Abstract
Our aim was to analyze the prevalence of unhealthy movement behavior clusters before and during the COVID-19 pandemic, as well as to investigate whether changes in the number of unhealthy behaviors during the COVID-19 pandemic quarantine were associated with mental health indicators. Data of 38,353 Brazilian adults from a nationwide behavior research were used. For movement behaviors, participants reported the frequency and duration of physical activity and daily time on TV viewing and computer/tablet use before and during the pandemic period. Participants also reported the frequency of loneliness, sadness (feeling sad, crestfallen, or depressed), and anxiety feelings (feeling worried, anxious, or nervous) during the pandemic period. Sex, age group, highest academic achievement, working status during quarantine, country region, and time adhering to the quarantine were used as correlates. We used descriptive statistics and logistic regression models for the data analysis. The prevalence of all movement behavior clusters increased during the COVID-19 pandemic. The cluster of all three unhealthy movement behaviors increased from 4.6% (95% confidence interval [CI]: 3.9–5.4) to 26.2% (95% CI: 24.8–27.7). Younger adults, people with higher academic achievement, not working or working at home, and those with higher time in quarantine presented higher clustering. People that increased one and two or three unhealthy movement behaviors were, respectively, more likely to present loneliness (odds ratio [OR] = 1.41 [95% CI: 1.21–1.65] and OR = 1.71 [95% CI: 1.42–2.07]), sadness (OR = 1.25 [95% CI: 1.06–1.48] and OR = 1.73 [95% CI: 1.42–2.10]), and anxiety (OR = 1.34 [95% CI: 1.13–1.57] and OR = 1.78 [95% CI: 1.46–2.17]) during the COVID-19 quarantine. Clustering of unhealthy movement behaviors substantially increased and was associated with poorer mental health during the COVID-19 pandemic.
Keywords: Exercise, Sitting, Sedentary behavior, Sedentary lifestyle
Implications.
Practice: Individuals should practice physical activity according to the recommendations during the quarantine, as well as decrease the time in sedentary behaviors with the objective of protecting mental health during the quarantine.
Policy: Policymakers should be aware of increases in the prevalence of clusters of unhealthy movement behaviors, which can be associated with increases in chronic diseases, and develop public policies to encourage the practice of physical activity according to the recommendations, especially considering the mostly affected subgroups of the population.
Research: Researchers should continue to monitor the prevalence of unhealthy movement behaviors clusters and determinants as well as to formulate as well as test possible interventions during the COVID-19 period and after.
INTRODUCTION
The practice of physical activity and low sedentary behavior are important behaviors for health promotion, reported as protective factors for several negative physical and mental health outcomes [1–3]. In addition to their isolated approach, the co-occurrence of physical inactivity and sedentary behavior is associated with a greater increase in the risk for mental and physical negative health outcomes [4–6]. However, the prevalence of physical inactivity and elevated sedentary behavior are high worldwide [7,8], especially considering Latin America countries, which present even higher prevalences of physical inactivity and elevated sedentary behavior [7–9].
Although these unhealthy behaviors have been public health concerns for several years, the current COVID-19 pandemic has made this situation even worse [10]. The measures of social distancing and “stay-at-home” messages, effective for controlling the pandemic, have directly affected these movement behaviors [11]. Quarantine measures reduce opportunities for physical activity, especially outdoor activities, and increase daily sedentary behaviors [12], which can affect cardiovascular [13], metabolic [14], and mental health [15]. However, although recent studies have shown the potentially harmful effects of physical inactivity and sedentary behaviors during the COVID-19 pandemic [16,17], less attention has been paid to the population groups that are clustering these unhealthy behaviors. In recent years, physical inactivity and sedentary behaviors have been pointed out as distinct behaviors; however, stronger evidence suggests that the coexistence of both increases the risk of many negative health outcomes and mortality [18,19]. In addition, it was shown that the different types of sedentary behaviors (e.g., TV viewing and computer use) are specifically associated with mortality risk in interactions with physical activity [4], and the effects of the different sedentary behaviors have been especially identified regarding mental health outcomes [20]. Given that previous findings showed that sedentary behavior and reductions in physical activity can be negatively associated with mental health even after periods as short as 2 weeks [21,22], the negative effect of clustering physical inactivity and different types of sedentary behaviors during the COVID-19 pandemic may not only be summed but also amplified. Thus, we identified unhealthy movement behavior clusters before and during the COVID-19 pandemic and investigated whether changes in the number of unhealthy behaviors due to the COVID-19 pandemic quarantine are associated with mental health issues.
METHODS
Sample
The “Brazilian behavioral research during the COVID-19 pandemic” is a nationwide health survey that used a virtual questionnaire to assess the changes that occurred in the lives of Brazilians after the arrival of the coronavirus pandemic in the country, related to social restriction initiatives to protect people, including quarantine. Data collection was conducted between April 24 and May 24, 2020.
Participants were invited through a chain sampling procedure. In the first stage, the 15 researchers involved in the study chose a total of 200 other researchers from different states in Brazil, as well as 20 people each from their social networks, making a total of 400 people chosen. The people chosen in the first stage were denominated influencers. These 400 sent the survey link to at least 12 people from their social networks, obeying a stratification by sex, age range (18–39; 40–59; and 60+), and education level (incomplete high school or less; education complete medium or more). In addition, information about the study was disseminated through press releases, social communications from participating research institutions, state health departments, and social media. The survey link was also available at the influencers’ research institutions. All procedures were approved by the National Research Ethics Commission (process: 30598320.1.0000.5241). Initially, 45,161 participants completed the questionnaire. The sample was weighted according to characteristics from the 2019 National Household Sample Survey (conducted annually), considering the population in each state, education, age, sex, and prevalence of chronic diseases, aiming to include a nationally representative sample.
Movement behaviors
The questionnaires of physical activity and TV viewing were based on the questionnaire of the “Brazilian Telephone-based Risk Factor Surveillance System for Chronic Diseases,” which is an annual Brazilian survey begun in 2006. A previous study found good reproducibility for physical activity during leisure time (K = 0.70) and moderate reproducibility for TV viewing (K = 0.56) and also good values in comparison with the global physical activity questionnaire [23]. For physical activity before the COVID-19 pandemic, participants were asked “Before the COVID-19 pandemic, how many days a week did you practice any type of physical exercise or sport? (do not consider physical therapy).” Possible answers were: (a) less than 1 day/week; (b) 1–2 days/week; (c) 3–4 days/week; or (d) 5 or more days/week. For those reporting physical activity practice, we also asked: “How long did this activity last?” Possible answers were: (a) less than 30 min; (b) 30–45 min; (c) 46–60 min; or (d) more than 1 hr. For physical activity during the COVID−19 pandemic, participants were asked: “During the COVID-19 pandemic how many days a week did you practice any type of physical exercise or sport? (do not consider physical therapy).” Possible answers were: (a) less than 1 day/week; (b) 1–2 days/week; (c) 3–4 days/week; or (d) 5 or more days/week. For those reporting physical activity practice, we also asked: “How long did this activity last?” Possible answers were: (a) less than 30 min; (b) 30–45 min; (c) 46–60 min; or (d) more than 1 hr. We classified activities using the recommendation of 150 min/week [24], which was calculated using the median point of frequency and duration in each category.
For TV viewing, participants were asked: “Usually, before the pandemic, how many hours a day did you spend watching television?” and “During the pandemic, how many hours a day did you watch television?” Possible answers for both were (a) none; (b) less than 1 hr/day; (c) between 1 and less than 2 hr/day; (d) between 2 and less than 3 hr/day; (e) between 3 and less than 4 hr/day; (f) between 4 and less than 5 hr/day; (g) between 5 and less than 6 hr/day; and (h) 6 hr/day or more. For the assessment of computer/tablet use, we also used two questions “Usually, before the pandemic, how many hours a day did you spend using a computer or tablet?” and “During the pandemic, how many hours a day did you spend using a computer or tablet?” with an open answer. TV viewing and computer/tablet use were classified using the cutoff point of 4 hr/day at both moments (before and during the quarantine), especially considering the substantial increase in cardiovascular risk and depressive symptoms of 4 hr/day of TV viewing, which we standardized to computer use [25,26]. We created four mutually exclusive clusters of unhealthy movement behaviors: (a) inactive + high TV viewing; (b) inactive + high computer/tablet use; (c) high TV viewing + high computer/tablet use; and (d) inactive + high TV viewing + high computer/tablet use.
Mental health
As mental health indicators, we adopted three questions regarding feelings of loneliness, sadness, and anxiety. For loneliness, participants were asked: “During the pandemic period, how often did you feel isolated or alone?,” for sadness: “During the pandemic period, how often did you feel sad, crestfallen, or depressed?,” and for anxiety: “During the pandemic period, how often did you feel worried, anxious, or nervous?” Possible answers for each question were: (a) “Never,” (b) “A few times,” (c) “Often,” or (d) “Always.” We classified participants as positive for loneliness, sadness, and anxiety if they answered “often” or “always.”
Correlates
We used sex, age group (18–39, 40–59, and ≥ 60 years), country region (North, Northeast, Southeast, South, and Midwest), highest academic achievement, working status during the pandemic, change in income, and time adhering to quarantine as correlates. Academic achievement was classified as no academic achievement or elementary school, high school, and higher education or more. Working status during quarantine was classified as currently not working, working in a normal routine, and home office. Change in income was assessed by asking the participants about how their income had changed since the beginning of the COVID−19 pandemic, classified as (a) maintained or increased, (b) slightly reduced, or (c) substantially reduced or lost their income. The time adhering to quarantine was assessed through a question asking about adherence to quarantine. Those that answered adherence through staying at home and just going shopping at the supermarket and pharmacy or staying strictly at home, leaving only for health care needs also reported the duration of these measures. We classified adherence into no adherence to quarantine, less than 1 month, 1–2 months, and 2 or more months in quarantine.
Statistical procedures
Weighted frequencies, 95% confidence intervals, and difference in percentage points (p.p.) were used to describe the clustering of unhealthy movement behaviors in the general sample, as well as according to correlates. Crude and adjusted (adjusting for sex, age group, academic achievement, working status during the quarantine, change in income, and quarantine adherence) logistic regression models were created to analyze the association of changes in the number of unhealthy movement behaviors with mental health indicators. All analyzes were conducted using the software Stata 15.1.
RESULTS
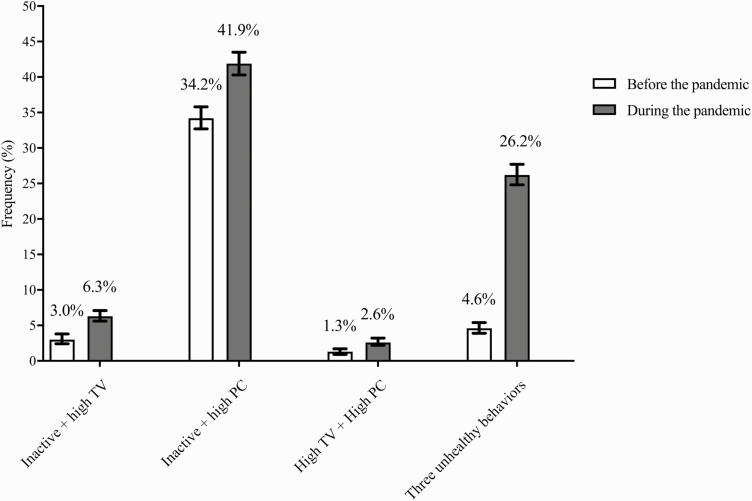
Due to missing data, our final sample was composed of 38,353 adults. The prevalences of each cluster of unhealthy movement behaviors are presented in Fig. 1. All clusters presented increased prevalence, including inactive + high TV viewing (3.3 p.p.), inactive + high computer/tablet use (7.7 p.p.), high TV viewing + high computer/tablet use (1.3 p.p.), and inactive + high TV viewing + high computer/tablet use (21.6 p.p.).
Fig 1.
Changes in the prevalence of clustering movement behaviors during the COVID-19 pandemic in Brazil (N = 38,353). PC computer/tablet use. Inactive refers to not attending the current physical activity recommendations (<150 min/week). High TV or computer/tablet use refers to the cutoff point of 4 hr/day.
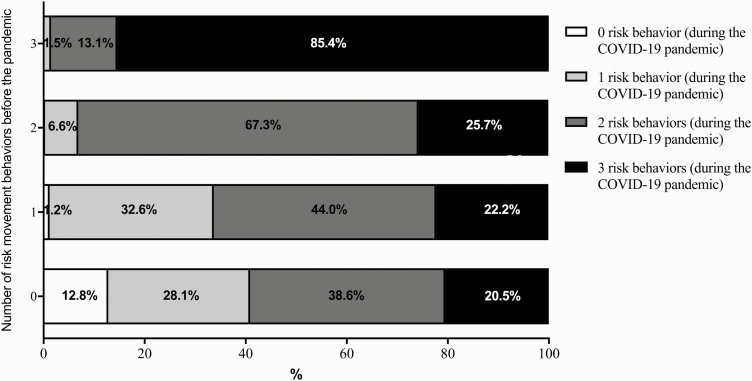
The increase in the number of unhealthy movement behaviors was substantial (Fig. 2) considering that 20.5% of those reporting no unhealthy behaviors before the pandemic changed to reporting three during the pandemic and 38.6% changed to reporting two. Similarly, those reporting only one unhealthy behavior before the pandemic were more likely to increase to two (44.0%) or three (22.2%) during the pandemic, while those reporting two or three unhealthy behaviors before the pandemic presented a stability pattern. The prevalence of people that presented two or three unhealthy behaviors before the pandemic and reduced to zero during the pandemic was lower than 1% each.
Fig 2.
Prevalence of the number of unhealthy movement behaviors during the COVID-19 pandemic according to the number of unhealthy behaviors before the pandemic in Brazil (N = 38,353)
Table 1 shows the changes in the prevalence of clustering of physical inactivity and sedentary behaviors according to correlates. In general, the clustering of the three unhealthy movement behaviors was high, with a crude difference ranging between 13.5% and 26.0% depending on the subgroup. Considering the correlates, a greater increase in the prevalence of clustering unhealthy movement behaviors occurred among younger adults, people with higher academic achievement, those with a different routine of working during the pandemic (not working or home office), and those with a longer time adhering to quarantine.
Table 1.
Changes in the prevalence of unhealthy movement behaviors clusters according correlates before and during the COVID-19 pandemic, Brazil 2020
| Inactive + high TV | Inactive + high PC | High TV + high PC | Inactive + high TV + high PC | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Before (n = 808) | During (n = 2,359) | Δ | Before (n = 13,383) | During (n = 16,405) | Δ | Before (n = 420) | During (n = 1,116) | Δ | Before (n = 1,188) | During (n = 9,068) | Δ | |
| Gender | ||||||||||||
| Female | 2.8 (2.4–3.4) | 7.0 (6.2–7.9) | 4.2 | 33.9 (32.2–35.5) | 40.5 (38.8–42.2) | 6.6 | 0.8 (0.6–1.2) | 2.6 (2.0–3.3) | 1.8 | 4.9 (4.0–6.1) | 27.8 (26.1–29.5) | 22.9 |
| Male | 3.2 (2.2–4.7) | 5.7 (4.6–7.1) | 2.5 | 34.6 (32.1–37.2) | 43.3 (40.6–46.0) | 8.7 | 1.7 (1.1–2.6) | 2.7 (1.9–3.6) | 1.0 | 4.2 (3.3–5.4) | 24.7 (22.4–27.2) | 20.5 |
| Age group | ||||||||||||
| 18–39 | 1.3 (0.7–2.4) | 3.8 (3.2–4.6) | 2.5 | 39.4 (37.1–41.7) | 50.4 (48.0–52.8) | 11.0 | 1.0 (0.6–1.6) | 2.3 (1.8–2.9) | 1.3 | 2.7 (2.1–3.5) | 25.4 (23.3–27.6) | 22.7 |
| 40–59 | 3.4 (2.3–5.0) | 7.9 (6.5–9.6) | 4.5 | 33.2 (30.8–35.7) | 36.2 (33.6–38.9) | 3.0 | 1.1 (0.7–1.6) | 3.0 (2.0–4.4) | 1.9 | 5.4 (4.3–6.9) | 28.0 (25.8–30.0) | 22.6 |
| ≥60 | 7.2 (5.4–9.4) | 10.5 (8.5–12.9) | 3.3 | 21.4 (18.3–24.9) | 28.4 (24.9–32.2) | 7.0 | 2.3 (1.1–4.7) | 2.9 (2.0–4.4) | 0.6 | 8.3 (5.9–11.5) | 25.0 (21.3–29.1) | 16.7 |
| Academic achievement | ||||||||||||
| Less than high school | 4.0 (2.5–6.4) | 6.3 (4.1–9.6) | 2.3 | 22.6 (17.6–28.4) | 27.7 (22.2–33.9) | 5.1 | 3.7 (1.4–9.8) | 4.2 (2.0–8.6) | 0.5 | 7.1 (4.2–11.9) | 29.5 (23.5–36.2) | 22.4 |
| High school | 3.3 (2.5–4.4) | 6.6 (5.7–7.7) | 3.3 | 34.8 (32.8–36.8) | 42.2 (40.1–44.3) | 7.4 | 1.0 (0.7–1.5) | 2.4 (1.9–3.2) | 1.4 | 4.8 (4.0–5.9) | 26.9 (25.0–28.8) | 22.1 |
| More than high school | 1.5 (1.3–1.6) | 5.3 (5.0–5.7) | 3.8 | 36.9 (36.2–37.6) | 46.4 (45.6–47.1) | 9.5 | 1.1 (1.0–1.3) | 2.7 (2.5–3.0) | 1.6 | 2.6 (2.4–2.9) | 22.6 (22.0–23.2) | 20.0 |
| Country region | ||||||||||||
| North | 5.6 (1.7–17.0) | 6.6 (3.0–13.8) | 1.0 | 31.8 (25.4–38.9) | 38.9 (31.9–46.4) | 7.1 | 1.2 (0.4–3.0) | 1.9 (1.1–3.3) | 0.7 | 7.6 (3.6–15.5) | 31.1 (23.6–39.7) | 23.5 |
| Northeast | 1.9 (1.3–2.9) | 5.3 (4.0–6.9) | 3.4 | 35.6 (31.7–39.6) | 41.9 (37.8–46.1) | 6.4 | 1.3 (0.5–3.4) | 3.7 (2.3–5.9) | 2.4 | 3.4 (2.3–5.0) | 28.1 (24.3–32.2) | 24.7 |
| Southeast | 3.3 (2.7–4.1) | 7.2 (6.3–8.2) | 3.9 | 33.9 (32.3–35.5) | 40.5 (38.9–42.2) | 6.6 | 1.3 (1.0–1.8) | 3.0 (2.4–3.7) | 1.7 | 4.2 (3.6–5.0) | 25.6 (24.1–27.2) | 21.4 |
| South | 3.2 (2.0–5.0) | 5.9 (4.3–8.0) | 2.7 | 34.1 (30.4–38.0) | 43.5 (39.7–47.5) | 9.4 | 1.2 (0.6–2.6) | 1.0 (0.6–1.5) | 0.2 | 5.7 (3.9–8.2) | 26.2 (23.0–29.7) | 20.5 |
| Midwest | 1.6 (0.8–3.3) | 5.0 (3.1–8.0) | 3.4 | 35.0 (27.6–43.2) | 50.4 (41.7–59.2) | 15.4 | 0.7 (0.3–1.7) | 1.5 (0.7–2.9) | 0.8 | 5.3 (2.7–9.9) | 18.8 (14.3–24.3) | 13.5 |
| Working during the pandemic | ||||||||||||
| No | 3.7 (3.0–4.6) | 8.1 (7.1–9.3) | 4.4 | 28.6 (26.6–30.7) | 36.2 (34.0–38.5) | 7.6 | 1.6 (1.0–2.4) | 2.9 (2.2–3.8) | 1.3 | 4.6 (3.6–5.8) | 29.1 (27.0–31.3) | 24.5 |
| Normal routine | 3.7 (1.9–7.1) | 5.6 (3.9–8.1) | 1.9 | 32.5 (29.0–36.2) | 42.0 (38.3–45.9) | 9.5 | 0.6 (2.5-1.4) | 1.5 (0.9–2.5) | 0.9 | 5.1 (3.6–7.1) | 22.6 (18.9–26.6) | 17.5 |
| Home office | 1.3 (0.9–2.0) | 3.7 (2.9–4.6) | 2.4 | 45.4 (42.6–48.2) | 51.7 (48.9–54.5) | 6.3 | 1.2 (0.8–1.8) | 3.0 (2.1–4.3) | 1.8 | 4.2 (3.1–5.5) | 23.8 (21.7–26.1) | 19.6 |
| Change in the income during the pandemic | ||||||||||||
| Maintained or increased | 3.6 (2.8–4.6) | 7.4 (6.3–8.8) | 3.8 | 35.5 (33.2–37.8) | 42.5 (40.3–44.9) | 7.0 | 1.5 (1.0–2.2) | 2.6 (2.0–3.3) | 1.1 | 5.6 (4.4–7.2) | 22.9 (20.9–25.0) | 17.3 |
| Slightly reduced | 1.7 (1.2–2.3) | 4.8 (4.0–5.8) | 3.1 | 34.9 (32.4–37.6) | 45.1 (42.3–47.9) | 10.2 | 1.4 (0.7–2.9) | 3.1 (2.1–4.7) | 1.7 | 3.1 (2.4–4.0) | 26.0 (23.5–28.8) | 22.9 |
| Substantially reduced or lost | 3.5 (2.1–5.8) | 6.3 (4.9–8.1) | 2.8 | 32.0 (29.0–35.1) | 38.0 (34.6–41.5) | 6.0 | 0.8 (0.5–1.3) | 2.2 (1.5–3.3) | 1.4 | 4.7 (3.5–6.3) | 30.7 (27.7–33.8) | 26.0 |
| Time under quarantine adherence | ||||||||||||
| No | 3.2 (1.9–5.3) | 5.9 (4.3–8.0) | 2.7 | 34.4 (31.3–37.8) | 43.5 (40.1–46.9) | 9.1 | 1.0 (0.5–1.9) | 2.3 (1.4–3.8) | 1.3 | 4.7 (3.4–6.4) | 20.8 (18.1–23.8) | 16.0 |
| <1 month | 2.7 (1.9–3.9) | 5.5 (4.3–7.0) | 2.8 | 32.4 (28.7–36.3) | 42.0 (37.8–46.4) | 9.6 | 1.2 (0.6–2.4) | 2.9 (1.8–4.7) | 1.7 | 4.9 (3.1–7.7) | 27.9 (24.1–32.0) | 23.0 |
| 1–2 months | 2.8 (2.0–3.9) | 6.6 (5.7–7.7) | 3.8 | 35.2 (33.2–37.2) | 42.4 (40.3–44.6) | 7.2 | 1.4 (0.9–2.2) | 2.8 (2.2–3.6) | 1.4 | 4.5 (3.6–5.5) | 27.7 (25.8–29.7) | 23.2 |
| >2 months | 5.1 (3.2–8.1) | 8.2 (5.6–12.0) | 3.1 | 31.8 (26.5–37.7) | 32.1 (27.1–37.4) | 0.3 | 1.1 (0.6–2.3) | 2.0 (1.2–3.3) | 0.9 | 4.1 (2.7–6.2) | 31.2 (25.7–37.4) | 27.1 |
Data are described using values of percentage (95% confidence interval). 22,554 (56.9%) participants did not present any cluster of unhealthy movement behaviors before the pandemic and 9,405 (22.9%) participants did not present any cluster of unhealthy movement behaviors during the pandemic.
The association between changes in the number of unhealthy movement behaviors and mental health is presented in Table 2. In the adjusted analyses, people that reported increases of one and two or three unhealthy movement behaviors were more likely to present loneliness, sadness, and anxiety in comparison to those who maintained their number of unhealthy behaviors. In addition, reductions in the number of unhealthy behavior clusters were associated with lower odds for anxiety during the COVID-19 quarantine.
Table 2.
Associations between change in the number of movement behaviors and mental health and sleep outcomes during the COVID-19 pandemic, Brazil 2020 (N = 38,353)
| Change in risk movement behaviors | Loneliness OR (95% CI) | Sadness OR (95% CI) | Anxiety OR (95% CI) |
|---|---|---|---|
| Crude models | |||
| Reduced | 1.08 (0.79–1.49) | 0.83 (0.62–1.13) | 0.68 (0.51–0.92) |
| Maintained | REF | REF | REF |
| Increased one | 1.48 (1.27–1.73) | 1.34 (1.14–1.56) | 1.43 (1.23–1.67) |
| Increased 2 or 3 | 1.82 (1.50–2.19) | 1.86 (1.54–2.24) | 1.88 (1.56–2.27) |
| Adjusted models | |||
| Reduced | 1.07 (0.75–1.52) | 0.86 (0.65–1.14) | 0.74 (0.56–0.96) |
| Maintained | REF | REF | REF |
| Increased one | 1.40 (1.20–1.64) | 1.24 (1.05–1.46) | 1.32 (1.12–1.55) |
| Increased 2 or 3 | 1.65 (1.36–1.99) | 1.66 (1.36–2.02) | 1.69 (1.39–2.06) |
CI confidence interval; OR odds ratio.
Adjusted for age group, sex, highest academic achievement, working status during the COVID-19 quarantine, change in the income, and time under quarantine adherence.
DISCUSSION
The current study investigated the prevalence of unhealthy movement behavior clustering before and during the COVID-19 pandemic, as well as the association between changes in the clustering of unhealthy movement behaviors and mental health indicators during the COVID-19 pandemic among Brazilian adults. Our main findings were that the clustering of physical inactivity and sedentary behaviors substantially increased during the COVID-19 pandemic, especially considering the clustering of all three unhealthy behaviors. A quarter of Brazilian adults are inactive and spend more than 8 hr in sedentary behaviors during the day (TV viewing + computer/tablet use), which significantly increases the risk for mortality [18]. Furthermore, the increase in the number of unhealthy movement behaviors was associated with loneliness, sadness, and anxiety feelings during the COVID-19 pandemic.
Both physical inactivity and sedentary behavior were highly prevalent before the COVID-19 pandemic. It is estimated that the prevalence of physical inactivity was approximately 40% in Latin America [7] and the prevalence of high sedentary behavior was between 14% and 58%, depending on the indicator [9]. However, the co-occurrence of physical inactivity and sedentary behavior was not evaluated using nationally representative cohorts. In our study, we found that the co-occurrence of physical inactivity, high TV viewing, and high computer/tablet use substantially increased, more than doubling in all the population subgroups. However, some subgroups were more affected by the elevation in the clustering rates. Young adults, those with higher academic achievement, without a normal work routine, and with a longer time adhering to quarantine presented higher rates of clustering.
Some aspects could underlie these associations. Younger adults present lower rates of physical inactivity, as well as TV viewing, which could contribute to a higher increase in the clustering of both behaviors [8,9]. Similarly, participants with higher educational status present lower physical inactivity, especially during leisure time, as well as TV viewing, which could be associated with a higher increase in these behaviors [9,27]. The exception is considering the higher prevalence of clustering of high computer/tablet use and physical inactivity, which is consistently high among younger adults and people with higher academic achievement. These findings highlight that, with the increases in the clustering rates during the COVID-19 quarantine, the subgroups with lower rates before the pandemic became similar (younger adults, higher academic achievement, and working in home office) or higher (longer time adhering to quarantine and not working during the pandemic). Thus, to tackle physical inactivity and elevated sedentary behaviors during the pandemic, it is necessary to change the target subgroups and strategies used before the pandemic [28].
Our study also found that the increase in the number of unhealthy behaviors during the COVID-19 pandemic increased the odds for poorer mental health indicators. These findings agree with a potential joint association between physical activity and sedentary behavior in the association with mental health, with an additive association [5,6]. In this sense, both sedentary behavior and physical activity are risk factors for mental health and their co-occurrence can increase the risk [5,6], especially considering the substantial increase in the odds given an increase of two or three unhealthy movement behaviors.
Several mechanisms can explain part of the association of changes in physical activity and sedentary behavior during the COVID-19 quarantine with poorer mental health. Biologically, sedentary behavior can be associated with inflammatory markers even after short periods of time, which can be associated with poorer mood indicators [22]. As a social aspect, lower physical activity may be associated with lower social interactions, which can be detrimental for mental health, especially for loneliness feelings [29,30]. In addition, the COVID-19 pandemic brought a massive amount of negative news both on the television and internet (especially social media), which is associated with worse mental health indicators, and could also partly explain the association of TV viewing and computer use with mental health [31–33].
Our study analyzed more than 35,000 Brazilian adults from a nationwide sample, weighted for national representativity to investigate the pattern of clustering unhealthy movement behaviors during the COVID-19 quarantine, as well as its association with mental health indicators in one of the countries most affected by the COVID-19 pandemic [34]. Given the urge for representative studies to identify the impacts of the COVID-19 pandemic quarantine on movement behaviors and their consequences, we consider that these findings advance the knowledge and reinforce the need to promote active lifestyles that can mitigate the harmful effects of the quarantine period on people’s health. Despite this, our findings should be considered in the light of potential limitations. First, the self-reported data and retrospective design are prone to recall bias. Second, considering the web-based assessment, participants with extremely low socioeconomic conditions, who were more affected by the pandemic, were underrepresented, potentially affecting the results. Third, physical activity and sedentary behavior questionnaires have some bias as participants frequently overestimate time in leisure-time physical activity and underestimate sedentary behavior [35,36]. Fourth, we adopted a specific indicator of physical activity (exercise/sport), which did not consider other domains of the day (e.g., domestic, transport, and occupational activities), as well as the pattern of the movement behaviors in terms of breaks and bouts.
In conclusion, the clustering of unhealthy movement behaviors substantially increased during the COVID-19 pandemic quarantine, especially considering some subgroups of the population (e.g., younger adults, higher academic achievement, working in home office, not working during the pandemic, and longer time adhering to quarantine). These increases are associated with poorer mental health outcomes.
Acknowledgments
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. A.O.W. is supported by the São Paulo Research Foundation with a PhD scholarship (FAPESP process: 2019/24124–7). D.C.M. (process 308250/2017-6), M.B.A.B. (process: 303241/2019-5), and C.L.S. are supported by the National Council of Technological and Scientific Development, which funded the productivity scholarship. This paper presents an independent research. The views expressed in this publication are those of the authors and not necessarily those of the acknowledged institutions.
Compliance with Ethical Standards
Conflicts of Interest: The authors declare no conflict of interest.
Authors’ Contributions: A.O.W. conceptualization, formal analysis, writing - original draft, writing - review & editing, visualization. D.R.S.: conceptualization, writing - original draft, writing - review & editing, visualization. D.C.M. methodology, project administration, writing - review & editing, validation. P.R.B.S.: project administration, investigation writing - review & editing, validation. L.O.A.: project administration, investigation writing - review & editing, validation. M.B.A.B.: methodology, project administration, writing - review & editing, validation. C.L.S.: supervision, methodology, project administration, writing - review & editing, validation.
Ethical Approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by the National Research Ethics Commission (process: 30598320.1.0000.5241). This article does not contain any studies with animals performed by any of the authors.
Informed Consent: Informed consent was obtained from all individual participants included in the study.
References
- 1. Firth J, Siddiqi N, Koyanagi A, et al. The Lancet Psychiatry Commission: A blueprint for protecting physical health in people with mental illness. Lancet Psychiatry. 2019;6(8):675–712. [DOI] [PubMed] [Google Scholar]
- 2. Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT; Lancet Physical Activity Series Working Group Effect of physical inactivity on major non-communicable diseases worldwide: An analysis of burden of disease and life expectancy. Lancet. 2012;380(9838):219–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Rezende LFM, Sá TH, Mielke GI, Viscondi JYK, Rey-López JP, Garcia LMT. All-cause mortality attributable to sitting time. Am J Prev Med. 2016;51(2):253–263. [DOI] [PubMed] [Google Scholar]
- 4. Ekelund U, Steene-Johannessen J, Brown WJ, et al. ; Lancet Physical Activity Series 2 Executive Committe ; Lancet Sedentary Behaviour Working Group. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet. 2016;388(10051):1302–1310. [DOI] [PubMed] [Google Scholar]
- 5. Liao Y, Shibata A, Ishii K, Oka K. Independent and combined associations of physical activity and sedentary behavior with depressive symptoms among Japanese adults. Int J Behav Med. 2016;23(4):402–409. [DOI] [PubMed] [Google Scholar]
- 6. Werneck AO, Stubbs B, Fernandes RA, Szwarcwald CL, Silva DR. Leisure time physical activity decreases the association between TV-viewing and depressive symptoms: A large study among 60,202 Brazilian adults. J Affect Disord. 2019;252:310–314. [DOI] [PubMed] [Google Scholar]
- 7. Guthold R, Stevens GA, Riley LM, Bull FC. Worldwide trends in insufficient physical activity from 2001 to 2016: A pooled analysis of 358 population-based surveys with 1·9 million participants. Lancet Glob Health. 2018;6(10):e1077–e1086. [DOI] [PubMed] [Google Scholar]
- 8. Hallal PC, Andersen LB, Bull FC, Guthold R, Haskell W, Ekelund U. Global physical activity levels: Surveillance progress, pitfalls, and prospects. Lancet. 2012;380(9838):247–257. [DOI] [PubMed] [Google Scholar]
- 9. Werneck AO, Baldew SS, Miranda JJ, Díaz Arnesto O, Stubbs B, Silva DR; on the behalf of the South American Physical Activity and Sedentary Behavior Network (SAPASEN) collaborators Physical activity and sedentary behavior patterns and sociodemographic correlates in 116,982 adults from six South American countries: The South American physical activity and sedentary behavior network (SAPASEN). Int J Behav Nutr Phys Act. 2019;16(1):68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. World Health Organization. Coronavirus Disease (COVID-19): Situation Report—124. Geneva, Switzerland: World Health Organization; 2020. Available at https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200523-covid-19-sitrep-124.pdf?sfvrsn=9626d639_2. Accessibility verified July 15, 2020. [Google Scholar]
- 11. Ammar A, Brach M, Trabelsi K, et al. Effects of COVID-19 home confinement on eating behaviour and physical activity: Results of the ECLB-COVID19 international online survey. Nutrients. 2020;12(6):1583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Pépin JL, Bruno RM, Yang RY, et al. Wearable activity trackers for monitoring adherence to home confinement during the COVID-19 pandemic worldwide: data aggregation and analysis. J Med Internet Res. 2020;22(6):e19787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Peçanha T, Goessler KF, Roschel H, Gualano B. Social isolation during the COVID-19 pandemic can increase physical inactivity and the global burden of cardiovascular disease. Am J Physiol Heart Circ Physiol. 2020;318(6):H1441–H1446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. King AJ, Burke LM, Halson SL, Hawley JA. The challenge of maintaining metabolic health during a global pandemic. Sports Med. 2020;50(7):1233–1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Arora T, Grey I. Health behaviour changes during COVID-19 and the potential consequences: A mini-review. J Health Psychol. 2020;25(9):1155–1163. [DOI] [PubMed] [Google Scholar]
- 16. Maugeri G, Castrogiovanni P, Battaglia G, et al. The impact of physical activity on psychological health during Covid-19 pandemic in Italy. Heliyon. 2020;6(6):e04315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Meyer J, McDowell C, Lansing J, et al. Changes in physical activity and sedentary behavior in response to COVID-19 and their associations with mental health in 3052 US adults. Int J Environ Res Public Health. 2020; 17(18):E6469. [DOI] [PMC free article] [PubMed]
- 18. Stamatakis E, Gale J, Bauman A, Ekelund U, Hamer M, Ding D. Sitting time, physical activity, and risk of mortality in adults. J Am Coll Cardiol. 2019;73(16):2062–2072. [DOI] [PubMed] [Google Scholar]
- 19. Ekelund U, Tarp J, Steene-Johannessen J, et al. Dose-response associations between accelerometry measured physical activity and sedentary time and all cause mortality: Systematic review and harmonised meta-analysis. BMJ. 2019;366:l4570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hallgren M, Dunstan DW, Owen N. Passive versus mentally active sedentary behaviors and depression. Exerc Sport Sci Rev. 2020;48(1):20–27. [DOI] [PubMed] [Google Scholar]
- 21. Edwards MK, Loprinzi PD. Effects of a sedentary behavior-inducing randomized controlled intervention on depression and mood profile in active young adults. Mayo Clin Proc. 2016;91(8):984–998. [DOI] [PubMed] [Google Scholar]
- 22. Endrighi R, Steptoe A, Hamer M. The effect of experimentally induced sedentariness on mood and psychobiological responses to mental stress. Br J Psychiatry. 2016;208(3):245–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Moreira AD, Claro RM, Felisbino-Mendes MS, Velasquez-Melendez G. Validity and reliability of a telephone survey of physical activity in Brazil. Rev Bras Epidemiol. 2017;20(1):136–146. [DOI] [PubMed] [Google Scholar]
- 24. World Health Organization. Global Recommendations on Physical Activity for Health. Geneva, Switzerland: World Health Organization; 2010. [PubMed] [Google Scholar]
- 25. Werneck AO, Oyeyemi AL, Szwarcwald CL, Vancampfort D, Silva DR. Associations between TV viewing and depressive symptoms among 60,202 Brazilian adults: The Brazilian national health survey. J Affect Disord. 2018;236:23–30. [DOI] [PubMed] [Google Scholar]
- 26. Patterson R, McNamara E, Tainio M, et al. Sedentary behaviour and risk of all-cause, cardiovascular and cancer mortality, and incident type 2 diabetes: A systematic review and dose response meta-analysis. Eur J Epidemiol. 2018;33(9):811–829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. O’Donoghue G, Kennedy A, Puggina A, et al. Socio-economic determinants of physical activity across the life course: a “DEterminants of DIet and Physical ACtivity” (DEDIPAC) umbrella literature review. PLoS One. 2018;13(1):e0190737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Sallis JF, Adlakha D, Oyeyemi A, Salvo D. An international physical activity and public health research agenda to inform coronavirus disease-2019 policies and practices. J Sport Health Sci. 2020;9(4):328–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Andersen MH, Ottesen L, Thing LF. The social and psychological health outcomes of team sport participation in adults: An integrative review of research. Scand J Public Health. 2019;47(8):832–850. [DOI] [PubMed] [Google Scholar]
- 30. Hallgren M, Lundin A, Tee FY, Burström B, Forsell Y. Somebody to lean on: Social relationships predict post-treatment depression severity in adults. Psychiatry Res. 2017;249:261–267. [DOI] [PubMed] [Google Scholar]
- 31. Ni MY, Yang L, Leung CMC, et al. Mental health, risk factors, and social media use during the COVID-19 epidemic and cordon Sanitaire among the community and health professionals in Wuhan, China: Cross-sectional survey. JMIR Ment Health. 2020;7(5):e19009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Gao J, Zheng P, Jia Y, et al. Mental health problems and social media exposure during COVID-19 outbreak. PLoS One. 2020;15(4):e0231924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Nekliudov NA, Blyuss O, Cheung KY, et al. Excessive media consumption about COVID-19 is associated with increased state anxiety: Outcomes of a large online survey in Russia (Preprint) (preprint). J Med Internet Res. 2020;22(9):e20955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. World Health Organization. Coronavirus Disease (COVID-19): Situation Report—165. Geneva, Switzerland: World Health Organization; 2020. Available at https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200703-covid-19-sitrep-165.pdf?sfvrsn=b27a772e_2. Accessibility verified July 15, 2020. [Google Scholar]
- 35. Prince SA, LeBlanc AG, Colley RC, Saunders TJ. Measurement of sedentary behaviour in population health surveys: A review and recommendations. PeerJ. 2017;5:e4130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Shephard RJ. Limits to the measurement of habitual physical activity by questionnaires * Commentary. Br J Sports Med. 2003;37(3):197–206. [DOI] [PMC free article] [PubMed] [Google Scholar]