ABSTRACT
Introduction
Historical changes have transformed Sweden from being an offensive to a defensive and collaborative nation with national and international engagement, allowing it to finally achieve the ground for the civilian–military collaboration and the concept of a total defense healthcare. At the same time, with the decreasing number of international and interstate conflicts, and the military’s involvement in national emergencies and humanitarian disaster relief, both the need and the role of the military healthcare system within the civilian society have been challenged. The recent impact of the COVID-19 in the USA and the necessity of military involvement have led health practitioners to anticipate and re-evaluate conditions that might exceed the civilian capacity of their own countries and the need to have collaboration with the military healthcare. This study investigated both these challenges and views from practitioners regarding the benefits of such collaboration and the manner in which it would be initiated.
Material and Method
A primary study was conducted among responsive countries using a questionnaire created using the Nominal Group Technique. Relevant search subjects and keywords were extracted for a systematic review of the literature, according to the PRISMA model.
Results
The 14 countries responding to the questionnaire had either a well-developed military healthcare system or units created in collaboration with the civilian healthcare. The results from the questionnaire and the literature review indicated a need for transfer of military medical knowledge and resources in emergencies to the civilian health components, which in return, facilitated training opportunities for the military staff to maintain their skills and competencies.
Conclusions
As the world witnesses a rapid change in the etiology of disasters and various crises, neither the military nor the civilian healthcare systems can address or manage the outcomes independently. There is an opportunity for both systems to develop future healthcare in collaboration. Rethinking education and training in war and conflict is indisputable. Collaborative educational initiatives in disaster medicine, public health and complex humanitarian emergencies, international humanitarian law, and the Geneva Convention, along with advanced training in competency-based skill sets, should be included in the undergraduate education of health professionals for the benefit of humanity.
INTRODUCTION
Experiences from the medical management of victims during armed conflicts have resulted in numerous medical achievements in the use of both civilian healthcare system (CHS) and military healthcare system (MHS), and a significant reduction in the war- and trauma-related mortality rate.1–5 However, since 1946, there has been a steady decrease in the number of colonial, imperial, and interstates wars, whereas the number of civilian conflicts (with and without foreign state intervention) as well as natural and man-made disasters has increased.6–8 Consequently, the need for a war-related international engagement of the military and its healthcare system has been reduced in favor of an increased international and national disaster relief assistance. The increasing number of requests for military aid from civilian societies and foreign governments in various crises is an obvious sign of the need for close civilian–military collaboration, particularly in healthcare-related and humanitarian incidents.9–13
Whereas many of the required skills could gradually be transferred between the two systems, to both incorporate and improve medical advances and the capacity and capability of countries, the long-term consequences of such collaboration, defined here as Civilian Military Collaboration (CMC), and its efficiency in the management of future complexities of evolving health crises might still not be clear.1,3–5 A collaboration between the CHS and the MHS may not only develop a trustful civilian–military relationship and offer an opportunity and responsibility to engage strategically to improve performance and to eliminate domestic and international security issues, but it also raises the question as to whether dual healthcare organizations are needed.11–14
The approach to, and the usefulness of a CMC might be interpreted differently. In Europe, historical changes have transformed Sweden from being an offensive to a defensive and collaborative nation with national and international engagement, allowing it to finally recognize the need, and to achieve the ground, for the CMC and the concept of a Total Defense Healthcare (TDH). In the USA, however, the highly respected Uniformed Services University of the Health Sciences is facing serious closure threats. There are proposed plans to eliminate more than 17,000 uniformed medical billets across the military health system starting in October 2020.15 However, with an increasing trend toward the civilianization of war and conflict and an increasing number of unique threats that impact the security of a civilian population, the requests for military medical assistance and interventions on a national scale have actually become more frequent (Table I).16 Although the critics in the USA aim to close medical facilities and outsource the care to the private sector because of the high costs, uneven quality in care delivery, and scarcity in the number of complex cases to keep provider skills sharp between deployments, the Swedish approach aims to retain and strengthen the MHS as a powerful instrument for potential conflicts, and to treat nonbattle injuries among military staff.14,17 The concept of a TDH System is characterized by the need to use both the MHS and CHS to facilitate the care of military staff and particularly the civilian population during times of armed conflicts and humanitarian disasters.
TABLE I.
Changing Face of Global Crises: More Frequent, Expansive, and Long-Lasting
|
For Sweden, the implementation of a TDH system offers an opportunity to expand the MHS in collaboration with its civilian partners. In 2020, a Part I review in Military Medicine described the historical development of the Swedish MHS and its path toward civilian–military collaboration and a TDH system. From a Swedish defense perspective, the military operational activity cannot be maintained without an integration between the military and the civilian healthcare philosophy.17 Therefore, the current approach to achieve integration and collaborative work facilitates resource allocation, knowledge sharing, and determination of responsibilities and limitations. Additionally, it has a profound impact on the guidelines and procedures as well as the choice of equipment to support the most critically injured in the military context.17 Altogether, there would be numerous long-term socioeconomic benefits as a result of such collaboration.
What form the military aid responses might take remains under debate and dependent on whether the threat meets the capability of military medical skills or a combination of the two. During the current coronavirus disease of 2019 (COVID-19) emergency, the U.S. military forces are being used to enforce civilian quarantine, deploy hospital ships, enforce the quarantine of citizens returning from overseas, and “support law enforcement with supplies, communications, and transportation.”18 However, by using the U.S. military domestically, the matter of “authorities become paramount.” The authority to do so is “intentionally narrow, not allowing federal troops to be used in a humanitarian situation such as a pandemic,” leaving that role to each state’s National Guard and/or reservists. The deployment of military medical assets during COVID-19 generated debate among U.S. medical leadership as to what models are best for engagement and ongoing and future insults to society. Those in the European Union (EU) and other countries who observed the civilian–military decisions in the USA began to actively discuss and debate the anticipated similar responsibilities, not only regarding the current tragedy but also regarding how the civilian–military relationship and responsibilities would play out in the future. In this perspective, the Swedish concept of a TDH systems’ integration and defined collaboration seems to be a more fruitful approach. Such integration aims to retain each organization intact, whereas integration offers defined responsibility, collaboration, and knowledge of each other’s capabilities and limitations.19
The aim of this Part II study is to investigate the perceived (or lack of) benefits of the CMC as well as the potential need for a distinct MHS within the civilian society in a cross-section of countries that were experiencing serious healthcare requirements above the civilian capacity alone. A qualitative methodology study was conducted, together with a literature review.
MATERIALS AND METHODS
As a first step, a survey was conducted among experienced healthcare professionals with and without military background, inquiring about their personal opinions, in order to identify the keywords needed for a literature review.
Questionnaire Study
The questionnaire consisted of three questions, which were formulated using the Nominal Group Technique. The principal author (A.K.) assembled a group (E.C. and Y.R.). Thereafter, ideas were generated, recorded, discussed, and ranked within the group. The questions were reviewed based on a combination of logic, relevance, comprehension, legibility, clarity, usability, and consensus.20 Subsequently, they were summarized as follows:
Do you have an independent/separate MHS in your country?
Name five pros/advantages of having an independent/separate MHS.
Name five cons/disadvantages of having an independent/separate MHS.
The final questionnaire was placed on ResearchGate, a European social networking site for over 19 million scientists and researchers, which is the largest European academic network in terms of active users. Scientists and researchers share papers, ask and answer questions, and find research collaborators using this site.21 Respondents commenting on the study questionnaire were contacted by the Senior author (A.K.) and asked to voluntarily complete their comments alone or together with other or recommended subject matter experts on civilian–military health issues known to be in their network. The optimized questionnaires were forwarded to representatives from 17 countries: Belgium, Croatia, Denmark, England, Finland, Germany, Greece, Iran, the Netherlands, Norway, Romania, Saudi Arabia, Sweden, Philippines, Poland, Thailand, and Turkey. All respondents were identified as having expertise in research or holding clinical positions or both, including up-to-date knowledge of MHS and CHS. Participation was not mandatory, and their responses were processed anonymously. The results were collected and analyzed using qualitative research methods. A qualitative content analysis of the manifest content was used.22,23 First, the thematic contents were identified and then condensed into core contents. At a point where no new novel information was extracted from the data, the statements of the representatives were outlined.
Literature Review
The outcome of the questionnaire was summarized in the text and inserted into Mesh on Demand from PubMed. The keywords extracted were used in a systematic literature search using PubMed, Scopus, and Gothenburg University’s electronic database according to the PRISMA review model.24 The keywords were military, civilian, medicine, healthcare system, armed conflicts, disaster medicine, emergencies, international law, public health, relief work, advantages, and disadvantages, alone or in combination. The inclusion criteria were studies published in English from 1990 to 2020. The titles and abstracts of the identified publications were studied. Case reports, nonscientific papers, nonrelevant documents, studies that did not address or discuss the aim of this report, or were not accessible in full text were excluded. Owing to the nonquantitative nature of the research question, no meta-analysis was attempted. The findings were distributed by statements/questions based on qualitative saturation of thematic areas, divided into advantages and disadvantages of having MHS.
RESULTS
The Questionnaire
Fourteen out of 17 countries (18 individuals, three women) responded to the questionnaire (response rate = 82%). The three countries that did not respond to the first call were contacted two more times, with no results. Half of the participants had a separate MHS in their country. The backgrounds of the respondents were as follows: Belgium (M.D. with military knowledge), Croatia (M.D. with military background), England (R.N. with military background), Finland (M.D. with military background), Germany (M.D. in emergency management), Greece (M.D. in emergency management), Iran (Ph.D. in disaster management and R.N. in disaster management), the Netherlands (M.D., with military knowledge), Norway (Ph.D. in crisis management), Saudi Arabia (R.N. in emergency management), Sweden (Ph.D. in crisis management, M.D. with military background, Ph.D. in theology), Philippines (M.D. in crisis management, M.D. in emergency management), Poland (Ph.D. in crisis management and public health), and Thailand (M.D. in emergency management). The responses could be categorized into medical and nonmedical advantages and disadvantages of having a dedicated MHS. All findings are presented in Table II. Some of the statements are as follows:
TABLE II.
Advantages/Disadvantages of Having an Independent Military Healthcare System, International Perspectives
| Pros | Advantages of having a separate military healthcare system |
|---|---|
| Nonmedical |
|
| Medical |
|
| Cons | Disadvantages with a separate military healthcare system |
| Nonmedical |
|
| Medical |
|
“The most important advantage is the fact that in most austere environments, an independent military healthcare system can thrive effectively. It is easier for them to be deployed urgently to any part of the country, especially because they are under the command of the President. They receive mandatory regular training which keeps them updated; hence, they are knowledgeable and well-trained in responding urgently to emergencies on the ground.” (Cited by a M.D. without military background)
The economic resources consumed by a dedicated MHS and its effects on healthcare and the defense budget were noted as a downside.
“The most significant disadvantage is the extremely high cost of the MHS on the national budget. It is only good for countries, which are in the war, are preparing for the war, or will benefit from participation in a war. For small countries, it is certainly better to form an integrated healthcare system.” (Cited by a M.D. with military background)
In some countries, distrust towards independent military agencies disturbs the further development of an increased CMC, as well as the establishment of a dedicated MHS.
“Historically, the military has been a feared agency of the government because of the historical Martial Law abuses; hence, the trust in them has not been firmly regained.” (Cited by a M.D. and a nurse without military background)
Literature Review
The keywords the questionnaire were used to search for related literature (Fig. 1). The findings from the literature review were categorized into medical and nonmedical advantages and disadvantages of having a MHS. The majority favored advantages included collaboration, resource and information sharing, and experiences of working in an austere environment, namely the MHS. The most critical nonmedical aspects included a fear of the military’s political and economic control and the high cost of having a separate system. At the same time, the inconsistencies in knowledge, different privileges, and resource incompatibility were significant items found in the medical record. Table III extracted from outlines the advantages and disadvantages of having a separate MHS based on the literature review. The historical perspectives of military engagement in political and economic affairs were highlighted.3,5,13–16,25–57
FIGURE 1.
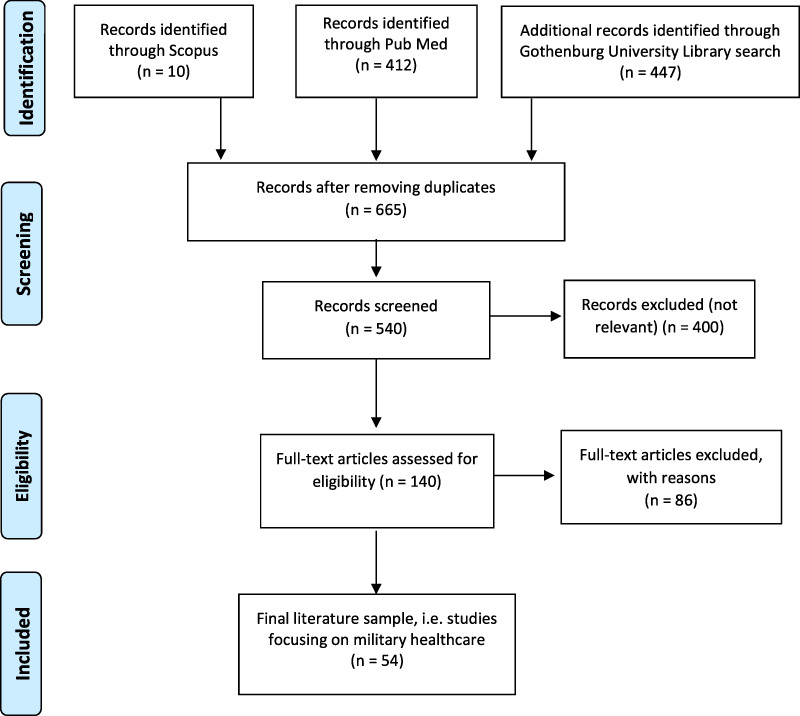
Process of literature search according to PRISMA review method/flow diagram (24).
TABLE III.
Advantages/Disadvantages of Having an Independent Military Healthcare System, Based on the Literature Review3–5,9–14,16–17,25–57
| Pros | Advantages of having a separate military healthcare system |
|---|---|
| Nonmedical |
|
| Medical |
|
| Cons | Disadvantages of having a separate military healthcare system |
| Nonmedical |
|
| Medical |
|
DISCUSSION
The results of this study emphasize the need for a separate MHS and CHS, and a long-term collaboration and investment building on the historical development in the Swedish MHS first described in Part I.17 According to all 14 different nations included in this study, there are advantages and disadvantages of a dedicated MHS. Although the respondents identified the necessity of implementing disaster and military medicine in medical education programs, the cost-effectiveness of a dedicated MHS over an integrated civilian–military solution is dependent on multiple unknown covariates and requires further study.
The current global sociopolitical situations have challenged the rules of engagement in emergencies. The threats imposed by radical organizations and terrorists have brought the intensity and cruelty of armed conflicts to civilian society.3,25–28 The lack of civilian experience in handling complex, military-like penetrating and blast injuries, economic strains, and unprepared leadership within the CHS, along with emerging and unforeseen diseases and pandemics, indicates a need for a closer partnership between the CHS and the MHS.26–30 On the other hand, the low number of emergencies and surgical procedures in peacetime demonstrates a need for MHS to establish a closer collaboration with the CHS.3,28 Such integration has been achieved within the trauma care system. It could also be facilitated in pandemic and disaster management, as is evident in the current COVID-19 pandemic.18,29–33 Furthermore, collaboration in research and clinical practice, along with developing new technologies and improved treatment strategies for subsequent conflicts or pandemics, are needed to establish updated best practices for treating nonbattle injuries, and conflict-related injuries among the military and civilian population.3,31,34–38
Irrespective of the system and size, the MHS is a separate and necessary part of the Armed Forces during deployment, not only because of unplanned wars and armed conflicts but also for the nonbattle injuries that are very specific to the military staff.14,32 Additionally, a recent increase in civilian incidents has raised an awareness of the civilian society’s vulnerability and resulted in a regeneration of the total defense concept from post-World War II, i.e., a collaborative MHS and CHS.17 Such a partnership encompasses both medical and nonmedical attachments and shortcomings, and requires reliable compatibility. Although most of the nonmedical defects can be mitigated or prevented successfully, the medical aspects and skills needed for the management of future armed conflict injuries, including exposure to chemical, biological, radiological, and nuclear (CBRN) threats, may create new challenges.3,25,35–39 A single civilian or military medical system can neither address nor manage these challenges, independently. Consequently, the outcome and survival of both the military and civilian populations can be jeopardized if the knowledge needed is not shared and addressed collaboratively.3,37–46
The MHS dedication to military missions and military staff, their expertise, their unique operational environment, experience of working in austere environments, and organized approach to emergencies complete the CHS disaster response capability and knowledge. The MHS knowledge of preventive medicine, risk assessment, and medical intelligence is instrumental in the handling of fluctuating and rising threats, unpredictability, and urgency associated with all emergencies and disasters. Military experts are invaluable assets in domestic and international operations, and their knowledge in command and control, communication, logistics, engineering support, and CBRN decontamination and care are all essential parts of emergency management.3,33,39,52 A collaborative link between the two organizations provides an academic exchange of knowledge and competency. It creates opportunities for both to realize their weaknesses and strengths, and the difficulties that each organization may face in an incident.3–5,16,54–57 This exchange is particularly valuable in situations when the experience of one organization is inferior to the other, e.g., CBRN management.36 Finally, a well-developed CMC contributes to a constructive discussion of the role of both the MHS and CHS, their moral and ethical responsibilities, and the rules of engagement. These discussions are needed as witnessed in the current political turbulences in the USA.
This study listed a few disadvantages of having a separate MHS, such as a fear of a political and economic involvement by the military, asymmetric relations, and inconsistencies. However, the positive impact of military assistance in humanitarian disaster relief has paved the way for the participation of military personnel and assets in civilian events.46,49–52 The lack of integration and asymmetric relationships between the MHS and the CHS calls for improved collaboration before the next disaster or armed conflict strikes. One way to encourage mutual adjustment and improve trust can be joint exercises and the practice of CMC during civilian activities such as mass gatherings.16,38,41,47,54–57
Limitations
The number of countries included in this study might be considered small; however, the combination of the questionnaire study and literature search can give a valid picture of the field internationally. To mitigate the selection bias, the survey was completed by a literature review. The methods used for content analysis22,23 and the PRISMA model for systematic review23 are well-known scientific instruments. However, the review has a language bias, as it included scientific articles in English and the Swedish language. Several countries have national publications in their own languages, which were not accessible or not available in translated form. Consequently, some critical information published in other languages may have been missed.
The use of the ResearchGate to recruit respondents represents a so-called “virtual snowball sampling,” which has previously been used in other published studies.21,52 This type of sampling has many advantages and disadvantages. Specifically, it helps to identify individuals of interest for this research, allows for the possibility to increase the representativeness of the results, can increase the number of responses and decrease the sampling time, and is inexpensive. On the other hand, the sample selection is biased toward the characteristics of the online population such as gender, age, education level, and socioeconomic belonging.52
We did not include countries with large military organizations such as the USA, Russia, and China, purposefully to avoid the bias that would be evident. However, although none of the countries included in this study can compare their military healthcare to the U.S. system, the USA was used as a major comparing counterpart for the following reasons: (1) Despite political challenges in the USA, it is still the most democratic country among superpowers where data for comparison is available. Consequently, several, if not the most, of internet hits result in papers written and studies performed in the USA, (2) the USA is the major actor in NATO (North Atlantic Treaty Organization), where most of the countries included in this study are either a part of it or have a collaboration with it, and (3) finally, it is not the size of the country that matters but how they managed the issues. As a result, it is clear that all these medium-sized countries not only follow up U.S. military medicine development but all social and political changes in the country. The U.S. military healthcare as well as its political agenda has dominated and played a significant role globally, and thus, should not be puzzled by being compared.
This article may have raised more questions than answers. Hopefully, it initiates the engagement and discussion needed to find a better way for benchmarking civilian–military collaborative responses, with respect to validity and reliability.
CONCLUSIONS
Global security issues, national and international terrorism, the pattern of injuries, resource scarcity, the emergence of new unpredicted and complex global public health crises, necessitate complementary knowledge in various fields and all phases of disaster management. These crises are beyond the capability of one agency and entail close interagency cooperation. They present an opportunity for the structured development of a Health Crisis Management Framework to oversee the phase-related strategic and operational requirements for the prevention, preparedness, response, recovery, and rehabilitation challenges of major global public health crises.3,16,35,36,54,55
To realize new ways of guiding and governing military engagement in global health may result in achieving a balance between the military and civilian global health capacities. Such achievement requires mechanisms for communication, coordination, and joint action across relevant entities at the national and global levels.55 Besides adding new components such as interactive training, shared resources, and higher qualifications to the existing military and civilian elements, it is more important to use the gained experiences of the previous crises to decide what assets need to be shared between the military and civilian healthcare in the future. A TDH system, consisting of a well-trained and collaborative CHS and MHS, can operate confidently in peace times and during conflicts. Moreover, it is a cost-effective strategy, which offers a high quality of care in both CHS and MHS.
The short-term impact of the downgrading, limitation, or elimination of one of the systems for the sake of economic gain, unilateral quality improvement of care and betterment of provider skills is not the answer to our needs, may cost more, and jeopardize human lives. The only solution to retain advanced and high-quality care is a partnership between the CHS and MHS. Such a partnership motivates the introduction of the military medicine curriculum at the civilian undergraduate level to increase the competency of young graduates and to strengthen the foundation of professional knowledge of potential military healthcare staff. The need for rethinking education and training in war and conflict is indisputable. Possessing clinical skills needed to manage sudden-onset disasters, public health emergencies, complex humanitarian emergencies, and training in International Humanitarian Law and Geneva Convention, along with advanced training in competency-based skill sets, should all be included in such a curriculum for the benefit of humanity.17,56,57
Contributor Information
Amir Khorram-Manesh, Institute of Clinical Sciences, Department of Surgery, Sahlgrenska Academy, Gothenburg University, 405 30, Gothenburg, Sweden; Department of Research and Development, Swedish Armed Forces Center for Defense Medicine, 426 76 Västra Frolunda, Gothenburg, Sweden.
Frederick M Burkle, Harvard Humanitarian Initiative, T.H. Chan School of Public Health, Harvard University, Cambridge, MA 02138, USA.
Phatthranit Phattharapornjaroen, Department of Emergency Medicine, Faculty of Medicine, Ramathibodi Hospital, Mahidol University, Ratchathewi, Bangkok, 10400, Thailand.
Milad Ahmadi Marzaleh, Department of Health in Disasters and Emergencies, Health Human Resources Research Center, School of Management and Medical Informatics, Shiraz University of Medical Sciences, Shiraz, 14336-71348, Iran.
Mohammed Al Sultan, Department of Emergency Medicine, King Khalid Hospital, Najran, 66262, Saudi Arabia.
Matti Mäntysaari, Aeromedical Centre, Centre for Military Medicine, PO BOX 5, 11311 Riihimäki, Helsinki, Finland.
Eric Carlström, Health and Crisis Management and Policy, Sahlgrenska Academy, Gothenburg University, Gothenburg, 40530, Sweden; Department of Business, History, and Social Sciences, University of South-Eastern Norway, 3679 Notodden, Kongsberg, Norway.
Krzysztof Goniewicz, Military University of Aviation, Dywizjonu 303 35, 08-521, Dęblin, Poland.
Emelia Santamaria, Health Emergencies and Disasters (HEAD) Study Group, National Institute of Health, University of the Philippines-Manila, 623 Pedro Gil Street, Ermita 1000 Manila, the Philippines.
John David Comandante, Department of Emergency Medicine, Prehospital Disaster and Ambulatory Care Medicine, Ospital ng Makati, Makati City, 1218 Metro Manila, the Philippines.
Robert Dobson, London Ambulance Service UK, 220 Waterloo Road, SE1 8SD, London, UK.
Boris Hreckovski, Department of Surgery, General Hospital, Slavonski Brod 35000, Croatia.
Glenn-Egil Torgersen, Harvard Humanitarian Initiative, T.H. Chan School of Public Health, Harvard University, Cambridge, MA 02138, USA.
Luc J Mortelmans, Center for Research and Education in Emergency Care, University of Leuven, Oude Markt 13, 3000, Leuven, Belgium.
Mirjam de Jong, Major Incident Hospital, University Medical Center (UMC) Utrecht, Heidelberglaan 100, 3584 CX, Utrecht, Netherland.
Yohan Robinson, Institute of Clinical Sciences, Department of Surgery, Sahlgrenska Academy, Gothenburg University, 405 30, Gothenburg, Sweden; Department of Research and Development, Swedish Armed Forces Center for Defense Medicine, 426 76 Västra Frolunda, Gothenburg, Sweden.
FUNDING
None declared.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Pruitt BA: Combat casualty care and surgical progress. Ann Surg 2006; 243(6): 715-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bowyer CMW: Surgical education in the new millennium: the military perspective. Surg Clin N Am 2004; 84(6): 1453-70. [DOI] [PubMed] [Google Scholar]
- 3. Khorram-Manesh A: Facilitators and constrainers of civilian–military collaboration: the Swedish perspectives. Eur J Trauma Emerg Surg 2020; 46: 649-56. doi: 10.1007/s00068-018-1058-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Interagency Standing Committee (IASC) . Civil–military coordination during humanitarian health action. Global health cluster. Position Paper. 2011. Available at: https://www.who.int/hac/global_health_cluster/about/ghc_annex5_civil_military_coordination_february2011.pdf?ua=1; accessed July 11, 2020.
- 5. Marklund L, Graham AM, Morton PG, et al. : Collaboration between civilian and military healthcare professionals: a better way for planning, preparing, and responding to all hazard domestic events. Prehosp Disaster Med 2010; 25(5): 399-412. [DOI] [PubMed] [Google Scholar]
- 6. Roser M: War and Peace. Our World in Data. Available at: https://ourworldindata.org/grapher/ number-of-conflicts-and-incidences-of-one-sided-violence; accessed July 11, 2020.
- 7. Ritchie H, Roser M: Natural Disasters. Our World in Data. Available at: https://ourworldindata.org/grapher/number-of-natural-disaster-events; accessed July 11, 2020.
- 8. Ritichie H, Hasell J, Appel C, Roser M: Terrorism. Our World in Data. Available at: https://ourworldindata.org/terrorism; accessed July 11, 2020.
- 9. Mullins MR, Nakano K: Disasters and Social Crisis in Contemporary Japan: Political, Religious, and Sociocultural Responses. London, UK: Palgrave Macmillan; 2016. [Google Scholar]
- 10. Interagency Standing Committee (IASC) . Operational Guidelines on the Protection of Persons in Situations of Natural Disasters, Brookings–LSE Project on Internal Displacement, 2011. Available at: https://www.ohchr.org/Documents/Issues/IDPersons/OperationalGuidelines_IDP.pdf; accessed July 11, 2020.
- 11. Jacob C: Civilian protection in the context of disaster planning and response. In: Cook ADB (ed). World Humanitarian Summit – Implications for the Asia-Pacific. RSIS Policy Report 2017; Available at: https://ebs.dai.csd.disa.mil/cgi-bin/banner_appsLogin; accessed July 11, 2020. [Google Scholar]
- 12. Inter-American Defense Board . Natural disaster in Venezuela; update January 12, 2000. ReliefWeb. Available at: https://reliefweb.int/report/venezuela-bolivarian-republic/natural-disaster-venezuela-update-12-jan-2000; accessed July 11, 2020.
- 13. Monitor EU: Military support to EU disaster response: identification and coordination of available assets and capabilities. Available at: https://www.eumonitor.eu/9353000/1/j9vvik7m1c3gyxp/vi7jgt4jbmr5; accessed July 11, 2020.
- 14. Kellerman A: The United States’ Military Health System. Health Affairs Blog 2017. doi: 10.1377/hblog20170427.059833 [DOI] [Google Scholar]
- 15. Philpott T: Plan to reduce ranks of military doctors concerns head of uniformed services medical school. February 23, 2019. Available at: https://www.thenewstribune.com/news/business/biz-columns-blogs/article226574664.html; accessed July 11, 2010.
- 16. Burkle FM Jr.: Challenges of global public health emergencies: development of health-crisis management framework. Editorial Tohoku, J Exp Med 2019; 249(1): 33-41. [DOI] [PubMed] [Google Scholar]
- 17. Khorram-Manesh A, Robinson Y, Boffard K, Örtenwall P: The history of Swedish military healthcare system and its path toward civilian-military collaboration from a total defense perspective. Mil Med 2020. doi: 10.1093/milmed/usaa071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Cancian ME: Use of military forces in the COVID-19 emergency. Center for Strategic & International Studies. (CSIS). Available at: https://www.csis.org/analysis/use-military-forces-covid-19-emergency; accessed July 11, 2020.
- 19. Melkon J, Embrey J, Bader H, Mennes B: Civil-Military interaction during infantry operations. In: Lucius G, Rietjens S (eds). Effective Civil-Military Interaction in Peace Operations. Springer Cham, 2016, 137-51. [Google Scholar]
- 20. Harvey N, Holmes CA: Nominal group technique: an effective method for obtaining group consensus. Int J Nurs Pract 2012; 18(2): 188-94. [DOI] [PubMed] [Google Scholar]
- 21. Nicholas D, Clark D, HermanHerman E: ResearchGate: reputation uncovered. Learn Publ 2016; 29(3): 173-82. [Google Scholar]
- 22. Sandelowski M: Whatever happened to qualitative description?. Res Nurse Health 2000; 23(4): 334-40. [DOI] [PubMed] [Google Scholar]
- 23. Graneheim UH, Lundman B: Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today 2004; 24(2): 105-12. [DOI] [PubMed] [Google Scholar]
- 24. Moher D, Liberati A, Tetzlaff J, Altman DG: The PRISMA Group (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009; 6(7): e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Khorram-Manesh A, Lönroth H, Rotter P, et al. : Non-medical aspects of civilian–military collaboration in management of major incidents. Eur J Trauma Emerg Surg 2017; 43(5): 595-603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hirsch M, Carli P, Nizard R, et al. : The medical response to multisite terrorist attacks in Paris. Lancet. 2015; 386(10012): 2535-8. [DOI] [PubMed] [Google Scholar]
- 27. Khorram-Manesh A: Europe on fire; medical management of terror attacks—new era and new considerations. Bull Emerg Trauma 2016; 4(4): 183-5. [PMC free article] [PubMed] [Google Scholar]
- 28. Stinner DJ, Wenke JC, Ficke JR, et al. : Extremity injuries military and civilian collaboration: the power of numbers. Mil Med 2017; 182(3/4): 10-17. [DOI] [PubMed] [Google Scholar]
- 29. Perlman S: Another Decade, Another Coronavirus. N Engl J Med 2020; 382: 760-2. doi: 10.1056/NEJMe2001126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Zhonghua Jie SY: He He Hu Xi Za Zhi. What are the highlights of diagnostic and treatment of disease 2019 Novel Coronavirus infection suitable for military support Hubei medical team. Chinese Journal of Tuberculosis and Respiratory Medicine. 2020; 43(0): E025. doi: 10.3760/cma.j.cn112147-20200225-00183 [DOI] [PubMed] [Google Scholar]
- 31. Anderson JE, Farmer DL, Hight R, Galante JM: Achieving zero preventable deaths: a model of a military–civilian medical training partnership. 2018. Available at: http://bulletin.facs.org/2018/06/achieving-zero-preventable-deaths-a-model-of-a-military-civilian-medical-training-partnership/; accessed July 11, 2020.
- 32. Schoff J: In Times of Crisis: Global and Local Civil-military Disaster Relief Coordination in the United States and Japan. Institute for Foreign Policy Analysis, Interim Report. Cambridge. Massachusetts USA: IFPA; 2007. Available at: http://www.ifpa.org/research/researchPages/TimesofCrisis.php; accessed July 11, 2020. [Google Scholar]
- 33. U.S. Department of Veterans Affairs . Public Health. Military exposures. Available at: https://www.publichealth.va.gov/index.asp; accessed July 11, 2020.
- 34. Hussain S, Azam N, Malik B, Hashim RS: Undergraduate Military Medicine—an essential need of the present time. PAFMJ 2020; 69(5): 981-5. [Google Scholar]
- 35. Kartoch A: Assessing the possible contribution of the military and the challenges faced in their deployment. Remarks at Wilton Park conference; Steyning, West Sussex: 2007. Available at: https://reliefweb.int/sites/reliefweb.int/files/resources/236476AD3257088DC125741000474F20-sipri_mar2008.pdf; accessed July 11, 2020. [Google Scholar]
- 36. Mortelmans L, Lievers J, Sabbe M, Dieltiens G: Are Belgian military trained medical officers better prepared for CBRN incidents than civilian emergency physicians? Int Rev Armed Forces Med Serv 2017; 90(2): 24-7. [Google Scholar]
- 37. Burkle FM Jr.: Population-based triage management in response to surge-capacity requirements during a large-scale bioevent disaster. Acad Emerg Med 2006; 13(11): 1118-29. [DOI] [PubMed] [Google Scholar]
- 38. Khorram-Manesh A, Berner A, Carlström E: Facilitating multiagency collaboration before mass gathering- The development of MAGRAT (Mass Gathering Risk Assessment Tool). Biomed J Sci & Tech Res 2020; 24(5): 18607-16. doi: 10.26717/BJSTR.2020.24.004114 [DOI] [Google Scholar]
- 39. Canyon DV, Ryan BJ, Burkle FM Jr.: Rationale for military involvement in humanitarian assistance and disaster relief. Prehosp Disaster Med 2020; 35(1): 92-7. [DOI] [PubMed] [Google Scholar]
- 40. UNISDR : The Human Cost of Weather-Related Disasters 1995–2015. Geneva, Switzerland: UNDRR. 2015; Available at: https://www.unisdr.org/files/46796_cop21weatherdisastersreport2015.pdf; accessed July 11, 2020. [Google Scholar]
- 41. Yates A, Bergin A: More than Good Deeds: Disaster Risk Management and Australian, Japanese and US Defense Forces, Special Report. Canberra, Australia: Australian Strategic Policy Institute; Vol. 43: 2011; 15. Available at: www.aspi.org.au/publications/publication_details.aspx?ContentID=322; accessed July 11, 2020. [Google Scholar]
- 42. Yamada S: Hearts and minds: typhoon Yolanda/Haiyan and the use of humanitarian assistance/disaster relief to further strategic ends. Soc Med 2017; 11(2): 76-82. [Google Scholar]
- 43. Fukushima AI, Ginoza A, Hase M, Kirk G, Lee D, Shefler T: Disaster militarism: rethinking US relief in the Asia-Pacific. Foreign Policy in Focus. 2014. Available at: http://fpif.org/disaster-militarism-rethinking-u-s-relief-asia-pacific/; accessed July 11, 2020.
- 44. Wiharta S, Ahmad H, Haine JY, Löfgren J, Randall T: The effectiveness of foreign military assets in natural disaster response. Stockholm International Peace Research Institute. 2008. Available at: https://www.sipri.org/publications/2008/effectiveness-foreign-military-assets-natural-disaster-response; accessed July 11, 2020.
- 45. Wooten LP, James EH: Linking crisis management and leadership competencies: the role of human resource development. Advan Develop Human Res 2008; 10(3): 352-79. [Google Scholar]
- 46. Boin A, t’Hart P: Public Leadership in Times of Crisis: mission Impossible?. Public Admin Rev 2003; 63(5): 544-53. [Google Scholar]
- 47. Eibner C: Maintaining Military Medical Skills During Peacetime. Rand Corporation. 2008; Available at: https://www.rand.org/pubs/monographs/MG638.html; accessed July 11, 2020.
- 48. Loayza NV, Olaberría E, Rigolini J, Christiaensen L: Natural disasters and growth: going beyond the averages. World Develop 2012; 40(7): 1317-36. [Google Scholar]
- 49. Benson C, Clay E: Understanding the Economic and Financial Impacts of Natural Disasters. Disaster Risk Management Series. Vol. 4: Washington, DC USA: World Bank; 2004. https://openknowledge.worldbank.org/handle/10986/15025 Available at: accessed July 11, 2020. [Google Scholar]
- 50. Omelicheva MY: Natural disasters: triggers of political instability?. Int Interact 2011; 37(4): 441-65. [Google Scholar]
- 51. Nye JS: The benefits of soft power. Working Knowledge, Harvard Business School. Available at: http://hbswk.hbs.edu/archive/4290.html; accessed July 11, 2020.
- 52. Wheeler V, Harmer A: Resetting the rules of engagement: trends and issues in military–humanitarian relations. Humanitarian Policy Group Briefing Paper. March 21, 2006. Available at: https://www.odi.org/sites/odi.org.uk/files/odi-assets/publications-opinion-files/273.pdf; accessed July 11, 2020.
- 53. Khorram-Manesh A, Plegas P, ÅHögstedt A, Peyravi M, Carlström E: Immediate response to major incidents: defining an immedi-ate responder!. Eur J Trauma Emerg Surg 2019. doi: 10.1007/s00068-019-01133-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Canyon D V, Ryan BJ, Burkle FM: Military Provision of Humanitarian Assistance and Disaster Relief in Non-Conflict Crises. J Homeland Security Emerg Manag 2017; 14(3). doi: 10.1515/jhsem-2017-0045 [DOI] [Google Scholar]
- 55. Michaud J, Moss K, Licina D, et al. : Militaries and global health: peace, conflict, and disaster response. Security and Public Health. The Lancet 2019; 393(10168): 276-86. [DOI] [PubMed] [Google Scholar]
- 56. Burkle FM, Kushner AL, Giannou C, Paterson MA, Wren SM, Burnham G: Health Care Providers in War and Armed Conflict: operational and Educational Challenges in International Humanitarian Law and the Geneva Conventions, Part II. Educational and Training Initiatives. Disas Med Public Health Prepare 2019; 13(3): 383-96. [DOI] [PubMed] [Google Scholar]
- 57. Khorram-Manesh A, Berlin J, Carlström E: Two validated ways of improving the ability of decision-making in emergencies; Results from a literature review. Bull Emerg Trauma 2016; 4(4): 186-96. [PMC free article] [PubMed] [Google Scholar]


