Abstract
Sedentary behavior is associated with poor physical and mental health. Targeting sedentary behavior is a simple strategy that may help counter physical and mental health concerns associated with COVID-19-related social restrictions. Of course, traditional strategies such as achieving optimal exercise and physical activity levels are also important and should be recommended. However, even under normal circumstances, the difficulty in promoting lasting exercise habits at multiple levels (e.g. individual, environment, policy) are well documented, and chances of maintaining or improving these factors is now even lower. Thus, relative to other lifestyle behaviors – sedentary behavior may be more amenable to change. Moreover, reducing sedentary behavior may be less susceptible to influence from factors associated with health disparities such as age, race, and socio-economic status compared to exercise or physical activity. Sedentary behavior is a feasible health strategy that should be targeted during COVID-19.
Keywords: Sedentary behavior, COVID-19, Physical health, Mental health, Lifestyle behaviors, Socioecological model
Implications.
Practice: Community- and home-based efforts to reduce sedentary behavior are practical strategies to promote health during COVID-19.
Policy: Policymakers should consider promoting strategies to interrupt sedentary behavior—such as by making safe, open outdoor spaces available for socially distant physical activity—as a means to encourage healthy lifestyle behaviors while not compromising the social restrictions necessary to curb the spread of COVID-19.
Research: Future research is needed to better understand and modify determinants of key lifestyle behaviors (e.g., sedentary behavior) during COVID-19, including at individual, environmental, and policy levels.
INTRODUCTION
Humanity is facing unprecedented challenges as the coronavirus (COVID-19) pandemic has infected over 11 million individuals worldwide and impacted (e.g., financially and mentally) many more [1, 2]. It now appears unlikely that the virus and the resulting social restrictions (e.g., social distancing, self-isolation, and remote working/learning) will subside in the short term, forcing humans to adapt to a new way of living and interacting with each other. While social restrictions are critical strategies to combat the spread of the virus, they also promote negative lifestyle behaviors, such as physical inactivity and sedentary behavior. These behaviors are associated with poor cardiometabolic and mental health [3, 4] and with COVID-19 severity [5]. Thus, behavioral strategies are necessary to offset the negative health consequences of COVID-19-related social restrictions while minimizing the likelihood of severe COVID-19 outcomes [6]. In this commentary, we argue that sedentary behavior is an achievable target for behavior change during COVID-19.
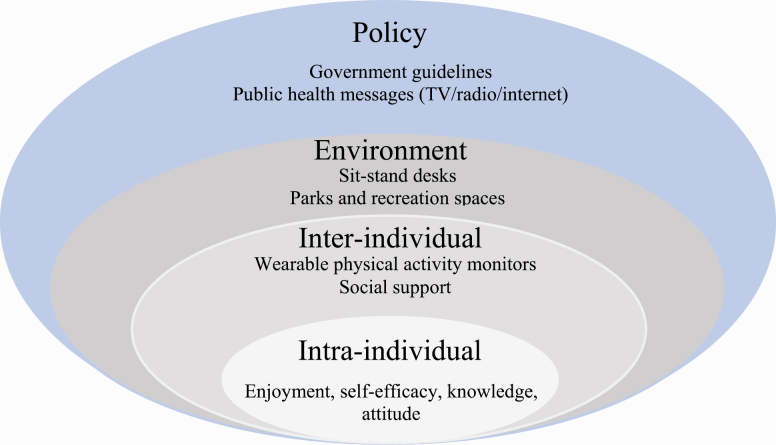
Healthy behaviors, such as structured exercise to combat physical inactivity, should be promoted as part of a balanced lifestyle. However, even during normal times, it is challenging to promote lasting healthy exercise habits [7]. When considering the many determinants and barriers to exercise (e.g., access to safe, open spaces), the complexity and difficulty of promoting exercise in the midst of COVID-19-related social restrictions are even more readily apparent. A useful framework for contextualizing the determinants of and barriers to behavior change is the socioecological model, which recognizes that individuals exist within the context of their environment [8]. Specifically, behavior change is likely to be restricted if the physical and sociocultural environments do not support behavior change. Intraindividual (e.g., self-efficacy and enjoyment), interindividual (e.g., social support), physical environment (e.g., home and neighborhood), and policy-level (e.g., government guidelines) determinants are unique factors that must be considered in the context of promoting exercise. The determinants of exercise are indeed traditionally dependent on factors higher in the socioecological model (e.g., policy/environment). However, it is particularly important to consider the socioecological framework now as the supportive influences of exercise (e.g., economic and infrastructural resources) have been directly, negatively affected by social restrictions associated with COVID-19. Mixed evidence has pointed to both increases and decreases in exercise in the wake of COVID-19 [3, 9, 10] (although some COVID-19-related policies/recommendations may actually decrease sedentary behavior, such as the removal of chairs or benches in workplaces and public places [11, 12]). However, for individuals in lower socioeconomic status (SES) segments of the population, the chances of improving already low levels of exercise are now even less [13]. Additionally, these individuals are more likely to contract COVID-19, as well as suffer more severe outcomes, compared to higher SES individuals and are arguably most in need of healthy behavior adoption [14–17].
Compared to exercise, sedentary behavior, defined as any waking activity in a seated or reclining position (≤1.5 metabolic equivalents) [18], may be less susceptible to factors associated with health disparities, such as race and SES. For example, low-income individuals are less likely to be able to afford home exercise equipment or have access to high-quality parks and recreation facilities [13]. Not only is sedentary behavior an independent risk factor for cardiometabolic diseases [19, 20] but it can also be safely modulated during the pandemic to a greater extent than exercise. For example, interrupting sedentary behavior with a simple low-intensity physical activity (e.g., standing calf raises) at home or work does not risk compromising social distancing to the same degree as visiting a gym or a park to engage in traditional exercise [21]. Reducing sedentary behavior is a realistic and feasible target that may confer physical and mental health benefits, including in adults, adolescents, and children [22–27]. Thus, while exercise is a potent health-promoting behavior and should continue to be encouraged, a particular emphasis should be placed on reducing sedentary behavior. This commentary will further outline the connections between sedentary behavior and physical and mental health and, through the lens of a socioecological model of behavior change, provide recommendations for reducing sedentary behavior during COVID-19.
COVID-19 and increased sedentary behavior
Available evidence indicates that increased sedentary behavior has been an unintended consequence of the social restrictions needed to combat the spread of COVID-19 [28–30]. Remote working, social distancing, and self-isolating at home have interrupted normal daily routines. For example, leisurely walking in public places and movement around a typical office or workspace have largely been abated as a result of the decreased human contact needed to contain COVID-19 [31, 32]. Moreover, it is likely that COVID-19 has indirectly caused already low exercise levels to decrease even further, particularly amongst individuals in lower SES populations, racial minorities, and other at-risk segments of the population [33]. Thus, it is plausible that sedentary behavior has been increased at the expense of both traditional moderate-vigorous-intensity physical activity (e.g., formal exercise), as well as low-intensity physical activity that normally accompanies daily work, recreational, and social routines. Of concern, the lack of moderate-vigorous physical activity and increased sedentary behavior are independent risk factors for cardiometabolic diseases, which are associated with more severe COVID-19 outcomes [34, 35].
Sedentary behavior and physical health
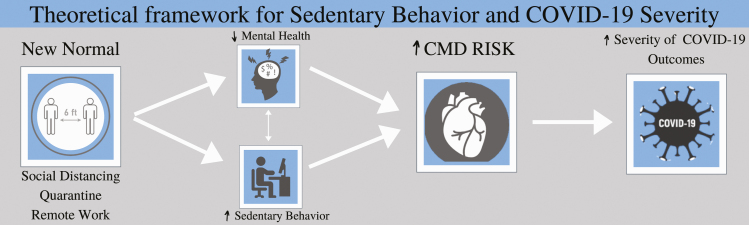
Strong longitudinal associations exist between sedentary behavior, cardiometabolic disease risk, and all-cause mortality [19]. For example, sitting ≥6 hr per day is associated with a 1.28-fold increase in all-cause mortality compared to those that sat <3 hr per day [36]. Sedentary behavior negatively impacts health by decreasing vascular function, energy expenditure, and glucose/insulin regulation—all of which are strongly associated with cardiometabolic disease risk [27, 37, 38]. Importantly, the presence of cardiometabolic disease risk factors (e.g., insulin resistance and hypertension) and overt cardiometabolic disease (e.g., obesity, coronary artery disease, and diabetes) have been associated with more severe COVID-19 outcomes, such as hospitalization, intubation, and death [5, 39, 40]. For instance, data from the Centers of Disease Control indicated that considerable proportions of underlying cardiometabolic conditions were present among COVID-19 hospitalizations in March 2020, including hypertension (49.7%), obesity (48.3%), diabetes (28.3%), and cardiovascular disease (27.8%) [41]. As such, increased sedentary behavior as a result of COVID-19 threatens cardiometabolic health, which is concerning in and of itself yet is doubly troublesome given the links between poor cardiometabolic health and severe COVID-19 outcomes (Fig. 1).
Fig 1.
Theoretical framework for sedentary behavior and COVID-19 severity.
Sedentary behavior and mental health
Increased sedentary behavior and physical inactivity have both been implicated in poor mental health outcomes, including stress, anxiety, and depression [33, 42–45]. Additionally, increases in stress, anxiety, depression, frustration, anger, loss of freedom, inadequate information, financial struggle, and uncertainty regarding the future have been reported in past epidemics, as well as in COVID-19 [46–52]. It is important to note that mental stress directly confers cardiometabolic risk via sympathetic overactivation and also interacts in a bidirectional manner with poor lifestyle factors known to increase cardiometabolic risk [48, 53]. Regarding the latter point, COVID-19 may promulgate harmful cycles in which elevated mental stress exacerbates poor lifestyle behaviors, which, in turn, may lead to even greater stress [48]. This is especially concerning since both mental stress and other negative lifestyle factors associated with mental stress, such as sedentary behavior, increase cardiometabolic disease risk and may, thus, elevate the likelihood for negative COVID-19 outcomes [38, 54] (Fig. 1).
Recommendations and considerations
In the context of mitigating vascular and metabolic dysfunction associated with sedentarism, strategies to interrupt sedentary behavior should be emphasized, particularly those that can be implemented in the home or neighborhoods. Effective sedentary behavior interruption strategies include fidgeting, bodyweight or resistance band exercises, standing, and walking [23,24,55–57]. Though specific guidelines for limiting sedentary behavior are currently lacking, current evidence, including from our group’s recent meta-analysis, indicates that the most extensively reported and efficacious strategies seem to be standing and walking 2–5 min every 20–30 min (Table 1) [23,24,55–57]. While strategies designed to interrupt sedentary behavior for the purpose of improving mental health have been less extensively studied, available evidence does suggest the possibility that such strategies may indeed benefit mental health [22, 44].
Table 1.
Best evidence for breaking up sedentary behavior in the context of feasibility and reducing cardiometabolic disease risk
| Best evidence for sitting interruption [55] | |
| Frequency | Every 20–30 min |
| Intensity | Light |
| Time | 2–5 min |
| Type | Walking and standing |
Linking back to the socioecological model of behavior change, we recommend that reducing sedentary behavior be considered and promoted within the context of each level of the socioecological model (Fig. 2). At the policy level, international research efforts, such as the Collaborative Outcomes Study on Health and Function During Infection Times are needed to better understand the social and behavioral determinants of negative health outcomes during COVID-19, which, in turn, can help shape appropriate, preventive health-promoting policies [58]. As an example, municipalities should consider implementing measures to promote breaking up sedentary behavior while maintaining safe social distancing. One option could be to prohibit automobile traffic in urban neighborhoods on select days or weekends to better enable easily accessible socially distant time spent outdoors, as has already been demonstrated in cities such as Oakland, CA, Boston, MA, and New York, NY [59]. Such policies may not only encourage traditional recreation and moderate-vigorous physical activity but could also facilitate true sedentary behavior interruption strategies, such as an easily accessible 5 min walk outdoors between video (e.g., Zoom) meetings.
Fig 2.
Socioecological model of behavior change for sedentary behavior.
At the level of the physical environment, stand-up desks could be implemented for employees who have returned to traditional work environments. Similarly, employers could offer financial assistance to incorporate stand-up desks and/or wearable physical activity monitors at employees’ homes for remote workers. Moreover, such action need not be viewed as altruistic as sedentary behavior and cardiometabolic conditions are known to reduce worker productivity and increase employer costs [60, 61].
The individual-level determinants of sedentary behavior are arguably most important to consider in that they are closely related to an individual’s locus of control. Unlike exercise, sedentary behavior does not rely on difficult-to-modify determinants higher up in the socioecological model. At the interindividual level, social support to reduce sedentary behavior may include encouraging colleagues to take standing-up or stretching breaks during work-related video meetings or challenging family and friends to friendly step-count competitions via wearable or smart-phone-based physical activity monitors. Technological strategies, such as physical activity monitors, are particularly attractive as they can be implemented/modulated at multiple levels of the socioecological model and have been shown to successfully (a) increase cognitive/emotional constructs related to motivation and positive behavior change, (b) reduce sedentary behavior, and (c) improve health [62–65].
At the intraindividual level, it is critical to consider the factor of enjoyment. Individuals will be more likely to adhere to behavior change if a particular activity is enjoyable [66]. If simply standing or doing repetitive resistance exercises is perceived as a mundane task, continued adherence will be compromised [67]. Health promotion efforts should encourage individuals to seek out creative strategies to interrupt sedentary behaviors that are enjoyable to them—whether that be spending a few minutes gardening throughout the day, dancing along to one’s favorite music, or playing with children or pets.
CONCLUSION
The COVID-19 pandemic is a rapidly changing global health crisis that will likely continue into 2021 and perhaps beyond. Efforts to contain the virus are centered on drastic social restrictions, which threaten cardiometabolic and mental health [35, 68]. Not only are decrements in health concerning in and of themselves, but cardiometabolic diseases and their risk factors predispose individuals to severe COVID-19 outcomes [5, 34]. Behavioral strategies, such as moderate-vigorous physical activity, provide potent protective effects against cardiometabolic disease risk, and such behaviors should of course be encouraged and promoted during COVID-19. However, even under normal circumstances, the difficulty in promoting healthy physical activity habits are well documented [69]. The chances of maintaining or improving exercise levels during the COVID-19 pandemic is now even more challenging, which is especially true for those segments of the population that are most physically and financially vulnerable. Considering a socioecological model of behavior change in which determinants of behavior change are considered at multiple levels (e.g., individual, environment, and policy), we posit that reducing sedentary behavior is a particularly important behavioral target. Reducing sedentary behavior is a simple strategy that may be more amenable to change compared to increasing exercise, which relies to a greater extent on higher-level environmental and policy-related determinants. Simple, enjoyable low-intensity sedentary behavior interruption strategies should be encouraged by policymakers, health care providers, academic institutions, and other work, social, and family networks to reduce sedentary behavior and promote health in the face of COVID-19.
Funding: None.
Conflicts of Interest: All authors declare that they have no conflicts of interest.
References
- 1. Sohrabi C, Alsafi Z, O’Neill N, et al. . World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19). Int J Surg. 2020;76(April):71–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. COVID-19 Map. Johns Hopkins Coronavirus Resource Center [Internet]. Available at https://coronavirus.jhu.edu/map.html. Accessibility verified May 25, 2020.
- 3. Cheval B, Sivaramakrishnan H, Maltagliati S, et al. (2020) Relationships between changes in self-reported physical activity and sedentary behaviours and health during the coronavirus (COVID-19) pandemic in France and Switzerland, SportRxiv, doi: 10.31236/osf/io/ydv84, 25 April 2020, preprint: not peer reviewed. [DOI] [PubMed]
- 4. Hall G, Laddu DR, Phillips SA, Lavie CJ, Arena R. A tale of two pandemics: How will COVID-19 and global trends in physical inactivity and sedentary behavior affect one another? Prog Cardiovasc Dis. 2020; doi: 10.1016/j.pcad.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Chow N, Fleming-Dutra K, Gierke R, et al. . Preliminary estimates of the prevalence of selected underlying health conditions among patients with coronavirus disease 2019—United States, February 12–March 28, 2020. Morb Mortal Wkly Rep. 2020;69(13):382–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Jiménez-Pavón D, Carbonell-Baeza A, Lavie CJ. Physical exercise as therapy to fight against the mental and physical consequences of COVID-19 quarantine: Special focus in older people. Prog Cardiovasc Dis. 2020;63(3):386–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Middleton KR, Anton SD, Perri MG. Long-term adherence to health behavior change. Am J Lifestyle Med. 2013;7(6):395–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Healthy Campus 2020. Ecological model [Internet]. Available online at https://www.acha.org/HealthyCampus/HealthyCampus/Ecological_Model.aspx. Accessibility verified August 10, 2019.
- 9. Harlow T. Pandemic fuels big increase in biking and walking across state Available online at https://www.startribune.com/covid-19-fuels-big-increase-in-biking-and-walking/569963482/. Accessibility verified July 23, 2020.
- 10. Peçanha T, Goessler KF, Roschel H, Gualano B. Social isolation during the COVID-19 pandemic can increase physical inactivity and the global burden of cardiovascular disease. Am J Physiol Heart Circ Physiol. 2020;318(6):H1441–H1446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. CDC. COVID-19 employer information for office buildings [Internet] Available online at https://www.cdc.gov/coronavirus/2019-ncov/community/office-buildings.html. Accessibility verified August 19, 2020.
- 12. City of Rehoboth. City removing benches due to COVID-19 threat [Internet] Available online at https://www.cityofrehoboth.com/news/general/city-removing-benches-due-covid-19-threat. Accessibility verified August 19, 2020.
- 13. Pampel FC, Krueger PM, Denney JT. Socioeconomic disparities in health behaviors. Annu Rev Sociol. 2010;36(August):349–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Webb Hooper M, Nápoles AM, Pérez-Stable EJ. COVID-19 and racial/ethnic disparities. JAMA. 2020;323(24):2466–2467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hawkins D. Social determinants of COVID-19 in Massachusetts: An ecological study. J Prev Med Public Health. 2020;53(4)220–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wiemers EE, Abrahams S, AlFakhri M, Hotz VJ, Schoeni RF, Seltzer JA (2020) Disparities in vulnerability to severe complications from COVID-19 in the United States, medRxiv, doi: 10.1101/2020.05.28.20115899, preprint: not peer reviewed.. Available online at http://www.ncbi.nlm.nih.gov/pubmed/32511522. Accessibility verified August 16, 2020. [DOI]
- 17. Rozenfeld Y, Beam J, Maier H, et al. . A model of disparities: Risk factors associated with COVID-19 infection. Int J Equity Health. 2020;19(126) doi: 10.1186/s12939-020-01242-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Gibbs BB, Hergenroeder AL, Katzmarzyk PT, Lee IM, Jakicic JM. Definition, measurement, and health risks associated with sedentary behavior. Med Sci Sports Exerc. 2015;47(6):1295–1300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Matthews CE, George SM, Moore SC, et al. . Amount of time spent in sedentary behaviors and cause-specific mortality in US adults. Am J Clin Nutr. 2012;95(2):437–445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Young DR, Hivert MF, Alhassan S, et al. ; Physical Activity Committee of the Council on Lifestyle and Cardiometabolic Health; Council on Clinical Cardiology; Council on Epidemiology and Prevention; Council on Functional Genomics and Translational Biology; and Stroke Council Sedentary behavior and cardiovascular morbidity and mortality: A science advisory from the American Heart Association. Circulation. 2016;134(13):e262–e279. [DOI] [PubMed] [Google Scholar]
- 21. TMA Chart Shows COVID-19 Risks for Various Activities [Internet] Available online at https://www.texmed.org/TexasMedicineDetail.aspx?Pageid=46106&id=54216. Accessibility verified August 18, 2020.
- 22. Mainsbridge CP, Cooley D, Dawkins S, et al. . Taking a stand for office-based workers’ mental health: The return of the microbreak. Front Public Health. 2020;8(June):215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Cho MJ, Bunsawat K, Kim HJ, Yoon ES, Jae SY. The acute effects of interrupting prolonged sitting with stair climbing on vascular and metabolic function after a high-fat meal. Eur J Appl Physiol. 2020;120(4):829–839. [DOI] [PubMed] [Google Scholar]
- 24. Clemes SA, Barber SE, Bingham DD, et al. . Reducing children’s classroom sitting time using sit-to-stand desks: Findings from pilot studies in UK and Australian primary schools. J Public Health (Oxf). 2016;38(3):526–533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Belcher BR, Berrigan D, Papachristopoulou A, et al. . Effects of interrupting children’s sedentary behaviors with activity on metabolic function: A randomized trial. J Clin Endocrinol Metab. 2015;100(10):3735–3743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Liu M, Wu L, Yao S. Dose-response association of screen time-based sedentary behaviour in children and adolescents and depression: A meta-analysis of observational studies. Br J Sports Med. 2016;50(20):1252–1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. de Rezende LFM, Rodrigues Lopes M, Rey-López JP, Matsudo VKR, Luiz O do C. Sedentary behavior and health outcomes: An overview of systematic reviews. PLoS One. 2014;9(8):e105620–e105620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Jakobsson J, Malm C, Furberg M, Ekelund U, Svensson M. Physical activity during the coronavirus (COVID-19) pandemic: Prevention of a decline in metabolic and immunological functions. Front Sport Act Living. 2020;2(April):57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ricci F, Izzicupo P, Moscucci F, et al. . Recommendations for physical inactivity and sedentary behavior during the coronavirus disease (COVID-19) pandemic. Front Public Health. 2020;8(May):199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Dunton GF, Do B, Wang SD. Early effects of the COVID-19 pandemic on physical activity and sedentary behavior in children living in the U.S. BMC Public Health. 2020;20(1):1351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Lippi G, Henry BM, Bovo C, Sanchis-Gomar F. Health risks and potential remedies during prolonged lockdowns for coronavirus disease 2019 (COVID-19). Diagnosis (Berl). 2020;7(2):85–90. [DOI] [PubMed] [Google Scholar]
- 32. Lippi G, Henry BM, Sanchis-Gomar F. Physical inactivity and cardiovascular disease at the time of coronavirus disease 2019 (COVID-19). Eur J Prev Cardiol. 2020;27(9):906–908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Schuch FB, Bulzing RA, Meyer J, et al. . Associations of moderate to vigorous physical activity and sedentary behavior with depressive and anxiety symptoms in self-isolating people during the COVID-19 pandemic: A cross-sectional survey in Brazil. Psychiatry Res. 2020;292(October):113339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Xiong TY, Redwood S, Prendergast B, Chen M. Coronaviruses and the cardiovascular system: Acute and long-term implications. Eur Heart J. 2020;41(19):1798–1800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. King AJ, Burke LM, Halson SL, Hawley JA. The challenge of maintaining metabolic health during a global pandemic. Sports Med. 2020;50(7):1233–1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Patel AV, Bernstein L, Deka A, et al. . Leisure time spent sitting in relation to total mortality in a prospective cohort of US adults. Am J Epidemiol. 2010;172(4):419–429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Dempsey PC, Owen N, Biddle SJ, Dunstan DW. Managing sedentary behavior to reduce the risk of diabetes and cardiovascular disease. Curr Diab Rep. 2014;14(9):522. [DOI] [PubMed] [Google Scholar]
- 38. Carter S, Hartman Y, Holder S, Thijssen DH, Hopkins ND. Sedentary behavior and cardiovascular disease risk: Mediating mechanisms. Exerc Sport Sci Rev. 2017;45(2):80–86. [DOI] [PubMed] [Google Scholar]
- 39. Emami A, Javanmardi F, Pirbonyeh N, Akbari A. Prevalence of underlying diseases in hospitalized patients with COVID-19: A systematic review and meta-analysis. Arch Acad Emerg Med. 2020;8(1):e35. [PMC free article] [PubMed] [Google Scholar]
- 40. Dietz W, Santos-Burgoa C. Obesity and its implications for COVID-19 mortality. Obesity (Silver Spring). 2020;28(6):1005. [DOI] [PubMed] [Google Scholar]
- 41. Garg S, Kim L, Whitaker M, et al. . Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019. MMWR Morbid Mortal Wkly Rep. 2020;69(15):458–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Zhai L, Zhang Y, Zhang D. Sedentary behaviour and the risk of depression: A meta-analysis. Br J Sports Med. 2015;49(11):705–709. [DOI] [PubMed] [Google Scholar]
- 43. Dėdelė A, Miškinytė A, Andrušaitytė S, Bartkutė Ž. Perceived stress among different occupational groups and the interaction with sedentary behaviour. Int J Environ Res Public Health. 2019;16(23): 4595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Hallgren M, Nguyen TTD, Owen N, et al. . Associations of interruptions to leisure-time sedentary behaviour with symptoms of depression and anxiety. Transl Psychiatry. 2020;10(1):128. doi: 10.1136/bjsports-2013-093613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Hallgren M, Nguyen TT, Owen N, et al. . Associations of sedentary behavior in leisure and occupational contexts with symptoms of depression and anxiety. Prev Med. 2020;133(January):106021. [DOI] [PubMed] [Google Scholar]
- 46. Brooks SK, Webster RK, Smith LE, et al. . The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet. 2020;395(10227):912–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Holmes EA, O’Connor RC, Perry VH, et al. . Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. Lancet Psychiatry. 2020;7(6):547–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Burtscher J, Burtscher M, Millet GP. (Indoor) isolation, stress and physical inactivity: Vicious circles accelerated by Covid-19? Scand J Med Sci Sports. 2020;30(8):1544–1545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Pfefferbaum B, North CS. Mental health and the Covid-19 pandemic. N Engl J Med. 2020;383(6):510–512. [DOI] [PubMed] [Google Scholar]
- 50. Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. Gen Psychiatr. 2020;33(2):e100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Wang C, Pan R, Wan X, et al. . Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17(5):1729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Zhang SX, Wang Y, Rauch A, Wei F. Unprecedented disruption of lives and work: Health, distress and life satisfaction of working adults in China one month into the COVID-19 outbreak. Psychiatry Res. 2020;288(June):112958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Cameron AJ, Magliano DJ, Dunstan DW, et al. . A bi-directional relationship between obesity and health-related quality of life: Evidence from the longitudinal AusDiab study. Int J Obes (Lond). 2012;36(2):295–303. [DOI] [PubMed] [Google Scholar]
- 54. Black PH, Garbutt LD. Stress, inflammation and cardiovascular disease. J Psychosom Res. 2002;52(1):1–23. [DOI] [PubMed] [Google Scholar]
- 55. Paterson C, Fryer S, Zieff G, et al. . The effects of acute exposure to prolonged sitting, with and without interruption, on vascular function among adults: A meta-analysis. Sport Med. 2020; doi: 10.1007/s40279-020-01325-5. [DOI] [PubMed] [Google Scholar]
- 56. Morishima T, Restaino RM, Walsh LK, Kanaley JA, Padilla J. Prior exercise and standing as strategies to circumvent sitting-induced leg endothelial dysfunction. Clin Sci. 2018;131:1045–1053. [DOI] [PMC free article] [PubMed]
- 57. Barone Gibbs B, Kowalsky RJ, Perdomo SJ, Taormina JM, Balzer JR, Jakicic JM. Effect of alternating standing and sitting on blood pressure and pulse wave velocity during a simulated workday in adults with overweight/obesity obesity. J Hypertens. 2017;35:2411–2418. [DOI] [PubMed] [Google Scholar]
- 58. COH-FIT. Collaborative outcomes study on health and functioning during infection times [Internet] Available online at https://www.coh-fit.com/. Accessibility verified August 18, 2020.
- 59. Diaz J. Cities close streets to cars, opening space for social distancing [Internet]. Available from: https://www.nytimes.com/2020/04/11/us/coronavirus-street-closures.html. Accessibility verified July 10, 2020.
- 60. Hammond RA, Levine R. The economic impact of obesity in the United States. Diabetes Metab Syndr Obes. 2010;3(August):285–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Ding D, Lawson KD, Kolbe-Alexander TL, et al. ; Lancet Physical Activity Series 2 Executive Committee The economic burden of physical inactivity: A global analysis of major non-communicable diseases. Lancet. 2016;388(10051):1311–1324. [DOI] [PubMed] [Google Scholar]
- 62. Roberts LM, Jaeger BC, Baptista LC, et al. . Wearable technology to reduce sedentary behavior and CVD risk in older adults: A pilot randomized clinical trial. Clin Interv Aging. 2019;14(October):1817–1828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. O’keeffe N, Scheid JL, West SL. Sedentary behavior and the use of wearable technology: An editorial. Int J Environ Res Public Health. 2020; 17(12):4181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Berninger NM, Ten Hoor GA, Plasqui G, Kok G, Peters GY, Ruiter RAC. Sedentary work in desk-dominated environments: A data-driven intervention using intervention mapping. JMIR Form Res. 2020;4(7):e14951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Bice MR, Ball JW, McClaran S. Technology and physical activity motivation. Int J Sport Exerc Psychol. 2016;14(4):295–304. [Google Scholar]
- 66. Schwarzer R. Modeling health behavior change: How to predict and modify the adoption and maintenance of health behaviors. Appl Psychol. 2008;57(1):1–29. [Google Scholar]
- 67. Burnet K, Kelsch E, Zieff G, Moore JB, Stoner L. How fitting is F.I.T.T.?: A perspective on a transition from the sole use of frequency, intensity, time, and type in exercise prescription. Physiol Behav. 2019;199(February):33–34. [DOI] [PubMed] [Google Scholar]
- 68. Madjid M, Safavi-Naeini P, Solomon SD, Vardeny O. Potential effects of 1coronaviruses on the cardiovascular system: A review. JAMA Cardiol. 2020;5(7):831–840. [DOI] [PubMed] [Google Scholar]
- 69. Peters GJ, de Bruin M, Crutzen R. Everything should be as simple as possible, but no simpler: Towards a protocol for accumulating evidence regarding the active content of health behaviour change interventions. Health Psychol Rev. 2015;9(1):1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]