Abstract
Objective
The objective was to evaluate implementation of telehealth physical therapy in response to COVID-19 and identify implementation strategies to maintain and scale up telehealth physical therapy within a large urban academic medical center.
Methods
The Reach Effectiveness Adoption Implementation Maintenance (RE-AIM) framework was used to evaluate telehealth physical therapy implementation. Patient-level data were extracted from electronic medical records between March 16, 2020, and May 16, 2020 (implementation phase). Reach was defined as the proportion of physical therapy sessions completed via telehealth. Effectiveness was assessed using a patient-reported satisfaction survey with a 5-point Likert scale. Adoption was defined as the proportion of physical therapists who used telehealth. Implementation was assessed through qualitative analysis of patient and clinician perspectives to identify emergent themes, retrospectively classify strategies used during the implementation phase, and prospectively identify evidence-based strategies to increase telehealth maintenance and scale-up. Maintenance of telehealth was defined as the proportion of patients who indicated they would attend another telehealth session.
Results
There were 4548 physical therapy sessions provided by 40 therapists from March 22, 2020, to May 16, 2020, of which 3883 (85%) were telehealth. Ninety-four percent of patients were satisfied. All physical therapists (100%) used telehealth technology at least once. Retrospectively classified and prospectively identified evidence-based strategies were organized into 5 qualitative themes that supported implementation: organizational factors (policies, preexisting partnerships), engaging external stakeholders (satisfaction survey), champions (clinician leaders), clinician education (dynamic, ongoing training), and process (promote adaptability, small tests of change). Ninety-two percent of patients reported they would attend another telehealth session.
Conclusion
Findings from this study suggest that implementation of telehealth physical therapy during the COVID-19 pandemic was feasible and acceptable in this setting.
Impact
These results can be used to guide future health policy, quality improvement, and implementation science initiatives to expand the use and study of telehealth for physical therapy.
Keywords: Telehealth, Quality Improvement, Implementation Science, Outpatient Physical Therapy, Hospital-Based
Introduction
Telehealth technology has long been considered an option for delivering high-quality, high-value physical therapist intervention.1 Use of telehealth within physical therapist practice has promising efficacy for improving rehabilitation outcomes in patients with orthopedic conditions (eg, total joint arthroplasty, low back pain), neurologic injury (eg, stroke, amyotrophic lateral sclerosis), and chronic, disabling health conditions.2–8 Further, the estimated cost of using telehealth technology in physical therapist practice appears feasible.9
Reimbursement limitations have been a significant barrier to widespread telehealth physical therapy adoption in the United States. For example, the Centers for Medicare and Medicaid Services did not have billing codes for telehealth physical therapy services, and physical therapists were not eligible telehealth providers prior to the COVID-19 pandemic. In the early stages of the pandemic, local and state policies were enacted to slow the spread of the virus.10,11 Specifically, the San Francisco Bay Area, a region with early community spread of COVID-19, initiated an aggressive shelter-in-place plan, limiting contact with people outside of their immediate household and nonessential travel, and closing nonessential operations.11 During the months of March and April, many commercial insurance providers minimized barriers to reimbursement of telehealth physical therapy. On April 30, the Centers for Medicare and Medicaid Services issued policy changes to include physical therapists as eligible providers of telehealth services, allowing beneficiaries to access rehabilitative care during the public health emergency.12
Implementation of promising innovations (eg, telehealth physical therapy) within health care operations should consider the complex interactions of contextual factors (eg, patient, clinician, administrative) with a guiding framework.13–15 The Reach Effectiveness Adoption Implementation Maintenance (RE-AIM) framework has been used to prospectively, concurrently, and retrospectively plan and evaluate the translation of scientific innovations into a variety of pragmatic, “real-world” settings.15,16 The elements of the RE-AIM framework guide the planning and evaluation process by focusing efforts in 5 key domains. The domains, including reach, effectiveness, adoption, implementation, and maintenance, are extensively described elsewhere.15,16 Implementation outcomes, which are measures of implementation success, can be particularly relevant in early implementation stages to understand the context and strategies (eg, Expert Recommendations for Implementation Change [ERIC] project) that should be used to facilitate maintenance and scale-up.17,18
To date, there have been few published reports describing telehealth physical therapy implementation planning or evaluation. Additionally, implementation strategies to maintain and scale up telehealth physical therapy remain unclear. Therefore, the purpose of this study was to evaluate implementation of telehealth physical therapy in response to COVID-19 from patient and clinician perspectives and identify implementation strategies to maintain and scale up long-term telehealth physical therapy within a large urban academic medical center.
Methods
Implementation Site
Telehealth physical therapy was implemented at the University of California, San Francisco Medical Center Outpatient Physical Therapy Faculty Practice on March 15, 2020. The first week of implementation was a transition period when patients were contacted and rescheduled with telehealth physical therapy sessions. In-person physical therapy sessions were permitted through the first week of implementation for patients who were unable to be contacted or rescheduled.
The faculty practice operates 3 clinics within the city and county of San Francisco and has 44 practicing physical therapist clinicians who have board certification in orthopedics (n = 27), neurology (n = 5), geriatrics (n = 2), and sports (n = 2). The 3 outpatient clinics serve patient populations with a range of socioeconomic, educational, racial, ethnic, and geographic diversity. Although use of telehealth physical therapy was minimal prior to the public health emergency, University of California, San Francisco Medical Center had an electronic medical record, technology infrastructure, and clinical expertise to support a large-scale transition to telehealth physical therapy.
Data Sources and Collection
The COVID-19 pandemic disrupted clinical care at a rapid pace. The RE-AIM framework can accommodate for ongoing, iterative planning and was used to evaluate the implementation phase success.15,16 The implementation phase was defined by the city and county of San Francisco shelter-in-place order from March 16, 2020, to May 16, 2020.11,19 Patient-level data were extracted from electronic medical records between March 16, 2020, and May 16, 2020. Data included number of sessions (new, follow-up) delivered using telehealth or in-person, patient demographics (eg, age, sex, race/ethnicity), and patient clinical characteristics, (eg, referring diagnosis, comorbidity burden). Faculty practice administrative scheduling groups were used to categorize referring diagnosis as orthopedic (eg, spine pain, osteoarthritis, sprain/strain, tendonitis, postoperative rehabilitation [eg, anterior cruciate ligament repair, joint replacement]), neurology (eg, amyotrophic lateral sclerosis, vestibular disorders, multiple sclerosis, abnormality of gait, falls), pelvic health (eg, stress incontinence, pelvic and perineal pain), and other/nonspecified (eg, amputation, oncology). Comorbidity burden was measured using the Charlson comorbidity index.20 To contextualize potential differences in telehealth use, data were also extracted from March 16 to May 16, 2019. Administrative incident reports related to telehealth physical therapy were also extracted from the implementation phase to identify potential safety concerns.
A patient satisfaction survey (Fig. 1) was administered to all patients who received telehealth physical therapy using the Research Electronic Data Capture platform.21 The satisfaction survey contained 10 items that requested patients rate their satisfaction in a variety of domains (eg, getting connected, using telehealth, hearing, seeing, feeling safe, comfort, the physical therapist, additional information, meeting expectations, and overall session) on a 5-point Likert scale (1: Not at all satisfied; 3: Satisfied; 5: Very satisfied). The satisfaction survey also included a single yes/no question—“Would you participate in another telehealth physical therapy session?”—and 3 open-ended questions eliciting patient feedback for the best aspects of telehealth, how to improve the telehealth experience, and other comments.
Figure 1.
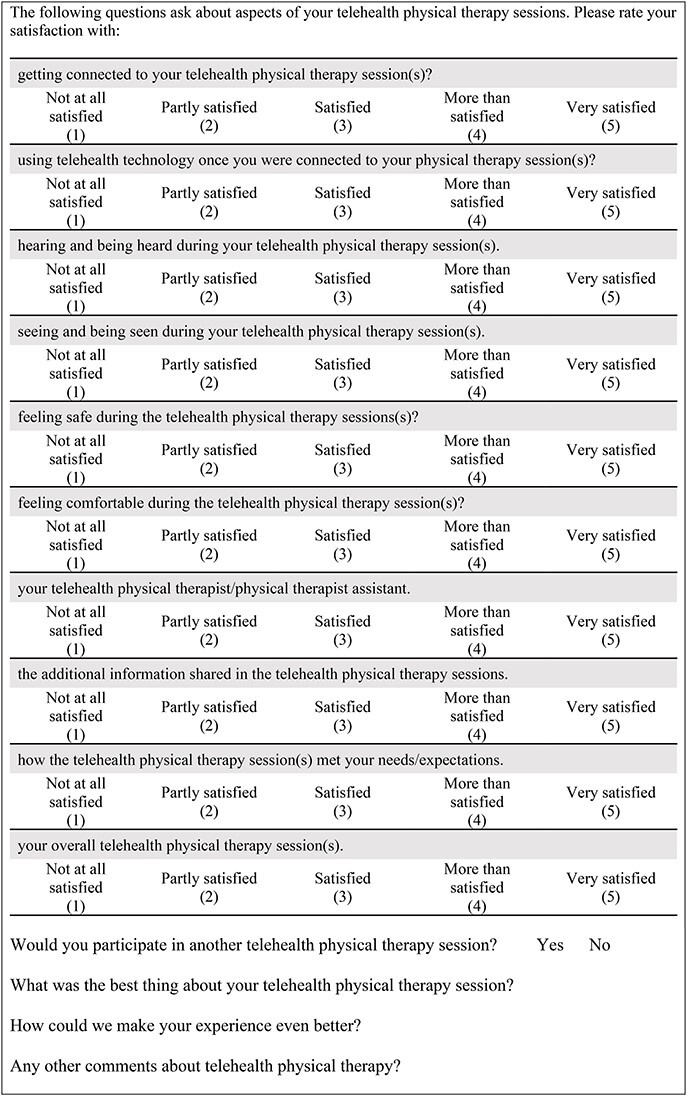
Patient satisfaction survey.
Clinic clinicians’ and supervisors’ perspectives were obtained using qualitative methods. The lead author (M.J.M.) took extensive field notes while engaging in telehealth-focused staff meetings, task force meetings, educational sessions, and clinician interviews. During these meetings, clinician leaders (ie, champions) described patient, clinician, and administrative barriers to telehealth implementation, facilitated problem solving to address barriers, and provided education. Clinicians volunteered for one-time videoconference interviews (approximately 45 minutes each) in groups of 1 to 3 participants with a stated goal to understand how clinicians are adapting to telehealth sessions, identify emergent challenges, and explore potential solutions. Clinician interview procedures included a welcome, introductions, description of interview goals, a statement of interview confidentiality, and interview questions (eg, “What is going well with telehealth?” “What isn’t going well with telehealth?” “What would you change to make improvements?” “What aspects of telehealth do you need more training in?”). Throughout qualitative data collection from clinicians and supervisors, the lead author had opportunities to ask clarifying and probing questions to obtain additional detail and perspectives. The University of California, San Francisco Institutional Review Board determined that this study involved quality improvement activities and did not require Institutional Review Board oversight.
Analysis
Each element of the RE-AIM framework was analyzed separately. The primary measure of reach was the proportion of sessions that were telehealth physical therapy (new, follow-up). Secondary measures of reach included patient demographic and clinical characteristics. Measures of reach were analyzed using data from March 22 to May 16 because the first week (March 16, 2020, to March 21, 2020) was a transition period. Reach in 2019 versus 2020 was compared using Fischer exact and Pearson χ2 tests, where P < .05 indicated significance. Effectiveness was conceptualized as patient satisfaction and safety.18 Satisfaction was measured as the proportion of patients who had an average score of 3 or more (at least satisfied) on the 10-item satisfaction survey. Safety was assessed as the number and description of adverse events during the implementation phase. Adoption was measured as the proportion of physical therapists using telehealth technology at least once and the average proportion of physical therapists’ sessions that were delivered using telehealth technology during the implementation phase.
Qualitative methods have previously been used to assess implementation with the RE-AIM framework.22 An applied thematic analysis approach, which emphasizes pragmatic, efficient, and rigorous analysis, was selected for the purpose of identifying emergent themes from qualitative data.23 Patient satisfaction survey open-ended questions and field notes (clinician interviews, implementation-focused meetings) were coded by the lead author (M.J.M.) using a structural coding strategy, where responses to primary questions were assigned unique codes.23 Following coding, data from patients and field notes were merged, similar codes and concepts were condensed into categories, and emergent themes (barriers/facilitators) were identified. The iterative qualitative analysis was led by M.J.M. and enhanced by weekly feedback from a clinical champion (D.R.K.) and/or clinic supervisors to discuss, refine, and finalize emergent themes.
Potential for maintenance and scale-up of telehealth implementation was assessed as the proportion of patients who responded “yes” to the single question regarding participation in another telehealth physical therapy session.
Finally, M.J.M. and D.R.K. used the ERIC framework17 to retrospectively classify strategies used in the implementation phase, prospectively identify strategies to maintain and scale up telehealth, and identify strategy application exemplars. A stakeholder meeting with champions, supervisors, and academic stakeholders was convened to obtain feedback and consensus on prospective implementation strategies for telehealth maintenance and scale-up.
Role of the Funding Source
Dr Miller’s time was supported by the National Institutes of Health (NIH 5T32AG000212–27). The funders played no role in the design, conduct, or reporting of this study.
Results
Reach
There were 4548 physical therapy sessions from March 22, 2020, to May 16, 2020 (Tab. 1). Telehealth physical therapy comprised 85% of sessions (84% new, 91% follow-up) during the implementation phase in 2020 (Tab. 1), and the comparison period had a higher total volume of sessions (9255) and lower proportion of telehealth physical therapy (<1%). The week-by-week distribution of telehealth and in-person (new and follow-up) sessions during the implementation phase is represented in Figure 2. There were 1501 unique patients served during the implementation phase. Compared with the prior year, a greater proportion of patients reached were younger, primarily English speaking, non-Hispanic White, commercially insured, and had fewer medical comorbidities (Tab. 2).
Table 1.
Comparison of Physical Therapy Session Types Completed During Telehealth Implementation Phase (2020) and Comparison Period (2019)a
| Physical Therapy Session Types | Comparison Periodb | Implementation Phasec | P |
|---|---|---|---|
| New physical therapy sessions (N = 2604) | |||
| In-person | 1785 (100) | 74 (9) | <.001d |
| Telehealth | 0 (0) | 745 (91) | |
| Follow-up physical therapy sessions (N = 11,199) | |||
| In-person | 7452 (>99) | 591 (16) | <.001d |
| Telehealth | 18 (<1) | 3138 (84) | |
a Data presented as n (%).
b Comparison period: March 22, 2019, to May 16, 2019.
c Implementation phase: March 22, 2020, to May 16, 2020.
d Significant Fisher exact test (P < .05).
Figure 2.
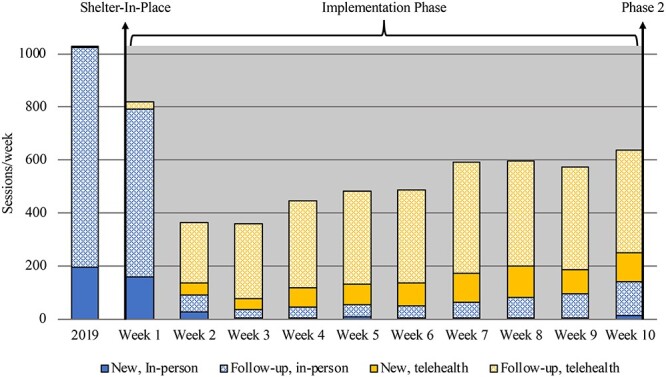
Distribution of in-person and telehealth sessions (new and follow-up) by week during implementation phase (March 22, 2020, to May 16, 2020) and average sessions/week during comparison period (March 22, 2019, to May 16, 2019).
Table 2.
Unique Patient Characteristics During Implementation Phase (2020) and Comparison Period (2019)a
| Characteristics | Comparison Periodb | Implementation Phasec | P |
|---|---|---|---|
| (N = 3169) | (N = 1501) | ||
| Age, y | <.001d | ||
| < 45 | 1287 (41) | 732 (49) | |
| 45–65 | 1025 (32) | 486 (32) | |
| > 65 | 857 (27) | 283 (19) | |
| Men | 1118 (35) | 532 (35) | .51 |
| English speaking | 2981 (94) | 1475 (98) | <.001d |
| Race/ethnicity | .002d | ||
| Non-Hispanic White | 1639 (52) | 826 (55) | |
| Black/African American | 190 (6) | 91 (6) | |
| Asian | 666 (21) | 240 (16) | |
| Hispanic/Latino | 298 (9) | 152 (10) | |
| Unknown | 376 (12) | 192 (13) | |
| Comorbidity burden | <.001d | ||
| No comorbid conditions | 2260 (71) | 1153 (77) | |
| 1-2 comorbid conditions | 558 (18) | 205 (14) | |
| ≥ 3 comorbid conditions | 351 (11) | 143 (10) | |
| Referral diagnosis category | <.001d | ||
| Orthopedic | 2485 (78) | 1131 (75) | |
| Neurologic | 298 (9) | 119 (8) | |
| Pelvic health | 227 (7) | 158 (11) | |
| General/unspecified | 159 (5) | 93 (6) | |
| Insurance type | <.001d | ||
| Commercial | 2060 (65) | 1091 (73) | |
| Medicaid | 357 (11) | 136 (9) | |
| Medicare | 725 (23) | 255 (17) | |
| Other | 27 (1) | 19 (1) |
a Data presented as n (%).
b Comparison period: March 22, 2019, to May 16, 2019.
c Implementation phase: March 22, 2020, to May 16, 2020.
d Significant Fisher exact test (P < .05).
Effectiveness
The satisfaction survey was sent to 1153 (75%) patients, and surveys were returned by 307 (27%) patients. The 10-item patient satisfaction survey was complete for 270 patients, and 254 (94%) were at least satisfied. There was 1 adverse event during the implementation phase, which was a noninjurious controlled fall.
Adoption
All physical therapists conducted at least 1 telehealth session, indicating 100% adoption. The average (SD) proportion of physical therapists’ sessions that were delivered using telehealth technology during the implementation phase was 89% (16%).
Implementation
Qualitative analysis of patient satisfaction open-ended questions, and field notes from clinician interviews (n = 19 clinicians) and implementation-focused meetings resulted in 5 emergent themes (barriers/facilitators). These emergent themes were placed within a context that shelter-in-place was perceived as temporary, and would move to a new phase with less restrictive guidelines. Specific to the shelter-in-place, clinician discussions and open-ended satisfaction survey responses indicated satisfaction with telehealth physical therapy sessions and physical therapy outcomes could be highest with a mix of in-person and telehealth sessions. The 5 emergent themes were: organizational factors, engaging external stakeholders, champions, clinician education, and process. Implementation phase strategies were retrospectively classified according to the ERIC framework and organized by emergent themes (Tab. 3). Organizational factors that facilitated telehealth implementation included organizational policy changes, preexisting academic partnerships, and access to previously untapped telehealth resources (eg, software, hardware). Clinician leaders (ie, champions) were critical factors for addressing 2 significant patient- and clinician-level barriers to telehealth implementation: clinician education and process. Champions spearheaded clinician education efforts through multiple mechanisms and worked with leadership to conduct small tests of change that could be expanded to the larger group of clinicians. Engagement with external stakeholders through a satisfaction survey was a necessary step toward developing an understanding of potential for future adaptations of telehealth physical therapy. Finally, consensus for which strategies should be used to maintain and scale up telehealth physical therapy was achieved among supervisors, champions, and academic stakeholders (Tab. 3).
Table 3.
Strategies and Examples Organized by Emergent Themes for Implementation Phase and Implementation Maintenance and Scale-Upa
| Emergent Themes: ERIC Strategy | Implementation Phase: Strategy Application Exemplar | Maintenance and Scale-Up: Strategy Application Exemplar |
|---|---|---|
| ORGANIZATIONAL FACTORS | ||
| Mandate change | • The primary factors for implementation were mandated physical distancing and hospital system policies that did not restrict access to services due to insurance coverage (eg, telehealth physical therapy) | • Clinicians, supervisors, academic partners, and stakeholders will continue to advocate for ongoing telehealth insurance coverage and reimbursement • Ongoing identification and education of external opinion |
| Access new funding Inform local opinion leaders |
• CMS policies and other insurance providers expanded telehealth access | leaders to maintain and scale-up telehealth physical therapy by champions, supervisors, and academic partners |
| Conduct local consensus discussions | • Departmental consensus discussions occurred during the week prior to shelter-in-place and the decision was made to implement telehealth physical therapy | • Champions and supervisors to expand academic partnerships to facilitate telehealth physical therapy network weaving refinement and growth |
| Develop academic partnerships | • Existing academic partnerships facilitated the identification of data experts (eg, informatics, implementation science) to guide implementation | • Champions and academic partners will identify external organizations for information sharing to facilitate collaborative problem solving |
| Use data experts | • Existing collaborations to facilitate reach of telehealth were preliminarily identified | • Supervisors and clinician leaders will conduct quarterly audits for billing, consent, and documentation guidelines |
| Promote network weaving | • Hospital system had adequate technology and financial resources to support telehealth physical therapy implementation and educational meetings | |
| Audit and provide feedback | • Supervisors conducted audits (eg, billing, consent documentation) and electronically reported findings to clinicians weekly | |
| ENGAGING EXTERNAL STAKEHOLDERS | ||
| Intervene with patients/consumers to enhance uptake and adherence | • Scheduling algorithm was used by administrative staff to identify and intervene on specific patient concerns (eg, technology, perceptions of telehealth physical therapy) when needed | • Clinicians and champions will develop and refine marketing materials for patients and referring providers • Expand use of social media and clinic website • In addition to satisfaction survey use, data experts and |
| • Patients with unaddressed concerns were encouraged to speak with a physical therapist to answer specific questions | academic partners will iteratively explore qualitative barriers to telehealth within specific patient populations | |
| Use mass media | • Supervisors, champions, and clinicians contacted referring providers to inform them of telehealth implementation | • Champions, supervisors, and academic partners will target specific populations to increase reach and uptake of |
| Involve patients/consumers and family members | • Social media and websites were updated to reflect implementation of telehealth sessions | telehealth |
| • Satisfaction survey was developed and implemented to obtain patient feedback | ||
| CLINICIAN LEADERS (CHAMPIONS) | ||
| Identify and prepare champions | • Champions were identified by supervisors for smaller implementation-focused task forces, and led small cycles of change to inform planned scale-up strategies | • Champions will be an ongoing departmental resource for supervisors, clinicians, administrative staff, and administrative staff |
| Identify early adopters | • Champions communicated, at least daily, with supervisors, clinicians, and administrative staff, facilitating education and problem solving | • New champions will be identified by supervisors, when needed, to lead implementation scale-up efforts |
| Recruit, designate, and train for leadership | • Champions and supervisors led weekly video-based implementation-focused meetings to engage clinicians as stakeholders by identifying and discussing their specific concerns | • Dependent on the implementation scale-up project, supervisors will consider the use of protected time |
| Organize clinician implementation team meetings | • Champions were allotted protected time to complete implementation-focused tasks | |
| CLINICIAN EDUCATION | ||
| Develop educational materials | • Ongoing education was provided to clinicians by champions and supervisors using multiple modes (eg, staff meetings, lunch-and-learn presentations, in-services, email, videos, cheat sheets) | • Clinicians will have ongoing knowledge sharing through case presentations, one-on-one mentorship, shadowing experts, and grand rounds presentations |
| • Informal communication methods (eg, email, online message boards, texting, web-conferencing) supported clinician local knowledge sharing beyond formal pathways | • Clinicians, champions, and supervisors will identify additional sources of local knowledge (eg, orthopedics, telehealth) and external experts to advance clinician education about telehealth practices | |
| Conduct educational meetings | • Champions developed short videos and tip sheets as a reference for | • Future education topics selected by clinicians include: |
|
Make training dynamic |
dissemination to clinicians • Education topics included, but were not limited to: |
 Advanced telehealth clinical decision making Advanced telehealth clinical decision making Selecting and administering objective measures using telehealth Selecting and administering objective measures using telehealth |
| Conduct ongoing training |  Basic telehealth software troubleshooting Basic telehealth software troubleshooting |
 Telehealth exercise prescription and progression Telehealth exercise prescription and progression |
| Capture and share local knowledge |  Tips and tricks for patient education Tips and tricks for patient education |
• Clinicians, champions, and academic partners will promote |
| Shadow other experts |  Patient scheduling workflows Patient scheduling workflows |
relationships with consultants who have expertise in telehealth |
| Conduct educational outreach visits |  Benefits of telehealth Benefits of telehealth |
technology, implementation science, and/or physical therapist |
| Provide ongoing consultation |  Basic clinical decision making with telehealth Basic clinical decision making with telehealth |
practice |
| PROCESS | ||
| Assess for readiness and identify barriers and facilitators | • Clinician needs (eg, work-from-home agreements, hardware, software) to conduct telehealth sessions were assessed by supervisors and met a minimum standard. Needs regarding telehealth sessions from home with limited exercise equipment were not specifically addressed | • Assessment of barriers, facilitators, and needs by champions and supervisors will be ongoing. For example, adjustment to clinical environment to include telehealth physical therapy while maintaining physical distancing • Supervisors and data experts will use satisfaction surveys and |
| Change physical structure and equipment | • Patient barriers to access (eg, technology, scheduling) were identified using satisfaction surveys and open forums for discussion with clinical and administrative staff | qualitative engagement with external stakeholders to guide targeting of specific barriers to telehealth access • Supervisors will explore centralized technical support for patients |
| Conduct local needs assessment | • Local technical assistance for patients was provided by Rehabilitation Aides when needed | with UCSFMC Telehealth Department for technical issues, previsit education |
| Centralize technical assistance | • Hospital system IT department was consulted for clinician technical assistance when needed | • Champions to lead scale-up of higher volume of in-person visits and flexibility of mixed in-person and telehealth physical therapy sessions |
| Provide local technical assistance | • Small tests of change throughout implementation, led by champions, created opportunities for planned scale-up | • Scale-up to include increasing reach to specialty populations (eg, neurology, pelvic health) |
| Stage implementation scale-up | • Patient satisfaction survey, specific to telehealth physical therapy, was developed, tested, and implemented by data experts using Redcap | • Patient satisfaction survey will continue, potentially managed by a third party to centralize data collection and management • Supervisors and champions to lead reassessment and testing |
| Promote adaptability | • Informal quality monitoring pathways (eg, patient report to staff) provided insight for implementation success until formal mechanisms were in place with satisfaction survey and administrative reports stabilized | electronic collection of patient-reported outcome measures |
| Conduct cyclical small tests of change | • Mechanisms to electronically collect patient-reported outcome measures, potential measures of quality, were identified by champions, data experts, and supervisors | |
| Purposely reexamine the implementation | ||
| Develop and implement tools for quality monitoring | ||
a CMS = Centers for Medicare & Medicaid Services; ERIC = Expert Recommendations for Implementing Change; UCSFMC = University of California, San Francisco Medical Center.
Maintenance
The single yes/no question was completed by 305 patients, with 92% of respondents reporting willingness to participate in additional telehealth physical therapy sessions.
Discussion
The purpose of this study was to evaluate implementation of telehealth physical therapy in response to COVID-19 and identify implementation strategies to maintain and scale up long-term telehealth physical therapy within a hospital-based outpatient clinic. During the implementation phase, telehealth was used to reach patients in 85% of sessions, and adopted by 100% of physical therapists. Patients were largely satisfied and indicated they would attend another telehealth physical therapy session. Finally, implementation strategies were retrospectively classified with the ERIC framework, and prospectively identified for future telehealth maintenance and scale-up.
There is mounting evidence supporting telehealth physical therapy for people with a variety of disabling health conditions.2–9 Despite this evidence, the rigorous methods used in prior research limits generalizability of findings into “real-world” settings, where telehealth is yet to be adopted.15,16 Telehealth physical therapy implementation has previously been evaluated in the skilled nursing facility setting,8 but reports from other practice settings are limited. The positive findings from the present study contribute to the understanding of telehealth physical therapy implementation by providing evidence of the feasibility and potential for success within a large urban medical center.
Evaluating reach during the implementation phase can inform future work to make access to telehealth equitable.15 For example, patient characteristics from the implementation phase and comparison period suggest that specific populations can experience barriers to telehealth physical therapy. Patients reached during the implementation phase were predominantly under the age of 65, non-Hispanic White, English speaking, commercially insured, and had a Charlson comorbidity index of 0. Compared with the prior year, the representation of patients who were older than 65, non–English speaking, Asian, had a Charlson comorbidity index of at least 1, and had noncommercial insurance that was smaller, suggesting potential interrelatedness of these characteristics. Alternatively, the smaller representation could be a response to initial Centers for Disease Control and Prevention recommendation for people with underlying health conditions.24 Importantly, age, race, ethnicity, insurance status, among other patient characteristics, are associated with telehealth access and use across health care disciplines.25–28 Further research is needed to understand potential mechanisms of equitable access for physical therapy when using telehealth technology.
Low acceptability, satisfaction, and adoption can be a significant barrier to implementation maintenance.18 In general, patients were more than satisfied, and 92% of patients reported willingness to participate in another telehealth session. Additionally, an average of 89% of physical therapist caseloads was completed using telehealth. For patients and clinicians, the perception of shelter-in-place as a temporary period placed telehealth as a suitable alternative to no physical therapy, and many patients and clinicians desired maintenance of telehealth sessions beyond the pandemic. Although there is risk of response bias toward those who had a telehealth session and were sent and then completed the satisfaction survey, the positive findings suggest there are patients who find telehealth an acceptable option for physical therapy access.
The application of evidence-based implementation strategies from the ERIC project is relevant for the generalizability of the present study findings.17 Although a priori implementation planning is recommended,16,18 prospective selection of telehealth implementation strategies was not feasible for this study. Therefore, strategies from the implementation phase were retrospectively classified, and prospectively identified to increase the potential for maintenance and scale-up of telehealth. The majority of prospectively identified strategies were a progression of retrospectively classified strategies. For example, clinician education will be progressed from basic topics (eg, connectivity troubleshooting, benefits of telehealth) to advanced topics (eg, screensharing anatomic images, exercise videos, telehealth clinical decision making). Alternatively, some prospective strategies were not formally used during the implementation phase, and require ongoing effort. For example, collaborative rehabilitation clinics (eg, Integrated Sports Rehabilitation Group, Pelvic Health, Amyotrophic Lateral Sclerosis Clinic) were aware of the telehealth implementation efforts; yet, formal engagement and network weaving was not undertaken during the implementation phase. Iterative, small tests of change will inform the development of specialized processes to optimize the function of collaborative clinics using telehealth technology.
Limitations
This quality improvement study using the RE-AIM framework was conducted within 1 setting, and emergent themes (barriers/facilitators) might not generalize to other contexts. Although the RE-AIM framework is used for implementation planning, research suggests the application of multiple theories, models, and/or frameworks is needed to optimize implementation success at different stages.29 For example, determinant frameworks (eg, consolidated framework for implementation research,14 theoretical domains framework30) and/or implementation theory (eg, normalization process theory31) could be used to formally assess barriers, facilitators, and strategies of telehealth physical therapy implementation during subsequent maintenance, scale-up, and optimization phases.
The pragmatic nature of this study was largely a retrospective analysis of administratively collected data that could be queried from the medical record during a relatively short period of time, therefore analyses of prospectively planned quantitative and qualitative data collection were limited. The use of a satisfaction survey has potential to increase the risk of response bias toward patients who participated in telehealth physical therapy and completed the survey. The early stage of this implementation effort necessitated the use of implementation outcomes,18 and clinical effectiveness indicators were not available. Prospective quantitative and qualitative methods should be conducted to further investigate patient-, clinician-, and organization-level implementation barriers, especially for underrepresented patient populations, and effectiveness of selected implementation strategies. Research is also needed for methods to collect clinical effectiveness measures through remote means.
Conclusions
Implementation of telehealth physical therapy during the COVID-19 pandemic was successful in a large urban medical center. Compared to prior use, the reach and adoption of telehealth physical therapy during the implementation phase were higher. Further, patients’ satisfaction and willingness to have additional telehealth physical therapy sessions were high.
The positive findings from this study demonstrate that patients find telehealth acceptable and physical therapy services can be delivered using telehealth technology. These study findings can be used to guide future policy, quality improvement, and implementation science initiatives to expand the use and study of telehealth for physical therapy.
Acknowledgments
The authors thank the patients, clinicians, and leaders at the University of California, San Francisco Medical Center (UCSFMC) Outpatient Physical Therapy Faculty Practice who participated in the telehealth physical therapy implementation.
Contributor Information
Matthew J Miller, Department of Physical Therapy and Rehabilitation Science, and Division of Geriatrics, University of California, San Francisco, 1500 Owens Street, Box 0736, San Francisco, CA 94158, USA.
Sang S Pak, Department of Physical Therapy and Rehabilitation Science, University of California, San Francisco, San Francisco, California, USA.
Daniel R Keller, Department of Physical Therapy and Rehabilitation Science, University of California, San Francisco, San Francisco, California, USA.
Deborah E Barnes, Department of Psychiatry and Behavioral Sciences, and Department of Epidemiology and Biostatistics, University of California, San Francisco; and San Francisco VA Health Care System, San Francisco, California, USA.
Author Contributions
Concept/idea/research design: M.J. Miller, D.R. Keller, D.E. Barnes
Writing: M.J. Miller, S. Pak, D.R. Keller
Data collection: M.J. Miller, S. Pak, D.R. Keller
Data analysis: M.J. Miller, S. Pak, D.R. Keller
Project management: M.J. Miller
Providing institutional liaisons: D.R. Keller
Consultation (including review of manuscript before submitting): D.E. Barnes
Funding
This work was supported by the National Institutes of Health (NIH 5T32AG000212–27).
Disclosures
The authors completed the ICMJE Form for Disclosure of Potential Conflicts of Interest and reported no conflicts of interest.
References
- 1. Digital Physical Therapy Task Force . Report of the WCPT/INPTRA Digital Physical Therapy Task Force. In: World Confederation for Physical Therapy and International Network of Physiotherapy Regulatory Authorities. 2020.
- 2. Nelson M, Bourke M, Crossley K, Russell T. Telerehabilitation is non-inferior to usual care following total hip replacement—a randomized controlled non-inferiority trial. Physiotherapy. 2020;107:19–27. [DOI] [PubMed] [Google Scholar]
- 3. Paxton RJ, Forster JE, Miller MJ, Gerron KL, Stevens-Lapsley JE, Christiansen CL. A feasibility study for improved physical activity after total knee arthroplasty. J Aging Phys Act. 2018;26:7–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Laver KE, Adey-Wakeling Z, Crotty M, Lannin NA, George S, Sherrington C. Telerehabilitation services for stroke. Cochrane Database Syst Rev. 2020. doi: 10.1002/14651858.CD010255.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sarfo FS, Ulasavets U, Opare-Sem OK, Ovbiagele B. Tele-rehabilitation after stroke: an updated systematic review of the literature. J Stroke Cerebrovasc Dis. 2018;27:2306–2318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Helleman J, Van Eenennaam R, Kruitwagen ET, et al. Telehealth as part of specialized ALS care: feasibility and user experiences with “ALS home-monitoring and coaching”. Amyotroph Lateral Scler Front Degener. 2020;21:183–192. [DOI] [PubMed] [Google Scholar]
- 7. Christiansen CL, Miller MJ, Murray AM, et al. Behavior-change intervention targeting physical function, walking, and disability after dysvascular amputation: a randomized controlled pilot trial. Arch Phys Med Rehabil. 2018;99:2160–2167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lee ACW, Billings M. Telehealth implementation in a skilled nursing facility: case report for physical therapist practice in Washington. Phys Ther. 2016;96:252–259. [DOI] [PubMed] [Google Scholar]
- 9. Middleton A, Simpson KN, Bettger JP, Bowden MG. COVID-19 pandemic and beyond: considerations and costs of telehealth exercise programs for older adults with functional impairments living at home—lessons learned from a pilot case study. Phys Ther. 2020;100:1278–1288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. California Department of Public Health . Order of the State Public Health Officer. 2020. Accessed September 29, 2020. https://www.cdph.ca.gov/Programs/CID/DCDC/CDPH Document Library/COVID- 19/Health Order 3.19.2020.pdf .
- 11. City and County of San Francisco Department of Public Health . Order of the Health Officer No. C19-07. San Francisco, CA, USA: City and County of San Francisco Department of Public Health; 2020. Accessed September 29, 2020. https://oewd.org/sites/default/files/Documents/2020.03.16 Final Order C19-07 - Shelter in Place.pdf.
- 12. Centers for Medicare & Medicaid Services . COVID-19 Emergency Declaration Blanket Waivers for Health Care Providers. Baltimore, MD, USA: Centers for Medicare & Medicaid Services; 2020. Accessed September 29, 2020. https://www.cms.gov/files/document/summary-covid-19-emergency-declaration-waivers.pdf.
- 13. Stetler CB, Legro MW, Wallace CM, et al. The role of formative evaluation in implementation research and the QUERI experience. J Gen Intern Med. 2006;2:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Published online August 7, 2009. Implement Sci. doi: 10.1186/1748-5908-4-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Glasgow RE, Harden SM, Gaglio B, et al. RE-AIM planning and evaluation framework: adapting to new science and practice with a 20-year review. Published online March 29, 2019. Front Public Health. doi: 10.3389/fpubh.2019.00064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Harden SM, Smith ML, Ory MG, Smith-Ray RL, Estabrooks PA, Glasgow RE. RE-AIM in clinical, community, and corporate settings: perspectives, strategies, and recommendations to enhance public health impact. Published online March 22, 2018. Front Public Health. doi: 10.3389/fpubh.2018.00071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Powell BJ, Waltz TJ, Chinman MJ, et al. A refined compilation of implementation strategies: results from the expert recommendations for implementing change (ERIC) project. Published online February 12, 2015. Implement Sci. doi: 10.1186/s13012-015-0209-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Proctor E, Silmere H, Raghavan R, et al. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Heal Ment Heal Serv Res. 2011;38:65–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. City and County of San Francisco Department of Public Health . Order of the Health Officer No. C19-07d. San Francisco, CA, USA: City and County of San Francisco Department of Public Health; 2020. Accessed September 29, 2020. https://sfbos.org/sites/default/files/20200517_FINAL_signed_Health_Officer_Order_C19-07d_Shelter_in_Place.pdf.
- 20. Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–1139. [DOI] [PubMed] [Google Scholar]
- 21. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Holtrop JS, Rabin BA, Glasgow RE. Qualitative approaches to use of the RE-AIM framework: rationale and methods. BMC Health Serv Res. 2018;18:177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Guest G, MacQueen K, Namey E. Applied Thematic Analysis. Thousand Oaks, CA, USA: SAGE Publications, Inc.; 2012. [Google Scholar]
- 24. CDC COVID-19 Response Team . Preliminary estimates of the prevalence of selected underlying health conditions among patients with coronavirus disease 2019—United States, February 12–March 28, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:382–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. McDonnell ME. Telemedicine in complex diabetes management. Curr Diab Rep. 2018;18:42. [DOI] [PubMed] [Google Scholar]
- 26. Yamin CK, Emani S, Williams DH, et al. The digital divide in adoption and use of a personal health record. Arch Intern Med. 2011;171:568–574. [DOI] [PubMed] [Google Scholar]
- 27. Kakkar A, Jacobson BC. Failure of an internet-based health care intervention for colonoscopy preparation: a caveat for investigators. JAMA Intern Med. 2013;173:1374–1376. [DOI] [PubMed] [Google Scholar]
- 28. Nelson MJ, Crossley KM, Bourke MG, Russell TG. Telerehabilitation feasibility in total joint replacement. Int J Telerehabilitation. 2017;9:31–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Nilsen P. Making sense of implementation theories, models and frameworks. Published online April 21, 2015. Implement Sci. doi: 10.1186/s13012-015-0242-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Cane J, O’Connor D, Michie S. Validation of the theoretical framework. Published online April 24, 2012. Implement Sci. doi: 10.1186/1748-5908-7-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. May C, Finch T. Implementing, embedding, and integrating practices: an outline of normalization process theory. Soc Forces. 2009;43:535–554. [Google Scholar]


