Abstract
Patients with schizophrenia (SCZ) represent a vulnerable population who have been understudied in COVID-19 research. We aimed to establish whether health outcomes and care differed between patients with SCZ and patients without a diagnosis of severe mental illness. We conducted a population-based cohort study of all patients with identified COVID-19 and respiratory symptoms who were hospitalized in France between February and June 2020. Cases were patients who had a diagnosis of SCZ. Controls were patients who did not have a diagnosis of severe mental illness. The outcomes were in-hospital mortality and intensive care unit (ICU) admission. A total of 50 750 patients were included, of whom 823 were SCZ patients (1.6%). The SCZ patients had an increased in-hospital mortality (25.6% vs 21.7%; adjusted OR 1.30 [95% CI, 1.08–1.56], P = .0093) and a decreased ICU admission rate (23.7% vs 28.4%; adjusted OR, 0.75 [95% CI, 0.62–0.91], P = .0062) compared with controls. Significant interactions between SCZ and age for mortality and ICU admission were observed (P = .0006 and P < .0001). SCZ patients between 65 and 80 years had a significantly higher risk of death than controls of the same age (+7.89%). SCZ patients younger than 55 years had more ICU admissions (+13.93%) and SCZ patients between 65 and 80 years and older than 80 years had less ICU admissions than controls of the same age (−15.44% and −5.93%, respectively). Our findings report the existence of disparities in health and health care between SCZ patients and patients without a diagnosis of severe mental illness. These disparities differed according to the age and clinical profile of SCZ patients, suggesting the importance of personalized COVID-19 clinical management and health care strategies before, during, and after hospitalization for reducing health disparities in this vulnerable population.
Keywords: COVID-19, schizophrenia, real-life data, health services research, psychiatry, public health
Introduction
By July 2020, approximately 30 000 French individuals had died from the SARS-CoV-2/coronavirus disease 2019 (COVID-19) infection, placing France in the absolute fifth place in the world behind the United States (130 000), Brazil (60 000), the United Kingdom (43 000), and Italy (34 000). The speed of the pandemic expansion and the risk of saturation of intensive care units (ICUs) led the French government to pronounce confinement for 2 months between mid-March and mid-May 2020. During this period, several regions were particularly affected by saturation of ICUs, such as the Paris Ile-de-France area and the northeast. This saturation may have led some services to “sort” patients, choosing those who were admitted to ICUs while being aware that patients admitted with respiratory failure could not be released from their respirators for several weeks. Learning the lessons of this first wave is crucial in anticipating another potential health crisis.
Schizophrenia (SCZ) patients are a population at particular risk of poor outcomes in COVID-19 infection. A recent Korean study has found SCZ to be associated with an increased risk of severe COVID-19 infection.1 SCZ individuals have multiple comorbidities that have been identified as risk factors for severe COVID-191: diabetes, hypertension, chronic obstructive respiratory disease, and end-stage renal disease. Previous studies have also shown reduced access to critical care for SCZ patients.2,3 More information is thus needed to determine whether COVID-19 patients with SCZ have the same health outcomes and care delivered as patients without a diagnosis of severe mental illness.
We aimed to establish whether health outcomes and care differed between patients with SCZ and patients without a diagnosis of severe mental illness. The primary objective was to compare in-hospital mortality between SCZ patients and patients without a diagnosis of severe mental illness after adjustment for main confounding factors (ie, sociodemographic data, clinical data at baseline, stay data, management data, hospital data, and geographical areas of hospitalization). The secondary objective was to compare ICU admissions between SCZ patients and patients without a diagnosis of severe mental illness.
Methods
Study Design and Data Sources
In this population-based cohort study, we used data from Programme de Médicalisation des Systèmes d’Information (PMSI database), the French national hospital database in which administrative and medical data are systematically collected for acute and psychiatric care. The PMSI database is based on diagnosis-related groups, with all diagnoses coded according to the 10th revision of the International Classification of Diseases (ICD-10) and procedural codes from the Classification Commune des Actes Médicaux (CCAM). In our study, we included all hospitalized patients between February 1, 2020, and June 9, 2020, aged 15 years or older with identified COVID-19 (ICD-10 codes: U07.10 or U07.12 or U07.14) and respiratory symptoms (ICD-10 = U07.10 or U07.11) and a length of hospital stay > 24 h (in order not to take into account pauci- or asymptomatic COVID-19 forms that did not actually require hospitalization) except if the patients died within 24 h. We excluded patients with a severe mental illness diagnosis other than SCZ: bipolar disorder or recurrent major depression (ICD-10 codes = F30* or F31* or F33*).
The PMSI database is used to determine financial resources and is frequently and thoroughly verified by both its producer and the paying party, with possible financial and legal consequences.4 Data from the PMSI database are anonymized and can be reused for research purposes.2,5 Due to its suitable accuracy and exhaustive data collection, no patients were lost to follow-up during the study period.
Procedures
We defined 2 populations. Cases were patients who had a diagnosis of SCZ according to specific ICD-10 codes (ie, F20*, F22*, or F25*) in either the acute care or psychiatric PMSI database. Controls were patients who did not have a diagnosis of severe mental illness according to specific ICD-10 codes in the acute care PMSI database and who were not listed in the PMSI psychiatry database.
The primary outcome was in-hospital mortality. The secondary outcome was ICU admission. We gathered patients’ sociodemographic data (age classes: <55, 55–65, 65–80, and >80 years; sex; social deprivation: favored/deprived6), clinical data at baseline (smoking status: yes/no; overweight and obesity: yes/no; Charlson Comorbidity Index score7 and main comorbidities: yes/no), stay data (origin of patients: from home or from hospital-institution; length of ICU and hospital stay), management data (Simplified Acute Physiology Score II (SAPS II) for ICU stay; recourse to mechanical ventilation: yes/no; recourse to renal replacement therapy: yes/no), hospital data (hospital category: public, university, or private; number of hospital stays for COVID-19), and geographical areas of hospitalization (4 areas grouped according to pandemic exposure from the highest to the lowest: Ile-de-France, northeast, southeast, and west, data from Sante Publique France: supplementary figure S1).
Statistical Analysis
Continuous variables are expressed as medians and interquartile ranges. Categorical variables are summarized as counts and percentages. No imputation was made for missing data.
The 2 outcomes were assessed with unadjusted (model 1) and multivariable (models 2 and 3) models. Univariable and multivariable generalized linear models with random effects and correlation matrices (to take into account the clustered effect of the hospitals) were used to estimate the association between SCZ and the 2 outcomes.
Model 2 incorporated sociodemographic data (ie, age, sex, social deprivation), clinical data at baseline (ie, smoking status, overweight and obesity, Charlson Comorbidity Index), stay data (ie, origin of the patient), hospital data (ie, hospital category, number of hospital stays for COVID-19), and geographical areas of hospitalization (ie, Ile-de-France, northeast, southeast, and west).
Model 3 incorporated model 2 plus 2 interaction terms, SCZ × age and SCZ × geographical areas of hospitalization, to check whether the association between SCZ and the 2 outcomes was homogenous across ages and geographical areas of hospitalization according to pandemic exposure. The 2 interactions were determined based on a previous work reporting the influence of age and overcrowding on the COVID-19 prognosis.8 In addition to aggregate analysis, we conducted stratified analyses when an interaction was statistically significant.
A significance threshold of P < .05 was used. All analyses were performed in SAS (version 9.4).
Results
Characteristics of the Patients
During the study period, 50 750 patients were included in the analysis (median age, 71 years [interquartile range, 57–83]; 43.2% female), with 823 SCZ patients (1.6%) and 49 927 non-SCZ patients (figure 1, table 1). SCZ patients were more likely to be female (51.2% vs 43.1%, P = .0005), to be younger (predominance of age between 65 and 80 years vs >80 years in controls), to be tobacco smokers (10.1% vs 4.2%, P < .0001), to be institutionalized (19.1% vs 9.7%, P < .0001), to have dementia (25.2% vs 9.6%, P < .0001), to be hospitalized in University hospitals (40.8% vs 33.1%, P < .0001), and to have a longer length of hospital stay (median [interquartile range], 11 [6–20] vs 9 [5–16], P < .0001) than controls. SCZ patients were less likely to have invasive care (ie, invasive mechanical ventilation: 10.7% vs 13.4%, P = .0443 and renal replacement therapy: 2.1% vs 3.6%, P = .0387) than controls.
Fig. 1.
Flow chart.
Table 1.
Baseline Characteristics and Health Outcomes of Hospitalized COVID-19 Patients With Schizophrenia and Without a Diagnosis of Severe Mental Illness (n = 50 750)
| Total | SCZ Patients | Controls | ||
|---|---|---|---|---|
| n = 50 750 | n = 823 | n = 49 927 | ||
| Characteristics | n (%) | n (%) | n (%) | P value |
| Sociodemographic data | ||||
| Age | <.0001 | |||
| <55 years | 10 538 (20.8) | 130 (15.8) | 10 408 (20.9) | |
| 55–65 years | 8582 (16.9) | 134 (16.3) | 8448 (16.9) | |
| 65–80 years | 15 517 (30.6) | 340 (41.3) | 15 177 (30.4) | |
| ≥80 years | 16 113 (31.7) | 219 (26.6) | 15 894 (31.8) | |
| Sex | ||||
| Male | 28 818 (56.8) | 402 (48.8) | 28 416 (56.9) | .0005 |
| Female | 21 932 (43.2) | 421 (51.2) | 21 511 (43.1) | |
| Social deprivation index | ||||
| More favored | 24 681 (48.6) | 442 (53.7) | 24 239 (48.6) | .1340 |
| More deprived | 24 126 (47.6) | 351 (42.7) | 23 775 (47.6) | |
| Missing | 1943 (3.8) | 30 (3.6) | 1913 (3.8) | |
| Clinical data at baseline | ||||
| Smoker | 2175 (4.3) | 83 (10.1) | 2092 (4.2) | <.0001 |
| Weighta | ||||
| Overweight and obesity | 7201 (14.2) | 138 (16.8) | 7063 (14.2) | .0576 |
| Comorbidities | ||||
| Charlson Comorbidity Index score | .0006 | |||
| 0 | 20 865 (41.1) | 287 (34.9) | 20 578 (41.2) | |
| 1–2 | 17 520 (34.5) | 343 (41.7) | 17 177 (34.4) | |
| ≥3 | 12 365 (24.4) | 193 (23.4) | 12 172 (24.3) | |
| Renal disease | 6125 (12.1) | 102 (12.4) | 6023 (14.1) | .7687 |
| Peripheral vascular disease | 2879 (5.7) | 41 (5.0) | 2838 (5.7) | .4534 |
| Hemiplegia or paraplegia | 2111 (4.2) | 40 (4.9) | 2151 (4.2) | .3558 |
| Cancer | 4482 (8.8) | 51 (6.2) | 4431 (8.9) | .0189 |
| HIV or AIDS | 304 (0.6) | 5 (0.6) | 299 (0.6) | .8935 |
| Diabetes with complications | 3112 (6.1) | 54 (6.6) | 3058 (6.1) | .6975 |
| Diabetes without complications | 10 999 (21.7) | 154 (18.7) | 10 845 (21.7) | .0584 |
| Dementia | 4983 (9.8) | 207 (25.2) | 4776 (9.6) | <.0001 |
| Cerebrovascular disease | 3191 (6.3) | 63 (7.7) | 3128 (6.3) | .1324 |
| Chronic obstructive pulmonary disease | 6425 (12.7) | 122 (14.8) | 6303 (12.6) | .0729 |
| Congestive heart failure | 8178 (16.1) | 110 (13.4) | 8068 (16.2) | .0646 |
| Myocardial infarct | 3740 (7.4) | 38 (4.6) | 3702 (7.4) | .0129 |
| Stay data | ||||
| Origin of the patient | ||||
| From home | 45 769 (90.2) | 666 (80.9) | 45 103 (90.3) | <.0001 |
| Other (hospital–institution) | 4981 (9.8) | 157 (19.1) | 4824 (9.7) | |
| Length of hospital stay, median (IQR)—number of days | 9 (5–16) | 11 (6–20) | 9 (5–16) | <.0001 |
| Length of ICU stay, median (IQR)—number of days | 9 (4–18) | 10 (4–18) | 9 (4–18) | .6695 |
| Management data | ||||
| SAPS II score at ICU admission, median (IQR) | 32.0 (22.0–45.0) | 31.0 (21.0–46.0) | 32.0 (22.0–45.0) | .3799 |
| Recourse to invasive mechanical ventilation | 6791 (13.4) | 88 (10.7) | 6703 (13.4) | .0443 |
| Recourse to continuous renal-replacement therapy | 1787 (3.5) | 17 (2.1) | 1770 (3.6) | .0387 |
| Hospital data | ||||
| Hospital category | .0001 | |||
| Public | 29 837 (58.8) | 448 (54.4) | 29 389 (58.9) | |
| University | 16 860 (33.2) | 336 (40.8) | 16 524 (33.1) | |
| Private | 4053 (8.0) | 39 (4.8) | 4014 (8.0) | |
| Geographical exposureb | .0251 | |||
| Ile-de-France | 18 770 (37.0) | 355 (43.1) | 18 415 (36.9) | |
| Northeast | 16 314 (32.2) | 225 (27.3) | 16 089 (32.2) | |
| Southeast | 8381 (16.5) | 134 (16.3) | 8247 (16.5) | |
| West | 7285 (14.4) | 109 (13.2) | 7176 (14.4) | |
| Outcomes | ||||
| In-hospital mortality | 11 065 (21.8) | 211 (25.6) | 10 854 (21.7) | .0188 |
| ICU admission | 14 351 (28.2) | 195 (23.7) | 14 156 (28.4) | .0113 |
Note: Comorbidities were based on the 10th revision of the International Statistical Classification of Diseases from the Programme de Medicalisation des Systèmes d’Information (PMSI)—French medico-administrative database based on diagnosis-related groups. P value in bold denotes statistical significance. N, effective; ICU, intensive care unit; IQR, interquartile range; SAPS II score, Simplified Acute Physiology Score II; SCZ, schizophrenia.
aIf the body mass index (BMI) is 18.5 to <25: normal weight; if the BMI is 25.0 to <30: overweight; and if the BMI is 30.0 or higher: obesity.
bGeographical exposure: 4 areas were identified with different pandemic exposure from the lowest to the highest: west, southeast, northeast, and Ile-de-France.
In-Hospital Mortality
The overall in-hospital mortality was 21.8%. The univariable analysis is presented in supplementary table S1. SCZ patients had an increased mortality compared to controls (25.6% vs 21.7%; P = .0188) (table 1), confirmed by the multivariable analysis (adjusted OR, 1.30 [95% CI, 1.08–1.56]; P = .0093) (table 2). There was a significant interaction between SCZ and age (P = .0006), with significantly increased mortality only for SCZ patients between 65 and 80 years (adjusted OR, 1.62 [95% CI, 1.27–2.06]; P = .0002). The characteristics of SCZ patients and controls according to age classes are presented in table 3. The difference in in-hospital mortality between SCZ and controls varied with age as follows: <55 years: +3.65%; 55–65 years: +4.64%; 65–80 years: +7.89%; and >80 years: −3.17% (figure 2). There was no heterogeneity in the interaction between SCZ and geographical areas of hospitalization (P = .0797).
Table 2.
Associations Between Schizophrenia, In-Hospital Mortality, and ICU Admission (n = 50 750)
| In-Hospital Mortality | ICU Admission | |||
|---|---|---|---|---|
| OR (95% CI) | P value | OR (95% CI) | P value | |
| Model 1 | 1.246 (1.045–1.485) | .0186 | 0.782 (0.653–0.937) | .0118 |
| Model 2 | 1.298 (1.080–1.561) | .0093 | 0.749 (0.619–0.906) | .0062 |
| Model 3 | ||||
| Interaction term, age × SCZ | .0006* | <.0001* | ||
| <55 years | 1.761 (0.912–3.401) | .0905 | 1.582 (1.087–2.299) | .0177 |
| 55–65 years | 1.577 (0.969–2.571) | .0661 | 0.919 (0.630–1.340) | .6561 |
| 65–80 years | 1.621 (1.276–2.062) | .0002 | 0.533 (0.405–0.702) | <.001 |
| ≥80 years | 0.873 (0.657–1.161) | .3429 | 0.509 (0.294–0.880) | .0168 |
| Interaction term, geographical areas of hospitalization × SCZ | .0797* | .0591* | ||
Note: Model 1: unadjusted model. Model 2: adjustment for sociodemographic data (age, sex, social deprivation), clinical data at baseline (smoking status, overweight and obesity, Charlson Comorbidity Index), stay data (origin of the patient), hospital data (hospital category, number of hospital stays for COVID-19), and geographical areas of hospitalization. Model 3: model 2 plus the interaction term age × SCZ. There was no heterogeneity in the interaction between SCZ and geographical areas of hospitalization. P value in bold denotes statistical significance. Reference: controls. ICU, intensive care unit; SCZ, schizophrenia.
*P value for interaction.
Table 3.
Baseline Characteristics of Hospitalized COVID-19 Patients With Schizophrenia and Without a Diagnosis of Severe Mental Illness by Age Classes (n = 50 750)
| Age Classes | <55 years | 55–65 years | 65–80 years | ≥80 years | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SCZ | Controls | SCZ | Controls | SCZ | Controls | SCZ | Controls | |||||
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |||||
| Characteristics | n = 130 | n = 10 408 | P value | n = 134 | n = 8448 | P value | n = 340 | n = 15 177 | P value | n = 219 | n = 15 894 | P value |
| Sociodemographic data | ||||||||||||
| Sex | .1766 | .0327 | .0002 | .0041 | ||||||||
| Male | 82 (63.1) | 5910 (56.8) | 73 (54.5) | 5458 (64.6) | 168 (49.4) | 9701 (63.9) | 75 (34.3) | 7347 (46.2) | ||||
| Female | 48 (36.9) | 4498 (43.2) | 61 (45.5) | 2990 (35.4) | 172 (50.6) | 5476 (36.1) | 144 (65.7) | 8547 (53.8) | ||||
| Social deprivation index | .8309 | .2608 | .2553 | .3974 | ||||||||
| More favored | 66 (50.8) | 5222 (50.2) | 74 (55.2) | 4123 (48.8) | 177 (52.0) | 7047 (46.4) | 125 (57.1) | 7847 (49.4) | ||||
| More deprived | 60 (46.2) | 4754 (45.7) | 61 (45.6) | 3968 (47.0) | 146 (43.0) | 7550 (50.0) | 88 (40.2) | 7503 (47.2) | ||||
| Missing | 4 (3.0) | 432 (4.1) | 3 (2.2) | 357 (4.2) | 17 (5.0) | 580 (3.6) | 6 (2.7) | 544 (3.4) | ||||
| Clinical data at baseline | ||||||||||||
| Smoker | 27 (20.8) | 376 (3.6) | <.0001 | 20 (14.9) | 496 (5.9) | .0013 | 6 (1.8) | 640 (4.2) | .0231 | 5 (2.3) | 325 (2.0) | .7926 |
| Weighta | .0018 | .7467 | .6550 | .0896 | ||||||||
| Overweight and obesity | 47 (36.2) | 2228 (21.4) | 25 (18.7) | 1673 (19.8) | 48 (14.1) | 2290 (15.1) | 18 (8.2) | 872 (5.5) | ||||
| Comorbidities | ||||||||||||
| Charlson Comorbidity Index score | .0043 | .0849 | .0465 | .2040 | ||||||||
| 0 | 69 (53.1) | 7071 (67.9) | 56 (41.8) | 4269 (50.5) | 119 (35.0) | 5265 (34.7) | 43 (19.6) | 3973 (25.0) | ||||
| 1–2 | 49 (37.7) | 2507 (24.1) | 55 (41.0) | 2686 (31.8) | 142 (41.8) | 5512 (36.3) | 97(44.3) | 6472 (40.7) | ||||
| ≥3 | 12 (9.2) | 830 (8.0) | 23 (17.2) | 1493 (17.7) | 79 (23.2) | 4400 (29.0) | 79 (36.1) | 5449 (34.3) | ||||
| Renal disease | 4 (3.1) | 374 (3.6) | .7586 | 11 (8.2) | 553 (6.6) | .4569 | 33 (9.7) | 1897 (12.5) | .1265 | 54 (24.7) | 3199 (20.1) | .1202 |
| Peripheral vascular disease | 1 (0.8) | 100 (1.0) | .8285 | 3 (2.2) | 299 (3.5) | .4389 | 22 (6.5) | 1139 (7.5) | .5214 | 15 (6.9) | 1300 (8.2) | .5201 |
| Hemiplegia or paraplegia | 5 (3.9) | 262 (2.5) | .3623 | 10 (7.5) | 352 (4.2) | .0907 | 16 (4.7) | 811 (5.3) | .6597 | 9 (4.1) | 686 (4.3) | .8862 |
| Cancer | 5 (3.9) | 305 (2.9) | .5542 | 8 (6.0) | 658 (7.8) | .4516 | 23 (6.8) | 681 (4.5) | .0098 | 15 (6.9) | 1623 (10.2) | .1110 |
| HIV or AIDS | 1 (0.8) | 126 (1.2) | .6617 | 2 (1.5) | 111 (1.3) | .8606 | 2 (0.6) | 58 (0.4) | .6986 | 0 (0.0) | 4 (0.0) | |
| Diabetes with complications | 4 (3.1) | 201 (1.9) | .3680 | 10 (7.5) | 449 (5.3) | .2970 | 27 (7.9) | 1338 (8.8) | .4361 | 13 (5.9) | 1070 (6.7) | .6127 |
| Diabetes without complications | 19 (14.6) | 1267 (12.2) | .4156 | 20 (14.9) | 1898 (22.5) | .0620 | 78 (22.9) | 4285 (28.2) | .0476 | 37 (16.9) | 3395 (21.4) | .1530 |
| Dementia | 3 (2.3) | 16 (0.2) | .0051 | 7 (5.2) | 77 (0.9) | .0017 | 78 (22.9) | 829 (5.5) | <.0001 | 119 (54.3) | 3854 (24.3) | <.0001 |
| Cerebrovascular disease | 2 (1.5) | 150 (1.4) | .9283 | 5 (3.7) | 343 (4.1) | .8514 | 34 (10.0) | 1024 (6.8) | .0403 | 22 (10.1) | 1611 (10.1) | .9169 |
| Chronic obstructive pulmonary disease | 27 (20.8) | 933 (9.0) | .0008 | 24 (17.9) | 931 (11.0) | .0288 | 53 (15.6) | 2382 (15.7) | .9839 | 18 (8.2) | 2057 (12.9) | .0628 |
| Congestive heart failure | 8 (6.2) | 281 (2.7) | .0400 | 11 (8.2) | 636 (7.5) | .7724 | 43 (12.7) | 2462 (16.22) | .1155 | 48 (21.9) | 4689 (29.50) | .0350 |
| Myocardial infarct | 5 (3.9) | 130 (1.3) | .0304 | 4 (3.0) | 425 (5.0) | .3079 | 11 (3.2) | 1410 (9.3) | .0036 | 18 (8.2) | 1737 (10.9) | .2605 |
| Stay data | ||||||||||||
| Origin of the patient | .0260 | .0062 | .0002 | .0002 | ||||||||
| From home | 117 (90.0) | 9894 (95.1) | 115 (85.8) | 7890 (93.4) | 277 (81.5) | 13 746 (90.6) | 157 (71.7) | 13 573 (85.4) | ||||
| Other (hospital-institution) | 13 (10.0) | 514 (4.9) | 19 (14.2) | 558 (6.6) | 63 (18.5) | 1431 (9.4) | 62 (28.3) | 2321 (14.6) | ||||
| Length of hospital stay, median (IQR)—number of days | 10.0 (5.0– 16.0) | 6.0 (3.0– 11.0) | .0006 | 12.0 (7.0– 15.0) | 9.0 (5.0– 16.0) | <.0001 | 10.5 (6.0– 19.0) | 11.0 (6.0– 18.0) | .0611 | 11.0 (5.0– 20.0) | 10.0 (5.0– 17.0) | .0021 |
| Length of ICU stay, median (IQR)—number of days | 7.0 (4.0– 17.0) | 7.0 (3.0– 16.0) | .7034 | 14.0 (9.0– 20.0) | 9.0 (4.0– 19.0) | .1016 | 8.0 (3.0– 15.0) | 10.0 (5.0– 20.0) | 0.1302 | 12.0 (9.0– 17.0) | 6.0 (2.0–11.0) | .0004 |
| Management data | ||||||||||||
| SAPS II score at ICU admission, median (IQR) | 27.5 (19.0– 40.5) | 24.0 (15.0– 36.0) | .3940 | 34.5 (23.0– 44.5) | 31.0 (22.0– 43.0) | .9193 | 32.0 (22.0– 50.0) | 37.0 (27.0– 50.0) | .0590 | 28.0 (0.0– 51.0) | 32.0 (0.0– 42.0) | .8248 |
| Recourse to invasive mechanical ventilation | 27 (20.8) | 1416 (13.6) | .0376 | 28 (20.9) | 1801 (21.3) | .9075 | 30 (8.8) | 3122 (20.6) | .0003 | 3 (1.4) | 364 (2.3) | .4023 |
| Recourse to continuous renal-replacement therapy | 4 (3.1) | 301 (2.9) | .9024 | 5 (3.7) | 400 (4.7) | .5977 | 5 (1.5) | 836 (5.5) | .0112 | 3 (1.4) | 233 (1.5) | .8879 |
| Hospital data | ||||||||||||
| Hospital category | .2472 | .8862 | .0075 | <.0001 | ||||||||
| Public | 72 (55.3) | 5742 (55.2) | 74 (55.2) | 4773 (56.5) | 199 (58.5) | 8912 (58.7) | 103 (47.0) | 9962 (62.7) | ||||
| University | 53 (40.8) | 3850 (37.0) | 50 (37.3) | 2990 (35.4) | 128 (37.7) | 4957 (32.7) | 105 (48.0) | 4727 (29.7) | ||||
| Private | 5 (3.9) | 816 (7.8) | 10 (7.5) | 685 (8.1) | 13 (3.8) | 1308 (8.6) | 11 (5.0) | 1205 (7.6) | ||||
| Geographical exposureb | .1433 | .9355 | .1529 | .0320 | ||||||||
| Ile-de-France | 57 (43.9) | 4635 (44.5) | 52 (38.8) | 3501 (41.4) | 152 (44.7) | 5119 (33.7) | 94 (42.9) | 5160 (32.5) | ||||
| Northeast | 46 (35.4) | 2763 (26.6) | 41 (30.6) | 2501 (29.6) | 84 (24.7) | 5276 (34.8) | 54 (24.7) | 5549 (34.9) | ||||
| Southeast | 16 (12.3) | 1562 (15.0) | 22 (16.4) | 1284 (15.2) | 59 (17.4) | 2497 (16.5) | 37 (16.9) | 2904 (18.3) | ||||
| West | 11 (8.4) | 1448 (13.9) | 19 (14.2) | 1162 (13.8) | 45 (13.2) | 2285 (15.0) | 34 (15.5) | 2281 (14.3) | ||||
Note: Comorbidities were based on the 10th revision of the International Statistical Classification of Diseases from the Programme de Medicalisation des Systèmes d’Information (PMSI)–French medico-administrative database based on diagnosis-related groups. N, effective; ICU, intensive care unit; IQR, interquartile range; SAPS II score, Simplified Acute Physiology Score II; SCZ, schizophrenia. P value in bold denotes statistical significance.
aIf the body mass index is 18.5 to <25: normal weight; if the BMI is 25.0 to <30: overweight; and if the BMI is 30.0 or higher: obesity.
bGeographical exposure: 4 areas were identified with different pandemic exposure from the lowest to the highest: west, southeast, northeast, and Ile-de-France.
Fig. 2.
In-hospital mortality by age classes. <55 years: P = .0643; ≥55 and <65 years: P = .1083; ≥65 and <80 years: P = .0063; >80 years: P = .3762.
ICU Admission
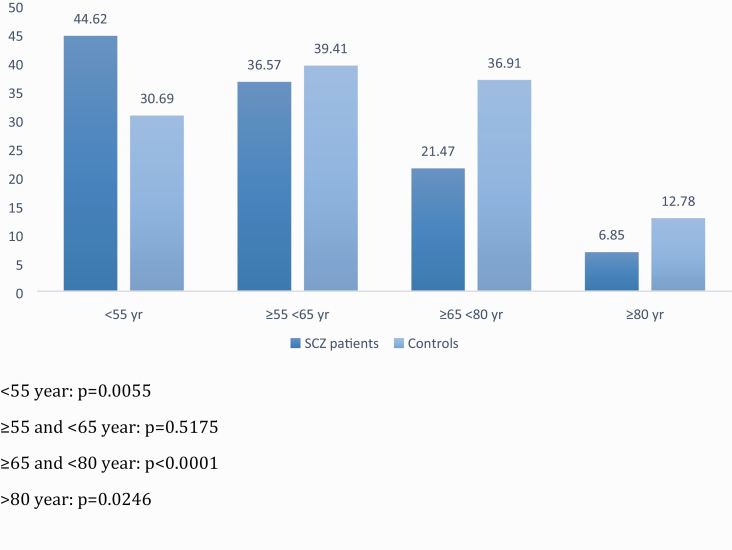
A total of 14 351 patients (28.3%) were admitted to the ICU. The univariable analysis is presented in supplementary table S2. SCZ patients were less frequently admitted to the ICU than controls (23.7% vs 28.4%; P = .0113) (table 1), confirmed by the multivariable analysis (adjusted OR, 0.75 [95% CI, 0.62–0.91]; P = .0062) (table 2). There was a significant interaction between SCZ and age (P < .0001), with more ICU admissions for SCZ patients younger than 55 years (adjusted OR, 1.58 [95% CI, 1.09–2.30]; P = .0177) and less ICU admissions for SCZ patients between 65 and 80 years (adjusted OR, 0.53 [95% CI, 0.41–0.70]; P < .001) and older than 80 years (adjusted OR, 0.51 [95% CI, 0.29–0.88]; P = .0168). The difference in ICU admission between SCZ patients and controls varied with age as follows: <55 years: +13.93%; 55–65 years: −2.84%; 65–80 years: −15.44%; and >80 years: −5.93% (figure 3). There was no heterogeneity in the interaction between SCZ and geographical areas of hospitalization (P = .0591).
Fig. 3.
ICU admission by age classes. <55 years: P = .0055; ≥55 and <65 years: P = .5175; ≥65 and <80 years: P < .0001; >80 years: P = .0246.
Discussion
To our knowledge, we report the largest series of SCZ patients with COVID-19 to date, including 823 SCZ patients hospitalized for COVID-19 infection with a nationwide geographical distribution. In this large population-based cohort study, we reported the existence of disparities in health and health care between hospitalized COVID-19 SCZ patients and patients without a diagnosis of severe mental illness. These disparities differed according to the age and clinical profile of SCZ patients.
SCZ patients under 55 years of age had 14% more ICU admissions than patients without a diagnosis of severe mental illness, suggesting more severe COVID-19 infection in SCZ patients.
SCZ patients under 55 years were mostly male, were more frequently smokers, were more overweight and obese, and had more multiple somatic comorbidities, including chronic obstructive pulmonary disease, than patients without a diagnosis of severe mental illness. Although the results are contradictory, smoking seems more likely to be associated with the negative progression and adverse outcomes of COVID-19.9 Obesity in patients younger than 60 years has been reported as a risk factor for COVID-19 hospital admission and worse outcomes.10 Chronic obstructive pulmonary disease has been also reported to worsen the progression and prognosis of COVID-19.11 A delay in access to hospital care may be evoked to explain the severity of SCZ patients although we do not have any prehospital data. The existence of barriers in access to somatic care for SCZ patients has been described in previous studies.2,10,12,13 Altogether, these findings suggest that young SCZ patients with the risk factors listed above should be targeted as a high-risk population for early intervention.14,15
These discrepancies in severity are apparently compensated by the important increase in ICU admissions that prevented increased mortality in SCZ patients. However, depression, anxiety, post-traumatic stress disorder, and cognitive dysfunction are increasingly recognized among patients who survive an ICU admission and these consequences have a significant impact on the patient’s long-term quality of life.16 Rehabilitation following critical illness has shown its efficacy to improve both physical and nonphysical recovery,17 and SCZ patients should benefit from these programs.
SCZ patients between 65 and 80 years had a higher risk of death (+7.89%), and SCZ patients between 65 and 80 years and over 80 years old had less ICU admissions than patients without a diagnosis of severe mental illness (−15.44% and −5.93%, respectively).
SCZ patients between 65 and 80 years were mostly female, had more dementia, and had more cerebrovascular disease than patients without a diagnosis of severe mental illness. Previous studies have confirmed the relationship between SCZ and dementia risk, especially in women.18,19 The diagnosis of dementia has been reported as an important risk factor for mortality in COVID-19 patients.20,21 Dementia has also been associated with increased aggressive behavior in institutionalized patients who may affect the care of these patients at the hospital.22 In addition, a new environment can lead to increased stress and behavioral problems.23 Delirium caused by hypoxia could complicate the presentation of dementia.24 Dementia as a preexisting condition may in part explain the lower ICU admissions in SCZ patients. All these elements demonstrate the importance of reinforcement of inpatient support for SCZ patients with dementia. To date, psychogeriatric teams remain insufficiently developed while demand in the aging population is growing.
SCZ patients between 65 and 80 years were more frequently referred from hospitals or institutions than patients without a diagnosis of severe mental illness, which can explain the poor health outcomes in SCZ patients. A French study reported that most psychiatric inpatients with a COVID-19 diagnosis were kept in dedicated psychiatric departments and not in general hospitals.25 The division between physical and psychiatric medicine results in confusion about which sector of the health service (ie, primary, mental health, or acute care levels) should take responsibility for the management of patients with complex health needs.10 We lack national data on the rate of elderly SCZ patients who are institutionalized, yet we can reasonably hypothesize that institutionalization is a risk factor for COVID-19 severe infection in elderly patients with SCZ. Our results support a strategy of systematic detection in institutionalized SCZ patients and early intervention in this population. This has already been done in a homeless shelter in Boston where 36% of the residents tested positive.26
The lower ICU admission rate in SCZ patients than in patients without a diagnosis of severe mental illness is a perfect illustration of the debate between utility- and equity-based arguments.27 SCZ patients had one of the poorest prognosis indicators justifying ICU triage. However, this triage based solely on prognosis exacerbates existing health inequities, leaving disadvantaged patients worse off. Factors consistently found in the literature to be associated with a decision to admit or refuse a patient to the ICU are age, severity of illness and functional status at baseline, initial ward or team the patient was referred from, bed availability, and do-not-resuscitate order status/patient preference.28 Although some factors are not modifiable (eg, age, functional status), others can be improved so as not to penalize SCZ patient ICU admission. The first one is to guarantee respect for the SCZ patient’s wishes and values expressed directly by the patient via advance directives or reported by relatives. However, the overrepresentation of institutionalized SCZ patients and dementia patients suggests an autonomy loss and probably increased social isolation of these patients. The absence of relatives may have impacted medical decisions of do-not-resuscitate orders, and a previous study has suggested that patients with severe mental illness may be more prone to ask for do-not-resuscitate orders than those without psychiatric disorders.29 Previous works have reported that implementation of advance directives is difficult in patients with psychiatric disorders.30 Efforts should be undertaken to embed the use of advance directives in routine mental health care.31 Second, the link between the hospital and/or the ICU team and the initial ward or team the patient was referred from needs to be strengthened. A psychiatrist on call must be reachable 24/7 to participate, if necessary, in a collegial decision to not admit the patient to the ICU. Third, as previously noted, the time of access to the hospital is a major issue and must be kept to a minimum as a condition to prevent patients from being admitted with very serious conditions. Finally, mental illness stigma may also play a specific role in the lower ICU admission rate of SCZ patients from nursing homes and psychiatric departments.32 ICUs may be less prone to admit a patient referred by a psychiatric department due to potential behavioral/aggressive disturbances of SCZ patients and the inability to monitor them properly. Some ICU staff report being unprepared to care for patients with severe mental illness.33 ICU staff should be specifically trained for the care of patients with severe mental illness.
Geographical areas of hospitalization did not influence the relationship between SCZ and mortality or ICU admission. We could have expected that access to care and health outcomes would be influenced in SCZ patients according to hospital overcrowding. However, our data may have been insufficiently accurate, and further studies will need to work with more accurate indicators such as bed occupancy rates at the hospital or ICU level.
Limits and Perspectives
The worldwide absolute mortality data suggest that COVID-19 infection may have different impacts across countries due to multiple factors (climate, facility organization, COVID-19 public management strategies). Thus, our results may not be extrapolated to other countries and should be replicated. Some data are known to be insufficiently coded in the medicoadministrative databases (eg, smoking, overweight, and obesity). We have no information on the contamination rate of SCZ patients34 and the delay between the onset of infection and hospitalization. Treatment variables including psychotropics and repurposed or experimental anti-COVID-19 treatments were not available in the PMSI database. Some experimental anti-COVID-19 treatments may have been contraindicated in SCZ patients because of potential interactions with psychotropics.35–38 No biological data are available in the PMSI database and SCZ has been shown to have different immune-inflammatory profiles39 that may also partly explain the observed differences. Further studies should be carried out to explore the influence of these data on the prognosis of COVID-19 in SCZ patients. Finally, we do not know if our results are specific to COVID-19 or if they would be similar in other urgent pathologies. Future studies should explore this issue.
Conclusion
This study reports the existence of disparities in health and health care between hospitalized COVID-19 SCZ patients and patients without a diagnosis of severe mental illness. These disparities differed according to the age and clinical profile of SCZ patients, suggesting the importance of personalized COVID-19 clinical management and health care strategies before, during, and after hospitalization for reducing health disparities in this vulnerable population.
Supplementary Material
Supplementary data are available at Schizophrenia Bulletin.
Figure S1. Geographical areas of hospitalization grouped according to pandemic exposure from the highest to the lowest: Ile-de-France, northeast, southeast and west; data from Sante Publique France. Peak of the epidemic in France: 04/04/2020. https://www.gouvernement.fr/info-coronavirus/carte-et-donnees.
Table S1. Factors associated with in-hospital mortality: Univariate analysis (n = 50 750). *If the body mass index (BMI) is 18.5 to <25: normal weight; if the BMI is 25.0 to <30: overweight; and if the BMI is 30.0 or higher: obesity. **Geographical exposure: 4 areas were identified with different pandemic exposure from the lowest to the highest: west, southeast, northeast and Ile-de-France. N: effective; %: percentage; ICU: intensive care unit; IQR: interquartile range; SAPS II score: Simplified Acute Physiology Score II; SCZ: schizophrenia. Comorbidities were based on the 10th revision of the International Statistical Classification of Diseases from the Programme de Medicalisation des Systèmes d’Information (PMSI)—French medico-administrative database based on diagnosis related-groups (DRG). P-value in bold: statistical significance.
Table S2. Factors associated with ICU admission: Univariate analysis (n = 50 750). *If the body mass index (BMI) is 18.5 to <25: normal weight; if the BMI is 25.0 to <30: overweight; and if the BMI is 30.0 or higher: obesity. **Geographical exposure: 4 areas were identified with different pandemic exposure from the lowest to the highest: west, southeast, northeast and Ile-de-France. N: effective; %: percentage; ICU: intensive care unit; IQR: interquartile range; SAPS II score: Simplified Acute Physiology Score II; SCZ: schizophrenia. Comorbidities were based on the 10th revision of the International Statistical Classification of Diseases from the Programme de Medicalisation des Systèmes d’Information (PMSI) – French medico-administrative database based on diagnosis related-groups (DRG). P-value in bold: statistical significance.
Funding
This work was funded by Assistance Publique–Hôpitaux Marseille (APHM)–Aix-Marseille University (AMU) and the PHRC National, Direction générale de l’offre de soins (DGOS), France.
Acknowledgments
David Braunstein, Myriam Dubuc, Cyprien Fabre, Marie-Thérèse Jimeno, Vincent Pradel, Anne Remacle, Fanny Romain, Catherine Seyler, Françoise Volot, and all the other members of the Department of Medical Information. We declare no competing interests.
Author Contributions
V.O. and V.P. had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Concept and design: L.B., G.F. Acquisition, analysis, or interpretation of data: P.A., K.B., L.B., C.L., P.-M.L., A.L., G.F., M.L., V.P., V.O. Drafting of the manuscript: L.B., G.F. Critical revision of the manuscript for important intellectual content: all the authors. Statistical analysis: V.P. Administrative, technical, or material support: V.O. Supervision: L.B.
References
- 1. Ji W, Huh K, Kang M, et al. Effect of underlying comorbidities on the infection and severity of COVID-19 in Korea: a Nationwide Case–Control Study. J Korean Med Sci. 2020;35(25):e237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Fond G, Salas S, Pauly V, et al. End-of-life care among the patients with schizophrenia and cancer: a population-based cohort study from the French national hospital database. Lancet Public Health. 2019;4(11):e583–e591. [DOI] [PubMed] [Google Scholar]
- 3. Melamed OC, Hahn MK, Agarwal SM, Taylor VH, Mulsant BH, Selby P. Physical health among people with serious mental illness in the face of COVID-19: concerns and mitigation strategies. Gen Hosp Psychiatry. 2020;66:30–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Boudemaghe T, Belhadj I. Data Resource Profile: The French National Uniform Hospital Discharge Data Set Database (PMSI). Int J Epidemiol. 2017;46(2):392–392d. [DOI] [PubMed] [Google Scholar]
- 5. Revon-Rivière G, Pauly V, Baumstarck K, et al. High-intensity end-of-life care among children, adolescents, and young adults with cancer who die in the hospital: a population-based study from the French national hospital database. Cancer. 2019;125(13):2300–2308. [DOI] [PubMed] [Google Scholar]
- 6. Rey G, Jougla E, Fouillet A, Hémon D. Ecological association between a deprivation index and mortality in France over the period 1997–2001: variations with spatial scale, degree of urbanicity, age, gender and cause of death. BMC Public Health. 2009;9:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bannay A, Chaignot C, Blotière PO, et al. The best use of the Charlson Comorbidity Index with electronic health care database to predict mortality. Med Care. 2016;54(2):188–194. [DOI] [PubMed] [Google Scholar]
- 8. Banerjee A, Pasea L, Harris S, et al. Estimating excess 1-year mortality associated with the COVID-19 pandemic according to underlying conditions and age: a population-based cohort study. Lancet. 2020;395(10238):1715–1725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Vardavas CI, Nikitara K. COVID-19 and smoking: a systematic review of the evidence. Tob Induc Dis. 2020;18:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Sheridan AJ. Palliative care for people with serious mental illnesses. Lancet Public Health. 2019;4(11):e545–e546. [DOI] [PubMed] [Google Scholar]
- 11. Zhao Q, Meng M, Kumar R, et al. The impact of COPD and smoking history on the severity of COVID-19: a systemic review and meta-analysis [published online ahead of print April 15, 2020]. J Med Virol. doi: 10.1002/jmv.25889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Fond G, Boyer L, Andrianarisoa M, et al. Self-reported pain in patients with schizophrenia. Results from the national first-step FACE-SZ cohort. Prog Neuropsychopharmacol Biol Psychiatry. 2018;85:62–68. [DOI] [PubMed] [Google Scholar]
- 13. Irwin KE, Henderson DC, Knight HP, Pirl WF. Cancer care for individuals with schizophrenia. Cancer. 2014;120(3):323–334. [DOI] [PubMed] [Google Scholar]
- 14. Sun Q, Qiu H, Huang M, Yang Y. Lower mortality of COVID-19 by early recognition and intervention: experience from Jiangsu Province. Ann Intensive Care. 2020;10(1):33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Goyal DK, Mansab F, Iqbal A, Bhatti S. Early intervention likely improves mortality in COVID-19 infection. Clin Med (Lond). 2020;20(3):248–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Needham DM, Davidson J, Cohen H, et al. Improving long-term outcomes after discharge from intensive care unit: report from a stakeholders’ conference. Crit Care Med. 2012;40(2):502–509. [DOI] [PubMed] [Google Scholar]
- 17. Kalfon P, Alessandrini M, Boucekine M, et al. Tailored multicomponent program for discomfort reduction in critically ill patients may decrease post-traumatic stress disorder in general ICU survivors at 1 year. Intensive Care Med. 2019;45(2):223–235. [DOI] [PubMed] [Google Scholar]
- 18. Harvey PD, Silverman JM, Mohs RC, et al. Cognitive decline in late-life schizophrenia: a longitudinal study of geriatric chronically hospitalized patients. Biol Psychiatry. 1999;45(1):32–40. [DOI] [PubMed] [Google Scholar]
- 19. Cai L, Huang J. Schizophrenia and risk of dementia: a meta-analysis study. Neuropsychiatr Dis Treat. 2018;14:2047–2055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hwang J, Kim J-H, Park J-S, Chang MC, Park D. Neurological diseases as mortality predictive factors for patients with COVID-19: a retrospective cohort study. Neurol Sci. 2020;41:2317–2324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bianchetti A, Rozzini R, Guerini F, et al. Clinical presentation of COVID19 in dementia patients. J Nutr Health Aging. 2020;24(6):560–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Cen X, Li Y, Hasselberg M, Caprio T, Conwell Y, Temkin-Greener H. Aggressive behaviors among nursing home residents: association with dementia and behavioral health disorders. J Am Med Dir Assoc. 2018;19(12):1104–1109.e4. [DOI] [PubMed] [Google Scholar]
- 23. Kales HC, Lyketsos CG, Miller EM, Ballard C. Management of behavioral and psychological symptoms in people with Alzheimer’s disease: an international Delphi consensus. Int Psychogeriatr. 2019;31(1):83–90. [DOI] [PubMed] [Google Scholar]
- 24. Marcantonio ER. Delirium in hospitalized older adults. N Engl J Med. 2017;377(15):1456–1466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Bocher R, Jansen C, Gayet P, Gorwood P, Laprévote V. [Responsiveness and sustainability of psychiatric care in France during COVID-19 epidemic]. Encephale. 2020;46(3S):S81–S84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Baggett TP, Keyes H, Sporn N, Gaeta JM. Prevalence of SARS-CoV-2 infection in residents of a large homeless Shelter in Boston. JAMA. 2020;323(21):2191–2192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ballantyne A, Rogers WA, Entwistle V, Towns C. Revisiting the equity debate in COVID-19: ICU is no panacea. J Med Ethics. 2020;46(10):641–645. [DOI] [PubMed] [Google Scholar]
- 28. James FR, Power N, Laha S. Decision-making in intensive care medicine – a review. J Intensive Care Soc. 2018;19(3):247–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ruijs CDM, Kerkhof AJFM, van der Wal G, Onwuteaka-Philipsen BD. Depression and explicit requests for euthanasia in end-of-life cancer patients in primary care in the Netherlands: a longitudinal, prospective study. Fam Pract. 2011;28(4):393–399. [DOI] [PubMed] [Google Scholar]
- 30. Zelle H, Kemp K, Bonnie RJ. Advance directives in mental health care: evidence, challenges and promise. World Psychiatry. 2015;14(3):278–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Tinland A, Leclerc L, Loubière S, et al. Psychiatric advance directives for people living with schizophrenia, bipolar I disorders, or schizoaffective disorders: study protocol for a randomized controlled trial – DAiP study. BMC Psychiatry. 2019;19(1):422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Murch R. Improving attitudes to mental health patients in ICU. Nurs N Z. 2016;22(8):30–31. [PubMed] [Google Scholar]
- 33. Weare R, Green C, Olasoji M, Plummer V. ICU nurses feel unprepared to care for patients with mental illness: a survey of nurses’ attitudes, knowledge, and skills. Intensive Crit Care Nurs. 2019;53:37–42. [DOI] [PubMed] [Google Scholar]
- 34. van der Meer D, Pinzón-Espinosa J, Lin BD, et al. Associations between psychiatric disorders, COVID-19 testing probability and COVID-19 testing results: findings from a population-based study. BJPsych Open. 2020;6(5):e87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Mansuri Z, Shah B, Adnan M, Chaudhari G, Jolly T. Ritonavir/Lopinavir and its potential interactions with psychiatric medications: a COVID-19 perspective. Prim Care Companion CNS Disord. 2020;22(3). [DOI] [PubMed] [Google Scholar]
- 36. May M, Slitzky M, Rostama B, Barlow D, Houseknecht KL. Antipsychotic-induced immune dysfunction: a consideration for COVID-19 risk. Brain Behav Immun Health. 2020;6:100097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Govind R, Freitas DF de, Pritchard M, Hayes RD, MacCabe JH. Clozapine treatment and risk of COVID-19 infection: retrospective cohort study [published online ahead of print July 27, 2020]. Br J Psychiatry. 2020:1–7. doi: 10.1192/bjp.2020.151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Ross SB, Wilson MG, Papillon-Ferland L, et al. COVID-SAFER: deprescribing guidance for hydroxychloroquine drug interactions in older adults [published online ahead of print May 22, 2020]. J Am Geriatr Soc. doi: 10.1111/jgs.16623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Upthegrove R, Khandaker GM. Cytokines, oxidative stress and cellular markers of inflammation in schizophrenia. Curr Top Behav Neurosci. 2020;44:49–66. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.