Abstract
Objective
To provide an update on Australian persistent pain services (number, structure, funding, wait times, activity).
Methods
An updated national search was conducted. Of those identified, 74 persistent pain services provided detailed responses between July 2016 and February 2018 (64 adult, seven pediatric, two pelvic pain, and one cancer pain). A similar structure to the original Waiting in Pain (WIP) survey was used, and participants chose online or telephone completion.
Results
Pediatric pain services had more than doubled but remained limited. Adult services had also increased, with a concurrent decrease in median wait times and an increase in the number of new referrals seen each year. Despite this, some lengthy wait times (≥3 years) persisted. Wait times were longest at clinics using public or combined funding models and offering pain management group programs (PMGPs). Although clinical activity had increased, medical staffing had not, suggesting that clinics were operating differently. Privately funded clinics performed more procedures than publicly funded services. Use of PMGPs had increased, but program structure remained diverse.
Conclusions
Specialist pain services have expanded since the original WIP survey, facilitating treatment access for many. However, wait time range suggested that the most disadvantaged individuals still experienced the longest wait times, often far exceeding the recommended 6-month maximum wait. More needs to be done. Numerous developments (e.g., National Strategic Action Plan for Pain Management, health system changes as a result of the COVID-19 pandemic) will continue to influence the delivery of pain services in Australia, and repeated analysis of service structures and wait times will optimize our health system response to the management of this condition.
Keywords: Chronic Pain, Persistent Pain, Pain Management, Wait Time, Treatment Access
Introduction
Persistent or chronic pain remains one of Australia’s largest (and arguably undertreated) health problems. With an estimated annual economic impact of A$139 billion—including health care provision, loss of income, and productivity costs—it is the country’s third most costly health condition [1]. More than one in five Australians will suffer persistent pain in their lifetime, including children [2]. As the population ages, the prevalence and cost of this condition will increase [3].
Persistent pain is associated with significant physical and psychological impairment. Impacts include poor fitness, psychological distress, depression, anxiety [4], low self-esteem, reduced workforce engagement [5], social isolation, and decreased quality of life [6]. Increased suicidality has also been demonstrated [7].
Timely and coordinated multidisciplinary treatment, which includes both physical and psychological methods, has been shown to be best-practice care for individuals with persistent pain [8]. It is also cost-effective care and is estimated to nearly halve the economic impact of this condition due to the significant patient improvement it affords [3]. Despite this, multidisciplinary treatment is not well supported by current funding models for primary health and therefore reliance on the tertiary sector remains high.
Recognizing the demand that is placed on multidisciplinary pain services—and the clinical and fiscal benefits that they provide—the Waiting in Pain (WIP) project of the Australian Pain Society [9] (data collected from December 2008 to January 2010) sought to better understand the service structures and treatment access issues experienced by pain services in this country. In particular, WIP sought to systematically examine the wait times, clinical activity (number of new patients seen), staffing (amount, type), and funding sources of Australian persistent pain services. The results showed prolonged wait times for treatment access (>18 months for some clinics), suggesting that pain services were unable to meet the level of clinical demand that they experienced. This was significantly more pronounced within the public sector compared with private services and for provincial vs urban locations, with notable geographic variances. These unacceptably long wait times (>6 months) have been shown to result in physical and psychological deterioration for individuals awaiting specialist care [10], and thus it is imperative that treatment access be improved.
There have been a number of developments in the provision of pain services in Australia since the publication of the original WIP article. For instance, significant investments have been made in persistent pain services throughout New South Wales, Queensland, and South Australia, changing the models of care and service profiles used in those regions. A national outcomes register has also been developed (Electronic Persistent Pain Outcomes Collaboration [ePPOC]) (refer to https://ahsri.uow.edu.au/eppoc/index.html), creating a standard set of core outcome measures to help services evaluate their clinical performance and inform the development of best-practice models of care. More recently, a National Strategic Action Plan for Pain Management was released by the Department of Health that called for more timely access to evidence-based assessment and treatment for individuals with persistent pain [11].
Calls to improve the health service response to persistent pain have been echoed internationally. For instance, Britain recently reported wait times of 6–112 weeks to access specialist pain services; with many clinics in breach of National Health Service–set targets, there is now a deliberate focus on building capacity within community services to alleviate pressure on specialist centers [12]. Similarly, after reporting wait times of up to 5 years to access specialist pain care [13, 14], Canada also has a renewed focus on improving the experience of individuals who are seeking treatment for this condition [15].
Given the developments since the first review, it is appropriate to again assess the state of play for persistent pain services in Australia. Accordingly, the Waiting in Pain project was updated (WIP-II) to provide a current overview of the wait times, clinical activity, staffing, and funding for Australian persistent pain services.
Methods
A national search for persistent pain services was conducted using the databases of the Australian Pain Society, Painaustralia, and the state-based Department of Health, as well as internet searches. Once the detailed list was compiled, a research and survey consulting firm (InSync) was engaged to build an online survey portal, conduct the survey, and collate the results in a de-identified manner.
In total, 109 services were identified and invited to participate in the project: 99 adult services, seven pediatric services, two services specializing in pelvic pain, and one dedicated to the management of cancer pain. All services were contacted via email and invited to participate in the project either through an online portal (link and password emailed with the invitation to participate) or via telephone interview. The research consulting firm or the primary author followed up with nonresponders.
Surveys were conducted between July 2016 and February 2018. The survey structure was similar to that used in the original WIP project; core quantitative questions explored the primary source(s) of funding for each service (>90% public, >90% private, combined); amount (full-time equivalent [FTEs]) and type (discipline) of staffing; amount of clinical activity (number of new referrals received and seen each year); and wait times that newly referred individuals experienced before attending a first appointment. Services were asked to respond to these questions using data from their previous 12 months of operation.
Consistent with the original project, services were grouped by state or territory and classified by location (as per the Australian Bureau of Statistics, “urban” = located within a capital city; “provincial” = located outside a capital city) and the updated International Association for the Study of Pain (IASP) classification levels (Level 1 refers to a multidisciplinary pain [MDP] management center with multiple disciplines, education, and research; Level 2 refers to an MDP management clinic operating as per Level 1 but without research and/or teaching; and Level 3 refers to a pain practice without multidisciplinary or interdisciplinary care, including a single practitioner or pain management modality).
Data Analysis
Data were collated, de-identified, and initially analyzed by the research consulting firm using Microsoft Excel. They were further analyzed, where appropriate, using SPPS version 26 [16]. Preliminary analysis involved calculating descriptive statistics for each of the core questions. Where appropriate, comparisons were made with data from the original WIP study.
Data were examined to assess the impact of service factors (i.e., location, predominant funding source, IASP classification) on wait times, clinical activity, and staffing. Specifically, analysis of variance and t tests were used to explore the impact of service factors on clinical activity as a function of medical staff FTE. Medical FTE were specifically chosen because doctors tend to be involved in all new assessments at Level 1 and 2 services. Mann-Whitney U or Kruskal-Wallis tests were used to examine the impact of service factors on wait times due to the skewed distribution of these data. A chi-squared test (χ2) was used to assess differences in the frequency of IASP classification according to service activity. Pearson correlation coefficients were calculated to assess the correlation between wait times and proportional levels of private funding for those services that had a combined funding model. Findings with a probability of P<0.05 were considered statistically significant.
Ethics and Funding
This study was approved by the Human Research and Ethics Review Committee of Royal Melbourne Hospital (HREC QA2016072). Funding was provided by the Australian Pain Society, with additional funding from the Department of Anaesthesia and Pain Management at Royal Melbourne Hospital.
Results
Overview of Services
This survey identified 109 persistent pain services throughout Australia, an increase of 41 clinics since the original WIP project (Nidentified = 68). For adult services, the largest growth occurred in clinics that were predominantly privately funded (WIP: n = 23; WIP-II: n = 48), with comparatively smaller increases in the number of clinics that utilized public or combined funding models (WIP: n = 45; WIP-II: n = 51). Pediatric pain services also increased (WIP: n = 3; WIP-II: n = 7), and three specialist clinics had been created to cater specifically to adults with cancer (n = 1) or pelvic (n = 2) pain.
Of the 109 services that were identified and invited to participate in the WIP-II project, 33 declined to participate or failed to respond despite several invitations. Most (n = 27) of the nonparticipating services were identified as being predominantly privately funded. In total, 76 Australian persistent pain services agreed to participate and responded to the WIP-II survey: sixty-six general adult services, seven pediatric services, and the three specialist adult services. Two general adult services were subsequently excluded due to incomplete data collation.
Of those clinics that went on to respond to the survey, growth in adult persistent pain services was most common throughout Victoria, in provincial areas, and in the public sector. These were typically structured as IASP Level 1 clinics (refer to Supplementary Data). Data regarding pediatric pain services were limited but indicated that the number of clinics had more than doubled since the original WIP project. New services were identified in Queensland, New South Wales, Victoria, and Western Australia. All services were publicly funded, and most (n = 6) were urban clinics that were classified as IASP Level 1 MDP management centers. Pediatric services reported seeing a total of 997 new patients in the preceding 12 months, equating to 0.03% of the Australian population aged 14 years or younger (the age used by the Australian Bureau of Statistics when defining the pediatric population). The median wait time for a new assessment was 32.5 days, with medical staff seeing an average of 110 new patients per FTE.
Given the limited representation of pediatric and specialist adult (pelvic pain, cancer pain) clinics in survey responders, subsequent analyses were focused exclusively on the 64 remaining general adult persistent pain services.
Adult Persistent Pain Services
As outlined in Table 1, the majority of adult services were classified as Level 1 MDP management centers (n = 44, 69%) that were primarily publicly funded (n = 37, 58%) and urban based (n = 48, 75%). Approximately half were associated with a hospital inpatient acute pain service (ntotal = 34, 53%; public = 28, private = 4, combined = 2), offered telehealth services (ntotal = 33, 52%; urban = 23, provincial = 10), and/or participated in the ePPOC (n = 37, 58%). Preclinic education was offered by 32 clinics (50%), with marked variation in the format (e.g., mandatory vs voluntary), timing (e.g., on referral, within a few weeks, just before initial appointment), and duration (range: 1.5–5 hours) of sessions. A total of 97 research projects were identified across 32 services. Although the majority (n = 43, 67%) of services used multiple sources of data (e.g., electronic and paper records), activity estimates for nearly a third (n = 10, 27%) of all publicly funded services were made independent of any formal health system for data collection. As per the original WIP survey, publicly funded services were more likely to be classified as Level 1 MDP management centers than were privately funded clinics (χ2[2] = 8.5, P < 0.014). Fewer services reported using a combination of public and private funding in this survey compared with the original WIP project (WIP: n = 13, 23%; WIP-II: n = 7, 11%), but this difference was not significant (χ2[2] = 3.4, P = 0.18) (refer to Supplementary Data).
Table 1.
Data for Australian adult persistent pain services by population, clinical activity, service type, and funding sources
| State or Region | Adult Population* | No. of Patients Seen | No. (%) of Services | IASP Classification Level |
Funding |
Services with PMGPs | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | >90% Public | >90% Private | Combined | |||||
| National | 19,966,901 | 36,650 | 64 (100) | 44 (69) | 14 (22) | 6 (9) | 37 (58) | 20 (31) | 7 (11) | 53 (83) |
| ACT | 332,052 | 900 | 1 (1.5) | — | 1 (100) | — | — | 1 (100) | — | 1 (100) |
| QLD | 3,961,732 | 3,279 | 6 (10) | 6 (100) | — | — | 5 (83) | 1 (17) | — | 6 (100) |
| NSW | 6,396,242 | 8,467 | 18 (28) | 13 (72) | 5 (28) | — | 13 (72) | 3 (17) | 2 (11) | 16 (89) |
| NT | 192,356 | 242 | 3 (5) | 1 (33) | 1 (33) | 1 (33) | 2 (67) | 1 (33) | — | 1 (33) |
| SA | 1,417,961 | 3,577 | 4 (6) | 3 (75) | — | 1 (25) | 2 (40) | 2 (60) | — | 3 (75) |
| VIC | 5,157,216 | 16,693 | 27 (42) | 17 (63) | 6 (22) | 4 (15) | 13 (55) | 10 (32) | 4 (13) | 22 (81) |
| TAS | 427,391 | 500 | 1 (1.5) | 1 (100) | — | — | 1 (100) | — | — | 1 (100) |
| WA | 2,078,147 | 4,479 | 4 (6) | 3 (75) | 1 (25) | — | 1 (40) | 2 (40) | 1 (20) | 3 (75) |
| Region | ||||||||||
| Urban | 30,720 | 48 (75) | 35 (73) | 8 (17) | 5 (10) | 24 (50) | 18 (38) | 6 (12) | 40 (83) | |
| Provincial | 5,930 | 16 (25) | 9 (56) | 6 (38) | 1 (6) | 13 (81) | 2 (13) | 1 (6) | 13 (81) | |
IASP = International Association for the Study of Pain; IASP classification Level 1=multidisciplinary pain (MDP) management center with several disciplines, education, and research; IASP classification Level 2=MDP clinic but without research and/or teaching; IASP classification Level 3=pain clinic without multidisciplinary or interdisciplinary care or modality-oriented clinic using single practice or pain management modality; PMGP = pain management group program; ACT = Australian Capital Territory; QLD = Queensland; NSW = New South Wales; NT = Northern Territory; SA = South Australia; VIC = Victoria; TAS = Tasmania; WA = Western Australia.
Figures are N (%).
Australian Bureau of Statistics estimation from September 2017, released March 2018, population aged ≥15 years. An estimated 33% of the adult population resides in provincial areas (2016).
Clinical activity data were not consistently reported by all survey responders. Those who did report this information (n = 61) saw a combined total of 36,650 new patients during the preceding 12 months, equating to 0.18% of the Australian adult population. This represented an average of 600.8 new patients (SD = 789.2) per service and was comparable to the level of clinical activity that was reported in the original WIP study (Nnew patients = 31,779, Nservices = 57; M = 557.5, SD = 631.4) (t[116] = 0.3, P = 0.74). As might be expected, most of this activity was conducted in metropolitan services, with urban clinics seeing the equivalent of 0.23% and provincial clinics seeing the equivalent of 0.09% of their respective populations. A total of 9,442 individuals were wait-listed across 48 services, with the greatest number of people being wait-listed at publicly funded clinics and level 1 services (Table 2).
Table 2.
Number of people on waiting list and wait times experienced at Australian adult persistent pain services
| Total Pain Management Services | No. of People on Waiting List |
Waiting Time, Days |
|||||
|---|---|---|---|---|---|---|---|
| Total | Average per Service | Range | Median | Range | IQR | ||
| National | 64 | 9,442 | — | 0–1,000 | 60 | 2–1,277 | 20.5–170 |
| ACT | 1 | 120 | 120 | — | 10 | — | — |
| QLD | 6 | 2,018 | 404 | 40–800 | 138 | 7–173 | 90–163 |
| NSW | 18 | 2,360 | 169 | 0–600 | 60 | 12–280 | 21–90 |
| NT | 3 | 70 | 35 | 15–55 | 40 | 5–240 | 22.5–140 |
| SA | 4 | 455 | 228 | 43–412 | 178 | 28–1,277 | 49–544 |
| VIC | 27 | 4,119 | 206 | 0–1,000 | 60 | 2–1,095 | 21–177.5 |
| TAS | 1 | 50 | 50 | — | 100 | — | — |
| WA | 4 | 250 | 83 | 50–100 | 13 | 6–84 | 10.5–31.5 |
| Region | |||||||
| Urban | 48 | 7,158 | 205 | 0–1,000 | 56 | 3–1,277 | 17–170 |
| Provincial | 16 | 2,284 | 176 | 0–543 | 85 | 2–1,095 | 29–162 |
| Funding | |||||||
| >90% public | 37 | 7,528 | 235 | 0–1,000 | 110 | 12–1,277 | 62–201 |
| >90% private | 20 | 359 | 40 | 0–120 | 14.5 | 2–60 | 7–23.5 |
| Combination | 7 | 1,555 | 22 | 16–600 | 42 | 7–546 | 16.5–190 |
| IASP Classification | |||||||
| Level 1 | 44 | 7,626 | 224 | — | 62 | 2–1,277 | 22–179 |
| Level 2 | 14 | 1,606 | 146 | — | 57 | 7–240 | 15.5–170 |
| Level 3 | 6 | 210 | 210 | 70 | 16.5 | 3–100 | 5–52 |
IQR = interquartile range; ACT = Australian Capital Territory; QLD = Queensland; NSW = New South Wales; NT = Northern Territory; SA = South Australia; VIC = Victoria; TAS = Tasmania; WA = Western Australia; IASP = International Association for the Study of Pain; IASP classification Level 1=multidisciplinary pain (MDP) management center with several disciplines, education, and research; IASP classification Level 2=MDP clinic but without research and/or teaching; IASP classification Level 3=pain clinic without multidisciplinary or interdisciplinary care or modality-oriented clinic using single practice or pain management modality.
Wait Times for Adult Persistent Pain Services
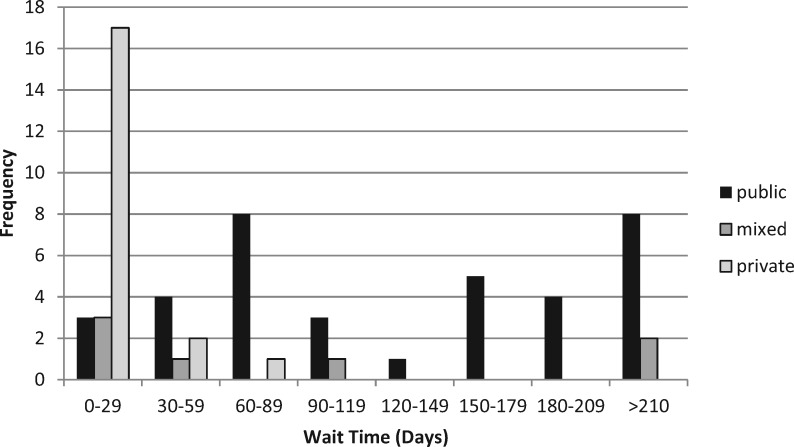
The median values, ranges, and interquartile ranges (IQRs) for wait time information based on location, funding, and IASP classification are presented in Table 2. Figure 1 shows the skewed frequency distribution of wait time data (Shapiro-Wilk statistic = 0.581; P < 0.001). Overall, the national median wait time for a first appointment at an adult persistent pain service was 60 days (IQR: 20–170). However, most services (n = 57) used a structured triage process for urgent referrals (e.g., persons with cancer pain, acute neuropathic pain states, high levels of distress), and the median wait time for those individuals was 14 days within a skewed distribution (Shapiro-Wilk statistic = 0.74; P < 0.001). Overall, this represents a significant reduction in wait times since the original WIP project (WIP: median = 103; IQR: 43.5–210; WIP-II: median = 60; IQR: 20–170) (Mann-Whitney U = 1,380; P < 0.029), suggesting that access to treatment for adults with persistent pain has improved in Australia. However, although median wait times significantly decreased, the range in wait times experienced in many states and territories continued to exceed the recommended maximum wait of 6 months (< 180 days), with South Australia and Victoria in particular reporting wait times of up to 3 years (or longer) for some individuals (Table 2).
Figure 1.
Wait times (days) experienced at Australian adult persistent pain services.
In terms of factors that may contribute to wait times, there was no significant difference in wait times across IASP classification level (Level 1: median = 62; IQR: 21–185; Level 2: median = 57; IQR: 13.5–173; Level 3: median = 16.5; IQR: 4.5–70) (Kruskal-Wallis H[df, 2] = 4.52, P = 0.11) or location of service (urban: median = 56; IQR: 14–170; provincial: median = 85; IQR: 28.5–175.5) (Mann-Whitney U = 440; P = 0.31). Funding type was a significant factor for wait time variance (mean rank: public = 41.89; combined = 31.57; private = 14.35) (Kruskal-Wallis H[df, 2] = 29.05, P < 0.001), with post hoc pairwise comparisons suggesting that private services (median = 14.5; IQR: 6.3–24.5) had significantly shorter wait times than either combined (median = 42; IQR: 12–280) (r = 2.14, P<0.032) or publicly funded services (median = 110; IQR: 62–203.8) (r = 5.39, P < 0.001). There was, however, no significant difference between public and combined funded facilities (r = 1.36, P = 0.52), echoing the findings from the original study. A smaller proportion of services reported using a combined funding model than they had in the original study, but this difference was not significant (WIP: 22.8%; WIP-II: 10.9%; P = 0.18) (refer to Supplementary Data). For those that used combined funding, the variance in the overall percentage that came from private sources was not related to wait times (r = 0.12, P = 0.8). Wait times were, however, significantly longer at services that offered a multidisciplinary pain management group program (PMGP: median = 80; IQR: 21.5–179.8) than they were at clinics that did not (median = 21; IQR: 5–60) (Mann-Whitney U = 420; P < 0.015).
Clinical Activity and Medical Staffing for Adult Persistent Pain Services
The 64 adult services that participated in the WIP-II project reported seeing a total of 36,650 new referrals in the preceding 12 months—a 15.3% increase in the overall number of new appointments provided in Australia per annum since the original study (31,779) (refer to Supplementary Data). Although this additional clinical activity is consistent with the identified growth in pain services, it was not associated with a concurrent increase in the average amount of medical FTE (minus psychiatry) that was employed nationally (WIP: 1.97; WIP-II: 2.29) (t[119] = 0.9, P = 0.37). This suggests that services were operating more efficiently, such that medical clinicians were seeing more new patients within the same staffing establishment, and/or that additional activity was being undertaken by nonmedical staff.
Overall, IASP Level 2 clinics saw more new referrals per medical FTE (minus psychiatry) (M = 636, SD = 380) than Level 1 centers (M = 280, SD = 214) (t[51] = 4.2, P < 0.001). However, the number of new referrals seen per medical FTE did not differ as a function of the funding model used by the service (private: M = 635, SD = 931; public: M = 368, SD = 292; combined: M = 264, SD = 191) (F[2,54] = 1.6, P < 0.2).
Throughout the nation, adult persistent pain services performed an estimated 24,000 minor (e.g., epidural steroid injections, joint injections, or denervation) and 1,300 major (e.g., implantable neuromodulation systems) interventional procedures. This represents a similar number of minor procedures to that reported in the original WIP study, but a relative increase in major activity (WIP: Nminor = 22,300, Nmajor = 380). The combined number of major and minor procedures differed significantly between the three types of funding sources (F[2,61] = 3.43, P < 0.05), with post hoc analysis suggesting that privately funded clinics performed more procedures overall than did publicly funded services (private: M = 669.2; public: M = 223.4) (t[55] = 2.56, P < 0.013).
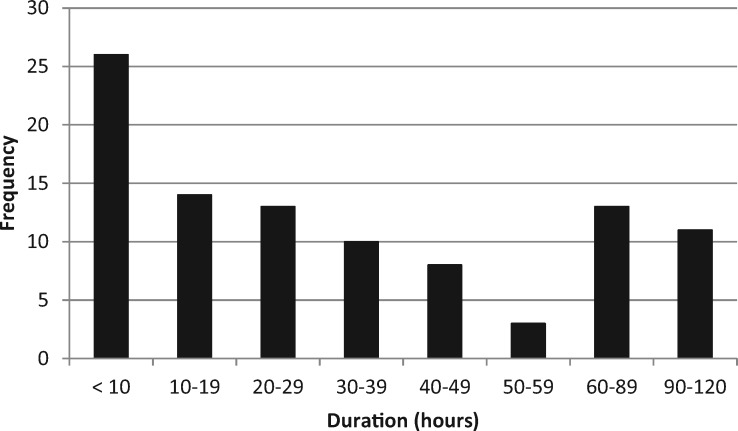
Allied Health–Led Pain Management Group Programs
The use of allied health–led multidisciplinary PMGPs has increased since the original survey, with 83% of services now offering this form of treatment compared with 74% previously (refer to Supplementary Data). Overall, 98 PMGPs were described, with many of the Level 1 centers (n = 23) offering more than one option. Group programs ranged in duration from 2 hours (pain education groups) to 120 hours (intensive multidisciplinary programs) (Figure 2). Qualitative data regarding program description and purpose suggested that shorter programs focused on pain education, patient assessment, goal identification, and introductory education modules regarding pain management, whereas programs of longer duration focused on physical restoration with integrated psychological therapy.
Figure 2.
Duration (hours) of pain management group programs offered by Australian adult persistent pain services.
Discussion
The provision of specialist multidisciplinary pain services in Australia has evolved over several decades. Our original WIP project documented the service structures, wait times, and staffing levels that were associated with these specialist clinics. This follow-up assessment (WIP-II) sought to provide an update to the original survey and, in doing so, documented an expansion of pain services in Australia, specifically in the areas of pediatric services and privately funded adult clinics. However, data regarding the number of patients who were wait-listed for treatment were not consistently reported (Nreported = 48, Nparticipated = 64), meaning that the extent to which this expansion meets clinical needs is not yet clear.
Treatment access has improved overall since the original WIP survey, resulting in a significant decrease in national wait times and a >15% increase in the number of people who are able to access a new appointment with a specialist pain service each year. There also appears to have been a change in the model of care that pain services are using. For instance, although there are now more pain clinics seeing more new patients each year, this was not associated with a concurrent increase in medical FTEs, suggesting perhaps that medical staff may be deploying their services differently than they had at the time of the original survey, such that they can see more new patients within the same allocated time (e.g., via group assessments). Alternatively, it may be that some (or all) of the additional activity is being undertaken by nonmedical personnel, and this would be reflected within changes to service structures more broadly. Allied health–led multidisciplinary PMGPs have become more common over time, with a greater percentage of services offering this form of treatment now compared with the original survey. Together, these findings suggest a move toward more integrated multidisciplinary, or perhaps allied health led, activities within Australian pain services, an assertion that requires specific exploration.
Despite these improvements, wait times remain longer for clinics that offer multidisciplinary PMGPs compared with those that do not. Moreover, the range in reported wait times was diverse, with some individuals being wait-listed for 3 years or longer, often with no clear indication of when they may expect to receive an appointment. Given that group programs are commonly recommended for individuals who are most negatively affected by persistent pain and that wait times of 6 months or longer have been associated with further deterioration [10], this means that treatment access remains most restricted for those individuals at the greatest disadvantage and that many will be further disadvantaged by being indefinitely wait-listed for specialist care.
Access also continues to vary by location and age, with urban clinics seeing the equivalent of 2.5 times more of their local population than provincial clinics, and 7.7 times more of the adult population than the equivalent for pediatric services. These disparate rates of treatment access suggest that the provincially-based and pediatric populations continue to experience a significant disadvantage. However, the full extent of this disadvantage has yet to be clarified. A number of adult-based services (public and private) reported providing input to the pediatric population, but that was not specifically reflected herein, as activity numbers were difficult to delineate. The same is likely true for provincially-based patients, with many receiving appointments at urban-based clinics. Moreover, although growth in specialist pediatric pain services was noted since the original project, the authors are aware that further growth has occurred following completion of the WIP-II survey (refer to http://www.wch.sa.gov.au/services/az/divisions/psurg/acutepain/index.html). As such, the data contained herein are likely to be an underestimation of the amount of pediatric and provincial pain service activity that is actually provided throughout Australia.
These findings are consistent with updated data from the Canadian Pain Task Force [17], which indicate a small reduction in wait times (2006: median = 6 months; maximum = ≥5 years; 2018: median = 5.5 months; maximum = ≥4 years) and a doubling of pediatric pain services (2006: N = 5; 2018: N = 9) throughout Canada in the past 12 years. However, it seems that rural populations may have comparatively better access to specialist pain services in Australia, with 25% of Australian clinics being provincially-based compared with 9% in Canada.
Although we identified an increase in the number of persistent pain services in Australia, a large number of privately funded clinics declined to participate in the assessment. As such, our interpretation of staffing, activity, and wait times may not be representative of activity in that part of the pain sector. Indeed, the improved treatment access experienced in certain areas may be better attributed to growth in the private sector than to improved public services, but this remains to be tested.
The finding that private clinics performed more procedures than their publicly funded counterparts and were less likely to be associated with a hospital inpatient acute pain service suggests that service profiles may differ between public and private clinics. Similarly, the finding that the number of combined public and private service delivery models has decreased since the original WIP investigation potentially suggests that there may be a level of incompatibility between the two funding models, potentially driving different activity targets. Integration of persistent pain expertise with inpatient acute pain services is of particular relevance given the importance of early identification of the development of persistent pain and concerns regarding opioid prescribing on discharge from the hospital. Improving linkages, particularly for privately funded services, should be a focus of future service developments. Collaborative cross-sector policies, co-located services with shared staffing models, interclinic collaboration and training, and shared research agendas could facilitate this.
Any assessment of this sort relies on self-reported data. Data collation processes have improved since the original WIP survey, but further improvements are anticipated with the increasing availability of integrated hospital electronic medical record systems. Similarly, survey participation remains voluntary and, unsurprisingly, private clinics had the lowest participation rates. The complex electronic survey used in this study, although time consuming to develop, ensures more cohesive de-identified data collection and analysis, and facilitates the ability to conduct repeated surveys to track developments over time. The consistency of data in relation to the previous assessment and between like services suggests a degree of validity for the technique, especially as the previous assessment predominantly consisted of in-person interviews.
Conclusion
The WIP-II survey indicates that specialist pain services have expanded in Australia over the past several years. This has resulted in decreased wait times to access specialist care and a 15% increase in the number of new referrals that are able to be seen each year. Despite these improvements, the range in wait times remains diverse—extending to 3 years and beyond in some areas—and wait times are longest at clinics offering multidisciplinary group programs, the type of treatment offered to individuals who are most disabled by their pain. The original WIP project provided some initial staffing profiles to aid service design and development [18]—data that now need to be revisited in light of this national expansion of pain services. Hence, there is more to be done to improve treatment access in this sector. Numerous developments will continue to influence the delivery of specialist pain management services in Australia, including the rollout of the National Strategic Action Plan for Pain Management, government investment in the design and delivery of multidisciplinary pain education (e.g., https://www.grants.gov.au/? event=public.GO.show&GOUUID=55D024DB-FDD4-46E9-C77A3C54B4E9155A), and advances in aged care processes that seek to support the identification and timely treatment of pain in the elderly (refer to https://agedcare.royalcommission.gov.au/Pages/default.aspx). Geographic boundaries will also be unpacked by the advances in telehealth processes and billing structures that have been escalated in response to the COVID-19 pandemic, facilitating connections between urban-based specialist services and provincially-based consumers and clinicians. As these changes affect our community, repeated analysis of service structures and wait times will help to optimize our health system response to the issues confronting those living with persistent pain. Establishing clinical benchmarks will be pivotal.
Supplementary Material
Acknowledgments
The authors wish to acknowledge the support of InSync, specifically the efforts of Christie Lum and Stephen Herbert; Fiona Hodson, immediate past President of the Australian Pain Society; and the staff of the participating pain management services.
Supplementary Data
Supplementary Data may be found online at http://painmedicine.oxfordjournals.org.
Funding sources: This study was approved by the Human Research and Ethics Review Committee of Royal Melbourne Hospital (HREC QA2016072). Funding was provided by the Australian Pain Society, with additional funding from the Department of Anaesthesia and Pain Management at Royal Melbourne Hospital.
Disclosure: Although these do not represent a conflict of interest, the authors wish to disclose their commercial engagements. Malcolm N. Hogg’s employer has received an honorarium for medical education and advisory board activity for Mundipharma Pty Ltd and Seqirus Pty Ltd. A.L.J. Burke has received honoraria for General Practitionerand nursing education sessions and steering committee participation from Mundipharma, Therapeutic Guidelines, and Pfizer/Elixir Health. Malcolm N. Hogg is a past president and A.L.J. Burke is the current president of the Australian Pain Society, which receives sponsorship for its annual scientific meeting and research scholarship program from a range of pharmaceutical and medical device companies, including Seqirus, Mundipharma, and Pfizer Australia. The Waiting in Pain II project, which forms the basis of this analysis, is a systematic investigation of persistent pain services in Australia and was funded via a grant from the Australian Pain Society and with the support of the Department of Anaesthesia and Pain Management at Royal Melbourne Hospital.
References
- 1. Deloitte Access Economics. The Cost of Pain in Australia. Australia: Painaustralia; 2019. Available at: https://www.painaustralia.org.au/static/uploads/files/the-cost-of-pain-in-australia-final-report-12mar-wfxbrfyboams.pdf (accessed January 22, 2020).
- 2. Blyth FM, March LM, Brnabic AJM, Jorm LR, Williamson M, Cousins MJ. Chronic pain in Australia: A prevalence study. Pain 2001;89(2–3):127–34. [DOI] [PubMed] [Google Scholar]
- 3. Access Economics. The high price of pain: The economic impact of persistent pain in Australia. 2007. Available at: http://www.bupa.com.au/staticfiles/BupaP3/Health%20and%20Wellness/MediaFiles/PDFs/MBF_Foundation_the_price_of_pain.pdf (accessed November 2011).
- 4. Burke ALJ, Mathias JL, Denson LA. Psychological functioning of people living with chronic pain: A meta-analytic review. Br J Clin Psychol 2015;54(3):345–60. [DOI] [PubMed] [Google Scholar]
- 5. Leeuwen MT, Blyth FM, March LM, Nicholas MK, Cousins MJ. Chronic pain and reduced work effectiveness: The hidden cost to Australian employers. Eur J Pain 2006;10(2):161–6. [DOI] [PubMed] [Google Scholar]
- 6. Kerr S, Fairbrother G, Crawford M, Hogg MN, Fairbrother D, Khor KE. Patient characteristics and quality of life among a sample of Australian chronic pain clinic attendees. Intern Med J 2004;34(7):403–9. [DOI] [PubMed] [Google Scholar]
- 7. Tang N, Crane C. Suicidality in chronic pain: A review of the prevalence, risk factors and psychological links. Psychol Med 2006;36(5):575–86. [DOI] [PubMed] [Google Scholar]
- 8. National Pain Summit Initiative. National Pain Strategy: Pain management for all Australians. 2011. Available at: http://www.anzspm.org.au/c/anzspm?a=sendfile&ft=p&fid=1320268502&sid (accessed November 2012).
- 9. Hogg MN, Gibson S, Helou A, DeGabriele J, Farrell MJ. Waiting in pain: A systematic investigation into the provision of persistent pain services in Australia. Med J Aust 2012;196(6):386–90. [DOI] [PubMed] [Google Scholar]
- 10. Burke ALJ, Mathias JL, Denson LA. Waiting for multidisciplinary chronic pain services: A prospective study over 2.5 years. J Health Psychol 2020;25(9):1198–212. [DOI] [PubMed] [Google Scholar]
- 11. Commonwealth of Australia. National Strategic Action Plan for Pain Management. Canberra: Commonwealth of Australia; 2019. [Google Scholar]
- 12. Connelly D. Losing faith: The patients waiting years for specialist pain treatment. Pharm J 2020;304(7934):(doi: 10.1211/PJ.2020.20207656). [Google Scholar]
- 13. Lynch ME, Campbell F, Clark AJ, et al. A systematic review of the effect of waiting for treatment for chronic pain. Pain 2008;136(1–2):97–116. [DOI] [PubMed] [Google Scholar]
- 14. Peng P, Choiniere M, Dion D, et al. Challenges in accessing multidisciplinary pain treatment facilities in Canada. Can J Anaesth 2007;54(12):977–84. [DOI] [PubMed] [Google Scholar]
- 15. Liddy C, Poulin PA, Hunter Z, Smyth C, Keely E. Patient perspectives on wait times and the impact on their life: A waiting room survey in a chronic pain clinic. Scand J Pain 2017;17(1):53–7. [DOI] [PubMed] [Google Scholar]
- 16. SPSS Inc. IBM SPSS Statistics. 20th ed Chicago, IL: IBM; 2011. [Google Scholar]
- 17. Campbell FA, Hudspith M, Anderson M, et al. Chronic pain in Canada: Laying a foundation for action. Health Canada 2019. Available at: https://www.canada.ca/en/health-canada/corporate/about-health-canada/public-engagement/external-advisory-bodies/canadian-pain-task-force/report-2019.html (accessed October 25, 2019). [Google Scholar]
- 18. Burke ALJ, Denson LA, Mathias JL, Hogg MN. An analysis of multidisciplinary staffing levels and clinical activity in Australian tertiary persistent pain services. Pain Med 2015;16(6):1221–37. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.