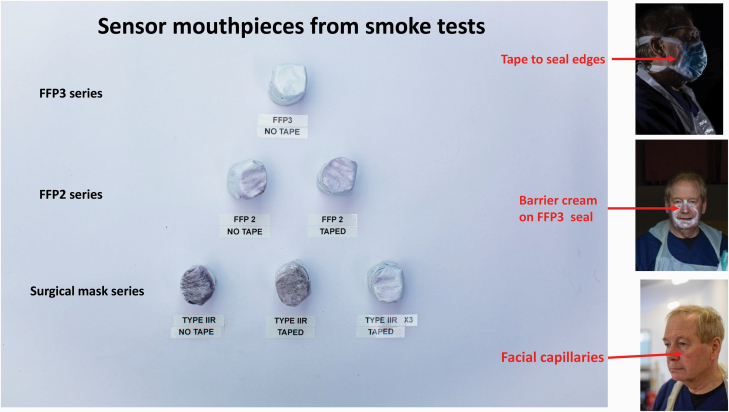
Figure 6.
Sensor mouthpieces from smoke tests and barrier cream.
We then layered up three FRSM and applied surgical tape. This shows less smoke contamination of the sensor mouthpiece and more staining of the exterior surfaces, but incomplete protection when viewed against the control and FFP3 runs.
When PHE PPE policy changed on 21 May 2020 to use a face visor, rather than goggles, with the FRSM, we retested the Type 11R with smoke for 5 min underneath a visor instead of the previous disposable goggles. We again found heavy smoke contamination of the mouthpiece sensor tube.
The surgical tape required a buddy to apply to the face and was painful to remove. We concluded that the Type 11R Fluid-Resistant Surgical Mask did not offer any protection to smoke size particles in the breathing zone of the wearer. Even layered up with three layers, the protection was incomplete and the ‘PPE hack’ was considered unviable in use (Figure 6). The addition of a visor to the FRSM added nothing to respiratory protection.
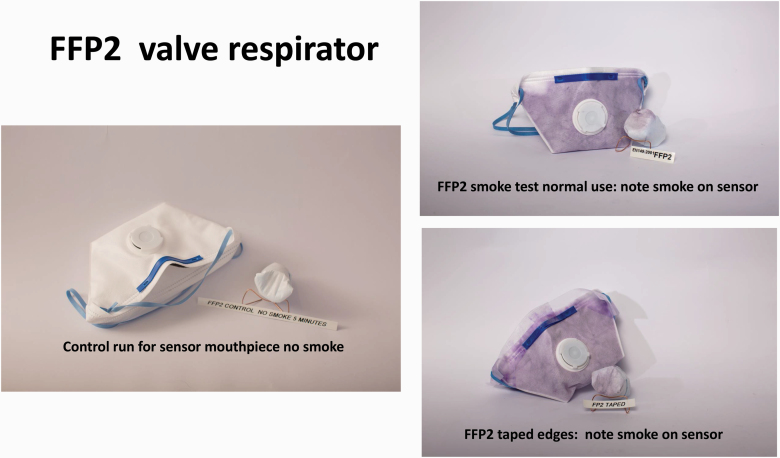
Industrial FFP2 respirators add an exhalation valve and do not require fit testing. They draw inspiration through the filter layers rather than being open at the sides, as in the FRSM (Figures 2 and 4).
Figure 4.
FFP2 industrial mask.
The smoke test showed heavy contamination of the outer surface, suggesting the inspired air is being drawn through the filter layers, but they are still insufficient to stop the mouthpiece sensor being contaminated. Adding surgical tape around the edges resulted in a similar picture on both the outside surface and the sensor.
We concluded that FFP2 would give inadequate protection to smoke size particles in a clinical setting because the inspiration layers (Figures 2 and 4) were insufficient despite adding a seal like an FFP3.
The FFP3 mask gave complete respiratory protection when smoke tested, with no contamination of the mouthpiece sensor when compared to control. We also noticed heavy contamination of the outside inspiratory surface filter, which suggested that the three layers design, including padding (Figures 2 and 5), was effective against smoke size particles in the health care setting.
Figure 5.
FFP3 industrial mask.
The FFP3 layers of inspiratory protection with a reliable seal gave complete respiratory protection to the user when compared against FRSM Type 11R and FFP2 respirator in our smoke test model.
Our own clinical experience found that FFP3 respirator supplies were limited in surgical practice. We were aware that small size FFP3 respirators were in short supply for female faces and colleagues at fit testing were being advised to tighten their masks to the level of experiencing pain to gain a seal. We also became aware of colleagues using FFP3 reporting facial trauma around the area of the mask seal. We therefore ran a second series of orange smoke tests to consider face fit during COVID-19.
We found that the normal ‘just enough tension’ gave complete protection with no smoke deposits on the mouthpiece sensor tube. We then tried an ‘overtightened to pain level’ of face fit with the FFP3 mask.
The mouthpiece sensor remained clear of smoke deposits but we observed distortion of the seal shape and we observed capillary skin trauma over the left cheek (Figure 6).
We considered usage of a barrier cream to mitigate the reported facial trauma. Sudocrem was applied to the FFP3 respirator seal. The smoke test showed no contamination of the mouthpiece sensor when compared with the no smoke and smoke control runs. However, we identified a major hazard at doffing. The white cream had spread around the face during donning and achieving a face fit seal (Figure 6). This left barrier cream deposits out with the mask seal area in the epicanthic region, close to the eye sockets. The barrier cream would be exposed to virus particles, which could adhere to the sticky surface. Indeed a few traces of smoke particles were observed medial to the eye. SARS-CoV-2 particles would pose a substantial infection risk to the HCWs when washing the barrier cream off the face after doffing the mask. SARS-CoV-2 virus is considered transmissible through conjunctiva [20].
Discussion
This qualitative study used smoke particles to simulate respirable size SARS-CoV-2 particles. It showed that Fluid Resistant Surgical Mask Type 11R , in usual usage, does not offer respiratory protection to the HCWs.
FFP2 respirators also failed to give adequate protection against smoke sized respiratory particles. However, disposable FFP3 respirators gave complete protection against smoke sized respirable particles.
We give visual confirmation for HCWs and policy makers of existing quantitative data in the literature [9,10] on the lack of protection against inspired aerosol afforded by surgical masks compared to industrial FFP3 respirators.
We tested ‘PPE hacks’ which could potentially enhance FRSM during the PPE supply issues experienced during the COVID-19 pandemic [21,22]. However, none have been found secure or safe enough to recommend for clinical practice.
We also explored the experience of FFP3 fit testing, for front line clinical staff. We confirmed that FFP3 mask strap tension needs to the ‘just right’ for an effective seal, in order to reduce face trauma [22].
We raise the potential infection hazard of barrier creams applied to the face in an attempt to reduce facial skin trauma.
We accept the fundamental limitations of our study with no quantitative measurements, but find the visual evidence compelling. Feedback from HCWs on our videos, published on YouTube, has suggested that they now understand how the masks work, in a manner not possible from technical publications. We present our smoke tests as a qualitative study which has explored PPE themes during COVID-19.
Our model uses mouth breathing with a blocked nose, which is not physiological. The 5-min intense smoke exposure may not mimic the dynamics of an 8-h shift exposure with changing stress, heat and exercise patterns.
The evidence base for UK COVID-19 PPE policy is weak [4]. Policy extrapolates from influenza and SARS, but excluded evidence from norovirus aerosol sampling, despite evidence that SARS-CoV-2 may have faecal viral transmission [20,23,24]. It is understood that there was no occupational medicine or occupational hygiene input to UK PPE policy.
The NHS has never before had to consider widespread fatalities in health and social care staff by an infective agent beyond HIV, hepatitis or rare imported pathogens such as Ebola. The Health and Safety at Work Act has required actions by employers ‘as far as reasonably practical’ since 1974 [24]. The Control of Substances Hazardous to Health Regulations (COSHH) have been in place since 1988 [24].
It is suggested in UK PHE PPE policy, that the main mode of transmission of COVID-19 is via droplet spread and that SARS-CoV-2 transmission via aerosol is only a concern during specified AGPs. AGP areas require FFP3 and all other areas must use a FRSM. The risk of transmission via AGPs is deemed high enough to warrant FFP3 respiratory protection, eye protection, face shield and gown, regardless of whether the patient has symptoms; any AGP should be treated as if COVID-19 positive irrespective of status. Droplets (5–10 μm) and aerosol particles (<5 μm) are determined by an arbitrary cut-off. Of note, cardiopulmonary resuscitation, chest physiotherapy and swabbing the respiratory tracts of patients with suspected or confirmed COVID-19 are currently not classed as AGP [12].
The UK ENT community had early warnings from colleagues abroad and altered their clinical guidelines beyond AGPs to recommend FFP3 for all nose and throat examinations [13]. ENT then had an early consultant death. All other UK surgical specialties followed [25].
Analysis of 119 HCW deaths in UK [26] found no mortality in staff afforded FFP3 protection in ‘high risk’ intensive care and anaesthetics settings. The reported HCW COVID-19 deaths were working in locations classified as ‘low risk’ including general practice, ambulance staff, care home workers, general wards and emergency departments, where PPE policy provides FRSM. Young women working in the NHS have twice the risk of death from COVID-19 compared to their general population counterparts [26]. There have now been 247 HCW deaths reported in the UK [27].
SARS-CoV-2 is transmissible via aerosol and survives as fomites on surfaces for up to 72 h [6,14]. Greatest seroconversion rates (34%) have been found in NHS housekeeping staff, followed by those working in acute medicine (33%) and general internal medicine (30%) [28].
Emerging evidence on cough clouds demonstrated a range of respirable particle size projecting 7 m without an ‘aerosol-generating procedure’ [5]. UK Government guidelines advise the public to stay 2 m apart with social distancing, to reduce SARS-CoV-2 transmission, while HCWs providing patient care at intimate distances from coughing patients with confirmed COVID-19 are wearing only FRSM. Previous work has confirmed viral content (papillomavirus and HIV) within surgical smoke and documented operator contraction of a papilloma virus using carbon dioxide laser [29].
No air sampling has been published from community locations. Community nursing homes have small rooms. Intimate care is usually delivered with closed windows while showering and toileting care are given in the same space. Nursing homes in the UK are a major locus of COVID-19 care and worker deaths [27,30].
A COSHH risk assessment grid with a ‘possible’ outcome of death in an employee with a ‘low’ likelihood of occurrence still requires maximum worker protection with PPE as the last resort in the industrial context [24]. The precautionary principle applies to provide the best PPE available [14,15]. The Fluid Resistant Surgical Mask is clearly lacking from our analysis and we advocate a complete shift of UK PPE policy for COVID-19 to require FFP3 in all clinical areas in hospital and community locations, where COVID-19 is suspected or where care is being given within the coughing zone of the patient.
The new evidence on cough clouds, the analysis of HCW deaths and our visual evidence on the failure in respiratory protection from the FRSM suggests early review of PPE guidance in settings out with ‘aerosol-generating procedures’ zones. The precautionary principle enshrined in COSHH would suggest FFP3 for all areas where HCW are assessing or caring for patients with SARS-CoV-2.
Acknowledgements
The NHS authors gratefully acknowledge Geo-Rope Ltd for providing the facilities and industrial skill to conduct this research. The smoke chamber facility was designed by Neil MacLean and Christopher Horsely. Both provided their skill and time as a voluntary contribution to help understand COVID transmission in health care workers. James Douglas, Gillian Higgins, Eleanor Robertson and Catriona Douglas are NHS clinical employees.
Competing interest
None declared.
References
- 1. World Health Organization (WHO). Coronavirus Disease 2019 (COVID-19): Situation Report 73 2 April 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200402-sitrep-73-covid-19.pdf?sfvrsn=5ae25bc7_6 (17 June 2020, date last accessed).
- 2. Asadi S, Wexler AS, Cappa CD, Barreda S, Bouvier NM, Ristenpart WD. Aerosol emission and superemission during human speech increase with voice loudness. Sci Rep 2019;9:2348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Chan JYK, Wong EWY, Lam W. Practical aspects of otolaryngologic clinical services during the 2019 novel coronavirus epidemic: an experience in Hong Kong. JAMA Otolaryngol Head Neck Surg 2020;146:519–520. [DOI] [PubMed] [Google Scholar]
- 4. Greenhalgh T, Hui Chan X, Kunti K et al. What Is the Efficacy of Standard Surgical Masks Compared to Respirator Masks. Centre for Evidence Based Medicine, Oxford, 24 March 2020. https://www.cebm.net/covid-19/what-is-the-efficacy-of-standard-face-masks-compared-to-respirator-masks-in-preventing-covid-type-respiratory-illnesses-in-primary-care-staff/?utmcampaign=1382156PPE%20in%20general%20practice&utmmedium=email&utmsource=Dotmailer&dmi=49LX,TMH8,GBY8G,3L3S4,1 (28 September 2020, date last accessed). [Google Scholar]
- 5. Bourouiba L. Turbulent gas clouds and respiratory pathogen emissions: potential implications for reducing transmission of COVID-19. J Am Med Assoc 2020;323:1837–1838. [DOI] [PubMed] [Google Scholar]
- 6. van Doremalen N, Bushmaker T, Morris DH et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med 2020;382:1564–1567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Brosseau L. Commentary: COVID-19 Transmission Messages Should Hinge on Science Center for Infectious Disease Research and Policy, University of Minnesota, 25 May 2020. https://www.cidrap.umn.edu/news-perspective/2020/03/commentary-covid-19-transmission-messages-should-hinge-science (17 June 2020, date last accessed). [Google Scholar]
- 8. Guzman M. Bioaerosol Size Effect in COVID-19 Transmission 2020. https://www.preprints.org/manuscript/202004.0093/v2 (17 June 2020, date last accessed).
- 9. Gawn J, Clayton M, Makison C, Crook B. Evaluating the Protection Afforded by Surgical Masks Against Influenza Bioaerosols: Gross Protection of Surgical Masks Compared to Filtering Facepiece Respirators Health Safety Executive, 2008. https://www.hse.gov.uk/research/rrhtm/rr619.htm (17 June 2020, date last accessed). [Google Scholar]
- 10. Occupational Safety and Health Administration. 2007. https://www.osha.gov/ (28 September 2020, date last accessed).
- 11. World Health Organization (WHO). COVID 19 PPE Advice 6 April 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance-publications (28 September, date last accessed).
- 12. Public Health England (PHE). PPE Guidance 21 May 2020. https://www.gov.uk/government/publications/wuhan-novel-coronavirus-infection-prevention-and-control/covid-19-personal-protective-equipment-ppe (17 June 2020, date last accessed).
- 13. Philpott C, Burrows S. ENTUK 23 April 2020. https://www.entuk.org/aerosol-generating-procedures-ent (17 June 2020, date last accessed).
- 14. Cherrie JW, Loh M, Aitken RJ. Protecting healthcare workers from inhaled SARS-CoV-2 virus. Occup Med (Lond) 2020;70:335–337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Howie R. Respiratory protective equipment and Covid 19. J Int Soc Res Protect 2020;37:69–71. [Google Scholar]
- 16. Lee SA, Hwang DC, Li HY, Tsai CF, Chen CW, Chen JK. Particle size-selective assessment of protection of European standard FFP respirators and surgical masks against particles-tested with human subjects. J Healthcare Eng 2016. https://www.hindawi.com/journals/jhe/2016/8572493/ (28 September 2020, date last accessed). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Guo ZD, Wang ZY, Zhang SF et al. Aerosol and Surface Distribution of Severe Acute Respiratory Syndrome Coronavirus 2 in Hospital Wards, Wuhan, China, 2020 Emerging Infectious Disease, CDC, 2020. https://wwwnc.cdc.gov/eid/article/26/7/20-0885_article (28 September 2020, date last accessed). [Google Scholar]
- 18. The Engineering ToolBox. Smoke Particle Size https://www.engineeringtoolbox.com/particle-sizes-d_934.html (28 September 2020, date last accessed).
- 19. 3M. Respiratory Protection for Airborne Exposures to Biohazards Technical Data Bulletin, 5 June 2020, #174. https://multimedia.3m.com/mws/media/409903O/respiratory-protection-against-biohazards.pdf (17 June 2020, date last accessed).
- 20. Beeching NJ, Fletcher TE, Fowler R. Coronavirus2019 (COVID-19) Best Practice https://bestpractice.bmj.com/topics/en-gb/3000168 (17 June 2020, date last accessed).
- 21. Cowper A. Ambitious rhetoric and appalling reality: the UK government’s response to Covid-19. Br Med J 2020;369:m2321. [DOI] [PubMed] [Google Scholar]
- 22. Payne A. Covid-19: skin damage with prolonged wear of FFP3 masks. Br Med J 2020;369:m1743. [DOI] [PubMed] [Google Scholar]
- 23. Bonifait L, Charlebois R, Vimont A et al. Detection and quantification of airborne norovirus during outbreaks in healthcare facilities. Clin Infect Dis 2015;61:299–304. [DOI] [PubMed] [Google Scholar]
- 24. Health and Safety Executive UK. Control of Substances Hazardous to Health Regulations https://www.hse.gov.uk/coshh/basics/index.htm (11 June 2020, date last accessed).
- 25. Jessop ZM, Dobbs TD, Ali SR et al. Personal Protective Equipment (PPE) for Surgeons During COVID-19 Pandemic: A Systematic Review of Availability, Usage, and Rationing BJS Society, 12 May 2020. https://bjssjournals.onlinelibrary.wiley.com/doi/abs/10.1002/bjs.11750 (28 September 2020, date last accessed). [Google Scholar]
- 26. Cook T, Kursumonic E, Lennane S. Exclusive: Deaths of NHS Staff From Covid-19 Analysed Health Service, 22 April 2020. https://www.hsj.co.uk/exclusive-deaths-of-nhs-staff-from-covid-19-analysed/7027471.article (17 June 2020, date last accessed). [Google Scholar]
- 27. Nursing Notes. https://nursingnotes.co.uk/ (28 September 2020, date last accessed).
- 28. Shields AM, Faustini SE, Peres-Toledo M et al. SARS-CoV-2 Seroconversion Rates in Healthcare Workers Birmingham, April 2020. https://www.medrxiv.org/content/10.1101/2020.05.18.20105197v1.full.pdf (28 September 2020, date last accessed).
- 29. Liu Y, Song Y, Hu X, Yan L, Zhu X. Awareness of surgical smoke hazards and enhancement of surgical smoke prevention among the gynecologists. J Cancer 2019;10:2788–2799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. UK Government. Death by Occupation https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/causesofdeath/bulletins/coronaviruscovid19relateddeathsbyoccupationenglandandwales/deathsregisteredbetween9marchand25may2020 (28 September 2020, date last accessed).